Abstract
Background: Pediatric obesity is a significant public health problem with a prevalence of 16.9% among US children. School-based obesity interventions show promise for reducing adiposity in elementary age children. This pilot study evaluated the impact of the Let’s Go! 5-2-1-0 pediatric obesity intervention program in an elementary school setting. Methods: This was a cluster randomized controlled field trial comprising 8 classrooms of second- and third-grade children. The impact of implementation of a standardized 5-2-1-0 curriculum was evaluated in the classrooms by looking at health behavior (self-reported fruit and vegetable and sugar-containing beverage intake, and screen time), physical activity (steps measured by pedometer), and body mass index (BMI). Half of the classrooms were given 5-2-1-0 teaching over a 4-month period. Results: There was no statistical difference in improvement of healthy habits, BMI, or physical activity in the intervention group compared with the control group. Conclusions: The 5-2-1-0 intervention used in this study was feasible. There was no significant change in healthy habits, likely due to the small number of participants in the study. The intervention and control sites were in different classrooms and there could be factors such as teacher enthusiasm, socioeconomic factors, and individual traits affecting habits. Future studies could use pre- and post-intervention quizzes to assess healthy habits knowledge retention, involving the environments the child participates in outside of school, using research-grade pedometers or accelerometers for measuring activity data collection, and recruiting larger samples to ensure adequate statistical power.
Keywords: health promotion, lifestyle change, obesity, pediatrics, physical activity, prevention, primary care, progam evaluation
Background
Childhood obesity is currently the focus of public health efforts in the United States.1,2 The prevalence of obesity in children between the ages of 6 and 11 years was 17.7% in 2011-2012.3,4 The Institute of Medicine has recommended making schools a national focus for obesity prevention efforts.5 A number of recent reviews and meta-analyses have highlighted the effectiveness of school-based interventions in improving body mass index (BMI) and/or healthy behaviors,6-11 while others have shown these interventions are not effective.12-14
The Let’s Go! 5-2-1-0 program has been implemented in many school and community settings in the United States to prevent and treat obesity.15 The curriculum, developed as part of the national Let’s Go! Program at Maine Medical Center, is available without cost through the program website.15 The key daily messages of the program are for children to eat at least 5 servings of fruits and vegetables, limit recreational screen time to 2 or fewer hours, participate in at least 1 hour of physical activity, and to ingest 0 sugar-containing drinks, including soda, juice, and sports drinks. This program has been studied and found to be feasible in both school and clinical settings.16,17 Although many successful school-based nutritional and physical activity programs involve components similar to 5-2-1-0, the outcomes of implementing this specific program in second- and third-grade children have been published to a very limited degree, but have shown promise in fourth- and fifth-grade children.18
In this pilot study, we compare the standardized 5-2-1-0 curriculum for children in second and third grades with a control group. We hypothesize that implementation of a 5-2-1-0 curriculum will improve healthy behavior (affecting fruit/vegetable intake, sugar-containing beverage intake, fast food intake, and television viewing time) and physical activity (as measured by steps).
Methods
Participants
All second- and third-grade students at a local elementary school (n = 183) in Rochester, Minnesota, were invited to participate in the study. Out of the 183 invitations sent, 100 did not respond, 29 declined participation, and 54 caregivers provided consent. Of those 54 eligible to participate, 3 children did not give assent, for a total of 51 participating children. Publicly available data from the Minnesota Department of Education shows the following demographics for the school at the time of the study: white (non-Hispanic) = 47%, black (non-Hispanic) = 20%, Hispanic = 19%, Asian/Pacific Islander = 14%, limited English proficient = 34.5%, free or reduced-price lunch = 70.9%.19
Children were included in the study if a caregiver signed the HIPAA (Health Insurance Portability and Accountability Act) form, completed the initial study surveys, and if the child gave assent. For families whose primary language was Spanish, documents were translated to Spanish by the Mayo Clinic Language Department.
Second- and third-grade teachers sent home a packet of information, prepared by the study team, to each student’s legal guardian caregiver, including a letter of invitation, which explained the study, a 5-2-1-0 Healthy Habits survey, a demographic survey, and a HIPAA form accompanied by a return envelope. The contact letter also stated that, by completing questionnaires, caregivers authorized the use of pedometers for their child both at the beginning and the end of the study. For families whose primary language was not English or Spanish, school interpreters were available to translate information via phone; all school interpreters satisfy the Minnesota Court Interpreter training requirements.20
Study Instruments
5-2-1-0 Educational Curriculum
The educational curriculum was designed by a committee including an Olmsted County Public Health Nurse, a Rochester Public School teacher, the Rochester Public School Curriculum Coordinator, the Rochester Public School District Lead Dietitian, a Mayo Clinic Pediatric Patient Education Specialist, and a Mayo Clinic Pediatric RN; the committee met monthly between January and May 2014. The curriculum involved 8 sessions anchored around the 5-2-1-0 curriculum (Figure 1). The curriculum for the study was administered by 1 of these 3 individuals: a nursing student, a public health nurse, or a patient education specialist.
Figure 1.
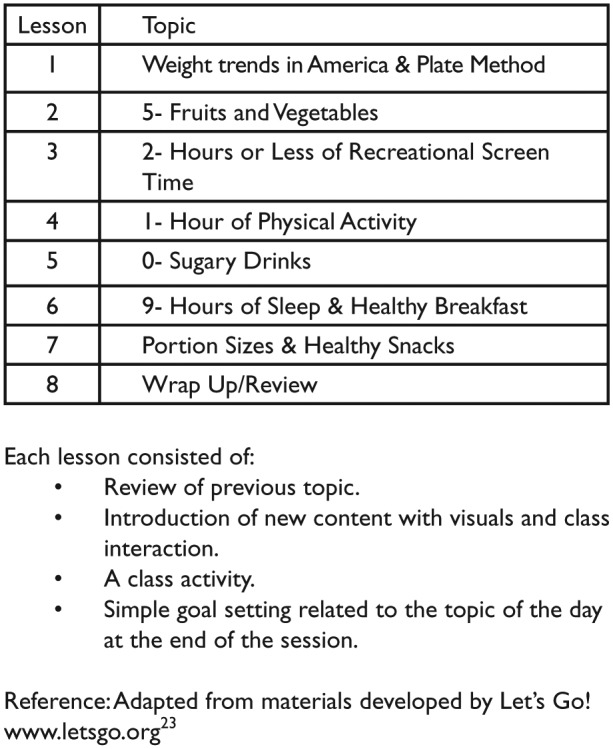
5-2-1-0 eight-week school curriculum.
Healthy Habits Survey
This was a 10-question survey completed by the caregiver designed to address health habits of children aged 2 to 9 years, including physical activity, screen time, takeout or fast-food intake, frequency of eating meals together as a family, fruit and vegetable intake, sugar-containing beverage intake, and the presence of a television or computer in the bedroom.21 We amended the survey so that it contained multiple choice responses instead of free text answers and added a question that elicited the number of hours a night that the child sleeps. This survey has been used in previous studies;12 however, its psychometric properties have not been established.
Pedometer
The Omron HJ-321 pedometer (Omron Healthcare, Inc, Lake Forest, IL) was clipped to clothing, 3 × 1.2 × 0.3 inches, weighs 9.6 ounces, and indicated the total number of steps, which can be viewed by the participant.
Demographic Survey
The investigative team developed a family demographic survey completed by the caregiver to provide information on the child’s gender, race/ethnicity, and insurance type.
Procedure
Study Design
This was a cluster randomized controlled field trial wherein randomization occurred at the classroom level. The 8 participating classrooms were randomly assigned using the experiment package (version 1.1-1) in R (version 3.0.2). There were 4 classes in the control group and 4 in the intervention group, with the intervention occurring over a 4-month period.
Study Procedures
After caregivers provided consent, only those children who gave their assent to participate were accrued to the study. The child’s height and weight were measured twice consecutively by study staff in a private office at the school during school day mornings using a Seca 882 scale and Seca 217 stadiometer, respectively. The pedometer was also distributed at that time. Students were instructed to wear the pedometer at all times that they were awake for the next 7 days. At initiation of the study, children in intervention classrooms received 5-2-1-0 information and a Small Steps Every Day 5-2-1-0 Mayo Action Card.15 Pedometers were retrieved by study staff after a minimum of 7 days. If students wore pedometers more than 7 days (including over the weekend), the last 7 consecutive days of steps were used for the study.
The 5-2-1-0 curriculum was taught to all children in classes receiving the intervention, even to students not participating in the study. The 8 in-school sessions were completed every 1-2 weeks until the study period ended. With 1 week left in the study, pedometers were redistributed to all subjects with instructions to wear at all times while awake for 7 consecutive days. Subjects were provided up to 2 replacement pedometers during the study.
Poststudy Procedures
At the end of the study period, teachers sent home a letter provided by Mayo Clinic research staff to families thanking them for participation and requesting that caregivers complete the poststudy Healthy Habits Survey. Participating children had their height and weight measured in the same manner as at study commencement and the pedometers were collected by study staff. An approved reminder message requesting completion of the Healthy Habits Survey was sent in standard teacher communications in the 2 weeks poststudy. If there was no response from caregivers within 2 weeks, then study investigators sent a reminder letter with the Healthy Habits Survey questionnaire to caregivers through standard mail communication (take-home folder) from the teacher.
Data Analysis
Data were entered into REDCap for analysis.22 To be included in the pre- or poststudy daily step analysis, children needed to have step data during 5 or more days during the 7-day measurement period. The measurement of the effect of the 5-2-1-0 curriculum on BMI, all self-reported health behaviors as documented on the Healthy Habits Survey, and number of steps per day were compared between the intervention and control groups using a chi-square test for categorical variables and Wilcoxon rank sum test for continuous variables. Logistic regression was used to assess predictors of not completing the final survey. Multivariate models simultaneously assessed age, sex, and insurance status.
The goal was to enroll 82 children in both the intervention and control group (average of 20 per class) to estimate an effect size of 1700 steps per day (predicted sigma level 2750), assuming α = 0.05 for a 2-sided t test and a power of 80%. To account for the cluster randomized design, an inflation factor (1 + (m − 1)p where m = average cluster size of 20 and p = intraclass correlation [assumed 0.05]) was applied.
Results
The baseline characteristics of those in the intervention and control groups are described in Table 1. The only demographic difference between intervention and control groups was that 48.3% (14/29) children had a baseline BMI ≥85th percentile compared with 18.2% (4/22), respectively (P = .0259). No children joined the classes during the study and one child from the intervention moved away during the study period and was not included in the poststudy analysis.
Table 1.
Baseline Characteristics for Those in the Intervention and Control Groups.
| Intervention (n = 29) | Control (n = 22) | P | |
|---|---|---|---|
| Child demographics | |||
| Age, years, median (Q1, Q3) | 8 (7, 8) | 8 (7, 9) | .4501 |
| Gender, male, n (%) | 13 (44.8) | 10 (45.4) | .9645 |
| Race, n (%) | .1695 | ||
| White | 20 (69) | 11 (50.0) | |
| Othera | 9 (31) | 11 (50.0) | |
| Insurance status, n (%) | .2928 | ||
| Government/uninsuredb | 11 (42.3) | 8 (36.4) | |
| Private insurance | 15 (57.7) | 14 (63.6) | |
| Body mass index, kg/m2, median (Q1, Q3) | 17.9 (16.0, 21.9) | 16.9 (15.7, 18.1) | .4697 |
| Body mass index percentile, n (%) | .0259 | ||
| 0 to <85 | 15 (51.7) | 18 (81.8) | |
| 85+ | 14 (48.3) | 4 (18.2) | |
| Parent demographics | |||
| Involved caregiverc | .8609 | ||
| Mother | 23 (79.3) | 17 (77.3) | |
| Other | 6 (20.7) | 5 (22.7) | |
| Age, years, median (Q1, Q3) | 35 (32.5, 40.5) | 36 (32, 38) | .4274 |
| Marital status, n (%) | .5427 | ||
| Single/Divorced or separated | 7 (24.1) | 7 (31.8) | |
| Married/Live with a partner | 22 (75.9) | 15 (68.2) | |
| Caregiver employment, n (%) | .2965 | ||
| Full time | 17 (58.6) | 16 (72.7) | |
| Part time/Not employed | 12 (41.4) | 6 (27.3) | |
| Educational level, n (%) | .8817 | ||
| High school diploma or less | 8 (29.6) | 6 (27.3) | |
| Some college/2-year degree | 8 (29.6) | 8 (36.4) | |
| College degree/4-year degree/ | |||
| Postbaccalaureate | 11 (40.7) | 8 (36.4) | |
| Baseline health habits | |||
| Servings of fruit/day, n (%) | .4435 | ||
| 0-2 | 15 (51.7) | 9 (40.9) | |
| 3+ | 14 (48.3) | 13 (59.1) | |
| Times with dinner at the table/week, n (%) | .1469 | ||
| 0-4 | 9 (31.0) | 3 (13.6) | |
| 5+ | 20 (69.0) | 19 (86.4) | |
| Times eat breakfast/week, n (%) | .3883 | ||
| 0-6 | 5 (17.2) | 6 (27.3) | |
| 7+ | 24 (82.8) | 16 (72.7) | |
| Times eating take-out food/week, n (%) | .4843 | ||
| 0-1 | 17 (58.6) | 15 (68.2) | |
| ≥2 | 12 (41.4) | 7 (31.8) | |
| Juice, sports drink, or soda punch/day, n (%) | .3272 | ||
| 0 | 8 (29.6) | 3 (14.3) | |
| 1 | 6 (22.2) | 8 (38.1) | |
| ≥2 | 13 (48.2) | 10 (47.6) | |
| 8-ounce servings of water/day, n (%) | .1153 | ||
| 0-3 | 17 (58.6) | 8 (36.4) | |
| ≥4 | 12 (41.4) | 14 (63.6) | |
| 8-ounce servings nonfat or reduced fat milk/day, n (%) | .5887 | ||
| 0-2 | 18 (62.1) | 12 (54.6) | |
| ≥3 | 11 (37.9) | 10 (45.4) | |
| 8-ounce servings whole milk/day, n (%) | .6471 | ||
| 0 | 18 (66.7) | 16 (72.7) | |
| ≥1 | 9 (33.3) | 6 (27.3) | |
| Hours screen time/day, n (%) | .8609 | ||
| 0-2 | 23 (79.3) | 17 (77.3) | |
| ≥3 | 6 (20.7) | 5 (22.7) | |
| Minutes active/day, n (%) | .4800 | ||
| 0-15 | 6(21.4) | 2 (9.1) | |
| 30 | 9 (32.1) | 9 (40.9) | |
| 1 hour or more | 13 (46.4) | 11 (50.0) | |
| Hours of sleep/night | .9027 | ||
| 5-8 | 11 (37.9) | 7 (31.8) | |
| 9 | 12 (41.4) | 10 (45.5) | |
| ≥10 | 6 (20.7) | 5 (22.7) | |
| Presence of TV in child’s bedroom, n (%) | 10 (34.5) | 7 (31.8) | .8514 |
| Behavior change goal, n (%) | .3117 | ||
| Improved eatingd | 13 (46.4) | 9 (52.9) | |
| Improved beverage intakee | 5 (17.9) | 0 (0.0) | |
| Improved activityf | 10 (35.7) | 8 (47.1) | |
| Pedometer, median (Q1, Q3) | |||
| No. of steps per day | 5173.4 (2834.5, 7120.3) | 4731.3 (3284, 5871.4) | .5066 |
Other race includes Hispanic, black, and other races.
One child had no insurance.
Other caregiver includes father and other.
Eating more fruits or vegetables per day, or eating less takeout or fast food, eating breakfast more often, or eating at the dinner table more often.
Drinking less soda, punch, fruit drinks, sports drinks or 100% juice, drinking more water, drinking more nonfat or reduced fat milk or drinking less whole milk
Less time watching screens, more time in active play, increasing the amount of sleep per night, and removing the TV from the bedroom.
There were no significant differences in baseline healthy habits between the intervention and control groups. Table 2 compares the healthy habit categories in those subjects whose caregivers completed the poststudy survey as well as step and BMI data pre- and postintervention. No significant differences in healthy habits were identified between the 2 groups for any of the individual questions (data not shown). No significant changes in BMI or steps per day were noted between the intervention and control groups. Pedometers were misplaced or broken by subjects 36 times during either the pre- or poststudy step measurement period.
Table 2.
Comparison of Healthy Habits and Objective Outcomes Pre- and Postintervention.
| Intervention (n = 17) | Control (n = 14) | P a | |
|---|---|---|---|
| Healthy Habits Survey, n (%) | |||
| Improved eating behaviorb | .7495 | ||
| 0-1 | 13 (76.47) | 10 (71.43) | |
| 2+ | 4 (23.53) | 4 (28.57) | |
| Improved beverage intake behaviorc | .8705 | ||
| 0-1 | 8 (47.1) | 7 (50.0) | |
| 2+ | 9 (52.9) | 7 (50.0) | |
| Improved activity behaviord | .3973 | ||
| 0-1 | 11 (64.7) | 11 (78.6) | |
| 2+ | 6 (35.3) | 3 (21.4) | |
| Objective measures | |||
| No. of pedometer steps per day (n = 18), post − pre, n; median (Q1, Q3) | n = 10; 2293.5 (745.3, 3783.4) | n = 8; 2651.3 (104, 3466.9) | .9292 |
| Body mass index percentile, n (%) | Total n = 28 | Total n = 22 | .2320 |
| Decrease | 9 (32.1) | 12 (54.5) | |
| Stay same | 10 (35.7) | 4 (18.2) | |
| Increase | 9 (32.1) | 6 (27.3) | |
| Body mass indexe | 0.2 (−0.1, 0.4) | 0.1 (−0.3, 0.4) | .4691 |
χ2 P value.
Eating more fruits or vegetables per day, or eating less takeout or fast food, eating breakfast more often, or eating at the dinner table more often.
Drinking less soda, punch, fruit drinks, sports drinks or 100% juice, drinking more water, drinking more nonfat or reduced fat milk or drinking less whole milk.
Less time watching screens, more time in active play, increasing the amount of sleep per night, and removing the TV from the bedroom.
Median (Q1, Q3) of change in body mass index from pre to post (BMI post − BMI pre)
Discussion
The 5-2-1-0 intervention used in this study was feasible. We had hypothesized that this program would improve measures such as fruit/vegetable intake, sugar containing beverage intake, fast-food intake, television viewing time, and physical activity; however, there was no statistical difference in these measures between pre- and postintervention groups.
As a pilot study, our project was not powered high enough to assess the effectiveness of our intervention, especially with study participation rate much lower than predicted. We had hoped that significant involvement of the classroom teachers in distributing study information and forms, as well as the use of a consent letter instead of a research consent form, would achieve higher participation rates. Completing the study in an afterschool or evening setting where caregivers could be more directly involved may be a way to improve study participation and possibly behavior changes, but did not fit our study goal of implementing the curriculum within the typical school setting and environment.
A previous study in our local community tested an obesity prevention and treatment intervention that involved classroom 5-2-1-0 teaching followed by one-on-one coaching delivered by nursing students to fourth- and fifth-grade children in 2 schools.18 At one school where 10 to 14 one-hour nursing student follow-up visits occurred over 4 months, there were significant decreases in BMI percentile and servings of sugar-containing beverages as well as increases in servings of fruits/vegetables and daily steps.18 It is plausible that the one-on-one nurse motivational interviewing visits were a key component of this previous intervention in our community, which was not used in this study. There is growing evidence that motivational interviewing can be a successful intervention for obesity in the clinical setting.23-26 Nurse-led motivational interviewing sessions, though, are likely not feasible or sustainable in most school settings.
The step counts in our study increased from pre- to postintervention by 2293 steps per day in the intervention group and by 2651 steps in the control group but our overall step count was lower than predicted.18 The younger age of participants in this study (second and third graders instead of fourth and fifth graders) could be associated with less compliance with pedometer use. Future studies could focus on older children (>10 years of age) with the assumption that this age group may be more reliable with pedometer use. The pedometers used in the study by Tucker et al18 were different than ours in that they were time-stamped to verify that the pedometer was worn for an expected amount of time during the day (only appropriate days were used in the analysis) and they were strapped on the ankle and not clipped to clothing and these were likely factors that could have improved compliance. Misplaced or broken pedometers were common in our study and may have negatively affected the volume of data collected. In the future, it may be more controlled to only collect data during the school day; however, this is not representative of the complete day of a child, and would lack the activity input while outside of school.
Prior evidence shows that implementing programs that support healthy habits in a school environment are effective as they allow for passage of knowledge from the students to the families and eventually into the community.17,27,28 Incorporating relationships beyond the school such as with local physicians, recreation facilities, and churches could ensure more effective and sustainable interventions.17
The ultimate goal of projects like this is to identify feasible, reproducible and effective pediatric obesity intervention components for dissemination and implementation in education and healthcare environments. Future projects using 5-2-1-0 should use some lessons learned from our project, including using pre- and post-intervention quizzes to assess healthy habits knowledge retention, involving the environments the child participates in outside of school; using research-grade pedometers or accelerometers for measuring activity data collection, and recruiting larger samples to ensure adequate statistical power.
Acknowledgments
The authors would like to acknowledge Amie Jones, MD, Seema Kumar, MD, and Valeria Cristiani, MD, for their role in developing the protocol and Bridget Biggs, PhD, for her help in developing the surveys. We would like to acknowledge Joan Kotschevar, RN, MS, PHN, and Kimberly Griffin, RN, for teaching the 5-2-1-0 curriculum and Brent Lexvold RD, LD, and Lisa Lenoch, RN, for their help in devising the curriculum. The authors would also like to thank Cindy McHugh, LPN, who assisted with data collection. We are also grateful to the local elementary school and the School Board in Rochester, Minnesota, for allowing us to conduct this study at their facility. We also thank Olmsted County Public Health for allowing their public health nursing staff to participate in the project.
Author Biographies
Brian A. Lynch is an assistant professor of Pediatrics. His areas of research interest include childhood obesity, community engagement and early childhood development.
Natalie Gentile is a second-year Family Medicine resident at the Mayo Clinic in Rochester, Minnesota. Her research interests include childhood obesity, community engagement, and physician wellness.
Julie Maxson, BA, is a clinical research coordinator for the Department of Family Medicine at Mayo Clinic in Rochester, Minnesota. Her research interests include obesity prevention and women’s health.
Stephanie Quigg is a clinical research coordinator in both Primary Care and Family Medicine at the Mayo Clinic in Rochester, MN. She received her Master’s Degree in Marriage and Family Therapy from the University of Wisconsin-Stout. Her research interests include studying issues relevant to children and the elderly.
Laura Swenson, RN, MSN is a patient education specialist in the Office of Patient Education at Mayo Clinic, Rochester, MN.
Tara Kaufman is an assistant professor of Family Medicine. Her research interests include adult and childhood obesity.
Footnotes
Authors’ Note: The contents of this study are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by a grant from the Ben and Zelma Dorson Family Charitable Foundation as well as funding through the Mayo Clinic Department of Family Medicine. This publication was made possible by the CTSA Grant UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH).
References
- 1. Let’s move. http://www.letsmove.gov/. Accessed May 15, 2014.
- 2. National Collaboration on Childhood Obesity Research (NCCOR). http://www.nccor.org/. Accessed May 15, 2014.
- 3. Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242-249. [DOI] [PubMed] [Google Scholar]
- 4. Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311:806-814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Institute of Medicine. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington DC: Institute of Medicine; 2012. [Google Scholar]
- 6. Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: a meta-analysis. Am J Prev Med. 2009;37:418-427. [DOI] [PubMed] [Google Scholar]
- 7. Katz DL. School-based interventions for health promotion and weight control: not just waiting on the world to change. Annu Rev Public Health. 2009;30:253-272. [DOI] [PubMed] [Google Scholar]
- 8. Kothandan SK. School based interventions versus family based interventions in the treatment of childhood obesity—a systematic review. Arch Public Health. 2014;72:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Krishnaswami J, Martinson M, Wakimoto P, Anglemeyer A. Community-engaged interventions on diet, activity, and weight outcomes in U.S. schools: a systematic review. Am J Prev Med. 2012;43:81-91. [DOI] [PubMed] [Google Scholar]
- 10. Lavelle HV, Mackay DF, Pell JP. Systematic review and meta-analysis of school-based interventions to reduce body mass index. J Public Health (Oxf). 2012;34:360-369. [DOI] [PubMed] [Google Scholar]
- 11. Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity (Silver Spring). 2013;21:2422-2428. [DOI] [PubMed] [Google Scholar]
- 12. Dobbins M, Husson H, DeCorby K, LaRocca RL. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst Rev. 2013;2:CD007651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: a meta-analysis. CMAJ. 2009;180:719-726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Williams AJ, Henley WE, Williams CA, Hurst AJ, Logan S, Wyatt KM. Systematic review and meta-analysis of the association between childhood overweight and obesity and primary school diet and physical activity policies. Int J Behav Nutr Phys Act. 2013;10:101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. 5-2-1-0 Let’s Go. http://www.letsgo.org. Accessed May 16, 2014.
- 16. Polacsek M, Orr J, Letourneau L, et al. Impact of a primary care intervention on physician practice and patient and family behavior: keep ME Healthy—the Maine Youth Overweight Collaborative. Pediatrics. 2009;123(suppl 5):S258-S266. [DOI] [PubMed] [Google Scholar]
- 17. Rogers VW, Motyka E. 5-2-1-0 goes to school: a pilot project testing the feasibility of schools adopting and delivering healthy messages during the school day. Pediatrics. 2009;123(suppl 5):S272-S276. [DOI] [PubMed] [Google Scholar]
- 18. Tucker S, Lanningham-Foster L, Murphy J, et al. A school-based community partnership for promoting healthy habits for life. J Community Health. 2011;36:414-422. [DOI] [PubMed] [Google Scholar]
- 19. Minnesota Department of Education. Minnesota Report Card. http://rc.education.state.mn.us/#mySchool. Accessed June 10, 2014.
- 20. Branch MJ. Court interpreter program. http://www.mncourts.gov/?page=3937. Accessed June 10, 2014.
- 21. Maine Healthy Habits Survey ages 2-9 years. https://cdn1.sph.harvard.edu/wp-content/uploads/sites/84/2012/11/5210_healthy_habits_survey_age2-9.pdf. Accessed June 10, 2014.
- 22. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Foster BA, Farragher J, Parker P, Sosa ET. Treatment interventions for early childhood obesity: a systematic review. Acad Pediatr. 2015;15:353-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Huber JM, Shapiro JS, Wieland ML, et al. Telecoaching plus a portion control plate for weight care management: a randomized trial. Trials. 2015;16:323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. LeRouge C, Dickhut K, Lisetti C, Sangameswaran S, Malasanos T. Engaging adolescents in a computer-based weight management program: avatars and virtual coaches could help. J Am Med Inform Assoc. 2016;23:19-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Resnicow K, McMaster F, Bocian A, et al. Motivational interviewing and dietary counseling for obesity in primary care: an RCT. Pediatrics. 2015;135:649-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Amaya-Castellanos C, Shamah-Levy T, Escalante-Izeta E, et al. Development of an educational intervention to promote healthy eating and physical activity in Mexican school-age children. Eval Program Plann. 2015;52:159-168. [DOI] [PubMed] [Google Scholar]
- 28. van Sluijs EM, McMinn AM, Griffin SJ. Effectiveness of interventions to promote physical activity in children and adolescents: systematic review of controlled trials. BMJ. 2007;335:703. [DOI] [PMC free article] [PubMed] [Google Scholar]


