In a recent national cohort, low family satisfaction, cyberbullying victimization, and unmet medical needs were unique contributors to sexual orientation disparities in adolescent depressive symptoms.
Abstract
OBJECTIVES:
Sexual orientation disparities in adolescent depressive symptoms are well established, but reasons for these disparities are less well understood. We modeled sexual orientation disparities in depressive symptoms from late adolescence into young adulthood and evaluated family satisfaction, peer support, cyberbullying victimization, and unmet medical needs as potential mediators.
METHODS:
Data were from waves 2 to 6 of the NEXT Generation Health Study (n = 2396), a population-based cohort of US adolescents. We used latent growth models to examine sexual orientation disparities in depressive symptoms in participants aged 17 to 21 years, conduct mediation analyses, and examine sex differences.
RESULTS:
Relative to heterosexual adolescents, sexual minority adolescents (those who are attracted to the same or both sexes or are questioning; 6.3% of the weighted sample) consistently reported higher depressive symptoms from 11th grade to 3 years after high school. Mediation analyses indicated that sexual minority adolescents reported lower family satisfaction, greater cyberbullying victimization, and increased likelihood of unmet medical needs, all of which were associated with higher depressive symptoms. The mediating role of cyberbullying victimization was more pronounced among male than female participants.
CONCLUSIONS:
Sexual minority adolescents reported higher depressive symptoms than heterosexual adolescents from late adolescence into young adulthood. Collectively, low family satisfaction, cyberbullying victimization, and unmet medical needs accounted for >45% of differences by sexual orientation. Future clinical research is needed to determine if interventions targeting these psychosocial and health care–related factors would reduce sexual orientation disparities in depressive symptoms and the optimal timing of such interventions.
What’s Known on This Subject:
Sexual orientation disparities in depressive symptoms are well established, but it is unclear whether the magnitude of these disparities changes over time. Moreover, researchers have previously tested family- and/or peer-level factors as mediators but did not include unmet medical needs.
What This Study Adds:
Sexual minority status was associated with the baseline but not changes in depressive symptoms. We identified cyberbullying victimization and unmet medical needs as novel mediators of sexual orientation disparities in depressive symptoms above and beyond the effect of low family satisfaction.
Disparities between sexual minority and heterosexual adolescents (ie, sexual orientation disparities) in depressive symptoms, major depression, and suicidality are well documented.1–3 Adolescent depressive symptoms, as early signs of psychological maladjustment, can be used to prospectively predict major depression, anxiety disorders, substance use problems, as well as suicidal ideation and attempts during adulthood.4–6 To optimize prevention efforts targeting depressive symptoms among sexual minority adolescents, it is important to understand whether sexual orientation disparities in depressive symptoms increase, decrease, or remain stable during the critical developmental transition from adolescence into young adulthood (to determine the appropriate timing of prevention programs) and identify factors that may explain why these disparities exist (to determine intervention targets).
Although many researchers have examined sexual orientation disparities in depressive symptoms at specific time points,1–3,7,8 few have modeled trajectories of depressive symptoms by sexual orientation during the transition from adolescence into young adulthood. Initial evidence concerning sexual orientation disparities in depressive symptoms trajectories comes from the National Longitudinal Study of Adolescent to Adult Health.9–11 Using 4 waves of National Longitudinal Study of Adolescent to Adult Health data covering a 13-year period (from wave 1 in 1994–1995 to wave 4 in 2007–2009), trajectory analyses revealed that sexual orientation disparities in depressive symptoms were present as early as adolescence (grades 7–12) and persisted into early adulthood (ages 24–32 years),10 and these disparities were more pronounced among female participants.11
Trajectory studies using more recent samples revealed conflicting evidence. In a Chicago sample of sexual minority adolescents aged 16 to 20 years, depressive symptoms were found to decrease over a 3.5-year period.12 In the Dutch Tracking Adolescents’ Individual Lives Survey cohort, sexual minority status was associated with increases in depressive symptoms among younger adolescents who were longitudinally followed from age 11 to 22 years.13 To more fully understand whether these mixed findings are due to variations in the measurement of sexual orientation, when and where the study took place, or differences in the developmental stage examined, trajectory studies of depressive symptoms using more recent population-based samples are needed.
According to the minority stress theory, sexual minorities face heightened social stress in a hostile cultural environment and perceive reduced support and greater rejection in interpersonal relationships.14,15 Consistent with this theory, empirical studies indicate that lower parental support,16 increased parental rejection,13 and more frequent peer harassment17 or victimization13,18 experienced by sexual minority adolescents contributed to higher depressive symptoms. However, these studies were typically focused on 1 or 2 psychosocial mediators in the parental or peer context. Potential mechanisms in alternative contexts are understudied.
In the current study, we tested cyberbullying victimization and unmet medical needs as novel mediators reflecting negative experiences in cyberspace and health care settings. Past research revealed that victimization from both general bullying19 and homophobic name-calling20 was associated with higher depressive symptoms. Furthermore, peer harassment17 or victimization13 and sexual minority–related victimization18 were significant mediators of the association between sexual minority status and depressive symptoms. However, empirical evidence on whether this extends to cyberbullying victimization remains unclear because traditional bullying was a stronger correlate of depression than cyberbullying victimization in 1 study.21 Although less frequent than traditional bullying victimization, the adverse impact of cyberbullying victimization tends to be more pervasive because it can occur beyond the school setting.22 Thus, understanding whether cyberbullying victimization contributes to sexual orientation disparities in depressive symptoms would fill an important knowledge gap.
The medical setting is a context in which sexual minority adolescents could acquire medical care and tangible support from their health care providers. Barriers to health care and unmet medical needs among sexual minority adults have been previously reported.23–25 The smaller but growing literature on adolescents and young adults reveals that sexual minority youth tend to report more unmet medical needs and may be more afraid of what their providers would say or do, be more worried about sexual identity disclosure to their parents, and are more likely to feel embarrassed to use mental health services than their heterosexual peers.26–28 The lack of a secure environment for disclosing sexual orientation may be an important barrier to quality health care and the effective screening of depression.29 Critically, no previous study has documented unmet medical needs as a mediator of sexual orientation disparities in depressive symptoms. Thus, it is unclear if improving medical care access has the potential to reduce depressive symptoms among sexual minority adolescents.
In the current study, we had 3 goals. First, we examined the association of sexual minority status with the initial level of and change in depressive symptoms from 11th grade to 3 years after high school. Next, we tested 4 mediators (family satisfaction, peer support, cyberbullying victimization, and unmet medical needs) of sexual orientation disparities in depressive symptoms. Specifically, we tested cyberbullying victimization and unmet medical needs as novel mediators while controlling for previously established psychosocial mediators in the parental and peer context. This approach allows us to control for potential shared variance in the mediational pathways and can shed light on the relative importance of different mediators. Finally, we examined sex differences in both the direct and indirect paths from sexual minority status to depressive symptoms.
Methods
Participants
The NEXT Generation Health Study (NEXT) is an ongoing 7-year longitudinal study of a nationally representative sample of US adolescents. By using a 3-stage stratified design, a diverse sample of 2785 adolescents enrolled in US high schools from 22 states was obtained and followed annually since the 2009–2010 year. For these analyses, we used data from waves 2 to 6 because sexual orientation was first measured in wave 2 (n = 2439; 87.6% of the full sample). The current analytic sample consisted of 2396 adolescents (98.2% of the wave 2 sample; mean age = 17.2 years) who provided valid responses to questions related to sexual orientation, race and/or ethnicity, family affluence, and at least 1 wave of depressive symptoms. Weighted percentages of racial and/or ethnic groups were 58.8% white, 17.3% African American, 19.7% Hispanic, and 4.3% other. Adolescent socioeconomic inequalities were measured by using the Health Behaviour in School-Aged Children Family Affluence Scale,30 with weighted percentages of 23.1% low, 50.0% middle, and 27.0% high. Parents provided written consent, and participants provided assent to participate in this study. Participants provided consent when they turned 18 years old. This study was approved by the Institutional Review Board of the Eunice Kennedy Shriver National Institute of Child Health and Human Development.
Measures
Sexual Orientation (Wave 2)
Sexual attraction is considered the most important dimension of sexual orientation during adolescence because adolescents typically find it harder to answer questions about sexual behavior and/or identity.31–33 Thus, participants were asked, “Which of the following best describes your sexual orientation?” In Table 1, we present the frequencies and percentages of responses endorsing attraction to opposite sex, attraction to same sex, attraction to both sexes, or questioning at wave 2. Because of low frequencies, the last 3 categories were combined as a sexual minority group for analyses. In this study, those who reported sexual attraction only to the opposite sex are referred to as heterosexual adolescents.
TABLE 1.
Measure of Sexual Orientation and Corresponding Level of Depressive Symptoms at Wave 2 by Sex
| Which of the Following Best Describes Your Sexual Orientation? | Male Participants, n = 1050 | Female Participants, n = 1346 | ||
|---|---|---|---|---|
| Frequency (%) | Weighted Mean of Depressive Symptoms (SE) | Frequency (%) | Weighted Mean of Depressive Symptoms (SE) | |
| Attracted to opposite sex | 933 (94.6) | 0.82 (0.05) | 1198 (89.0) | 1.22 (0.06) |
| Attracted to same sex | 26 (2.5) | 0.93 (0.27) | 19 (1.4) | 1.67 (0.47) |
| Attracted to both sexes | 20 (1.9) | 1.76 (0.21) | 99 (7.4) | 1.93 (0.25) |
| Questioning | 11 (1.1) | 2.03 (0.56) | 30 (2.2) | 1.23 (0.29) |
This same measure was administered in waves 3 and 4 of the NEXT Generation Health Study. Considering the last 3 categories as sexual minority youth, 86.8% (n = 2080) of the sample endorsed sexual attraction to the opposite sex throughout waves 2–4, 9.1% (n = 217) endorsed both heterosexual and sexual minority statuses across waves 2–4, and 4.1% (n = 99) endorsed sexual minority status throughout waves 2–4.
Family Satisfaction (Wave 2)
Participants were asked to rate on a ladder scale (0 [very bad] to 10 [very good]) how satisfied they were with the relationships in their families. Responses were coded as low (0–5), moderate (6–7), high (8–9), and very high (10).
Peer Support (Wave 2)
Participants were asked to nominate up to 3 of their closest male friends and up to 3 of their closest female friends and then indicate (0 [no] and 1 [yes]) whether they have talked with each of these friends about a problem in the last 7 days. Responses were coded as 0 (0 friends), 1 (1 to 2 friends), 2 (3 to 4 friends), and 3 (5 to 6 friends).
Cyberbullying Victimization (Wave 2)
Participants were first given a definition of bullying, emphasizing the deliberate and repeated nature of bullying between 2 parties of unequal power, and then were asked, “In the past couple of months, how often have you been bullied at school or work using a computer, e-mail messages, or cell phone?”34 Responses options were coded as 0 (none), 1 (once or twice), and 2 (2 to 3 times a month, approximately once a week, or several times a week).
Unmet Medical Needs (Wave 2)
Participants were asked if they thought they should but did not get medical care in the past 12 months (0 [no unmet needs] vs 1 [yes, unmet needs]).
Depressive Symptoms (Waves 2–6)
The mean scores of the 8-item pediatric Patient-Reported Outcomes Measurement Information System scale35 were used. Sample items include, “I felt like I couldn’t do anything right,” “I feel lonely,” “I feel sad,” and “I thought that my life was bad.” Response options ranged from 0 (never) to 4 (almost always) in the last 7 days. Cronbach’s alphas across waves ranged from 0.94 to 0.96.
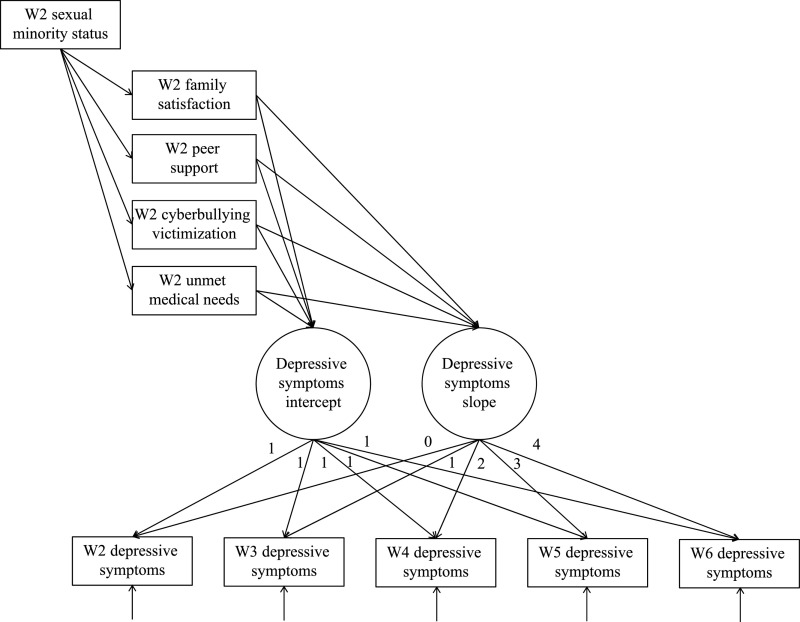
Statistical Analysis
We used latent growth curve models to estimate sexual orientation differences in depressive symptoms from waves 2 to 6, conduct mediation analyses for the involvement of family satisfaction, peer support, cyberbullying victimization, and unmet medical needs in sexual orientation disparities (Fig 1), and evaluate sex differences. Unconditional latent growth models were used to capture mean levels of depressive symptoms at baseline (intercept) and potential linear and nonlinear patterns (slope and quadratic factors) in depressive symptoms over time. Conditional latent growth models controlling for race and/or ethnicity and family affluence were used to examine sexual orientation disparities in depressive symptoms.
FIGURE 1.
Conceptual latent growth model of depressive symptoms with mediation. W2, wave 2; W3, wave 3; W4, wave 4; W5, wave 5; W6, wave 6.
Mediation analyses were conducted in 2 steps and were focused on significant associations between sexual orientation and the depressive symptoms identified in the conditional latent growth model. First, single-mediator models were fitted. For each mediator, sex differences were evaluated by using χ2 difference tests of the indirect effects between male and female participants in multiple-group analyses. Unless the χ2 difference test result was significant, indirect effects were estimated for male and female participants together. Subsequently, all significant mediators were simultaneously included in a final mediation model.
Analyses accounting for the complex survey design were conducted in Stata 14 (StataCorp, College Station, TX) and Mplus 7.4. Mediation effects were tested by using the model indirect command, with the bias-corrected 95% confidence intervals (CIs) of the mediated effects being obtained via bootstrapping (with replicate weights) in Mplus. Missing data were handled by using the full information maximum likelihood method.36
Results
Descriptive Statistics
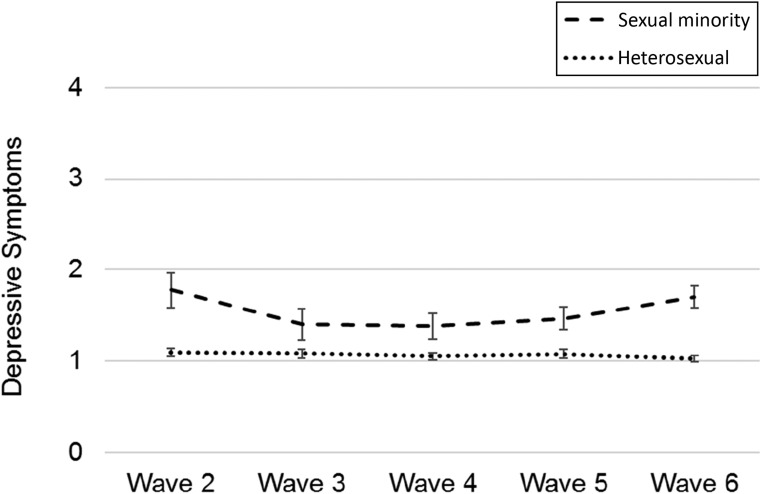
Descriptive statistics for the 4 mediators and depressive symptoms across waves are presented in Table 2. Sexual minority adolescents, who comprised 6.3% (weighted) of the sample, reported lower family satisfaction, more frequent cyberbullying victimization, and a greater likelihood of unmet medical needs but did not differ in peer support when compared with heterosexual adolescents. Sexual minority adolescents consistently reported higher depressive symptoms than heterosexual adolescents over time. This pattern is illustrated in Fig 2.
TABLE 2.
Descriptive Statistics for Mediators and Depressive Symptoms in the Full Sample and by Sexual Orientation (n = 2396)
| Full Sample (n = 2396) | Heterosexual (n = 2191) | Sexual Minority (n = 205) | P | ||||
|---|---|---|---|---|---|---|---|
| Frequency | Weighted % | Frequency | Weighted % | Frequency | Weighted % | ||
| Family satisfaction | .010 | ||||||
| Low (0–5) | 506 | 20.5 | 424 | 19.3 | 82 | 38.5 | |
| Moderate (6–7) | 552 | 23.6 | 508 | 23.9 | 44 | 18.1 | |
| High (8–9) | 783 | 33.7 | 740 | 34.0 | 43 | 30.1 | |
| Very high (10) | 551 | 22.2 | 516 | 22.8 | 35 | 13.3 | |
| Peer support, No. friends | .200 | ||||||
| 0 | 335 | 14.5 | 301 | 14.5 | 34 | 14.1 | |
| 1–2 | 787 | 32.1 | 727 | 32.2 | 60 | 31.8 | |
| 3–4 | 802 | 33.4 | 723 | 32.8 | 79 | 42.5 | |
| 5–6 | 449 | 20.0 | 421 | 20.6 | 28 | 11.6 | |
| Cyberbullying victimization | .003 | ||||||
| None in the past couple of months | 1800 | 82.8 | 1690 | 83.7 | 110 | 67.8 | |
| 1–2 times in the past couple of months | 217 | 11.5 | 185 | 11.1 | 32 | 16.8 | |
| 2–3 times a month or more | 112 | 5.8 | 88 | 5.2 | 24 | 15.5 | |
| Unmet medical needs | .003 | ||||||
| No | 1971 | 80.5 | 1821 | 81.2 | 150 | 70.6 | |
| Yes | 416 | 19.5 | 362 | 18.8 | 54 | 29.4 | |
| Depressive symptoms (0–4) | Weighted Mean | Weighted SE | Weighted Mean | Weighted SE | Weighted Mean | Weighted SE | |
| Wave 2 | 1.14 | 0.04 | 1.10 | 0.04 | 1.78 | 0.19 | .001 |
| Wave 3 | 1.10 | 0.05 | 1.08 | 0.05 | 1.40 | 0.18 | .020 |
| Wave 4 | 1.08 | 0.04 | 1.05 | 0.04 | 1.38 | 0.14 | .012 |
| Wave 5 | 1.10 | 0.05 | 1.08 | 0.05 | 1.47 | 0.12 | .005 |
| Wave 6 | 1.07 | 0.04 | 1.03 | 0.04 | 1.70 | 0.12 | <.001 |
Frequencies and weighted percentages for the mediators were based on data from wave 2. χ2 (for mediators) and t (for depressive symptoms) tests were conducted to compare sexual orientation differences.
FIGURE 2.
Trajectories of depressive symptoms by sexual orientation. Error bars represent SEs.
Trajectory of Depressive Symptoms
Fit statistics for a series of latent growth models are presented in Table 3. In the initial unconditional model (model 1), the intercept means were significant for both male (mean = 0.82; SE = 0.06; P < .001) and female (mean = 1.26; SE = 0.04; P < .001) participants. The slope means were nonsignificant for male (mean = 0.01; SE = 0.01; P = .190) but were significant for female (mean = −0.03; SE = 0.01; P = .035) participants. In the second unconditional model (model 2), the quadratic factor was not significant among male or female participants and was excluded from subsequent models.
TABLE 3.
Model Fit Statistics From the Multiple-Group Latent Growth Models of Depressive Symptoms
| Models | χ2 | df | P | RMSEA (95% CI) | CFI | TLI | χ2 Difference Test P |
|---|---|---|---|---|---|---|---|
| Unconditional and conditional models | |||||||
| 1. Unconditional with intercept and slope | 47.679 | 20 | .001 | 0.034 (0.022–0.047) | 0.962 | 0.962 | — |
| 2. Unconditional with intercept, slope, and quadratic | 29.522 | 12 | .003 | 0.035 (0.019–0.051) | 0.976 | 0.960 | — |
| 3a. Conditional with sexual minority status freed | 61.012 | 26 | <.001 | 0.034 (0.023–0.045) | 0.957 | 0.950 | — |
| 3b. Conditional with sexual minority status fixed | 57.923 | 28 | .001 | 0.030 (0.019–0.041) | 0.963 | 0.961 | .829 |
| 4. Sexual minority status with covariates fixed | 106.546 | 60 | <.001 | 0.025 (0.017–0.033) | 0.954 | 0.946 | — |
| Single-mediator models | |||||||
| 5a. Family satisfaction: free both paths | 94.950 | 76 | .070 | 0.014 (0.000–0.023) | 0.978 | 0.974 | — |
| 5b. Family satisfaction: fix both paths | 93.666 | 78 | .109 | 0.013 (0.000–0.022) | 0.982 | 0.979 | .854 |
| 6a. Peer support: free both paths | 91.931 | 76 | .103 | 0.013 (0.000–0.022) | 0.977 | 0.973 | — |
| 6b. Peer support: fix both paths | 92.562 | 78 | .125 | 0.012 (0.000–0.021) | 0.979 | 0.976 | .494 |
| 7a. Cyberbullying victimization: free both paths | 97.828 | 76 | .047 | 0.015 (0.002–0.024) | 0.972 | 0.967 | — |
| 7b. Cyberbullying victimization: fix both paths | 103.607 | 78 | .028 | 0.017 (0.006–0.025) | 0.967 | 0.962 | .040 |
| 7c. Cyberbullying victimization: fix path “a” only | 99.177 | 77 | .045 | 0.016 (0.002–0.024) | 0.971 | 0.967 | .194 |
| 7d. Cyberbullying victimization: fix path “b” only | 101.441 | 77 | .033 | 0.016 (0.005–0.024) | 0.968 | 0.963 | .035 |
| 8a. Unmet medical needs: free both paths | 87.823 | 76 | .167 | 0.011 (0.000–0.021) | 0.984 | 0.981 | — |
| 8b. Unmet medical needs: fix both paths | 87.992 | 78 | .206 | 0.010 (0.000–0.020) | 0.986 | 0.984 | .539 |
| Final multiple-mediator model | |||||||
| 9. Full model with significant mediators | 137.583 | 116 | .084 | 0.012 (0.000–0.020) | 0.975 | 0.970 | — |
Sex differences in the direct and indirect mediation paths were tested by using χ2 difference tests within a multiple-group analysis framework. "Free" refers to the specified parameters beingfreed across groups. "Fix" refers to the specified parameters being fixed across groups. Mediation paths “a” (predictor to mediator) and “b” (mediator to outcome) in models 5–8 are referred to as "both paths." Nonsignificant χ2 difference tests revealed no significant variation by sex. Because the omnibus χ2 difference test in model 7b was significant, models 7c and 7d were estimated to test whether only 1 or both mediation paths differed across sex. The regression path from cyberbullying victimization to depressive symptoms (model 7d) was more pronounced among male than female participants. CFI, comparative fit index; df, degrees of freedom; RMSEA, root mean square error of approximation; TLI, Tucker-Lewis index; —, not applicable.
Examining Sexual Orientation and the Trajectory of Depressive Symptoms
The conditional latent growth models (models 3a and 3b) fit the data well. Sexual minority status was associated with the intercept but not the slope of depressive symptoms. These estimates (intercept: mean = 0.43, SE = 0.18, P = .020; slope: mean = 0.01, SE = 0.04, P = .889) remained consistent after controlling for race and/or ethnicity and family affluence (model 4) and did not vary between male and female participants.
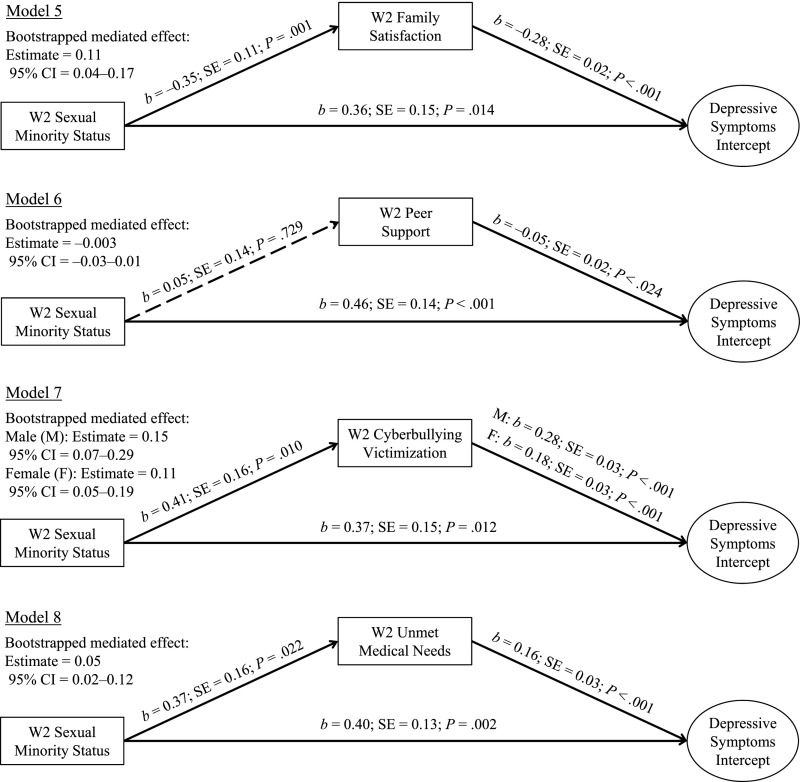
Mediators of Sexual Orientation Disparities
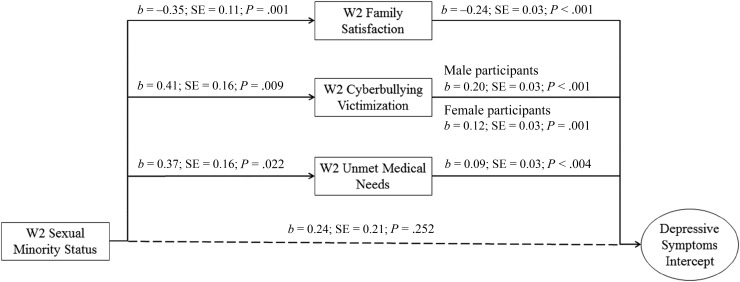
Mediation tests were conducted for paths from sexual orientation to depressive symptoms. Unstandardized path coefficients and the bootstrapped mediated effects from the single-mediator models are presented in Fig 3 (models 5–8). Examination of sex differences revealed that only the path from cyberbullying victimization to depressive symptoms was stronger among male than female participants. Individually, sexual orientation was associated with all the mediators in the expected direction except for peer support, whereas all mediators were associated with depressive symptoms in the 11th grade. In the final mediation model (model 9; Fig 4), the indirect paths through family satisfaction (mediated effect = 0.09; 95% CI = 0.04–0.15), cyberbullying victimization (male participants: mediated effect = 0.11, 95% CI = 0.05–0.26; female participants: mediated effect = 0.08, 95% CI = 0.04–0.14), and unmet medical needs (mediated effect = 0.03; 95% CI = 0.01–0.07) remained significant and attenuated the direct association between sexual orientation and depressive symptoms. The combined indirect effects were 0.23 (95% CI = 0.15–0.38) among male and 0.20 (95% CI = 0.13–0.28) among female participants, whereas the total effects were 0.47 (95% CI = 0.11–0.91) among male and 0.43 (95% CI = 0.09–0.84) among female participants. The proportions of the total effect mediated by these 3 mediators were 49.5% among male and 45.3% among female participants.
FIGURE 3.
Single-mediator, multiple-group models of the direct and indirect effects of sexual minority status on depressive symptoms. Guided by the results of the χ2 difference tests, paths were constrained to be equal across groups unless otherwise specified. F, female participant; M, male participant; W2, wave 2.
FIGURE 4.
Multiple-mediator, multiple-group model of the direct and indirect effects of sexual minority status on depressive symptoms. Arrows leading to wave 2 mediators (family satisfaction, cyberbullying victimization, and unmet medical needs) represent the coefficients for the associations between sexual minority status and each mediator. Arrows leading to depressive symptoms represent the coefficients for the associations between each mediator and baseline depressive symptoms, controlling for sexual minority status and covariates. The coefficient above the dashed arrow leading to depressive symptoms shows the quantified direct association between sexual minority status and baseline depressive symptoms not through the mediators examined. W2, wave 2.
Discussion
In a recent cohort of US adolescents, sexual orientation disparities in depressive symptoms were observable among 11th-graders and persisted into young adulthood within a 5-year time frame. These findings are important within the context of past research revealing a diminishing gap in depressive symptoms between sexual minority and heterosexual adolescents with age12 as well as popular press messages suggesting that depressive symptoms among sexual minority adolescents may decrease with age (eg, the “it gets better” media campaign).37–39 We caution against an overoptimistic message because reductions in depressive symptoms may not occur naturally at the population level and/or may not happen until later in development (eg, after 21 years old). Different from the Dutch Tracking Adolescents’ Individual Lives Survey study, we did not find any increase in depressive symptoms, which likely occurred earlier in development and coincided with pubertal changes and sexual identity development.13 Because sexual minority adolescents had higher levels of depressive symptoms than heterosexual adolescents at all 5 assessment time points, our findings reveal that the developmental period from late adolescence to young adulthood remains a critical window for the intervention of depressive symptoms among sexual minority adolescents. Importantly, the early prevention of depressive symptoms among sexual minority adolescents needs to begin before the 11th grade. Future longitudinal studies are needed to examine the emergence of sexual orientation disparities in depressive symptoms during early- to mid-adolescence.
This study is unique in that we simultaneously examined 4 mediators from multiple contexts. Although the relative importance of peer to parental influence may increase during the transition from late adolescence into young adulthood,40 our findings reveal that family satisfaction was a significant mediator, whereas peer support was not. Consistent with past research, peer support was associated with lower levels of depressive symptoms.41 However, sexual minority adolescents did not receive less peer support, reflecting that by the time they reached late adolescence, sexual minority adolescents may have developed a circle of supportive friends. Importantly, lower family satisfaction remained apparent in late adolescence and was associated with elevated depressive symptoms. More research is needed to understand whether family dissatisfaction during this stage may be driven by parental rejection, struggling with the coming-out process, and/or the perception of being a burden to loved ones.42
Cyberbullying victimization and unmet medical needs were significant mediators in the final model, in which the pathway through low family satisfaction was included. The mediating role of cyberbullying victimization may reflect an extension of bullying in traditional and/or school settings to the cyberspace.43,44 Recent studies reveal that sexual minority adolescents could benefit from accessing information and resources related to their sexual identity through electronic means,45,46 although this might also make them more vulnerable to the experience of cyberbullying.47 Accordingly, the experience of cyberbullying could limit sexual minority adolescents’ comfort level in using these resources. More broadly, cyberbullying victimization has been linked to headaches, abdominal pain, and sleep difficulties.48 Along with the significant indirect effect through unmet medical needs, the current findings support the potential utility of nontraditional interventions (eg, training for medical providers to screen for cyberbullying victimization and medical problems and to provide timely support, treatment, and appropriate referral) to reduce sexual orientation disparities in depressive symptoms.49 Ensuring a safe and supportive environment for adolescents’ disclosure of sexual orientation may be particularly critical to improving health care quality and screening for depression.29
Formal tests of sex differences revealed 1 moderated path from cyberbullying victimization to depressive symptoms that was stronger among male than female participants. In a previous study, male cyberbullying victims were more likely to be victims of physical and verbal bullying as well.43 Possibly, the collective adverse effects of bullying subtypes could have contributed to the stronger association with depressive symptoms among male participants. Overall, our findings reveal that pathways underlying sexual orientation disparities in depressive symptoms were similar for male and female participants.
A central study limitation concerns omitted confounders related to the mediators and depressive symptoms. Notably, traditional and/or school bullying was not controlled for, which limits our interpretation regarding cyberbullying victimization as a unique mediator. Another key limitation concerns the measurement of sexual orientation by using a single item on sexual attraction. Although adolescents generally prefer being asked about their sexual attraction than identity and/or behavior,31 measuring multiple dimensions of sexual orientation would be preferable, especially because disparities in internalizing psychopathology may vary on the basis of how sexual orientation was measured.1 Third, because of low frequencies, we combined adolescents who were attracted to the same sex and both sexes and were questioning for analyses, and we were not able to explore sexual minority subgroup differences. Fourth, data regarding the treatment of depression were not available. Fifth, the NEXT study began in late adolescence and the analysis did not capture the initial emergence of sexual orientation disparities in depressive symptoms; relatedly, we did not address sexual minority status that emerged for the first time after wave 2 (11th grade). Finally, unmet medical needs were assessed by using a single item. An improved assessment of various aspects of unmet medical needs will further inform targeted intervention.
Conclusions
Sexual orientation disparities in depressive symptoms persisted from late adolescence into young adulthood and were partially explained by low family satisfaction, cyberbullying victimization, and unmet medical needs. Pediatricians and health care providers may be particularly well positioned to address both the psychosocial and medical needs experienced by sexual minority adolescents.49,50 The identified mediators warrant further evaluation as intervention targets in future clinical research.
Glossary
- CI
confidence interval
Footnotes
Dr Luk identified and formulated the research questions, conducted the literature review, structured and ran the statistical analyses, and drafted the initial manuscript; Dr Gilman contributed to the conceptualization of the study and the statistical analyses and critically revised the manuscript; Dr Haynie supervised data collection, contributed to the conceptualization of the study, and critically revised the manuscript; Dr Simons-Morton designed the parent study, contributed to the conceptualization of the study, and critically revised the manuscript; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: This project (contract HHSN275201200001I) was supported in part by the Intramural Research Program of the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the National Heart, Lung, and Blood Institute; the National Institute on Alcohol Abuse and Alcoholism; the National Institute on Drug Abuse; and the Maternal and Child Health Bureau of the Health Resources and Services Administration. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest relevant to this article to disclose.
References
- 1.Marshal MP, Dietz LJ, Friedman MS, et al. . Suicidality and depression disparities between sexual minority and heterosexual youth: a meta-analytic review. J Adolesc Health. 2011;49(2):115–123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Russell ST, Joyner K. Adolescent sexual orientation and suicide risk: evidence from a national study. Am J Public Health. 2001;91(8):1276–1281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fergusson DM, Horwood LJ, Beautrais AL. Is sexual orientation related to mental health problems and suicidality in young people? Arch Gen Psychiatry. 1999;56(10):876–880 [DOI] [PubMed] [Google Scholar]
- 4.Fergusson DM, Horwood LJ, Ridder EM, Beautrais AL. Subthreshold depression in adolescence and mental health outcomes in adulthood. Arch Gen Psychiatry. 2005;62(1):66–72 [DOI] [PubMed] [Google Scholar]
- 5.McLeod GFH, Horwood LJ, Fergusson DM. Adolescent depression, adult mental health and psychosocial outcomes at 30 and 35 years. Psychol Med. 2016;46(7):1401–1412 [DOI] [PubMed] [Google Scholar]
- 6.Aalto-Setälä T, Marttunen M, Tuulio-Henriksson A, Poikolainen K, Lönnqvist J. Depressive symptoms in adolescence as predictors of early adulthood depressive disorders and maladjustment. Am J Psychiatry. 2002;159(7):1235–1237 [DOI] [PubMed] [Google Scholar]
- 7.Rosario M, Reisner SL, Corliss HL, Wypij D, Frazier AL, Austin SB. Disparities in depressive distress by sexual orientation in emerging adults: the roles of attachment and stress paradigms. Arch Sex Behav. 2014;43(5):901–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Russell ST, Fish JN. Mental health in lesbian, gay, bisexual, and transgender (LGBT) youth In: Cannon TD, Widiger T, eds. Annual Review of Clinical Psychology. Vol 12 Palo Alto, CA: Annual Reviews; 2016:465–487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fish JN, Pasley K. Sexual (minority) trajectories, mental health, and alcohol use: a longitudinal study of youth as they transition to adulthood. J Youth Adolesc. 2015;44(8):1508–1527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Needham BL. Sexual attraction and trajectories of mental health and substance use during the transition from adolescence to adulthood. J Youth Adolesc. 2012;41(2):179–190 [DOI] [PubMed] [Google Scholar]
- 11.Marshal MP, Dermody SS, Cheong J, et al. . Trajectories of depressive symptoms and suicidality among heterosexual and sexual minority youth. J Youth Adolesc. 2013;42(8):1243–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Birkett M, Newcomb ME, Mustanski B. Does it get better? A longitudinal analysis of psychological distress and victimization in lesbian, gay, bisexual, transgender, and questioning youth. J Adolesc Health. 2015;56(3):280–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.la Roi C, Kretschmer T, Dijkstra JK, Veenstra R, Oldehinkel AJ. Disparities in depressive symptoms between heterosexual and lesbian, gay, and bisexual youth in a Dutch cohort: the TRAILS study. J Youth Adolesc. 2016;45(3):440–456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135(5):707–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Needham BL, Austin EL. Sexual orientation, parental support, and health during the transition to young adulthood. J Youth Adolesc. 2010;39(10):1189–1198 [DOI] [PubMed] [Google Scholar]
- 17.Martin-Storey A, Crosnoe R. Sexual minority status, peer harassment, and adolescent depression. J Adolesc. 2012;35(4):1001–1011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burton CM, Marshal MP, Chisolm DJ, Sucato GS, Friedman MS. Sexual minority-related victimization as a mediator of mental health disparities in sexual minority youth: a longitudinal analysis. J Youth Adolesc. 2013;42(3):394–402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Berlan ED, Corliss HL, Field AE, Goodman E, Austin SB. Sexual orientation and bullying among adolescents in the growing up today study. J Adolesc Health. 2010;46(4):366–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tucker JS, Ewing BA, Espelage DL, Green HD Jr, de la Haye K, Pollard MS. Longitudinal associations of homophobic name-calling victimization with psychological distress and alcohol use during adolescence. J Adolesc Health. 2016;59(1):110–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang J, Nansel TR, Iannotti RJ. Cyber and traditional bullying: differential association with depression. J Adolesc Health. 2011;48(4):415–417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith PK, Mahdavi J, Carvalho M, Fisher S, Russell S, Tippett N. Cyberbullying: its nature and impact in secondary school pupils. J Child Psychol Psychiatry. 2008;49(4):376–385 [DOI] [PubMed] [Google Scholar]
- 23.Everett BG, Mollborn S. Examining sexual orientation disparities in unmet medical needs among men and women. Popul Res Policy Rev. 2014;33(4):553–577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dahlhamer JM, Galinsky AM, Joestl SS, Ward BW. Barriers to health care among adults identifying as sexual minorities: a US National Study. Am J Public Health. 2016;106(6):1116–1122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vogt LE, Rukooko B, Iversen PO, Eide WB. Human rights dimensions of food, health and care in children’s homes in Kampala, Uganda - a qualitative study. BMC Int Health Hum Rights. 2016;16(1):10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Williams KA, Chapman MV. Comparing health and mental health needs, service use, and barriers to services among sexual minority youths and their peers. Health Soc Work. 2011;36(3):197–206 [DOI] [PubMed] [Google Scholar]
- 27.Luk JW, Gilman SE, Haynie DL, Simons-Morton BG. Sexual orientation differences in adolescent health care access and health-promoting physician advice. J Adolesc Health. 2017;61(5):555–561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dunbar MS, Sontag-Padilla L, Ramchand R, Seelam R, Stein BD. Mental health service utilization among lesbian, gay, bisexual, and questioning or queer college students. J Adolesc Health. 2017;61(3):294–301 [DOI] [PubMed] [Google Scholar]
- 29.Hubach RD. Disclosure matters: enhancing patient-provider communication is necessary to improve the health of sexual minority adolescents. J Adolesc Health. 2017;61(5):537–538 [DOI] [PubMed] [Google Scholar]
- 30.Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M. Researching health inequalities in adolescents: the development of the Health Behaviour in School-Aged Children (HBSC) family affluence scale. Soc Sci Med. 2008;66(6):1429–1436 [DOI] [PubMed] [Google Scholar]
- 31.Saewyc EM. Research on adolescent sexual orientation: development, health disparities, stigma, and resilience. J Res Adolesc. 2011;21(1):256–272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saewyc EM, Bauer GR, Skay CL, et al. . Measuring sexual orientation in adolescent health surveys: evaluation of eight school-based surveys. J Adolesc Health. 2004;35(4):345.e1–345.e15 [DOI] [PubMed] [Google Scholar]
- 33.Friedman MS, Silvestre AJ, Gold MA, et al. . Adolescents define sexual orientation and suggest ways to measure it. J Adolesc. 2004;27(3):303–317 [DOI] [PubMed] [Google Scholar]
- 34.Wang J, Iannotti RJ, Nansel TR. School bullying among adolescents in the United States: physical, verbal, relational, and cyber. J Adolesc Health. 2009;45(4):368–375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Irwin DE, Stucky B, Langer MM, et al. . An item response analysis of the pediatric PROMIS anxiety and depressive symptoms scales. Qual Life Res. 2010;19(4):595–607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Little RJ, Rubin DB. Statistical Analysis With Missing Data. Hoboken, NJ: John Wiley & Sons; 2014 [Google Scholar]
- 37.Savage D, Miller T, eds. It Gets Better: Coming Out, Overcoming Bullying, and Creating a Life Worth Living. New York, NY: Penguin Books; 2011 [Google Scholar]
- 38.Kelley T. It gets better: coming out, overcoming bullying, and creating a life worth living. Arch Pediatr Adolesc Med. 2012;166(2):195 [Google Scholar]
- 39.Cardom R, Rostosky S, Danner F. Does “it get better” for depressed sexual minority youth in young adulthood? J Adolesc Health. 2013;53(5):671–673 [DOI] [PubMed] [Google Scholar]
- 40.Laible DJ, Carlo G, Raffaelli M. The differential relations of parent and peer attachment to adolescent adjustment. J Youth Adolesc. 2000;29(1):45–59 [Google Scholar]
- 41.Ueno K. The effects of friendship networks on adolescent depressive symptoms. Soc Sci Res. 2005;34(3):484–510 [Google Scholar]
- 42.Baams L, Grossman AH, Russell ST. Minority stress and mechanisms of risk for depression and suicidal ideation among lesbian, gay, and bisexual youth. Dev Psychol. 2015;51(5):688–696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang J, Iannotti RJ, Luk JW, Nansel TR. Co-occurrence of victimization from five subtypes of bullying: physical, verbal, social exclusion, spreading rumors, and cyber. J Pediatr Psychol. 2010;35(10):1103–1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Juvonen J, Gross EF. Extending the school grounds?—Bullying experiences in cyberspace. J Sch Health. 2008;78(9):496–505 [DOI] [PubMed] [Google Scholar]
- 45.Magee JC, Bigelow L, Dehaan S, Mustanski BS. Sexual health information seeking online: a mixed-methods study among lesbian, gay, bisexual, and transgender young people. Health Educ Behav. 2012;39(3):276–289 [DOI] [PubMed] [Google Scholar]
- 46.Harper GW, Serrano PA, Bruce D, Bauermeister JA. The internet’s multiple roles in facilitating the sexual orientation identity development of gay and bisexual male adolescents. Am J Men Health. 2016;10(5):359–376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kahle L. Are sexual minorities more at risk? Bullying victimization among lesbian, gay, bisexual, and questioning youth [published online ahead of print July 1, 2017]. J Interpers Violence. doi:1177/0886260517718830 [DOI] [PubMed] [Google Scholar]
- 48.Sourander A, Brunstein Klomek A, Ikonen M, et al. . Psychosocial risk factors associated with cyberbullying among adolescents: a population-based study. Arch Gen Psychiatry. 2010;67(7):720–728 [DOI] [PubMed] [Google Scholar]
- 49.Williams SG, Godfrey AJ. What is cyberbullying & how can psychiatric-mental health nurses recognize it? J Psychosoc Nurs Ment Health Serv. 2011;49(10):36–41 [DOI] [PubMed] [Google Scholar]
- 50.Rafla M, Carson NJ, DeJong SM. Adolescents and the internet: what mental health clinicians need to know. Curr Psychiatry Rep. 2014;16(9):472. [DOI] [PubMed] [Google Scholar]