Abstract
Uterine leiomyomas, also known as uterine fibroids, are the most common pelvic tumors, occurring in nearly 70% of all reproductive-aged women and are the leading indication for hysterectomy worldwide. The development of uterine leiomyomas involve a complex and heterogeneous constellation of hormones, growth factors, stem cells, genetic, and epigenetic abnormalities. An increasing body of evidence emphasizes the important contribution of epigenetics in the pathogenesis of leiomyomas. Genome-wide methylation analysis demonstrates that a subset of estrogen receptor (ER) response genes exhibit abnormal hypermethylation levels that are inversely correlated with their RNA expression. Several tumor suppressor genes, including Kruppel-like factor 11 (KLF11), deleted in lung and esophageal cancer 1 (DLEC1), keratin 19 (KRT19), and death-associated protein kinase 1 (DAPK1) also display higher hypermethylation levels in leiomyomas when compared to adjacent normal tissues. The important role of active DNA demethylation was recently identified with regard to the ten-eleven translocation protein 1 and ten-eleven translocation protein 3-mediated elevated levels of 5-hydroxymethylcytosine in leiomyoma. In addition, both histone deacetylase and histone methyltransferase are reported to be involved in the biology of leiomyomas. A number of deregulated microRNAs have been identified in leiomyomas, leading to an altered expression of their targets. More recently, the existence of side population (SP) cells with characteristics of tumor-initiating cells have been characterized in leiomyomas. These SP cells exhibit a tumorigenic capacity in immunodeficient mice when exposed to 17β-estradiol and progesterone, giving rise to fibroid-like tissue in vivo. These new findings will likely enhance our understanding of the crucial role epigenetics plays in the pathogenesis of uterine leiomyomas as well as point the way to novel therapeutic options.
Keywords: DNA methylation, oxidative DNA demethylation, TET proteins, histone modification, miRNA, leiomyoma, stem cells, epigenetics
Introduction
Uterine leiomyomas, or fibroids, are the most common benign tumors of the reproductive tract and serve as the single most common indication for hysterectomies.1,2 Uterine leiomyomas typically cause severe menstrual bleeding, pelvic pain, preterm labor, recurrent abortion, and infertility. Hysterectomy is currently the main treatment used in women who no longer desire childbearing. This surgery is associated with morbidity and mortality as along with a huge economic impact on the health care delivery system. In the United States, this translates into a cost in the range of US$5.9 to US$34.4 billion/year for uterine leiomyoma management annually.3 Despite its high prevalence, knowledge about the exact pathogenesis of these tumors is still largely unknown.4,5
Epigenetics refers to changes in phenotype mediated by altered gene expression—these changes do not occur as a result of the alteration in DNA sequencing. There are 3 major mechanisms of epigenetic regulation: (a) DNA methylation mediated by DNA methyltransferases as well as active and passive DNA demethylation, (b) modification of histone proteins, and (c) microRNAs. The DNA methylation, histone modification, and miRNA as the mechanisms of epigenetic regulation are involved in a complex network to allow aberrant gene expression for cellular transformation and development of many diseases.6,7 Thus, the understanding of these mechanisms may provide great opportunities for the optimization of diagnostic and prognostic systems as well as generation of novel therapeutic approaches.
DNA Methylation and Demethylation
Methylation of cytosine residues in CpG dinucleotides within the context of a CpG island is one of the common epigenetic regulation mechanisms in eukaryotes. Hypermethylation of CpG island in the promoter region generally results in repression of gene expression, while hypomethylation leads to active transcription.8 Aberrant DNA methylation occurs in many diseases including cancers,9–14 diabetes mellitus,15,16 vascular diseases,17 immune system-related disorders,18 and skin diseases.19 The methylation of cytosine is catalyzed by specific DNA methyltransferases that transfer a methyl group from the donor S-adenosyl methionine to the 5’-position of the pyrimidinic ring. Genomic methylations in mammals appear to be established by a complex interplay of at least 3 DNA methyltransferases (DNMT1, DNMT3A, and DNMT3B).20,21 DNMT1 is considered to maintain DNA methylation patterns during DNA replication. In contrast, DNMT3A and DNMT3B act primarily as de novo methyltransferases in establishing methylation patterns.21–26 Furthermore, a number of alternatively spliced DNA methyltransferases or isoforms have been identified in a variety of cancer types. These isoforms either lack DNA binding or catalytic domains that alter gene expression and methylation patterns, which account for the complex epigenome network in cancers.27–32
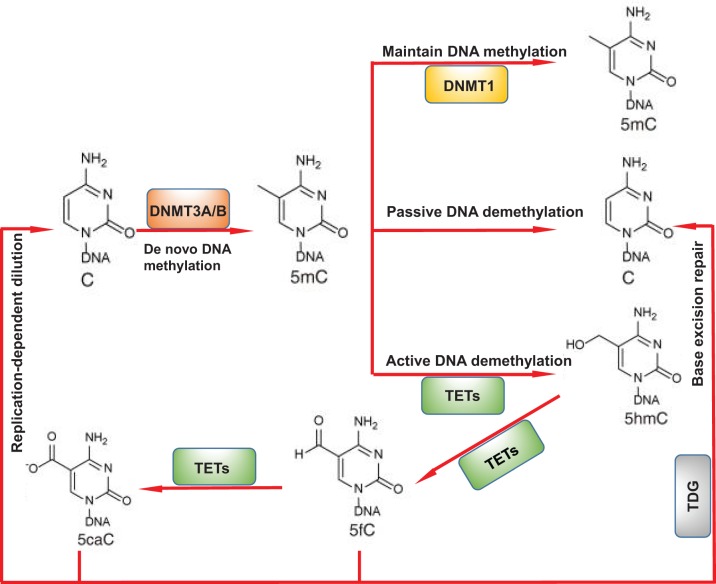
DNA demethylation can occur passively during successive rounds of replication in the absence of functional DNA methylation maintenance machinery. However, this passive model does not adequately explain the loss of DNA methylation in nonreplicating cells, which has been reliably established.33 In contrast, active DNA demethylation refers to an enzymatic process that removes or modifies 5-methylcytosine (5-mC) with regeneration of unmodified cytosine.33–35 Ten-eleven-translocation (TET) enzymes convert 5-mC to 5-hydroxymethylcytosine (5-hmC), hence, TET-mediated DNA demethylation processes are considered as active DNA demethylation (Figure 1).
Figure 1.
Schematic representation of DNA demethylation pathways. TET proteins can oxidize 5mC to generate 5hmC. 5hmC can also be further oxidized by TET proteins to produce 5fC and 5caC. The above 3 modified C, served as intermediates for DNA demethylation, can be diluted during DNA replication. On the other hand, 5fC and 5caC can be excised from DNA by TDG generating an abasic site as part of the base excision repair process that regenerates unmodified C. DNMT indicates DNA methyltransferase; TET, ten-eleven translocation protein; TDG, thymine DNA glycosylase; C, cytosine; 5mC, 5-methylcytosine; 5hmC, 5-hydroxymethylcytosine; 5fC, formylcytosine; 5caC, 5-carboxylcytosine.
Modifications of Histone Proteins
Yet another key component in the epigenetic regulation of gene expression is posttranslational modifications of N-terminal tails or the globular domains of core histones. Histone modifications are involved in many biological processes36–40 and alter DNA accessibility, thereby modulating the expression of genetic information. Epigenetic modifications of histone tails include acetylation, methylation, phosphorylation, ubiquination, and SUMOylation. In contrast to DNA methylation, histone methylation can result in either activation or repression of gene transcription, while histone acetylation is correlated with gene activation.41,42 Varying combinations of histone modifications are believed to comprise a histone code that directs biological processes by the recruitment of specific chromatin-associated proteins leading to distinct gene expression patterns.43
Posttranslational modifications of histones is one of the major mechanisms for the assembly and compaction of chromatin.44 Many enzymes, which are involved in their addition and removal, have been identified. These include histone acetyltransferases and deacetylases,45 lysine methyltransferases and demethylases,46,47 arginine methyltransferases and demethylases,48 serine/threonine/tyrosine kinases and phosphatases,49 and lysine ubiquitinases and deubiquitinases.50,51 These enzymes exist in multi-subunit complexes and act on distinct amino acid residues of specific histones and within chromatin at certain genomic regions that allow a vast range of flexibility in regulating chromatin dynamics and signaling transmission.52
MicroRNAs
MicroRNAs (miRNAs) are evolutionarily conserved, small noncoding RNA molecules (21–2 3nt) that play an important role in transcriptional and posttranscriptional regulation of gene expression.53 The miRNAs function by binding to complementary sequences within messenger RNA (mRNA) molecules, usually, but not exclusively, resulting in gene silencing via translational repression or target degradation.54,55 At the same time, a single mRNA can be modulated by multiple different miRNAs, resulting in a sophisticated gene regulatory network. Since the first miRNAs were characterized in the early 1990s,56 miRNAs have been found to be involved in multiple biological events including numerous diseases.57–66
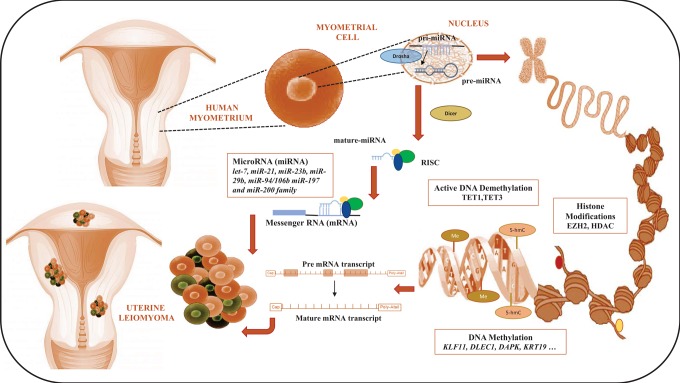
Moreover, increasing evidence in human and experimental animal models has further substantiated the role epigenetic alterations play in reprogramming key sensing and signaling pathways leading to leiomyoma formation (Figure 2). The focus of this review is to provide a comprehensive summary of our current scientific knowledge of epigenetic factors related to human myometrium and their putative implications in leiomyoma formation.
Figure 2.
Schematic representation of epigenetic mechanisms involved in human leiomyoma formation. DNA methylation, histone modifications, and micro RNA (miRNA) play a crucial role in modulating the gene expression pattern in the pathogenesis of leiomyoma. TET1 indicates ten-eleven translocation protein 1; TET3, ten-eleven translocation protein 3; EZH2, enhancer of zeste 2; HDAC, histone deacetylase; Dicer, an enzyme that cleaves double-stranded RNA (dsRNA) and pre-microRNA (pre-miRNA) into short double-stranded RNA fragments called small-interfering RNA and microRNA, respectively; RISC, RNA-induced silencing complex; KLF11, Kruppel-like factor 11; DLEC1, deleted in lung and esophageal cancer 1; DAPK1, death-associated protein kinase 1; KRT19, keratin 19.
DNA Methylation in Uterine Leiomyoma
The mechanism of deregulation of ER response genes in leiomyoma was recently described by Maekawa et al using genome-wide DNA methylation and mRNA profiling in paired specimens of leiomyoma and adjacent normal myometrium from Japanese women.67 Although a similar methylation pattern between the myometrium with leiomyoma and the normal myometrium was observed, the methylation pattern in leiomyoma is different from the one in myometrium with leiomyoma or the normal myometrium. Importantly, among 120 genes whose DNA methylation and mRNA expression patterns differed between leiomyoma and the adjacent myometrium, 22 genes including Collagen Alpha-1(IV) Chain (COL4A1), Collagen Alpha-3(VI) Chain (COL6A3), glutathione S-transferase mu 5 (GSTM5), NUAK Family SNF1-Like Kinase 1 (NUAK1), the death-associated protein kinase I (DAPK1), have the consensus sequence of estrogen receptor (ER) response elements.67 The latter one, a proapoptotic Ca(2+) calmodulin-regulated serine/threonine kinase, participates in a wide array of apoptotic systems initiated by interferon-γ, TNF-α, activated Fas, and detachment from extracellular matrix.68 It was found that the mRNA and protein expression of DAPK1 is frequently lost in various human cancer cells due to DNA methylation in the DAPK1 promoter region.69–73 Interestingly, DAPK1 was also identified as a target gene for DNA hypermethylation in leiomyoma.74 The DNA methylation analysis demonstrated that fully methylated methylation-specific PCR products in sera of patients with leiomyoma. In contrast, sera from otherwise healthy women showed only partially methylated DAPK sequences.
It is well known that hypermethylation of tumor suppressor genes and hypomethylation of oncogenes contributes to the development of tumorigenesis.75,76 Another genome-wide DNA methylation study using the high-throughput Illumina Infinium Methylation Readchip (Illumina Inc., San Diego, California) and parallel mRNA expression profiles was performed by Navarro et al.77 This study was conducted among African American women in which they examined uterine leiomyoma and matched adjacent myometrial tissue. The authors concluded that 55 genes showed differential promoter methylation with concomitant differences in mRNA expression in uterine leiomyoma, when compared to normal myometrium. DLEC1, Keratin 19 (KRT19), and KLF11 were among the 3 top tumor suppressor genes found with the latter tumor suppressor gene, KLF11 considered a target of progesterone or antiprogestins in uterine leiomyoma tissue. The methylation status of these genes was further investigated by bisulfite sequencing. The methylation levels of CpG islands located at the promoter region of KLF11, DLEC1, and KRT19 were higher in leiomyoma when compared to adjacent myometrial tissue. These studies suggest the critical role of DNA hypermethylation in the pathogenesis of leiomyoma. Both of the previously mentioned independent studies were performed using genome-wide DNA methylation analysis and mRNA profiling techniques, however, the differential methylated genes and deregulated expressed genes identified by the 2 groups differed substantially. Possible explanations in this discrepancy may lie in (a) the difference in methylation and mRNA platforms used and (b) racial differences and attributes relative to the different gene expression and DNA methylation pattern in leiomyoma.
Additionally, aberrant DNA methylation status of X chromosome-related genes has been observed in leiomyoma. Sato et al78 demonstrated a higher incidence of aberrant DNA hypomethylation on the X chromosome when compared to the whole genome in uterine leiomyoma. The aberrant hypomethylation gene includes Testis-Specific Protein Y Encoded-Like 2 (TSPYL2), which was hypomethylated in 68% of multiple leiomyoma samples. However, the expression of TSPYL2 was not upregulated in leiomyoma samples.78
Leiomyomas are estrogen-dependent tumors. A growing body of evidence within the literature has investigated a link between the ER signaling and epigenetic regulation. Estrogen receptor α (ERα) is highly expressed in uterine leiomyomas when compared to normal myometrium, suggesting its role in the pathogenesis of uterine leiomyomas.79 Recent studies demonstrate that ERα expression is regulated by DNA methylation in uterine leiomyoma formation. Asada et al80 reported a potential link between ERα gene expression and hypomethylation. They compared the DNA methylation status around the ERα promoter region (−1188 to +299) in myometrium and leiomyoma using the bisulfite sequencing approach and demonstrated that 49 CpG sites in the proximal promoter region of ERα gene exhibit no cytosine methylation in either normal myometrium or leiomyomas. However, at 7 CpG sites in the distal promoter region of ERα gene, variation appeared in DNA methylation status between normal myometrium and leiomyoma. The hypomethylation status of ERα distal promoter region is correlated with high ERα mRNA expression—such a correlation does not generally seem to be conserved in other uterine diseases. For example, Hori et al81 reported that ERα transcription from the distal promoter, rather than from the proximal promoter, predominates in the proliferative phase of the normal menstrual cycle because hypermethylation of the proximal promoter region was not observed during that phase. However, methylation of the promoter regions of ERα gene did not correlate with lack of ERα protein in human patient samples with endometrial disease, including stromal sarcoma, hyperplasia, and adenocarcinoma. In their study, they examined the cytosine methylation status in the proximal promoter region in exon 1 and the distal promoter region in exon 1’ of the ERα gene in various human endometrial diseases by semiquantitative competitive polymerase chain reaction assay using restriction enzymes (HpaII, NotI, and SacII). One possible explanation for this discrepancy may lie in the location of CpG sites they examined. Additionally, the use of different methods in determining the methylation status of the ERα promoter region in uterine disease may further explain this incongruence. Yet another possible explanation may lie in the translational failure from RNA to protein within the samples examined. Finally, the methylation pattern in the promoter region of ERα between myometrium and endometrial disease may differ in response to environmental factors. The validated methylation-regulated targets in leiomyoma are summarized in Table 1.
Table 1.
Validated Epigenetic Targets in Uterine Leiomyoma.
| Validated Target Genes | Epigenetic Mechanism | Species | References |
|---|---|---|---|
| ERα | DNA methylation | Human | Hori M et al81 |
| ERα | DNA hypomethylation | Human | Asada et al80 |
| DAPK1 | DNA methylation | Human | Hafner et al74 |
| KLF11 | DNA methylation | Human | Navarro et al77 |
| DLEC1 | DNA methylation | Human | Navarro et al77 |
| KRT19 | DNA methylation | Human | Navarro et al77 |
| IRS1 | DNA methylation | Human | Maekawa et al67 |
| COL4A1 | DNA methylation | Human | Maekawa et al67 |
| GSTM5 | DNA methylation | Human | Maekawa et al67 |
| TSPYL2 | DNA hypomethylation | Human | Sato et al78 |
| OCRL | DNA hypomethylation | Human | Sato et al78 |
| HMGA2 | let-7 miRNA | Human | Wang et al28 |
| TUBB,CYPIB1, CTBP2 | miR-200a | Human | Zavadil et al82 |
| F3, IL8 | miR-94/106b | Human | Chuang et al83. |
| ZEB1/ZEB2,TIMP2, FBLN5,VEGFA | miR-200c | Human | Chuang et al84 |
| IKBKB | miR-200c | Human | Chuang et al85 |
Abbreviations: DAPK1, death-associated protein kinase 1; DLEC1, deleted in lung and esophageal cancer 1; ERα, estrogen receptor α; HMGA2, high-mobility group A2 protein; KLF11, Kruppel-like factor 11; KRT19, keratin 19; IRS1, insulin receptor substrate 1; COL4A1, collagen Alpha-1(IV) Chain; GSTM5, glutathione S-Transferase M5; TSPYL2, TSPY-Like 2; OCRL, oculocerebrorenal syndrome of Lowe; HMGA2, high mobility group AT-hook 2; TUBB, tubulin, beta class I; CYP1B1, cytochrome P450 1B1; CTBP2, c-terminal binding protein 2; F3, coagulation factor III ; IL8, interleukin 8 ; ZEB1, zinc finger E-box binding homeobox 1; ZEB2, zinc finger E-box binding homeobox 2 ; TIMP2, TIMP metallopeptidase inhibitor 2; FBLN5, fibulin 5 ; VEGFA, vascular endothelial growth factor A; IKBKB, inhibitor of kappa light polypeptide gene enhancer in B-cells, kinase beta.
Active DNA Demethylation in Uterine Leiomyoma
Reduced levels of 5-hmC have been found in various solid tumors, indicating that TET enzymes may contribute to cellular transformation via regulation of DNA demethylation.86–88 In addition, TET proteins oxidize 5-mC not only to 5-hmC but also to 5-formylcytosine (5-fC) and 5-carboxylcytosine (5-caC) in a stepwise manner.89,90 As a new epigenetic modification, 5-hmC may be a useful biomarker for the diagnosis of cancers. These studies challenge the traditional view of DNA methylation as permanent and suggest that DNA methylation in the promoter region may be transient under certain conditions. First evidence of the dysregulation of 5-hmC in uterine leiomyoma was provided by Dr Bulun’s group.91 They demonstrated that an epigenetic imbalance in the 5-hmC content of leiomyoma tissue, caused by upregulation of the TET protein 1 (TET1) and TET protein 3 (TET3) enzymes, contributes to promoting proliferation of human uterine leiomyoma. In contrast to general findings which suggest that 5-hmC levels from malignant cancers including human skin, breast, liver, lung, prostate, pancreatic, and melanoma, are lower, studies from Bulun group showed that 5-hmC levels from leiomyoma were significantly higher when compared to normal myometrial tissue. The increase in 5-hmC levels was associated with the upregulation of TET1 or TET3 mRNA and protein expression in leiomyoma tissue. TET1 or TET3 knockdown significantly reduced 5-hmC levels in leiomyoma cells and decreased cell proliferation. Similarly, treatment with 2-HG, a competitive TET enzyme inhibitor, significantly decreased both 5-hmC content and cell proliferation of leiomyoma cells. These studies suggest that an unusual DNA methylation/demethylation dynamic may be attributable to the alteration of the epigenome and phenotype in leiomyoma. Interestingly, TET1 upregulation leading to a global increase in 5-hmC levels was also found in mixed lineage leukemia (MLL)-rearranged leukemia,92 indicating that TET proteins may play an oncogenic role in certain tumors.
Histone Modifications in Uterine Leiomyoma
Although epigenetic analysis for the pathogenesis of leiomyoma hasbeen focused on DNA methylation, a couple of studies have demonstrated that histone modification is directly involved in leiomyoma development.93,94
The plasticity of gene expression patterns in the developing fetus allows for adaptations of growing tissues/organs to various environmental stimuli in optimizing fetal survival. However, when the in utero environment is suboptimal, permanent developmental reprogramming of the epigenome could take place. Environmental exposure during development can alter susceptibility later in life to adult diseases, including uterine leiomyoma.95 Currently, the best experimental animal model for studying uterine leiomyoma is the Eker rat model. Eker rats carry a germ line mutation in the tuberous sclerosis complex-2 tumor suppressor gene.96 Greathouse et al95 demonstrated that when exposed to diethylstilbestrol (DES) as newborns, adult Eker rats manifested permanent changes in gene expression of the myometrium throughout their adult lifetime. They demonstrated that 171 genes were differentially expressed in leiomyoma, relative to normal myometrium using microarray-based analysis. Among them, several genes (S100 Calcium Binding Protein G [Calbindin D9K]; Deiodinase, Iodothyronine, Type II [Dio2]; growth differentiation factor 10 [Gdf10]; carbonic anhydrase 8 [CA8]; glutamate receptor, ionotropic, AMPA 2 [Gria2]; and matrix metallopeptidase 3 [mmp3]) with putative estrogen responsive elements and confirmed estrogen responsive in the myometrium of 5-month-old rats were reprogrammed by neonatal DES exposure. In animals carrying a germ line defect in Tsc-2, early life exposure to DES during development of the uterus increased tumor-suppressor gene penetrance from 65% to >90% and tumor multiplicity and size. Tumors that developed in exposed animals displayed an enhanced proliferative response to steroid hormones relative to tumors that developed in unexposed animals, suggesting that gene–environment interactions through epigenetic regulation are important determinants of tumor risk including leiomyoma.96,97
Histone methyltransferase enhance of zeste homolog 2 (EZH2) is a member of the polycomb repressive complex 2 (PRC2), which catalyzes trimethylation of lysine 27 of histone H3. Abnormal EZH2 expression has been associated with various cancers.98,99 Dr Walker’s group reported on xenoestrogen-induced regulation of EZH2 and histone methylation via ER signaling to phosphatidylinositol 3-kinase (PI3K)/serine-threonine protein kinase (AKT).93 They found that in response to both 17β-estradiol (E2) and xenoestrogen diethylstilbestrol, ER signaling via PI3K/protein kinase B phosphorylated EZH2 at S21 and reduced levels of trimethylation of lysine 27 on histone H3 in hormone-responsive cells.93 A further study indicated that another environmental estrogen, genistein, also induced PI3K/AKT nongenomic ER signaling to the histone EZH2.94 These studies provide a direct link between xenoestrogen-induced nuclear hormone receptor signaling and modulating of epigenetic machinery during developmental reprogramming in response to environmental estrogen in leiomyoma.
More recently, long noncoding RNAs (lncRNAs) have emerged as important players in the regulation of gene expression in a variety of biological processes.100–108 The LncRNAs may provide potential guides to complex with chromatin-modifying proteins and recruit their catalytic activity to specific sites in the genome, thereby modifying chromatin states and modulating gene expression.109,110 For instance, lncRNA has functional links with PRC2,110 and the direct interactions between PRC2 and RepA/Xist RNAs target PRC2 in cis to the mammalian X chromosome.111 The involvement of lnc RNAs would provide targeting specificity and introduce new regulatory capabilities.112 So far the role of lncRNAs in pathogenesis of uterine fibroids has not been identified, therefore, it is encouraged to determine how the lncRNAs alter the chromatin state, especically how lncRNAs interact with polycom group proteins to influence the gene expression pattern through epigenetic machinery.
Histone deacetylases (HDACs), a class of enzymes that remove acetyl groups from an e-N-acetyl-lysine amino acid, also participate in the regulation of gene expression. The HDAC has been shown to be involved in the regulation of tumor suppressor gene, KLF11’s function relevant to uterine disease.113 KLF11 belongs to the family of Sp1/Krüppel-like zinc finger transcription factors that play important roles in a variety of cell types and tissues.114,115 KLF11 was found to be diminished in uterine leiomyomas.116 Zheng et al113 recently suggested that KLF11 repressed most endometrial cytochrome (CYP) enzymes in Ishikawa cells. They further demonstrated that KLF11 bound to the estrogen-metabolizing enzyme CYP3A4 promoter GC elements and thereby repressed its promoter and enzymatic function. This repression was epigenetically mediated as KLF11 recruited the coreceptor SIN3A/HDAC resulting in selective deacetylation of the CYP3A4 promoter. Moreover, this repression was pharmacologically reversible with an HDAC inhibitor. KLF11 is highly expressed in reproductive tissues, suggesting that cofactor (HDAC) binding likely plays a critical role in the regulation of transcription factors related to the development of uterine diseases including leiomyoma.
Besides DNA methylation-mediated regulation of ERα expression, Wei et al reported that HDAC6 regulated ERα in uterine leiomyoma.117 HDAC6 belongs to class I HDAC family. It is a unique member of the HDAC family that primarily localizes to the cytoplasm.118 Wei et al found that HDAC6 expression is mainly detected in the cytoplasm of smooth muscle cells associated with ERα expression. In uterine leiomyomas, a strong staining for the HDAC6 in the cytoplasm was frequently observed, where weak staining of HDAC6 was seen in matched normal myometrium. Silencing of HDAC6 expression using the small-interfering (siRNA) approach led to a significant reduction in ERα protein levels but not ERα mRNA levels. Furthermore, treatment with lysosome inhibitor CQ, but not with a proteasome inhibitor (MG132), blocked the depletion of ERα protein levels by HDAC6 siRNA, suggesting that HDAC6 siRNA decreased the ERα protein levels by promoting the degradation of ERα protein in the lysosome. Although the role of histone modification on ERα signaling regulation in leiomyoma has not been characterized, a previous study demonstrated that H3K27 methylation imposed ligand-dependent of the ERα-dependent apoptotic response via Bcl-2 in breast cancer cells.119
Interplay Between Epigenetics and Genomics
An increasing body of evidence shows that a link between genetics and epigenetics occurs in many biological events including tumorigenesis. For instance, silencing of DNA Mismatch Repair Protein (MLH1) gene expression due to its promoter methylation prevents the normal activation of the DNA repair gene, leading to genomic instability in colorectal cancer formation.120 Another DNA repair gene, O6-methylguanine-DNA methyltransferase (MGMT1), is hypermethylated in cancers and inactivation of MGMT1 is associated with TP53 and K-Ras mutations.121–123 Although little is known regarding the relationship between genetic and epigenetics in uterine leiomyoma, Moore et al124 previously reported that the chromosomal aberration, t (10:17), in uterine leiomyoma disrupted histone acetyltransferase, monocytic leukemia zinc finger protein-related factor (MORF).125 Since MORF is a member of the MYST family (the name of this family is derived from its 4 founding members: MOZ, YBF2/SAS3 and, SAS2, and TIP60) of histone acetyltransferases,126 it is conceivable that dysfunction of MORF by genetic disruption alters chromatin regulation and confers a distinct gene expression pattern in leiomyoma pathogenesis.
Dysregulation of miRNA in Uterine Leiomyoma
Micro-RNAs are deregulated in many biological pathways that may lead to the pathogenesis of leiomyoma. A number of studies have been conducted to perform profiling and function analyses of miRNAs in human uterine leiomyoma using microarray and deep sequencing.82,127–129 These studies demonstrate that many miRNAs regulating cellular processes including cell proliferation, apoptosis, cell adhesion, WNT signaling, mitogen-activated protein kinase (MAPK) signaling, nuclear factor κB (NF-κB) activation, and insulin signaling are deregulated in leiomyoma when compared to normal tissues. Importantly, the predicted targets of these deregulated miRNAs including let-7, miR-21, miR-23b, miR-29b, and miR-197 in leiomyoma play an important role in the pathogenesis of leiomyoma. For example, let-7, whose expression is upregulated in leiomyoma, targets high-mobility group A2 protein (HMGA2), which has been implicated in the pathogenesis of mesenchymal tumors such as leiomyoma, lipoma, and hamartoma.130 Furthermore, subsets of miRNAs are strongly associated with race and tumor size in human uterine leiomyomas.128 In addition to HMGA2, Fitzgerald et al131 reported that increased miR-21 levels are predicted to decrease programmed cell death (PDCD-4) expression. In many malignant tumors, PDCD-4 is downregulated and acts as a tumor suppressor, however, PDCD-4 exhibits a unique expression profile, with almost complete absence of PDCD-4 in normal myometrium and high overexpression of PDCD-4 proteins in leiomyoma. Knockdown of miRNA-21 increases PDCD-4 levels in immortalized leiomyoma and myometrium cells indicating that miRNA-21 can regulate PDCD-4 expression. Furthermore, several other miRNA direct targets have been characterized in leiomyoma.82,83,84 More recently, Chuang et al85 reported that miR-200c regulates IL8 expression by direct targeting IKBKB and alteration of NF-κB activity in leiomyoma.
A functional and essential role of miR-29b in the uterine leiomyoma formation was recently determined by Qiang et al.132 In uterine leiomyoma xenografts, restoring miR-29b inhibited the accumulation of extracellular matrix (ECM) and the development of solid tumors, indicating that the downregulation of miR-29b is essential for uterine leiomyoma tumorigenesis. In addition, 17β-estradiol and progesterone downregulated miR-29b and upregulated mRNAs for multiple collagens in uterine leiomyoma xenografts. This study suggests that excessive ECM production in uterine leiomyoma is regulated by steroid hormones via downregulation of miR-29b.132 The validated miRNA-regulated targets in leiomyoma are summarized in Table 1.
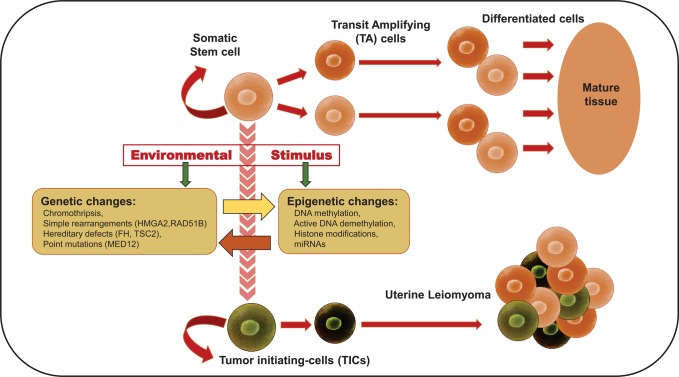
Epigenetic Regulation of Stem Cells in Leiomyoma, Future Directions
Somatic stem cells (SSCs) are undifferentiated cells, presented throughout the body, that multiply by cell division to replenish dying cells and regenerate damaged tissues and thereafter differentiate into tissue-specific types. The SSCs create the dynamic system required for cellular/tissue homeostasis. Accordingly, tumor stem cells have the capacity for self-renewal and tumor maintenance and growth.
Many chromatin regulators are required for development, stem cell maintenance, and differentiation. Epigenetic mechanisms allow genetically identical cells to stably adopt different phenotypes by controlling the transcriptional availability of different regions of genome packing or opening different regions of the chromatin. The combination of transcriptional factors and chromatin remodeling factors might be essential for different aspects of stem cell phenotype.133 Emerging evidence indicates that PRC1 and PRC2 and HDAC1- and HDAC2-containing complexes (NuRD, Sin3, and CoREST) play a crucial role in stem cell function and cancer pathogenesis.134–136 Moreover, an increasing body of evidence suggests that specific CpG methylation regions are altered during differentiation of multipotent stem cells.137–140 Recently, a new epigenetic landscape has been described by genome-wide mapping of 5-mC and 5-hmC and active/repressive histone code marks associated with DNMT3A expression in hematopoietic stem cells.7
Uterine leiomyomas are monoclonal tumors that arise from the uterine smooth muscle tissue.2,141 A limited number of genetic defects transmitted by germ cells have been associated with familial uterine leiomyoma syndromes. So far, there are no published data showing the involvement of epigenetic changes in these patients, for example, hereditary leiomyomatosis and renal cell carcinoma which are linked with germ line mutation of fumarate hydratase.142–144 Although the cellular origin of uterine leiomyoma remains largely unknown, several lines of evidence suggests that each leiomyoma originates from the transformation of a single somatic stem cells.145–153 Moreover, stem cells derived from leiomyoma carry Med12 mutations, which suggests that at least 1 genetic hit is initially required to transform myometrial stem cells.2
The existence of putative SSCs was first identified in 2007 in mouse myometrium and nonpregnant human myometrium using 5-bromo-2’-deoxyuridine (which permits the identification of label-retaining cells), and side population technique, respectively.145,154 A subset of myometrial cells isolated from human myometrium (side population) exhibit characteristics similar to stem cells. In contrast to the main population of myometrial cells, the side population of myometrial cells are capable of generating functional human myometrial tissues efficiently when transplanted into the uteri of severely immunodeficient mice.145 Subsequently, the leiomyoma-derived side population, which have stem cell characteristics, were characterized and demonstrated to be responsible for cell proliferation and tumor growth146,151 (Figure 3). Although leiomyomas have a lower percentage of side population cells when compared to normal myometrium,150 the wingless-type MMTV integration site family (WNT)/β-catenin pathway in leiomyoma stem cells is activated in a paracrine manner leading to the promotion of tumor growth. WNT/β-catenin signaling is a key regulator of multiple aspects of tumorigenesis,155 embryonic development, and tissue homeostasis. In a cell coculture system, where both leiomyoma stem cells and mature myomentrial cells exist, estrogen–progesterone selectively induced nuclear translocation of β-catenin, leading to the proliferation of leiomyoma stem cells.147 Accordingly, aberrant regulation of the canonical signaling (WNT/β-catenin/glycogen synthase kinase 3 (GSK-3)-3 axis) has been reported to be involved in the formation and maintenance of cancer stem cells.156
Figure 3.
Hierarchy of differentiation of stem cells and specific genetic/epigenetic abnormalities relevant to human leiomyoma formation. Environmental factor-induced genetic/epigenetic abnormalities alter the gene expression pattern and function of undifferentiated stem/transit amplifying (TA) cells leading to the formation of a population of proliferating cells, called tumor-initiating cells (TICs), which differ from the rest and could develop into a uterine leiomyoma. HMGA2 indicates high mobility group AT-Hook 2; RAD51B, RAD51 Paralog B; FH, fumarate hydratase; TSC2, tuberous sclerosis 2; MED12, mediator complex subunit 12.
Improved approaches in the characterization and isolation of myometrium and leiomyoma derived SSCs will shed new light on how deregulated epigenetic factors promote the pathogenesis of leiomyoma and provide a potential therapeutic approach for targeting leiomyoma stem cells.
Concluding Remarks
Aberrant epigenetic changes including DNA methylation, histone modifications, and miRNAs are common molecular lesions in tumor cells. Although great progress has been made in understanding the epigenetic mechanisms related to tumor development, little is known about the mechanisms and function of epigenetics in uterine leiomyoma formation. Recently, several approaches including mapping of the genome-wide distribution of 5mC and oxidized 5mc derivatives have led to a better understanding as to the epigenome in tumor biology and stem cell somatic cell reprogramming.157–159 The dynamic of active DNA demethylation and DNA methylation in leiomyoma provides a network for regulating DNA methylation status across the genome.
In contrast to intensive genome-wide studies on DNA methylation and miRNAs, little is known about the regulation of histone modifications globally as well as the interplay between DNA methylation and histone modifications in the development and pathogenesis of leiomyoma. These studies will lead to a better understanding as to the mechanisms and pathology of leiomyoma formation. Comprehensive studies on histone modifications are needed to fully explore several available and underdeveloped histone-based therapeutic agents for the treatment of uterine leiomyoma.
Similarly, recent studies demonstrating the existence of side populations with stem cell characteristics in myometrium and leiomyoma will be helpful in determining how leiomyoma stem cells are derived and what role epigenetic events play during these processes. Understanding the abnormal signaling and epigenetic regulation within leiomyoma stem cells will provide new opportunities to develop an efficient therapeutic approach, capable of effectively reducing the severity and size of uterine leiomyoma while avoiding side effects.
Acknowledgments
We would like to thank Walidah Walker, MPH, for editing this manuscript.
Footnotes
Authors’ Note: The authors involved in the development of this manuscript certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on him/herself or on any associate organization and, if applicable, the authors certify that all financial and material support for this research (e.g., NIH or NHS grants) and work are clearly identified within the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by the National Institutes of Health grant HD04622811 (to AA).
References
- 1. Al-Hendy A, Salama S. Gene therapy and uterine leiomyoma: a review. Hum Reprod Update. 2006;12(4):385–400. [DOI] [PubMed] [Google Scholar]
- 2. Bulun SE. Uterine fibroids. N Engl J Med. 2013;369(14):1344–1355. [DOI] [PubMed] [Google Scholar]
- 3. Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012;206(3):211. e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Sabry M, Al-Hendy A. Medical treatment of uterine leiomyoma. Reprod Sci. 2012;19(4):339–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Segars JH, Parrott EC, Nagel JD, et al. Proceedings from the Third National Institutes of Health International Congress on Advances in Uterine Leiomyoma Research: comprehensive review, conference summary and future recommendations. Hum Reprod Update. 2014;20(3):309–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kim GH, Ryan JJ, Marsboom G, Archer SL. Epigenetic mechanisms of pulmonary hypertension. Pulm Circ. 2011;1(3):347–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jeong M, Sun D, Luo M, et al. Large conserved domains of low DNA methylation maintained by Dnmt3a. Nat Genet. 2014;46(1):17–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones PA. DNA methylation and cancer. Oncogene. 2002;21(35):5358–5360. [DOI] [PubMed] [Google Scholar]
- 9. Nagasaka T, Goel A, Notohara K, et al. Methylation pattern of the O6-methylguanine-DNA methyltransferase gene in colon during progressive colorectal tumorigenesis. Int J Cancer. 2008;122(11):2429–2436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kobayashi Y, Absher DM, Gulzar ZG, et al. DNA methylation profiling reveals novel biomarkers and important roles for DNA methyltransferases in prostate cancer. Genome Res. 2011;21(7):1017–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yang Q, Liu S, Tian Y, et al. Methylation-associated silencing of the heat shock protein 47 gene in human neuroblastoma. Cancer Res. 2004;64(13):4531–4538. [DOI] [PubMed] [Google Scholar]
- 12. Yang Q, Kiernan CM, Tian Y, et al. Methylation of CASP8, DCR2, and HIN-1 in neuroblastoma is associated with poor outcome. Clin Cancer Res. 2007;13(11):3191–3197. [DOI] [PubMed] [Google Scholar]
- 13. Agrawal S, Unterberg M, Koschmieder S, et al. DNA methylation of tumor suppressor genes in clinical remission predicts the relapse risk in acute myeloid leukemia. Cancer Res. 2007;67(3):1370–1377. [DOI] [PubMed] [Google Scholar]
- 14. Berg T, Steigen SE. DNA methylation in breast and colorectal cancer. Mod Pathol. 2008;21(8):1063; author reply -4. [DOI] [PubMed] [Google Scholar]
- 15. de Mello VD, Pulkkinen L, Lalli M, Kolehmainen M, Pihlajamaki J, Uusitupa M. DNA methylation in obesity and type 2 diabetes. Ann Med. 2014;46(3):103–113. [DOI] [PubMed] [Google Scholar]
- 16. Toperoff G, Aran D, Kark JD, et al. Genome-wide survey reveals predisposing diabetes type 2-related DNA methylation variations in human peripheral blood. Hum Mol Genet. 2012;21(2):371–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jamaluddin MS, Yang X, Wang H. Hyperhomocysteinemia, DNA methylation and vascular disease. Clin Chem Lab Med. 2007;45(12):1660–1666. [DOI] [PubMed] [Google Scholar]
- 18. Suarez-Alvarez B, Rodriguez RM, Fraga MF, Lopez-Larrea C. DNA methylation: a promising landscape for immune system-related diseases. Trends Genet. 2012;28(10):506–514. [DOI] [PubMed] [Google Scholar]
- 19. Li Y, Sawalha AH, Lu Q. Aberrant DNA methylation in skin diseases. J Dermatol Sci. 2009;54(3):143–149. [DOI] [PubMed] [Google Scholar]
- 20. Jones PA. DNA methylation and cancer. Cancer Res. 1986;46(2):461–466. [PubMed] [Google Scholar]
- 21. Jones PA, Baylin SB. The epigenomics of cancer. Cell. 2007;128(4):683–692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Robertson KD. DNA methylation, methyltransferases, and cancer. Oncogene. 2001;20(24):3139–3155. [DOI] [PubMed] [Google Scholar]
- 23. Baylin SB, Esteller M, Rountree MR, Bachman KE, Schuebel K, Herman JG. Aberrant patterns of DNA methylation, chromatin formation and gene expression in cancer. Hum Mol Genet. 2001;10(7):687–692. [DOI] [PubMed] [Google Scholar]
- 24. Esteller M, Fraga MF, Guo M, et al. DNA methylation patterns in hereditary human cancers mimic sporadic tumorigenesis. Hum Mol Genet. 2001;10(26):3001–3007. [DOI] [PubMed] [Google Scholar]
- 25. Taberlay PC, Jones PA. DNA methylation and cancer. Prog Drug Res. 2011;67:1–23. [DOI] [PubMed] [Google Scholar]
- 26. Sharma S, Kelly TK, Jones PA. Epigenetics in cancer. Carcinogenesis. 2010;31(1):27–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Gopalakrishnan S, Van Emburgh BO, Shan J, et al. A novel DNMT3B splice variant expressed in tumor and pluripotent cells modulates genomic DNA methylation patterns and displays altered DNA binding. Mol Cancer Res. 2009;7(10):1622–1634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wang J, Bhutani M, Pathak AK, et al. Delta DNMT3B variants regulate DNA methylation in a promoter-specific manner. Cancer Res. 2007;67(22):10647–10652. [DOI] [PubMed] [Google Scholar]
- 29. Weisenberger DJ, Velicescu M, Cheng JC, Gonzales FA, Liang G, Jones PA. Role of the DNA methyltransferase variant DNMT3b3 in DNA methylation. Mol Cancer Res. 2004;2(1):62–72. [PubMed] [Google Scholar]
- 30. Saito Y, Kanai Y, Sakamoto M, Saito H, Ishii H, Hirohashi S. Overexpression of a splice variant of DNA methyltransferase 3b, DNMT3b4, associated with DNA hypomethylation on pericentromeric satellite regions during human hepatocarcinogenesis. Proc Natl Acad Sci U S A. 2002;99(15):10060–10065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ostler KR, Davis EM, Payne SL, et al. Cancer cells express aberrant DNMT3B transcripts encoding truncated proteins. Oncogene. 2007;26(38):5553–5563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Ostler KR, Yang Q, Looney TJ, et al. Truncated DNMT3B Isoform DNMT3B7 Suppresses Growth, Induces Differentiation, and Alters DNA Methylation in Human Neuroblastoma. Cancer Res. 2012;72(18):4714–4723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Shen L, Song CX, He C, Zhang Y. Mechanism and function of oxidative reversal of DNA and RNA methylation. Annu Rev Biochem. 2014;83:585–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bhutani N, Burns DM, Blau HM. DNA demethylation dynamics. Cell. 2011;146(6):866–872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carey N, Marques CJ, Reik W. DNA demethylases: a new epigenetic frontier in drug discovery. Drug Discov Today. 2011;16(15-16):683–690. [DOI] [PubMed] [Google Scholar]
- 36. Albert M, Helin K. Histone methyltransferases in cancer. Semin Cell Dev Biol. 2010;21(2):209–220. [DOI] [PubMed] [Google Scholar]
- 37. Cao R, Wang L, Wang H, et al. Role of histone H3 lysine 27 methylation in Polycomb-group silencing. Science. 2002;298(5595):1039–1043. [DOI] [PubMed] [Google Scholar]
- 38. Shi Y. Histone lysine demethylases: emerging roles in development, physiology and disease. Nat Rev Genet. 2007;8(11):829–833. [DOI] [PubMed] [Google Scholar]
- 39. Simon JA, Lange CA. Roles of the EZH2 histone methyltransferase in cancer epigenetics. Mutat Res. 2008;647(1-2):21–29. [DOI] [PubMed] [Google Scholar]
- 40. Ho L, Crabtree GR. Chromatin remodelling during development. Nature. 2010;463(7280):474–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wischnewski F, Pantel K, Schwarzenbach H. Promoter demethylation and histone acetylation mediate gene expression of MAGE-A1, -A2, -A3, and -A12 in human cancer cells. Mol Cancer Res. 2006;4(5):339–349. [DOI] [PubMed] [Google Scholar]
- 42. Verdone L, Caserta M, Di Mauro E. Role of histone acetylation in the control of gene expression. Biochem Cell Biol. 2005;83(3):344–353. [DOI] [PubMed] [Google Scholar]
- 43. Bartova E, Krejci J, Harnicarova A, Galiova G, Kozubek S. Histone modifications and nuclear architecture: a review. J Histochem Cytochem. 2008;56(8):711–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Chen T, Dent SY. Chromatin modifiers and remodellers: regulators of cellular differentiation. Nat Rev Genet. 2014;15(2):93–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mai A, Cheng D, Bedford MT, et al. epigenetic multiple ligands: mixed histone/protein methyltransferase, acetyltransferase, and class III deacetylase (sirtuin) inhibitors. J Med Chem. 2008;51(7):2279–2290. [DOI] [PubMed] [Google Scholar]
- 46. Spannhoff A, Hauser AT, Heinke R, Sippl W, Jung M. The emerging therapeutic potential of histone methyltransferase and demethylase inhibitors. ChemMedChem. 2009;4(10):1568–1582. [DOI] [PubMed] [Google Scholar]
- 47. Yokoyama A, Fujiki R, Ohtake F, Kato S. Regulated histone methyltransferase and demethylase complexes in the control of genes by nuclear receptors. Cold Spring Harb Symp Quant Biol. 2011;76:165–173. [DOI] [PubMed] [Google Scholar]
- 48. Chang B, Chen Y, Zhao Y, Bruick RK. JMJD6 is a histone arginine demethylase. Science. 2007;318(5849):444–447. [DOI] [PubMed] [Google Scholar]
- 49. Besant PG, Attwood PV. Histone H4 histidine phosphorylation: kinases, phosphatases, liver regeneration and cancer. Biochem Soc Trans. 2012;40(1):290–293. [DOI] [PubMed] [Google Scholar]
- 50. Gutierrez L, Oktaba K, Scheuermann JC, Gambetta MC, Ly-Hartig N, Muller J. The role of the histone H2A ubiquitinase Sce in Polycomb repression. Development. 2012;139(1):117–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Hussain S, Foreman O, Perkins SL, et al. The de-ubiquitinase UCH-L1 is an oncogene that drives the development of lymphoma in vivo by deregulating PHLPP1 and Akt signaling. Leukemia. 2010;24:1641–1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Cohen I, Poreba E, Kamieniarz K, Schneider R. Histone modifiers in cancer: friends or foes? Genes Cancer. 2011;2:631–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Chen K, Rajewsky N. The evolution of gene regulation by transcription factors and microRNAs. Nat Rev Genet. 2007;8(2):93–103. [DOI] [PubMed] [Google Scholar]
- 54. Bartel DP. MicroRNAs: target recognition and regulatory functions. Cell. 2009;136(2):215–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Kusenda B, Mraz M, Mayer J, Pospisilova S. MicroRNA biogenesis, functionality and cancer relevance. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2006;150(2):205–215. [DOI] [PubMed] [Google Scholar]
- 56. Lee RC, Feinbaum RL, Ambros V. The C. elegans heterochronic gene lin-4 encodes small RNAs with antisense complementarity to lin-14. Cell. 1993;75:843–854. [DOI] [PubMed] [Google Scholar]
- 57. Lim LP, Lau NC, Garrett-Engele P, et al. Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature. 2005;433(7027):769–773. [DOI] [PubMed] [Google Scholar]
- 58. Chen CZ, Li L, Lodish HF, Bartel DP. MicroRNAs modulate hematopoietic lineage differentiation. Science. 2004;303(5654):83–86. [DOI] [PubMed] [Google Scholar]
- 59. Brennecke J, Hipfner DR, Stark A, Russell RB, Cohen SM. bantam encodes a developmentally regulated microRNA that controls cell proliferation and regulates the proapoptotic gene hid in Drosophila. Cell. 2003;113(1):25–36. [DOI] [PubMed] [Google Scholar]
- 60. Srivastava K, Srivastava A. Comprehensive review of genetic association studies and meta-analyses on miRNA polymorphisms and cancer risk. PloS One. 2012;7(11):e50966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Xu X, Yang X, Xing C, Zhang S, Cao J. miRNA: The nemesis of gastric cancer (Review). Oncol Lett. 2013;6(3):631–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. White K, Kane NM, Milligan G, Baker AH. The role of miRNA in stem cell pluripotency and commitment to the vascular endothelial lineage. Microcirculation. 2012;19(3):196–207. [DOI] [PubMed] [Google Scholar]
- 63. Duan L, Xiong X, Liu Y, Wang J. miRNA-1: functional roles and dysregulation in heart disease. Mol Biosyst. 2014;10(11):2775–2782. [DOI] [PubMed] [Google Scholar]
- 64. Kaucsar T, Racz Z, Hamar P. Post-transcriptional gene-expression regulation by micro RNA (miRNA) network in renal disease. Adv Drug Deliv Rev. 2010;62(14):1390–1401. [DOI] [PubMed] [Google Scholar]
- 65. Chakraborty C, Doss CG, Bandyopadhyay S, Agoramoorthy G. Influence of miRNA in insulin signaling pathway and insulin resistance: micro-molecules with a major role in type-2 diabetes. Wiley Interdiscip Rev RNA. 2014;5(5):697–712. [DOI] [PubMed] [Google Scholar]
- 66. Yang S, Banerjee S, Freitas A, et al. miR-21 regulates chronic hypoxia-induced pulmonary vascular remodeling. Am J Physiol Lung Cell Mol Physiol. 2012;302(6):L521–L529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Maekawa R, Sato S, Yamagata Y, et al. Genome-wide DNA methylation analysis reveals a potential mechanism for the pathogenesis and development of uterine leiomyomas. PloS One. 2013;8(6):e66632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Cohen O, Kimchi A. DAP-kinase: from functional gene cloning to establishment of its role in apoptosis and cancer. Cell Death Differ. 2001;8(1):6–15. [DOI] [PubMed] [Google Scholar]
- 69. Eisenberg-Lerner A, Kimchi A. DAPk silencing by DNA methylation conveys resistance to anti EGFR drugs in lung cancer cells. Cell Cycle. 2012;11(11):2051. [DOI] [PubMed] [Google Scholar]
- 70. Ahmad ST, Arjumand W, Seth A, Saini AK, Sultana S. Methylation of the APAF-1 and DAPK-1 promoter region correlates with progression of renal cell carcinoma in North Indian population. Tumour Biol. 2012;33(2):395–402. [DOI] [PubMed] [Google Scholar]
- 71. Kato K, Iida S, Uetake H, et al. Methylated TMS1 and DAPK genes predict prognosis and response to chemotherapy in gastric cancer. Int J Cancer. 2008;122(3):603–608. [DOI] [PubMed] [Google Scholar]
- 72. Christoph F, Hinz S, Kempkensteffen C, Schostak M, Schrader M, Miller K. mRNA expression profiles of methylated APAF-1 and DAPK-1 tumor suppressor genes uncover clear cell renal cell carcinomas with aggressive phenotype. J Urol. 2007;178(6):2655–2659. [DOI] [PubMed] [Google Scholar]
- 73. Christoph F, Kempkensteffen C, Weikert S, et al. Methylation of tumour suppressor genes APAF-1 and DAPK-1 and in vitro effects of demethylating agents in bladder and kidney cancer. Br J Cancer. 2006;95(12):1701–1707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Hafner N, Diebolder H, Jansen L, Hoppe I, Durst M, Runnebaum IB. Hypermethylated DAPK in serum DNA of women with uterine leiomyoma is a biomarker not restricted to cancer. Gynecol Oncol. 2011;121:224–229. [DOI] [PubMed] [Google Scholar]
- 75. Feinberg AP. Phenotypic plasticity and the epigenetics of human disease. Nature. 2007;447(7143):433–440. [DOI] [PubMed] [Google Scholar]
- 76. Yang QW, Liu S, Tian Y, et al. Methylation-associated silencing of the thrombospondin-1 gene in human neuroblastoma. Cancer Res. 2003;63(19):6299–6310. [PubMed] [Google Scholar]
- 77. Navarro A, Yin P, Monsivais D, et al. Genome-wide DNA methylation indicates silencing of tumor suppressor genes in uterine leiomyoma. PloS One. 2012;7(3):e33284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Sato S, Maekawa R, Yamagata Y, et al. Potential mechanisms of aberrant DNA hypomethylation on the x chromosome in uterine leiomyomas. J Reprod Dev. 2014;60(1):47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Sadan O, van Iddekinge B, van Gelderen CJ, et al. Oestrogen and progesterone receptor concentrations in leiomyoma and normal myometrium. Ann Clin Biochem. 1987;24(pt 3):263–267. [DOI] [PubMed] [Google Scholar]
- 80. Asada H, Yamagata Y, Taketani T, et al. Potential link between estrogen receptor-alpha gene hypomethylation and uterine fibroid formation. Mol Hum Reprod. 2008;14(9):539–545. [DOI] [PubMed] [Google Scholar]
- 81. Hori M, Iwasaki M, Shimazaki J, Inagawa S, Itabashi M. Assessment of hypermethylated DNA in two promoter regions of the estrogen receptor alpha gene in human endometrial diseases. Gynecol Oncol. 2000;76(1):89–96. [DOI] [PubMed] [Google Scholar]
- 82. Zavadil J, Ye H, Liu Z, et al. Profiling and functional analyses of microRNAs and their target gene products in human uterine leiomyomas. PloS One. 2010;5(8):e12362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Chuang TD, Luo X, Panda H, Chegini N. miR-93/106b and their host gene, MCM7, are differentially expressed in leiomyomas and functionally target F3 and IL-8. Mol Endocrinol. 2012;26(6):1028–1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Chuang TD, Panda H, Luo X, Chegini N. miR-200c is aberrantly expressed in leiomyomas in an ethnic-dependent manner and targets ZEBs, VEGFA, TIMP2, and FBLN5. Endocr Relat Cancer. 2012;19(4):541–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Chuang TD, Khorram O. miR-200c regulates IL8 expression by targeting IKBKB: a potential mediator of inflammation in leiomyoma pathogenesis. PloS One. 2014;9(4):e95370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Kohli RM, Zhang Y. TET enzymes, TDG and the dynamics of DNA demethylation. Nature. 2013;502(7472):472–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Bagci H, Fisher AG. DNA demethylation in pluripotency and reprogramming: the role of tet proteins and cell division. Cell Stem Cell. 2013;13(3):265–269. [DOI] [PubMed] [Google Scholar]
- 88. Mariani CJ, Vasanthakumar A, Madzo J, et al. TET1-mediated hydroxymethylation facilitates hypoxic gene induction in neuroblastoma. Cell Rep. 2014;7(5):1343–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Ito S, Shen L, Dai Q, et al. Tet proteins can convert 5-methylcytosine to 5-formylcytosine and 5-carboxylcytosine. Science. 2011;333(6047):1300–1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. He YF, Li BZ, Li Z, et al. Tet-mediated formation of 5-carboxylcytosine and its excision by TDG in mammalian DNA. Science. 2011;333(6047):1303–1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Navarro A, Yin P, Ono M, et al. 5-hydroxymethylcytosine Promotes Proliferation of Human Uterine Leiomyoma: a Biological Link to a New Epigenetic Modification in Benign Tumors. J Clin Endocrinol Metab. 2014;99(11):E2437–E2445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Huang H, Jiang X, Li Z, et al. TET1 plays an essential oncogenic role in MLL-rearranged leukemia. Proc Nat Acad Sci U S A. 2013;110(29):11994–1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Bredfeldt TG, Greathouse KL, Safe SH, Hung MC, Bedford MT, Walker CL. Xenoestrogen-induced regulation of EZH2 and histone methylation via estrogen receptor signaling to PI3K/AKT. Mol Endocrinol. 2010;24(5):993–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Greathouse KL, Bredfeldt T, Everitt JI, et al. Environmental estrogens differentially engage the histone methyltransferase EZH2 to increase risk of uterine tumorigenesis. Mol Cancer Res. 2012;10(4):546–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Greathouse KL, Cook JD, Lin K, et al. Identification of uterine leiomyoma genes developmentally reprogrammed by neonatal exposure to diethylstilbestrol. Reprod Sci. 2008;15(8):765–778. [DOI] [PubMed] [Google Scholar]
- 96. Cook JD, Walker CL. The Eker rat: establishing a genetic paradigm linking renal cell carcinoma and uterine leiomyoma. Curr Mol Med. 2004;4(8):813–824. [DOI] [PubMed] [Google Scholar]
- 97. Cook JD, Davis BJ, Cai SL, Barrett JC, Conti CJ, Walker CL. Interaction between genetic susceptibility and early-life environmental exposure determines tumor-suppressor-gene penetrance. Proc Natl Acad Sci U S A. 2005;102(24):8644–8649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Yoo KH, Hennighausen L. EZH2 methyltransferase and H3K27 methylation in breast cancer. Int J Biol Sci. 2012;8(1):59–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Bachmann IM, Halvorsen OJ, Collett K, et al. EZH2 expression is associated with high proliferation rate and aggressive tumor subgroups in cutaneous melanoma and cancers of the endometrium, prostate, and breast. J Clin Oncol. 2006;24(2):268–273. [DOI] [PubMed] [Google Scholar]
- 100. Bernard D, Prasanth KV, Tripathi V, et al. A long nuclear-retained non-coding RNA regulates synaptogenesis by modulating gene expression. EMBO J. 2010;29(18):3082–3093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Gupta RA, Shah N, Wang KC, et al. Long non-coding RNA HOTAIR reprograms chromatin state to promote cancer metastasis. Nature. 2010;464(7291):1071–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Fatica A, Bozzoni I. Long non-coding RNAs: new players in cell differentiation and development. Nat Rev Genet. 2014;15(1):7–21. [DOI] [PubMed] [Google Scholar]
- 103. Meng L, Ward AJ, Chun S, Bennett CF, Beaudet AL, Rigo F. Towards a therapy for Angelman syndrome by targeting a long non-coding RNA. Nature. 2015;518(7539):409–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Maclary E, Buttigieg E, Hinten M, et al. Differentiation-dependent requirement of Tsix long non-coding RNA in imprinted X-chromosome inactivation. Nat Commun. 2014;5:4209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Kretz M, Siprashvili Z, Chu C, et al. Control of somatic tissue differentiation by the long non-coding RNA TINCR. Nature. 2013;493(7431):231–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Anguera MC, Ma W, Clift D, Namekawa S, Kelleher RJ, III, Lee JT. Tsx produces a long noncoding RNA and has general functions in the germline, stem cells, and brain. PLoS Genet. 2011;7(9):e1002248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Gibb EA, Brown CJ, Lam WL. The functional role of long non-coding RNA in human carcinomas. Mol Cancer. 2011;10:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Wang KC, Yang YW, Liu B, et al. A long noncoding RNA maintains active chromatin to coordinate homeotic gene expression. Nature. 2011;472(7341):120–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lee H, Kim C, Ku JL, et al. A long non-coding RNA snaR contributes to 5-fluorouracil resistance in human colon cancer cells. Mol Cells. 2014;37(7):540–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Bonasio R, Shiekhattar R. Regulation of transcription by long noncoding RNAs. Annu Rev Genet. 2014;48:433–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Cifuentes-Rojas C, Hernandez AJ, Sarma K, Lee JT. Regulatory interactions between RNA and polycomb repressive complex 2. Mol Cell. 2014;55(2):171–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Lee JT. Epigenetic regulation by long noncoding RNAs. Science. 2012;338(6113):1435–1439. [DOI] [PubMed] [Google Scholar]
- 113. Zheng Y, Tabbaa ZM, Khan Z, et al. Epigenetic Regulation of Uterine Biology by Transcription Factor KLF11 via Post-translational Histone Deacetylation of Cytochrome p450 Metabolic Enzymes. Endocrinology. 2014;155(11):4507–4520. [DOI] [PubMed] [Google Scholar]
- 114. Spittau B, Krieglstein K. Klf10 and Klf11 as mediators of TGF-beta superfamily signaling. Cell Tissue Res. 2012;347(1):65–72. [DOI] [PubMed] [Google Scholar]
- 115. Daftary GS, Zheng Y, Tabbaa ZM, et al. A novel role of the Sp/KLF transcription factor KLF11 in arresting progression of endometriosis. PloS One. 2013;8(3):e60165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Yin P, Lin Z, Reierstad S, et al. Transcription factor KLF11 integrates progesterone receptor signaling and proliferation in uterine leiomyoma cells. Cancer Res. 2010;70(4):1722–1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Wei LH, Torng PL, Hsiao SM, Jeng YM, Chen MW, Chen CA. Histone deacetylase 6 regulates estrogen receptor alpha in uterine leiomyoma. Reprod Sci. 2011;18(8):755–762. [DOI] [PubMed] [Google Scholar]
- 118. Aldana-Masangkay GI, Sakamoto KM. The role of HDAC6 in cancer. J Biomed Biotechnol. 2011;2011:875824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Svotelis A, Bianco S, Madore J, et al. H3K27 demethylation by JMJD3 at a poised enhancer of anti-apoptotic gene BCL2 determines ERalpha ligand dependency. EMBO J. 2011;30(19):3947–3961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Niv Y. Microsatellite instability and MLH1 promoter hypermethylation in colorectal cancer. World J Gastroenterol. 2007;13(12):1767–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Esteller M, Risques RA, Toyota M, et al. Promoter hypermethylation of the DNA repair gene O(6)-methylguanine-DNA methyltransferase is associated with the presence of G:C to A:T transition mutations in p53 in human colorectal tumorigenesis. Cancer Res. 2001;61(12):4689–4692. [PubMed] [Google Scholar]
- 122. Esteller M, Garcia-Foncillas J, Andion E, et al. Inactivation of the DNA-repair gene MGMT and the clinical response of gliomas to alkylating agents. N Engl J Med. 2000;343(19):1350–1354. [DOI] [PubMed] [Google Scholar]
- 123. Esteller M, Toyota M, Sanchez-Cespedes M, et al. Inactivation of the DNA repair gene O6-methylguanine-DNA methyltransferase by promoter hypermethylation is associated with G to A mutations in K-ras in colorectal tumorigenesis. Cancer Res. 2000;60(9):2368–2371. [PubMed] [Google Scholar]
- 124. Moore SD, Herrick SR, Ince TA, et al. Uterine leiomyomata with t(10;17) disrupt the histone acetyltransferase MORF. Cancer Res. 2004;64(16):5570–5577. [DOI] [PubMed] [Google Scholar]
- 125. Champagne N, Bertos NR, Pelletier N, et al. Identification of a human histone acetyltransferase related to monocytic leukemia zinc finger protein. J Biol Chem. 1999;274(40):28528–28536. [DOI] [PubMed] [Google Scholar]
- 126. Pelletier N, Champagne N, Lim H, Yang XJ. Expression, purification, and analysis of MOZ and MORF histone acetyltransferases. Methods. 2003;31(1):24–32. [DOI] [PubMed] [Google Scholar]
- 127. Georgieva B, Milev I, Minkov I, Dimitrova I, Bradford AP, Baev V. Characterization of the uterine leiomyoma microRNAome by deep sequencing. Genomics. 2012;99(5):275–281. [DOI] [PubMed] [Google Scholar]
- 128. Wang T, Zhang X, Obijuru L, et al. A micro-RNA signature associated with race, tumor size, and target gene activity in human uterine leiomyomas. Genes Chromosomes Cancer. 2007;46(4):336–347. [DOI] [PubMed] [Google Scholar]
- 129. Marsh EE, Lin Z, Yin P, Milad M, Chakravarti D, Bulun SE. Differential expression of microRNA species in human uterine leiomyoma versus normal myometrium. Fertil Steril. 2008;89:1771–1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Ingraham SE, Lynch RA, Surti U, et al. Identification and characterization of novel human transcripts embedded within HMGA2 in t(12;14)(q15;q24.1) uterine leiomyoma. Mutat Res. 2006;602(1-2):43–53. [DOI] [PubMed] [Google Scholar]
- 131. Fitzgerald JB, Chennathukuzhi V, Koohestani F, Nowak RA, Christenson LK. Role of microRNA-21 and programmed cell death 4 in the pathogenesis of human uterine leiomyomas. Fertil Steril. 2012;98(3):726–734. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Qiang W, Liu Z, Serna VA, et al. Down-regulation of miR-29b is essential for pathogenesis of uterine leiomyoma. Endocrinology. 2014;155(3):663–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Rinaldi L, Benitah SA. Epigenetic regulation of adult stem cell function[published online July 24, 2014]. FEBS J. 2014. [DOI] [PubMed] [Google Scholar]
- 134. Laugesen A, Helin K. Chromatin repressive complexes in stem cells, development, and cancer. Cell Stem Cell. 2014;14(6):735–751. [DOI] [PubMed] [Google Scholar]
- 135. Mazzarella L, Jorgensen HF, Soza-Ried J, et al. Embryonic stem cell-derived hemangioblasts remain epigenetically plastic and require PRC1 to prevent neural gene expression. Blood. 2011;117(1):83–87. [DOI] [PubMed] [Google Scholar]
- 136. Majewski IJ, Blewitt ME, de Graaf CA, et al. Polycomb repressive complex 2 (PRC2) restricts hematopoietic stem cell activity. PLoS Biol. 2008;6(4):e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Ezura Y, Sekiya I, Koga H, Muneta T, Noda M. Methylation status of CpG islands in the promoter regions of signature genes during chondrogenesis of human synovium-derived mesenchymal stem cells. Arthritis Rheum. 2009;60(5):1416–1426. [DOI] [PubMed] [Google Scholar]
- 138. Kang MI, Kim HS, Jung YC, et al. Transitional CpG methylation between promoters and retroelements of tissue-specific genes during human mesenchymal cell differentiation. J Cell Bioch. 2007;102(1):224–239. [DOI] [PubMed] [Google Scholar]
- 139. Sakamoto H, Kogo Y, Ohgane J, et al. Sequential changes in genome-wide DNA methylation status during adipocyte differentiation. Biochem Biophys Res Commun. 2008;366(2):360–366. [DOI] [PubMed] [Google Scholar]
- 140. Mohn F, Weber M, Rebhan M, et al. Lineage-specific polycomb targets and de novo DNA methylation define restriction and potential of neuronal progenitors. Mol Cell. 2008;30(6):755–766. [DOI] [PubMed] [Google Scholar]
- 141. Linder D, Gartler SM. Glucose-6-phosphate dehydrogenase mosaicism: utilization as a cell marker in the study of leiomyomas. Science. 1965;150(3692):67–69. [DOI] [PubMed] [Google Scholar]
- 142. Alam NA, Rowan AJ, Wortham NC, et al. Genetic and functional analyses of FH mutations in multiple cutaneous and uterine leiomyomatosis, hereditary leiomyomatosis and renal cancer, and fumarate hydratase deficiency. Hum Mol Genet. 2003;12(11):1241–1252. [DOI] [PubMed] [Google Scholar]
- 143. Linehan WM, Rouault TA. Molecular pathways: Fumarate hydratase-deficient kidney cancer--targeting the Warburg effect in cancer. Clin Cancer Res. 2013;19(13):3345–3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Barker KT, Spendlove HE, Banu NS, et al. No evidence for epigenetic inactivation of fumarate hydratase in leiomyomas and leiomyosarcomas. Cancer Lett. 2006;235(1):136–140. [DOI] [PubMed] [Google Scholar]
- 145. Ono M, Maruyama T, Masuda H, et al. Side population in human uterine myometrium displays phenotypic and functional characteristics of myometrial stem cells. Proc Natl Acad Sci U S A. 2007;104(47):18700–18705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Ono M, Qiang W, Serna VA, et al. Role of stem cells in human uterine leiomyoma growth. PloS One. 2012;7(5):e36935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Ono M, Yin P, Navarro A, et al. Paracrine activation of WNT/beta-catenin pathway in uterine leiomyoma stem cells promotes tumor growth. Proc Natl Acad Sci U S A. 2013;110(42):17053–17058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Galvez BG, Martin NS, Salama-Cohen P, et al. An adult myometrial pluripotential precursor that promotes healing of damaged muscular tissues. In Vivo. 2010;24(4):431–441. [PubMed] [Google Scholar]
- 149. Zhou S, Yi T, Shen K, Zhang B, Huang F, Zhao X. Hypoxia: the driving force of uterine myometrial stem cells differentiation into leiomyoma cells. Med Hypotheses. 2011;77(6):985–986. [DOI] [PubMed] [Google Scholar]
- 150. Chang HL, Senaratne TN, Zhang L, et al. Uterine leiomyomas exhibit fewer stem/progenitor cell characteristics when compared with corresponding normal myometrium. Reprod Sci. 2010;17(2):158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Mas A, Cervello I, Gil-Sanchis C, et al. Identification and characterization of the human leiomyoma side population as putative tumor-initiating cells. Fertil Steril. 2012;98(3):741–751. e6. [DOI] [PubMed] [Google Scholar]
- 152. Maruyama T, Ono M, Yoshimura Y. Somatic stem cells in the myometrium and in myomas. Semin Reprod Med. 2013;31(1):77–81. [DOI] [PubMed] [Google Scholar]
- 153. Mas A, Cervello I, Gil-Sanchis C, Simon C. Current understanding of somatic stem cells in leiomyoma formation. Fertil Steril. 2014;102(3):613–620. [DOI] [PubMed] [Google Scholar]
- 154. Szotek PP, Chang HL, Zhang L, et al. Adult mouse myometrial label-retaining cells divide in response to gonadotropin stimulation. Stem Cells. 2007;25(5):1317–1325. [DOI] [PubMed] [Google Scholar]
- 155. Ono M, Yin P, Navarro A, et al. Inhibition of canonical WNT signaling attenuates human leiomyoma cell growth. Fertil Steril. 2014;101(5):1441–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Benoit YD, Guezguez B, Boyd AL, Bhatia M. Molecular pathways: epigenetic modulation of Wnt/glycogen synthase kinase-3 signaling to target human cancer stem cells. Clin Cancer Res. 2014;20(21):5372–5378. [DOI] [PubMed] [Google Scholar]
- 157. Pastor WA, Pape UJ, Huang Y, et al. Genome-wide mapping of 5-hydroxymethylcytosine in embryonic stem cells. Nature. 2011;473(7347):394–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Booth MJ, Branco MR, Ficz G, et al. Quantitative sequencing of 5-methylcytosine and 5-hydroxymethylcytosine at single-base resolution. Science. 2012;336(6083):934–937. [DOI] [PubMed] [Google Scholar]
- 159. Raiber EA, Beraldi D, Ficz G, et al. Genome-wide distribution of 5-formylcytosine in embryonic stem cells is associated with transcription and depends on thymine DNA glycosylase. Genome Biol. 2012;13(8):R69. [DOI] [PMC free article] [PubMed] [Google Scholar]