Key Points
Question
What is the association of long-term solid fuel use for cooking and heating with risk of cardiovascular and all-cause mortality in China, and the relevance of switching from solid to clean fuels and use of ventilation to this association?
Findings
In this prospective cohort study of 271 217 adults, self-reported solid fuel use was associated with significantly higher risks of cardiovascular mortality (hazard ratio, 1.20 for cooking; 1.29 for heating) and all-cause mortality (hazard ratio, 1.11 for cooking; 1.14 for heating). Lower risks were observed among solid fuel users who reported having switched to clean fuels before the study baseline or using ventilation.
Meaning
Solid fuel use was significantly associated with increased risks of cardiovascular and all-cause mortality; these risks may be lower among those switching from solid to clean fuels or using ventilation.
Abstract
Importance
When combusted indoors, solid fuels generate a large amount of pollutants such as fine particulate matter.
Objective
To assess the associations of solid fuel use for cooking and heating with cardiovascular and all-cause mortality.
Design, Setting, and Participants
This nationwide prospective cohort study recruited participants from 5 rural areas across China between June 2004 and July 2008; mortality follow-up was until January 1, 2014. A total of 271 217 adults without a self-reported history of physician-diagnosed cardiovascular disease at baseline were included, with a random subset (n = 10 892) participating in a resurvey after a mean interval of 2.7 years.
Exposures
Self-reported primary cooking and heating fuels (solid: coal, wood, or charcoal; clean: gas, electricity, or central heating), switching of fuel type before baseline, and use of ventilated cookstoves.
Main Outcomes and Measures
Death from cardiovascular and all causes, collected through established death registries.
Results
Among the 271 217 participants, the mean (SD) age was 51.0 (10.2) years, and 59% (n = 158 914) were women. A total of 66% (n = 179 952) of the participants reported regular cooking (at least weekly) and 60% (n = 163 882) reported winter heating, of whom 84% (n = 150 992) and 90% (n = 147 272) used solid fuels, respectively. There were 15 468 deaths, including 5519 from cardiovascular causes, documented during a mean (SD) of 7.2 (1.4) years of follow-up. Use of solid fuels for cooking was associated with greater risk of cardiovascular mortality (absolute rate difference [ARD] per 100 000 person-years, 135 [95% CI, 77-193]; hazard ratio [HR], 1.20 [95% CI, 1.02-1.41]) and all-cause mortality (ARD, 338 [95% CI, 249-427]; HR, 1.11 [95% CI, 1.03-1.20]). Use of solid fuels for heating was also associated with greater risk of cardiovascular mortality (ARD, 175 [95% CI, 118-231]; HR, 1.29 [95% CI, 1.06-1.55]) and all-cause mortality (ARD, 392 [95% CI, 297-487]; HR, 1.14 [95% CI, 1.03-1.26]). Compared with persistent solid fuel users, participants who reported having previously switched from solid to clean fuels for cooking had a lower risk of cardiovascular mortality (ARD, 138 [95% CI, 71-205]; HR, 0.83 [95% CI, 0.69-0.99]) and all-cause mortality (ARD, 407 [95% CI, 317-497]; HR, 0.87 [95% CI, 0.79-0.95]), while for heating, the ARDs were 193 (95% CI, 128-258) and 492 (95% CI, 383-601), and the HRs were 0.57 (95% CI, 0.42-0.77) and 0.67 (95% CI, 0.57-0.79), respectively. Among solid fuel users, use of ventilated cookstoves was also associated with lower risk of cardiovascular mortality (ARD, 33 [95% CI, −9 to 75]; HR, 0.89 [95% CI, 0.80-0.99]) and all-cause mortality (ARD, 87 [95% CI, 20-153]; HR, 0.91 [95% CI, 0.85-0.96]).
Conclusions and Relevance
In rural China, solid fuel use for cooking and heating was associated with higher risks of cardiovascular and all-cause mortality. These risks may be lower among those who had previously switched to clean fuels and those who used ventilation.
This cohort study conducted in 5 rural areas across China examines associations between solid fuel use for cooking and heating and cardiovascular and all-cause mortality.
Introduction
Worldwide, it has been estimated that more than 2.7 billion individuals were using solid fuels for domestic purposes in 2015, mostly in low- and middle-income countries including China, where an estimated 450 million people still heavily rely on solid fuels, which include biomass (eg, wood, charcoal, and dung) and coal. When combusted indoors, solid fuels generate a large amount of pollutants such as fine particulate matter (PM2.5).
Using interpolation from risk estimates of PM2.5 for cardiovascular death, the recent report from the Global Burden of Disease Study estimated that household air pollution from solid fuel use accounted for about 2.5 million deaths in 2016. However, reliable epidemiological evidence remains scarce, especially on the association between solid fuel use and cardiovascular mortality. Most of the previous studies were cross-sectional or case-control in design, and to date, only 2 prospective studies, each with moderate size and involving a single geographical location, have examined the associations of solid fuel use with cardiovascular and all-cause mortality, with inconsistent findings. Moreover, to our knowledge, few studies have examined solid fuel use for cooking and heating separately, which are different in exposure patterns. Furthermore, it remains unclear whether mortality risk associated with solid fuel use, if any, is lower among adults who had switched from solid to clean fuel use or used appropriate ventilation (eg, ventilated cookstoves). This nationwide prospective cohort study examined the association of solid fuel use with risk of cardiovascular and all-cause mortality in rural China.
Methods
Study Design
The China Kadoorie Biobank was approved by the ethics committees of the University of Oxford (Oxford, United Kingdom), the Chinese Center for Disease Control and Prevention, and the Chinese Academy of Medical Sciences. All participants provided written informed consent.
Details of the study design, methods, and participant characteristics have been previously reported. Briefly, between June 2004 and July 2008, 512 891 participants aged 30 to 79 years were recruited from 10 areas of China (5 rural and 5 urban, defined according to governmental administrative structure), and the study areas were selected from China’s nationally representative Disease Surveillance Point system. Overall, 1 801 167 registered residents aged 35 to 74 years and without known major disability in these study areas were invited, of whom 502 176 participated in the baseline survey (response rate, 33% in rural areas and 27% in urban areas), and another 10 715 people outside the targeted age range who came to the survey clinics were also included, making the actual baseline age range 30 to 79 years.
Trained health workers administered a standardized electronic questionnaire to collect information on sociodemographic characteristics (age, sex, education level, and household income), lifestyle behaviors (smoking, passive smoking, alcohol consumption, diet, and physical activity), household air pollution exposures (details described here), and personal medical history. The laptop-based questionnaire used stringent logic and error checks to minimize missing values and data errors. A range of physical measurements (height, weight, waist circumference, and blood pressure) were performed following standard procedures previously described, and onsite random blood glucose was tested using the SureStep Plus System (Johnson & Johnson). After completion of the baseline survey, about 4% (n = 19 788; 11 627 rural and 8161 urban) of the original participants were randomly selected for a resurvey, collecting the same information as baseline, from July to October 2008 after a mean interval of 2.7 years after baseline (response rate, 84% in rural areas and 75% in urban areas).
Assessment of Solid Fuel Exposure
Each participant was asked to provide detailed information about exposure to household air pollution related to cooking frequency, use of heating, and cookstove ventilation (chimney or extractor fan/hood) for up to their 3 most recent residences, and the duration (in years) lived in each residence (further details are available from the study website: http://www.ckbiobank.org). Participants who reported cooking at least monthly and those who used heating in winter were asked additional questions about the primary fuel type used, which included gas, electricity, coal, wood/charcoal, and other unspecified fuels, plus “central heating” (a system generating heat in a centralized location distant from residential areas and distributing the heat to individual households via underground hot water or steam pipes). If more than 1 fuel type was used at any residence, only the 1 used most frequently was recorded.
Wood and charcoal were collectively addressed as “wood” in this study because of their common wood-based origin and emission similarities. Coal and wood were considered “solid fuels,” while gas and electricity were considered “clean fuels” because they tended to generate much less air pollution than solid fuels, along with central heating. Questions about the availability of ventilation facilities were only asked in relation to cookstoves because heating was generally conducted with minimal ventilation to retain warmth.
Participants who cooked less than monthly were considered as noncooking, and those who cooked weekly or more were further classified into 2 groups according to the primary cooking fuel (ie, solid fuels or clean fuels) used in the baseline residence. Similarly, those who used heating were divided into 2 groups according to the primary heating fuel used. To approximate long-term exposure, the duration of continuous exposure to solid fuel for cooking or heating was calculated separately by aggregating the duration lived in consecutive residences during which solid fuels were primarily used.
For sensitivity analysis, a weighted duration of exposure was also calculated by multiplying a weight coefficient with reported duration of solid fuel use, according to cooking frequency or the proportion of heating months per year in each study area, where appropriate. For cooking, the weight coefficients were 0.5 for weekly and 1.0 for daily. For heating, the weight coefficients were 0.19 for Sichuan, 0.42 for Gansu, 0.27 for Henan, and 0.18 for Hunan, calculated by aggregating the number of months during which the average temperature was less than 8°C in each area from 1999 to 2013, then dividing the aggregate number by 180 months (the total number of months during these 15 years). Using information of fuel use in the 3 most recent consecutive residences collected at baseline, this study also examined self-reported switching from solid to clean fuel use, which involved participants who were using clean fuel in the baseline residence but having used solid fuel in 1 or more earlier residence(s). A more detailed description of the exposure assessment is provided in the eAppendix in the Supplement.
Follow-up and Outcome Measures
Information on cardiovascular and all-cause mortality was collected regularly from baseline until January 1, 2014, through linkages, via a unique national identification number, with China’s Disease Surveillance Point system, supplemented by health insurance database and annual active validation of survival using local residential and administrative records. Causes of death were classified by trained staff blinded to baseline information following the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision.
For the small number of deaths (<5%) that occurred without medical attention prior to death, standardized verbal autopsy was conducted by trained health care workers to determine the probable causes of death from symptoms or signs described by family members or caregivers. The main outcomes in analyses of this study were death from cardiovascular disease (I00-I25, I27-I88, and I95-I99), its main components including ischemic heart disease death (I20-I25), stroke death (I60-I61 and I63-I64), other cardiovascular death, and all-cause mortality.
Statistical Analysis
This study included participants from 5 rural areas (n = 286 705; eFigure 1 in the Supplement) among whom solid fuels were commonly used. Participants aged younger than 35 years (n = 5891) were excluded because no deaths were documented in the reference group (clean fuel users) of this age group. Participants with self-reported physician-diagnosed coronary heart disease, stroke, or transient ischemic attack (n = 8578), and those who reported unreliable recall information (ie, the total number of years of residence in their 3 most recent residences was greater than their baseline age, n = 2132) were also excluded. After these exclusions (1113 participants met multiple exclusion criteria), 271 217 participants remained, and among them, 10 892 participated in the resurvey.
Baseline characteristics of the study population are described as means with SDs or percentages by categories of cooking and heating exposure, with adjustment for age, sex, and study areas where appropriate. The reproducibility of cooking and heating exposure was assessed using a weighted κ statistic in the subsample with complete exposure information at baseline and resurvey. The mortality rate per 100 000 person-years was adjusted for age, sex, and study areas, and the absolute rate difference (ARD) was calculated as the adjusted mortality rate of the exposed group minus that of the reference group. Cox proportional hazards regression models were used to calculate hazard ratios (HRs) and 95% CIs for cardiovascular (overall and subtypes) and all-cause mortality in relation to solid fuel use as compared with clean fuel use, for cooking and for heating separately. All Cox regression models were stratified by age at risk (in 5-year intervals), sex, and study areas (5 groups for cooking-related analyses; 4 groups for heating-related analyses). Further adjustment for established risk factors included smoking status; passive smoking; alcohol consumption; body mass index (continuous); physical activity level (metabolic equivalent of tasks hours/day; continuous); variables related to socioeconomic status, including education, household income, and diet (consumption of preserved vegetables, fresh fruit, meat, fish, dairy, rice, poultry, and eggs); and cookstove ventilation (yes and no). In addition, cooking and heating exposures were mutually adjusted for in the final models. All analyses were performed with reported fuel use at baseline.
The associations of long-term fuel use with cardiovascular and all-cause mortality risk were assessed by comparing participants who reported fewer than 20 years, 20 to 39 years, and 40 or more years of solid fuel use (cutoffs rounded from the tertiles of 21 and 39 years for cooking), with those always using clean fuels, separately for cooking and heating. Analyses were repeated using weighted duration of reported solid fuel use, with weights assigned as previously described. Mortality risk was also compared between participants who reported having previously switched from solid to clean fuels and persistent solid fuel users, and between those who reported solid fuel use with ventilation and those without.
The additive interactions of solid fuel use with cigarette smoking (ever/never) were examined by calculating the HRs in association with combined exposure (ever smoking plus solid fuel use, as compared with never smoking plus clean fuel use [reference group]). The significance of additive interaction was indicated by a value of the relative excess risk due to interaction greater than zero. The combined exposure to solid fuel use for cooking and heating was examined similarly among the subgroup of participants who reported both regularly cooking and heating (n = 107 600, 40% of the study population).
Several sensitivity analyses were conducted to test the robustness of the results: (1) further adjusting for potential confounders including survey season, occupation, self-reported health status, and family history of cardiovascular disease; (2) excluding participants taking antihypertensive treatment; (3) excluding participants using clean fuels for less than 10 years who might have more recent previous exposure to solid fuels; and (4) excluding events occurring during the first 2 years of follow-up to scrutinize the possibility of reverse causation.
Comparison between adjusted HRs for the first 4 years and for the subsequent years of follow-up revealed no evidence of departure from the proportional hazards assumption for all analyses. For all analyses with 3 or more exposure categories, the floating absolute risk method was used to estimate group-specific 95% CIs, which enabled the comparisons across different exposure categories. Detailed information about the statistical analyses is provided in the eAppendix in the Supplement. Two-sided P values were used and P < .05 denoted statistical significance. All analyses were performed using SAS version 9.3 (SAS Institute Inc), and graphs were plotted using R version 3.4.2 (R Foundation).
Results
Characteristics of Study Participants
Of the 271 217 participants, the mean (SD) age was 51.0 (10.2) years and 59% were women. Overall, 66% and 60% of the participants reported regular cooking and winter heating, respectively, of whom 84% and 90% reported solid fuel use at baseline (Table 1). In general, solid fuel users for cooking and for heating were both older, more likely to be women, and had lower education level and household income compared with clean fuel users. Smoking was less prevalent among those reported to cook with solid fuels but similar across all heating categories (Table 1). Across the 5 rural areas, the proportion of participants using solid fuels varied from 36% (Zhejiang) to 64% (Hunan) for cooking, and 0% (Zhejiang) to 95% (Gansu) for heating (eTable 1 in the Supplement). No major differences were found between the participants in the baseline survey and those in the resurvey (eTable 2 in the Supplement). In the resurvey, 78.4% and 84.1% of the participants reported the same category of exposure from cooking and heating, respectively, as at baseline. The weighted κ value was 0.62 for cooking and 0.64 for heating (eTable 3 in the Supplement).
Table 1. Baseline Characteristics of the Study Participants According to Cooking and Heating Fuel Types and Behavior in Baseline Residencea.
| Characteristic | Cooking, %b | Heating, %c | All Participants, %d | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Clean Fuels | Coal | Wood | Not Cooking Regularly | Clean Fuels | Coal | Wood | No Heating | ||
| No. | 26 559 | 89 066 | 61 926 | 91 265 | 14 817 | 84 942 | 62 330 | 50 522 | 271 217 |
| Age, mean (SD), y | 48.2 (9.6) |
51.7 (9.9) |
55.2 (10.3) |
50.8 (10.5) |
48.1 (10.2) |
50.5 (10.1) |
51.8 (10.6) |
50.8 (10.3) |
51.0 (10.2) |
| Women | 72.6 | 81.6 | 81.7 | 10.9 | 56.1 | 58.9 | 60.5 | 56.9 | 58.6 |
| Socioeconomic factors | |||||||||
| Attained high school or higher | 20.7 | 9.3 | 4.7 | 12.0 | 26.2 | 10.5 | 8.8 | 9.0 | 9.2 |
| Household income ≥20 000 yuan/ye | 46.0 | 31.8 | 23.3 | 37.4 | 41.7 | 21.8 | 23.4 | 16.2 | 32.0 |
| Lifestyle factors | |||||||||
| Current smoker | |||||||||
| Men | 67.9 | 73.5 | 70.3 | 72.9 | 67.7 | 73.1 | 72.4 | 66.9 | 72.2 |
| Women | 3.1 | 3.3 | 3.7 | 3.7 | 4.3 | 4.4 | 4.3 | 3.9 | 3.7 |
| Current drinker | |||||||||
| Men | 35.9 | 32.0 | 27.4 | 29.9 | 34.1 | 28.1 | 26.1 | 25.0 | 30.1 |
| Women | 2.5 | 1.8 | 2.3 | 2.7 | 2.6 | 2.0 | 2.5 | 2.4 | 2.7 |
| Food consumption ≥4 d/wk | |||||||||
| Fresh fruit | 25.1 | 15.3 | 8.3 | 17.1 | 26.1 | 11.4 | 11.2 | 19.9 | 13.2 |
| Meat | 81.3 | 75.2 | 63.6 | 76.0 | 83.3 | 70.0 | 69.3 | 64.5 | 26.0 |
| Poultry | 22.6 | 15.5 | 9.5 | 16.5 | 17.5 | 5.7 | 4.5 | 6.0 | 86.5 |
| Fish | 33.3 | 26.3 | 19.9 | 26.4 | 29.9 | 19.2 | 16.3 | 20.1 | 75.9 |
| Preserved vegetables | 45.5 | 45.0 | 49.5 | 46.6 | 42.2 | 45.7 | 44.9 | 43.9 | 52.4 |
| Dairy | 18.0 | 7.2 | 2.9 | 9.1 | 23.8 | 6.8 | 7.2 | 7.7 | 93.9 |
| Egg | 73.7 | 67.6 | 61.0 | 64.9 | 73.7 | 66.1 | 64.7 | 64.8 | 34.5 |
| Rice | 87.0 | 82.7 | 76.0 | 81.2 | 86.6 | 75.8 | 77.3 | 76.6 | 19.5 |
| Physical activity, mean (SD) MET-h/d | 21.4 (14.7) |
23.6 (12.4) |
24.0 (13.0) |
22.8 (16.2) |
19.1 (11.5) |
21.5 (14.6) |
22.4 (13.1) |
22.4 (12.7) |
23.4 (14.4) |
| Physical measurements, mean (SD) | |||||||||
| BMI | 23.7 (3.2) |
23.4 (3.4) |
22.7 (3.3) |
23.2 (3.1) |
23.8 (3.2) |
23.3 (3.4) |
23.0 (3.1) |
23.2 (3.3) |
23.2 (3.3) |
| Systolic blood pressure, mm Hg | 130.9 (20.4) |
132.8 (21.4) |
132.2 (22.5) |
131.9 (20.1) |
130.2 (18.5) |
131.1 (21.4) |
130.7 (21.9) |
131.8 (19.7) |
132.4 (21.2) |
| Self-reported conditions at baseline | |||||||||
| Hypertension | 11.3 | 10.1 | 7.5 | 9.4 | 10.2 | 7.7 | 7.5 | 7.6 | 8.9 |
| Respiratory disease | 13.3 | 14.4 | 13.1 | 14.5 | 16.3 | 15.7 | 15.6 | 16.7 | 13.4 |
| Diabetes | 5.5 | 5.8 | 3.3 | 5.1 | 6.2 | 3.8 | 4.3 | 4.5 | 4.0 |
| Poor health | 8.8 | 11.4 | 13.2 | 12.5 | 11.9 | 13.9 | 14.5 | 15.7 | 10.6 |
| Other exposures | |||||||||
| Passive smoking >5 d/wk | 47.8 | 47.8 | 43.4 | 46.6 | 53.8 | 55.8 | 55.8 | 48.0 | 46.4 |
| At least some cookstove ventilation | 72.2 | 63.1 | 68.5 | 67.4 | 66.6 | ||||
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); MET, metabolic equivalent of tasks.
Data were adjusted for age, sex, and study areas for all factors except age, sex, smoking, and drinking. Data for age were adjusted for sex and study areas, and that for sex, smoking, and drinking were adjusted for age and study areas. Empty cells represent no information on cookstove ventilation for heating. Clean fuels included electricity, gas, or central heating (for heating only); wood included wood and charcoal.
Not cooking regularly denotes cooking monthly or less. Participants with unspecified fuel type (n = 2401) were excluded from the analysis.
Participants from Zhejiang were excluded (n = 56 813) because only 0.6% of residents in Zhejiang reported heating at baseline. Participants with unspecified fuel use (n = 1793) were also excluded.
Participants included in the data reported in the last column were those after exclusions of those aged younger than 35 years (n = 5891); those who self-reported physician-diagnosed coronary heart disease, stroke, or transient ischemic attack (n = 8578); and those who reported unreliable recall information (n = 2132), and not excluding those with unspecified fuel use and noncooking or nonheating participants.
At the exchange rate as of January 2018, 100 yuan is approximately equal to US $15.
Association of Solid Fuel Use With Cardiovascular and All-Cause Mortality
During a mean (SD) of 7.2 (1.4) years of follow-up, 15 468 death events were documented among the 271 217 participants, including 5519 cardiovascular deaths (ischemic heart disease deaths: 1687; stroke deaths: 3027; and other cardiovascular deaths: 805). Compared with reported clean fuel use for cooking, reported solid fuel use was significantly associated with higher risk of cardiovascular mortality (ARD, 135 [95% CI, 77-193]; HR, 1.20 [95% CI, 1.02-1.41]) and all-cause mortality (ARD, 338 [95% CI, 249-427]; HR, 1.11 [95% CI, 1.03-1.20]). For heating, reported solid fuel use was also associated with higher risk for cardiovascular mortality (ARD, 175 [95% CI, 118-231]; HR, 1.29 [95% CI, 1.06-1.55]) and all-cause mortality (ARD, 392 [95% CI, 297-487]; HR, 1.14 [95% CI, 1.03-1.26]; Table 2). Higher risks were also observed in association with reported coal use and wood use, when these fuel types were examined separately, except that statistical significance was not achieved for reported coal use (eFigure 2 in the Supplement). These associations were also consistent across study areas (P > .05 for heterogeneity; eFigure 3 in the Supplement). Moreover, the associations were similar for different subtypes of cardiovascular mortality (Table 2).
Table 2. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality by Baseline Cooking and Heating Fuel Typesa.
| Mortality | Cooking | Heating | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Deaths | Mortality Rate per 100 000 Person-Yearsb | Absolute Rate Difference per 100 000 Person-Years (95% CI)b |
Basic Adjustment, Hazard Ratio (95% CI)c |
Adjusted for Major Confounders, Hazard Ratio (95% CI)d |
Further Adjusted for Heating, Hazard Ratio (95% CI) |
No. of Deaths | Mortality Rate per 100 000 Person-Yearsb | Absolute Rate Difference per 100 000 Person-Years (95% CI)b |
Basic Adjustment, Hazard Ratio (95% CI)c |
Adjusted for Major Confounders, Hazard Ratio (95% CI)d |
Further Adjusted for Cooking, Hazard Ratio (95% CI) |
|
| Cardiovascular | ||||||||||||
| Clean fuels | 180 | 184 | 135 (77 to 193) |
[Reference] | [Reference] | [Reference] | 148 | 172 | 175 (118 to 231) |
[Reference] | [Reference] | [Reference] |
| Solid fuels | 2957 | 319 | 1.39 (1.19 to 1.63) |
1.23 (1.05 to 1.45) |
1.20 (1.02 to 1.41) |
3809 | 347 | 1.54 (1.29 to 1.85) |
1.29 (1.07 to 1.55) |
1.29 (1.06 to 1.55) |
||
| Ischemic Heart Disease | ||||||||||||
| Clean fuels | 42 | 62 | 34 (−4 to 72) |
[Reference] | [Reference] | [Reference] | 45 | 56 | 53 (25 to 81) |
[Reference] | [Reference] | [Reference] |
| Solid fuels | 899 | 96 | 1.28 (0.93 to 1.77) |
1.15 (0.83 to 1.59) |
1.12 (0.81 to 1.56) |
1280 | 109 | 1.37 (0.99 to 1.89) |
1.17 (0.84 to 1.63) |
1.13 (0.82 to 1.59) |
||
| Stroke | ||||||||||||
| Clean fuels | 107 | 91 | 85 (54 to 116) |
[Reference] | [Reference] | [Reference] | 78 | 75 | 112 (79 to 146) |
[Reference] | [Reference] | [Reference] |
| Solid fuels | 1612 | 176 | 1.39 (1.13 to 1.70) |
1.21 (0.98 to 1.48) |
1.16 (0.94 to 1.44) |
2049 | 187 | 1.74 (1.36 to 2.24) |
1.43 (1.11 to 1.86) |
1.45 (1.12 to 1.88) |
||
| Other Cardiovascular | ||||||||||||
| Clean fuels | 31 | 31 | 17 (−13 to 47) |
[Reference] | [Reference] | [Reference] | 25 | 41 | 10 (−25 to 45) |
[Reference] | [Reference] | [Reference] |
| Solid fuels | 446 | 48 | 1.59 (1.08 to 2.33) |
1.45 (0.98 to 2.14) |
1.42 (0.98 to 2.13) |
480 | 51 | 1.04 (0.71 to 1.53) |
1.01 (0.64 to 1.60) |
1.00 (0.63 to 1.59) |
||
| All-Cause | ||||||||||||
| Clean fuels | 855 | 563 | 338 (249 to 427) |
[Reference] | [Reference] | [Reference] | 628 | 540 | 392 (297 to 487) |
[Reference] | [Reference] | [Reference] |
| Solid fuels | 7955 | 901 | 1.26 (1.17 to 1.36) |
1.12 (1.04 to 1.21) |
1.11 (1.03 to 1.20) |
8780 | 932 | 1.32 (1.20 to 1.46) |
1.15 (1.04 to 1.26) |
1.14 (1.03 to 1.26) |
||
Clean fuels refer to electricity, gas, or central heating (for heating only); solid fuels refer to coal, wood, or charcoal. In the analyses of fuel use for cooking, we further excluded 2401 participants who reported unspecified fuel use and 91 265 noncooking participants, leaving 177 551 participants for the analysis (n = 26 559 [195 392 person-years] for clean fuels; n = 150 992 [1 097 985 person-years] for solid fuels). In the analyses of fuel use for heating, we excluded participants from Zhejiang (n = 56 813) where heating was rarely reported (0.6%), those who reported nonheating (n = 50 522), and those who reported unspecified fuel use (n = 1793), leaving 162 089 participants for the analysis (n = 14 817 [103 860 person-years] for clean fuels; n = 147 272 [1 060 159 person-years] for solid fuels).
The mortality rate per 100 000 person-years was adjusted for age, sex, and study areas, and the rate difference was calculated as the adjusted mortality rate of the exposed group minus that of the reference group. Among the 271 217 participants, 15 468 death events were documented, including 5519 cardiovascular deaths (ischemic heart disease deaths: 1687; stroke deaths: 3027; and other cardiovascular deaths: 805).
Basic adjustment refers to hazard ratios stratified for age at risk, sex, and study areas.
Hazard ratios were stratified according to age at risk, sex, and study areas, and they were adjusted for education level, income, alcohol consumption, smoking status, passive smoking, physical activity, body mass index, diet (consumption of fresh fruit, preserved vegetables, meat, fish, diary, rice, poultry, and eggs), and cookstove ventilation.
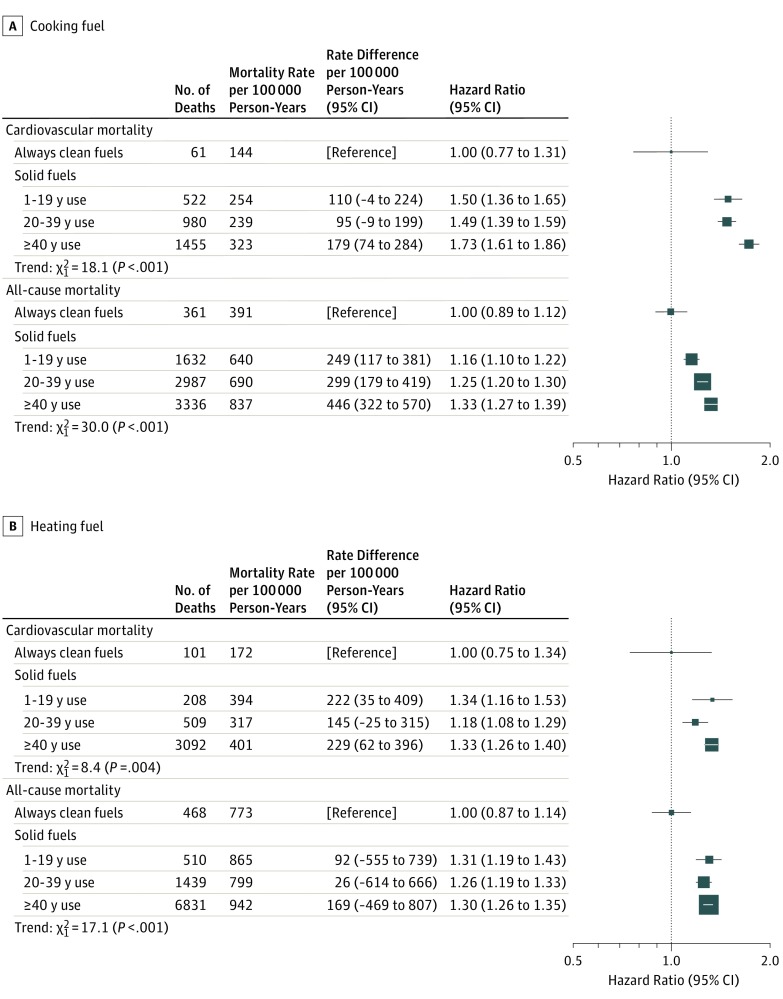
Participants with longer self-reported duration of solid fuel use had higher risks of cardiovascular and all-cause mortality (P < .001 for trend; Figure 1). For cooking, the ARDs for cardiovascular mortality were 110 (95% CI, −4 to 224), 95 (95% CI, −9 to 199), and 179 (95% CI, 74-284) among those who reported fewer than 20, 20 to 39, and 40 or more years of solid fuel use compared with those always using clean fuels, and the adjusted HRs were 1.50 (95% CI, 1.36-1.65), 1.49 (95% CI, 1.39-1.59), and 1.73 (95% CI, 1.61-1.86), respectively. The ARDs for all-cause mortality were 249 (95% CI, 117-381), 299 (95% CI, 179-419), and 446 (95% CI, 322-570), and the corresponding HRs were 1.16 (95% CI, 1.10-1.22), 1.25 (95% CI, 1.20-1.30), and 1.33 (95% CI, 1.27-1.39). For heating, the HRs were 1.34 (95% CI, 1.16-1.53), 1.18 (95% CI, 1.08-1.29), and 1.33 (95% CI, 1.26-1.40) for cardiovascular mortality, with ARDs of 222 (95% CI, 35-409), 145 (95% CI, −25 to 315), and 229 (95% CI, 62-396). The ARDs for all-cause mortality were 92 (95% CI, −555 to 739), 26 (95% CI, −614 to 666), and 169 (95% CI, −469 to 807), and the HRs were 1.31 (95% CI, 1.19-1.43), 1.26 (95% CI, 1.19-1.33), and 1.30 (95% CI, 1.26-1.35), respectively (Figure 1). When using weighted duration of self-reported solid fuel use, higher risks were also observed in association with longer duration of such use (eFigure 4 in the Supplement).
Figure 1. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Long-term Solid Fuel Use for Cooking and Heating.
For cooking-related analysis, participants who switched from solid to clean fuels at baseline (n = 15 475) were excluded, leaving 162 076 for the analysis. The numbers of participants (and person-years) included in the 4 categories (from always clean to always solid [≥40 years]) were 11 084 (82 206), 41 171 (304 674), 76 072 (553 267), and 33 749 (240 044), respectively. For heating-related analysis, participants who switched from solid to clean fuels at baseline (n = 5757) were excluded, leaving 156 332 for the analysis. The numbers of participants (and person-years) included in the 4 categories (from always clean to always solid [≥40 years]) were 9060 (61 981), 8292 (59 486), 45 460 (333 602), and 93 520 (667 071), respectively. The mortality rate per 100 000 person-years was adjusted for age, sex, and study areas, and the rate difference was calculated as the adjusted mortality rate of the exposed group minus that of the reference group. Hazard ratios were stratified according to age at risk, sex, and study areas, and adjusted for education level, income, alcohol consumption, smoking status, passive smoking, physical activity, body mass index, diet (consumption of fresh fruit, preserved vegetables, meat, fish, dairy, rice, poultry, and eggs), cookstove ventilation, and cooking and heating exposures, where appropriate. The floating absolute risk method provides the variance of the logarithm of the hazard ratio for each category (including the reference category) to facilitate comparisons across the different exposure categories. The boxes represent hazard ratios, with the size inversely proportional to the variance of the logarithm of the hazard ratio, and the horizontal lines represent 95% CIs.
Compared with persistent solid fuel users, participants who reported having switched from solid to clean fuels for cooking before the baseline survey had significantly lower risks of cardiovascular mortality (ARD, 138 [95% CI, 71-205]; HR, 0.83 [95% CI, 0.69-0.99]) and all-cause mortality (ARD, 407 [95% CI, 317-497]; HR, 0.87 [95% CI, 0.79-0.95]), while for heating the ARDs were 193 (95% CI, 128-258) and 492 (95% CI, 383-601), and the HRs were 0.57 (95% CI, 0.42-0.77) and 0.67 (95% CI, 0.57-0.79), respectively (Table 3). Compared with solid fuel users who reported no ventilation for cooking, those with cookstove ventilation also had lower risks for cardiovascular mortality (ARD, 33 [95% CI, −9 to 75]; HR, 0.89 [95% CI, 0.80-0.99]) and all-cause mortality (ARD, 87 [95% CI, 20-153]; HR, 0.91 [95% CI, 0.85-0.96]; Table 3).
Table 3. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality in Association With Previous Switch From Solid to Clean Fuels and Use of Cookstove Ventilationa.
| Cooking | Heating | |||||||
|---|---|---|---|---|---|---|---|---|
| No. of Deaths | Mortality Rate per 100 000 Person-Yearsb | Absolute Rate Difference per 100 000 Person-Years (95% CI)b |
Hazard Ratio (95% CI)c |
No. of Deaths | Mortality Rate per 100 000 Person-Yearsb | Absolute Rate Difference per 100 000 Person-Years (95% CI)b |
Hazard Ratio (95% CI)c |
|
| Previous Switch From Solid to Clean Fuelsd | ||||||||
| Cardiovascular mortality | ||||||||
| Solid fuel use | 2957 | 319 | 138 (71 to 205) |
[Reference] | 3809 | 347 | 193 (128 to 258) |
[Reference] |
| Solid to clean fuel use | 119 | 181 | 0.83 (0.69 to 0.99) |
46 | 154 | 0.57 (0.42 to 0.77) |
||
| All-cause mortality | ||||||||
| Solid fuel use | 7955 | 901 | 407 (317 to 497) |
[Reference] | 8780 | 932 | 492 (383 to 601) |
[Reference] |
| Solid to clean fuel use | 492 | 494 | 0.87 (0.79 to 0.95) |
159 | 440 | 0.67 (0.57 to 0.79) |
||
| Use of Cookstove Ventilatione | ||||||||
| Cardiovascular mortality | ||||||||
| Solid fuel use without ventilation | 1235 | 291 | 33 (−9 to 75) |
[Reference] | ||||
| Solid fuel use with ventilation | 1722 | 258 | 0.89 (0.80 to 0.99) |
|||||
| All-cause mortality | ||||||||
| Solid fuel use without ventilation | 3136 | 797 | 87 (20 to 153) |
[Reference] | ||||
| Solid fuel use with ventilation | 4819 | 710 | 0.91 (0.85 to 0.96) |
|||||
Clean fuels refer to electricity, gas, or central heating (for heating only); solid fuels refer to coal, wood, or charcoal. Empty cells represent no information on cookstove ventilation for heating.
The mortality rate per 100 000 person-years was adjusted for age, sex, and study areas, and the rate difference was calculated as the adjusted mortality rate of the exposed group minus that of the reference group.
Hazard ratios were stratified according to age at risk, sex, and study areas, and adjusted for education level, income, alcohol consumption, smoking status, passive smoking, physical activity, body mass index, diet (consumption of fresh fruit, preserved vegetables, meat, fish, diary, rice, poultry, and eggs), cookstove ventilation, and cooking and heating exposures, where appropriate.
Participants who always used clean fuels for cooking (n = 11 084) and for heating (n = 9060) were excluded from the cooking- or heating-related analyses, respectively. Among participants who reported using clean fuels in the present residence, those who reported use of solid fuels and “other unspecified fuels,” respectively, in each of the 2 previous residences (n = 45 for cooking and n = 37 for heating) were also classified as “solid to clean.” After exclusion, 166 467 participants were included in the cooking-related analysis (n = 150 992 [1 097 985 person-years] for solid fuel use; n = 15 475 [113 186 person-years] for previous switch from solid to clean fuels), and 153 029 were included in the heating-related analysis (n = 147 272 [1 060 159 person-years] for always solid fuel use; n = 5757 [41 879 person-years] for previous switch from solid to clean fuels).
Participants who used clean fuels for cooking at baseline (n = 26 559) were excluded, leaving 150 992 participants who used solid fuels at baseline for the cooking analysis (n = 55 589 [410 422 person-years] without ventilation; n = 95 403 [687 563 person-years] with ventilation). Hazard ratios were modeled as per footnote c, except without adjustment for cooking ventilation and cooking exposure.
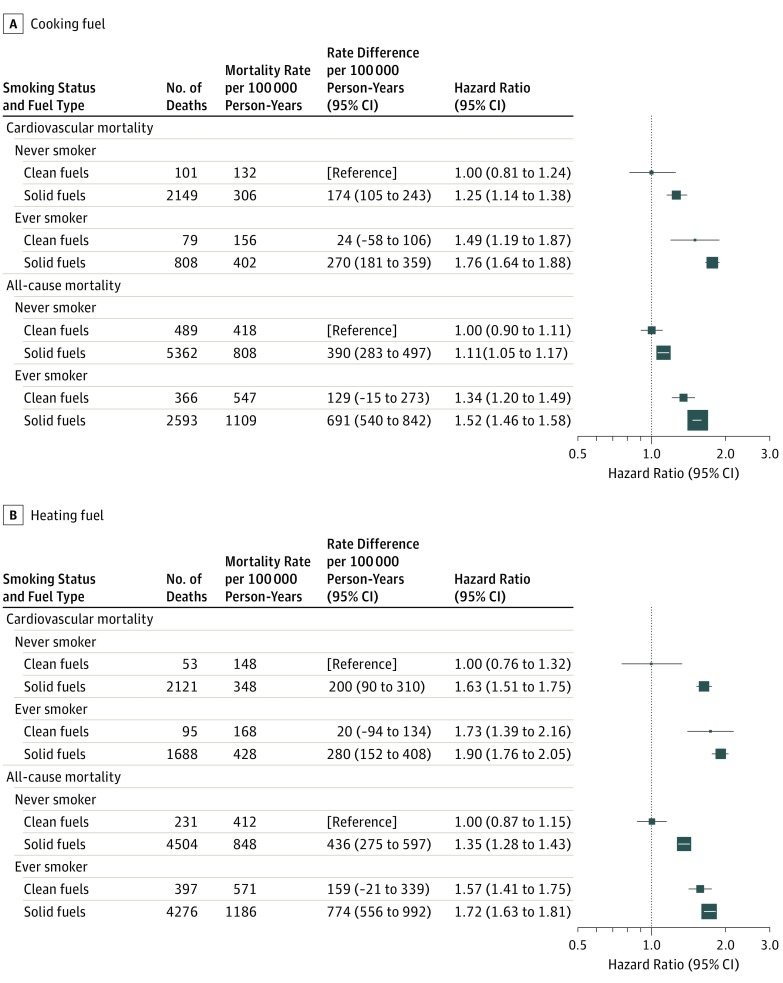
There were additive interactions of solid fuel use and smoking for both cardiovascular and all-cause mortality, with the risk highest among ever smokers who also used solid fuel for cooking for cardiovascular mortality (ARD, 270 [95% CI, 181-359]; HR, 1.76 [95% CI, 1.64-1.88]) and for all-cause mortality (ARD, 691 [95% CI, 540-842]; HR, 1.52 [95% CI, 1.46-1.58]) compared with never smokers using clean fuels (both P < .001 for additive interaction). For heating, the corresponding ARDs were 280 (95% CI, 152-408) and 774 (95% CI, 556-992), and the HRs were 1.90 (95% CI, 1.76-2.05) and 1.72 (95% CI, 1.63-1.81), respectively (P = .046 and .20 for additive interaction, respectively) (Figure 2). Similarly, the risks were higher among those who reported solid fuel use for both cooking and heating compared with those who reported using solid fuels for either (P < .01 for additive interaction; eFigure 5 in the Supplement).
Figure 2. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Fuel Used for Cooking and Heating in Never and Ever Smokers.
In the analyses of fuel use for cooking, this study further excluded 2401 participants who reported unspecified fuel use and 91 265 noncooking participants, leaving 177 551 participants for the analysis. The numbers of participants (and person-years) included in the 4 categories (never smoker, clean fuels; never smoker, solid fuels; ever smoker, clean fuels; and ever smoker, solid fuels) were 20 462 (151 563), 127 601 (931 784), 6097 (43 829), and 23 391 (166 201), respectively. The relative excess risk due to interaction was 0.05 (95% CI, 0.03-0.07) for cardiovascular mortality and 0.04 (95% CI, 0.02-0.05) for all-cause mortality. In the analyses of fuel use for heating, this study excluded participants from Zhejiang (n = 56 813) where heating was rarely reported (0.6%), those who reported nonheating (n = 50 522), and those who reported unspecified fuel use (n = 1793), leaving 162 089 participants for the analysis. The corresponding numbers of participants (and person-years) were 9412 (66 552), 98 640 (714 999), 5405 (37 308), and 48 632 (345 160), respectively. The mortality rate per 100 000 person-years was adjusted for age, sex, and study areas, and the rate difference was calculated as the adjusted mortality rate of the exposed group minus that of the reference group. The relative excess risk due to interaction was 0.03 (95% CI, 0.00-0.06) for cardiovascular mortality and −0.02 (95% CI, −0.05 to 0.01) for all-cause mortality. Hazard ratios were stratified according to age at risk, sex, and study areas, and adjusted for education level, income, alcohol consumption, smoking status, passive smoking, physical activity, body mass index, diet (consumption of fresh fruit, preserved vegetables, meat, fish, dairy, rice, poultry, and eggs), cookstove ventilation, and cooking and heating exposures. The floating absolute risk method provides the variance of the logarithm of the hazard ratio for each category (including the reference category) to facilitate comparisons across the different exposure categories. The boxes represent hazard ratios, with the size inversely proportional to the variance of the logarithm of the hazard ratio, and the horizontal lines represent 95% CIs.
In the sensitivity analyses of additional adjustment for survey season, occupation, self-rated health status, and family history of cardiovascular disease—and that of excluding those taking antihypertensive treatment, excluding those using clean fuels for less than 10 years, or excluding events occurring during the first 2 years of follow-up—higher risks were also observed for cardiovascular and all-cause mortality, although significance was not achieved when examining subtypes of cardiovascular death (eTables 4 and 5 in the Supplement).
Discussion
This large prospective cohort study found that in rural China, adults reporting the use of solid fuels for cooking and heating, particularly those who used for a longer duration, had higher risks of cardiovascular and all-cause mortality compared with clean fuel users. Among participants who reported having previously switched from solid to clean fuels before baseline, the risks were significantly lower compared with persistent solid fuel users for both cooking and heating. In addition, solid fuel users with ventilation for cookstoves also had lower mortality risks compared with those without.
To our knowledge, only 2 prospective studies to date have examined the associations of solid fuel use with mortality risk. One study in urban Shanghai, which included 74 941 women and documented 859 cardiovascular deaths, showed that ever use of coal for cooking was associated with excess cardiovascular mortality (HR, 1.18 [95% CI, 1.02-1.37]) and all-cause mortality (HR, 1.12 [95% CI, 1.05-1.21]). However, in another study of 50 045 Iranians among whom there were 1578 cardiovascular deaths, there was a significant higher risk associated with use of kerosene/diesel but not wood, which was used to a lesser scale in that population. With 5519 cardiovascular deaths documented, the current study found that solid fuel use for cooking and heating were both associated with higher risks of cardiovascular mortality, with similar excess risk for coal and wood use. In addition, there was a positive association between solid fuel use for heating and mortality risk, which has not been previously investigated independently.
This study found that longer duration of solid fuel use was associated with higher risk of cardiovascular and all-cause mortality, and these risks were lower in those who had switched from solid to clean fuels. The Shanghai Women’s Study had a similar finding that mortality risk was also higher among participants with longer duration of coal use, although with much smaller risk estimates, possibly owing to the fact that 99% of the participants had ceased coal use at baseline. In addition, this study found new evidence that the use of cookstove ventilation was associated with lower mortality risks. The cost of installing ventilation facilities is relatively lower compared with a complete switch to using clean fuels. Evidence from intervention studies also suggests that well-ventilated cookstoves could effectively lower an individual’s exposure from household air pollution and reduce levels of cardiovascular risk factors, although these trials were of short duration and did not measure morbidity or mortality end points. The findings of this study may have important public health significance because improving ventilation is often a more feasible alternative to clean fuel substitution and should be promoted in lower-income countries, which might reduce the disease risks associated with solid fuel use.
The exact mechanisms through which solid fuel use may contribute to mortality risk are not well understood. Burning of solid fuels releases substantially higher levels of various gaseous pollutants and PM2.5 than clean fuel, and it might increase cardiovascular disease and mortality risk through pathways such as cardiac autonomic dysfunction and atherothrombosis. These postulated mechanisms are supported by several cross-sectional studies in which exposure to household air pollution from solid fuel combustion was associated unfavorably with various cardiovascular risk factors. Furthermore, these impairments associated with solid fuel use is analogous to those related to cigarette smoking, which might explain the observations that combined exposure to solid fuel use and smoking was associated with a significantly higher mortality risk.
Apart from the large sample size, the main strengths of this study also include the prospective design and the inclusion of participants from 5 diverse rural areas, thereby permitting detailed examination of the association between solid fuel use and mortality risk in different settings. Moreover, to our knowledge, this study is the first to assess the mortality risk associated with cooking and heating separately, their additive interactions with smoking, switching from solid fuels to clean fuels, and use of appropriate ventilation.
Limitations
This study has several limitations. First, self-reported fuel use was used as a proxy for household air pollution exposure, which could vary by level and efficiency of ventilation, climate, and fuel properties. Direct measurement of household air pollution exposure (like PM2.5) was not feasible at baseline in this study, but future resurveys might include objective assessment in subsets of the participants to improve exposure assessment. Second, there was some disagreement of reported fuel use between baseline and resurvey, which was likely due to both random measurement error and actual changes over time. Nevertheless, the reproducibility was reasonably good based on the weighted κ values. Furthermore, random errors in reported fuel use could lead to underestimation of the associated risk due to regression dilution bias. Third, domestic fuel choice is closely related to socioeconomic status, which itself is associated with the risk of cardiovascular and all-cause mortality. Despite extensive adjustment for related variables (education level, household income, and various dietary variables) in this study, residual confounding remains likely.
Conclusions
In rural China, solid fuel use for cooking and heating was associated with higher risks of cardiovascular and all-cause mortality. These risks may be lower among those who had previously switched to clean fuels and those who used ventilation.
eAppendix. Supplementary Methods
eTable 1. Baseline Fuel Types According to Study Areas
eTable 2. Baseline Characteristics of Participants at Baseline Survey and Resurvey
eTable 3. Reproducibility of Reported Fuel Use for Cooking and for Heating Between Baseline and Resurvey
eTable 4. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Baseline Fuel Use for Cooking After Additional Adjustments or Further Exclusions
eTable 5. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Baseline Fuel Use for Heating After Additional Adjustments or Further Exclusions
eFigure 1. Locations of the 5 Rural Study Areas of the China Kadoorie Biobank Study in Mainland China
eFigure 2. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality by Baseline Cooking and Heating Fuel Types
eFigure 3. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality by Baseline Cooking and Heating Fuel Types, Stratified by Study Areas
eFigure 4. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Weighted Long-term Assessments of Fuel Use for Cooking and for Heating
eFigure 5. Association of Combined Solid Fuel Use for Cooking and for Heating With Cardiovascular and All-Cause Mortality
eReferences
References
- 1.International Energy Agency World Energy Outlook 2016. Paris, France: International Energy Agency; 2016. [Google Scholar]
- 2.Clark ML, Peel JL, Balakrishnan K, et al. Health and household air pollution from solid fuel use: the need for improved exposure assessment. Environ Health Perspect. 2013;121(10):1120-1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gordon SB, Bruce NG, Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2(10):823-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GBD 2016 Risk Factors Collaborators Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1345-1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fatmi Z, Coggon D. Coronary heart disease and household air pollution from use of solid fuel: a systematic review. Br Med Bull. 2016;118(1):91-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim C, Seow WJ, Shu XO, et al. Cooking coal use and all-cause and cause-specific mortality in a prospective cohort study of women in Shanghai, China. Environ Health Perspect. 2016;124(9):1384-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitter SS, Vedanthan R, Islami F, et al. Household fuel use and cardiovascular disease mortality: Golestan Cohort Study. Circulation. 2016;133(24):2360-2369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan KH, Lam KBH, Kurmi OP, et al. ; China Kadoorie Biobank Collaborative Group . Trans-generational changes and rural-urban inequality in household fuel use and cookstove ventilation in China: a multi-region study of 0.5 million adults. Int J Hyg Environ Health. 2017;220(8):1370-1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen Y, Shen G, Liu W, et al. Field measurement and estimate of gaseous and particle pollutant emissions from cooking and space heating processes in rural households, northern China. Atmos Environ. 2016;125:265-271. doi: 10.1016/j.atmosenv.2015.11.032 [DOI] [Google Scholar]
- 10.Chen Z, Lee L, Chen J, et al. Cohort profile: the Kadoorie Study of Chronic Disease in China (KSCDC). Int J Epidemiol. 2005;34(6):1243-1249. [DOI] [PubMed] [Google Scholar]
- 11.Chen Z, Chen J, Collins R, et al. ; China Kadoorie Biobank (CKB) Collaborative Group . China Kadoorie Biobank of 0.5 million people: survey methods, baseline characteristics and long-term follow-up. Int J Epidemiol. 2011;40(6):1652-1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lewington S, Lacey B, Clarke R, et al. ; China Kadoorie Biobank Consortium . The burden of hypertension and associated risk for cardiovascular mortality in China. JAMA Intern Med. 2016;176(4):524-532. [DOI] [PubMed] [Google Scholar]
- 13.Bragg F, Holmes MV, Iona A, et al. ; China Kadoorie Biobank Collaborative Group . Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA. 2017;317(3):280-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang S, Luo K. Life expectancy impacts due to heating energy utilization in China: distribution, relations, and policy implications. Sci Total Environ. 2018;610-611:1047-1056. [DOI] [PubMed] [Google Scholar]
- 15.National Bureau of Statistics of the People’s Republic of China China Yearbook of Rural Household Survey. http://www.stats.gov.cn/tjsj/ndsj/. Accessed March 2, 2018.
- 16.Yang GH, Stroup DF, Thacker SB. National public health surveillance in China: implications for public health in China and the United States. Biomed Environ Sci. 1997;10(1):1-13. [PubMed] [Google Scholar]
- 17.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159-174. [PubMed] [Google Scholar]
- 18.Li R, Chambless L. Test for additive interaction in proportional hazards models. Ann Epidemiol. 2007;17(3):227-236. [DOI] [PubMed] [Google Scholar]
- 19.Plummer M. Improved estimates of floating absolute risk. Stat Med. 2004;2(1):93-104 [DOI] [PubMed] [Google Scholar]
- 20.McCracken JP, Smith KR, Díaz A, Mittleman MA, Schwartz J. Chimney stove intervention to reduce long-term wood smoke exposure lowers blood pressure among Guatemalan women. Environ Health Perspect. 2007;115(7):996-1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Quansah R, Semple S, Ochieng CA, et al. Effectiveness of interventions to reduce household air pollution and/or improve health in homes using solid fuel in low-and-middle income countries: a systematic review and meta-analysis. Environ Int. 2017;103:73-90. [DOI] [PubMed] [Google Scholar]
- 22.Clark ML, Bachand AM, Heiderscheidt JM, et al. Impact of a cleaner-burning cookstove intervention on blood pressure in Nicaraguan women. Indoor Air. 2013;23(2):105-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexander D, Larson T, Bolton S, Vedal S. Systolic blood pressure changes in indigenous Bolivian women associated with an improved cookstove intervention. Air Qual Atmos Health. 2015;8(1):47-53. doi: 10.1007/s11869-014-0267-6 [DOI] [Google Scholar]
- 24.Ni K, Carter E, Schauer JJ, et al. Seasonal variation in outdoor, indoor, and personal air pollution exposures of women using wood stoves in the Tibetan Plateau: baseline assessment for an energy intervention study. Environ Int. 2016;94:449-457. [DOI] [PubMed] [Google Scholar]
- 25.Newby DE, Mannucci PM, Tell GS, et al. ; ESC Working Group on Thrombosis, European Association for Cardiovascular Prevention and Rehabilitation; ESC Heart Failure Association . Expert position paper on air pollution and cardiovascular disease. Eur Heart J. 2015;36(2):83-93b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dutta A, Mukherjee B, Das D, Banerjee A, Ray MR. Hypertension with elevated levels of oxidized low-density lipoprotein and anticardiolipin antibody in the circulation of premenopausal Indian women chronically exposed to biomass smoke during cooking. Indoor Air. 2011;21(2):165-176. [DOI] [PubMed] [Google Scholar]
- 27.Painschab MS, Davila-Roman VG, Gilman RH, et al. ; CRONICAS Cohort Study Group . Chronic exposure to biomass fuel is associated with increased carotid artery intima-media thickness and a higher prevalence of atherosclerotic plaque. Heart. 2013;99(14):984-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baumgartner J, Schauer JJ, Ezzati M, et al. Indoor air pollution and blood pressure in adult women living in rural China. Environ Health Perspect. 2011;119(10):1390-1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hutcheon JA, Chiolero A, Hanley JA. Random measurement error and regression dilution bias. BMJ. 2010;340:c2289. [DOI] [PubMed] [Google Scholar]
- 30.Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol. 2009;6(11):712-722. [DOI] [PubMed] [Google Scholar]
- 31.Wu Y, Benjamin EJ, MacMahon S. Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation. 2016;133(24):2545-2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stringhini S, Sabia S, Shipley M, et al. Association of socioeconomic position with health behaviors and mortality. JAMA. 2010;303(12):1159-1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplementary Methods
eTable 1. Baseline Fuel Types According to Study Areas
eTable 2. Baseline Characteristics of Participants at Baseline Survey and Resurvey
eTable 3. Reproducibility of Reported Fuel Use for Cooking and for Heating Between Baseline and Resurvey
eTable 4. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Baseline Fuel Use for Cooking After Additional Adjustments or Further Exclusions
eTable 5. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Baseline Fuel Use for Heating After Additional Adjustments or Further Exclusions
eFigure 1. Locations of the 5 Rural Study Areas of the China Kadoorie Biobank Study in Mainland China
eFigure 2. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality by Baseline Cooking and Heating Fuel Types
eFigure 3. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality by Baseline Cooking and Heating Fuel Types, Stratified by Study Areas
eFigure 4. Adjusted Hazard Ratios for Cardiovascular and All-Cause Mortality According to Weighted Long-term Assessments of Fuel Use for Cooking and for Heating
eFigure 5. Association of Combined Solid Fuel Use for Cooking and for Heating With Cardiovascular and All-Cause Mortality
eReferences