This study prospectively evaluates the quality of the field triage system to identify severely injured adult trauma patients.
Key Points
Question
What is the quality of the field triage system to identify severely injured adult trauma patients?
Findings
This study included 4950 trauma patients and shows that more than 20% of the patients with severe injuries were not transported to a level I trauma center.
Meaning
A significant group of severely injured trauma patients does not receive the appropriate level I trauma care, putting these patients at risk for increased morbidity and mortality; improvement of prehospital triage is necessary.
Abstract
Importance
A major component of trauma care is adequate prehospital triage. To optimize the prehospital triage system, it is essential to gain insight in the quality of prehospital triage of the entire trauma system.
Objective
To prospectively evaluate the quality of the field triage system to identify severely injured adult trauma patients.
Design, Setting, and Participants
Prehospital and hospital data of all adult trauma patients during 2012 to 2014 transported with the highest priority by emergency medical services professionals to 10 hospitals in Central Netherlands were prospectively collected. Prehospital data collected by the emergency medical services professionals were matched to hospital data collected in the trauma registry. An Injury Severity Score of 16 or more was used to determine severe injury.
Main Outcomes and Measures
The quality and diagnostic accuracy of the field triage protocol and compliance of emergency medical services professionals to the protocol.
Results
A total of 4950 trauma patients were evaluated of which 436 (8.8%) patients were severely injured. The undertriage rate based on actual destination facility was 21.6% (95% CI, 18.0-25.7) with an overtriage rate of 30.6% (95% CI, 29.3-32.0). Analysis of the protocol itself, regardless of destination facility, resulted in an undertriage of 63.8% (95% CI, 59.2-68.1) and overtriage of 7.4% (95% CI, 6.7-8.2). The compliance to the field triage trauma protocol was 73% for patients with a level 1 indication.
Conclusions and Relevance
More than 20% of the patients with severe injuries were not transported to a level I trauma center. These patients are at risk for preventable morbidity and mortality. This finding indicates the need for improvement of the prehospital triage protocol.
Introduction
Adequate prehospital trauma triage of injured patients is imperative for optimal trauma care. In an inclusive trauma system, it is essential to transport patients with severe injuries to a level I trauma center and patients without severe injuries to lower-level hospitals. Previous studies have clearly shown lower mortality rates in patients with severe injuries treated at a level I trauma center compared with patients treated at a lower-level hospitals.
Management of care of the injured trauma patient on the scene of injury remains challenging, and situations can be chaotic. After a rapid trauma assessment of clinical and physiological parameters, emergency medical services (EMS) professionals must identify patients at risk for severe injury and select the proper destination. Prehospital triage protocols are used to help define the patient destination. However, triage of patients without evident abnormality and instability at presentation remains challenging given the limited facilities on scene.
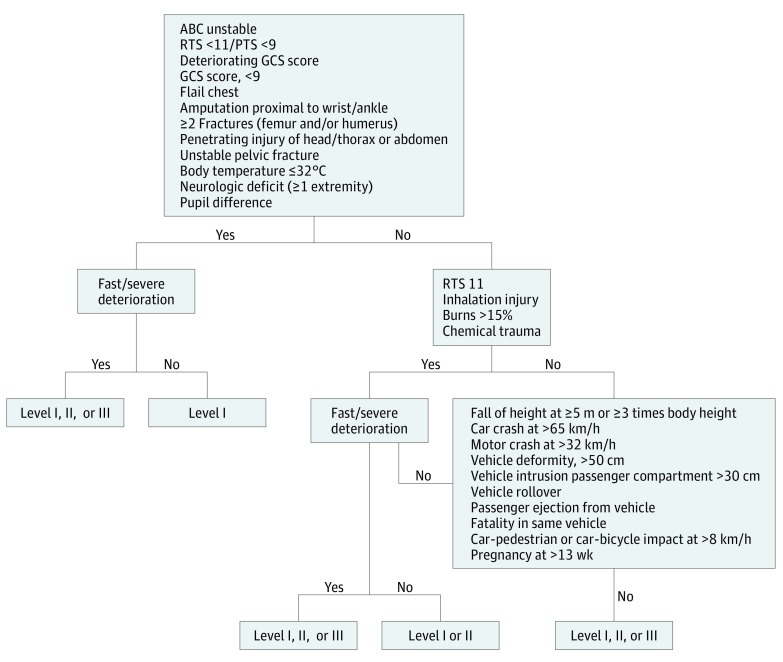
In the Netherlands, allocation of trauma patients to the appropriate level of trauma care is guided by the Dutch Field Triage Protocol (version 7.1, National Protocol of Ambulance Services), for EMS professionals (Figure 1). This protocol is based on the Field Triage Decision Scheme established by the American College of Surgeons Committee on Trauma (ACS-COT).
Figure 1. The Field Triage Protocol for the Distribution of Trauma Patients Over Different Hospitals.
ABC indicates airway, breathing, and circulation; GCS, Glasgow Coma Scale; PTS, Pediatric Trauma Score; RTS, Revised Trauma Score.
Quality of prehospital triage can be determined by rates of undertriage and overtriage. Undertriage is defined as the proportion of patients with severe injuries not transported to a level I trauma center. Overtriage is defined as the proportion of patients without severe injuries transported to a level I trauma center. Undertriage results in higher mortality and delay of adequate care, whereas overtriage limits the available level I resources for patients without severe injuries. To optimize the prehospital triage system, it is essential to gain insight in the quality of prehospital triage of the entire trauma system or region. The benchmark level in the ACS-COT guidelines is a maximum undertriage rate of 5%, allowing for an overtriage rate of up to 50%. In a Dutch population consisting of high-energy trauma patients only, the undertriage rate was 11%. The quality of triage in the complete trauma population is unknown.
This present study aims to evaluate the quality of the Dutch field triage protocol for identifying severely injured trauma patients in a population consisting of adult trauma patients transported by EMS professionals with the highest priority in the Central Netherlands region.
Methods
Study Design and Setting
The present study was performed in the Central Netherlands region using prospectively collected prehospital and hospital data of all adult trauma patients transported with the highest priority by the Regional Ambulance Service Utrecht to 1 of the 10 hospitals in Central Netherlands between January 2012 and July 2014. The region Central Netherlands consists of 9 level II and level III hospitals and 1 level I trauma center in a 2418-km2 region with a population of 1.2 million people. The University Medical Center Utrecht is designated as a level I trauma center, offering trauma care at the highest level for severely injured patients. The 9 surrounding level II and III hospitals are designed to treat patients without severe injuries. This regional trauma network is based on an inclusive and integrated trauma system. The ambulance care system is nurse-based. Ambulance nurses are licensed to administer medical treatment at advanced life support level, and ambulance drivers are qualified to provide medical assistance to the ambulance nurses. The present study protocol was reviewed and approved by the local medical ethical committee, and patient consent was waived. Analyses began in 2016.
Patients
All trauma patients 16 years and older transported by EMS professionals with the highest priority were included in the study. Patients transported to a hospital outside Central Netherlands and patients transported by helicopter were excluded. Patients were also excluded if insufficient data were available in the receiving hospital to properly calculate the Injury Severity Score (ISS).
Data Collection
Prehospital reports from EMS professionals were prospectively collected and included patient demographics, description of the trauma mechanism, physical examination data on site, prehospital treatment, and receiving hospital. Furthermore, the report included a standardized digital report of specific vital parameters, ie, Glasgow Coma Scale score, respiratory rate, systolic blood pressure level, heart rate, pupil deficit, and Revised Trauma Score.
The Dutch national trauma database registers in-hospital data regarding injuries and complications for all trauma patients admitted to a hospital. For patients who were discharged from the emergency department, data were extracted from the electronic patient documentation. Injuries were encoded according to the Abbreviated Injury Scale 90 Update 98. Injury Severity Scores were calculated and used to assess overall injury severity.
Outcome
Severe injury was defined as an ISS of 16 or more. The primary outcome of this study was the quality of the field triage system in terms of undertriage and overtriage. Undertriage was defined as the proportion of severely injured patients (ISS, ≥16) erroneously transported to level II or III hospitals. Overtriage was defined as the proportion of patients with an ISS of less than 16 transported to a level I trauma center.
The diagnostic accuracy of the Dutch field triage protocol was calculated for identifying patients with or without severe injuries, regardless of actual destination facility. For this purpose, the level I triage criteria were retrospectively applied to the data set. For this part of the analysis, undertriage was defined as the proportion of patients with severe injuries not identified by the prehospital trauma triage protocol, divided by the total number of severely injured patients. Overtriage was defined as the proportion of patients without severe injuries identified as severely injured patients using the prehospital trauma triage protocol. Prehospital level I criteria were penetrating injury (head, thorax, and/or abdomen), 2 or more fractures of long bones (humerus and/or femur), amputation proximal to wrist or ankle, neurologic failure in 1 or more extremity, unstable pelvic fracture, pupil difference, flail chest, Glasgow Coma Scale score more than 9, deteriorating Glasgow Coma Scale score, Revised Trauma Score less than 11, vitally compromised in airway and breathing or circulation, and body temperature of 32°C or more.
Finally, the compliance of EMS professionals for correct transportation of patients with prehospital level I trauma center criteria according to the Dutch field triage protocol was determined.
Statistical Analysis
Data were analyzed using descriptive statistics, and results were shown in frequencies and percentages. Undertriage and overtriage rates were presented with 95% CI. Multiple imputation was used for missing prehospital values and was performed with SPSS IBM statistical software (version 23.0). Missing values were predicted based on all other predictors, as well as the outcome (ISS). All logistic regression analyses were performed on 5 imputed data sets independently and pooled afterwards for missing prehospital values. Multiple imputation for missing prehospital values has been previously validated. Multiple imputation was used for pulse in 6.76%, respiratory rate in 6.52%, systolic blood pressure in 6.96%, Revised Trauma Score in 8.14%, and Glasgow Coma Scale score in 4.59%.
Results
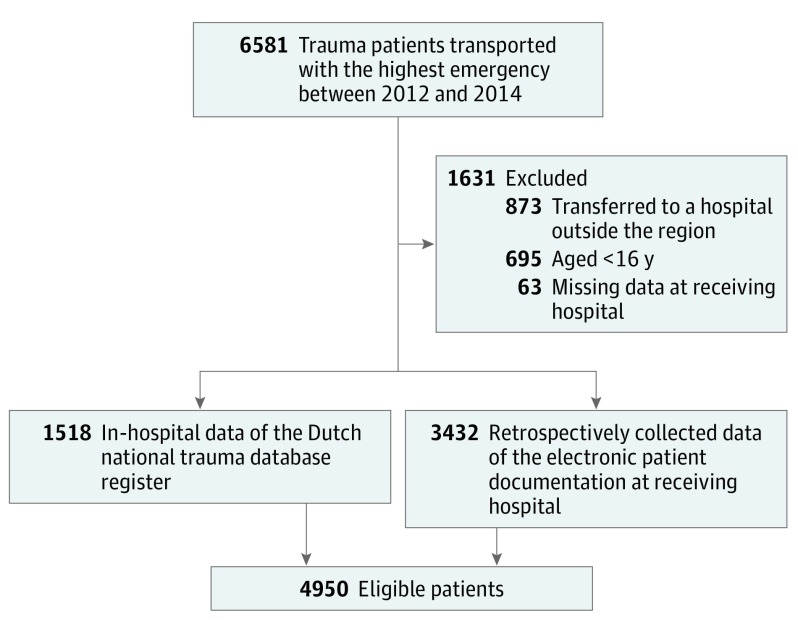
A total of 6581 trauma patients were transported by EMS professionals with the highest priority in Central Netherlands. Inclusion criteria were met in 4950 patients for the current analysis (Figure 2). Characteristics of the study sample are shown in Table 1. Patients were relatively equally distributed between the hospitals: level I, 1724 patients (34.8%); level II, 1326 patients (26.8%); and level III, 1900 patients (38.4%). The median age was 45 years, 2887 were male (58.3%), and 436 had an ISS of 16 or more (8.8%). Severe injury in 1 of the body regions (Abbreviated Injury Scale score, ≥3) was most frequently diagnosed in the head and extremities.
Figure 2. Flowchart of Patient Enrollment.
Table 1. Characteristics of the Study Population.
| Variable | Patients, No. (%) (N = 4950) |
|---|---|
| Male | 2887 (58.3) |
| Age, median (IQR), y | 45 (27-63) |
| Elderly adults (>65 y) | 1085 (21.9) |
| Prehospital GCS score <9 | 141 (2.8) |
| Triage criteria | |
| Mechanism of injury | 1300 (26.3) |
| Physiological criteria | 289 (5.8) |
| Injury criteria | 256 (5.2) |
| Assistance of air medical services | 119 (2.4) |
| Out-of-hospital intubation | 49 (1.0) |
| Transfer to | |
| Level I trauma center | 1724 (34.8) |
| Level II trauma center | 1326 (26.8) |
| Level III trauma center | 1900 (38.4) |
| ISS, median (IQR) | 2 (1-5) |
| Severely injured (ISS, ≥16) | 436 (8.8) |
| AIS score ≥3 per region | |
| Head and neck | 435 (8.8) |
| Face | 26 (0.5) |
| Thorax | 318 (6.4) |
| Abdomen | 61 (1.2) |
| Extremities | 496 (10.0) |
| External | 12 (0.2) |
| In-hospital stay | 2047 (41.4) |
| Mortality | 61 (1.2) |
Abbreviations: AIS, Abbreviated Injury Scale; GCS, Glasgow Coma Scale; IQR, interquartile range; ISS, Injury Severity Score.
Of 436 patients with severe injuries, 94 were erroneously transported to level II or level III hospitals, resulting in an undertriage of 21.6% (95% CI, 18.0-25.7). Transportation of 1382 of 4514 patients without severe injuries to the level I trauma center resulted in an overtriage of 30.6% (95% CI, 29.3-32.0) (Table 2).
Table 2. Quality of Field Triage System Regarding Correct Destination Facility for Patients With and Without Severe Injuries.
| Variable | Patients With Severe Injuries (ISS, ≥16) (n = 436) | Patients Without Severe Injuries (ISS, <16) (n = 4514) |
|---|---|---|
| Quality of field triage system regarding correct destination facility for patients with and without severe injuries | ||
| Level I trauma center, No. (%) | 342 (78.4) | 1382 (30.6) |
| Level II/III trauma center, No. (%) | 94 (21.6) | 3132 (69.4) |
| Undertriage, % (95% CI)a | 21.6 (18-25.7) | NA |
| Overtriage, % (95% CI)b | NA | 30.6 (29.3-32) |
| Diagnostic accuracy of the Dutch prehospital field triage protocol for identifying patients with and without severe injuries | ||
| Level I trauma center indication, No. (%) | 158 (36.2) | 334 (7.4) |
| No level I trauma center indication, No. (%) | 278 (63.8) | 4180 (92.6) |
| Undertriage, % (95% CI)c | 63.8 (59.2-68.1) | NA |
| Overtriage, % (95% CI)d | NA | 7.4 (6.7-8.2) |
Abbreviations: ISS, Injury Severity Score; NA, not applicable.
Proportion of patients with severe injuries (ISS, ≥16) not transported to level I trauma center.
Proportion of patients without severe injuries (ISS, <16) transported to level I trauma center.
Proportion of patients with severe injuries (ISS, ≥16) without positive prehospital level I criteria according to the field triage protocol.
Proportion of patients without severe injuries (ISS, <16) with positive prehospital level I criteria according to the field triage protocol.
The diagnostic accuracy of the Dutch field triage protocol is shown in Table 2. The protocol-based undertriage was 63.8% (95% CI, 59.2-68.1), and the protocol-based overtriage was 7.4% (95% CI, 6.7-8.2). The compliance of EMS professionals to the field triage was 72.6%. Overall, 30% of the patients with a positive injury and/or physiology criteria were not transported to a level 1 trauma center.
Table 3 illustrates the undertriage and overtriage rates for different subgroups of the study population regarding correct destination facility. The undertriage rate in elderly patients is high at 38.6% (95% CI, 30.8-47.2). A high-energy trauma mechanism resulted in an undertriage rate of 9.1% (95% CI, 5.8-14.2). The group of patients with a positive injury and/or physiological criteria showed low undertriage rates (0% and 2.6%, respectively).
Table 3. Quality of Field Triage System Regarding Correct Destination Facility for Different Subgroups.
| Variable | Total Patients, No. | Patients With Severe Injuries, No. (%) | Rate (95% CI) | |
|---|---|---|---|---|
| Undertriagea | Overtriageb | |||
| Men | 2887 | 295 (10.2) | 19.7 (15.5-24.6) | 32.8 (31-34.6) |
| Women | 2063 | 141 (6.8) | 25.5 (19.1-33.3) | 27.7 (25.8-29.8) |
| Adults (≤65 y) | 3865 | 304 (7.9) | 14.1 (10.7-18.5) | 33.2 (31.6-34.7) |
| Elderly adults (>65 y) | 1085 | 132 (12.2) | 38.6 (30.8-47.2) | 21.1 (18.6-23.8) |
| Mechanism criteria | 1301 | 186 (14.3) | 9.1 (5.8-14.2) | 55.3 (41.8-47.6) |
| Injury criteria | 256 | 81 (31.6) | 0 (0-4.5) | 33.1 (26.6-40.4) |
| Physiological criteria | 289 | 116 (40.1) | 2.6 (0.9-7.3) | 55.5 (48.1-62.7) |
| Head injury | 2143 | 304 (14.2) | 22 (17.7-27.1) | 32.7 (30.6-34.9) |
Proportion of patients with severe injuries (Injury Severity Score, ≥16) not transported to level I trauma center.
Proportion of patients without severe injuries (Injury Severity Score, <16) transported to level I trauma center.
Discussion
This study presents a quality assessment of prehospital triage in identifying severely injured trauma patients using prospectively collected data. Prehospital data were collected from EMS professionals and included every type of trauma patient transported with the highest priority, whether admitted or discharged from the emergency department in all types of hospitals.
The quality of the Dutch field triage protocol remains relatively low. The overall rate of undertriage of the prehospital trauma triage system was 22% and is significantly higher than the benchmark level of 5%, as set by the ACS-COT. This implies that a significant group of trauma patients with severe injuries does not receive the appropriate level I trauma care. These patients are therefore at risk for increased morbidity and mortality.
A variety of causes can be identified for undertriage. Closer examination of the elderly patients (aged ≥65 years) in the present study showed a high undertriage rate of 39%. The undertriage rate among the elderly patients was 25% higher compared with younger adults. These findings are in accordance with previous studies showing increased undertriage rates in elderly patients. Elderly patients tend to have more cognitive and physical impairments with preexisting comorbidity, and therefore low energy trauma mechanisms may result in serious injuries. Undertriage of elderly patients remains a substantial problem. Modifications to the adult criteria of the ACS-COT triage protocol have been made to accentuate these physiological and anatomical differences of the elderly population. However, the effect of these modifications has not yet been evaluated.
A considerable proportion of trauma patients in our study population experienced traumatic brain injury. Patients with traumatic brain injury are at risk of undertriage because the identification of significant traumatic brain injury can be demanding in the prehospital setting. Previous studies showed a high risk of undertriage in patients with isolated head injuries. In our study population, more than 75% of the undertriaged patients received a diagnosis of a cranial Abbreviated Injury Scale score of at least 3. These patients need access for direct neurosurgical care.
Overtriage is also an important outcome parameter to monitor because high overtriage rates lead to reduced system efficiency, unnecessary burden to the level I trauma center, and lower cost-effectiveness. Our study showed an acceptable overtriage rate of 31% (95% CI, 29.3-32.0). As undertriage and overtriage rates are inversely proportional quantities, overtriage will increase as undertriage is lowered. Overtriage rates of up to 50% are acceptable for prehospital triage to keep undertriage rates to a minimum. Therefore, an overtriage rate of 31% should provide room for improvement of undertriage rates.
Our findings support the results of previous studies and confirm that undertriage rates remain high. Although past studies were retrospective, 1 exception is a 2016 prospective study investigating the ACS-COT triage protocol including 17 633 trauma patients, of which 3% were seriously injured (ISS, ≥16). A large group of patients was excluded because of study sampling design, and Newgard et al reported a significant amount of missing hospital data. The authors reported an undertriage rate of 36.4% and an overtriage rate of 28.7% based on the initial receiving hospital. After accounting for interhospital transfers, the undertriage rate was 22%. This higher undertriage rate compared with our results cannot be explained by the difference in protocols because the Dutch field triage protocol has a higher threshold for transport to a level I trauma center. However, there are significant regional differences. Hospitals in Central Netherlands are clustered in relatively close proximity. The level I trauma center is always within a 15-minute drive for an ambulance, whereas this could be more than 60 minutes in some of the regions studied by Newgard et al. The significant lowering of the undertriage rate after accounting for interhospital transfers in the study of Newgard et al could suggest at least some role of hospital proximity. Previous research shows higher mortality rates in trauma patients after interhospital transfers. This emphasizes the need to correctly identify and transport patients with severe injuries directly to a level 1 trauma center.
A previous evaluation of the Dutch field triage protocol by our study group revealed undertriage and overtriage rates of 10.9% and 39.5%, respectively. However, this study exclusively included high-energy trauma patients, which could very well explain the difference in Dutch field triage protocol rates compared with the present study. Although high-energy trauma is not a strict level 1 criterion in the current field triage protocol, it can be hypothesized that patients who have an obvious high-energy trauma are more prone to be transported to a level I trauma center owing to EMS professionals’ judgement. Other studies have demonstrated that the use of a mechanism of injury criterion could lower undertriage and suggest that specific high-energy trauma criteria should be included in the level 1 criteria. Evaluation of the subgroup of patients after a high-energy trauma in the present study also revealed a lower undertriage rate of 9%, supporting the suggestion to include mechanism of injury as level 1 criterion.
The exceptionally high undertriage rate calculated for the prehospital protocol itself reflects the shortcomings of the currently used protocol. It truly fails to support EMS professionals to correctly identify severely injured patients in need of level I trauma care. Fortunately, owing to EMS professionals’ judgment, a large group of the severely injured trauma patients was still transported to the trauma center and received appropriate care. The discrepancy in undertriage rates between the protocol itself (64%) and actual undertriage based on destination facility (22%) is probably best explained by the correct assessment of the EMS professionals based on experience regardless of protocol. Previous studies also showed improved triage rates after including EMS professionals’ judgement as a triage criterion. The preference of the patient and existing transport patterns could also influence the decision for destination facility; however, the impact of these factors could not be assessed.
A validated definition of patients with severe injuries does not yet exist in prehospital trauma triage, to our knowledge. A panel of international experts advised to use a set of parameters for the definition, including 2 injuries with an Abbreviated Injury Scale score of 3 or more and 1 or more additional diagnosis. This would predict a mortality rate of 30% or greater for this group. We defined a severely injured patient as having an ISS of 16 or more. Patients’ needs should be matched to the hospital’s capability. In this study region, only 1 level I trauma center offers round-the-clock availability of a designated trauma team and continued availability of neurosurgical care. Most patients with an ISS of 16 or more are likely to benefit from level I trauma care.
Strengths and Limitations
A strength of this study is the prospective prehospital data collection and study design that included all trauma patients transported to all types of hospitals in a specific region. Furthermore, the triage protocol currently investigated is based on the ACS-COT triage protocol, which is adapted as a standard in many organizations worldwide. Therefore, the findings of this study may be of international importance.
This study has several limitations. The exclusion of patients transported to hospitals outside the study region could result in sampling bias, the extent of which is unknown. As mentioned, the Dutch national trauma database does not register patients who are not admitted to the hospital. Although data of admitted trauma patients were prospectively collected by a dedicated group of trained data managers, our research group collected the hospital data of patients discharged from the emergency department retrospectively. These retrospectively collected data are not expected to affect the study results because this group consists of patients with minor injuries.
Conclusions
The present study shows that more than 20% of the patients with severe injuries were not transported to a level I trauma center. These patients are at risk for preventable morbidity and mortality. It also showed that the accuracy of the Dutch field triage protocol in selecting patients with severe injuries is low and therefore of insufficient help to EMS professionals. Our findings indicate the need for improvement of the prehospital triage protocol.
References
- 1.Twijnstra MJ, Moons KG, Simmermacher RK, Leenen LP. Regional trauma system reduces mortality and changes admission rates: a before and after study. Ann Surg. 2010;251(2):339-343. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. . A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366-378. [DOI] [PubMed] [Google Scholar]
- 3.Celso B, Tepas J, Langland-Orban B, et al. . A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60(2):371-378. [DOI] [PubMed] [Google Scholar]
- 4.Newgard CD, Zive D, Holmes JF, et al. ; WESTRN investigators . A multisite assessment of the American College of Surgeons Committee on Trauma field triage decision scheme for identifying seriously injured children and adults. J Am Coll Surg. 2011;213(6):709-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sampalis JS, Denis R, Lavoie A, et al. . Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46(4):565-579. [DOI] [PubMed] [Google Scholar]
- 6.Sampalis JS, Denis R, Fréchette P, Brown R, Fleiszer D, Mulder D. Direct transport to tertiary trauma centers versus transfer from lower level facilities: impact on mortality and morbidity among patients with major trauma. J Trauma. 1997;43(2):288-295. [DOI] [PubMed] [Google Scholar]
- 7.Landelijk protocol ambulancezorg/LPA 7.2. https://www.ambulancezorg.nl/download/downloads/912/20110707-landelijk-protocol-ambulancezorg-versie-7-2.pdf. Accessed September 25, 2017.
- 8.Resources for optimal care of the injured patient 2014/resources repository. American College of Surgeons. https://www.facs.org/quality-programs/trauma/vrc/resources. Accessed September 25, 2017.
- 9.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehosp Emerg Care. 2006;10(3):287-294. [DOI] [PubMed] [Google Scholar]
- 10.van Laarhoven JJ, Lansink KW, van Heijl M, Lichtveld RA, Leenen LP. Accuracy of the field triage protocol in selecting severely injured patients after high energy trauma. Injury. 2014;45(5):869-873. [DOI] [PubMed] [Google Scholar]
- 11.Rating the severity of tissue damage: I: the abbreviated scale. JAMA. 1971;215(2):277-280. [DOI] [PubMed] [Google Scholar]
- 12.Champion HR, Copes WS, Sacco WJ, et al. . The Major Trauma Outcome Study: establishing national norms for trauma care. J Trauma. 1990;30(11):1356-1365. [PubMed] [Google Scholar]
- 13.Baker SP, O’Neill B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187-196. [PubMed] [Google Scholar]
- 14.Newgard CD, Haukoos JS. Advanced statistics: missing data in clinical research: part 2: multiple imputation. Acad Emerg Med. 2007;14(7):669-678. [DOI] [PubMed] [Google Scholar]
- 15.Committee on Trauma of the American College of Surgeons Hospital and prehospital resources for optimal care of the injured patient. Bull Am Coll Surg. 1986;71(10):4-23. [PubMed] [Google Scholar]
- 16.Mans S, Reinders Folmer E, de Jongh MA, Lansink KW. Direct transport vs inter hospital transfer of severely injured trauma patients. Injury. 2016;47(1):26-31. [DOI] [PubMed] [Google Scholar]
- 17.Newgard CD, Fu R, Zive D, et al. . Prospective validation of the national field triage guidelines for identifying seriously injured persons. J Am Coll Surg. 2016;222(2):146-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newgard CD, Richardson D, Holmes JF, et al. ; Western Emergency Services Translational Research Network (WESTRN) Investigators . Physiologic field triage criteria for identifying seriously injured older adults. Prehosp Emerg Care. 2014;18(4):461-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sasser SM, Hunt RC, Faul M, et al. ; Centers for Disease Control and Prevention (CDC) . Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1-20. [PubMed] [Google Scholar]
- 20.Nakahara S, Matsuoka T, Ueno M, et al. . Predictive factors for undertriage among severe blunt trauma patients: what enables them to slip through an established trauma triage protocol? J Trauma. 2010;68(5):1044-1051. [DOI] [PubMed] [Google Scholar]
- 21.Xiang H, Wheeler KK, Groner JI, Shi J, Haley KJ. Undertriage of major trauma patients in the US emergency departments. Am J Emerg Med. 2014;32(9):997-1004. [DOI] [PubMed] [Google Scholar]
- 22.Newgard CD, Staudenmayer K, Hsia RY, et al. . The cost of overtriage: more than one-third of low-risk injured patients were taken to major trauma centers. Health Aff (Millwood). 2013;32(9):1591-1599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacKenzie EJ, Weir S, Rivara FP, et al. . The value of trauma center care. J Trauma. 2010;69(1):1-10. [DOI] [PubMed] [Google Scholar]
- 24.Brown JB, Stassen NA, Bankey PE, Sangosanya AT, Cheng JD, Gestring ML. Mechanism of injury and special consideration criteria still matter: an evaluation of the National Trauma Triage Protocol. J Trauma. 2011;70(1):38-44. [DOI] [PubMed] [Google Scholar]
- 25.Lavoie A, Emond M, Moore L, Camden S, Liberman M. Evaluation of the Prehospital Index, presence of high-velocity impact and judgment of emergency medical technicians as criteria for trauma triage. CJEM. 2010;12(2):111-118. [DOI] [PubMed] [Google Scholar]
- 26.Newgard CD, Kampp M, Nelson M, et al. . Deciphering the use and predictive value of “EMS provider judgment” in out-of-hospital trauma triage: a multi-site, mixed methods assessment. J Trauma Acute Care Surg. 2012;72(5):1239-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pape HC, Lefering R, Butcher N, et al. . The definition of polytrauma revisited: an international consensus process and proposal of the new ‘Berlin definition’. J Trauma Acute Care Surg. 2014;77(5):780-786. [DOI] [PubMed] [Google Scholar]
- 28.Wong TH, Lumsdaine W, Hardy BM, Lee K, Balogh ZJ. The impact of specialist trauma service on major trauma mortality. J Trauma Acute Care Surg. 2013;74(3):780-784. [DOI] [PubMed] [Google Scholar]