Abstract
In rodents, complete bile duct ligation (cBDL) of the common bile duct is an established surgical technique for studying obstructive cholestasis and bile duct proliferation. However, long-term experiments can lead to increased morbidity and mortality. In select mouse strains with underlying liver disease, meaningful comparisons can be made even with ligation of a single lobe of the liver, which can reduce animal losses and expenses. Here, we describe partial bile duct ligation (pBDL) in the mouse, in which only the left hepatic bile duct is ligated, causing biliary obstruction in the left lobe but not the remaining lobes. With careful microsurgical technique, pBDL experiments can be cost-effective, since the unligated lobe serves as an internal control to the ligated lobes, when subjected to the same conditions in the same animal. Unlike cBDL, a separate sham-operated control group is not necessary. pBDL is highly useful to directly compare localized versus systemic effects of cholestasis and other retained bile components. pBDL can also be repurposed as a novel method to investigate mechanisms related to medications and cell migration.
Keywords: Biology, Issue 133, Mouse, Liver, BDL, pBDL, Cholestasis, Obstruction, Regeneration, Bile Acid, Fibrosis, Inflammation, Cholehepatic Shunt, Homing
Introduction
Surgical models of acute liver injury and repair, such as partial hepatectomy or common bile duct ligation (cBDL), have been used for decades in rodents to study liver regeneration and pathobiology1,2. In cBDL, the common bile duct (which drains all bile produced in the liver) is ligated, resulting in obstructive cholestasis, inflammation, and fibrosis in the first 2-3 weeks following surgery, with eventual progression to cirrhosis3. Bile duct proliferation, transdifferentiation, and induction of resident liver progenitor cells are also features of cBDL4,5. Although cBDL elucidates specific mechanisms of obstructive cholangiopathy, which are well-characterized with reproducible outcomes in wild-type mice and in those strains with normal livers6,7,8, the procedure can be technically demanding in some transgenic mouse models of liver diseases, requiring more animals than anticipated due to the higher morbidity and mortality of biliary obstruction over time. This technique is also beneficial for studying transgenic mice with underlying liver disease, which might not otherwise tolerate the stress of prolonged time course experiments following cBDL.
pBDL can provide a reasonable alternative to help overcome some of these challenges. Initial pBDL studies in wild-type mice aimed to distinguish locally acting and systemic mediators of inflammation9. In pBDL, the main biliary confluence of the right and left hepatic bile ducts above the common bile duct is carefully visualized at the hilum, and only the left hepatic bile duct is ligated to generate a localized obstructive cholestasis. pBDL offers several advantages to cBDL. In pBDL, the unligated right lobe serves as an identically matched internal control for the ligated left lobe, subjected to the same systemic effects, such as nutritional status or circulating factors. Although systemic pro-inflammatory mediators were present, Osawa et al. observed less fibrosis and necrosis in the unligated lobes, but increased inflammatory cells and transforming growth factor-β expression in the ligated lobe9.
More recently, pBDL has been redefined to study liver parenchymal effects of retained bile10. By using the same animal for internal control (unligated "sham") and experimental groups, pBDL effectively halves the number of animals needed per experiment, which in turn is more cost-effective. The mice tolerate the effects of pBDL much better, so that the ideal time course experiment (≥2 weeks) can be achieved in the ligated lobe. Most importantly, pBDL can distinguish direct intrahepatic effects of obstructive cholestasis and retained bile components in the ligated lobe, compared to the unligated control lobe. Overall, pBDL is an attractive method to study lobe-specific effects of localized cholestasis in the liver.
Protocol
All procedures were conducted in accordance with ethical guidelines of the Institutional Animal Care and Use Committee of the University of Pittsburgh.
1. Basic Techniques and Common Procedures
Autoclave all microsurgical equipment before use.
To avoid killing the mouse by anesthesia, check its breathing pattern carefully.
Touch organs and intestines as little as possible to avoid damaging organs and causing bleeding. Press bleeding points with wet cotton swabs or gauze sponges.
Use wet cotton swabs for gentle manipulation of organs. Wet, non-woven gauze sponges are used in two sizes, 3.5 × 3.5 cm and 6.0 × 6.0 cm. Use the smaller one to retract whole liver. Use the larger one to wrap the small and large intestines.
2. Presurgical Preparation
Use male c57/b6 mice, 8-12 weeks of age (when body weight is approximately 20-35 g) for partial bile duct ligation.
Allow the mice free access to water and food until induction of anesthesia.
3. Partial Bile Duct Ligation Operation
Anesthetize the mouse by putting the animal in an induction chamber with a mix of 1.5-2.0% isoflurane and 1 L/min oxygen. Monitor the animal carefully by observing the respiration rate. When the respiration rate of the animal is one breath per second, the mouse is well-anesthetized. Since front limb withdrawal reflex disappears more rapidly, pinch the hind limb foot as well to confirm complete absence of the withdrawal reflex. Eyes should be lubricated with an ophthalmic lubricating agent to prevent corneal ulcers. Note that first dose of analgesic can be given pre-operatively to prevent stimulation of pain receptors.
- Shave the abdominal wall with hair clippers, and place the mouse on the surgical table under the surgical microscope. Fix all limbs to the table with tape. Use isoflurane inhalation to maintain the mouse under general anesthesia.
- Adjust the isoflurane vaporizer and use 2.0-3.0% isoflurane for induction.
Using sterile swabs, disinfect the abdominal wall first with 0.3-0.5 mL povidone-iodine applied topically, followed by 70% ethanol. Animal should be covered with a sterile drape.
Make a long midline abdominal incision from the xiphoid to the pubis using the scissors and Adson Forceps. After making the abdominal incision, reduce isoflurane to 0.8-1.0% for maintenance.
Expose the abdominal cavity by using a Micro-retractor. Hold the xiphoid with mosquito forceps and retract toward the head of the mouse. Fix the mosquito forceps in place using soft clay.
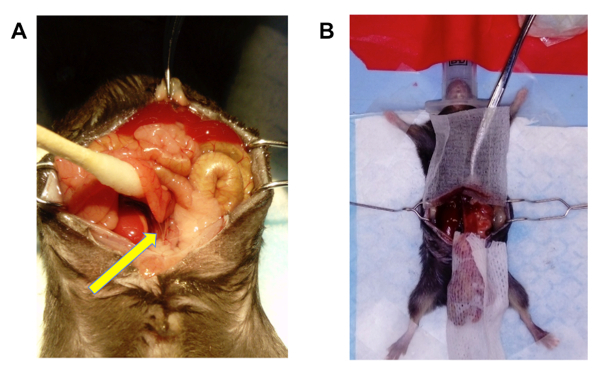
Instill 1-2 mL of warmed (37 °C) sterilized phosphate-buffered saline (PBS) into the abdominal cavity to avoid injuring abdominal organs. Hold the small intestines with wet cotton swabs and gently retract them toward the head of the mouse. Cut the ligaments between the small intestines and the retroperitoneum to avoid injuring the small intestines (Figure 1A).
Wrap the small and large intestines with a wet, non-woven gauze sponge. Place them on the caudal side of the abdominal cavity. Intestines wrapped in sterile gauze can be placed on the sterile draped field to avoid contamination.
Gently retract the whole liver toward the xiphoid by using a small wet non-woven gauze sponge to expose the hepatic hilum and hepato-duodenal ligament (Figure 1B).
Check to confirm the anatomy of the hepatic hilum. The common bile duct is located on ventral side of the portal vein. Confirm locations of the right and the left hepatic bile duct, which drain into the main biliary confluence at the hepatic hilum.
Identify the left hepatic bile duct which drains the left lobe, and encircle it with a 10-0 nylon suture using the blunt side of a suture needle (Figure 2A). Avoid injuring the portal vein, hepatic artery, and liver surface.
Ligate the left bile duct with 10-0 nylon. (Figure 2B).
Place the small and large intestines in the same position as before the operation by using wet cotton swabs.
Confirm there is no intestinal torsion and intra-abdominal bleeding, then close the muscle and the skin in two layers with 4-0 vicryl. Braided suture (Vicryl) was used for skin closure, but monofilament is preferred to reduce likelihood of infection. NOTE: Close fascia by continued suture from xiphoid to pubis, and close the skin by continued suture from pubis to xiphoid.
Stop anesthesia after closing the incision.

4. Postoperative Treatment and Follow-Up
Just after the surgery, pinch the dorsal skin of the mouse and inject Buprenex (0.1 mg/kg) and Cefazolin (100 mg/kg) subcutaneously, followed by Buprenex injection every 12 h for 3 days, and Cefazolin every 24 h for 3 days respectively11,12,13. Note that first dose of analgesic can be given pre-operatively to prevent stimulation of pain receptors. Cefazolin and other peri-operative antibiotics are only necessary for immune-suppressed animals, such as those used in transplantation studies. NOTE: If the surgery is successfully performed, the mouse usually recovers within 30 min. Activity of the mice will be almost the same as the preoperative condition.
- Check the mice daily for any signs of distress.
- Sacrifice the mice by the cervical dislocation under general anesthesia to procure livers and other tissue samples at defined time points (i.e., 7, 14, 21 days) after pBDL.
Representative Results
For this typical experiment, pBDL was performed in triplicate PiZ transgenic mice, which recapitulate the human liver disease found in alpha-1 antitrypsin (A1AT) deficiency. The PiZ mouse overexpresses a transgene consisting of multiple genomic fragments of DNA that contain the coding regions of the mutant human A1AT gene and promoter, together with introns and ~2 kilobases of upstream and downstream flanking regions14,15. Normal A1AT is a secreted serum protein produced in the liver. The mutant form of A1AT generates insoluble protein aggregates that spontaneously accumulate in the liver causing toxic stress. The experiments utilized 3-month old male PiZ mice, which express the most severe phenotype of this disease, when the protein aggregation peaks16.
Serum liver biochemistries were compared in pBDL and cBDL PiZ mice (Table 1)10. The liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are biomarkers of hepatocellular injury, while total serum bilirubin (TSB) measures the degree of cholestasis. Overall, mice subjected to pBDL did not show signs of severe liver injury or cholestasis, as their serum values were similar to baseline10. It is important to note that mice with failed pBDL (due to technical problems, such as bile duct or vascular injuries) will show serum values similar to cBDL mice, with significantly elevated liver enzymes and TSB. Clinically, mice with failed pBDL will appear more jaundiced and distressed, with findings of bile leaks, ascites, peritonitis, and/or hematoma, and will ultimately need to be sacrificed.
Since mice subjected to pBDL develop lobe-specific obstructive cholestasis, they do not acquire the distended, dark, bile-filled gallbladder seen in cBDL. Only the ligated lobe appears paler in color, while the unligated lobes will maintain their normal, dark, reddish-brown coloration (Figure 3). There are key differences in liver histology as well, with increased bile duct proliferation and fibrosis in the ligated lobe (Figure 4).10
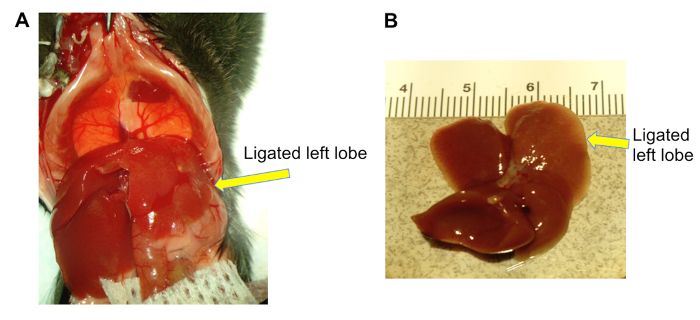
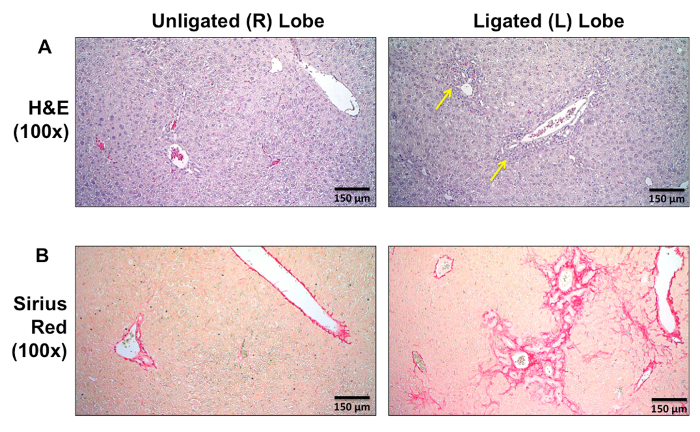
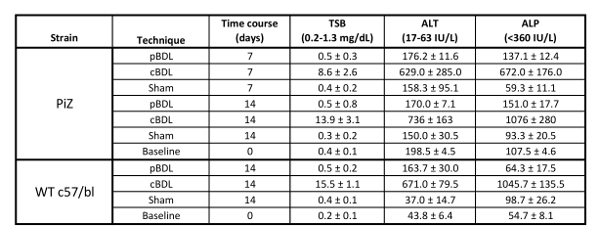 Table 1: Representative serum liver biochemistries from partial bile duct ligation (pBDL) compared to complete bile duct ligation (cBDL)10. Each time point represents 3-4 mice. Note PiZ transgenic mice are on a c57/bl6 background. Lab reference ranges are also given in parentheses. (WT, wild-type; TSB, total serum bilirubin; ALT, alanine aminotransferase; ALP, alkaline phosphatase).
Table 1: Representative serum liver biochemistries from partial bile duct ligation (pBDL) compared to complete bile duct ligation (cBDL)10. Each time point represents 3-4 mice. Note PiZ transgenic mice are on a c57/bl6 background. Lab reference ranges are also given in parentheses. (WT, wild-type; TSB, total serum bilirubin; ALT, alanine aminotransferase; ALP, alkaline phosphatase).
Figure 1:Exposure of abdominal cavity and hepatobiliary system. (A) Small intestines are gently retracted to avoid bowel injury, and the connecting ligaments are cut free from retroperitoneum. (B) Liver is gently retracted to allow maximal visualization of the biliary tree at the hepatic hilum (arrow). Please click here to view a larger version of this figure.
Figure 2: Partial bile duct ligation. (A) The blunt end of the surgical needle is used to carefully encircle the nylon suture around the left hepatic bile duct, above the confluence to the common bile duct (original magnification 40x). (B) Successful ligature of the left hepatic bile duct, which normally drains the left liver lobe. The remaining bile ducts are unligated (original magnification 40X). Please click here to view a larger version of this figure.
Figure 3: Gross appearance of the WT (c57/b6) mouse liver 14 days after pBDL. Note that the ligated left lobe appears paler in color (arrows), while the unligated lobes retain their normal, dark, reddish-brown coloration. Please click here to view a larger version of this figure.
Figure 4: Lobe-specific changes in representative liver tissue sections from day 14 pBDL comparing unligated right (R) lobe to ligated left (L) lobe in WT (c57/b6) mice. (A) Hematoxylin and eosin (H&E) staining showing increased bile duct proliferation (arrows) in the ligated lobe. (B) Sirius red stain showing bridging fibrosis accompanying bile duct proliferation in the ligated lobe. Histology for the PiZ mouse has been previously reported10. Please click here to view a larger version of this figure.
Discussion
Although cBDL is the most common experimental technique for obstructive cholestasis, it can present multiple challenges in rodents. Depending on the number of post-operative days required to achieve an endpoint, the animals can experience significant morbidity and mortality as time progresses. The degree of tissue injury and biliary necrosis is further exacerbated when working with some transgenic mouse models of liver disease, which demonstrate abnormal liver parenchyma and function at baseline. Compared to cBDL, reports of pBDL are limited, but this technique can be applied as an alternative in select experiments to reduce negative outcomes and animal losses.
Variations in the pBDL method have also been reported. In the method of Heinrich et al., an external curved needle is placed adjacent to the common bile duct, followed by ligature around both the common bile duct and the needle17. The needle is then removed prior to abdominal wall closure, resulting in limited bile flow through a narrowed lumen (i.e., subtotal obstruction) of the bile duct17. During this procedure, the gall bladder is also removed to prevent cholecystitis17. The authors concluded that this method was more beneficial to study acute cholestasis rather than chronic changes17. In contrast, the pBDL method we described here is tightly controlled, with both ligated and unligated ("sham") lobes in the same animal, so less animals are required per experiment. Even transgenic mice with severe underlying liver disease can be sustained for longer end points (2-3 weeks). Care must be taken to fully expose and identify the biliary tree using microdissection techniques, with limited manipulation of vascular structures and bile ducts to prevent injury.
In the ideal experiment, tissues from the ligated (left) and unligated (right) lobes will be harvested at the same time, so direct comparisons of bile secretory function and transporters can be made using histologic and molecular techniques. Although serum liver biochemistries will not reflect severe cholestasis, the ligated lobe will demonstrate histologic changes associated with obstructive cholestasis10. This model is useful to study direct microenvironmental effects of retained bile components (e.g., bile acids, lipids, cholesterol) within the liver. As a future study, pBDL may be considered to investigate cholehepatic shunting, where certain bile acids and drugs are reabsorbed directly from cholangiocytes to hepatocytes18,19. Endogenous bile acids inefficiently conjugated by hepatocytes are passively absorbed by biliary epithelium to undergo cholehepatic shunting as well, leading to hypercholeresis and alkanlinization of the bile by increased bicarbonate secretion20. Application of the pBDL technique could facilitate drug discovery by identifying pharmacologic mechanisms for novel bile acid therapeutics under investigation for liver disease.
Additional applications for pBDL can extend beyond the biliary tree. Reversibility of cBDL and its associated effects has been described, and this may also be applied to pBDL with direct comparison to the internal control21. Similarly, longitudinal in vivo bioimaging of fluorescent reporter expression in mouse liver has been studied after cBDL22, with powerful implications for pBDL experiments. Furthermore, rodent experiments using pBDL have the potential to incorporate lineage tracing or "homing" of circulating cells, such as bone marrow-derived mesenchymal cells, to the site of liver injury, allowing them to be tracked in vivo with more precision23,24,25.
Clearly, there are widespread applications for pBDL alone as an internally controlled and reproducible technique to study liver injury and repair, along with biliary physiology and drug metabolism. For experiments that aim to evaluate the progression and systemic effects of chronic cholestasis, cBDL is still the most preferred method; however, pBDL would still add complementary data to support such findings.
Disclosures
The authors have no disclosures.
Acknowledgments
Dr. Khan acknowledges grant support from NIH/NICHD K12HD052892, the Alpha-1 Foundation, the Hillman Foundation, and the Pittsburgh Liver Research Center. Dr. Michalopoulos acknowledges grant support from NIH/NIDDK P01DK096990. We appreciate the excellent and generous technical assistance of Anne Orr. We are also grateful to Dr. David A. Geller for providing access to the Transplant/Rodent Microsurgery lab.
References
- Higgins GM, Anderson R. Experimental pathology of the liver - Restoration of the liver of the white rat following partial surgical removal. Arch Pathol. 1931;12:186–202. [Google Scholar]
- Cameron GR, Oakley CL. Ligation of the common bile duct. The Journal of Pathology and Bacteriology. 1932;35(5):769–798. [Google Scholar]
- Kountouras J, Billing BH, Scheuer PJ. Prolonged bile duct obstruction: a new experimental model for cirrhosis in the rat. Br J Exp Pathol. 1984;65(3):305–311. [PMC free article] [PubMed] [Google Scholar]
- Michalopoulos GK, Barua L, Bowen WC. Transdifferentiation of rat hepatocytes into biliary cells after bile duct ligation and toxic biliary injury. Hepatology. 2005;41(3):535–544. doi: 10.1002/hep.20600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dipaola F, et al. Identification of intramural epithelial networks linked to peribiliary glands that express progenitor cell markers and proliferate after injury in mice. Hepatology. 2013;58(4):1486–1496. doi: 10.1002/hep.26485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyot C, Combe C, Desmouliere A. The common bile duct ligation in rat: A relevant in vivo model to study the role of mechanical stress on cell and matrix behaviour. Histochem Cell Biol. 2006;126(4):517–523. doi: 10.1007/s00418-006-0185-2. [DOI] [PubMed] [Google Scholar]
- Zhang Y, et al. Effect of bile duct ligation on bile acid composition in mouse serum and liver. Liver Int. 2012;32(1):58–69. doi: 10.1111/j.1478-3231.2011.02662.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tag CG, et al. Bile duct ligation in mice: induction of inflammatory liver injury and fibrosis by obstructive cholestasis. J Vis Exp. 2015. p. e52438. [DOI] [PMC free article] [PubMed]
- Osawa Y, et al. Systemic mediators induce fibrogenic effects in normal liver after partial bile duct ligation. Liver Int. 2006;26(9):1138–1147. doi: 10.1111/j.1478-3231.2006.01346.x. [DOI] [PubMed] [Google Scholar]
- Khan Z, et al. Bile Duct Ligation Induces ATZ Globule Clearance in a Mouse Model of alpha-1 Antitrypsin Deficiency. Gene Expr. 2017;17(2):115–127. doi: 10.3727/105221616X692991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birkhead HA, Briggs GB, Saunders LZ. Toxicology of cefazolin in animals. J Infect Dis. 1973;128:378. doi: 10.1093/infdis/128.supplement_2.s379. [DOI] [PubMed] [Google Scholar]
- Kunst MW, Mattie H, van Furth R. Antibacterial efficacy of cefazolin and cephradine in neutropenic mice. Infection. 1979;7(1):30–34. doi: 10.1007/BF01640554. [DOI] [PubMed] [Google Scholar]
- Traul KA, et al. Safety studies of post-surgical buprenorphine therapy for mice. Lab Anim. 2015;49(2):100–110. doi: 10.1177/0023677214554216. [DOI] [PubMed] [Google Scholar]
- Carlson JA, et al. Accumulation of PiZ alpha 1-antitrypsin causes liver damage in transgenic mice. J Clin Invest. 1989;83(4):1183–1190. doi: 10.1172/JCI113999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sifers RN, Finegold MJ, Woo SL. Alpha-1-antitrypsin deficiency: accumulation or degradation of mutant variants within the hepatic endoplasmic reticulum. Am J Respir Cell Mol Biol. 1989;1(5):341–345. doi: 10.1165/ajrcmb/1.5.341. [DOI] [PubMed] [Google Scholar]
- Rudnick DA, Shikapwashya O, Blomenkamp K, Teckman JH. Indomethacin increases liver damage in a murine model of liver injury from alpha-1-antitrypsin deficiency. Hepatology. 2006;44(4):976–982. doi: 10.1002/hep.21326. [DOI] [PubMed] [Google Scholar]
- Heinrich S, et al. Partial bile duct ligation in mice: a novel model of acute cholestasis. Surgery. 2011;149(3):445–451. doi: 10.1016/j.surg.2010.07.046. [DOI] [PubMed] [Google Scholar]
- Glaser SS, Alpini G. Activation of the cholehepatic shunt as a potential therapy for primary sclerosing cholangitis. Hepatology. 2009;49(6):1795–1797. doi: 10.1002/hep.22969. [DOI] [PubMed] [Google Scholar]
- Gurpinar E, et al. A novel sulindac derivative inhibits lung adenocarcinoma cell growth through suppression of Akt/mTOR signaling and induction of autophagy. Mol Cancer Ther. 2013;12(5):663–674. doi: 10.1158/1535-7163.MCT-12-0785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alpini GG, Francis H, Marzioni M, Venter J, Phinizy J, LeSage G. Madame Curie Bioscience Database. Austin, TX: Landes Bioscience; 2013. [Google Scholar]
- Kirkland JG, et al. Reversible surgical model of biliary inflammation and obstructive jaundice in mice. J Surg Res. 2010;164(2):221–227. doi: 10.1016/j.jss.2009.08.010. [DOI] [PubMed] [Google Scholar]
- Delhove JM, et al. Longitudinal in vivo bioimaging of hepatocyte transcription factor activity following cholestatic liver injury in mice. Sci Rep. 2017;7:41874. doi: 10.1038/srep41874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C, et al. Homing of bone marrow mesenchymal stem cells mediated by sphingosine 1-phosphate contributes to liver fibrosis. J Hepatol. 2009;50(6):1174–1183. doi: 10.1016/j.jhep.2009.01.028. [DOI] [PubMed] [Google Scholar]
- Xu J, et al. Factors released from cholestatic rat livers possibly involved in inducing bone marrow hepatic stem cell priming. Stem Cells Dev. 2008;17(1):143–155. doi: 10.1089/scd.2007.0094. [DOI] [PubMed] [Google Scholar]
- Sharma S, et al. Propitious role of bone marrow-derived mononuclear cells in an experimental bile duct ligation model: potential clinical implications in obstructive cholangiopathy. Pediatr Surg Int. 2013;29(6):623–632. doi: 10.1007/s00383-013-3314-8. [DOI] [PubMed] [Google Scholar]


