Abstract
This study examines the utility of excising facial nonmelanoma skin cancer in very elderly patients.
Facial nonmelanoma skin cancers (fNMSCs), consisting of basal cell carcinoma and squamous cell carcinoma, are the most common cancers diagnosed worldwide and increase with age. Standard treatment for fNMSCs requires biopsy for pathological confirmation, followed by excision. Excision can lead to a pathological diagnosis of no residual carcinoma (NRC) due to no identifiable carcinoma within the excisional specimen. This situation can occur owing to wound healing in the specimen clearing the carcinoma or to the original biopsy shaving off the entire lesion. This study assesses the utility of excising fNMSCs according to age, with the hypothesis that the indolent nature of fNMSCs and the high NRC rate, coupled with increasing age-related all-cause mortality, should cause the surgeon to counsel patients differently. Such counseling may prevent surgery among elderly patients (>90 years) who may never see a benefit from fNMSC excision.
Methods
This study was approved by the Richard L. Roudebush Veterans Affairs Medical Center institutional review board. We identified 440 patients older than 40 years of age who received standard excision for biopsy-proven fNMSC between January 1, 2013, and December 31, 2015. Patient demographics and carcinoma characteristics were analyzed. Overall survival and age-specific estimated survival from time of excision were assessed. χ2 Testing was used to compare groups, and odds ratios were calculated using logistic regression. Statistical significance was set at P ≤ .05, and statistical analysis was performed with SPSS software (IBM).
Results
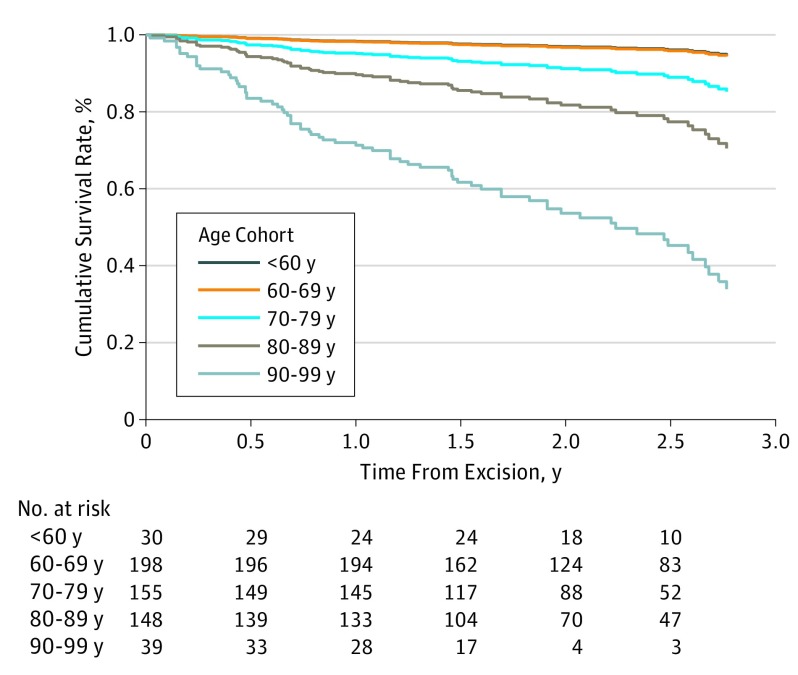
Standard excision was performed on 569 biopsy-proven NMSCs in 440 patients. Basal cell carcinoma comprised 316 lesions (55.5%), whereas 172 lesions (30.2%) were squamous cell carcinoma determined by biopsy. No residual carcinoma was found in 201 excisions (35.3%), with basal cell carcinoma having a lower NRC rate (78 [24.7%]) than squamous cell carcinoma in situ (16 [42.1%]). The highest rate of NRC occurred in reexcisions (24 [58.5%]; P < .001). The proportion of cases of basal cell carcinoma with NRC to cases of squamous cell carcinoma with NRC did not change as a function of age by decade. Although 50 patients (11.3%) died, no death was due to the spread of NMSC. The survival rate decreased by decade of life (Figure), with the lowest survival rate (52%) among patients who were older than 90 years and who also had the highest NRC rate (20 [51.2%]) (Table).
Figure. Kaplan-Meier Survival Stratified by Decade of Life.
Table. Overall Patient and Lesion Characteristics.
| Characteristic | All Patients, No. (%) | Deceased Patients, No. (% per Decade of Life) | Odds of Death (95% CI) | NMSCs Excised, No. (%) | NMSCs With NRC, No. (% per Decade of Life) |
|---|---|---|---|---|---|
| Patient Survival and NMSC NRC Rate by Decade of Life | |||||
| Age, y | |||||
| <60 | 28 (6.4) | 1 (3.6) | 1 [Reference] | 30 (5.3) | 10 (33.3) |
| 60-69 | 158 (35.9) | 7 (4.4) | 1.06 (0.13-8.54) | 198 (34.8) | 68 (34.3) |
| 70-79 | 131 (29.8) | 10 (7.6) | 2.92 (0.38-22.06) | 154 (27.1) | 67 (43.5) |
| 80-89 | 96 (21.8) | 19 (19.8) | 6.39 (0.87-46.87) | 148 (26.0) | 36 (24.3) |
| ≥90 | 27 (6.1) | 13 (48.1) | 19.75 (2.61-149.41) | 39 (6.9) | 20 (51.3) |
| Total | 440 (100) | 50 (11.4) | 569 (100) | 201 (35.3) | |
| NMSC Pathology and NRC Rate | |||||
| NMSCs, No. (%) | NMSCs With NRC, No. (% per Diagnosis) | ||||
| Biopsy pathology | |||||
| BCC | 316 (55.5) | 78 (24.7) | |||
| SCC | 172 (30.2) | 83 (48.3) | |||
| SCC-IS | 38 (6.7) | 16 (42.1) | |||
| BCC and SCC-IS | 1 (0.2) | 0 (0) | |||
| Atypia | 1 (0.2) | 0 (0) | |||
| Reexcision | 41 (7.2) | 24 (58.5) | |||
| Total | 569 (100) | 201 (35.3) | |||
Abbreviations: BCC, basal cell carcinoma; IS, in situ; NMSC, nonmelanoma skin cancer; NRC, no residual carcinoma; SCC, squamous cell carcinoma.
Discussion
Currently, age is not a consideration in the treatment of fNMSCs. Patients, whether they are 40 or 90 years of age, are treated the same for small, minimally morbid, nonlethal NMSCs. Two specific issues should guide the treatment of fNMSCs above the eighth decade of life, with the benefit weighed against the estimated life span of the patient. The first issue is the likelihood of NRC after lesion excision, which is demonstrated here to occur in older patients at a similar rate as the rate in multiple previously studied populations. More than a third of patients older than 80 years (and more than half of those >90 years) had no carcinoma present after biopsy when evaluated histologically after excision. This finding indicates that a large minority of patients would not have required either a primary excision or reexcision. The second issue is patient longevity. Actuarial tables can estimate with some certainty the relative probability of death, but, to our knowledge, this study is the first to indicate that disease-specific survival is not affected by the excision of small fNMSCs. No patient in the study died of fNMSC. In more than half of the cases of fNMSC excision in patients older than 90 years, death occurred within 1 year. These small fNMSCs would never have caused a problem. When coupled with an NRC rate of 50%, a strong argument can be made for a watchful-waiting approach for the amenable nonagenarian.
These 2 issues should be discussed with the patient on a case-by-case basis so that patient comfort and outcomes can be maximized. Future studies are needed to investigate if a watchful-waiting approach is cost-effective and has higher patient satisfaction than surgical excision in this elderly population.
References
- 1.Rogers HW, Weinstock MA, Harris AR, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146(3):283-287. [DOI] [PubMed] [Google Scholar]
- 2.National Comprehensive Cancer Network NCCN Clinical Practice Guidelines in Oncology. NCCN Guidelines. Squamous Cell Skin Cancer. Version 1.2017. https://www.nccn.org/professionals/physician_gls/pdf/squamous.pdf. Published October 3, 2016. Accessed November 16, 2017.
- 3.National Comprehensive Cancer Network NCCN Clinical Practice Guidelines in Oncology. NCCN Guidelines. Basal Cell Skin Cancer. Version 1.2017. https://www.nccn.org/professionals/physician_gls/pdf/squamous.pdf. Published October 3, 2016. November 16, 2017.
- 4.Gurunluoglu R, Kubek E, Arton J, Olsen A, Bronsert M. No residual basal cell carcinoma after excision for biopsy-proven tumor: clinical and medicolegal implications. Plast Reconstr Surg Glob Open. 2014;1(9):e87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stewart CMM, Garlick J, Mcmullin J, et al. Surgical excision of non-melanoma skin cancer in an elderly Veteran’s Affairs population. Plast Reconstr Surg Glob Open. 2015;2(12):e277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swetter SM, Boldrick JC, Pierre P, Wong P, Egbert BM. Effects of biopsy-induced wound healing on residual basal cell and squamous cell carcinomas: rate of tumor regression in excisional specimens. J Cutan Pathol. 2003;30(2):139-146. [DOI] [PubMed] [Google Scholar]