Abstract
The systemic administration of protective agents to treat drug-induced ototoxicity is limited by the possibility that these protective agents could interfere with the chemotherapeutic efficacy of the primary drugs. This is especially true for the drug cisplatin, whose anticancer actions are attenuated by antioxidants which provide adequate protection against hearing loss. Other current or potential otoprotective agents could pose a similar problem, if administered systemically. The application of various biologicals or protective agents directly to the cochlea would allow for high levels of these agents locally with limited systemic side effects. In this report, we demonstrate a trans-tympanic method of delivery of various drugs or biological reagents to the cochlea, which should enhance basic science research on the cochlea and provide a simple way of directing the use of otoprotective agents in the clinics. This report details a method of trans-tympanic drug delivery and provides examples of how this technique has been used successfully in experimental animals to treat cisplatin ototoxicity.
Keywords: Medicine, Issue 133, Ototoxicity, cochlea, trans-tympanic, cisplatin, NOX3, STAT1, TRPV1
Introduction
The peripheral auditory system is exquisitely sensitive to drugs such as cisplatin and aminoglycoside antibiotics. Cisplatin is a widely used chemotherapeutic agent for the treatment of a variety of solid tumors, such as ovarian, testicular, and head and neck cancers. Ototoxicity experienced with the use of this drug is dose-limiting and quite common, affecting 75-100% of patients treated1. Other drugs, such as carboplatin and oxaliplatin, have emerged as alternatives to cisplatin2,3,4,5, but their usefulness is limited to a few cancers.
Early studies have shown the critical role of reactive oxygen species (ROS) in mediating the ototoxicity produced by cisplatin and aminoglycosides. Subsequent studies showed that the NOX3 isoform of NADPH oxidase is the primary source of ROS in the cochlea, and is activated by cisplatin6,7. The generation of ROS compromises the antioxidant buffering capacity of cells, leading to increased lipid peroxidation of cellular membranes8. Furthermore, cisplatin increases the production of hydroxyl radicals which generate highly toxic aldehyde 4-hydroxynonenal (4-HNE), an initiator of cell death9,10. Based on these findings, several antioxidants have been examined for the treatment of cisplatin ototoxicity. These include N-acetyl cysteine (NAC), sodium thiosulfate (STS), amifostine, and D-methionine. However, a major concern of antioxidant therapy is that these antioxidants could reduce cisplatin chemotherapeutic efficacy when administered systemically11 through the interaction of cisplatin with thiol groups in the antioxidant molecules.
In view of these problems with antioxidant therapy, the goal of this study was to examine the trans-tympanic route of delivering antioxidants and other drugs to the cochlea to reduce hearing loss. The trans-tympanic route of drug and short interfering (si) RNA, described below, appears particularly promising.
Protocol
Male Wistar rats were handled in accordance with the National Institutes of Health animal use guidelines and a protocol approved by the Southern Illinois University School of Medicine Laboratory Animal Care and Use Committee. Auditory brainstem response (ABR) was performed on rats while under anesthesia prior to drug administration and 72 h after to verify the effect of the trans-tympanic drug delivery.
1. Auditory Brainstem Response (ABR)
Note: ABR measurements were collected using the auditory testing equipment and software. ABR represents evoked potentials or high-frequency waves generated by the eighth cranial nerve (wave I and II) and other higher auditory brain stem structures including anteroventral cochlear nucleus (wave III), lateral lemniscus (wave IV), and inferior colliculus (wave V). These waves are differentiated depending on the latency. ABR measurements were performed as described previously12.
Anesthetize rats with a mixture of 90 mg/kg ketamine and 17 mg/kg xylazine via intraperitoneal injection. Confirm the depth of anesthesia via toe-pinch reflex. Apply ophthalmic lubrication (or mineral oil drops) to both eyes to prevent the eyes from drying and avoid ulceration during anesthesia.
Place the rat in the prone position on a heating pad (37 °C) inside of a controlled acoustical booth. Audiology testing equipment is located outside and next to the booth.
Insert stainless steel electrodes accordingly: the ground electrode in the rear flank, the positive electrode between the two ears directly atop the skull, and the negative electrodes below the pinna of each ear.
Apply acoustic stimuli using High-Frequency Transducers as a 5 ms tone burst at 8, 16, and 32 kHz. Determine stimulus intensities as decibel sound pressure level (dB SPL). This begins at 10 dB SPL and reaches 90-dB SPL with a 10-dB step size. Calibrate the sound intensities to a maximum output of 90-dB SPL using an impulse precision sound level meter. Note: The test result gives an indication of the integrity of the peripheral hearing organ, the cochlea, and the aforementioned auditory structures. The waveforms are generated within 15 ms of stimulus input and the latency of the waves depends on conduction time, which in turn is regulated by three critical factors: volume of the brain, the intensity, and the frequency of the sound. Auditory evoked potentials were recorded using software provided by the manufacturer.
Consider the minimum intensity which can evoke two different waveforms (II and III) of 0.5 µV amplitude as threshold prominently. Note: Threshold shift represents the difference in the threshold measured after treatment compared with the threshold obtained prior to treatment.
2. Trans-Tympanic Injections
- To administer the drug trans-tympanically, place the rat in the left lateral decubitus position.
- Insert 2.5 mm disposable ear specula into the ear canal.
- With the use of a surgical scope, position the specula so that the tympanic membrane is visible.
- Using a 29 G X ½, 0.5 mL insulin syringe, draw up 50 µL of the [R]-N-phenyl isopropyl adenosine (R-PIA) solution (1 µM), 8-Cyclopentyl-1,3-dipropylxanthine (DPCPX) solution (3 µM), or siRNA solution (0.9 µg) to inject (5 units).
- Use the specula to direct the needle to the anterior inferior region of the tympanic membrane.
- Poke a hole through the membrane with the needle and administer the drugs mentioned in 1.2.3. Allow the rat to rest in this position for 15 min. Note: 50 µL should be the adequate volume to fit behind the tympanic membrane. No fluid should be in the ear canal after administration.
- Place the rat in the right lateral decubitus position and repeat steps 1.2.1 through 1.2.5 for administration in the other ear.
- For rats receiving cisplatin intraperitoneally, place the rat in the supine position on a heating pad at 37 °C.
- Using a 21 G X 3/4 butterfly needle (12" length tubing), draw up cisplatin (11 mg/kg, 1 mg/mL solution in sterile phosphate buffer saline [PBS]).
- Using a syringe pump, administer cisplatin (1 mg/mL) via intraperitoneal injection over 30 min. Note: For a 250-g rat, the volume would be 2.75 mL at a rate of approximately 0.1 mL per min.
Continue to monitor the depth of anesthesia throughout these procedures. Once cisplatin administration is complete, place the rat back in the cage in the prone position, making sure there is nothing to obstruct its breathing.
Monitor the rat until fully recovered.
3. Cochlea Dissection and Decalcification
Following the final ABR (after 72 h), anesthetize the rat with a mixture of 90 mg/kg ketamine and 17 mg/kg xylazine via intraperitoneal injection. Confirm anesthesia with a toe-pinch reflex. Euthanize the rat via decapitation.
Dissect out the temporal bone as described previously13.
Place cochlea in 4% paraformaldehyde in 1x PBS solution in a 7-mL glass scintillation vial (completely covering the cochlea). Refrigerate overnight at 4 °C. Remove paraformaldehyde and wash with 1x PBS at room temperature.
Remove PBS and fill the tube completely with a 120-mM solution of EDTA (pH 7.3). Place on a rotator at room temperature and allow decalcification for 2 to 3 weeks, changing the EDTA solution daily.
4. Cryosectioning
Upon the completion of decalcification, completely immerse the cochlea in the following solutions (7 mL each) for 24 h at 4 °C: 10% sucrose, 20% sucrose, 1:1 mixture of 20% sucrose, and optimal cutting temperature (OCT) embedding compound.
Place fresh OCT compound to fill and completely cover the cochlea in a 15 mm x 15 mm x 5 mm disposable embedding mold. Orient the cochlea on its side so that it is parallel to the bottom of the embedding mold, as described by Whitlon et al.14
Immediately place the mold on dry ice to solidify the OCT and store at -80 °C overnight.
Immerse microscope slides in 0.01% Poly-L Lysine at room temperature for 30 min. Remove the slides, do not rinse, and allow to dry overnight. Use these slides for cryosections.
Remove the cochlea in OCT from the -80 °C freezer and place it on dry ice. Using a sharp microtome blade (L x W: 80 mm x 8 mm, thickness 0.25 mm, cutting angle of 34 °), section the OCT blocks at 10 µm using a cryostat at -30 °C. Place two sections per slide.
Refrigerate slides at 4 °C when finished.
5. Immunohistochemistry
Place the slides in a glass microscope slide staining dish on a slide rack. Fill the dish with 350 mL of 1x PBS and wash the slides for 5 min three times at room temperature.
- Remove the slides from the dish and dry off the area surrounding the tissue using a dry wipe, being sure not to dry off the tissue.
- Using a liquid blocking pen, draw a circle around the tissue section.
Block the tissue for 1 h at room temperature by adding 150 µL of blocking solution containing 10% normal (donkey) serum, 1% nonionic detergent, and 1% BSA in 1x PBS.
Tap off excess blocking solution and incubate the tissue overnight at 4 °C in a humidified chamber with 150 µL of 10% normal (donkey) serum, 0.1% nonionic detergent, and primary antibody (see the Note below) in 1x PBS. Note: For the following antibodies, these dilutions were used: For Figure 2 and 3, p-STAT1 Ser727 1:300. For Figure 4, p-STAT1 Ser727, 1:100 and TRPV1 1:100.
Place the slides in the glass microscope slide staining dish on a slide rack. Fill the dish with 350 mL of 1x PBS and wash slides for 5 min three times at room temperature.
Incubate with the secondary antibodies diluted in a solution containing 0.01% nonionic detergent and 10% normal (donkey) serum in 1x PBS for 2 to 3 h at room temperature in a humidified chamber in the dark. Note: For the following secondary antibodies, these dilutions were used: For Figure 2 and 3, Donkey Anti-Rabbit IgG 1:600. For Figure 4, Rhodamine (TRITC) Donkey Anti-Rabbit IgG 1:500 and Donkey Anti-Goat IgG 1:500.
Place the slides in the glass microscope slide staining dish on a slide rack. Fill the dish with 350 mL of 1x PBS and wash slides for 5 min three times at room temperature.
Tap excess liquid off the slide, and dry the slide with a dry wipe around the tissue. Mount slides by adding one drop of the mounting agent with DAPI directly onto the tissue. Slowly place the coverslip on top, ensuring that no bubbles are formed underneath, and allow the slides to cure overnight at room temperature in the dark. Store slides at 4 °C.
Image slides using confocal microscopy. Use lasers for imaging as follows: UV laser for DAPI, 488 nm laser for Donkey Anti-Rabbit IgG, and 543 nm laser for rhodamine TRITC.
Representative Results
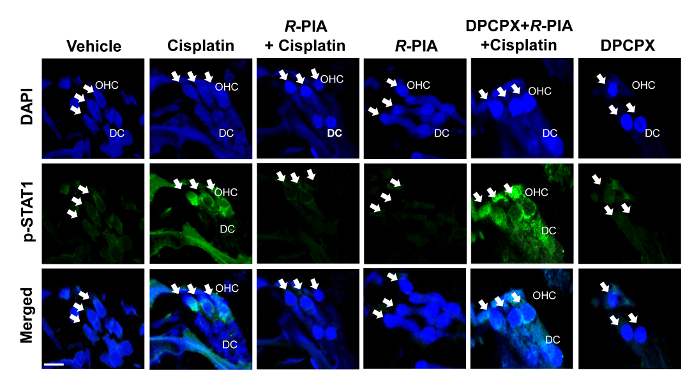
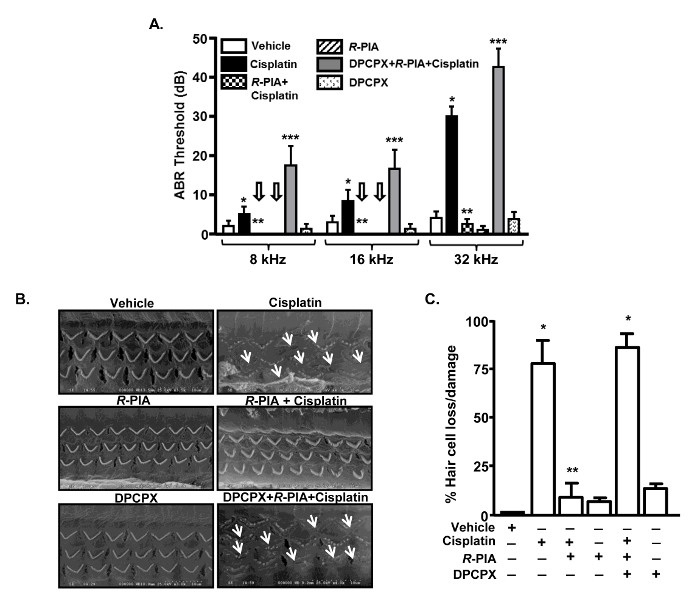
ABR responses measured in rats at three days following cisplatin administration showed a significant elevation in thresholds. Elevation of these thresholds was significantly reduced in rats administered with trans-tympanic [R]-N-phenylisopropyladenosine (R-PIA), adenosine A1 receptor agonist15, prior to cisplatin. The specificity of the action of R-PIA at the adenosine A1 receptor was demonstrated by the observation that it was antagonized by 8-Cyclopentyl-1,3-dipropylxanthine (DPCPX), an A1 receptor-specific antagonist16. This drug potentiated cisplatin-induced ABR threshold shifts (Figure 1A). Similar to its effect of producing hearing loss, cisplatin also increased the loss/damage to outer hair cells (assessed by scanning electron microscopy [SEM]) (Figure 1B). SEM images were obtained as previously described17. This effect was significantly reduced by trans-tympanic administration of R-PIA (Figure 1C). Furthermore, we show that trans-tympanic R-PIA reduces basal and cisplatin-induced p-STAT1 immunoreactivity in the cochlea, reflecting the anti-inflammatory property of this drug (Figure 2).
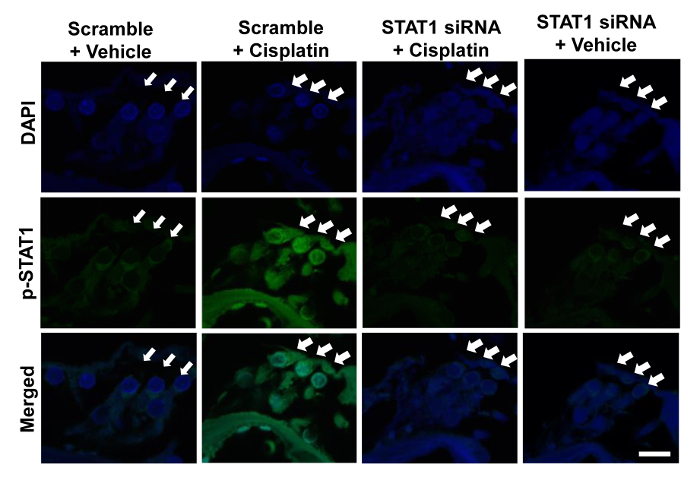
The trans-tympanic route could also be used to administer biologics such as siRNAs, which result in beneficial effects. Trans-tympanic administration of STAT1 siRNA to rats effectively reduced STAT1 and p-STAT1 levels and blocked the activation of this transcription factor by cisplatin (Figure 3).
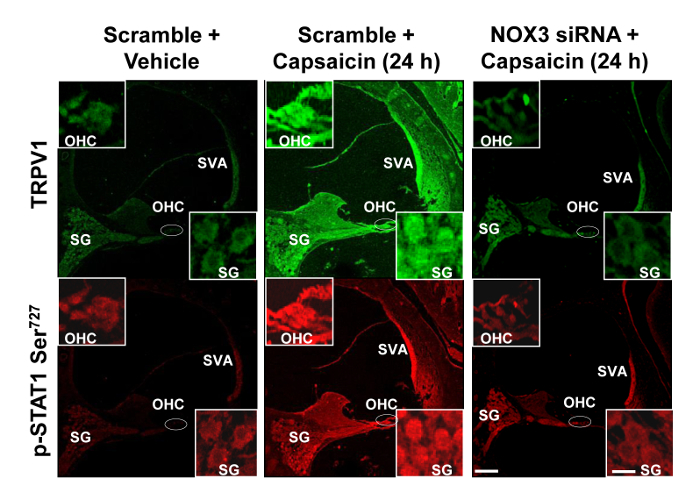
Additional studies show that trans-tympanic administration of another siRNA for the NOX3 mRNA reduced the ability of drugs such as capsaicin to increase some downstream mediators, such as transient receptor potential vanilloid 1 (TRPV1) channel and p-STAT1 (Figure 4). These mediators are implicated in capsaicin-induced hearing loss18.
Figure 1: Trans-tympanic Administration of R-PIA Reduced Cisplatin-induced Hearing Loss and Protected Against Loss of Outer Hair Cells. A. ABR thresholds were measured in rats before and 72 h after treating them with cisplatin (11 mg/kg, i.p.) following trans-tympanic administration of R-PIA or DPCPX + R-PIA. Cisplatin-induced elevation of ABR threshold was shown to be attenuated by the A1AR agonist, R-PIA. Co-administration of the A1AR antagonist, DPCPX, reversed the effect of R-PIA on ABR threshold and significantly elevated the ABR shifts produced by cisplatin at all the frequencies tested. The arrow indicates zero ABR threshold shift. B. Cisplatin treatment showed significant damage to the outer hair cells (OHC) (white arrow) as demonstrated by scanning electron microscopy (SEM). R-PIA protected the OHCs against cisplatin-induced damage, whereas DPCPX attenuated the protective effect of R-PIA. C. The bar graph shows the quantitative analysis of the SEM images shown in B. The error bars indicate the standard error of the mean. Asterisks (*) and (**) indicate a statistically significant difference from vehicle or cisplatin treatment groups, respectively, while (***) indicates a statistically significant difference from R-PIA+cisplatin-treated rats (p<0.05, n=5). This figure was adapted from Kaur et al.19 with permission. Please click here to view a larger version of this figure.
Figure 2: Trans-tympanic Administration of A1AR Agonist, R-PIA, Reduced Cisplatin-increased p-STAT1 Immunoreactivity in the Cochlea. Rats were administered an intraperitoneal dose of cisplatin (11 mg/kg), which increased p-STAT1 Ser727 immunoreactivity, assessed at 72 h post drug administration. However, 1 h pretreatment with trans-tympanic R-PIA blunted this increase in p-STAT1 immunoreactivity. Co-treatment of the A1AR antagonist, DPCPX, along with agonist reversed the inhibition of p-STAT1 immunoreactivity. Blue staining represents DAPI-stained nuclei, whereas green staining represents p-STAT1 immunolabeling. OHC and DC represent outer hair cell and Deiter's cell, respectively. White arrows indicate the three rows of OHCs. Scale bar shown in the lower left panel is 10 µm. This figure was adapted from Kaur et al.19 with permission. Please click here to view a larger version of this figure.
Figure 3: Trans-tympanic Administration of STAT1 siRNA Blocked Cisplatin-induced p-STAT1 Levels. Cochlear sections isolated from rats administered with cisplatin (11 mg/kg, i.p.) for 72 h showed increased Ser727 p-STAT1 immunoreactivity in OHCs. Pre-treatment with trans-tympanic STAT1 siRNA (0.9 mg) attenuated cisplatin-induced increase in p-STAT1 immunoreactivity, whereas scrambled treatment showed no effect. Blue staining represents DAPI-stained nuclei, whereas green staining represents p-STAT1 immunolabeling. White arrows indicate the three rows of OHCs. The scale bar shown in the lower right panel measures 10 µm. This figure was adapted from Kaur et al.20 with permission. Please click here to view a larger version of this figure.
Figure 4: Trans-tympanic Injection of NOX3 siRNA Reduces TRPV1 and p-STAT1 Levels in the Rat Cochlea. Anesthetized rats were administered scrambled siRNA (scramble) or NOX3 siRNAs by the trans-tympanic injections, which was followed two days later by trans-tympanic injections of capsaicin for 24 h. Isolated cochleae from these animals were stained for p-STAT1 Ser727 and TRPV1 immunoreactivity. Capsaicin increased both TRPV1 (green) and p-STAT1 Ser727 (red) immunoreactivity at 24 h in stria vascularis (SVA), outer hair cells (OHC), and spiral ganglion (SG) cells. However, animals pretreated with NOX3 siRNA did not show any visible induction of p-STAT1 Ser727 and TRPV1 immunolabeling. Scale bars (lower right panel) represent 50 and 10 µm for insets. This figure was adapted from Mukherjea et al.18 with permission. Please click here to view a larger version of this figure.
Discussion
The trans-tympanic administration route allows for localized delivery of drugs and other agents to the cochlea which could otherwise produce significant systemic side effects if administered systemically. This method of drug administration allows rapid access of drugs to the site of action at significantly higher doses than would be achieved through the systemic route. Results presented here and published previously showed that trans-tympanic administration of [R]-N-phenyl isopropyl adenosine (R-PIA) protected the cochlea from cisplatin-induced outer hair cell loss (Figure 1)19 and induction of inflammation as demonstrated by diminished activation of STAT1 transcription factor (compared to those treated with cisplatin or R-PIA+DPCPX+cisplatin) (Figure 2)19. These benefits could contribute to the protection from hearing loss afforded by this drug. Based on previous experience, we assert only one drug administration is needed. This could indicate that the drug is retained in the middle ear and could slowly be taken up into the cochlea to provide protection over the three days these animals are assessed for ototoxicity. This technique is currently being used to deliver other drugs into the inner ear to determine their efficacy as oto-protectants.
In addition to drugs, trans-tympanic administration of siRNAs can provide effective knockdown of selective RNAs to reduce their protein levels and provide oto-protection18,20. Again, these siRNAs would provide less toxicities if they are delivered in the proximity of the cochlea. The duration of the knockdown was up to three days (the limit of our assessment period). Importantly, the addition of siRNAs blocks the induction of their corresponding protein by ototoxic drugs, such as cisplatin. The duration of the knockdown is somewhat surprising given the abundance of nucleases in extracellular fluid, and in cells and the potential difficulty in getting these molecules into cochlear cells. However, demonstration of both knockdown of proteins and oto-protection would imply that these siRNAs are reaching the cochlea at effective concentrations.
Despite the benefits described above, certain limitations of this technique are anticipated. These include the need for anesthetizing the experimental animals prior to starting the procedure. Drugs must be administered at higher concentrations into the middle ear since only a small fraction (~1-10%) is anticipated to reach the perilymph. In addition, the distribution of applied drugs or biologicals is more concentrated at the base where the greatest effects are observed.
While trans-tympanic delivery of agents presented here was limited to rats, a similar method of drug delivery could be used prophylactically in patients who are expecting chemotherapy with drugs such as cisplatin. It is anticipated that this method of drug delivery could be adopted rapidly to humans to screen a large number of compounds which have shown efficacy in treating drug-induced hearing loss in experimental animals.
Disclosures
No conflict of interest declared.
Acknowledgments
The work described in this article was supported by a NCI RO1 CA166907, NIDCD RO1-DC 002396 and RO3 DC011621.
References
- McKeage MJ. Comparative adverse effect profiles of platinum drugs. Drug Saf. 1995;13(4):228–244. doi: 10.2165/00002018-199513040-00003. [DOI] [PubMed] [Google Scholar]
- Boulikas T, Vougiouka M. Cisplatin and platinum drugs at the molecular level. Oncol Rep. 2003;10(6):1663–1682. [PubMed] [Google Scholar]
- Fouladi M, et al. Phase II study of oxaliplatin in children with recurrent or refractory medulloblastoma, supratentorial primitive neuroectodermal tumors, and atypical teratoid rhabdoid tumors: a pediatric brain tumor consortium study. Cancer. 2006;107(9):2291–2297. doi: 10.1002/cncr.22241. [DOI] [PubMed] [Google Scholar]
- Pasetto LM, D'Andrea MR, Rossi E, Monfardini S. Oxaliplatin-related neurotoxicity: how and why. Crit Rev Oncol Hematol. 2006;59(2):159–168. doi: 10.1016/j.critrevonc.2006.01.001. [DOI] [PubMed] [Google Scholar]
- Ardizzoni A, et al. Cisplatin- versus carboplatin-based chemotherapy in first-line treatment of advanced non-small-cell lung cancer: an individual patient data meta-analysis. J Natl Cancer Inst. 2007;99(11):847–857. doi: 10.1093/jnci/djk196. [DOI] [PubMed] [Google Scholar]
- Banfi B, Malgrange B, Knisz J, Steger K, Dubois-Dauphin M, Krause KH. NOX3, a superoxide-generating NADPH oxidase of the inner ear. J Biol Chem. 2004;279(44):46065–46072. doi: 10.1074/jbc.M403046200. [DOI] [PubMed] [Google Scholar]
- Mukherjea D, Whitworth CA, Nandish S, Dunaway GA, Rybak LP, Ramkumar V. Expression of the kidney injury molecule 1 in the rat cochlea and induction by cisplatin. Neuroscience. 2006;139(2):733–740. doi: 10.1016/j.neuroscience.2005.12.044. [DOI] [PubMed] [Google Scholar]
- Rybak LP, Husain K, Morris C, Whitworth C, Somani S. Effect of protective agents against cisplatin ototoxicity. Am J Otol. 2000;21(4):513–520. [PubMed] [Google Scholar]
- Lee JE, et al. Role of reactive radicals in degeneration of the auditory system of mice following cisplatin treatment. Acta Otolaryngol. 2004;124(10):1131–1135. doi: 10.1080/00016480410017521. [DOI] [PubMed] [Google Scholar]
- Lee JE, et al. Mechanisms of apoptosis induced by cisplatin in marginal cells in mouse stria vascularis. ORL J Otorhinolaryngol Relat Spec. 2004;66(3):111–118. doi: 10.1159/000079329. [DOI] [PubMed] [Google Scholar]
- Lawenda BD, Kelly KM, Ladas EJ, Sagar SM, Vickers A, Blumberg JB. Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy. J Natl Cancer Inst. 2008;100(11):773–783. doi: 10.1093/jnci/djn148. [DOI] [PubMed] [Google Scholar]
- Akil O, Oursler AE, Fan K, Lustig LR. Mouse auditory brainstem response testing. Bio Protoc. 2016;6(6):1768. doi: 10.21769/BioProtoc.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery SC, Cox BC. Whole Mount Dissection and Immunofluorescence of the Adult Mouse Cochlea. J. Vis. Exp. 2016. p. e53561. [DOI] [PMC free article] [PubMed]
- Whitlon DS, Szakaly R, Greiner MA. Cryoembedding and sectioning of cochleas for immunocytochemistry and in situ hybridization. Brain Res Brain Res Protoc. 2001;6(3):159–166. doi: 10.1016/s1385-299x(00)00048-9. [DOI] [PubMed] [Google Scholar]
- Londos C, Cooper DM, Wolff J. Subclasses of external adenosine receptors. Proc Natl Acad Sci. 1980;77(5):2551–2554. doi: 10.1073/pnas.77.5.2551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohse MJ, Klotz KN, Lindenborn-Fotinos J, Reddington M, Schwabe U, Olsson RA. 8-Cyclopentyl-1,3-dipropylxanthine (DPCPX)--a selective high affinity antagonist radioligand for A1 adenosine receptors. Naunyn Schmiedebergs Arch Pharmacol. 1987;336(2):204–210. doi: 10.1007/BF00165806. [DOI] [PubMed] [Google Scholar]
- Rybak LP, Whitworth C, Scott V, Weberg AD, Bhardwaj B. Rat as a potential model for hearing loss in biotinidase deficiency. Ann Otol Rhinol Laryngol. 1991;100(4):294–300. doi: 10.1177/000348949110000406. Pt 1. [DOI] [PubMed] [Google Scholar]
- Mukherjea D, et al. NOX3 NADPH oxidase couples transient receptor potential vanilloid 1 to signal transducer and activator of transcription 1-mediated inflammation and hearing loss. Antioxid Redox Signal. 2011;14(6):999–1010. doi: 10.1089/ars.2010.3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur T, et al. Adenosine A1 receptor protects against cisplatin ototoxicity by suppressing the NOX3/STAT1 inflammatory pathway in the cochlea. J Neurosci. 2016;36(14):3962–3977. doi: 10.1523/JNEUROSCI.3111-15.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur T, Mukherjea D, Sheehan K, Jajoo S, Rybak LP, Ramkumar V. Short interfering RNA against STAT1 attenuates cisplatin-induced ototoxicity in the rat by suppressing inflammation. Cell Death Dis. 2011;2(180) doi: 10.1038/cddis.2011.63. [DOI] [PMC free article] [PubMed] [Google Scholar]


