Abstract
Intestinal obstructions, that impede or block peristaltic movement, can be caused by abdominal adhesions and most gastrointestinal (GI) diseases including tumorous growths. However, the cellular remodeling mechanisms involved in, and caused by, intestinal obstructions are poorly understood. Several animal models of intestinal obstructions have been developed, but the mouse model is the most cost/time effective. The mouse model uses the surgical implantation of an intestinal partial obstruction (PO) that has a high mortality rate if it is not performed correctly. In addition, mice receiving PO surgery fail to develop hypertrophy if an appropriate blockade is not used or not properly placed. Here, we describe a detailed protocol for PO surgery which produces reliable and reproducible intestinal obstructions with a very low mortality rate. This protocol utilizes a surgically placed silicone ring that surrounds the ileum which partially blocks digestive movement in the small intestine. The partial blockage makes the intestine become dilated due to the halt of digestive movement. The dilation of the intestine induces smooth muscle hypertrophy on the oral side of the ring that progressively develops over 2 weeks until it causes death. The surgical PO mouse model offers an in vivo model of hypertrophic intestinal tissue useful for studying pathological changes of intestinal cells including smooth muscle cells (SMC), interstitial cells of Cajal (ICC), PDGFRα+, and neuronal cells during the development of intestinal obstruction.
Keywords: Physiology, Issue 133, Gastrointestinal tract, smooth muscle, partial obstruction, hypertrophy, interstitial cells of Cajal, platelet-derived growth factor receptor A
Introduction
Intestinal obstructions are a partial or complete blockage in the small or large intestine which prevents digested food, fluids, and gas from moving through the intestines1. Due to the obstruction, the blockage induces the intestinal walls to become thickened, narrowing the lumen2. Intestinal obstruction can occur as a result of abdominal or pelvic surgeries that cause abdominal adhesion tissue formation or from GI disorders such as inflammatory bowel diseases (Crohn's disease), diverticulitis, hernias, volvulus, stricture, intussusception, constipation, fecal impaction, pseudo-obstruction, cancers and tumors3,4,5. Intestinal obstructions in these cases often lead to the hypertrophy of the tunica muscularis of the intestine6.
PO of the lumen induces intestinal distention, and increases smooth muscle layer thickness around the obstruction in response to the need to continue functional peristalsis7,8,9,10,11,12,13. Animal models of intestinal PO have been developed to study smooth muscle hypertrophy in mice7, rats10, guinea pigs11, dogs12, and cats13 that consistently develop similar hypertrophy within the intestinal muscle layers.
A mouse model of intestinal PO is the most cost effective way to generate and study intestinal obstructions in vivo. Small intestine obstructions are carried out in mice by using a silicone ring surgically placed surrounding the ileum. The PO mice showed an early increase in the number of cells (hyperplasia), and an increase in muscle layer thickness (hypertrophy) after PO surgery8,15. SMC are the primary plastic cells that are growing within smooth muscle layers in response to the hypertrophic conditions14, but other cells such as ICC and PDGFRα+ cells that are closely associated with SMC, are also repopulated. We have previously reported that the PO mice develop hypertrophy in the small intestine, in which SMC are dedifferentiated into PDGFRα+ cells that are highly proliferative7,15,16. Conversely, ICC are degenerated and lost within the hypertrophied smooth muscle layers during the development of intestinal obsruction7. Another major benefit of the PO model is its capacity to induce changes in the enteric nervous system and propagating neurogenic motor patterns. The major propagating neurogenic motor pattern in the mouse small bowel is the migrating motor complex (MMC), which is neurogenic and does not require ICC or electrical slow waves17. The PO model can provide clear insights into how MMCs and enteric nerves are remodeled by partial obstruction.
Here, we propose a murine protocol for intestinal PO surgery using a silicone ring. Mice receiving PO surgery reliably produce hypertrophy in the tunica muscularis of the small intestine. Within hypertrophic muscle, SMC, ICC, PDGFRα+, and neuronal cells are dramatically remodeled.
Protocol
The following protocol has been approved by the Institutional Animal Care and Use Committee (IACUC) at the University of Nevada-Reno (UNR) Animal Resources and complies with all institutional ethical guidelines regarding the use of research animals.
1. Animals.
Obtain mature (4-6 weeks old) C57BL/6 mice weighing between 20-30 g. House the colony of laboratory mice in a centralized animal facility at UNR Animal Resources.
2. Partial Obstruction Surgery
NOTE: Surgeries are performed in a room dedicated to surgical procedures. All surgical instruments are autoclaved prior to surgery. Sterile surgical gowns and gloves should be worn by all personnel in the surgical room at all times.
- Preparation for the surgical mouse
- Check the anesthetic delivery system to ensure the supply of oxygen and isoflurane is adequate for procedure. Turn on the supply oxygen. Turn on the gas flowmeter and adjust it to 500-1000 mL/min. Place the animal in the induction chamber and seal the top.
- Turn on the isoflurane vaporizer to 5%, and monitor the animal until it becomes recumbent. Switch the anesthetic delivery system to the nose cone.
- Flush the induction chamber of any residual gas with oxygen, then turn off the induction chamber line while keeping the nose cone line open.
- Remove the animal from the chamber and carefully place ophthalmic ointment on the eyes of the animal.
- Place the nose cone on a preheated warm pad when gas continues to flow.
- Change the oxygen flow to 100-200 mL/min, with 2-3 % isoflurane. If the animal begins to move, gentlyrestrain the animal with the nose cone on until fully anesthetized again.
- Monitor the respiration and response to stimulation during the procedure and adjust the percentage of isoflurane (2-5 %) as needed. Animal anesthetization level is monitored by the lack of toe pinch reflex before surgery is performed.
- Inject pain medicine (buprenorphine, 1 µg/g of body weight) intraperitoneally away from the incision site.
- Apply hair removal lotion on the abdomen using a clean cotton swab. Let the lotion sit for 3-5 min on mouse, then remove the hair using gauze and cotton swabs. Repeat this step until all hair has been removed from the abdomen of the mouse.
- Clean the skin with 70 % ethanol using gauze and cotton swabs. Apply swabsticks or povidone-iodine solution to clean the abdomen.
- Partial obstruction surgery
- Drape the surgical site using 25 x 50 cm sterile paper with a 2.5 x 2.5 cm opening in the middle for the surgery area. Secure the drape to the animal by placing sterile strips at the boundaries of the opening and skin.
- Make a ~3.0 cm abdominal incision longitudinally using a No. 15 blade scalpel, ensuring that only the skin is incised and avoiding cutting into the musculoperitoneal layer at this time.
- Using forceps and surgical scissors, carefully separate the skin from the musculoperitoneal layer without causing any incision to the musculoperitoneal layer. After the layers have been sufficiently separated (approximately 1 cm x 4 cm), identify the linea alba on the musculoperitoneal layer and cut ~2 cm along the linea alba to expose the intraperitoneal cavity using micro-forceps and scissors.
- Carefully locate and identify the cecum. Slowly and gently remove the cecum from the intraperitoneal cavity with micro-forceps, bringing the proximal colon and ileum with the cecum outside onto the sterile drape. Immediately moisten the intestinal tissue with 0.9 % sterile saline soaked gauze and keep exposed tissue moistened at all times while they are outside of the abdominal cavity.
- Locate and identify the mesentery between the ileum and proximal colon. Make an incision (~1 cm) parallel to, and just below, the ileum, in the mesentery and avoid cutting any vasculature.
- Take an autoclaved silicone ring (6 mm in length, 4 mm exterior diameter, 3.5 mm interior diameter). Cut longitudinally to open the tubing and open the ring with micro-forceps.
- Insert one end of the opened ring through the incision in the mesentery tissue. Return the ring to a completed ring shape by bringing one end into contact with another, with the ileum surrounded by the ring.
- Ensure that the silicone ring completely surrounds the ileum, close the ring with suture and carefully place the intestines back in the intraperitoneal cavity.
- Surgery closure
- Perform a simple continuous suture on the musculoperitoneal layer along the linea alba to close the musculoperitoneal wound with an absorbable suture. After the suture is complete, clean any bleeding with 0.9 % sterile saline soaked gauze.
- To completely close the wound, with a separate nylon suture, perform a simple continuous suture on the skin.
- After both sutures have been completed, clean the wound with new swabstick or povidone-iodine.
- Intraperitoneally inject antibiotics (gentamicin, 150 μL per mouse based on 20-30 g body weight).
- After the completion of procedure, turn off the isoflurane vaporizer and allow the animal to breathe only flowing oxygen until it start gaining consciousness.
- Once the animal is awake, place the animal into a separate recovery area with thermal support until fully recovered.
3. Post-operation observation.
After the completion of surgery, move the animals to an incubator in a recovery room where temperature and humidity is regulated. Monitor the animals postoperatively every 15 min for the first hour then every 30 min for the second hour while the animals are in the incubator.
As soon as the prescribed observation is complete, move the animals to their own individual cage and monitor them daily for clinical indications of pain18, and to ensure that the surgical wound is healing properly without any signs of complications (dehiscence) present.
Representative Results
Partial obstruction (PO) was surgically induced in one month old mice by placing a silicone ring around the ileum close to the ileocecal sphincter. This ring created a partial blockage in the ileum. Sham operations (SO) were also performed without a ring on age/sex matched mice and these mice did not show any symptoms similar to those found in PO mice. Mice quickly recovered from PO surgery within a few hours. They showed no obvious behavioral changes or weakness within the first week, but after the first week, they progressively began to show signs of PO: a distended abdomen and the production of fewer and smaller fecal pellets. PO mice were sacrificed at 8 and 13 days post-PO surgery along with SO control mice. The small intestine was partially filled and distended at 8 days post-PO surgery and fully filled and distended at 13 days post-PO surgery, compared to SO control mice (Figure 1A). Fecal pellet formation in the colon of 8 and 13 days post-PO surgery mice was reduced in comparison to SO control mice (Figure 1B). Ileal tissue that was just upstream of the ring was dissected and the smooth muscle was analyzed by hematoxylin & eosin (H&E) staining. The smooth muscle layer was hypertrophied at 8 days post-PO surgery and much further hypertrophied at 13 days post-PO surgery (Figure 2). We also observed changes in SMC, ICC, PDGFRα+, and neuronal cells within the tunica muscularis in PO mice through the use of immunochemistry. Each cell was labeled with cell-type specific markers: MYH11 (SMC), KIT (ICC), PDGFRA (PDGFRα+ cells), and PGP9.5 (neuronal cells). SMC are found within three layers of tissue: longitudinal muscle (LM), circular muscle (CM), and the muscularis mucosae (MM) in the ileum. SMC were progressively growing at rapid rates in all three layers at 8 and 13 days post-PO surgery (Figure 3). As for ICCs, their subpopulations are located in the deep muscular plexus (DMP), myenteric region (MY), and subserosal region (SS). However, ICC-DMP, ICC-MY, and ICC-SS were degenerated within the intra/intermuscular layers (Figure 3). Similar to ICC subpopulations, subpopulations of PDGFRα+ cells (PαC) are located in the DMP, MY, and SS. In PO mice, PαC-DMP, PαC-MY, and PαC-SS were dynamically remodeled within the intermuscular layers of PO mice: they were growing at 8 days post-PO surgery and degenerated at 13 days post-PO surgery (Figure 3). Finally, myenteric plexus (MP), submucosal plexus (SP), subserosal neurons (SS), and enteric motor neurons (EMN) were significantly lost in the inter/intramuscular regions of PO mice at 8 and 13 days post-PO surgery (Figure 3).
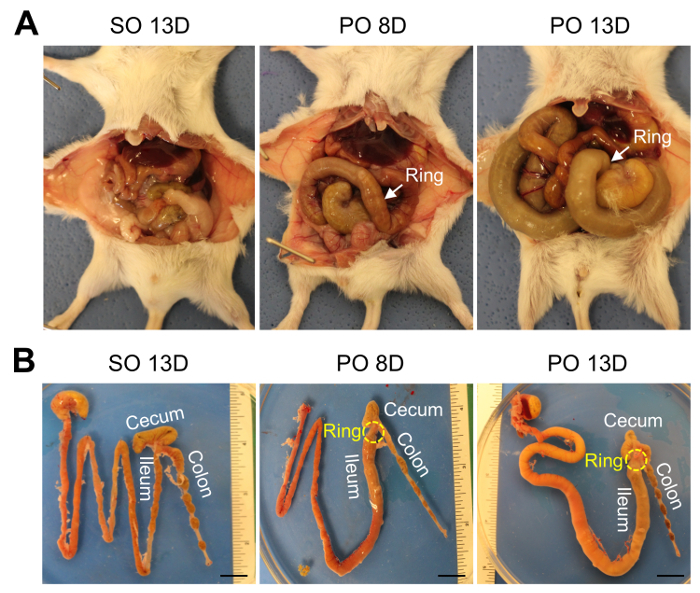
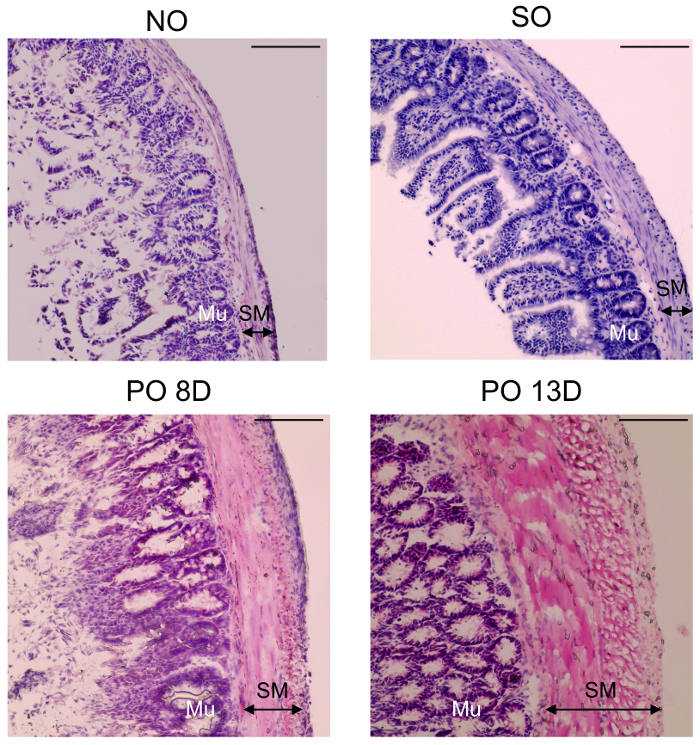
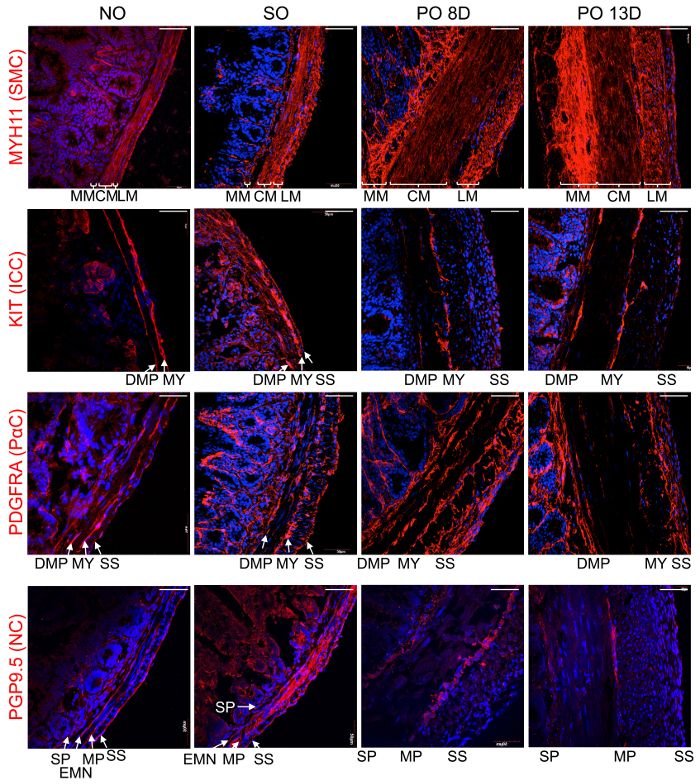
Figure 1. Intestinal partial obstruction surgically induced in a mouse model. PO was induced by PO surgery. One month old mice were anesthetized, their abdomen was opened by an incision, a silicone ring was placed surrounding the ileum, and the opening was closed by suturing. Mice that underwent surgery were allowed to recover for either 8 or 13 days. Age and sex matched SO mice were operated on in the same manner as PO mice except there was no placement of a ring. (A) Gross images of the GI tract in mice that underwent PO or SO surgery. Images are of mice at 8 and 13 days post-surgery (B) GI tract dissected from mice in A. Small intestine upstream of the ring was distended at both 8 and 13 days post-PO surgery and fecal pellets in the colon were also smaller at both 8 and 13 day post-PO surgery as compared to 13 days post-SO surgery mice due to the partially obstructive silicone ring. Scale bars are 0.5 cm. Please click here to view a larger version of this figure.
Figure 2. Smooth muscle layer changed in the surgical mouse model. Representative H&E staining of ileal cross sections from intestinal PO, SO and no operation (NO) mice. Smooth muscle (SM) and mucosa (Mu) layers are thicker in PO mice at 8 and 13 days post-PO surgery than those in SO and NO mice. Scale bars are 50 µm. Please click here to view a larger version of this figure.
Figure 3. Dynamic cellular remodeling in smooth muscle hypertrophy induced by intestinal partial obstruction. Representative confocal laser scanning images of hypertrophic ileal cross sections, from PO, SO and NO mice. Immunohistochemically staining with antibodies (red) of MYH11 (SMC), KIT (ICC), PDGFRA (PDGFRα+ cells) or PGP9.5 (NC; neuronal cells), co-stained with DAPI (blue). SMC in mucosa muscularis (MM), circular muscle (CM), and longitudinal muscle (LM) layers, as well as PDGFRα+ cells in deep muscular plexus (DMP), myenteric region (MY), and subserosal region (SS) were growing in hypertrophic ileum at 8 and 13 days post-PO surgery while ICC in DMP, MY, and SS, myenteric plexus (MP), submucosal plexus (SP), subserosal NC (SS), and enteric motor neurons (EMN) were degenerated. Scale bars are 50 µm. Please click here to view a larger version of this figure.
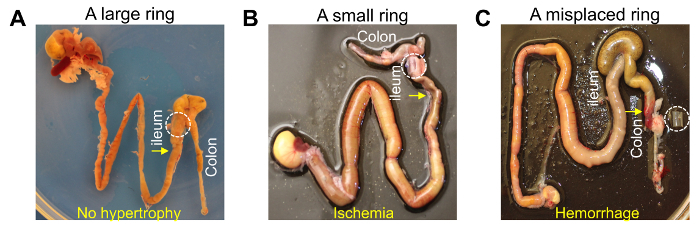
Figure 4. Results of silicone rings that are too large, too small or misplaced on the colon. (A) No smooth muscle hypertrophy develops in the ileum if the ring is too large to cause obstruction. The ring made little to no blockage of the ileum. (B) Intestinal ischemia develops in the ileum if the ring is too small. The ring made an almost complete blockage of the ileum, which can damage the tissue and lead to early death before hypertrophy develops. (C) Smooth muscle hypertrophy developed in the colon due to a misplaced ring. The ring on the colon was moved down by lumenal content (feces), which damaged mesentery vasculature and caused massive hemorrhaging in the colon. Please click here to view a larger version of this figure.
Discussion
We demonstrated that mice receiving the intestinal PO surgery consistently and reproducibly develop intestinal smooth muscle hypertrophy, which mimics human intestinal obstruction. Intestinal obstruction surgeries have been developed for different animals including mice7, rats10, guinea pigs11, dog12 and cats13. The mouse model of intestinal obstruction has time, cost, size, and phenotypic advantages over other larger animal models. The development of hypertrophy in mice or rats takes only 10-14 days10, compared to 2-4 weeks in guinea pigs, dogs and cats11,12,13. Cost for purchasing and maintaining mice is also a tremendous financial advantage when compared to other models. Additionally, mice are small and easy to handle for the PO surgery. Most importantly, mice receiving PO surgery progressively and extensively develop hypertrophy in the small intestine while other larger animals develop less extensive growth.
There are several key factors to consider when attempting to produce reliable hypertrophy through intestinal PO surgery. Several research groups have used rings of various sizes and placed a ring at various locations along the intestine to create partial obstructions7,9,10,11,12,13,14. However, a silicone ring of optimal size should be used for mice as a larger ring creates little or no blockage in the ileum where hypertrophy only partially, or never, developed (Figure 4A). Conversely, when a ring was too small, it created near complete blockage of the ileum which induced intestinal ischemia and/or damaged the mucosa causing sepsis, leading to early death within a week (Figure 4B). We used a silicone ring of a specific size (6 mm in length, 4 mm exterior diameter, 3.5 mm interior diameter) on one month old mice (Table of Materials). Different sizes of the rings should be tested and used for mice of different sizes in order to create the optimal blockage in the ileum. Another key factor is the location of the ring on the intestine. The ileum, close to ileocecal valve, is the best place to place the ring in order to robustly produce partial obstructions. Other regions, such as the jejunum or different regions of the ileum away from ileocecal valve, have had a similar ring placed on them in order to induce hypertrophy7. However, due to the serosal surface of the intestine being highly lubricated by peritoneal fluid, a ring placed on these parts of the intestine easily moves because of the contractile force of intestine pushing fecal material through. As the ring is pushed down the length of the intestine, it cuts off mesenteric arteries innervated into the myenteric region of intestine, causing hemorrhaging. When a ring is inserted at the end of ileum next to ileocecal valve, it is physically prevented from moving further by the bulky nature of the cecum. The cecum can be easily located and taken out of the abdomen in the surgery in order to locate the ileocecal valve region as the cecum connects to both the ileum and proximal colon. The ileum and colon connected at the cecum look quite similar and a ring can accidentally be placed on the proximal colon instead of the ileum. When a ring was misplaced on the proximal colon, as also seen on the jejunum, the ring was pushed downward and damaged mesenteric arteries, causing extensive hemorrhaging (Figure 4C). To avoid this misplacement, the ileum should always be properly located and identified before the ring is put into place. The ileum runs into the middle of cecum while the colon runs into one side of the cecum pouch.
This PO surgery protocol is considered as a major surgery for mice. All surgical instruments and materials should be sterilized before use, and surgery should be performed in the clean environment of a dedicated surgery room in order to minimize contamination, which can lead to infection and inflammation in mice. In addition, a pain medication should be provided to mice after surgery. We chose to use a slow release version of buprenorphine, which is efficacious up to 7-8 h22. Furthermore, after surgery, mice have difficulty chewing and swallowing solid food. For up to 5 days post-surgery, the mice should be provided with softened food (solid diet with a bit of water added to soften food) and switched to normal solid diet after 5 days.
Our intestinal PO surgery provides an in vivo hypertrophy model for intestinal obstruction in which SMC, ICC, and PDGFRα+ cells are abnormally remodeled. This PO model is also ideally suited to understanding how enteric neurons are modified by PO and how the major motor activities are affected in the small and large bowel23. These cells can be dynamically remodeled in pathological conditions as well as under cultured conditions15,16. We observed that these cells in SO mice behaved a bit differently than normal mice without operation (Figure 2 and Figure 3). Most intestinal obstruction in humans occurs by abdominal adhesions developed after surgery, leading to smooth muscle hypertrophy3,4,5,21. After SO surgery, we also found that SMC, ICC, and PDGFRα+ cells were slightly hypertrophic in the small intestine, compared to NO (Figure 3), suggesting that surgery itself can induce intestinal smooth muscle hypertrophy. If this is the case, SO surgery is not a complete negative control for PO surgery. NO as well as SO should be used as a comparison to PO intestine.
In summary, we have found a cost/time effective, reliable, and repeatable PO surgical protocol in mice that robustly generates intestinal obstructions. During the development of the obstruction, SMC, ICC, PDGFRα+, as well as neuronal cells are dynamically remodeled within various tissue layers and locales. This in vivo obstruction model offers new insights into our knowledge of how phenotypic changes occur in obstructed intestine at the cellular level.
Disclosures
The authors have nothing to disclose.
Acknowledgments
The authors would like to thank Benjamin J Weigler, D.V.M., Ph.D. and Walt Mandeville, D.V.M. (Animal Resources & Campus Attending Veterinarian, University of Nevada, Reno) for their excellent animal services provided to the mice as well as their counsel on surgical procedures.
References
- Millat B, Guillon F. Physiopathology and principles of intensive care in intestinal obstructions. Rev Prat. 1993;43:667–672. [PubMed] [Google Scholar]
- Tonelli P. New developments in Crohn's disease: solution of doctrinal mysteries and reinstatement as a surgically treatable disease. 1. The process is not a form of enteritis but lymphedema contaminated by intestinal contents. Chir Ital. 2000;52:109–121. [PubMed] [Google Scholar]
- Limsrivilai J. Meta-analytic Bayesian model for differentiating intestinal tuberculosis from Crohn's disease. Am J Gastroenterol. 2017;112:415–427. doi: 10.1038/ajg.2016.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dvorak D, Adamova Z, Bar T, Slovacek R. Internal hernia as a cause of small bowel obstruction. Rozhl Chir. 2017;96:34–36. [PubMed] [Google Scholar]
- Massani M, Capovilla G, Ruffolo C, Bassi N. Gastrointestinal stromal tumour (GIST) presenting as a strangulated inguinal hernia with small bowel obstruction. BMJ Case Rep. 2007. [DOI] [PMC free article] [PubMed]
- Chen J, Chen H, Sanders M, Perrino BA. Regulation of SRF/CArG-dependent gene transcription during chronic partial obstruction of murine small intestine. Neurogastroenterol Motil. 2008;20:829–842. doi: 10.1111/j.1365-2982.2008.01149.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang IY, et al. Loss of interstitial cells of Cajal and development of electrical dysfunction in murine small bowel obstruction. J Physiol. 2001;536(Pt 2):555–568. doi: 10.1111/j.1469-7793.2001.0555c.xd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu DH, et al. Voltage dependent potassium channel remodeling in murine intestinal smooth muscle hypertrophy induced by partial obstruction. PLoS One. 2014;9(2):e86109. doi: 10.1371/journal.pone.0086109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo X, et al. Down-regulation of hydrogen sulfide biosynthesis accompanies murine interstitial cells of Cajal dysfunction in partial ileal obstruction. PLoS One. 2012;7:e48249. doi: 10.1371/journal.pone.0048249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J, Zhao J, Chen P, Nakaguchi T, Grundy D, Gregersen H. Interdependency between mechanical parameters and afferent nerve discharge in hypertrophic intestine of rats. Am J Physiol-Gastr L. 2016;310:G376–G386. doi: 10.1152/ajpgi.00192.2015. [DOI] [PubMed] [Google Scholar]
- Zhao J, Liao D, Yang J, Gregersen H. Biomechanical remodeling of obstructed guinea pig jejunum. J Biomech. 2010;43:1322–1329. doi: 10.1016/j.jbiomech.2010.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen EJ, et al. Duodenal Brunner's glade adenoma causing chronic small intestinal obstruction in a dog. J Small Anim Pract. 2012;53:136–139. doi: 10.1111/j.1748-5827.2011.01153.x. [DOI] [PubMed] [Google Scholar]
- Bettini G, et al. Hypertrophy of intestinal smooth muscle in cats. Res Vet Sci. 2003;75:43–53. doi: 10.1016/s0034-5288(03)00041-9. [DOI] [PubMed] [Google Scholar]
- Macdonald JA. Smooth muscle phenotypic plasticity in mechanical obstruction of the small intestine. J Neurogastroenterol Motil. 2008;20:737–740. doi: 10.1111/j.1365-2982.2008.01148.x. [DOI] [PubMed] [Google Scholar]
- Ha SE, et al. Transcriptome analysis of PDGFRα+ Cells identifies T-types Ca2+ channel CACNA1G as a new pathological marker for PDGFRα+ cell hyperplasia. PLoS One. 2017;12:e0182265. doi: 10.1371/journal.pone.0182265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park C, et al. Serum response factor is essential for prenatal gastrointestinal smooth muscle development and maintenance of differentiated phenotype. J Neurogastroenterol Motil. 2015;21:589–602. doi: 10.5056/jnm15063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer NJ, Sanders KM, Smith TK. Migrating motor complexes do not require electrical slow waves in the mouse small intestine. J Physiol. 2003;553:881–893. doi: 10.1113/jphysiol.2003.049700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langford DJ, et al. Coding of facial expressions of pain in the laboratory mouse. Nat Methods. 2010;7:447–449. doi: 10.1038/nmeth.1455. [DOI] [PubMed] [Google Scholar]
- Terez SD, Notari L, Sun R, Zhao A. Mechanisms of smooth muscle responses to inflammation. Neurogastroenterol Motil. 2012;24:802–811. doi: 10.1111/j.1365-2982.2012.01986.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, et al. Smooth muscle hyperplasia/hypertrophy is the most prominent histological change in Crohn's fibrostenosing bowel strictures: A semiquantitative analysis by using a novel histological grading scheme. J Crohns Colitis. 2017;11:92–104. doi: 10.1093/ecco-jcc/jjw126. [DOI] [PubMed] [Google Scholar]
- Huizinga JD, Chen JH. Interstitial Cells of Cajal: Update on Basic and Clinical Science. Curr Gastroenterol Rep. 2014;16:363. doi: 10.1007/s11894-013-0363-z. [DOI] [PubMed] [Google Scholar]
- Jirkof P, Touvieille A, Cinelli P, Arras M. Buprenorphine for pain relief in mice: repeated injections vs sustained-release depot formulation. Lab Animal. 2015;49:177–187. doi: 10.1177/0023677214562849. [DOI] [PubMed] [Google Scholar]
- Spencer NJ, Dinning PJ, Brookes SJ, Costa M. Insights into the mechanisms underlying colonic motor patterns. J Physiol. 2016;594:4099–4116. doi: 10.1113/JP271919. [DOI] [PMC free article] [PubMed] [Google Scholar]


