Abstract
Background: Racial and ethnic minority infants and mothers have worse birth outcomes than Caucasian infants and mothers, specifically infant mortality. The purpose of this pilot study was to compare infant mortality rates from vital statistic data between mothers who participated in the Women, Infants, and Children (WIC) Program and the general population in Kansas. Methods: A retrospective secondary analysis of data received from the Kansas Department of Health and Environment (KDHE) was conducted. Data were provided on all mothers who delivered a child in the state of Kansas from 2009 to 2011. The data received from KDHE included maternal demographics, infant deaths, infant gestational age, infant weight at birth, and WIC program participation. Results: The overall infant mortality rate was 6.4 per 1000 births. Infant mortality for Caucasians was lower than for non-Caucasians. Infant mortality for blacks was greater than for non-blacks. Being Hispanic was not statistically associated with a difference in infant mortality. WIC program participation was associated with lower infant mortality in both blacks and Hispanics. After adjusting for WIC, infants born to black mothers were still more than twice as likely to die when compared with Caucasian infants. WIC services were not statistically associated with a reduction in infant mortality. Mother’s education showed a significant protective effect on the likelihood of infant death. Conclusion: The WIC program is associated with positive outcomes at the national level. However, widespread reductions in health disparities have not been reported. Differences in education levels between mothers affected infant mortality to a greater degree than WIC program participation alone in the analysis. The infant mortality rate for black and Hispanic mothers was lower for WIC program participants. The WIC program may be beneficial for reducing infant mortality racial disparities but program participation should be expanded to affect maternal health disparities at the population level.
Keywords: health outcomes, children, community health, program evaluation, prevention
Background
Health disparities continue to exist among maternal and infant health outcomes in Kansas and across the United States.1 Examining the health of infants and mothers, the most vulnerable population in communities, is a good indicator of the overall population’s health status.2 Commonly measured birth outcome indicators include: low birth weight, preterm birth, and infant mortality. For each indicator in the United States and Kansas, racial and ethnic minority infants and mothers have worse rates than Caucasian infants and mothers.3
According to the World Health Organization, approximately 13 million babies are born preterm each year.4 The proportion of premature births in Kansas were 8.3% for Caucasians, 12.9% for Blacks, and 9.1% for other racial subgroups in 2014.5 Various factors have been attributed to preterm births such as infection during pregnancy, or other conditions such as diabetes or hypertension.6
Low birth weight (LBW) is another factor of concern for improving pregnancy outcomes. LBW can be caused by preterm birth, or various other factors such as maternal heart disease, diabetes, hypertension, addiction such as smoking or alcohol, poor nutrition, and being a teenage mother.7 In 2014 in Kansas, the proportion of LBW were 6.5% for Caucasians, 13.4% for Blacks, and 7.6% for other racial subgroups.5
Preterm birth and LBW are risk factors for infant mortality, making infant mortality rate (IMR) a key indicator of health across and within population subgroups. In 2014, the Caucasian IMR was 5.1/1000 live births, the Black rate was 10.3, and the Hispanic rate was 7.5 in Kansas.8 Five-year rolling averages from 2010-2014 indicated the non-Hispanic Black IMR was 2.6 times higher than the Caucasian non-Hispanic IMR. The Hispanic IMR increased in Kansas from 1995-2014 and was 1.5 times higher than the Caucasian non-Hispanic IMR.9
In 1974, the US Department of Agriculture’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) was created to ameliorate birth outcomes and mitigate outcome disparities for at-risk populations. At-risk women that meet specific categorical, residential, income and nutritional criteria may receive services during pregnancy, postpartum and breastfeeding. These services include food packages, education, and health screenings and referrals.10 Early evaluations of the WIC program effect on birth outcomes within high-risk populations have been encouraging; however, the last large-scale evaluation was done in 2010.11 No comparable evaluation has recently been done in the state of Kansas. Given the large gap in IMR between racial subgroups in Kansas, an updated evaluation of birth outcomes for WIC participants is needed. Thus, the purpose of this independent study was to compare IMR between mothers participating in the WIC program and the general population in Kansas.
Methods
A retrospective secondary analysis of data received from the Kansas Department of Health and Environment (KDHE) was conducted to meet the study objective. KDHE provided data on all mothers who delivered a child in the state of Kansas from 2009 to 2011. The data received from KDHE included maternal demographics, infant deaths, infant gestational age, infant weight at birth, and WIC program participation. WIC program participation was self-reported and included any level of program participation.
Data Analysis
For univariate and bivariate analyses, comparisons of continuous and categorical data were conducted using t tests and chi-square analysis, respectively. For continuous variables that were not normally distributed, nonparametric methods were used for comparisons. Descriptive statistics are reported as mean ± SD or proportion where necessary.
Multivariable analysis was conducted using a complete case analysis. Logistic regression was used to examine the adjusted associations of race, mother’s education, and WIC participation with infant mortality. Mother’s education was included as a surrogate variable for socioeconomic status. Education had a significant negative correlation (Spearman’s ρ = −0.505) with WIC program participation, subsequently each variable was entered into a separate regression model with race as a covariate to avoid issues with collinearity. Receiver operating characteristic curves were plotted using the predicted probabilities from each of the 2 regression models to determine which set of predictors best fit the data. All statistical tests were 2-sided and analyses were considered significant when the resultant P value was <.05. All analyses were conducted using SPSS release 19.0 (IBM Corp, Somers, NY).
Results
The dataset received from KDHE included records from 121 458 births. Of these, 114 663 (94.3%) were categorized into 1 of 3 race/ethnic categories (Hispanic, non-Hispanic black, or non-Hispanic Caucasian) and 47 143 (38.8%) mothers participated in the WIC program at some point during pregnancy. The mean maternal age was 27.0 ± 5.8 years. Table 1 presents a summary of demographic variables by WIC program participation.
Table 1.
Demographics and Birth Outcomes by Women, Infants, and Children (WIC) Program Participation.
| Parameter | n | WIC Participants, Mean ± SD or % | Non-WIC Participants, Mean ± SD or % | P Value |
|---|---|---|---|---|
| Age, years | 120 297 | 24.6 ± 5.5 | 28.5 ± 5.4 | <.001 |
| Race/ethnicity | <.001 | |||
| Caucasian | 98 635 | 35.4% | 64.6% | |
| Black | 8413 | 61.7% | 38.3% | |
| Hispanic | 19 224 | 69.8% | 30.2% | |
| Gestational age, weeks | 120 296 | 38.6 ± 2.7 | 38.7 ± 3.0 | <.001 |
| Birth weight, g | 120 296 | 3236.8 ± 572.7 | 3330.5 ± 590.7 | <.001 |
Birth Outcomes
The overall IMR was 6.4 per 1000 births. Infant mortality for Caucasians was lower than for non-Caucasians (5.8/1000 vs 9.2/1000, P < .001). Infant mortality for Blacks was greater than for non-blacks (13.3/1000 vs 5.9/1000, P < .001). Being Hispanic was not statistically associated with a difference in infant mortality (P = .817). WIC program participation was associated with lower infant mortality in both Blacks (9.8/1000 vs 17.7/1000, P = .002) and Hispanics (5.5/1000 vs 7.7/1000, P = .070). However, WIC program participation was associated with a slightly higher infant mortality rate among Caucasians (6.6/1000 vs 5.2/1000, P = .004).
The logistic regression model with race and WIC program participation as predictors of infant mortality showed infants born to non-Hispanic black mothers were more likely to die (odds ratio [OR] = 2.30, 95% CI = 1.85-2.86, P < .001) than those born to non-Hispanic Caucasian mothers. WIC program participation and being Hispanic were not statistically associated with infant mortality. The regression model with race and mother’s education as predictors of infant mortality also showed non-Hispanic black mothers to have an increased risk for infant death but to a lesser degree (OR = 2.06, 95% CI = 1.67-2.55, P < .001). Hispanic ethnicity remained nonsignificant, and education had a significant protective effect on the likelihood of infant death [OR = 0.85, 95% CI = 0.81-0.89, P < .001).
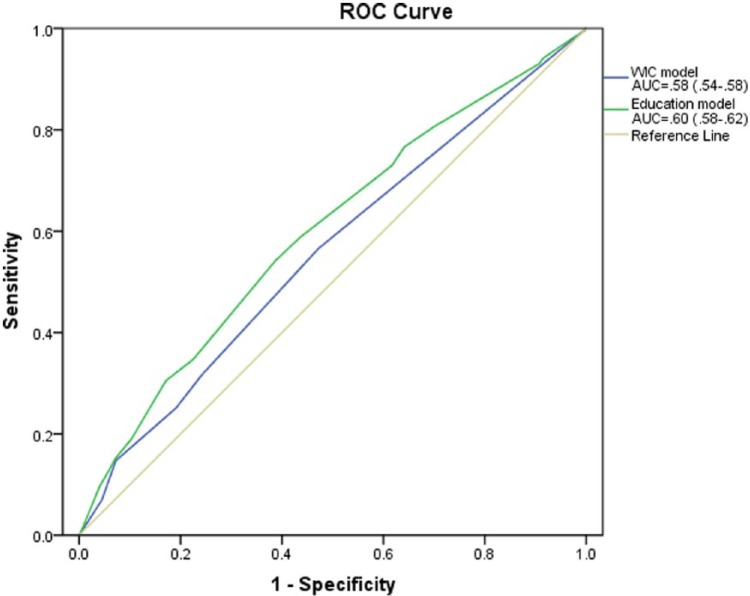
Results from receiver operating characteristic curve analysis showed the regression model with race and education to be a better predictor of infant mortality (area under the curve [AUC] = 0.60, 95% CI = 0.58-0.62, P < .001) than the model with race and WIC program participation as predictors (AUC = 0.56, 95% CI = 0.54-0.58, P < .001) (Figure 1). However, the low value of either AUC indicated that neither model alone was useful for predicting infant mortality.
Figure 1.
Comparison of true positives versus false positives for regression models using race and Women, Infants, and Children (WIC) or mother’s education as predictors of infant mortality.
Discussion
The objective of this study was to examine the distribution and probabilities of selected birth outcomes for Kansas mothers that participated in the WIC program between 2009 and 2011. Findings support the existing literature with regard to health disparities by race and ethnicity. More research is needed to further understand how WIC program participation can help mitigate such disparities.
Comparing the disparity in birth outcomes for Kansas to national data, Kansas has higher infant mortality and a greater disparity gap than what is reported nationally.12 This underlines the importance of the WIC program for potentially ameliorating outcomes in Kansas. Study results indicated the infant mortality rate for black and Hispanic mothers who participated in the WIC program was much lower than those who did not. The health disparities gap among WIC participants was significantly smaller than the health disparities gap of the general population in the same setting. While these findings were not consistent for all racial and ethnic groups and were not consistent across all health outcomes it may appear as if the WIC program does not achieve its desired effect for all populations served. However, at least two explanations exist: (a) some selection bias exists in those women who do and do not participate in the WIC program and/or (b) the benefit of the WIC program is outweighed by the effects of other confounding life-course variables.13
The WIC program is available to women who meet specific high-risk criteria. With these women being at a much higher risk for poor birth outcomes, it is possible for the WIC program to have had a benefit in reducing the risk without eliminating it altogether. Findings support such a hypothesis based on the significant negative association of education with infant mortality. Given the correlation between education and those who qualify for the WIC program, the possibility exists that the benefit of services are being masked by the larger effect of education. Unfortunately, data on individuals who met WIC program eligibility requirements but did not use the program were unavailable. Such information would be useful for future studies to establish the extent of risk reduction associated with receiving services. Other limitations included the lack of medical history and level of WIC program participation data. Certain medical conditions, particularly heart disease, hypertension, diabetes, alcohol and tobacco use, and addiction,6 are known to affect the risk for poor birth outcomes. Available data limited the ability to control for such conditions, it is possible that the effects of medical history and other pertinent variables confounded the results. Additionally, the birth cohort vital statistic dataset may not have included every infant death, as those deaths that occur in a later year can be difficult to capture in vital statistics data.
In conclusion, WIC program participation may be beneficial for reducing racial disparities in infant mortality. The WIC program has been previously well studied and is associated with positive outcomes at the national level. However, national reductions in health disparities have not been reported. Future work should focus on the types of services received with time-series analysis and qualitative work to understand the relative risks associated with choosing not to receive services. It is important to continue research in this area as the WIC program may be beneficial for reducing infant mortality racial disparities. However program participation should be expanded to impact maternal health disparities at the population level.
Acknowledgments
The authors would like to thank Greg Crawford and Carol Moyer at the Kansas Department of Health and Environment, Department of Vital Statistics for their assistance in data acquisition and review.
Author Biographies
Nikki Keene Woods is a maternal and infant health researcher and educator at Wichita State Unversity, Department of Public Health Sciences. Her current research is focused on eliminating health disparities through collaborative community action.
Jared Reyes is a doctoral student in the Department of Communication Sciences and Disorders (CSD) at Wichita State University. He currently works as a research associate for the general surgery residency program at The University of Kansas School of Medicine–Wichita and the Department of Surgery Education at Via Christi Hospitals in Wichita, KS. His research interests include typical and atypical speech-language development, telehealth and telerehabilitation, artificial neural networks for pattern analysis in non-linear systems, and health technology.
Amy Chesser is an assistant professor in the Department of Publice Health Sciences. Her primary research interests are health communication, health literacy, clincian/patient communication and aging studies. She is currently interested in how health communication and health literacy affect public health issues including the underserved.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research,authorship, and/or publication of this article: The research was supported by an internal grant from Wichita State Unviersity, Office of Research.
References
- 1. Blumenshine P, Egerter S, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes: a systematic review. Am J Prev Med. 2010;39:263-272. [DOI] [PubMed] [Google Scholar]
- 2. Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann N Y Acad Sci. 2010;1186:5-23. [DOI] [PubMed] [Google Scholar]
- 3. Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health. 2011;101(suppl 1):S149-S155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88:31-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kansas Department of Health and Environment. Kansas annual summary of vital statistics, 2014. http://www.kdheks.gov/hci/as/2014/2014_AS.pdf. Accessed February 2, 2016.
- 6. Simmons LE, Rubens CE, Darmstadt GL, Gravett MG. Preventing preterm birth and neonatal mortality: exploring the epidemiology, causes, and interventions. Semin Perinatol. 2010;34:408-415. [DOI] [PubMed] [Google Scholar]
- 7. Riccio CA, Sullivan JR, Cohen MJ. Low birth weight. In: Neuropsychological Assessment and Intervention for Childhood and Adolescent Disorders. New York, NY: Wiley; 2010:307-333. [Google Scholar]
- 8. Kansas Department of Health and Environment. Selected special statistics: stillbirths and infant deaths Kansas, 2014. Research summary. http://www.kdheks.gov/hci/IMR/2014_IMR_REPORT.pdf. Accessed February 4, 2016.
- 9. Kansas Department of Health and Environment. Infant mortality in Kansas, 2014. Research brief. http://www.kdheks.gov/hci/IMR/2014_Infant_Mortality_Research_Brief.pdf. Accessed February 2, 2016.
- 10. US Department of Agriculture. Women, Infants, and Children (WIC). http://www.fns.usda.gov/wic/women-infants-and-children-wic. Accessed December 31, 2015.
- 11. Foster EM, Jiang M, Gibson-Davis CM. The effect of the WIC program on the health of newborns. Health Serv Res. 2010;45:1083-1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Deaths: final data for 2013. http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_02.pdf. Accessed December 31, 2015.
- 13. Lu MC, Halfon N. Racial and ethnic disparities in birth outcomes: a life-course perspective. Matern Child Health J. 2003;7:13-30. [DOI] [PubMed] [Google Scholar]