Abstract
The authors hypothesize that consumption of interesterified fats may be the cause of the continuous increase in cardiovascular deaths in the United States which began in 2011. Interesterification is a method of producing solid fats from vegetable oil and began to supplant partial hydrogenation for this purpose upon recognition of the danger of trans fats to cardiovascular health. Long, straight carbon chains, as are present in saturated and trans fatty acids, decrease the fluidity of the erythrocyte cell membrane, which decreases erythrocyte deformability and increases blood viscosity. This decrease in cell membrane fluidity is caused by increased van der Waals interactions, which also solidify dietary fats. Elevated blood viscosity is favored as the pathogenic mechanism by which trans fats increase cardiovascular mortality because changes in lipoprotein levels do not account for all the mortality attributable to their consumption. The rapid changes in cardiovascular mortality noted with the introduction and withdrawal of trans fats from the food supply are reviewed. The evidence implicating elevated blood viscosity in cardiovascular disease is also reviewed. Data regarding the production and consumption of interesterified fats in the US should be released in order to determine if there is an association with the observed increase in cardiovascular deaths.
Keywords: blood, deformability, erythrocyte, interesterification, lipids, trans, triglycerides, viscosity
Introduction
The United States (US) Food and Drug Administration (FDA) initially expressed concern about the safety of trans fats in 1999. Subsequently, the US consumption of trans fats decreased 78% between 2003 and 2012. They are scheduled to be almost entirely removed from the US food supply by 2018.1 Trans fats are produced by partially hydrogenating liquid vegetable oils in order to produce solid fats. Interesterification is an alternative method of producing solid fats which does not generate trans fats. In this process, fatty acids are recombined between two different triglycerides, generating a variety of products with different melting points (Figure 1). Random interesterification can result in the unnatural placement of saturated fats in the second (sn-2) position of the glycerol backbone, which is usually occupied by an unsaturated fatty acid in vegetable oils.2 Interesterified triglycerides do not increase lipoprotein levels, and for this reason are considered to be safe.3
Figure 1.

Interesterification. In this example, enzymatic catalysis results in the transfer of fatty acids involving the sn-1,3 positions of the glycerol backbone. Chemical interesterification can result in the random transfer of fatty acids and involve the sn-2 position. Figure courtesy of Teledork at English Wikipedia.
Following continuous declines from 1985 to 2011, deaths from heart disease in the US increased 3% between 2011 and 2014.4 Although quantitative data about the production and consumption of interesterified triglycerides are not public knowledge, the temporal association between their presumably increased consumption as a replacement for trans fats and the increase in deaths from heart disease should raise concern about their safety. The brief interval between both the introduction and removal of trans fatty acids from the food supply and subsequent changes in cardiovascular mortality show that dietary fats can have an acute effect on coronary artery disease. Epidemiologic data, the physical chemistry of lipid bilayers, and the principles of hemorheology strongly suggest that the bulk of excess mortality due to dietary fats, including interesterified fats, is caused by elevated blood viscosity, not changes in lipoprotein levels.
Dietary fats can have an acute effect on cardiovascular mortality
Industrial trans fatty acids were introduced into the US food supply in 1911. One year later, the first diagnosis of myocardial infarction in a living patient was reported in the Journal of the American Medical Association. The death rate due to heart disease in the US rose from the 1920s until the late 1960s.5 Production and consumption of trans fats in the US also peaked in the 1960s.6
Similar changes occurred after trans fats were introduced in the United Kingdom (UK) in 1909. Sir James Mackenzie, the ‘father of cardiology in the UK,’ first mentioned angina in the third edition of his book Diseases of the Heart published in 1913. Deaths due to heart disease began to increase in England and Wales between 1922–1924 and peaked in the UK in 1970.7
Compared with their introduction and gradual dissemination, the acute effect of trans fats on mortality is better seen when they are abruptly removed from the food supply. In the three years after Denmark limited trans fat content to 2% of total fats, mortality due to cardiovascular disease dropped by an average of 14.2 per 100,000 people per year.8 After three years of restricting trans fat use in certain counties of New York state in the US, there was an additional 6.2% decrease beyond temporal trends in hospital admissions for myocardial infarction and stroke [95% confidence interval (CI), −9.2% to −3.2%, p < 0.001].9
Changes in lipoprotein levels do not account for the increased mortality associated with trans fats
Based solely on their impact on lipoprotein levels, trans fatty acids were estimated to cause 30,000 deaths due to myocardial infarction in the US annually. Epidemiologic data, however, suggested a number closer to 100,000.6 This discrepancy suggests that increased lipoprotein levels do not account for all the excess mortality.6 In another study, the association between trans fats and initial myocardial infarction remained strong after statistically controlling for lipoprotein levels, further suggesting that trans fatty acids have adverse effects beyond raising lipoprotein levels.10
Solid dietary fats, whether from partial hydrogenation or interesterification, increase blood viscosity
Partial hydrogenation of the cis bonds in unsaturated fats converts them to trans bonds, straightening their carbon chains. Saturated fatty acids naturally have straight carbon chains (Figure 2). Straight fatty acids can be tightly packed, increasing van der Waals interactions and raising their melting point, solidifying long-chain fatty acids at 37oC. Van der Waals interactions result from a momentary asymmetry in the electron cloud surrounding an atom, which induces a transient, focal charge called a ‘dipole.’ This induces a dipole in any nearby electron clouds, resulting in a weak attraction. The effect of increased van der Waals interactions on melting point is seen in stearic acid, an 18-carbon saturated fatty acid with a melting point of 63.9oC and elaidic acid, an 18-carbon trans fat with a melting point of 45oC. In contrast, linoleic acid, an 18-carbon cis unsaturated fat, melts between 13–14oC and is liquid at 37oC. Increased van der Waals attractions also makes the melting point of long-chain saturated fatty acids higher than those with shorter chains.
Figure 2.
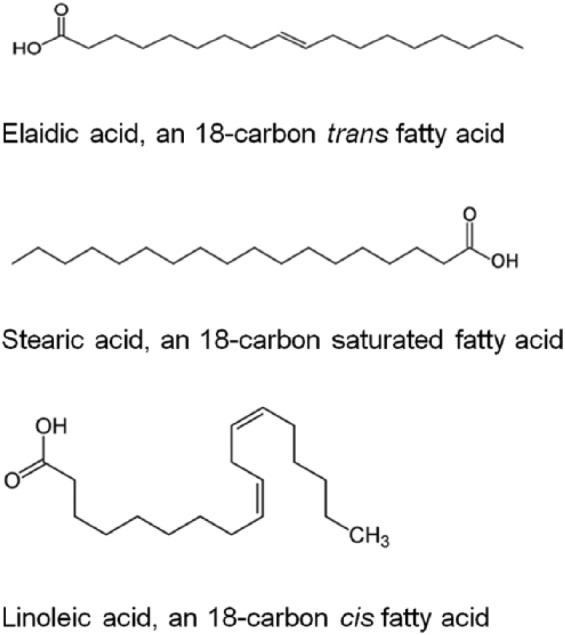
Structural formulae of 18-carbon fatty acids. The straight configuration of trans and saturated fatty acids allows them to be tightly packed in the erythrocyte plasma membrane, which maximizes van der Waals interactions and raises their melting point. Cis double bonds cause bends in the carbon chain, preventing close packing, decreasing van der Waals interactions and lowering the melting point of linoleic acid.
When dietary trans and long-chain saturated fatty acids are incorporated into an erythrocyte lipid bilayer, it stiffens just as liquid vegetable oils do (Figure 3). The effect of long-chain saturated and trans fatty acids on the erythrocyte plasma membrane fluidity are similar.11 Normal erythrocytes are the most deformable biomaterial.12 This allows erythrocytes to reversibly deform when blood velocity increases during systole, decreasing their surface area, resistance to flow, and lowering blood viscosity. Erythrocytes are the most numerous cell type in the body, numbering in the many trillions. Trillions of small decreases in deformability in otherwise extraordinarily deformable erythrocytes increases blood viscosity and resistance to flow. This necessitates increased driving pressure to cause blood flow. The effect of dietary fatty acids on erythrocyte membrane fluidity,13,14 blood viscosity,15 and blood pressure16 have been confirmed experimentally. The World Health Organization (WHO) has recognized the role of increased consumption of saturated fats and elevated blood viscosity in the pathogenesis of hypertension. According to the WHO website, “Saturated fat appears to influence blood viscosity. A higher proportional intake of fatty acids from polyunsaturated sources (linoleic acid and alpha-linolenic acids), compared with saturated fats, is associated with a lower risk of developing hypertension.”17
Figure 3.

The effect of bends in the carbon chains of fatty acids on lipid bilayer fluidity. The top lipid bilayer is composed entirely of triglycerides with saturated and trans fatty acids. The linear configuration of these carbon chains allows tight-packing. This maximizes van der Waals interactions and stiffens the plasma membrane. The lower lipid bilayer contains triglycerides with cis double bonds, which cause bends in carbon chains. This prevents close packing of triglycerides, increasing membrane fluidity. Figure courtesy of Wikimedia Commons.
Elevated blood viscosity increases cardiovascular mortality by promoting thrombosis
The viscosity of blood increases when blood flow decreases because erythrocytes return to their original shape, and form aggregates. This increased viscosity decreases flow and promotes thrombosis. Deep vein thrombosis of the lower extremities is an example of decreased flow causing thrombosis. Arterial thrombosis due to increased blood viscosity is the most common cause of death in polycythemia vera. Thus, while many studies show that lowering low-density lipoprotein cholesterol (LDL-C) with statin therapy decreases cardiovascular morbidity and mortality, increased blood viscosity may explain the excess mortality caused by dietary fats more completely than lipoprotein levels. Although epidemiologic data suggest an increased cardiovascular risk with consumption of long-chain saturated fats, the significance of those data is argued, possibly because LDL-C generally increases with decreasing chain length when these replace dietary carbohydrates. Stearic acid (C18:0) has a neutral effect on plasma lipid or lipoprotein profiles when replacing carbohydrate.18
Several lines of evidence show that elevated blood viscosity increases the risk of cardiovascular disease. First, the Edinburgh Artery Study prospectively demonstrated in 1592 subjects that mean blood viscosity was higher in subjects who suffered cardiovascular events, 3.70 versus 3.55 centipoise, p = 0.0003.19 Second, LDL increases and high-density lipoprotein (HDL) decreases blood viscosity due to their opposing effects on erythrocyte aggregation. Particles or molecules which are large enough to simultaneously bind two erythrocytes, such as fibrinogen or LDL, foster erythrocyte aggregation and increase blood viscosity. HDL, which is too small to simultaneously bind two erythrocytes, decreases blood viscosity by competing with LDL for erythrocyte binding. 20
Third, erythropoiesis-stimulating agents exhibit a dose-dependent risk of increased cardiovascular morbidity and mortality. These drugs carry a ‘black box’ warning for increasing the risk of myocardial infarction, stroke, venous thromboembolism, and death. Because hematocrit is the strongest determinant of blood viscosity, those complications are reasonably attributable to elevated blood viscosity. Finally, splenectomy increases blood viscosity and decreases erythrocyte deformability because the spleen removes older, stiffer erythrocytes. In one study, patients with hereditary spherocytosis who underwent splenectomy had an increased risk of cardiovascular events compared with those who did not (hazard ratio: 7.2, 95% CI 2.8–17.2).21 The only causes of death which were increased in World War II servicemen who underwent splenectomy for trauma were pneumonia and coronary artery disease.22 This epidemiologic, hemorheologic, pharmacologic, and hematologic evidence shows that elevated blood viscosity increases cardiovascular risk.
Additional evidence for an adverse hemorheologic effect of interesterified fats is offered by the LDL receptor knockout mouse model. Increased blood viscosity will create larger areas of slower flow or low shear in areas of flow separation adjacent to the vessel wall. Decreased shear will impair the barrier function of the underlying endothelium by causing endothelial cell loss and the development of gaps between endothelial cells.23 This will increase the accumulation of lipoproteins in the subendothelial space and subsequent macropinocytosis by dendritic cells. Afonso and colleagues fed LDL receptor knockout mice diets enriched in polyunsaturated fats, trans fats, palmitic acid, stearic acid, palmitic interesterified fat, and stearic interesterified fat.24 Mice fed trans fats had the greatest accumulation of fat in the intima and mice fed polyunsaturated fats had the least, consistent with their effects on erythrocyte membrane fluidity and blood viscosity. Mice fed interesterified palmitic acid had more fat accumulation than those fed palmitic acid. Macrophage accumulation and plasma concentrations of tumor necrosis factor-α and interleukin-1-β paralleled the intimal accumulation of lipids. Mice fed interesterified stearic acid showed a degree of intimal fat accumulation similar to those fed native stearic acid. The authors attributed this to the fact that interesterification did not increase the amount of saturated fat in the sn-2 position.24
Interesterified triglycerides are currently ‘under the radar’
As a cause of harm done to himself, dietary fats trail only warfare and cigarette smoking, and dwarf environmental contamination by lead and asbestos. Under pressure from activists and unaware of their danger, many purveyors switched from saturated to trans fats in the 1980s. In switching from trans fats to interesterified triglycerides, are we again unwittingly switching to a harmful dietary fat? Exchanging an unsaturated fatty acid (a ‘good’ fat) for a saturated one (a ‘bad’ fat)25 in interesterification is harmful; it decreases erythrocyte deformability and increases blood viscosity. Unsaturated fats are liquid at room and physiologic temperature, while all long-chain saturated fatty acids are solid at room and physiologic temperature. There are ample data to suggest that both erythrocyte plasma membranes and dietary lipids should be fluid. As Hayes and Pronczuk wrote in 2010, “more research is warranted to determine the appropriateness of interesterified fat consumption, particularly before it becomes insidiously embedded in the food supply similar to [trans fatty acids] and intake levels are achieved that compromise long-term health.”2
The effect of dietary fats on blood viscosity and erythrocyte deformability should be determined before science declares them harmless. This is especially important given the lack of regulatory oversight of these fats. Regulatory bodies encourage but do not require specific inclusion of the term ‘interesterified’ in food labeling. The Canadian Food Inspection Agency (CFIA) food labeling guidelines state, “Since interesterification is not hydrogenation or modification, the FDR [Food and Drug Regulations] do not specifically require that ‘interesterification’ be declared in the common name of the product. However, the CFIA encourages the use of the common name ‘interesterified (naming the vegetable oil)’.”26 Meanwhile, the US FDA food labeling requirements do not clearly address interesterified fats. While the US FDA has mandated phasing out of dietary trans fats, the food industry is reformulating many of its products with interesterified fats. Ambiguous labeling requirements enable these fats to appear in foods under umbrella terms such as ‘vegetable oils,’ ‘fully hydrogenated oils,’ ‘palm oil,’ ‘palm kernel oil,’ ‘high stearate,’ or ‘stearic rich’ fats. Ultimately, the very citizens which rely on and trust regulatory bodies to protect public health are ultimately the ones who may suffer potential health risks from this lack of transparency.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Gregory D. Sloop, 105 27th St S, Great Falls, Montana 59401, USA.
Joseph J. Weidman, Independent Researcher, Philadephia, PA, USA
John A. St Cyr, Jacqmar Inc., Minneapolis, MN, USA
References
- 1. Allday E. Damaging trans fat to be banished from US diet. SFGATE, http://www.sfgate.com/health/article/FDA-orders-trans-fat-removed-from-food-by-2018-6331260.php (2015, accessed 18 February 2017).
- 2. Hayes KC, Pronczuk AJ. Replacing trans fat: the argument for palm oil with a cautionary note on interesterification. J Am Coll Nutr 2010; 29: 253S–284S. [DOI] [PubMed] [Google Scholar]
- 3. Berry SEE, Miller GJ, Sanders TAB. The solid fat content of stearic acid-rich fats determines their postprandial effects. Am J Clin Nutr 2007; 85: 1486–1494. [DOI] [PubMed] [Google Scholar]
- 4. Heron M, Anderson RN. Changes in the leading cause of death. Recent patterns in heart disease and cancer mortality. CDC, https://www.cdc.gov/nchs/products/databriefs/db254.htm (2016, accessed 19 January 2017). [PubMed]
- 5. Dalen JE, Alpert JS, Goldberg RJ, et al. The epidemic of the 20(th) century: coronary heart disease. Am J Med 2014; 127: 807–812. [DOI] [PubMed] [Google Scholar]
- 6. Ascherio A, Stampfer MJ, Willett WC. Trans fatty acids and coronary artery disease. Departments of Nutrition and Epidemiology, Harvard School of Public Health. The Channing Laboratory, Department of Medicine, Brigham and Women’s Hospital, http://webcache.googleusercontent.com/search?q=cache:http://www.tfx.org.uk/docs/hsph_transfats.pdf (1999, accessed 22 March 2017). [Google Scholar]
- 7. Grimes DS. An epidemic of coronary heart disease. Q J Med 2012; 105: 509–518. [DOI] [PubMed] [Google Scholar]
- 8. Restrepo BJ, Rieger M. Denmark’s policy on artificial trans fat and cardiovascular disease. Am J Prev Med 2016; 50: 69–76. [DOI] [PubMed] [Google Scholar]
- 9. Brandt EJ, Myerson R, Perraillon MC. Hospital admissions for myocardial infarction and stroke before and after the trans-fat restrictions in New York. JAMA Cardiol 2017; 2: 627–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ascherio A, Hennekens CH, Buring JE, et al. Trans-fatty acids intake and risk of myocardial infarction. Circulation 1994; 89: 94–101. [DOI] [PubMed] [Google Scholar]
- 11. Zaloga GD, Harvey KA, Stillwell W, et al. Trans fatty acids and coronary heart disease. Nutr Clin Pract 2006; 21: 505–512. [DOI] [PubMed] [Google Scholar]
- 12. Kim J, Lee HY, Shin S. Advances in the measurement of red blood cell deformability: a brief review. J Cellular Biotech 2015; 1: 63–79. [Google Scholar]
- 13. Pacetti D, Gagliardi R, Balizano M, et al. Changes in the fatty acid profile and phospholipid molecular species composition of human erythrocyte membranes after hybrid palm and extra virgin olive oil supplementation. J Agric Food Chem 2016; 64: 5499–5507. [DOI] [PubMed] [Google Scholar]
- 14. Roach C, Feller SE, Ward JA, et al. Comparison of cis and trans containing phosphatidylcholines on membrane properties. Biochemistry 2004; 43: 6344–6351. [DOI] [PubMed] [Google Scholar]
- 15. Woodcock BE, Smith E, Lambert WH, et al. Beneficial effect of fish oil on blood viscosity in peripheral vascular disease. Br Med J (Clin Res Ed) 1984; 288: 592–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Terés S, Barceló-Coblijn G, Benet M, et al. Oleic acid content is responsible for the reduction in blood pressure induced by olive oil. Proc Natl Acad Sci U S A 2008; 105: 12811–12816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. The World Health Organization. World health day 2013: diet, nutrition, and hypertension, http://www.emro.who.int/world-health-days/2013/nutrition-hypertension-factsheet-whd-2013.html (2013, accessed 9 June 2017).
- 18. Siri-Tarino PW, Chiu S, Begeron N, et al. Saturated fats versus polyunsaturated fats versus carbohydrates for cardiovascular disease prevention and treatment. Annu Rev Nut 2015; 35: 517–543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lowe GDO, Lee AJ, Rumley A, et al. Blood viscosity and risk of cardiovascular events: the Edinburgh Artery Study. Br J Hematol 1997; 96: 168–173. [DOI] [PubMed] [Google Scholar]
- 20. Sloop GD, Garber DW. The effects of low-density lipoprotein and high-density lipoprotein on blood viscosity correlate with their association with risk of atherosclerosis in humans. Clin Sci (Lond) 1997; 92: 473–479. [DOI] [PubMed] [Google Scholar]
- 21. Schilling RF, Gangnon RE, Traver MJ. Delayed adverse vascular events after splenectomy in hereditary spherocytosis. J Thromb Haemost 2008; 6: 1289–1295. [DOI] [PubMed] [Google Scholar]
- 22. Robinette CD, Fraumeni JF., Jr. Splenectomy and subsequent mortality in veterans of the 1939-45 war. Br J Haemotol 2009; 145: 728–732. [DOI] [PubMed] [Google Scholar]
- 23. Malek AM, Alper SL, Izumo S. Hemodynamic shear stress and its role in atherosclerosis. JAMA 1999; 282: 2035–2042. [DOI] [PubMed] [Google Scholar]
- 24. Afonso MS, Lavrador MSF, Koike MK, et al. Dietary interesterified fat enriched with palmitic acid induces atherosclerosis by impairing macrophage cholesterol efflux and eliciting inflammation. J Nutr Biochem 2016; 32: 91–100. [DOI] [PubMed] [Google Scholar]
- 25. Zevenbergen H, de Bree A, Zeelenberg M, et al. Foods with a high fat quality are essential for healthy diets. Ann Nutr Metab 2009; 54(Suppl. 1): 15–24. [DOI] [PubMed] [Google Scholar]
- 26. Labelling Requirements for Fats and Oils. Canadian Food Inspection Agency, http://www.inspection.gc.ca/food/labelling/food-labelling-for-industry/fats-and-oils/eng/1392751693435/1392751782638?chap=0 (2016, accessed 23 March 2017).


