Abstract
This protocol offers a detailed description of a psychophysiological experiment using script-driven trauma-related imagery and standardized clinical instruments within a comparative design assessing physiological and psychopathological features of individuals with BPD. This method aims at studying the psychological and physiological effects of trauma-related dissociation. Since the psychodiagnostic classification of trauma-related disorders relies on the observation of evolutionarily determined responses to life-threat, an integrated assessment paradigm for the study of reactions to traumatic memories proposes a very appropriate methodological approach.
The employed script-driven imagery paradigm uses individual recall instructions to activate trauma-related memory networks and prompt associated emotional and physiological responses. These responses are measured by means of self-rating scales and physiological assessments. During the individual recall, participants are asked to vividly imagine traumatic and everyday experiences and other situations triggered by short personalized verbal scripts they authored beforehand together with the experimenters. A wide range of affective reactions and different physiological parameters can be measured. We used this paradigm to investigate dissociative states in BPD and to find physiological and affective correlates of dissociative states. Some of the participants were having severe traumatic antecedents.
To investigate different reaction patterns within the same diagnostic group, participants with different levels of traumatic histories, symptom severities, and co-morbidities should be included. By using short verbal scripts, the level of stress induced to participants is held as low as possible without affecting the validity of the object of investigation.
Keywords: Behavior, Issue 133, Script-driven imagery, heart rate, skin conductance, clinical assessment, borderline personality disorder, psychological trauma, trauma-related dissociation
Introduction
In perceiving danger, humans experience anxiety and the body reacts rapidly within the defense cascade to minimize injury and ensure survival. Defense reactions include initial stages of increasing arousal and sympathetic activation and, in event of inescapable threats (e.g., child abuse, rape, torture), parasympathetically modulated "shut-down" dissociative reactions (e.g., bradycardia, vasodilatation, sensory deafferentation, alterations of consciousness and speech1,2) become predominant. According to the theories of reactivation of trauma-related associative memory networks3,4, the prevalent type of the peritraumatic psychophysiological reactions (arousal vs. dissociation) would result in one of the two major subtypes of clinical profiles and reaction patterns to trauma-related stimuli2. Considering the heterogeneity of responses to activation of trauma-related memory across various neuroimaging PTSD studies, Lanius et al. (2006)5 argued that "grouping all PTSD subjects, regardless of their different symptom patterns, in the same diagnostic category may interfere with our understanding of posttrauma psychopathology". The influence of dissociative responding on the psychopathology and psychophysiology of traumatized persons has been studied in the area of PTSD. For example, Schalinski, Elbert & Schauer (2011)6 showed that shut-down dissociation predicts PTSD and other comorbid disorders. The use of psychophysiological assessments pointed to modifications of the defense cascade allowing for a rapid flight in response to threat7,8. Schalinski et al. (2013)8 revealed that the type of traumatic events seems to influence the cardiac startle response. Another study9 indicated a pattern of "blunted" reactivity — an arousal-dissociation mix characterized by simultaneous activation of both autonomous nervous system branches — in more severely traumatized individuals. So far, no studies in this regard have been conducted on other clinical populations often affected by psychological trauma and dissociative symptoms (e.g., BPD).
In the research of human emotion and behavior, it is of particular importance to examine and integrate information from several levels: subjective (verbal expression, prosody), behavioral (motor, facial expression, etc.), physiological (trembling, sweating, heart rate, etc.). By arguing that assessments that omit one or more of these three modes of emotional expression can be highly misleading, Lang (1998)10 emphasized the relevance of multimodal assessment that involves procedures of observation of behavior, self-report/clinical measures, and psychophysiological measurement.
Extreme states of anxiety and pronounced physiological arousal are characteristic of anxiety, trauma-, and stressor-related disorders. According to the psychophysiological concept, these disorders may be conceived as an outcome of the modified autonomic reactivity (generally higher) to negative stimuli. These measurable psychophysiological response indices as part of the diagnostic criteria made them obvious targets for psychophysiological research. Particularly PTSD, as a psychological disorder with a definite event criterion (i.e., life-threatening experiences, such as accidents, physical/sexual assaults, natural disasters, incarceration, military combat, and torture), offered a valuable opportunity for psychophysiological assessments.
Various assessment designs using different paradigms, stimuli, and physiological parameters have been used for the study of PTSD. Monitoring peripheral physiological parameters provide reliable measures of changes in autonomic activity, related to emotional and cognitive states. Among these, skin conductance is a common measure with a long history in psychophysiological research and is regarded as a highly sensitive index11. Its monitoring is often combined with the recording of heart rate, a further autonomically dependent variable.
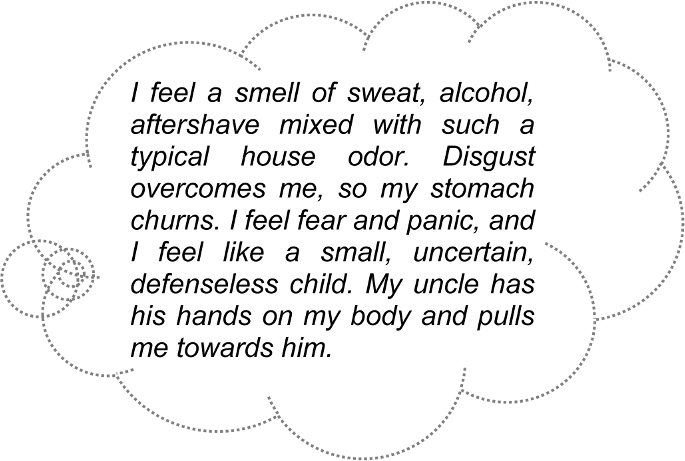
For the measurement of peripheral physiological parameters, the use of script-driven imagery experiments was a major paradigm for the investigation of emotional and physiological reactions to the activation of trauma-related memory. Within the script-driven imagery paradigm12, participants are asked to vividly imagine aversive situations triggered by short verbal scripts13,14,15,16. The subject is solicited to imagine a situation as if he/she was reliving the real course of events, including actions, persons, and emotions present during the real situation (see Figure 1 for an example of a traumatic script). The traumatic situation imagined is usually compared with other kinds of not-traumatic scenes.
Script-driven imagery was mainly employed in various populations affected by PTSD, e.g. Vietnam veterans15,17, victims of accidents18, and former political prisoners19. An enhanced reactivity to traumatic cues was usually found, but there are also several findings of absence of such a higher reactivity to trauma-related stimuli (e.g., Orr & Roth, 2000; Davis et al., 1996)15,20. Growing knowledge on the psychophysiology of PTSD was followed by an increased bulk of psychophysiological research in the area of trauma-related and other psychological disorders. Meanwhile, however, script-driven imagery paradigms have been successfully applied to study dissociative processes in BPD 21,22.
This paper presents a protocol to investigate whether persons with BPD reporting high levels of PD predominantly exhibit dissociative reactions with suppression of autonomic responses during the script-driven trauma-related imagery23,24. Additionally, our study aimed at proving whether there are clinically different BPD subgroups, as tested by structured clinical interviews and symptom scales. The present protocol combines extensive, standardized clinical assessments with measuring physiological (HR and SC) and subjective responses within a script-driven imagery paradigm. Reactions to trauma-related personalized scripts compared to scripts portraying everyday events were analyzed. The protocol provides a model for the investigation of dissociative processes and their impact on psychopathological and psychophysiological features of BPD.
Protocol
Our study was approved by the Ethical Committee at the Ulm University. All investigation proceedings were non-invasive and conducted in accordance with the guidelines for good clinical practice and the Declaration of Helsinki.
1. General procedures for the preparation of the psychophysiological experiment
Obtain ethical approval for the protocol and written informed consent from all participants after giving them detailed information (including information about the possibility of earlier termination without any negative consequences).
Prepare the introductory instruction for the experimental procedure and the participant tasks over the course of the experiment, record it, and save it in the appropriate format within the stimuli presentation software. NOTE: Here is an example how to formulate the initial instruction: "This measurement records your physiological activity while listening to scripts about personal events. This happens through the electrodes attached to your forehead, shoulders, and hand. Try to take a comfortable position in the chair. Your room is closed to shield noises. I can see you through the window, just as you can see me. If something is not right, you can always give me a sign and I'll be right next to you. It is important that you sit still during the measurement and do not move. There are regular breaks in which you can move. Overall, the investigation will take about half an hour. Each script presentation consists of four consecutive 30-second periods: rest condition, script listening, imagination, and relaxation. Please listen carefully to each script, and try to vividly imagine the illustrated experience in chronological order, both during the script presentation and afterwards, until you hear a new instruction. Each script is displayed totally three times. The measurement starts from now in about one minute, as soon as your physiological readings have reached a stable level. So you can relax first."
Proceed similarly for the relaxation and self-report instruction that will be presented between each two scripts. NOTE: Here is a possible formulation of such an instruction: "Please relax. If you want, you can now move a little bit. Fill the questionnaire in by marking the answer options that best describe your feelings during the imagination of the event. Afterwards, try to find again a comfortable position, try to sit still again and continue to relax. Soon you will hear another script. Please listen carefully to it and try to imagine as vividly as possible and in chronological order the illustrated experience until you hear the next instruction."
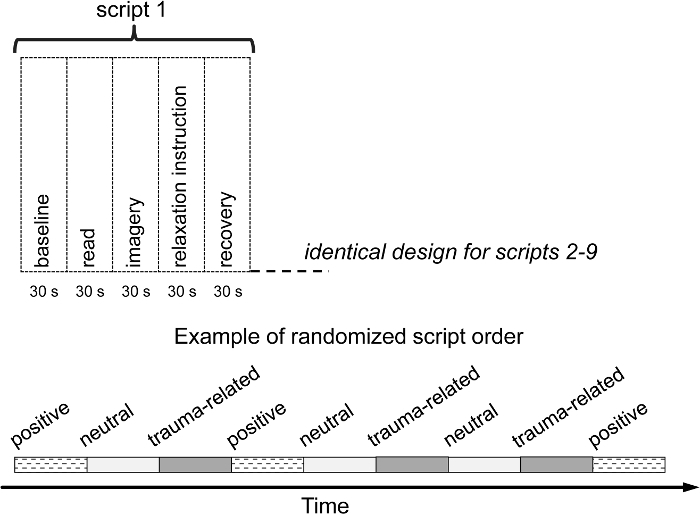
For the presentation of auditory instructions and scripts, use a stimulus computer and a scripting language-based computer software. Play back each script three times and insert four sequential 30-s periods within each script presentation as follows: resting baseline, read (listening to the spoken script), imagery (imagination of the described experience), and recovery (see Figure 2). In-between two script presentations, reserve a period of 1 - 2 minutes for filling the self-report measures in.
Use an appropriate recording computer and software to collect physiological data during the experiment. Depending on the software for recording physiological data, prepare the necessary channels for the recording of physiological parameters (SC and HR).
- Set up markers or use separate channels for the depiction of the time course of the instructions and script presentations.
- To subsequently facilitate the removal of artifacts from the physiological data, incorporate the possibility to flag movements. Save this recording set-up to allow its availability for all planned measurements.
2. Participant selection
NOTE: For the selection and recruitment of the clinical study participants, available standards were considered (Sullivan-Bolyai et al., 2007)25.
If possible, recruit clinical participants from a clinical setting for obtaining reliable information regarding the inclusion and exclusion criteria. Review medical records and clinical files, consult clinical-therapeutic staff (if possible), and ask participants to ascertain relevant information for the participant selection.
Select clinical participants according to the following inclusion criteria: (a) ICD-10 diagnosis F60.31; (b) no medication (ask participants to abstain for 1 week prior to the laboratory experiment from any psychotropic medication or medication with potentially confounding autonomic effects, e.g. anticholinergic, α- or β-adrenergic blockers, digitals, and GABA-(A)-receptor-agonists including benzodiazepine); (c) legal competence, sufficient cognitive function, sufficiently stable psychological state, language proficiency; and (d) informed consent after detailed explanation of the objectives and procedure as well as answers to all the potential questions.
Exclude potential clinical participants if the following criteria apply: (a) internal, neurological, musculoskeletal or endocrinological disorders; (b) acute suicidal ideation, history of schizophrenia-type disorders or bipolar disorder, substance abuse within the last week.
Select control subjects with trauma histories, but without trauma-related or other psychological disorders and match those to the BPD group on age, gender, and education. NOTE: If BPD participants are recruited from a clinical setting, it is possible to select controls by approaching stuff and trainees from the same institution. Since most people experience at least one threatening event during their lives, it is not difficult to find healthy subjects with trauma histories.
3. Clinical assessment
- Carry out an extensive evaluation of the psychological status of all participants with a focus on dissociative phenomena by clinically experienced investigators. Plan enough time for clinical assessment sessions (1 - 2 sessions of 60 - 90 min in length for each patient). Employ the following instruments (or equivalent ones):
- Approach potential clinical participants and, after informed consent (see above), hand over self-report questionnaires and instruct the participant appropriately.
- Obtain information on age, graduation, marital and occupational status. NOTE: In case study participants are recruited from a clinical setting, obtain sociodemographic from the documentation system of the clinic or routine data sets, if available.
- Inquire active substances consumed within the last weeks.
- Hand over the following instruments to the clinical participants.
- Use the Childhood Trauma Questionnaire (CTQ)26, a 28-item questionnaire composed of five subscales, each containing 5 items (emotional abuse, emotional neglect, physical abuse, physical neglect, and sexual abuse) and one response bias subscale, the minimization and denial scale including three items; the items consist of statements to be rated by choosing one of five response options: (1) "never true," (2) "rarely true," (3) "sometimes true," (4) "often true," and (5) "very often true."
- Use the Life Event Checklist27 for the further assessment of traumatic exposure.
- Use the Peritraumatic Dissociative Experiences Scale (PDEQ)28, a 10-item self-report questionnaire measuring the extent of dissociation during the traumatic event and in the subsequent minutes and hours, accompanied by the instruction to fill in the questionnaire relating to their most severe traumatic event from the Life Event Checklist; score items on a 5-point Likert scale from 1 (not at all true) to 5 (extremely true).
- Use the initial questions from the Structured Clinical Interview for DSM-IV-TR Axis I Disorders and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-I and SCID-II)29,30 administrated as a self-rating screening instrument allowing a reduction of the number of domains to be evaluated for the diagnosis of Axis I and personality disorders.
- Use the Borderline Symptom List (BSL)31, a 99-item self-report instrument assessing the severity of borderline symptoms within the previous week on a 5-point Likert scale, with the following answer possibilities: "not at all," "a little," "rather," "much," and "very strong"; it contains the following scales: self-perception (19 items), affect regulation (13 items), self-destruction (12 items), dysphoria (10 items), loneliness (12 items), intrusions (11 items), and hostility (6 items).
- Use the Dissociative Experiences Scale (DES)32, a 28-item questionnaire to screen for dissociative symptoms; items assess the intensity of dissociative experiences from 0% of the time (never) to 100% of the time (always).
- Use the Symptom Check List-90-Revised (SCL-90-R)33, a 90-item self-report instrument evaluating a broad range of psychological problems and symptoms; it contains nine scales (Somatization, Obsessive-Compulsive, Interpersonal Sensitivity, Depression, Anxiety, Hostility, Phobic Anxiety, Paranoid Ideation, Psychoticism) and provides an index of symptom severity as the summary of the test; Construct items on a 5-point Likert-scale, from 0 (not at all) to 4 (very strong).
Proceed similarly for the self-report assessment of the control subjects, except for the following: (a) do not hand any SCID-I and SCID-II questions to control participants (see below in the clinical interview section); (b) for reasons of effort-reduction, employ only a short SCL-version instead of SCL-90-R (namely SCL-14)34.
Arrange an appointment soon for the clinical interview, making sure that the participant can fill in all self-report measures by then.
At the beginning of the clinical Interview session, make sure that the participants filled in all self-report items in the first place, clarify unresolved items, and ask supplementary questions if necessary.
Discuss in-depth the items of the CTQ and Life Event Checklist by asking questions about the type and time of the inquired experiences; if necessary, correct the reports accordingly.
- Use clinical standardized interviews for a differentiate diagnosis of both groups, as follows. NOTE: For reasons of effort reduction, use less extensive, but equivalent diagnostic instruments, to screen for mental disorders within the control group.
- Employ a broader battery of clinical diagnostic interviews for the clinical group: (a) the Clinician Administered PTSD Scale (CAPS)35 for the diagnosis of PTSD; (b) the Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D)36 for diagnosing dissociative disorders; and (c) SCID-I and SCID-II interviews. Within the SCID interviews, conduct detailed inquiries only of the domains indicated by the self-report screening questions.
- Administrate only the Mini-International Neuropsychiatric Interview (M.I.N.I.)37 to control participants. Based on this short structured clinical interview that allows diagnosis of psychiatric disorders according to both DSM-IV and ICD-10 criteria, ascertain the absence of mental disorders as well as the report of at least one past traumatic experience for the inclusion in the control group.
4. Procedures for the preparation of the psychophysiological experiment for each participant
At the end of the clinical interview section, ask the participant to specify and vividly describe the following three types of events: a traumatic one (in case of several traumatic experiences, instruct the participant to choose the one perceived as the worst), as well as two further individual experiences, a neutral one (e.g., cleaning the house, getting up early, or accomplishing other usual, slightly unpleasant everyday duties) and an everyday moderately positive event (e.g., enjoyable, relaxing or fun activities).
Within the event descriptions, inquire objective happenings (i.e., time, place, and context) as well as subjective information (i.e., emotions, sensory perception); take detailed notes allowing subsequent draft of the three verbal scripts (neutral, negative, and traumatic/aversive), which will be used as individualized emotional cues.
Make an appointment for the psychophysiological experiment within the next few days. Instruct the participant not to use any hand lotion or cream before the experiment.
- Shortly after the clinical interview, compose verbal scripts of ca. 30 s duration that portray the three recalled personal experiences in the first person singular, present tense and register them on a voice recorder. Stick as much as possible to the individual formulations of the participants when describing their experiences (see Figure 1 for an example of traumatic script).
- Save them as audio files in the appropriate format and transfer them in the software program on the stimulus computer, serving to present the recorded auditory scripts.
Randomize the order of the script presentation. Adopt and save the resulted order of the scripts in the presentation program and put it on record, to account for it during data analyses.
Transfer and save the scripts in the resulting order into the presentation program. Use a scripting language based computer program which sends simultaneously auditory stimuli to a headphone and marker signals to the psychophysiological recording device at millisecond accuracy. NOTE: To avoid overstraining severely traumatized persons, use a pseudorandomized script sequence by beginning with the presentation of either a neutral or positive script and not leaving any consecutive presentations of the traumatic script. Based on our experience, we cannot confirm the participation of severely traumatized persons in such experiments as being potentially stressful in any way. For this reason, we regard the randomization of scripts under these constraints as only optionally.
Prepare the sheets and a pencil to collect subjective evaluative judgments of affective states during the script-driven imagery tasks. Employ a battery of visual analog 9-point Likert scales: (a) the Self-Assessment Manikin (SAM)38 to evaluate the degree of arousal and dominance of the imagery; (b) similarly constructed scales to assess a set of other discrete emotions (e.g., fear, disgust); and (c) a short version of the scale Dissociation Tension Scale-acute (DSS-4)39 to measure the state dissociation. NOTE: There are also other instruments assessing responses to trauma-related memory. We also suggest the use of the Responses to Script-driven Imagery (RSDI)40 that additionally assesses re-experiences and re-experiencing and avoidance.
Prepare receipts of monetary compensations as well as the corresponding amount of money. NOTE: Our participants received 20 Euros.
5. Psychophysiological experiment
NOTE: Experimental set-up: The experiment followed the guidelines of psychophysiological measurements for the measurement of reactions to emotional cues41.
Conduct the psychophysiological experimental session in a sound-attenuated and temperature- and humidity-controlled laboratory connected via wires and window to an adjoining portion of the laboratory in which the experimental equipment is located.
Reserve enough time for conducting the physiological assessments (ca. 60 - 90 min per participant).
Once the participant arrived at the laboratory, show him/her the facilities and the recording instruments and explain their function.
Seat the participant in a comfortable chair and allow a period of adaptation to the recording environment while explaining again the procedure from the informed consent and answering any further questions.
- Ask participants whether they used any hand lotion in advance and, if necessary, ask them to clean and dry their hands. Clean the required contact skin areas with alcohol solution pads. Attach physiological monitoring devices.
- Use adhesive, pregelled, 279 AgAg/Cl snap electrodes with circular contact areas, filled with an appropriate electrode gel: (a) for the SC measurement, place electrodes on the palmar surface (hypothenar and thenar eminence of the non-dominant hand); (b) for HR recording, use a Lead II configuration of three electrodes (two electrodes placed on the chest below the left and the right shoulder and reference electrode placed e.g. on the forehead). Apply headphones for the presentation of the instruction and scripts.
Perform a test run of the measurements to make sure that the participant hears the instructions and the physiological recordings are running well.
Begin the assessment approximately five minutes later in order to allow physiological readings to stabilize.
Pay attention to any movements of the participant during the experiment and, depending on the software, press a key/take notes to mark artifacts when necessary.
At the end of the experiment, remove all devices and clean the skin areas if requested. Provide monetary compensation and receipts. Offer the participant the opportunity to show and explain the physiological recordings. Ask whether the participant needs to share thoughts and experiences or to receive any further assistance.
Clean the electrodes with cold water to allow the removal of any gel rests.
Representative Results
There are many behaviors reflected in emotional and physiological reactions that can be studied by script-driven imagery paradigms. For instance, the design is suitable to investigate patterns of emotional and physiological response to trauma-related memory. We were particularly interested in verifying whether there is a distinct BPD subgroup mainly characterized by a dissociative reaction pattern.
In our study42, the assessments took place at the Department of Psychiatry and Psychotherapy I of the University of Ulm/Centre for Psychiatry Suedwuerttemberg. The recruitment was realized at the in-patient section 2056 of the headquarters Weissenau, Centre for Psychiatry Suedwuerttemberg. We recruited 28 participants with a clinical diagnosis of BPD. The BPD group was divided according to the established cutoff score of 1.5 of the PDEQ questionnaire for a peritraumatic dissociative reaction (low vs. high): BPD and PD (n = 15) and BPD only (n = 13). A control group of 15 persons with trauma histories, but without trauma-related or other psychological disorders was recruited from the staff of the Centre for Psychiatry Suedwuerttemberg.
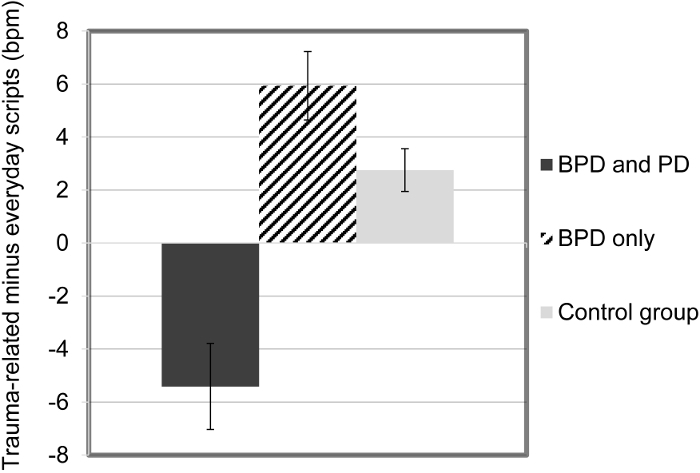
Our study investigated differences between groups with regard to physiological and psychological measures. Among representative findings demonstrating the efficacy of the protocol, significant group differences resulted with respect to the HR differences between trauma-related scripts and scripts of everyday events (positive and neutral), due to a significant decrease of HR during memory of traumatic events in participants with BPD and a history of PD as compared to the BPD only group and controls (Figure 3). Yet, the analyses of SC responses did not show such differences.
Regarding self-report ratings, traumatic memories triggered for instance more dissociation than both positive and neutral memories (Figure 4). Besides, subjects with BPD and PD rated all memories as more dissociation provoking than other BPD participants and controls. The analyses of clinical data added valuable insight in the clinical profiles of BPD participants affected by severe PD responses who also showed a higher traumatic exposure, more severe symptoms and more comorbid disorders than the other BPD participants in Table 1. A multiple linear regression analysis to determine predictors of HR responses to trauma-related memory within the clinical sample indicated that PD level was the strongest predictor, followed by borderline symptom severity and level of dissociative experiences (Table 2).
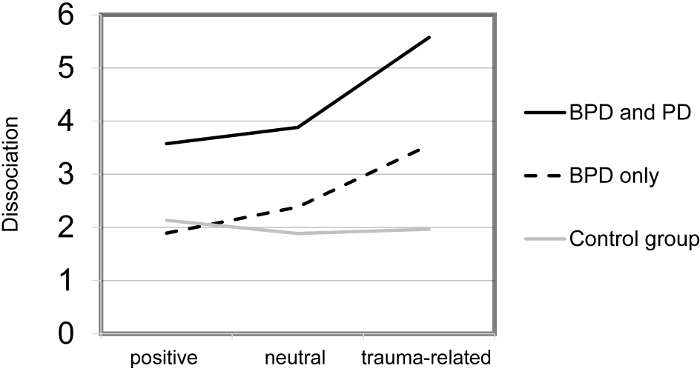
Figure 1. Example of a personalized trauma-related script for the use within a script-driven experiment. Please click here to view a larger version of this figure.
Figure 2. Graphic representation of the experimental design. Please click here to view a larger version of this figure.
Figure 3. Means (and SE) of heart rate responses (difference score trauma-related minus everyday scripts) during memory of traumatic situations, by groups. This figure has been modified from the original figure [Bichescu-Burian et al.38], with permission from Psychophysiology. Please click here to view a larger version of this figure.
Figure 4. Means of self-rated levels of dissociation during memory of positive, neutral, and traumatic situations, by groups. This figure has been modified from the original figure [Bichescu-Burian et al.38], with permission from Psychophysiology. Please click here to view a larger version of this figure.
| (A) | ||||
| BPD and PD (n = 15) | BPD only (n= 13) | Control group (n =15) | p | |
| Demographics | ||||
| Age, M (SD) | 25.53 (9.4) | 24.38 (8.8) | 23.87 (6.3) | n.s. |
| Education (years), M (SD) | 10.40 (1.2) | 10.54 (1.3) | 11.13 (1.1) | n.s. |
| Traumatic events | ||||
| CAPS event types, M (SD) | 7.40 (2.9)a | 6.08 (3.0) | 3.87 (2.3)a | < .01 |
| Rape/rape attempt (%) | 13 (86.7) | 8 (61.5) | 2 (13.3) | < .001 |
| CTQ score, M (SD) | 88.47 (28.0)a | 69.54 (18.5) b | 39.67 (10.4) a, b | < .001 |
| Emotional abuse (SD) | 18.27 (6.7)a | 14.62 (5.9)a, b | 7.67 (2.0)b | < .001 |
| Emotional neglect (SD) | 19.27 (5.3)a | 16.31 (4.4)a, b | 9.60 (4.1)b | < .001 |
| Physical abuse (SD) | 12.07 (6.0)a | 9.38 (6.1) | 5.53 (0.9)a | < .01 |
| Physical neglect (SD) | 12.60 (4.3)a | 10.23 (3.1)a, b | 5.50 (0.8)b | < .001 |
| Sexual abuse (SD) | 14.53 (8.3)a | 10.92 (7.1) | 6.67 (5.2)a | < .05 |
| Unpredictability (SD) | 11.07 (3.9)a, b | 8.08 (3.2)a, c | 4.33 (2.2)b. c | < .001 |
| PDEQ score (SD) | 2.71 (0.7)a, b | 1.21 (.2)a, b, c | 0.86 (0.6)c | < .001 |
| Clinical symptoms | ||||
| BSL score, M (SD) | 2.52 (0.8)a, b | 1.78 (0.7)a, c | 0.48 (0.4)b, c | < .001 |
| DES score, M (SD) | 34.66 (20.9)a, b | 15.91 (11.8)a | 4.90 (2.5)b | < .001 |
| SCL-14 score, M (SD) | 2.21 (0.9)a, b | 1.36 (.6)a, c | 0.18 (0.1)b, c | < .001 |
| Note. Significant differences between each pair of groups as revealed by post hoc comparisons are marked by identical characters. | ||||
| (B) | ||||
| BPD and PD (n = 15) | BPD only (n = 13) | p | ||
| Clinical symptoms | ||||
| CAPS score, M (SD) | 83.7 (28.0) | 58.5 (25.9) | < .05 | |
| GSI score of the SCL-90-R, M (SD) | 2.1 (0.7) | 1.3 (0.6) | < .01 | |
| Diagnoses | ||||
| PTSD, as diagnosed by CAPS (%) | 14 (93.3) | 7 (53.8) | < .05 | |
| Dissociative disorder, based on SCID-D (%) | 12 (80.0) | 1 (7.7) | < .001 | |
| Number of SCID-I diagnoses, M (SD) | 3.20 (1.5) | 1.77 (0.8) | < .01 | |
| Major depression disorder, by SCID-I (%) | 10 (66.7) | 5 (38.5) | n.s. | |
| Anxiety disorders, by SCID-I (%) | 8 (53.3) | 6 (46.2) | n.s. | |
| Substance use disorders, by SCID-I (%) | 9 (60.0) | 1 (7.7) | < .01 | |
| Eating disorders, by SCID-I (%) | 8 (53.3) | 2 (15.4) | < .05 | |
| Obsessive-compulsive disorders, by SCID-I (%) | 4 (26.7) | 1 (7.7) | n.s. | |
| Bipolar disorders, by SCID-I (%) | 1 (6.7) | 3 (23.1) | n.s. | |
| Adjustment disorders, by SCID-I (%) | 1 (6.7) | 2 (15.4) | n.s. | |
| Note. For continuous variables, t tests were calculated; for dichotomous variables, χ2 tests were applied. |
Table 1. Clinical and other characteristics (A) of the three groups and (B) of the two clinical groups. This table was published in Bichescu-Burian et al.42, with permission from Psychophysiology.
| Model and significant predictor variables | R2 | df | p | B | SE | β | t | Partial regression p |
| Model 1 | .42 | 5 | < .01 | |||||
| PDEQ score | -5.81 | 1.96 | -.66 | -2.96 | < .01 | |||
| BSL score | -5.67 | 3.37 | -.60 | -1.68 | n.s. | |||
| DES score | -0.18 | 0.11 | -.47 | -1.66 | n.s. | |||
| SCL-90-R score | -0.12 | 3.60 | -.01 | -0.03 | n.s. | |||
| DSS-4 score | -0.05 | 0.75 | -.01 | -0.06 | n.s. | |||
| Model 2 | .45 | 4 | < .01 | |||||
| PDEQ score | -5.83 | 1.81 | -.66 | -3.22 | < .01 | |||
| BSL score | -5.75 | 2.23 | -.60 | -2.57 | < .05 | |||
| DES score | -0.18 | 0.10 | -.47 | -1.70 | n.s. | |||
| DSS-4 score | -0.04 | 0.73 | -.01 | -0.06 | n.s. | |||
| Model 3 | .48 | 3 | < .001 | |||||
| PDEQ score | -5.85 | 1.74 | -.66 | -3.36 | < .01 | |||
| BSL score | -5.77 | 2.15 | -.61 | -2.68 | < .05 | |||
| DES score | -0.18 | 0.10 | -.47 | -1.75 | n.s. |
Table 2. Linear regression analyses within the BPD Sample (N = 28) for factors of HR responses to Traumatic Imagery. This table was published in Bichescu-Burian et al.42, with permission from Psychophysiology.
Discussion
The present protocol describes an integrated assessment of peripheral physiological responding, self-reports, and clinical assessments for the study of trauma-related dissociation in BPD. For the realization of this procedure, it is important to control for confounders of physiological activity, to ensure functional recordings of physiological data before measurements, and to collect clinical data by expert investigators.
Limits of such integrated assessments protocols may concern the sensitivity and specificity of the measurement, the imperfect covariation between subjective and psychophysiological levels, the role of individual variability as well as the adequacy of the stimuli. Particularly for studies using such a protocol of integrated clinical and psychophysiological assessment, a main limitation is related to small sample sizes in the majority of cases, which do not allow a finer differentiation among subgroups clinical participants and allow the calculation of underpowered models, at best. Another limitation regards the main memory contents related to the selected scripts: Whereas trauma-related scripts reflect episodic memory, everyday experiences as comparison scripts may have also involved semantic contents. Yet in part inevitable, the cross-sectional design impedes causal conclusions and allows correlative implications at best. Moreover, the retrospective recall may be prone to serious biases and influenced by characteristics such as age, pathology, and affective state.
Another possible limitation concerns the assessment of trauma-related dissociation. There are findings in the area of PTSD weakening the proven impact of PD on PTSD symptoms and arguing for a major role of the persistence of dissociative responding over time (e.g., Briere et al., 2005; Werner & Griffin, 2012)43,44. Although in our study PD seemed to mainly influence later responding, the role of the time course of reactions and symptoms should not be underestimated in the search for alternative explanations. For this reason, the employed measures of state and trait dissociation should capture the actual level of persistent dissociation, such as the Shutdown Dissociation Scale (Shut-D)45.
This protocol has several advantages for researchers aiming to study trauma-related dissociation in clinical samples: Employing an integrated assessment with extensive psychodiagnostic testing and measurement of reliable peripheral psychophysiological parameters assure increased diagnostic validity and allows corroboration of findings across measures.
The further investigation of the role of trauma-related dissociation in the etiology of BPD and other clinical samples affected by psychological trauma should comprise larger samples, preferably prospective study designs, and a more thorough assessment of type, occurrence time, and number of traumatic events. Reactions to different types of aversive situations should be investigated, and several psychophysiological parameters should be involved. The selection of other clinical groups inclusive of resilient participants may provide significant clinically and therapeutically useful evidence.
Disclosures
The authors declare no conflict of interest.
Acknowledgments
We particularly thank Dr. Stefan Tschöke and Luisa Steib for scientific advice and assistance with the recruitment of clinical participants, as well as all participants who enabled us to conduct the study and learn from them.
References
- Scaer RC. The neurophysiology of dissociation and chronic disease. Appl. Psychophysiol. Biofeedback. 2001;26(1):73–91. doi: 10.1023/a:1009571806136. [DOI] [PubMed] [Google Scholar]
- Schauer M, Elbert T. Dissociation following traumatic stress. Etiology and treatment. Z. Psychol. 2010;218(2):109–127. [Google Scholar]
- Brewin CR, Dalgleish T, Joseph S. A dual representation theory of post-traumatic stress disorder. Psychol. Rev. 1996;103:670–686. doi: 10.1037/0033-295x.103.4.670. [DOI] [PubMed] [Google Scholar]
- Schauer M, Neuner F, Elbert T. Narrative exposure therapy: A short-term treatment for traumatic stress disorders. Cambridge, MA: Hogrefe; 2011. [Google Scholar]
- Lanius RA, Bluhm R, Lanius U, Pain C. A review of neuroimaging studies in PTSD: heterogeneity of response to symptom provocation. J Psychiatr Res. 2006;40(8):709–729. doi: 10.1016/j.jpsychires.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Schalinski I, Elbert T, Schauer M. Female dissociative responding to extreme sexual violence in a chronic crisis setting: The case of Eastern Congo. J. Trauma. Stress. 2011;24(2):235–238. doi: 10.1002/jts.20631. [DOI] [PubMed] [Google Scholar]
- Adenauer H, Catani C, Keil J, Aichinger H, Neuner F. Is freezing an adaptive reaction to threat? Evidence from heart rate reactivity to emotional pictures in victims of war and torture. Psychophysiology. 2010;47(2):315–322. doi: 10.1111/j.1469-8986.2009.00940.x. [DOI] [PubMed] [Google Scholar]
- Schalinski I, Elbert TR, Schauer M. Cardiac defense in response to imminent threat in women with multiple trauma and severe PTSD. Psychophysiology. 2013;50(7):691–700. doi: 10.1111/psyp.12051. [DOI] [PubMed] [Google Scholar]
- D'Andrea W, Pole N, DePierro J, Freed S, Wallace DB. Heterogeneity of defensive responses after exposure to trauma: Blunted autonomic reactivity in response to startling sounds. Int. J. Psychophysiol. 2013;90(1):80–89. doi: 10.1016/j.ijpsycho.2013.07.008. [DOI] [PubMed] [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN. Emotion and motivation: measuring affective perception. J. Clin. Neurophysiol. 1998;15(5):397–408. doi: 10.1097/00004691-199809000-00004. [DOI] [PubMed] [Google Scholar]
- Boucsein W. Electrodermal activity. Springer Science & Business Media; 2012. [Google Scholar]
- Lang PJ, Levin DN, Miller GA, Kozak MJ. Fear behavior, fear imagery, and the psychophysiology of emotion: The problem of affective-response integration. J. Abnorm. Psychol. 1983;92:276–306. doi: 10.1037//0021-843x.92.3.276. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, et al. Psychophysiology of posttraumatic stress disorder related to motor vehicle accidents: replication and extension. J. Consult. Clin. Psychol. 1996;64:742–751. doi: 10.1037//0022-006x.64.4.742. [DOI] [PubMed] [Google Scholar]
- Orr SP, et al. Psychophysiologic assessment of women with PTSD resulting from childhood sexual abuse. J. Consult. Clin. Psychol. 1998;66:906–913. doi: 10.1037//0022-006x.66.6.906. [DOI] [PubMed] [Google Scholar]
- Orr SP, Roth WT. Psychophysiological assessment: clinical applications for PTSD. J. Affect. Disord. 2000;61:225–240. doi: 10.1016/s0165-0327(00)00340-2. [DOI] [PubMed] [Google Scholar]
- Pitman RK, Orr SP, Forgue DF, de Jong JB, Claiborn JM. Psychophysiologic assessment of posttraumatic stress disorder imagery in Vietnam combat veterans. Arch. Gen. Psychiatry. 1987;44:970–975. doi: 10.1001/archpsyc.1987.01800230050009. [DOI] [PubMed] [Google Scholar]
- Stanford MS, Vasterling JJ, Mathias CW, Constans JI, Houston RJ. Impact of threat relevance on P3 event-related potentials in combat-related post-traumatic stress disorder. Psychiatry Res. 2001;102(2):125–137. doi: 10.1016/s0165-1781(01)00236-0. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Harvey AG, Gordon E, Barry RJ. Eye movement and electrodermal responses to threat stimuli in post-traumatic stress disorder. Int. J. Psychophysiol. 1995;20(3):209–213. doi: 10.1016/0167-8760(95)00036-4. [DOI] [PubMed] [Google Scholar]
- Bichescu-Burian D. Psychophysiological Imagery Assessment in Chronic Posttraumatic Stress Disorder. Analele Ştiinţifice ale Universităţii» Alexandru Ioan Cuza «din Iaşi. Psihologie. 2009;2(2):5–26. [Google Scholar]
- Davis JM, Adams HE, Uddo M, Vasterling JJ, Sutker PB. Physiological arousal and attention in veterans with posttraumatic stress disorder. J. Psychopathol. Behav. Assess. 1996;18:1–20. [Google Scholar]
- Barnow S, et al. Dissociation and emotion regulation in borderline personality disorder. Psychol. Med. 2012;42(04):783–794. doi: 10.1017/S0033291711001917. [DOI] [PubMed] [Google Scholar]
- Ludaescher P, et al. Pain sensitivity and neural processing during dissociative states in patients with borderline personality disorder with and without comorbid posttraumatic stress disorder: A pilot study. J. Psychiatry Neurosci. 2010;35(3):177–184. doi: 10.1503/jpn.090022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin MG, Resick PA, Mechanic MB. Objective assessment of peritraumatic dissociation: Psychophysiological indicators. Am. J. Psychiatry. 1997;154(8):1081–1088. doi: 10.1176/ajp.154.8.1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medina AM, Mejia VY, Schell AM, Dawson ME, Margolin G. Startle reactivity and PTSD symptoms in a community sample of women. Psychiatry Res. 2001;101(2):157–169. doi: 10.1016/s0165-1781(01)00221-9. [DOI] [PubMed] [Google Scholar]
- Sullivan-Bolyai S, et al. Barriers and strategies of recruiting study participants in clinical settings. West. J. Nurs. Res. 2007;29(4):486–500. doi: 10.1177/0193945907299658. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Childhood trauma questionnaire: A retrospective self-report questionnaire and manual. San Antonio, TX: The Psychological Corporation; 1998. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. ASMNT. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The peritraumatic dissociative experiences questionnaire. Assessing Psychological Trauma and PTSD. 1997;2:144–168. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II) Washington, D.C: American Psychiatric Press, Inc; 1997. [Google Scholar]
- Bohus M, Limberger MF, Frank U, Sender I, Gratwohl T, Stieglitz RD. Development of the Borderline Symptom List. Psychother. Psychosom. Med. Psychol. 2001;51(5):201–211. doi: 10.1055/s-2001-13281. [DOI] [PubMed] [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J. Nerv. Ment. Dis. 1986;174:727–735. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring of procedures manual-ii for the revised version and other instruments of the psychopathology rating scale series. Baltimore, MD: Clinical Psychometric Research Incorporated; 1992. [Google Scholar]
- Prinz U, Nutzinger DO, Schulz H, Petermann F, Braukhaus C, Andreas S. Die Symptom-Checkliste-90-R und ihre Kurzversionen: Psychometrische Analysen bei Patienten mit psychischen Erkrankungen [The Symptom Check List-90-R and its short versions: Psychometric analyses in patients with psychological disorders] Phys. Med. Rehab. Kuror. 2008;18(06):337–343. [Google Scholar]
- Blake DD, et al. The development of a clinician-administered PTSD scale. J. Trauma. Stress. 1995;8(1):75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Steinberg M. Interviewers guide to the Structured Clinical Interview for DSM-IV Dissociative Disorders (SCID-D) Washington: American Psychiatric Press; 1994. [Google Scholar]
- Lecrubier Y, et al. The Mini International Neuropsychiatric Interview (MINI). A short diagnostic structured interview: Reliability and validity according to the CIDI. Eur. Psychiatry. 1997;12(97):224–231. [Google Scholar]
- Lang PJ, Bradley MM, Cuthbert BN, Patrick CJ. Emotion and psychopathology: A startle probe analysis. Prog. Exp. Pers. Psychopathol. Res. 1993;16:163–199. [PubMed] [Google Scholar]
- Stiglmayr C, Schmahl C, Bremner JD, Bohus M, Ebner-Priemer U. Development and psychometric characteristics of the DSS-4 as a short instrument to assess dissociative experience during neuropsychological experiments. Psychopathology. 2009;42(6):370–374. doi: 10.1159/000236908. [DOI] [PubMed] [Google Scholar]
- Hopper JW, Frewen PA, Sack M, Lanius RA, Van der Kolk BA. The Responses to Script-Driven Imagery Scale (RSDI): assessment of state posttraumatic symptoms for psychobiological and treatment research. J Psychopathol Behav Assess. 2007;29(4):249–268. [Google Scholar]
- Lang P, Bradley MM, Cuthbert BN. Emotion, motivation, and anxiety: Brain mechanisms and psychophysiology. Biol. Psychiatry. 1998;44:1248–1263. doi: 10.1016/s0006-3223(98)00275-3. [DOI] [PubMed] [Google Scholar]
- Bichescu-Burian D, Steyer J, Steinert T, Grieb B, Tschöke S. Trauma-related dissociation: Psychological features and psychophysiological responses to script-driven imagery in borderline personality disorder. Psychophysiology. 2016;54:452–461. doi: 10.1111/psyp.12795. [DOI] [PubMed] [Google Scholar]
- Briere J, Scott C, Weathers F. Peritraumatic and persistent dissociation in the presumed etiology of PTSD. Am. J. Psychiatry. 2005;162(12):2295–2301. doi: 10.1176/appi.ajp.162.12.2295. [DOI] [PubMed] [Google Scholar]
- Werner KB, Griffin MG. Peritraumatic and persistent dissociation as predictors of PTSD symptoms in a female cohort. J. Trauma. Stress. 2012;25(4):401–407. doi: 10.1002/jts.21725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalinski I, Schauer M, Elbert T. The shutdown dissociation scale (Shut-D) Eur. J. Psychotraumatol. 2015;6 doi: 10.3402/ejpt.v6.25652. [DOI] [PMC free article] [PubMed] [Google Scholar]


