Abstract
Objectives: To document the temporal trends in alternative primary care models in which physicians, nurse practitioners (NPs), or physician assistants (PAs) engaged in care provision to the elderly, and examine the role of these models in serving elders with multiple chronic conditions and those residing in rural and health professional shortage areas (HPSAs). Design: Serial cross-sectional analysis of Medicare claims data for years 2008, 2011, and 2014. Setting: Primary care outpatient setting. Participants: Medicare fee-for-service beneficiaries who had at least 1 primary care office visit in each study year. The sample size is 2 471 498. Measurements: Physician model—Medicare beneficiary’s primary care office visits in a year were conducted exclusively by physicians; shared care model—conducted by a group of professionals that included physicians and either NPs or PAs or both; NP/PA model: conducted either by NPs or PAs or both. Results: There was a decrease in the physician model (85.5% to 70.9%) and an increase in the shared care model (11.9% to 23.3%) and NP/PA model (2.7% to 5.9%) from 2008 to 2014. Compared with the physician model, the adjusted odds ratio (AOR) of receiving NP/PA care was 3.97 (95% CI 3.80-4.14) in rural and 1.26 (95% CI 1.23-1.29) in HPSAs; and the AOR of receiving shared care was 1.66 (95% CI 1.61-1.72) and 1.14 (95% CI 1.13-1.15), respectively. Beneficiaries with 3 or more chronic conditions were most likely to received shared care (AOR = 1.67, 95% CI 1.65-1.70). Conclusion: The increase in shared care practice signifies a shift toward bolstering capacity of the primary care delivery system to serve elderly populations with growing chronic disease burden and to improve access to care in rural and HPSAs.
Keywords: primary care, multiple chronic conditions, access to care, nurse practitioners, physician assistants
Primary care serves as the cornerstone of a high-performing and sustainable health care delivery system.1 Several concurrent trends have challenged the capacity of the US primary care system; these include shortages of primary care physicians, an aging population, and the growing complexity of chronic disease conditions with compounding psychosocial and health behavior problems.2 In 2012, 1 in 4, or 60 million US adults had multiple (≥2) chronic conditions.3 Resources required to care for this medically complex population are great: the 68% of the Medicare beneficiaries with multiple chronic conditions consumed 93% of Medicare spending in 2010.2 The need for care management of multiple chronic conditions, provision of both health prevention and treatment, and interventions for psychosocial and health behavior problems has challenged the traditional physician delivery model and has led to calls for greater multidisciplinary collaboration.4,5
A collaborative model with shared care of patient panels among primary care professionals, including physicians and nurse practitioners (NPs) or physician assistants (PAs), has been increasingly recognized as a potentially efficient care delivery model that maximizes the roles of primary care clinicians in response to the growing complexity of primary care delivery.5-9
Innovations in the primary care workforce are critical components of primary care reform;7,10 which hinges on effective collaboration.11 Evidence indicates that most NPs and PAs prefer collaborating with physicians.12 In light of increasing demand for primary care, current and projected shortages in primary care physicians, and growth in NPs and PAs,13 it is critical to understand the temporal trends in how primary care physicians, NPs, and PAs are engaged in their practice. Such knowledge is central to the development of strategies to enhance multidisciplinary collaboration and improve the capacity and efficiency of primary care delivery. Yet, very little is known in this regard. This study fills this gap in our knowledge by addressing 2 objectives: (1) document the temporal trends in alternative primary care delivery models among physicians, NPs, and PAs from 2008 to 2014 and (2) examine the role of these models in care provision to beneficiaries with multiple chronic conditions and those in health professional shortage areas (HPSAs) and rural areas, 2 pressing critical issues under primary care reform.
Methods
Source of Data and Study Cohort
We used Medicare claims data for a 5% national random sample of Medicare beneficiaries from years 2008, 2011, and 2014, including Medicare Beneficiary Summary file, Medicare Carrier file, Outpatient Standard Analytic file (OUTSAF), and Medicare Provider Analysis and Review file (MedPAR). The initial sample consisted of Medicare fee-for-service beneficiaries who had Part A and B coverage and resided in the 50 US states and District of Columbia; beneficiaries who were originally entitled to Medicare due to disability or end-stage renal disease and those with any nursing home stay were excluded. The final sample is limited to those beneficiaries who had at least one outpatient primary care office visit in each study year. We included all visits that each beneficiary had in each study year. The sample size is 775 556 for 2008, 854 418 for 2011, and 841 524 for year 2014. The study was approved by the institutional review board.
Identification of Primary Care Office Visits
Primary care visits were identified using the Medicare Claims Criteria for Selection of Primary Care Visits developed by the Health Resources and Services Administration, which include services rendered by offices, hospital outpatient clinics, rural health clinics, and federally qualified health centers.14 Primary care professionals included physicians as well as NPs and PAs. Physician specialties include general practice, family practice, internal medicine, and geriatrics, which were identified in Part B Medicare claims. Nurse practitioner specialties include general, adult, family, gerontology, and women’s health and physician assistant specialties include medical; which were identified through linking Medicare data with the National Provider Identifier registry.15
Classification of Primary Care Models
We classified 3 primary care models: (1) physician model—if a Medicare beneficiary’s primary care office visits in a year were conducted exclusively by physicians; (2) shared care model—if a Medicare beneficiary’s primary care office visits in a year were provided by a group of professionals that included physicians and either NPs or PAs or both; and (3) NP/PA model—if a Medicare beneficiary’s primary care office visits in a year were conducted either by NPs or PAs or both, and not by physicians. We use the term of shared care in its extended definition that encompasses broad multidisciplinary care provision,5,9 including care provided by a team or by a group.
Measures
Patient age, sex, race or ethnicity, and Medicaid eligibility were obtained from the Medicare Beneficiary Summary file. We defined and classified 15 chronic conditions according to the classification scheme developed by the Department of Health and Human Services.16 Chronic conditions and the number of hospitalizations were generated from the claims in the year prior to each study year. Geographic location, including urban/rural, primary care HPSA designation, and region, was determined based on residential zip code. Urban/rural location was categorized into metropolitan (if in a metropolitan county), nonmetropolitan urban (if in a county with an urban population of 2500 or more), or rural (if in a county that was completely rural or had less than 2500 urban populations) based on rural-urban continuum codes.17 The primary care HPSA designation was determined using data from the Health Resources and Services Administration.18
Statistical Analyses
We evaluated beneficiary characteristics, including demographics, clinical conditions, and geographic location, for years 2008, 2011, and 2014. To examine whether a primary care model was more likely to be delivered to beneficiaries with multiple chronic conditions and those who resided in rural and HPSAs, we performed multinomial logistic regression, adjusting for beneficiary characteristics, using 2014 data. To assess which patient characteristics were associated with the largest increase in shared care, we built a multinomial logistic regression model to test the interaction between year and the characteristics using all 3 years of data. Since all interactions were statistically significant, stratified models were conducted for each level of the characteristics to estimate the adjusted odds ratio (AOR) of increasing use of the shared care model compared with the physician model. We used Bonferroni correction to adjust for multiple comparisons in the stratified models.
We conducted sensitivity analyses to examine whether the number of primary care office visits per beneficiary in a year affected the designation of primary care model and beneficiary characteristics. First, we assessed the proportion of beneficiaries assigned to each primary care model stratified by number of primary care office visits, ranging from 1 to 20, for each year. The results showed that the proportion of shared care increased and the proportion of physician care decreased in samples with a higher number of primary care office visits (Supplementary Table S1). Second, we ran the analyses using different cutoff values for the sample inclusion criteria: ≥1 visit or ≥2 visits. Using the criterion of at least 1 visit underestimated the proportion of shared care; however, using the criterion of at least 2 visits excluded patients with only a single visit (less morbid patients), which biased the results as the NP/PA model tended to serve a larger proportion of patients with 1 visit. Despite these differences, the sensitivity analysis indicated that the overall temporal trends in care models are consistent using either criterion. Therefore, we chose to use the more complete sample with at least one primary care office visit. Furthermore, we validated our multinomial logistic regression models by comparing models with and without adjustment for number of primary care office visits, while adjusting for the same set of variables for beneficiary characteristics; and we found consistent results. All statistical tests were 2-sided with significance level set at .05. Analyses were performed using SAS version 9.3 (SAS Inc, Cary, NC).
Results
Beneficiary Characteristics
Supplementary Table S2 shows the characteristics of beneficiaries by primary care model for years 2008, 2011, and 2014. The age distribution was similar between the shared care model and the physician model over time. The shared care model served a lower proportion of racial/ethnic minorities and Medicaid eligible beneficiaries than the physician model and the NP/PA model.
The average number of chronic conditions among beneficiaries was highest in the shared care model, and it increased in all care models from 2008 to 2014. In 2014, the average number of chronic conditions was 2.5 in the shared care model, 2.1 in the physician model, and 1.8 in the NP/PA model. Further, the shared care model had a higher proportion of beneficiaries with 3 or more chronic conditions than the physician model or the NP/PA model in all study years, which was 47% in 2014. Examination of each of 15 chronic conditions separately by type of care model showed that the shared care model tended to have a higher prevalence of each chronic condition compared with the physician model and the NP/PA model (Supplementary Table S3). Similarly, the number of hospitalizations was highest in the shared care model followed by the physician model and the NP/PA model.
Rural beneficiaries accounted for a small proportion of the total beneficiaries in each care model. The proportion ranged from 4.1% in 2008 to 3.1% in 2014 in the shared care model, 2.2% to 1.9% in the physician model, and 7.6% to 6.5% in the NP/PA model. The proportion of beneficiaries in primary care HPSAs in the shared care model ranged from 50% in 2008 to 61.4% in 2014, compared with 45.1% to 56.8% in the physician model, and 53.8% to 66.7% in the NP/PA model. A large proportion of beneficiaries were in the South across care models.
Trends in the Proportion of Primary Care Models
Figure 1 shows the trends in the prevalence of primary care models. The shared care model increased from 11.9% in 2008 to 23.3% in 2014, and the physician model decreased from 85.5% to 70.9% during the same period. The NP/PA model accounted for a very small proportion and increased from 2.7% to 5.9%. We further examined 3 types of shared care: MD-NP, MD-PA, and MD-NP-PA. We found that MD-NP increased from 6.2% in 2008 to 11.5% in 2014; MD-PA increased from 4.9% to 9.0%; and MD-NP-PA increased from 0.8% to 2.8%.
Figure 1.
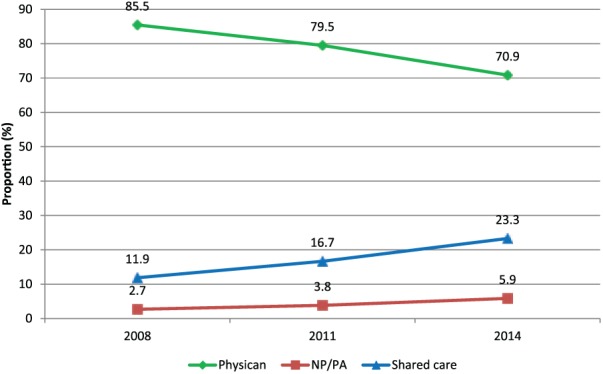
Trends in the proportion of primary care model, Medicare beneficiaries, years 2008, 2011, and 2014.
Data presented were based on Medicare claims data for a 5% national random sample of Medicare beneficiaries who had at least 1 outpatient primary care office visit: for year 2008, for year 2011, and for year 2014. The figure shows the proportion of beneficiaries assigned to each primary care model.
NP, nurse practitioner; PA, physician assistant.
We next examined which patient characteristics were associated with the largest increase in shared care (Table 1). We present the growth by characteristics in two ways. The first is the absolute increase in the percentage of beneficiaries receiving shared care. The second is the relative increase compared with the physician model from the stratified adjusted models. The shared care model increased in all demographics categories, clinical conditions, and geographic locations. There was higher initial use and higher increased use of the shared care model in Whites compared with Blacks and Hispanics. Higher initial use and higher increased use was also found in sicker beneficiaries shown in 2 aspects: beneficiaries with 3 or more chronic conditions and those with previous hospitalizations.
Table 1.
Proportion of Medicare Beneficiaries Served by Shared Care Model by Beneficiary Characteristics, Years 2008, 2011, and 2014.
| Year |
Difference Between 2008 and 2014 |
||||||
|---|---|---|---|---|---|---|---|
| 95% CI |
|||||||
| Characteristics | 2008 (%) | 2011 (%) | 2014 (%) | Absolute Increase in % | AOR | Lower Limit | Upper Limit |
| Overall | 11.86 | 16.66 | 23.29 | 11.43 | 2.32 | 2.30 | 2.34 |
| Age group, years | |||||||
| 66-70 | 11.56 | 16.27 | 22.57 | 11.01 | 2.37 | 2.30 | 2.43 |
| 71-75 | 12.00 | 16.77 | 23.57 | 11.57 | 2.35 | 2.29 | 2.41 |
| 76-80 | 12.22 | 17.30 | 24.22 | 12.00 | 2.33 | 2.26 | 2.40 |
| 81-85 | 11.98 | 16.99 | 23.98 | 12.00 | 2.34 | 2.27 | 2.42 |
| >85 | 11.36 | 15.79 | 21.79 | 10.43 | 2.19 | 2.11 | 2.27 |
| Sex | |||||||
| Male | 11.29 | 15.83 | 22.26 | 10.97 | 2.30 | 2.25 | 2.35 |
| Female | 12.24 | 17.15 | 23.93 | 11.69 | 2.34 | 2.30 | 2.38 |
| Race | |||||||
| White | 12.32 | 17.37 | 24.24 | 11.92 | 2.33 | 2.30 | 2.36 |
| Black | 8.17 | 11.77 | 16.82 | 8.65 | 2.29 | 2.15 | 2.44 |
| Hispanic | 7.57 | 9.89 | 14.76 | 7.57 | 2.14 | 1.84 | 2.48 |
| Other | 7.49 | 9.24 | 14.11 | 6.62 | 2.00 | 1.83 | 2.18 |
| Medicaid eligibility | |||||||
| Yes | 11.12 | 14.44 | 19.74 | 8.62 | 2.06 | 1.97 | 2.16 |
| No | 11.94 | 16.89 | 23.60 | 11.66 | 2.34 | 2.31 | 2.38 |
| No. of chronic conditions | |||||||
| 0 | 9.88 | 12.63 | 17.61 | 7.73 | 2.12 | 2.06 | 2.19 |
| 1 | 11.50 | 15.63 | 21.68 | 10.18 | 2.25 | 2.19 | 2.32 |
| 2 | 11.78 | 16.26 | 22.81 | 11.03 | 2.33 | 2.26 | 2.39 |
| 3+ | 13.78 | 19.40 | 27.09 | 13.31 | 2.47 | 2.41 | 2.52 |
| No. of prior hospitalizations | |||||||
| 0 | 11.25 | 15.91 | 22.43 | 11.18 | 2.31 | 2.28 | 2.34 |
| 1 | 14.48 | 20.12 | 28.11 | 13.63 | 2.40 | 2.31 | 2.48 |
| 2 | 15.69 | 21.98 | 29.76 | 14.07 | 2.36 | 2.20 | 2.54 |
| 3+ | 17.15 | 22.58 | 31.26 | 14.11 | 2.33 | 2.10 | 2.58 |
| Urban/rural | |||||||
| Metro | 10.73 | 15.45 | 22.07 | 11.34 | 2.39 | 2.35 | 2.42 |
| Urban | 15.48 | 20.93 | 27.67 | 12.19 | 2.20 | 2.14 | 2.27 |
| Rural | 19.12 | 23.08 | 29.92 | 10.80 | 1.96 | 1.82 | 2.11 |
| Primary care HPSA | |||||||
| Yes | 12.91 | 17.71 | 24.46 | 11.55 | 2.28 | 2.24 | 2.32 |
| No | 10.97 | 15.57 | 21.63 | 10.66 | 2.39 | 2.34 | 2.44 |
| Region | |||||||
| Northeast | 11.46 | 15.31 | 20.71 | 9.25 | 2.11 | 2.05 | 2.19 |
| Midwest | 12.48 | 18.23 | 25.21 | 12.73 | 2.35 | 2.29 | 2.41 |
| South | 11.29 | 16.75 | 24.37 | 13.08 | 2.60 | 2.55 | 2.66 |
| West | 12.19 | 15.61 | 20.91 | 8.00 | 1.91 | 1.85 | 1.97 |
Abbreviations: AOR, adjusted odds ratio; CI, confidence interval; HPSA, health professional shortage area.
Use of Primary Care Models in Beneficiaries With Multiple Chronic Conditions and Beneficiaries in Rural and HPSAs
Table 2 presents beneficiary characteristics associated with care models in 2014. The shared care model was more likely to be used than the physician model in caring for beneficiaries with chronic conditions, with previous hospitalizations, and those residing in rural or primary care HPSAs. Among those with 1, 2, or at least 3 chronic conditions, the AORs were 1.3, 1.3, and 1.7, respectively; among beneficiaries with 1, 2, or at least 3 previous hospitalizations, the AORs were 1.2, 1.3, and 1.4, respectively. Conversely, the NP/PA model was less likely to be used in beneficiaries with a chronic condition than the physician model. These findings indicate that the shared care model served a sicker population.
Table 2.
Result of Multinomial Logistic Regression of Medicare Beneficiaries’ Characteristics on Primary Care Model, Year 2014.a
| NP/PA Model |
Shared Care Model |
|||||
|---|---|---|---|---|---|---|
| 95% CI |
95% CI |
|||||
| Characteristics | Odds Ratio | Lower Limit | Upper Limit | Odds Ratio | Lower Limit | Upper Limit |
| Age group, years | ||||||
| 71-75 vs 66-70 | 0.87 | 0.85 | 0.90 | 0.99 | 0.98 | 1.01 |
| 76-80 vs 66-70 | 0.78 | 0.76 | 0.80 | 0.97 | 0.96 | 0.99 |
| 81-85 vs 66-70 | 0.71 | 0.69 | 0.73 | 0.93 | 0.92 | 0.95 |
| >85 vs 66-70 | 0.63 | 0.61 | 0.65 | 0.82 | 0.80 | 0.83 |
| Sex | ||||||
| Male vs female | 0.91 | 0.89 | 0.93 | 0.87 | 0.87 | 0.88 |
| Race/ethnicity | ||||||
| Black vs white | 0.75 | 0.71 | 0.78 | 0.60 | 0.59 | 0.62 |
| Hispanic vs white | 0.70 | 0.63 | 0.78 | 0.59 | 0.56 | 0.63 |
| Other vs white | 0.57 | 0.54 | 0.60 | 0.55 | 0.53 | 0.57 |
| Medicaid eligibility | ||||||
| Yes vs no | 1.35 | 1.31 | 1.40 | 0.88 | 0.86 | 0.89 |
| Number of chronic conditions | ||||||
| 1 vs 0 | 0.74 | 0.72 | 0.76 | 1.27 | 1.24 | 1.29 |
| 2 vs 0 | 0.62 | 0.60 | 0.64 | 1.34 | 1.32 | 1.37 |
| 3+ vs 0 | 0.57 | 0.55 | 0.58 | 1.67 | 1.65 | 1.70 |
| Hospitalizations in prior year | ||||||
| 1 vs 0 | 1.20 | 1.16 | 1.24 | 1.17 | 1.15 | 1.19 |
| 2 vs 0 | 1.19 | 1.12 | 1.28 | 1.27 | 1.23 | 1.31 |
| 3+ vs 0 | 1.24 | 1.12 | 1.37 | 1.37 | 1.31 | 1.44 |
| Rural/urban | ||||||
| Urban vs metro | 2.35 | 2.30 | 2.41 | 1.37 | 1.35 | 1.39 |
| Rural vs metro | 3.97 | 3.80 | 4.14 | 1.66 | 1.61 | 1.72 |
| Primary care HPSA | ||||||
| Yes vs no | 1.26 | 1.23 | 1.29 | 1.14 | 1.13 | 1.15 |
| Region | ||||||
| Midwest vs Northeast | 1.18 | 1.14 | 1.21 | 1.29 | 1.27 | 1.31 |
| South vs Northeast | 1.11 | 1.08 | 1.15 | 1.27 | 1.25 | 1.28 |
| West vs Northeast | 1.36 | 1.32 | 1.41 | 1.15 | 1.13 | 1.18 |
Abbreviations: CI, confidence interval; NP, nurse practitioner; PA, physician assistant.
Reference: physician model.
Compared with beneficiaries residing in metropolitan areas, those residing in nonmetropolitan urban or rural areas had 37% and 66% greater odds of being in the shared care model than in the physician model. Compared with beneficiaries residing in non-HPSA areas, beneficiaries residing in HPSA areas had 14% greater odds of being cared for by the shared care model than by the physician model. Although the NP/PA model served the smallest proportion of beneficiaries in urban/rural and HPSAs/non-HPSAs, beneficiaries residing in nonmetropolitan urban (AOR = 2.35), rural (AOR = 3.97), or HPSA areas (AOR = 1.26) were the most likely to receive care from the NP/PA model.
Discussion
In 2014, the shared care model accounted for 23%, an increase from 12% in 2008. Nationally, the traditional physician care model remains the most prevalent model, followed by the shared care model. However, a decrease in the physician model and concomitant increase in the shared care model indicates a significant shift in primary care delivery.
Our study showed that this shift toward increased shared care was associated with the care delivery to select groups. Beneficiaries with multiple chronic conditions and hospitalizations were most likely to receive shared care. Furthermore, the shared care model played a considerable role in caring for beneficiaries in rural and HPSAs. These findings provided empirical evidence in support of a prior recommendation of sharing the care to improve primary care system capacity.5 As the presence of multiple chronic conditions represents high costs to health care and as its prevalence continues to increase, especially among vulnerable populations in rural and HPSAs,19,20 fostering the shared care model is very likely to attain synergistic and double-edge effects. It will bolster primary care system capacity for care delivery to individuals with multiple chronic conditions and will expand access to care to populations most in need. The former is consistent with 1 of the 4 overarching goals established by the Department of Health and Human Services, which is to “Foster health care and public health system changes to improve the health of individuals with multiple chronic conditions.”21 The latter, improving access to care for vulnerable populations, is a national priority.
A pronounced change in Medicare to incentivize primary care professionals to improve the health of individuals with multiple chronic conditions is the new payment policy for chronic care management. Medicare began to reimburse non–face-to-face primary care services to physicians, NPs, and PAs for managing the care of fee-for-service beneficiaries with two or more chronic conditions in 2015.22 One of the requirements for billing is the provision of 24/7 chronic care management services. This policy might stimulate more shared care practices among physicians and NPs or PAs in undertaking required chronic care management services.
The NP/PA model accounted for a very small proportion of care provision to Medicare beneficiaries and increased slightly over time, which is consistent with a previous study.23 Although many states have granted greater practice authority to NPs and PAs since 2008 and NPs can do solo practice,24,25 our study demonstrates that the majority of care provided by NPs and PAs consisted of shared care with physicians. These findings are consistent with the evidence that most NPs and PAs prefer collaborating with physicians.12 Care provided solely by NPs and/or PAs were most likely to be in rural and health professional shortage areas where accessibility of physicians was low. The NP/PA model helped fill the primary care needs of these underserved populations.
It is important to continue to monitor trends in these primary care models. The Health Resources and Services Administration estimated that there will be a shortage of 23 640 full-time equivalent primary care physicians by 2025, with shortages prevalent in most states.13 In contrast, all states are predicted to have a surplus of NPs and most states will have a surplus of PAs.13 Based on the patterns of provider utilization and health care delivery in 2013, the period covered by our study, HRSA indicated that the projected shortage of physicians can be effectively mitigated if NP and PA services are fully utilized. As shown in our study, NP and PA care are provided through either the shared care model or NP/PA model. A continued growth of these models is likely. However, it should be recognized that the models of primary care delivery can be affected by many factors. For example, there has been a growth in adoption of telehealth, which can help expand access to primary care and influence how primary care professionals are involved in care delivery.8,26
Our study was based on services billed in Medicare claims data, which limited the research questions that could be addressed. Future studies are warranted to investigate the nature of shared care among primary care professionals and its impact on patient centered outcomes. The shared care we defined in this paper includes care provided by a team in the same practice location or care provided by a group that may or may not be in the same practice location. Team care and group care are distinct in the way professionals work together.27 The value of effective team care has been well documented,28 research is needed for group care in patient-centered integrated delivery system. We also need to better understand the factors that underlie these observed shifts in primary care delivery from health care financing and organizational perspectives. Our study included primary care physicians, NPs, and PAs as primary care professionals.13 Other professionals such as pharmacists have been recognized as primary care clinician in some states.29 Future research needs to consider this issue. Nonetheless, the growing trend toward shared care aligns with the extant evidence of a substantial adoption of team care in primary care delivery. Nationally, 53% of office-based primary care physicians worked with NPs or PAs in 2012.30
The study findings and their implications should be interpreted in the context of the following limitations. First, there might be bias in the estimation of the prevalence of actual care delivery models as the classification of care model is based on claim data. Nonetheless, our primary purpose was to examine the temporal trends among alternative primary care models. Second, this study might underestimate the shared care model or the NP/PA model, and overestimate the traditional physician model due to “incident billing,” in which NPs and PAs who provide care under the direct supervision of a physician are billed under the physician. To examine whether “incident billing” would affect the study results, we repeated our analyses using data from the states that NPs had full scope-of-practice authority and were not required to provide care under a collaborative agreement with or the direct supervision of a physician. The rate of incident billing was lower in these states compared to states with reduced or restricted NP practice authority.31 We found consistent results. Third, we were unable to calculate patient panel size due to the limitation that the data is a 5% random sample, which would otherwise provide a more thorough picture of the capacity of the primary care model. Fourth, our study was based on office visits and did not include nonoffice visits. In our data, we observed a general decline in rural beneficiaries across three care models over time, which might be due to increased use of telemedicine visits.32 Fifth, focusing on patients with Medicare fee-for-service coverage limits generalization to Medicaid beneficiaries and privately insured patients. Future studies are needed to examine whether similar patterns and rates of growth of the three care models exist in patients with Medicaid or commercial insurance.
Conclusions
We found that primary care physicians, NPs, and PAs are increasingly engaged in shared care practice. The increase in shared care practice signifies a shift toward bolstering capacity of the primary care delivery system to serve elderly populations with a growing chronic disease burden and improving access to care in rural and HPSAs.
Author Biographies
Ying Xue, DNSc, is an associate professor in the School of Nursing, University of Rochester. Her research interests are in the areas of nursing workforce and healthcare delivery and outcomes.
James S. Goodwin, MD, is the George and Cynthia Mitchell Distinguished Chair of Geriatric Medicine at the University of Texas Medical Branch (UTMB) in Galveston, Texas. He has been continuously NIH funded to study patterns and outcomes of medical care for the elderly for more than 25 years. Much of his work has involved systematic studies into the mechanisms underlying differences in medical care and outcomes in the elderly and in racial and ethnic minorities.
Deepak Adhikari, MS, was a biostatistician at the UTMB Department of Preventive Medicine and Community Health. His areas of expertise include data management, statistical programming – SAS, R, and Stata, and analysis of Medicare and other large claims data.
Mukaila A. Raji, MD MS, FACP, is the Edgar Gnitzinger Distinguished professor of Aging and director of the UTMB Division of Geriatric Medicine. He is a board-certified geriatrician with over 15 years’ experience in comparative drug effectiveness and toxicity research, cognitive aging and disability, and health policy and outcomes.
Yong-Fang Kuo, PhD is a professor of Preventive Medicine and Community Health, and director of the UTMB Office of Biostatistics. She has over 15 years’ experience in health policy and outcomes, comparative effectiveness, and toxicity research. Her statistics expertise includes hierarchical generalized linear mix model, survival data analysis, and instrumental variable analysis.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study was supported by grants R01-HS020642 and R24-HS022134 from the Agency for Healthcare Research and Quality and UL1TR001439 from the National Institutes of Health.
Supplementary Material: Supplementary material is available for this article online.
References
- 1. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83:457-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Centers for Medicare and Medicaid Services. Chronic Conditions Among Medicare Beneficiaries, Chartbook, 2012 Edition. Baltimore, MD: Centers for Medicare and Medicaid Services; 2012. [Google Scholar]
- 3. Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: a 2012 update. Prev Chronic Dis. 2014;11:E62. doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Osborn R, Moulds D, Schneider EC, Doty MM, Squires D, Sarnak DO. Primary care physicians in ten countries report challenges caring for patients with complex health needs. Health Aff (Millwood). 2015;34:2104-2112. [DOI] [PubMed] [Google Scholar]
- 5. Ghorob A, Bodenheimer T. Sharing the care to improve access to primary care. N Engl J Med. 2012;366:1955-1957. [DOI] [PubMed] [Google Scholar]
- 6. Everett C, Thorpe C, Palta M, Carayon P, Bartels C, Smith MA. Physician assistants and nurse practitioners perform effective roles on teams caring for Medicare patients with diabetes. Health Aff (Millwood). 2013;32:1942-1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Friedman A, Hahn KA, Etz R, et al. A typology of primary care workforce innovations in the United States since 2000. Med Care. 2014;52:101-111. [DOI] [PubMed] [Google Scholar]
- 8. Green LV, Savin S, Lu Y. Primary care physician shortages could be eliminated through use of teams, nonphysicians, and electronic communication. Health Aff (Millwood). 2013;32:11-19. [DOI] [PubMed] [Google Scholar]
- 9. Thompson M, Walter F. Increases in general practice workload in England. Lancet. 2016;387:2270-2272. [DOI] [PubMed] [Google Scholar]
- 10. Tinetti ME, Basu J. Research on multiple chronic conditions: where we are and where we need to go. Med Care. 2014;52(suppl 3):S3-S6. [DOI] [PubMed] [Google Scholar]
- 11. Blumenthal D, Abrams MK. Putting aside preconceptions—time for dialogue among primary care clinicians. N Engl J Med. 2013;368:1933-1934. [DOI] [PubMed] [Google Scholar]
- 12. Buerhaus PI, DesRoches CM, Dittus R, Donelan K. Practice characteristics of primary care nurse practitioners and physicians. Nurs Outlook. 2015;63:144-153. [DOI] [PubMed] [Google Scholar]
- 13. US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. National and Regional Projections of Supply and Demand for Primary Care Practitioners: 2013-2025. Rockville, MD: Health Resources and Services Administration; 2016. [Google Scholar]
- 14. Health Resources and Services Administration. Primary Care Service Area Version 3.1 Methods. https://datawarehouse.hrsa.gov/DataDownload/PCSA/2010/PCSA_Version3.1_methods_9_17_2013.pdf. Published September 17, 2013. Accessed September 26, 2017.
- 15. Center for Medicare and Medicaid Services. National Provider Identifier. 2017. https://nppes.cms.hhs.gov/NPPES/Welcome.do. Accessed September 26, 2017.
- 16. Goodman RA, Posner SF, Huang ES, Parekh AK, Koh HK. Defining and measuring chronic conditions: imperatives for research, policy, program, and practice Prev Chronic Dis. 2013;10:E66. doi: 10.5888/pcd10.120239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Department of Agriculture, Economic Research Service. Rural-urban continuum codes. 2013. http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx. Accessed September 26, 2017.
- 18. US Health Resources and Services Administration. Health professional shortage area data. http://datawarehouse.hrsa.gov/data/datadownload/hpsadownload.aspx. Accessed February 3, 2016.
- 19. Huang ES, Finegold K. Seven million Americans live in areas where demand for primary care may exceed supply by more than 10 percent. Health Aff (Millwood). 2013;32:614-621. [DOI] [PubMed] [Google Scholar]
- 20. Ku L, Jones K, Shin P, Bruen B, Hayes K. The states’ next challenge—securing primary care for expanded Medicaid populations. N Engl J Med. 2011;364:493-495. [DOI] [PubMed] [Google Scholar]
- 21. US Department of Health and Human Services. Multiple Chronic Conditions—A Strategic Framework: Optimum Health and Quality of Life for Individuals with Multiple Chronic Conditions. Washington, DC: US Department of Health and Human Services; 2010. [Google Scholar]
- 22. US Department of Health and Human Services, Center for Medicare and Medicaid Services. Chronic Care Management Services. 2015. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/Downloads/ChronicCareManagement.pdf. Accessed February 19, 2016.
- 23. Kuo YF, Loresto FL, Jr, Rounds LR, Goodwin JS. States with the least restrictive regulations experienced the largest increase in patients seen by nurse practitioners. Health Aff (Millwood). 2013;32:1236-1243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Gadbois EA, Miller EA, Tyler D, Intrator O. Trends in state regulation of nurse practitioners and physician assistants, 2001 to 2010. Med Care Res Rev. 2015;72:200-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Xue Y, Ye Z, Brewer C, Spetz J. Impact of state nurse practitioner scope-of-practice regulation on healthcare delivery: systematic review. Nurs Outlook. 2016;64:71-85. [DOI] [PubMed] [Google Scholar]
- 26. Dorsey ER, Topol EJ. State of telehealth. N Engl J Med. 2016;375:1400. doi: 10.1056/NEJMc1610233. [DOI] [PubMed] [Google Scholar]
- 27. Grumbach K, Bodenheimer T. Can health care teams improve primary care practice? JAMA. 2004;291:1246-1251. [DOI] [PubMed] [Google Scholar]
- 28. Mitchell P, Wynia M, Golden R, et al. Core Principles & Values of Effective Team-Based Health Care (Discussion paper). Washington, DC: Institute of Medicine; 2012. [Google Scholar]
- 29. Gabay M. A step forward: review of the new California provider status law. Hosp Pharm. 2014;49:435-436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hing E, Hsiao CJ. State variability in supply of office-based primary care providers: United States, 2012. NCHS Data Brief. 2014;(151):1-8. [PubMed] [Google Scholar]
- 31. Park J, Athey E, Pericak A, Pulcini J, Greene J. To what extent are state scope of practice laws related to nurse practitioners’ day-to-day practice autonomy? [published online November 11, 2016] Med Care Res Rev. doi: 10.1177/1077558716677826. [DOI] [PubMed] [Google Scholar]
- 32. Mehrotra A, Jena AB, Busch AB, Souza J, Uscher-Pines L, Landon BE. Utilization of Telemedicine among rural Medicare beneficiaries. JAMA. 2016;315:2015-2016. doi: 10.1001/jama.2016.2186. [DOI] [PMC free article] [PubMed] [Google Scholar]


