Abstract
Spontaneous splenic hematoma occurring during pregnancy is a rare entity. It often occurs in preexisting pathology of the spleen such as thalassemia or infectious etiologies such as malaria, typhoid, dengue, or infectious mononucleosis but most commonly after a trauma. The occurrence of splenic hematoma during pregnancy without any underlying cause is rare. Here, we present such a case and the diagnostic dilemma associated with it.
Keywords: Pregnancy, rupture uterus, splenic hematoma, splenomegaly
Introduction
Spontaneous splenic hematoma with laceration occurring during pregnancy is a rare entity. It often occurs in preexisting pathology of the spleen such as thalassemia or infectious etiologies such as malaria, typhoid dengue or infectious mononucleosis but most commonly after a trauma.[1] Because of vague presentation, the diagnosis is usually made late in the course of the disease with poor outcome. Splenomegaly can lead to splenic hematoma with laceration and the incidence is 2%–5%.[2] Further, the risk of splenic rupture may increase in pregnancy due to several physiological and mechanical reasons.[3] The causes of massive splenomegaly are chronic infections and inflammatory and hematological conditions. Spontaneous rupture of an enlarged spleen though rare can be catastrophic.[3] Our case is unique in view of idiopathic cause of splenomegaly which leads to splenic hematoma along with laceration in the third trimester of pregnancy.
Case Report
A 24-year-old primigravida at 36 weeks of gestation was admitted to the Gynec causality in view of severe anemia and pain in the abdomen with heart failure. No history of trauma, fever, bleeding per vaginam, blood transfusion, and hypertension was present. On examination, the patient had severe pallor (5–6 g%), tachycardia, hypotension (blood pressure [BP] 90/60 mmHg), and signs of congestive heart failure. Per-abdominal examination revealed tense and distended abdomen, uterine contour, and fetal part could not be made out and fetal heart was not localized. Transabdominal scan revealed moderate free fluid, single intrauterine dead fetus, no retroplacental clot, anterior uterine wall intact, and posterior uterine wall could not be made out because of distended bowel loops with approximately 14 cm × 12 cm of heteroechoic collection seen around the splenic area. Paracentesis revealed frank blood. On investigation, hemoglobin (Hb) was 6.4 g/dl and total leukocyte count and platelet count were normal. Her liver function test and kidney function test and coagulation profile were normal. Probable diagnosis of rupture uterus was made and she was immediately shifted for laparotomy. Peroperative findings revealed massive hemoperitoneum (2.5 L of blood), clear liquor, and no retroplacental clots. A dead female baby weighing 2.4 kg was extracted as cephalic presentation [Figure 1]. Uterus was intact, bilateral adnexa was normal, and there was no uterine cause of bleeding. Large splenic hematoma of approximately 15 cm × 10 cm with 3-cm splenic laceration was found. Splenectomy was performed by surgeons.
Figure 1.
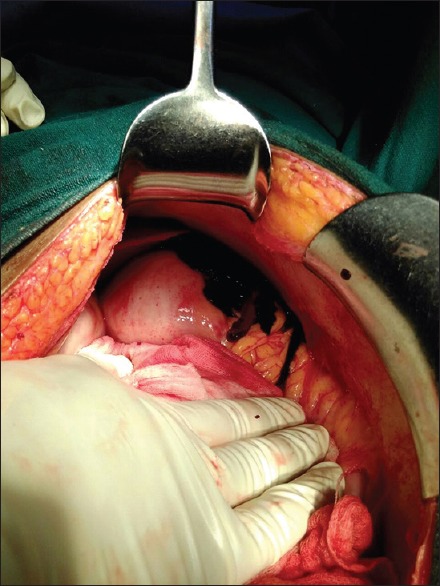
Splenic hematoma with laceration
She was given 6 units of packed cells (2 units intraoperative and 4 postoperative) over 3 days and hemoglobin increased to 8.8 g. Peripheral smear revealed hemolysis with erythroblast 30%, microcytic hypochromic anemia along with basophilic stippling. Iron studies were normal with reticulocytosis. Malaria and dengue were ruled out. Hb electrophoresis was also normal ruling out hemoglobinopathies. Her antinuclear antibody and RNA factor were negative. Postoperative period was uneventful. She was discharged on the 7th postoperative day. Her histopathology revealed congestive splenomegaly which was idiopathic [Figure 2]. She was followed up after 1 month and was fine.
Figure 2.
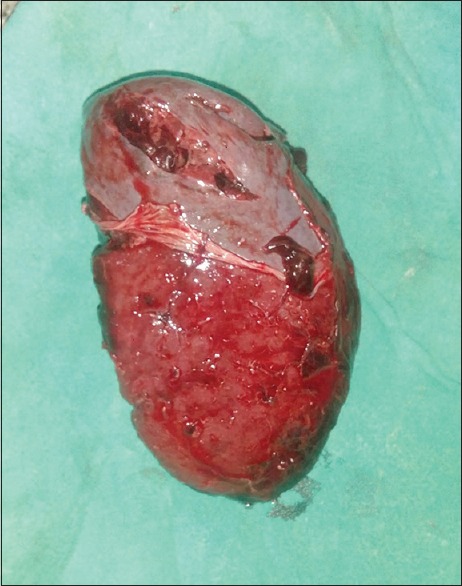
Congestive splenomegaly
Discussion
Splenic hematoma with laceration or rupture of the spleen is usually secondary to trauma to an enlarged spleen and is found approximately in 30% of patients undergoing surgery following blunt abdominal injury. It can present as sudden fatal hemorrhage or self-limited bleeding.[3] It is usually associated with 72% maternal mortality rate without proper diagnosis. About 80% splenic rupture occurs during the third trimester. Three cases of splenic rupture associated with pregnancy have been described, two during the antenatal period by de Graaff and Pijpers where neither mother nor fetus survived despite surgical intervention.[4] Even in the diseased spleen, spontaneous rupture is a rare event and occurs most commonly as a complication of malaria. Splenic preservation was achieved in one case of rupture in the third trimester by Fletcher et al.[5]
Another case was reported by Bhagrath et al. occurring in the early puerperium, where splenectomy was performed with a successful outcome.[6]
Hamsho and Mouchanta presented a study in November 1998 of rupture of the spleen during normal pregnancy following trauma in the third trimester of pregnancy.[7] Abruptio placenta was suspected preoperatively, but after cesarean section, exploration of abdominal cavity revealed a ruptured spleen and splenectomy was performed. Cause of rupture was large subcapsular central hematoma of the spleen with a central capsular tear. Disseminated intravascular coagulation, renal failure, adult respiratory distress syndrome, necrotizing enterocolitis, and bilateral hydrothorax were complications which were managed conservatively. The patient was discharged on 44th day and followed after 2 months without any complications.
Pregnancy can increase the risk of spontaneous rupture of the enlarged spleen as in. Pregnancy can worsen preexisting anemia and also trigger red blood cell hemolysis which in turn induces massive extramedullary hematopoiesis giving rise to increase in splenic size and finally splenic rupture. Mechanical factors such as reduction in the volume of peritoneal cavity and uterine contractions during pregnancy cause compression of the diaphragm which predisposes to splenic trauma. Frequent abdominal examinations and manipulation during labor can also give rise to splenic trauma. Fatal splenic rupture without any history of trauma has been reported in a pregnant woman with beta-thalassemia minor by Boldorini et al.[8] Three case reports have been reported of massive splenomegaly in pregnancy by Mittal et al. in 2013,[9] all presented differently and posed a diagnostic challenge, first presented with severe anemia, second as chronic pain abdomen, and third as recurrent fever and its adverse effects on pregnancy outcomes. Although none of their patients had life-threatening splenic rupture, they found an association of massive splenomegaly with fetal growth restriction and aggravation of preexisting anemia requiring blood components. All three cases managed conservatively. Causes of splenomegaly were beta thalassemia minor, extrahepatic portal hypertension, and third case with tropical splenomegaly syndrome. First, two of the cases underwent cesarean section and third had normal vaginal delivery.
But in our case, the patient presented with severe anemia with congestive heart failure in shock with no fetal growth restriction, but excessive hemorrhage lead to uteroplacental insufficiency which in turn lead to intrauterine fetal death.
Although splenectomy is the treatment of choice, it does result in reduced immune competence and therefore splenic tissue should be preserved wherever possible. Maternal death is mainly due to massive hemorrhage, shock, and consumptive coagulopathy.
Hamedi and Shomali reported a case of postpartum spontaneous rupture of the spleen in a woman with severe preeclampsia in 2013.[10] The patient underwent cesarean delivery for uncontrolled BP and low platelet count. She developed coffee-ground vomiting postoperatively and clinical evidence of free fluid was present. Emergent laparotomy was performed and a 2–3-cm splenic laceration was found bleeding actively from the ruptured site and was managed conservatively packing with gauge.
Conclusion
Splenic hematoma may mimic a clinical feature of ectopic pregnancy, abdominal pregnancy, uterine rupture, or an abruption of the placenta. The delay in recognition of the condition can lead to catastrophic consequences for both the mother and fetus. It should be considered as differential diagnosis of hemorrhagic shock in pregnancy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ali J. Spontaneous rupture of the spleen in patients with infectious mononucleosis. Can J Surg. 1993;36:49–52. [PubMed] [Google Scholar]
- 2.Kaplan LJ, Coffman D. Splenomegaly. eMedicine from WebMD. [Last accessed on 2004 Dec 29]. Available from: http://www.emedicine.com/med/topic2156.
- 3.Huchzermeyer H. Extrahepatic portal hypertension and pregnancy (author's transl) Leber Magen Darm. 1975;5:209–13. [PubMed] [Google Scholar]
- 4.de Graaff J, Pijpers PM. Spontaneous rupture of the spleen in third trimester of pregnancy. Report of a case and review of the literature. Eur J Obstet Gynecol Reprod Biol. 1987;25:243–7. doi: 10.1016/0028-2243(87)90105-5. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher H, Frederick J, Barned H, Lizarraga V. Spontaneous rupture of the spleen in pregnancy with splenic conservation. West Indian Med J. 1989;38:114–5. [PubMed] [Google Scholar]
- 6.Bhagrath R, Bearn P, Sanusi FA, Najjar S, Qureshi R, Simanovitz A, et al. Postpartum rupture of the spleen. Br J Obstet Gynaecol. 1993;100:954–5. doi: 10.1111/j.1471-0528.1993.tb15117.x. [DOI] [PubMed] [Google Scholar]
- 7.Hamsho MA, Mouchantat MR. Ruptured spleen in pregnancy. Qatar Med J. 1998;7:65–6. [Google Scholar]
- 8.Boldorini R, Bozzola C, Gallarotti E, Ribaldone R. Fatal splenic rupture in a pregnant woman with hemoglobin C/beta-thalassemia and myeloid metaplasia. Arch Pathol Lab Med. 2006;130:1231–2. doi: 10.5858/2006-130-1231-FSRIAP. [DOI] [PubMed] [Google Scholar]
- 9.Mittal P, Suri J, Bansiwal R. Massive splenomegaly in pregnancy: A review of three cases. J Evol Med Dent Sci. 2013;2:5042–6. [Google Scholar]
- 10.Hamedi B, Shomali Z. Postpartum spontaneous rupture of spleen in a woman with severe preeclampsia: Case report and review of the literature. Bull Emerg Trauma. 2013;1:46–8. [PMC free article] [PubMed] [Google Scholar]


