Abstract
Background
Both anemia and blood transfusion are associated with poor outcomes. The aim of this study was to evaluate the effect of preoperative blood transfusion on postoperative outcomes after colectomy, stratified by severity of anemia.
Methods
Patients undergoing colectomy from 2012–2014 were selected from the National Surgical Quality Improvement Program targeted colectomy database. Patients were divided into 2 groups based on receipt of preoperative transfusion and then stratified by hematocrit. Univariate and multivariate analyses were used to compare 30-day outcomes between the 2 groups.
Results
A total of 60,785 patients were included in the study, with an overall preoperative transfusion rate of 3.4% (n = 2,073). On univariate analysis, transfusion was associated with significantly greater rates of postoperative morbidity. The risk-adjusted, multivariate model confirmed increased risk of complications with preoperative transfusion (odds ratio 1.32, 95% confidence interval, 1.18–1.48). Furthermore, transfusion did not improve outcomes even in the setting of moderate anemia (odds ratio 1.35, 95% confidence interval, 1.14–1.60) or severe anemia (odds ratio 0.97, 95% confidence interval, 0.66–1.41).
Conclusions
Preoperative transfusion is an independent predictor of complications in patients with mild and moderate anemia. Furthermore, these retrospective data suggest that even severely anemic patients do not benefit from preoperative transfusion and empiric transfusion therefore should be avoided. Alternatives to preoperative optimization of this high-risk surgical population should be sought. (Surgery 2017;161:1067-75.)
Preoperative anemia is an exceedingly common finding among patients undergoing colorectal surgery, with prior studies suggesting that up to 50–75% of patients have at least some degree of anemia.1,2 Preoperative anemia not only is highly prevalent in this population but anemia is also a known predictor of poor postoperative outcomes, including a greater incidence of composite morbidity, increased mortality, and a greater duration of hospital stay.1,3,4
The primary treatment for anemia deemed to be clinically relevant is blood transfusion,5–7 which unfortunately also is known to be associated with many adverse effects. Like anemia itself, perioperative blood transfusions in surgical patients also has been associated with increased risk of postoperative complications, greater mortality, and greater duration of hospital stay.8,9 Additionally, and particularly relevant in the treatment of patients with colorectal cancer, blood transfusion is associated with worse, long-term oncologic outcomes.10
Currently, there is poor standardization of practices surrounding preoperative blood transfusion. An estimated 14–28% of patients undergoing surgery for colorectal cancer receive a perioperative transfusion,8 but the threshold at which transfusion is indicated is poorly defined.7,11 In the trial titled Transfusion Requirements in Critical Care, critically ill patients who were randomized to a restrictive blood transfusion protocol had improved in-hospital outcomes compared to those managed according to a more liberal transfusion protocol, particularly among patients <55 years of age and with less severe disease.12 In contrast, in patients undergoing hip and cardiac operations, randomized controlled trials have failed to demonstrate a benefit of restrictive transfusion thresholds (hemoglobin triggers of 7.5–8 g/dL) compared to more liberal thresholds (hemoglobin of 9–10 g/dL) in the treatment of postoperative anemia.13,14 Therefore, the risk-to-benefit ratio of transfusion in surgical patients, particularly in the setting of various degrees of anemia, remains unclear.
Several prior studies have evaluated the effect of perioperative blood transfusion on postoperative outcomes in colorectal surgery patients. Although worse outcomes have been reported almost universally in association with perioperative transfusion, these studies often have failed to address the severity of preoperative anemia and have not stratified by timing of blood transfusion (ie, preoperative versus intra- or postoperative). Therefore, the purpose of this study was to examine whether preoperative blood transfusion can improve postoperative outcomes in moderately to severely anemic patients undergoing colectomy. We hypothesized that only in severely anemic patients would preoperative blood transfusion prove beneficial in decreasing the incidence of postoperative complications.
METHODS
Study design and data collection
This study is a retrospective cohort study evaluating the effect of preoperative blood transfusion on postoperative outcomes in patients undergoing colectomy. The colectomy-targeted database of the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) was used as the source of data for this study. This database is a prospectively maintained, clinical outcomes database including data from up to 203 participating hospitals. Starting in 2011–2012, a targeted colectomy participant use file is available, which contains patients specifically undergoing colon resection and includes variables more specific to this patient population. Data are available currently through 2014. This study was deemed exempt from review by the University of Wisconsin-Madison Institutional Review Board.
Patient selection
Adult patients undergoing partial or total colectomy (Current Procedural Terminology codes 44140, 44141, 44143, 44144, 44145, 44146, 44147, 44150, 44151, 44160, 44204, 44205, 44206, 44207, 44208, and 44210) for any indication from January 1, 2012 to December 31, 2014 were selected from the ACS-NSQIP targeted-colectomy participant use file. Exclusion criteria included unavailability of a preoperative hematocrit value (n = 2,494), American Society of Anesthesiologists (ASA) class 5 (n = 408) or ASA class unknown (n = 60), and missing age (n = 1). A small percentage of patients (2.3%) were excluded from the multivariate models due to missing data for key adjustment variables in the model. Additionally, for analyses comparing rates of anastomotic leak, only the subset of patients actually undergoing primary anastomosis, with or without proximal diversion, were included (Current Procedural Terminology codes 44140, 44145, 44160, 44204, 44205, and 44207).
Variable definitions and cohort assignment
Patients were divided into 2 groups based on receipt of preoperative blood transfusion, which was classified using the preoperative blood transfusion variable available in the NSQIP database. This variable is defined as preoperative transfusion of at least 1 unit of whole or packed red blood cells in the 72 hours prior to colectomy. The exact number of units transfused is not available in the ACS-NSQIP targeted colectomy participant use file. Additionally, patients were stratified by severity of preoperative anemia. These groups included normal hematocrit (hematocrit ≥36), mild anemia (30–35.9), moderate anemia (24–29.9), and severe anemia (<24), based on clinical utility and cutoffs reported previously in the literature.15 Laboratory values are reported in NSQIP for tests performed up to 90 days before the colectomy.
Body mass index (BMI) and age were both treated as categorical variables. Age groups were defined as follows: <65 years, 65–79 years, 80 + years. Operative approach was classified as open, minimally invasive, or minimally invasive with unplanned conversion to open.
End points
The primary outcome for this study was occurrence of any 30-day postoperative complication, which included the standard complications reported in the NSQIP database as well as anastomotic leak, exclusive of the bleeding transfusion outcome. Given the previously reported association between blood transfusion and immune suppression, a composite outcome of “infectious complications” also was evaluated, which included superficial surgical site infection (SSSI), deep surgical site infection, organ space surgical site infection, pneumonia, urinary tract infection, sepsis, and septic shock. Additional secondary outcomes included 30-day mortality, SSSI as an individual complication, and anastomotic leak.
Statistical analysis
Patient characteristics, including demographics and baseline comorbidities as well as indication for operation and severity of preoperative anemia, were compared between the 2 groups (receipt versus no receipt of preoperative transfusion) using χ2 tests. Univariate analysis using χ2 tests was performed to compare unadjusted rates of postoperative complications between the 2 transfusion groups, both with and without stratification by severity of preoperative anemia. To control for baseline differences between the 2 groups, a multivariate analysis was performed using multiple logistic regression for each of the outcomes. Explanatory variables for the multivariate model were selected based on clinical relevance and availability in the NSQIP database and included age, BMI, preoperative comorbidities, degree of preoperative anemia, operative approach, indication for colectomy, and emergency designation. Multivariate analysis also was performed after stratifying by severity of preoperative anemia. Finally, a sensitivity analysis was performed, excluding patients who underwent emergent operations. The same analysesas described previously were performed on this smaller analytic cohort. Statistical analysis was performed using SPSS, version 22 (IBM Corporation, Armonk, NY).
RESULTS
A total of 60,785 patients were identified for inclusion in the study, with an overall preoperative transfusion rate of 3.4% (n = 2,073). The majority of patients had a normal preoperative hematocrit (65%, n = 39,359), while 24% (n = 14,478) of patients had mild anemia, 10% had moderate anemia (n = 6,133), and only 1.3% were severely anemic (n = 815; Fig 1). The overwhelming majority of patients had their preoperative hematocrit measured within 30 days of the colectomy (n = 57,355, 94.4%).
Fig 1.
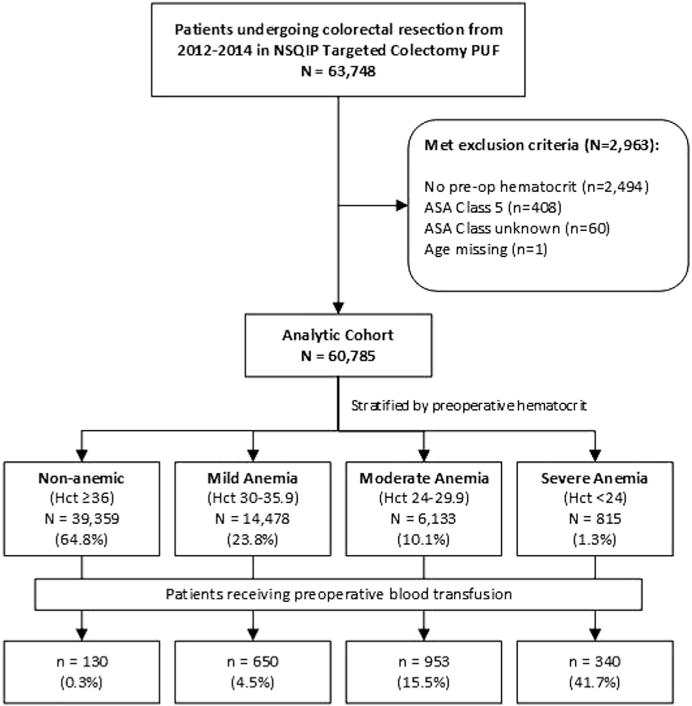
Flow diagram showing selection of analytic cohort, stratification based on anemia severity and receipt of preoperative blood transfusion. PUF, Participant use file; Hct, hematocrit.
Characteristics of the 2 groups
Patients receiving a preoperative transfusion and those not receiving transfusion differed significantly at baseline (Table I). The transfusion group was less healthy by nearly every measure. Transfused patients were older on average, more likely to be of ASA class 3 or 4, had more baseline comorbidities, and were more severely anemic compared with those not being transfused. Transfused patients also were more likely to be undergoing emergency operation or open colectomy and to have an indication of cancer or bleeding.
Table I.
Characteristics of patients receiving and not receiving preoperative blood transfusion
| Preoperative transfusion
|
|||
|---|---|---|---|
| Characteristic, % | No (n = 58,712), 96.6% |
Yes (n = 2,073), 3.4% |
X2 P value |
| Female | 53 | 49 | .002 |
| Age, y | <.001 | ||
| <65 | 55 | 34 | |
| 65–79 | 33 | 39 | |
| 80+ | 12 | 27 | |
| Body mass index | <.001 | ||
| <18.5 | 3.2 | 5.3 | |
| 18.5–24.9 | 31 | 35 | |
| 25–29.9 | 33 | 30 | |
| 30–34.9 | 20 | 16 | |
| 35+ | 14 | 13 | |
| ASA class 3 or 4 | 55 | 86 | <.001 |
| Emergency case | 15 | 40 | <.001 |
| Indication | <.001 | ||
| Cancer | 38 | 41 | |
| Diverticulitis | 23 | 9.8 | |
| Polyp | 8.6 | 1.0 | |
| Inflammatory bowel disease | 8.0 | 7.6 | |
| Bleeding | 0.5 | 18 | |
| Volvulus | 2.8 | 1.3 | |
| Other | 20 | 21 | |
| Operative approach | <.001 | ||
| Open | 40 | 65 | |
| Minimally invasive | 52 | 29 | |
| Converted | 7.9 | 6.5 | |
| Sepsis | 6.1 | 11 | <.001 |
| Septic shock | 1.8 | 8.0 | <.001 |
| Hematocrit | <.001 | ||
| ≥36 | 67 | 6.3 | |
| 30–35.9 | 24 | 31 | |
| 24–29.9 | 8.8 | 46 | |
| <24 | 0.8 | 16 | |
| Chemotherapy within 90 d | 5.5 | 4.9 | .375 |
| Diabetes | 15 | 22 | <.001 |
| Current smoker | 17 | 14 | <.001 |
| Dyspnea | 6.9 | 14 | <.001 |
| Dependent functional status | 3.3 | 9.4 | <.001 |
| Ventilator-dependent | 0.8 | 6.6 | <.001 |
| COPD | 5.5 | 10 | <.001 |
| Ascites | 1.0 | 4.0 | <.001 |
| Congestive heart failure | 1.0 | 5.4 | <.001 |
| Hypertension | 49 | 63 | <.001 |
| Acute renal failure | 0.6 | 3.5 | <.001 |
| Dialysis-dependent | 1.0 | 5.5 | <.001 |
| Disseminated cancer | 6.4 | 11 | <.001 |
| Open wound/wound infection | 2.0 | 6.5 | <.001 |
| Steroid use | 9.5 | 14 | <.001 |
| >10% weight loss in past 6 mo | 5.0 | 11 | <.001 |
| Coagulopathy | 4.6 | 19 | <.001 |
| Intra/postoperative transfusion | 11 | 48 | <.001 |
| Operative time, min | <.001 | ||
| <60 | 3.9 | 5.5 | |
| 60–119 | 26 | 33 | |
| 120–179 | 32 | 33 | |
| 180+ | 38 | 29 | |
COPD, Chronic obstructive pulmonary disease.
Missing data: approach (n = 50, 0.1%), body mass index (n = 1,100, 1.8%), functional status (n = 273, 0.4%), operative time (n = 16, <0.1%).
Transfusion utilization
As expected, preoperative transfusion correlated strongly with degree of preoperative anemia, with 42% (n = 340) of severely anemic patients receiving a transfusion, but only 0.3% (n = 130) of nonanemic, 5% of mildly anemic, and 16% of moderately anemic patients being transfused. Of those receiving a preoperative transfusion, 48% went on to also receive an intra- or postoperative transfusion within 72 hours of the colectomy, compared with only 11% of the nonpreoperative transfusion group.
Unadjusted comparison of postoperative complications
On univariate analysis, transfusion was associated with worse postoperative outcomes for all end points analyzed. Transfusion was associated with nearly double the incidence of overall postoperative complications (45% vs 23%, P < .001) and quadruple the 30-day mortality (12% vs 3%, P < .001; Fig 2). Anastomotic leak also was associated with preoperative transfusion, occurring in 5.7% of transfused patients but in only 3.7% of the nontransfused group (P < .001). When stratified by severity of preoperative anemia, transfusion continued to be associated with worse postoperative outcomes, although to a less dramatic degree in the more severely anemic subsets of patients (Fig 3). Among patients with moderate anemia, transfusion was associated with a greater incidence of postoperative complications (44% vs 34%, P < .001) and 30-day mortality (13.4% vs 7.2%, P < .001). Similarly, patients with severe anemia experienced worse outcomes in the setting of preoperative transfusion, including approximately a 10% greater incidence of any postoperative complication (50% vs 40%, P = .004), but there was no difference in mortality (12% vs 10%, P = .226).
Fig 2.
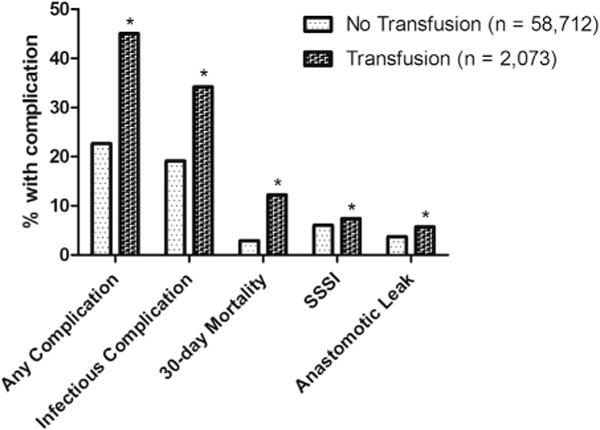
Results of univariate analysis comparing outcomes between patients receiving and not receiving a preoperative blood transfusion. *P < .05.
Fig 3.
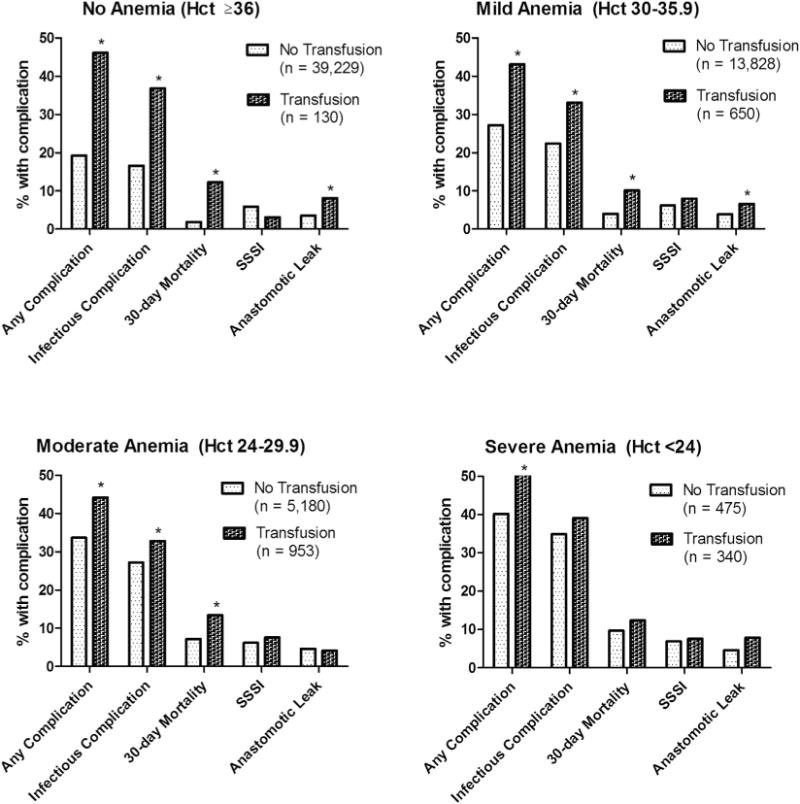
Results of the univariate analysis comparing outcomes between patients receiving and not receiving preoperative blood transfusion, when stratified by severity of preoperative anemia. *P < .05.
Multivariate analysis
The results of the multivariate analysis are depicted in Table II. Among all patients, transfusion was an independent predictor of occurrence of any complication, infectious complications, and increased mortality. There was also a trend toward increased risk of SSSI (P = .062) but not anastomotic leak. Again, in the setting of mild and moderate anemia, transfusion was associated with a greater risk of any postoperative complication but otherwise seemed to have less of an effect on outcomes. Transfusion neither helped nor harmed the severely anemic patients; however, it is worth noting that confidence intervals are quite wide given the smaller sample size of this group.
Table II.
Results of multivariate analysis: risk of complications with preoperative blood transfusion
| Population | Outcome | OR | 95% CI | P value |
|---|---|---|---|---|
| All patients | Any complication | 1.317 | 1.176–1.475 | <.001 |
| Infectious complication | 1.157 | 1.029–1.300 | .014 | |
| Mortality | 1.281 | 1.061–1.546 | .010 | |
| SSSI | 1.207 | 0.991–1.471 | .062 | |
| Leak | 1.146 | 0.866–1.515 | .341 | |
| Mild anemia | Any complication | 1.231 | 1.017–1.491 | .033 |
| Infectious complication | 1.125 | 0.924–1.369 | .241 | |
| Mortality | 1.039 | 0.744–1.453 | .821 | |
| SSSI | 1.272 | .923–1.752 | .141 | |
| Leak | 1.248 | 0.792–1.967 | .340 | |
| Moderate anemia | Any complication | 1.350 | 1.139–1.601 | .001 |
| Infectious complication | 1.130 | 0.947–1.350 | .176 | |
| Mortality | 1.460 | 1.118–1.907 | .005 | |
| SSSI | 1.229 | 0.913–1.654 | .173 | |
| Leak | 0.962 | 0.610–1.516 | .867 | |
| Severe anemia | Any complication | 0.965 | 0.661–1.409 | .854 |
| Mortality | 0.903 | 0.498–1.636 | .736 | |
| Infectious complication | 0.909 | 0.628–1.314 | .611 | |
| SSSI | 1.187 | 0.623–2.263 | .602 | |
| Leak | 0.853 | 0.260–2.805 | .794 |
Bold type indicates P < .05.
The sensitivity analysis performed using only nonemergency cases yielded similar results, with greater odds of any postoperative complication (odds ratio [OR] 1.346; 95% confidence interval [CI], 1.173–1.544), infectious complications (OR 1.191; 95% CI, 1.028–1.380), and 30-day mortality (OR 1.571; 95% CI, 1.204–2.049) in the setting of preoperative transfusion after adjusting for severity of anemia.
DISCUSSION
In this study, we found that preoperative transfusion is an independent predictor of postoperative complications after colectomy. Patients receiving preoperative blood transfusions had a greater incidence of overall complications, infectious complications, mortality, and anastomotic leak compared to nontransfused patients. Furthermore, stratification by severity of preoperative anemia did not qualitatively alter this association. Although the magnitude of the deleterious effect of transfusion seems to diminish as the severity of anemia worsens, based on these retrospective data, preoperative transfusion does not seem to have a beneficial effect even in patients with hematocrit of <24. Although it is clear that sicker patients tend to receive transfusions, our findings suggest that at a minimum, transfusion is a marker of worse operative outcomes, but likely also contributes to postoperative morbidity. In fact, we identified similar rates of complications (40–50%) among all subsets of patients receiving a transfusion, regardless of severity of preoperative anemia, again suggesting that transfusion itself is associated with complications.
Several possible mechanisms by which transfusion causes harm have been proposed. Although our study does not clarify further the mechanism by which transfusions are detrimental, our study nonetheless adds to the body of evidence that perioperative transfusion has an adverse effect on short-term outcomes. It has long been recognized that autologous transfusion results in a state of relative immunosuppression,8,16 which likely accounts for the increased risk for infectious complications. Paradoxically, transfusion also increases inflammation by inducing alloimmunization, which is the underlying mechanism for transfusion reactions, such as transfusion-related acute lung injury and multiorgan failure.17
To our knowledge, our study is the first to look specifically at the impact of preoperative, rather than any perioperative, transfusion on outcomes. By looking only at preoperative transfusion, our study removes some of the potential confounding regarding why a patient may have received an intra- or postoperative transfusion, such as unexpected intraoperative hemorrhage or a postoperative bleeding event. We were interested particularly in whether transfusion is a potentially useful adjunct for optimizing patients with pre-existing anemia, given the greater morbidity and mortality in this population. Nonetheless, our finding of increased complications in those receiving preoperative transfusion is consistent with observations reported by other authors.4,8,9,18,19
Using NSQIP data from 2005–2010, Halabi et al8 found that patients undergoing operation for colorectal cancer who received a perioperative blood transfusion had significantly worse outcomes, including more complications, greater mortality and durations of hospital stay, and a greater incidence of pneumonia and SSSI compared with those not requiring transfusion. Interestingly, in their subgroup analysis of anemic patients (defined as hematocrit <38), transfusion was associated with a 30% decreased risk of overall postoperative complications, which is contrary to our results. Their population consisted entirely of patients undergoing operation for colorectal cancer, and as mentioned, did not differentiate between pre-, intra-, and postoperative transfusions, which resulted in a more heterogeneous indication for transfusion compared with our study. The otherwise-healthy patient who experiences an intraoperative hemorrhage leading to an intraoperative transfusion likely has a much lower baseline risk for complications compared to the frail, chronically anemic patient who is transfused preoperatively in an attempt to mitigate the risk of anemia.
Another interesting finding in our study that speaks to the relative lack of standardization of transfusion across centers and surgeons is that 6% of patients being transfused had a normal hematocrit and nearly one-third had only mild anemia. Although the NSQIP database does not specify the timing of laboratory tests in relation to transfusion, it is likely that at least a portion of these patients were transfused unnecessarily. Prior studies have documented the overuse of transfusions in colorectal surgery patients,20 and our results suggest possible overuse or at least poor standardization of practices. Similarly, severely anemic patients, a population that might be expected to universally receive a transfusion prior to operation, were actually split nearly evenly with regard to receipt of preoperative transfusion. This observation highlights the variation in practice patterns among surgeons.
The present study has several important limitations. First, given the retrospective and non-randomized design, we cannot ascertain causation but merely association. It is evident that patients receiving preoperative blood transfusion differ substantially from those not being transfused. Although we attempted to control for these differences by performing a multivariable analysis and stratifying by severity of anemia, there remain unmeasured confounders for which we have been unable to adjust. Second, the NSQIP database offers no insight into why the decision was made to transfuse any given patient, such as ongoing bleeding, symptoms, comorbidities, hypotension, hypovolemia, or other underlying reasons. Such information would have been useful to understand the clinical circumstances under which transfusions are being given and to understand further the circumstances in which transfusion may be of benefit. Third, we were unable to quantify the volume of blood transfusion. Given prior reports suggesting a dose-response, harmful effect of transfusion,8,9 it would have been helpful to have this information for further adjustment of the model. Finally, we were also unable to ascertain whether the reported preoperative hematocrit values were obtained pre- or post-transfusion. We performed our analysis under the assumption that these values were measured pretransfusion; however, these data were not available. It is important to note that this latter limitation could have a marked impact on our results. It is possible that some patients were allocated incorrectly to a less severe class of anemia than was present prior to receiving a transfusion. Assuming that patients with severe anemia are at the greatest risk for complications, this type of bias potentially would artificially increase the observed rate of complications in the subset of mild and moderately anemic patients receiving preoperative transfusion.
In conclusion, we found that preoperative transfusion seems to be an independent predictor of worse postoperative outcomes. Importantly, based on this retrospective data, it does not seem that even severely anemic patients derive a clinically protective benefit from transfusion. It will be important to continue to seek alternatives for preoperative optimization of this patient population, which is clearly at high risk for a difficult postoperative course after colectomy. Additionally, a more clear understanding of which patients are most likely to benefit from transfusion will allow for standardization of practices and may assist with resource utilization and the provision of greater value care to patients.
Acknowledgments
Salary support for C.M. Papageorge is provided by a T32 Surgical Oncology Training Grant (NIH NCI T32 CA090217-11).
Footnotes
C.M. Papageorge, G.D. Kennedy, and E.H. Carchman have no disclosures, industry funding, or other conflicts of interest to report.
Presented at the 11th Annual Academic Surgical Congress in Jacksonville, FL, February 2–4, 2016.
References
- 1.Leichtle SW, Mouawad NJ, Lampman R, Singal B, Cleary RK. Does preoperative anemia adversely affect colon and rectal surgery outcomes? J Am Coll Surg. 2011;212:187–94. doi: 10.1016/j.jamcollsurg.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 2.Shander A, Knight K, Thurer R, Adamson J, Spence R. Prevalence and outcomes of anemia in surgery: a systematic review of the literature. Am J Med. 2004;116(Suppl 7A):58s–69s. doi: 10.1016/j.amjmed.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 3.Richards T, Musallam KM, Nassif J, Ghazeeri G, Seoud M, Gurusamy KS, et al. Impact of preoperative anaemia and blood transfusion on postoperative outcomes in gynaecological surgery. PLoS One. 2015;10:e0130861. doi: 10.1371/journal.pone.0130861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A, et al. Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet. 2011;378:1396–407. doi: 10.1016/S0140-6736(11)61381-0. [DOI] [PubMed] [Google Scholar]
- 5.Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database Syst Rev. 2012:CD002042. doi: 10.1002/14651858.CD002042.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Klein HG, Spahn DR, Carson JL. Red blood cell transfusion in clinical practice. Lancet. 2007;370:415–26. doi: 10.1016/S0140-6736(07)61197-0. [DOI] [PubMed] [Google Scholar]
- 7.Wang JK, Klein HG. Red blood cell transfusion in the treatment and management of anaemia: the search for the elusive transfusion trigger. Vox Sang. 2010;98:2–11. doi: 10.1111/j.1423-0410.2009.01223.x. [DOI] [PubMed] [Google Scholar]
- 8.Halabi WJ, Jafari MD, Nguyen VQ, Carmichael JC, Mills S, Pigazzi A, et al. Blood transfusions in colorectal cancer surgery: incidence, outcomes, and predictive factors: an American College of Surgeons National Surgical Quality Improvement Program analysis. Am J Surg. 2013;206:1024–32. doi: 10.1016/j.amjsurg.2013.10.001. discussion 1032-3. [DOI] [PubMed] [Google Scholar]
- 9.Bernard AC, Davenport DL, Chang PK, Vaughan TB, Zwischenberger JB. Intraoperative transfusion of 1 U to 2 U packed red blood cells is associated with increased 30-day mortality, surgical-site infection, pneumonia, and sepsis in general surgery patients. J Am Coll Surg. 2009;208:931–7. 937.e1–2. doi: 10.1016/j.jamcollsurg.2008.11.019. discussion 938-9. [DOI] [PubMed] [Google Scholar]
- 10.Schiergens TS, Rentsch M, Kasparek MS, Frenes K, Jauch KW, Thasler WE. Impact of perioperative allogeneic red blood cell transfusion on recurrence and overall survival after resection of colorectal liver metastases. Dis Colon Rectum. 2015;58:74–82. doi: 10.1097/DCR.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 11.Spahn DR, Shander A, Hofmann A. The chiasm: transfusion practice versus patient blood management. Best Pract Res Clin Anaesthesiol. 2013;27:37–42. doi: 10.1016/j.bpa.2013.02.003. [DOI] [PubMed] [Google Scholar]
- 12.Hebert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion Requirements in Critical Care Investigators, Canadian Critical Care Trials Group. N Engl J Med. 1999;340:409–17. doi: 10.1056/NEJM199902113400601. [DOI] [PubMed] [Google Scholar]
- 13.Murphy GJ, Pike K, Rogers CA, Wordsworth S, Stokes EA, Angelini GD, et al. Liberal or restrictive transfusion after cardiac surgery. N Engl J Med. 2015;372:997–1008. doi: 10.1056/NEJMoa1403612. [DOI] [PubMed] [Google Scholar]
- 14.Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG, et al. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med. 2011;365:2453–62. doi: 10.1056/NEJMoa1012452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu WC, Smith TS, Henderson WG, Eaton CB, Poses RM, Uttley G, et al. Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann Surg. 2010;252:11–7. doi: 10.1097/SLA.0b013e3181e3e43f. [DOI] [PubMed] [Google Scholar]
- 16.Hart S, Cserti-Gazdewich CM, McCluskey SA. Red cell transfusion and the immune system. Anaesthesia. 2015;70:38–45. e13–36. doi: 10.1111/anae.12892. [DOI] [PubMed] [Google Scholar]
- 17.Raghavan M, Marik PE. Anemia, allogenic blood transfusion, and immunomodulation in the critically ill. Chest. 2005;127:295–307. doi: 10.1378/chest.127.1.295. [DOI] [PubMed] [Google Scholar]
- 18.Obi AT, Park YJ, Bove P, Cuff R, Kazmers A, Gurm HS, et al. The association of perioperative transfusion with 30-day morbidity and mortality in patients undergoing major vascular surgery. J Vasc Surg. 2015;61:1000–1009.e1. doi: 10.1016/j.jvs.2014.10.106. [DOI] [PubMed] [Google Scholar]
- 19.Tan TW, Eslami M, Rybin D, Doros G, Zhang WW, Farber A. Blood transfusion is associated with increased risk of perioperative complications and prolonged hospital duration of stay among patients undergoing amputation. Surgery. 2015;158:1609–16. doi: 10.1016/j.surg.2015.04.039. [DOI] [PubMed] [Google Scholar]
- 20.Hallissey MT, Crowson MC, Kiff RS, Kingston RD, Fielding JW. Blood transfusion: an overused resource in colorectal cancer surgery. Ann R Coll Surg Engl. 1992;74:59–62. [PMC free article] [PubMed] [Google Scholar]


