Abstract
Bedside use of Doppler echocardiography is being featured as a promising, clinically useful tool in assessing the pulmonary circulation in patients with acute respiratory distress syndrome (ARDS). The present review is aimed at summarizing the available evidence obtained with echocardiography on right ventricle (RV) function and pulmonary circulation in ARDS and to highlight the potential of this technique in clinical practice (only articles in English language were considered). According to the available evidence on echocardiographic findings, the following conclusions can be drawn: (a) echocardiography (transthoracic and transesophageal) has a growing role in the management ARDS patients mainly because of the strict interactions between the lung (and ventilation) and the RV and pulmonary circulation; (b) there may be a continuum of alterations in RV size and function and pulmonary circulation which may end in the development of acute cor pulmonale, probably paralleling ARDS disease severity; and (c) the detection of acute cor pulmonale should prompt intensivists to tailor their ventilatory strategy to the individual patient depending on the echocardiography findings. Bearing in mind the clinical role and growing importance of echocardiography in ARDS and the available evidence on this topic, we present a flow chart including the parameters to be measured and the timing of echo exams in ARDS patients. Despite the important progress that echocardiography has gained in the evaluation of patients with ARDS, several open questions remain and echocardiography still appears to be underused in these patients. A more systematic use of echocardiography (mainly through shared protocols) in ARDS could help intensivists to tailor the optimal treatment in individual patients as well as highlighting the limits and potential of this methodology in patients with ALI.
Keywords: acute respiratory distress syndrome, echocardiography, pulmonary systolic arterial hypertension, right ventricle
Introduction
In acute respiratory distress syndrome (ARDS), the treatment of lung injury is based mainly on supportive therapy with lung-protective ventilation; but pulmonary vascular injury associated with this condition is being considered as yet another therapeutic target, together with its effects on the right ventricle (RV) and on systemic hemodynamics. In this context, bedside use of Doppler echocardiography is being featured as a promising, clinically useful tool [Mayo et al. 2015] in assessing the pulmonary circulation and RV function (as well as biventricular function) in ARDS patients [Repessé et al. 2015; Chiumello and Pesenti, 2013; Vieillard-Baron, 2009; Khrishnan and Schmidt, 2015]. Since the first report in 1985 [Jardin et al. 1985] describing the RV and left ventricle (LV) functions with echocardiography in a small subset of patients with acute respiratory failure, an increasing number of papers have been published on this topic, but the available evidence mainly concerns the prevalence and the prognostic impact of acute cor pulmonale (ACP) in ARDS [Repessé et al. 2015; Chiumello and Pesenti, 2013; Vieillard-Baron, 2009].
The present review is aimed at summarizing the available evidence obtained with echocardiography on RV function and pulmonary circulation in ARDS and to highlight potentials of this technique in clinical practice.
A PubMed search was conducted combining the words ‘acute lung injury and/or ARDS’, and ‘echocardiography’, and ‘adult’, and ‘pulmonary vascular dysfunction and/or right ventricle’. Only articles in English language were considered and case reports were excluded.
The term ‘pulmonary vascular dysfunction’ was first introduced by Zapol and Snider in 1977 [Zapol and Snider, 1977] when describing ARDS patients with elevated pulmonary vascular resistance, an increase in RV stroke-work index and progressive RV dysfunction resulting in cor pulmonale and refractory circulatory failure after several days on respiratory support.
Three elements, which can be investigated by echocardiography, characterize the pulmonary vascular alterations and their effects on the RV in ARDS: (a) pulmonary systolic arterial hypertension (sPAP); (b) RV dimension and function; and (c) septal dyskinesia. Using echocardiography, Boissier and colleagues [Boissier et al. 2013] stratified ARDS patients with pulmonary circulatory system dysfunction into three groups as follows.
No dysfunction [pulmonary systolic arterial pressure (sPAP) of more than or equal to 40 mmHg with normal right RV size and normal interventricular septum kinetics].
Moderate dysfunction (sPAP more than 40 mmHg or dilated RV but without cor pulmonale).
Severe dysfunction (ACP). Cor pulmonale is defined as an alteration in the structure and function of the RV caused by a primary disorder of the respiratory system. RV impairment can quickly turn into ACP due to an increase in RV afterload. Common causes of ACP in the ICU are ARDS, ‘aggressive’ mechanical ventilation and massive pulmonary embolism [Bouferrache and Vieillard-Baron, 2011; Repessé et al. 2015].
The prevalence and clinical significance of each grade of pulmonary circulatory system dysfunction has not been completely elucidated to date, even if previous investigations assessed the prognostic impact of ACP (that is severe pulmonary dysfunction) on mortality in ARDS patients [Boissier et al. 2013, Jardin et al. 1997, 1999; Lhéritier et al. 2013; Vieillard-Baron et al. 2001, 2002, 2013].
Pulmonary systolic arterial hypertension
Pulmonary hypertension (PH) is defined as a condition characterized by an increase in mean arterial pulmonary pressure more than or equal to 25 mmHg measured at rest with right heart catheterization [Galié et al. 2009], which typically coincides with pulmonary systolic arterial pressure more than 40 mmHg. [McQuillan et al. 2001]. This definition mainly reflects chronic PH, which is further classified in five categories [Simonneau et al. 2009]. To date there is no specific agreement in the definition of PH in the acute setting of acute lung injury (ALI) or ARDS, in which other factors such as RV dysfunction and mechanical ventilation play a pivotal role.
Boissier and colleagues [Boissier et al. 2013] considered an sPAP cut off of 40 mmHg in defining the presence of moderate pulmonary vascular dysfunction in ARDS patients using echocardiography.
sPAP can be calculated with echocardiography from the tricuspid regurgitant velocity [Howard et al. 2012; Portnoy and Rudski, 2015; Rudski et al. 2010]. However, this value may be underestimated due to an insufficient Doppler envelope or eccentric tricuspid regurgitation jet and it should be interpreted with caution because pulmonary systolic artery pressure also depends on right ventricular systolic function [Rudski et al. 2010; Caille and Vieillard-Baron, 2010; Jardin and Vieillard-Baron, 2007]. The gold standard for the diagnosis of PH is right-heart catheterization, whose main disadvantage is that it is an invasive test, associated with increased morbidity and mortality even in experienced centers. In a systematic review and meta-analysis only a modest correlation between sPAP estimated from echocardiography was reported compared with that measured by right-heart catheterization from mild-to-moderate sPAP. This can be related to the potential limitations of echocardiography itself, including the technical difficulties in detecting a tricuspid regurgitant jet of good quality [Fisher et al. 2009, Janda et al. 2011]. However, in ARDS patients, right heart catheterization is more often quite difficult to perform, while echocardiography can be performed at the bedside and can provide more information on anatomical and functional cardiac abnormalities. Bearing in mind the potential limitations of echocardiography, especially in ventilated patients [Fougeres et al. 2010], serial measurements of PH and cardiac function can be performed using echocardiography, therefore allowing the monitoring of therapies and ventilatory strategy.
In ARDS, pulmonary arterial pressure has been investigated, mainly invasively, with pulmonary arterial catheterization [Squara et al. 1998; Ryan et al. 2014; Beiderlinden et al. 2006; Osman et al. 2009; Bull et al. 2010], and only a few reports assessed pulmonary systolic arterial pressure with echocardiography in patients with ALI with or without ARDS [Jardin et al. 1985; Boissier et al. 2013; Vieillard-Baron et al. 2001; Cepkova et al. 2007; Mekontso-Dessap et al. 2010] (Table 1). Clinical interpretation of these data is challenging, since definition of ARDS has changed over time [Murray et al. 1988; Bernard et al. 1994; Force et al. 2012], as well as the standard of care in ARDS with the introduction of lung-protective ventilation [The Acute Respiratory Distress Syndrome Network, 2000] and conservative fluid management [Wiedemann et al. 2006].
Table 1.
Echocardiography in ARDS.
| Number of patients | Study design | TTE/TEE | Echocardiographic findings | |||
|---|---|---|---|---|---|---|
| Jardin et al. [1985] | 23 patients requiring mechanical ventilation for acute respiratory failure | Prospective observational study | TTE | Right ventricular dysfunction (RV enlargement with abnormal contractile pattern) in 5/23 (21.7%)% | 9 patients had RV dilation with normal systolic function (9/23, 39.1%) | In all patients, LV function was normal |
| Jardin et al. [2007] | 352 patients | Prospective observational study | TTE and TEE | Incidence of acute cor pulmonale: 56% with plateau pressure > 35 cm H2O; 32%, when plateau pressure was between 27 and 35 cm H2O; 13% when plateau pressure was < 27 cm H2O |
Odds ratio of dying for an increase in plateau pressure from 18–26 to 27–35 cm H2O in patients without cor pulmonale was 1.05 (p = 0.635), it was 3.32 in patients with cor pulmonale (p < 0.034). | A clear interaction between plateau pressure and cor pulmonale was documented |
| Lung protective ventilation | ||||||
| Vieillard-Baron et al. [2001] | 75 patients | Prospective open clinical study | TEE | ACP was present in 19/75 25% | RVF reversible in survivors PaCO2 level as the sole factor independently associated with ACP |
ACP was associated with pulmonary artery hypertension |
| Page et al. 2003 | 150 patients | Retrospective study | TTE and TEE | Incidence of ACP 18% (no differences between survivors and nonsurvivors) | ||
| Cepkova et al. [2007] | 42 patients with ALI mechanically ventilated | Prospective observational cohort study | TTE | 7% had RV dysfunction | RV and sPAP dysfunction not predictive of increased mortality |
No differences in sPAP between patients who survived and those who did not. |
| Vieillard-Baron et al. [2007] | 42 severe ARDS patients treated with prone positioning | Prospective study | TEE | ACP was detected in the 50% | Prone positioning, applied for 18 h, was associated with a reduction in RV dilation | |
| Fougereset al. [2010] | 21 ARDS patients ventilated with a tidal volume of 6.0 +/– 0.5 mL/kg of predicted body weight |
Prospective study | TEE | Increasing PEEP did not affect mean arterial pulmonary pressure | ||
| Mekontso-Dessap et al. [2010] | 203 ARDS patients | Prospective study | TEE performed within 3 days after diagnosis | sPAP was higher in patients with a patent forame ovale | ||
| Boissier et al. [2013] | 226 moderate to severe ARDS | Prospective observational study | TEE performed within 3 days after the diagnosis of ARDS | ACP in 49 patients (22.5%) | The 28-day mortality rate was significantly higher in the group with cor pulmonale (60 versus 36 %, p = 0.01) ACP was an independent risk for 28-day mortality |
|
| Lhéritier et al. [2013] | 200 patients with moderate-to-severe ARDS | Prospective multicenter study | TTE and TTE | ACP was detectable in the 22.5% (TEE) pCO2 was strongly associated with ACP |
TTE showed a low sensitivity in detecting ACP in ventilated
ARDS The presence of ACP, PFO or both was not associated with outcome |
|
| Legras et al. [2015] | 195 moderate-to-severe ARDS | Prospective observational study | TEE performed within 48 hours after admission | sPAP did not differ among subgroups sPAP significantly correlated with PaCO2 |
ACP: 36 patients PFO: 21 patients ACP and PFO: 8 patients No ACP no PFO: 130 patients |
|
ACP, acute cor pulmonale; ARDS, acute respiratory distress syndrome; ALI, acute lung injury; PEEP, positive-end respiratory pressure; PFO, patent foramen ovale; Pplat, plateau pressure; RVF, right ventricular failure; sPAP, systolic pulmonary arterial pressure; TEE, transesophageal echocardiography; TTE, transthoracic echocardiography.
Fougeres and colleagues [Fougeres et al. 2010] used both echocardiography and pulmonary arterial catheterization to assess the hemodynamic impact of increasing positive-end expiratory pressure (PEEP) when tidal volume and the plateau pressure were limited in 21 ARDS patients. Pulmonary arterial pressure (mean) was measured invasively and it was not affected by increasing PEEP while this maneuver induced an increase in RV and diastolic area, and pulmonary vascular resistance.
In the era of protective ventilation, ARDS patients with ACP showed significantly higher sPAP [Vieillard-Baron et al. 2001] when compared with those without ACP (even if an adequate measurement of this parameter was easily obtained only in 22 out of 56), while no difference in sPAP was detected in patients who survived compared with those who did not [Cepkova et al. 2007]. Interestingly, in this investigation, values of sPAP reported in ACP patients (47 ± 8 mmHg) were comparable with those of ALI patients (42.1 ± 9.1 mmHg) [Cepkova et al. 2007], despite discrepancies in number consistency of the two groups (19 ACP patients versus 42 ALI patients). Similar results were reports a few years later by Boissier and colleagues [Boissier et al. 2013] who observed that sPAP was significantly higher in patients with ACP than in those without (ACP, 44 ± 20 mmHg versus no ACP, 31 ± 15 mmHg). However, in this paper RV function was not investigated, even if ACP patients showed a higher incidence of RV dilatation. In a large series of 203 ARDS patients, Mekontso-Dessap and colleagues [Mekontso-Dessap et al. 2010] observed that patients with a patent foramen ovale (PFO) [detectable in the about 20% of their population with contrast transesophageal echocardiography (TEE) as the reference method] showed a significantly higher pulmonary systolic arterial pressure in respect to those without a PFO (PFO, 43 ±17 mmHg versus no PFO, 35 ±18 mmHg, p = 0.04). Systolic arterial pressure was available only in 133 patients (65.5%). However, in 257 ARDS patients, Zhang and colleagues [Zhang et al. 2014] documented that echocardiography tended to overestimate pulmonary systolic arterial pressures in respect to right-heart catheterization in patients with atrial septal defect. Nevertheless, since the presence of PFO may worsen hypoxemia in ARDS patients, the echocardiographic assessment should rule out the presence of PFO and whenever detected (especially if moderate to severe), serial echocardiograms should be performed in order to assess sPAP and RV function in these patients.
On the other hand, in moderate-to-severe ARDS, evaluated using echocardiography within the first 48 hours after admission, sPAP was not significantly different in ACP patients (irrespective of associated PFO) when compared with the patients without PFO. This finding may be related to the fact that ACP patients showed an altered systolic RV function (as indicated by median RV fractional area contraction) . These data strongly suggest that, in clinical practice, the measurements of sPAP should always be associated with the assessment of RV function. Interestingly, in the same investigation, sPAP significantly correlated with PaCO2, a finding in agreement with the effect of PaCO2 on pulmonary vascular bed [Balanos et al. 2003].
When clinically interpreting the echocardiographic values of sPAP obtained at bedside, intensivists should also bear in mind that pulmonary arterial pressure is influenced by several factors [Price et al. 2012] which are related to the severity of lung disease (that is, changes occurring within the pulmonary vasculature, the degree of hypercapnia and hypoxia) as well as to RV function and contractility (Table 2). Moreover, mechanical ventilation itself (PEEP, tidal volume and plateau pressure) is able to influence pulmonary arterial pressure directly via changes in RV after load and indirectly via alterations in pCO2 and pH. Mekontso-Dessap and colleagues [Mekontso-Dessap et al. 2009] assessed the effects of different PEEP on RV function in patients with severe ARDS and observed that high PEEP values (which were associated with more severe hypercapnia and acidosis) were related to a lower RV stroke index. However, a multivariate analysis on changes in pH (and not in PEEP) were correlated with impaired RV function. The authors hypothesized that the reduction in RV function was due to an increase in pulmonary vascular resistance but, unfortunately, pulmonary systolic pressures were not measured; the finding of increased pulmonary arterial pressures would have supported the hypothesis that RV dysfunction was caused by RV overload.
Table 2.
Main factors influencing pulmonary arterial pressure.
| Factor | Mechanism | Effect |
|---|---|---|
| Endothelial dysfunction/imbalance of vasoactive mediators | Initiation of inflammation and intravascular coagulation. Intravascular microthrombi, fibrin, and intravascular sequestration of cells lead to pulmonary capillary occlusion, and clots |
Increased PVR |
| Hypoxia | Increased vascular tone in muscular arterioles and veins | Increased PVR |
| Atelectasia, reduction in lung volume, high PEEP | Extrinsic vessel compression | Increased PVR |
| Hypercapnia/acidosis | Increase vascular tone | Increased PVR |
| Increased LA pressure and or LV dysfunction | Pulmonary vein constriction | Post capillary pulmonary hypertension |
PEEP, peak expiratory pressure; LA, left atrial; LV, left ventricle; PVR, pulmonary vascular resistance.
RV dilatation
Assessment of RV dimension with echocardiography is mainly qualitative (due to the peculiar, complex anatomic shape of RV chamber), using a focused approach mainly based on the four-chamber and short-axis views in the transthoracic approach. [Lang et al. 2015]. Since in mechanically ventilated patients normal values for RV dimension with echocardiography have not been established [Rudski et al. 2010], it is accepted that comparison with LV size furnishes a good estimated of RV size. RV dilatation is defined as moderated when the ratio between right (RVEDA) and left-ventricular end diastolic area (LVEDA) is more than 0.6, and severe when this ratio is more than 1.0 [Boissier et al. 2013; Jardin et al. 1999; Vieillard-Baron et al. 2001; Portnoy and Rudski, 2015].
Cepkova and colleagues [Cepkova et al. 2007] assessed RV size qualitatively, according to their ‘laboratory protocol’ and, among the 42 patients with ALI included in their investigation, RV dilatation was observed in 26% (11 out of 42).
Conversely, RV dilatation was quantitatively assessed and detected in patients with ACP, indicated as RVEDA alone [Vieillard-Baron et al. 2001] or as the ratio RVEDA to LVEDA [Mekontso-Dessap et al. 2009]. In ARDS patients with a PFO, when compared with those without, Mekontso-Dessap and colleagues [Mekontso-Dessap et al. 2010] observed significant higher values of RVEDA to LVEDA ratio associated with higher sPAP and similarly, Legras and colleagues [Legras et al. 2015] reported that ARDS with ACP and PFO exhibited the highest RVEDA to LVEDA ratio, associated with RV dysfunction. Interestingly, Boissier and colleagues [Boissier et al. 2013] observed that moderate RV dilatation (defined as RV to LDVEDA ratio more than 0.6 and less than 1.0) was detectable in the 49% of patients without ACP, thus suggesting that RV dilatation may precede ACP development.
Septal dyskinesia
Septal dyskinesia is present when the interventricular septum shows a paradoxical motion, characterized by its displacement leftward at the onset of left ventricular diastole followed by a sudden return rightward when the LV resumes contraction. This phenomenon is related to interventricular dependence and is due to the fact that right ventricular systolic overload increases the duration of RV systole, which occurs when the LV begins to relax, thus reversing the left-to-right pressure gradient at end systole or onset diastole. As the interventricular septum flattens and progressively loses its convexity during diastole, the LV assumes a progressively more D-shaped cavity [Rudski et al. 2010]. The detection of paradoxical septal motion is qualitative [Repessé et al. 2012] and it is part of the definition of ACP [Jardin et al. 1997]. Speckle-tracking echocardiography can allow the assessment of the local rate of wall deformation (strain rate) and the degree of deformation (strain). However, this parameter, which describes RV function in relation to both its preload and its afterload, has not been investigated in patients with RV dysfunction and ARDS yet.
The incidence and the prognostic impact of ACP in ARDS patients has been extensively addressed in previous papers [Jardin et al. 1997; Vieillard-Baron et al. 2001, 2002, 2007; Mekontso-Dessap et al. 2009; Boissier et al. 2013; Lhéritier et al. 2013; Legras et al. 2015] so will not be discussed extensively in the present review. ACP is defined as the association of RV dilatation with a paradoxical septal motion at end systole [Repessé et al. 2015]. Briefly, in the era of protective ventilation, ACP occurs in the 20–25% of ARDS patients and its development seems to be especially related to plateau pressure, driving pressure and pCO2 [Repessé et al. 2015]. The presence of ACP may cause or precipitate circulatory failure and it seems to have an impact on prognosis since it presented as an independent risk factor for 28-day mortality in moderate-to-severe ARDS patients [Boissier et al. 2013]. In 226 ARDS patients, ACP was associated with lower systolic and mean arterial pressures, a higher heart rate and a higher incidence of shock [Boissier et al. 2013]. In another study including 200 ARDS patients, 64% of patients with ACP required norepinephrine infusion, compared with 49% of patients without ACP [Lhéritier et al. 2013]. Based on the echocardiographic findings on ACP in ARDS patients and its clinical meaning, it has been proposed as an approach to protect the RV by setting or adapting the ventilatory strategy in the presence of the echocardiographic finding of RV overload [Jardin et al. 1997; Vieillard-Baron et al. 2001, 2002, 2007; Mekontso-Dessap et al. 2009, 2011; Boissier et al. 2013; Lhéritier et al. 2013; Legras et al. 2015; Repessé et al. 2015]. Though this ‘protective RV approach’ (avoidance of intrinsic PEEP, limiting plateau pressure, PEEP and permissive hypercapnia as feasible, without compromising protective lung ventilation strategy) has to be validated in a randomized controlled trial, it seems to protect both the lung and the ventricle by an individual patient-tailored strategy. In this context, in ARDS patients, it is now recommended to perform at least one echocardiographic examination per day during the first three days to evaluate RV function and to adapt the ventilator.
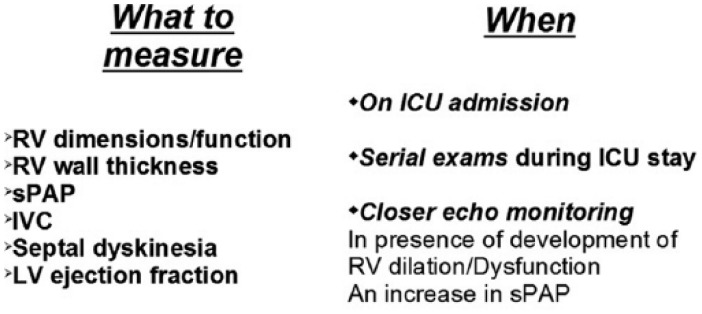
Figure 1.
Flow chart.
RV, right ventricle; IVC, inferior vena cava; sPAP, pulmonary systolic arterial pressure; LV, left ventricle; ICU, intensive care unit.
Overall, according to the available evidence on echocardiographic findings in patients with ALI/ARDS, the following considerations can be drawn.
Echocardiography (transthoracic and transesophageal) has a growing role in the management ARDS patients, mainly because of the strict interactions between the lung (and ventilation) and the RV and pulmonary circulation. These two techniques are not completely interchangeable. The choice of one instead of the other is usually made on the acoustic windows (i.e. TEE is performed because of the absence of transthoracic windows) as well as on the clinical needs (i.e. TEE is needed for the detection of a PFO). However, both techniques should be performed together in peculiar clinical settings such as venovenous extracorporeal membrane oxygenation implantation to optimize echocardiographic views [Peris et al. 2015].
The detection of ACP should make intensivists critically evaluate the possibility of tailoring their ventilatory strategy to the individual patient depending on the echocardiography findings.
It may be suggested that there is a continuum of alterations in RV size and function and pulmonary circulation which may end in the development of ACP, probably paralleling ARDS disease severity. The findings by Boissier and colleagues [Boissier et al. 2013] strongly support this assumption. In fact, in their paper, moderate pulmonary dysfunction (defined as the presence of pulmonary dysfunction or isolated RV dilatation without ACP) was detected in 48% of patients and a progressive increase in mortality was observed with an increase in pulmonary dysfunction severity.
Bearing in mind the clinical role and growing importance of echocardiography in ARDS and the available evidence on this topic, we present a flow chart (mainly based on the protocol used at our institute [Peris et al. 2015; Cianchi et al. 2011], including the parameters measured at echocardiography examination (What to measure) and the timing of echo exams (When) in ARDS patients (Table 3).
Table 3.
Main echocardiographic parameters for the right ventricle.
| View | Normal values |
|---|---|
| RV dimensions | |
| RV-focused four apical chamber view | Base: < 41 mm Midlevel: < 35 mm |
| RV area | |
| Manual tracing of RV endocardial border from the lateral
tricuspid annulus along the free wall to the apex and back to
medial tricuspid annulus, along the interventricular septum at end-diastole and at end-systole |
RV EDA indexed to BSA (cm2/m2) Men normal range 5–12.6 Women normal range 4.5–11.5 RV ESA indexed to BSA (cm2/m2) Men normal range 2.0–7.4 Women normal range 1.6–6.4 |
| RV wall thickness | |
| Linear measurement of RV free wall thickness performed at end-diastole, below the tricuspid annulus at a distance approximating the length of anterior tricuspid leaflet, when it is fully open and parallel to the RV free wall. | Normal value: < 5 mm |
| TAPSE tricuspid annular plane systolic excursion | |
| Tricuspid annular longitudinal excursion is measured by M-mode by proper alignment of M-mode cursor with the direction of RV longitudinal excursion from apical view | 24 ± 3.5 mm Abnormal < 15 mm |
| Systolic (S’) wave velocity | |
| It is obtained by pulsed wave DTI (cm/s), from the apical approach, in the view that achieves parallel alignment of Doppler beam with RV free wall longitudinal excursion | 14.1 ± 2.3 cm/s Abnormal: < 9.5 cm/s |
| Right ventricle outflow tract acceleration time | |
| By positioning the sample volume at the center of the pulmonary artery (ideally at the annulus) in the short-axis view | Abnormal < 105 ms |
DTI, Doppler tissue imaging; RV, right ventricle.
What to use
The choice of the modality of echocardiograhy (transthoracic versus transesophageal) strictly depends on the clinical condition of individual patients as well as on the clinical inquiry. In ventilated patients, TEE is to be preferred since it overcomes technical problems with acoustic views and measurements can usually be easily performed [Jardin et al. 1997; Vieillard-Baron et al. 2001, 2002, 2007; Mekontso-Dessap et al. 2009, 2011; Boissier et al. 2013; Lhéritier et al. 2013; Legras et al. 2015; Repessé et al. 2015]. Whenever the patient is spontaneously breathing with or without noninvasive ventilation, transthoracic echocardiography (TTE) is more feasible and in many cases can provide enough information to meet the clinical inquiries [Joseph et al. 2004; Howard et al. 2012].
What to measure
According to existing evidence and to our experience, the following parameters (mainly focused on RV and pulmonary circulation) should also be measured in a patient with ALI/ARDS. These parameters have been selected on the basis of their feasibility (that is, easy to be measured, even in a short time), and of the existing literature data (that is, clinical significance documented in previous reports).
RV dimensions
RV size can be assessed visually by the ‘eyeball’ method in the short axis and four-chamber views, but it can be quantitatively evaluated by the ratio RV to LV end-diastolic area. The RV to LV area ratio is measured at end diastole by tracing the areas of the two chambers in the apical four-chamber view on TTE or the midesophageal four-chamber view on TEE [Jardin et 1997; Khrishnan and Schmidt, 2015]. According to recent guidelines [Lang et al. 2015], RV dimensions are best estimated by a RV-focused apical four-chamber view and RV dilatation is identified by a diameter of more than 41 mm at the base and more than 35 mm at the midlevel.
RV wall thickness
This measurement is easily performed in diastole, preferably from the subcostal view, using either M-mode or two-dimensional imaging [Rudski et al. 2010]. Thickness of more than 5 mm indicates RV hypertrophy. In a patient with ARDS evaluated for the first time on ICU admission, the detection of RV thickness of more than 5 mm may have indicated a chronic RV overload (i.e. in the presence of previously unknown chronic obstructive pulmonary disease). Otherwise, since the RV is able in only a few days to thicken in response to an increase in pulmonary pressure, RV hypertrophy may develop under mechanical ventilation and it may be detected on serial echo exams. In fact, Vieillard-Baron and colleagues [Vieillard-Baron et al. 2002] described a moderate thickness of the right ventricular free wall after two days of mechanical ventilation. The detection of severe RV hypertrophy (more than 1 cm) is thought to be related to pre-existing chronic diseases.
Pulmonary systolic arterial pressure
As discussed above, in presence of tricuspid regurgitation, the RV-right atrial pressure gradient can be estimated by measuring the peak regurgitant jet velocity (v) using continuous-wave Doppler echocardiography and the modified Bernoulli equation (RV systolic pressure = 4v2 + right atrial pressure) [Jardin et al. 1997; Khrishnan and Schmidt, 2015].
Inferior vena cava diameter
Inferior vena cava (IVC) and its collapse: It can be used as a good estimated of right atrial (RA) pressure in nonventilated patients (in whom central venous pressure is preferred) [Vieillard-Baron et al. 2002]. The subcostal view is most useful for imaging the IVC, making it visible in its long axis. IVC diameter of less than 2.1 cm that collapses more than 50% with a sniff suggests a normal RA pressure of 3 mmHg (range, 0–5 mmHg), whereas an IVC diameter of more than 2.1 cm that collapses less than 50% with a sniff suggests a high RA pressure of 15 mmHg (range, 10–20 mmHg) [Brennan et al. 2007]. In patients with RV dysfunction, the interpretation of IVC collapsibility is more challenging and it should be interpreted, taking into account its trend and central venous pressure.
Septal dyskynesia
Septal dyskynesia has been discussed previously. In patients with pulmonary embolism, acute RV overload may be associated with a specific pattern, the so called ‘McConnell’s sign’, which is characterized by abnormal regional wall motion with akinesia of the mid-free wall, while simultaneously having normal or increased motion at the apex [McConnell et al., 1996; Vieillard-Baron et al. 2002].
Tricuspid lateral annular motion
Tricuspid annular plane systolic excursion (TAPSE) is used as an index of RV function. Since the RV contracts largely along its length, M-mode imaging through the lateral tricuspid valve plane captures this longitudinal motion [Vieillard-Baron et al. 2002; Portnoy and Rudski, 2015]. This measurement requires a proper alignment of M-mode cursor with the direction of RV longitudinal excursion from the apical view. Angle dependence is therefore one of its main limitations, together with the fact that TAPSE is not representative of global RV function [Lang et al. 2015]. However, this parameter has shown a good correlation with RV fractional area change and radionuclide-derived RV ejection fraction [Kaul et al. 1984]. Obviously, interpreting TAPSE as an index of RV function assumes that RV basal segment is representative of global function. A TAPSE of more than 15 mm indicates RV dysfunction [Vieillard-Baron et al. 2002; Portnoy and Rudski, 2015; Khrishnan and Schmidt, 2015], and it has been associated with a poor prognosis in patients with chronic right-sided heart disease [Forfia et al. 2006; Damy et al. 2012] and in critically ill patients [Gajanana et al. 2015]. A strong relation between TAPSE and LV ejection fraction has been reported in 86 critically ill patients admitted to ICU for acute respiratory failure, circulatory failure or coma [Lamia et al. 2007]. In a multicenter, noninvasive hemodynamic study including 195 patients with moderate-to-severe ARDS, ACP was associated with a reduced RV function, as indicated by lower values of TAPSE and RV fractional area change [Legras et al. 2015].
Left ventricle
When evaluating patients with ARDS with echocardiography, LV ejection fraction should also be assessed and clinically interpreted taking into account also the dosage of inotropic drugs, if administered. Valvular diseases (mitral and aortic) should also be investigated and, if present, estimated, especially when examining the patient using echocardiography for the first time. The presence of valvular disease (i.e. mitral regurgitation) could influence the course and severity of the lung disease and therefore it will influence treatments (i.e. fluid prescription). Moreover, LV diastolic dysfunction (even in presence of normal ejection fraction) can contribute to increased pulmonary arterial pressures and to the development of RV dysfunction.
When using TEE, the following parameters can also be checked: Superior vena cava collapse (absent or present), filling pressures (low, normal, or high), and shunting across PFO (absent or present). Moreover, since patients with severe ARDS often require prolonged periods of the prone position because of refractory hypoxemia, TEE can thus be safely and efficiently performed.
When to perform echo cardiogram
According to our experience, we suggest that echocardiography should be performed on ICU admission in patients with ALI or ARDS and should be periodically repeated according to the clinical course. On admission, an echocardiogram is able to provide valuable information, not only on the clinical status of that moment but may also highlight clinical elements indicating previous diseases (i.e. severe RV hypertrophy, suggesting pre-existing chronic lung disease). If the clinical course is uneventful, echocardiograms should be done at least once a week (i.e. to monitor fluid therapy), before weaning off ventilation and after extubation. The patients should be re-evaluated with TTE or TEE any time higher ventilatory parameters are required to maintain adequate oxygenation or any new, undifferentiated state of shock develops, including hyperlactatemia, acidosis, oliguria or other signs of hypoperfusion. In the presence of progressive respiratory failure, the echocardiographic evaluation could help in identifying the reasons (or cofactors) such as increased sPAP, the development of RV dilatation, progressive RV or LV failure and in tailoring the treatment. Whenever RV dilatation or dysfunction is detected (even at an echocardiogram performed routinely), treatments (ventilatory and nonventilatory) should be re-examined; other options (i.e. inhaled nitric oxide and prone position) should be considered and patients should be more closely monitored by use of echocardiography .
Other echocardiographic parameters (such as systolic wave velocity) have thus far not been fully investigated in ALI and ARDS, and therefore they have not been discussed in detail in the present review. Systolic (S’) wave velocity is a measure of myocardial contraction (though it cannot be representative of global RV function) and, similarly to TAPSE, it is load dependent. Right ventricle outflow tract (RVOT) acceleration time may be used when the tricuspid velocity cannot be measured and a value of less than 105 msec is suggestive of PH. In an elegant investigation, Arkles documented that the differences the RV Doppler velocity pattern identified marked differences in pulmonary vascular characteristics, and could help in establishing the hemodynamic basis for PH [Arkles et al. 2011]. In particular, a ‘notched’ Doppler signal strongly suggested an increased pulmonary vascular resistance and poor vascular compliance, while the absence of a ‘notched’ pattern was typically associated with the absence of pulmonary vascular disease, and with PH of pulmonary venous origin. Also, the pulmonary vascular resistance can be calculated with echocardiography, that could be part of the comprehensive assessment in patients with RV dysfunction [Abbas et al. 2003] but no data are yet available at this time in ARDS patients.
Overall, the echocardiographic examination is practical and feasible in ARDS patients, and is able to provide valuable information for their management.
However, despite the important progress that echocardiography has made in the evaluation of patients with ARDS, several open questions remain and echocardiography still appears to be underused (or at least not routinely used) in these patients. In other words, a more systematic use of echocardiography (mainly through shared protocols) in ARDS could help intensivists tailor the optimal treatment in individual patients as well as highlight limits and potentials of this methodology in patients with ALI.
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Conflict of interest statement: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Chiara Lazzeri, Intensive Care Unit of Heart and Vessels Department, University of Florence, AOU Careggi, Fondazione Don Carlo Gnocchi IRCCS, viale Morgagni 8550134, Florence, Italy.
Giovanni Cianchi, Intensive Care Unit and Regional ECMO Referral Center, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy.
Manuela Bonizzoli, Intensive Care Unit and Regional ECMO Referral Center, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy.
Stefano Batacchi, Intensive Care Unit and Regional ECMO Referral Center, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy.
Adriano Peris, Intensive Care Unit and Regional ECMO Referral Center, Azienda Ospedaliero-Universitaria Careggi, Florence, Italy.
Gian Franco Gensini, Intensive Care Unit of Heart and Vessels Department, University of Florence, AOU Careggi, Fondazione Don Carlo Gnocchi IRCCS, Florence, Italy.
References
- Abbas A., Fortuin D., Schiller N., Appleton C., Moreno C., Lester S. J., et al. (2003) A simple method for noninvasive estimation of pulmonary vascular resistance. J Am Coll Cardiol 19: 1021–1027. [DOI] [PubMed] [Google Scholar]
- Arkles J., Opotowsky A., Ojeda J., Rogers F., Liu T., Prassana V., et al. (2011) Shape of the right ventricular Doppler envelope predicts hemodynamics and right heart function in PH. Am J Respir Crit Care Med 183: 268–276. [DOI] [PubMed] [Google Scholar]
- Balanos G., Talbot N., Dorrington K., Robins P. (2003) Human pulmonary resistance vascular response to 4 hours of hypercapnia and hypocapnia measured using Doppler echocardiography. J Appl Physiol 94: 1543–1551. [DOI] [PubMed] [Google Scholar]
- Beiderlinden M., Kuehl H., Boes T., Peters J. (2006) Prevalence of PH associated with severe ARDS: predictive value of computed tomography. Intensive Care Med 32: 852–857. [DOI] [PubMed] [Google Scholar]
- Bernard G., Artigas A., Brigham K., Carlet J., Falke K., Hudson L., et al. (1994) The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med 149: 818–824. [DOI] [PubMed] [Google Scholar]
- Boissier F., Katsahian S., Razazi K., Thille A., Roche-Campo F., Leon R., et al. (2013) Prevalence and prognosis of cor pulmonale during protective ventilation for ARDS. Intensive Care Med 39: 1725–1733. [DOI] [PubMed] [Google Scholar]
- Bouferrache K., Vieillard-Baron A. (2011) ARDS, mechanical ventilation, and right ventricular function. Curr Opin Crit Care 17: 30–35. [DOI] [PubMed] [Google Scholar]
- Brennan J., Blair J., Goonewardena S., Shah D., Vasaiwala S., Kirkpatrick J., et al. (2007) Re-appraisal of the use of inferior vena cava for estimating right atrial pressure. J Am Soc Echocardiogr 20: 857–861. [DOI] [PubMed] [Google Scholar]
- Bull T., Clark B., McFann K., Moss M. (2010) Pulmonary vascular dysfunction is associated with poor outcomes in patients with ALI. Am J Respir Crit Care Med 182: 1123–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caille V., Vieillard-Baron A. (2010) The RV During the ARDS revisited by echocardiography. The Open Nuclear Medicine Journal 2: 119–124. [Google Scholar]
- Cepkova M., Kapur V., Ren X., Quinn T., Zhuo H., Foster E., et al. (2007) Pulmonary dead space fraction and pulmonary artery systolic pressure as early predictors of clinical outcome in ALI. Chest 132: 836–842. [DOI] [PubMed] [Google Scholar]
- Chiumello D., Pesenti A. (2013) The monitoring of ACP is still necessary in ‘Berlin’ ARDS patients. Intensive Care Med. 39: 1864–1866. [DOI] [PubMed] [Google Scholar]
- Cianchi G., Bonizzoli M., Pasquini A., Bonacchi M., Zagli G., Ciapetti M., et al. (2011) Ventilatory and ECMO treatment of H1N1-induced severe respiratory failure: results of an Italian referral ECMO center. BMC Pulm Med 11: 2 DOI: 10.1186/1471-2466-11-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Damy T., Kallvikbacka-Bennett A., Goode K., Khaleva O., Lewinter C., Hobkirk J., et al. (2012) Prevalence of, associations with, and prognostic value of tricuspid annular plane systolic excursion (TAPSE) among outpatients referred for the evaluation of heart failure. J Card Fail 18: 216–225. [DOI] [PubMed] [Google Scholar]
- Fisher M., Forfia P., Chamera E., Housten-Harris T., Champion H., Girgis R. E., et al. (2009) Accuracy of Doppler echocardiography in the hemodynamic assessment of PH. Am J Respir Crit Care Med 179: 615–621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Force A., Ranieri V., Rubenfeld G., Thompson B., Ferguson N., Caldwell E., et al. (2012) ARDS: the Berlin Definition. JAMA 307: 2526–2533. [DOI] [PubMed] [Google Scholar]
- Forfia P., Fisher M., Mathai S., Housten-Harris T., Hemnes A., Borlaug B., et al. (2006) Tricuspid annular displacement predicts survival in PH. Am J Respir Crit Care Med 174: 1034–1041. [DOI] [PubMed] [Google Scholar]
- Fougeres E., Teboul J., Richard C., Osman D., Chemla D., Monnet X. (2010) Hemodynamic impact of a PEEP setting in ARDS: Importance of the volume status. Crit Care Med 38: 802–807. [DOI] [PubMed] [Google Scholar]
- Gajanana D., Rammohan H., Alli O., Romero-Corral A., Purushottam B., Pomamgi S., et al. (2015) Tricuspid annular Plane Systolic Excursion and its association with mortality in critically ill patient. Echocardiography 32: 1222–1227. [DOI] [PubMed] [Google Scholar]
- Galié N., Hoeper M., Humbert M., Torbicki A., Vachiery J., Barbera J., et al. (2009) Guidelines for the diagnosis and treatment of PH. Eur Respir J 34: 1219–1263. [DOI] [PubMed] [Google Scholar]
- Howard L., Grapsa J., Dawson D., Bellamy M., Chambers J., Masanic N., et al. (2012) Echocardiographic assessment of PH: standard operating procedure. Eur Respir Rev 21: 239–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janda S., Shahidi N., Gin K., Swiston J. (2011) Diagnostic accuracy of echocardiography for PH: a systematic review and meta-analysis. Heart 97: 612–622. [DOI] [PubMed] [Google Scholar]
- Jardin F., Dubourg O., Bourdarias J. (1997) Echocardiographic pattern of ACP. Chest 111: 209–217. [DOI] [PubMed] [Google Scholar]
- Jardin F., Fellahi J., Beauchet A., Vieillard-Baron A., Loubieres Y., Page B. (1999) Improved prognosis of ARDS 15 years on. Intensive Care Med 25: 936–941. [DOI] [PubMed] [Google Scholar]
- Jardin F., Gueret P., Dubourg O., Farcot J., Margairaz A., Bourdarias J. (1985) Two-dimensional echocardiographic evaluation of right ventricular size and contractility in acute respiratory failure. Crit Care Med 13: 952–956. [DOI] [PubMed] [Google Scholar]
- Jardin F., Vieillard-Baron A. (2007) Is there a safe plateau pressure in ARDS? The right heart only knows. Intensive Care Med 33: 444–447. [DOI] [PubMed] [Google Scholar]
- Joseph M., Disney P., Da Costa R., Hutchison S. (2004) Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest 126: 1592–1597. [DOI] [PubMed] [Google Scholar]
- Kaul S., Tei C., Hopkins J., Shah P. (1984) Assessment of right ventricular function using two-dimensional echocardiography. Am Heart J 107: 526 –531. [DOI] [PubMed] [Google Scholar]
- Khrishnan S., Schmidt G. (2015) Acute right ventricular dysfunction. A real-time management with echocardiography. Chest 147: 835–846. [DOI] [PubMed] [Google Scholar]
- Lang R., Badano L., Mor-Avi V., Afilalo J., Armstrong A., Ernarnde L., et al. (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28: 1–39. [DOI] [PubMed] [Google Scholar]
- Lamia B., Teboul J., Monnet X., Richard C., Chemia D. (2007) Relationship between the tricuspid annular plane systolic excursion and right and left ventricular function in critically ill patients. Intensive Care Med 33: 2143–2149. [DOI] [PubMed] [Google Scholar]
- Legras A., Caille A., Begot E., Lhéritier G., Lherm T., Mathonnet A., et al. (2015) ARDS-associated ACP and PFO: a multicenter noninvasive hemodynamic study. Critical Care 19: 174 DOI: 10.1186/s13054-015-0898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lhéritier G., Legras A., Caille A., Lherm T., Mathonnet A., et al. (2013) Prevalence and prognostic value of ACP and PFO in ventilated patients with early ARDS: a multicenter study. Intensive Care Med 39: 1734–1742. [DOI] [PubMed] [Google Scholar]
- McConnell M., Solomon S., Rayan M., Come P., Glodhaber S., Lee R. T., et al. (1996) Regional right ventricular dysfunction detected by echocardiography in acute pulmonary embolism. Am J Cardiol 78: 469–473. [DOI] [PubMed] [Google Scholar]
- McQuillan B., Picard M., Leavitt M., Weyman A. (2001) Clinical correlates and reference intervals for pulmonary artery systolic pressure among echocardiographically normal subjects. Circulation 104: 2797–2802. [DOI] [PubMed] [Google Scholar]
- Mayo P., Mekontso-Dessap A., Vieillard-Baron A. (2015) Myths about critical care echocardiography: the ten false beliefs that intensivists should understand. Intensive Care Med. DOI 10.1007/s00134-014-3622-z. [DOI] [PubMed] [Google Scholar]
- Mekontso-Dessap A., Boissier F., Leon R., Carreira S., Roche-Campo F., Lemaire F., et al. (2010) Prevalence and prognosis of shunting across PFO during ARDS. Crit Care Med 38: 1786–1792. [DOI] [PubMed] [Google Scholar]
- Mekontso-Dessap A., Charron C., Devaquet J., Aboab J., Jardin F., Brochard L., et al. (2009) Impact of acute hypercapnia and augmented PEEP on RV function in severe ARDS. Intensive Care Med 35: 1850–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mekontso-Dessap A., Proost O., Boissier F., Louis B., Roche-Campo F., Brochard L. (2011) TEE in prone position during severe ARDS. Intensive Care Med 37: 430–434. [DOI] [PubMed] [Google Scholar]
- Murray J., Matthay M., Luce J., Flick M . (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138: 720–723. [DOI] [PubMed] [Google Scholar]
- Osman D., Monnet X., Castelain V., Anguel N., Warszawski J., Teboul J., et al. (2009) Incidence and prognostic value of right ventricular failure in ARDS. Intensive Care Med 35: 69–76. [DOI] [PubMed] [Google Scholar]
- Peris A., Lazzeri C., Cianchi G., Bonizzoli M., Batacchi S., Bernardo P., et al. (2015) Clinical Significance of echocardiography in patients supported by venous-venous extracorporeal membrane oxygenation. Journal of Artificial Organs 18: 99–105. [DOI] [PubMed] [Google Scholar]
- Portnoy S., Rudski L. (2015) Echocardiographic evaluation of the RV: a 2014 perspective. Curr Cardiol Rep 17: 21. [DOI] [PubMed] [Google Scholar]
- Price L., McAuley D., Marino P., Finney S., Griffiths M., Wort S. (2012) Pathophysiology of pulmonary hypertension in ALI. Am J Physiol Lung Cell Mol Physiol 302: L803–L815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Repessé X., Charron C., Vieillard-Baron A. (2012) Right ventricular failure in ALI and ARDS. Minerva Anestesiol 78: 941–948. [PubMed] [Google Scholar]
- Repessé X., Charron C., Vieillard-Baron A. (2015) ACP in ARDS: rationale for protecting the RV. Chest. 147: 259–265. [DOI] [PubMed] [Google Scholar]
- Rudski L., Lai W., Afilalo J., Hua L., Handschumacher M., Chandrasekaran K., et al. (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography. J Am Soc Echocardiogr 23: 685–713. [DOI] [PubMed] [Google Scholar]
- Ryan D., Frohlich S., McLoughlin P. (2014) Pulmonary vascular dysfunction in ARDS. Annals of Intensive Care 4: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonneau G., Robbins I., Beghetti M., Channick R., Delcroix M., Denton C., et al. (2009) Updated clinical classification of PH. J Am Coll Cardiol 54: S43–S54. [DOI] [PubMed] [Google Scholar]
- Squara P., Dhainaut J., Artigas A., Carlet J. (1998) Hemodynamic profile in severe ARDS: results of the European Collaborative ARDS Study. Intensive Care Med 24: 1018–1028. [DOI] [PubMed] [Google Scholar]
- The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for ALI and the ARDS. N Engl J Med 342: 1301–1308. [DOI] [PubMed] [Google Scholar]
- Vieillard-Baron A. (2009) Assessment of right ventricular function. Curr Opin Crit Care 15: 254–260. [DOI] [PubMed] [Google Scholar]
- Vieillard-Baron A., Charron C., Caille V., Belliard G., Page B., Jardin F. (2007) Prone positioning uploads the RV in severe ARDS. Chest 132: 1440–1446. [DOI] [PubMed] [Google Scholar]
- Vieillard-Baron A., Price L., Matthay M. (2013) ACP in ARDS. Intensive Care Med 39: 1836–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vieillard-Baron A., Prin S., Chergui K., Dubourg O., Jardin F. (2002) Echo-Doppler demonstration of ACP at the bedside in the medical intensive care unit. Am J Respir Crit Care Med 166: 1310–1319. [DOI] [PubMed] [Google Scholar]
- Vieillard-Baron A., Schmitt J., Augarde R., Fellahi J., Prin S., Page B., et al. (2001) ACP in ARDS submitted to protective ventilation: incidence, clinical implications, and prognosis. Crit Care Med 29: 1551–1555. [DOI] [PubMed] [Google Scholar]
- Wiedemann H., Wheeler A., Bernard G., Thompson B., deBoisblanc B., et al. (2006) National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Clinical Trials Network. Comparison of two fluid-management strategies in ALI. N Engl J Med 354: 2564–2575. [DOI] [PubMed] [Google Scholar]
- Zhang C., Huang T., Huang X., Huang Y., Chen J., Chen J., et al. (2014) Inaccuracy of Doppler echocardiographic estimates of pulmonary arterial pressures in adult atrial septal defect patients with pulmonary arterial hypertension. Chin Med J (Engl) 127: 33389–33395. [PubMed] [Google Scholar]
- Zapol W., Snider M. (1977) PH in severe acute respiratory failure. N Engl J Med 296: 476–480. [DOI] [PubMed] [Google Scholar]