Abstract
Background:
With this study, we sought to identify patient characteristics associated with clopidogrel prescription and its relationship with in-hospital adverse events in an unselected cohort of ACSs patients.
Materials and Methods:
We studied all consecutive patients admitted at our institution for ACSs from 2012 to 2014. Patients were divided into two groups based on clopidogrel or novel P2Y12 inhibitors (prasugrel or ticagrelor) prescription and the relationship between clopidogrel use and patient clinical characteristics and in-hospital adverse events was evaluated using logistic regression analysis.
Results:
The population median age was 68 years (57–77 year) and clopidogrel was prescribed in 230 patients (46%). Patients characteristics associated with clopidogrel prescription were older age, female sex, non-ST-elevation ACS diagnosis, the presence of diabetes mellitus and anemia, worse renal and left ventricular functions and a higher Killip class. Patients on clopidogrel demonstrated a significantly higher incidence of in-hospital mortality (4.8%) than prasugrel and ticagrelor-treated patients (0.4%), while a nonstatistically significant trend emerged considering bleeding events. However, on multivariable logistic regression analysis female sex, the presence of anemia and Killip class were the only variables independently associated with in-hospital death.
Conclusion:
Patients treated with clopidogrel showed a higher in-hospital mortality. However, clinical variables associated with its use identify a population at high risk for adverse events and this seems to play a major role for the higher in-hospital mortality observed in clopidogrel-treated patients.
Keywords: acute coronary syndromes, clopidogrel, dual antiplatelet therapy, prasugrel, ticagrelor
Introduction
Since its introduction in the clinical arena, clopidogrel, a P2Y12 adenosine diphosphate receptor antagonist, has been largely and successfully used in patients with acute coronary syndromes (ACSs), paving the way to dual antiplatelet therapy (DAPT) utilization as the cornerstone of the contemporary management of patients with ACS.1–6 Clopidogrel, however, has several drawbacks consisting of delayed onset, potential interactions with other drugs, and variable platelet responses due to genetic polimorphisms.7,8 In recent years several new antithrombotic treatments have been evaluated and new data regarding novel antiplatelet drugs have been published. In particular, two new P2Y12 receptor inhibitors, prasugrel and ticagrelor, have been introduced in clinical practice.9,10 In randomized clinical trials, these two inhibitors resulted to be superior in major cardiac adverse event (MACE) reduction in ACS patients compared to clopidogrel; the latter however, remains largely used in daily clinical practice, as described in some large multicenter and singlecenter observational studies.11–13
In this study, we evaluated the patterns of DAPT prescription in an unselected cohort of patients admitted at our institution for ACS. In particular, we sought to identify the clinical variables associated with clopidogrel use and its relationship with in-hospital adverse events.
Methods and materials
Study population
All consecutive patients admitted to the Coronary Care Unit (CCU) of the San Paolo Hospital (Milan) with diagnosis of ACS between 2012 and 2014 composed our study population. The diagnosis of ACS was based on new onset ischemia-related symptoms and the presence of at least one of the following criteria: (i) electrocardiographic changes indicative of myocardial ischemia; and (ii) troponin elevation above the 99th percentile threshold of a healthy reference population, with 10% variability coefficient. Patients were classified as having ST-elevation myocardial infarction (STEMI) or non-ST-elevation ACS (NSTE-ACS) according to the standardized electrocardiographic criteria.
An all-comers design study was adopted with no restriction on age or on critically ill patients inclusion.
Patients were treated according to usual clinical practice. Coronary angiography and percutaneous coronary intervention (PCI) were performed using standard techniques.
The study complies with the Declaration of Helsinki and was approved by the Clinical Research Ethics Committee of the San Paolo Hospital. For this type of study, a formal consent was not required by the Ethical Committee; however, all the patients signed a standard consent regarding sensitive personal data treatment.
Data collection and variables definitions
Baseline clinical characteristics, medical history, biochemical variables, angiographic data and pharmacologic and invasive treatments employed during hospitalization were prospectively collected and recorded on a computer database designed for ACS patients admitted to our CCU. Based on clinical and laboratory data collected at admission, GRACE (Global Registry of Acute Coronary Events)14 and CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA (American College of Cardiology/American Heart Association) Guidelines)15 risk scores were calculated in order to quantify the risk of in-hospital death and bleeding events. Finally, on the base of the P2Y12 inhibitor prescribed, patients were divided in two groups: those treated with clopidogrel and those treated with prasugrel or ticagrelor.
In-hospital adverse events considered for our analysis were: (i) myocardial infarction/re-infarction (ReMI), diagnosed in the presence of new ischemic symptoms and an elevation or re-elevation of biomarkers of myocardial necrosis with or without concurrent electrocardiographic changes; (ii) urgent percutaneous revascularization (UPR); (iii) bleedings, classified according to the Bleeding Academic Research Consortium (BARC) criteria;16 and (iv) mortality.
Statistical analysis
Continuous variables are presented as medians and interquartile ranges and categorical variables are presented as absolute values and percentages. Comparisons between continuous variables were performed using Mann–Whitney or Kruskall–Wallis tests and comparisons between categorical variables were performed using the Chi-squared or Fisher’s exact test. Statistical significance was defined as p < 0.05.
In order to find an association between clinical variables and clopidogrel prescription, univariable logistic regression analysis was performed. All the variables with a p value <0.05 at the univariable analysis were included along with clopidogrel prescription in a multivariable stepwise logistic regression analysis to identify the independent predictors of in-hospital adverse events. Results of logistic regression are presented as odds ratios with 95% confidence interval.
MedCalc Statistical Software version 16.2.0 and Graph Pad Prism version 6 were the statistical packages used.
Results
Baseline characteristics
The study cohort enrolled during the two-year study period consisted of 501 patients (median age 68 years, 31% females), 45% of whom had a STEMI and 55% had a NSTE-ACS. Baseline clinical characteristics are summarized in Table 1. No statistically significant difference was found regarding age and sex distribution between the two ACS groups. In the whole population, hypertension was present in 63% of patients, diabetes mellitus in 27%, a history of prior myocardial infarction or PCI in 22% and 18%, respectively, a stage III or higher renal failure in 25%, and a Killip class ⩾2 at admission in 16%. The median GRACE risk score was 139 (113–167) and the median CRUSADE risk score was 27 (15–40). Patients with NSTE-ACS presented a significantly higher prevalence of arterial hypertension and diabetes mellitus and had more often a history of coronary artery disease compared with those in the STEMI group. Moreover, they presented at admission a higher prevalence of renal failure and anemia. Finally, the GRACE risk score was higher in STEMI patients, while the CRUSADE score was higher in NSTE-ACS group.
Table 1.
Clinical characteristics of the study population. Values are presented as median (interquartile range) or n (%).
| Overall n = 501 | STEMI n = 225 | NSTE-ACS n = 276 | p value | |
|---|---|---|---|---|
| Age (years) | 68 (57–77) | 67 (58–76) | 70 (57–78) | 0.26 |
| Age ⩾ 75 years | 165 (33) | 67 (30) | 98 (35) | 0.18 |
| Female | 157 (31) | 66 (29) | 91 (33) | 0.38 |
| MEDICAL HISTORY | ||||
| Diabetes mellitus | 136 (27) | 48 (21) | 88 (32) | 0.008 |
| Hypertension | 317 (63) | 124 (55) | 193 (70) | 0.0007 |
| Dyslipidemia | 213 (42) | 91 (40) | 122 (44) | 0.39 |
| Active smokers | 185 (37) | 93 (41) | 92 (33) | 0.07 |
| Prior MI | 108 (22) | 22 (10) | 86 (31) | <0.0001 |
| Prior PCI | 89 (18) | 21 (9) | 68 (25) | <0.0001 |
| Prior CABG | 38 (8) | 5 (2) | 33 (12) | <0.0001 |
| Prior stroke/TIA | 25 (5) | 13 (6) | 12 (4) | 0.53 |
| CLINICAL PRESENTATION | ||||
| eGFR < 60 ml/min/m2 | 125 (25) | 46 (20) | 79 (29) | 0.03 |
| Anemia | 92 (18) | 31 (14) | 61 (22) | 0.02 |
| EF (%) | 54 (45–58) | 51 (43-56) | 55 (45–60) | <0.0001 |
| Killip class ⩾ 2 | 78 (16) | 28 (12) | 50 (18) | 0.08 |
| Atrial fibrillation | 59 (12) | 29 (13) | 30 (11) | 0.49 |
| Acute pulmonary edema | 19 (4) | 3 (1) | 16 (6) | 0.009 |
| Cardiogenic shock | 12 (2) | 9 (4) | 3 (1) | 0.04 |
| Cardiac arrest | 11 (2) | 10 (4) | 1 (0.4) | 0.003 |
| GRACE risk score | 139 (113–167) | 149 (125–170) | 131 (103–160) | <0.0001 |
| CRUSADE risk score | 27 (15–40) | 24 (12–38) | 29 (17–40) | 0.03 |
| IN-HOSPITAL MANAGEMENT | ||||
| Aspirin | 488 (97) | 222 (99) | 266 (96) | 0.15 |
| P2Y12 inhibitors | 470 (94) | 219 (98) | 251 (91) | 0.003 |
| Clopidogrel | 230 (46) | 89 (40) | 141 (51) | 0.001 |
| Prasugrel | 92 (18) | 78 (35) | 14 (5) | <0.0001 |
| Ticagrelor | 148 (29) | 52 (23) | 96 (35) | 0.001 |
| Anti-GPIIbIIIa | 120 (25) | 91 (41) | 29 (11) | <0.0001 |
| UFH | 212 (42) | 112 (50) | 100 (36) | <0.0001 |
| LMWH | 47 (9) | 6 (3) | 41 (15) | <0.0001 |
| Fondaparinux | 100 (20) | 9 (4) | 91 (33) | <0.0001 |
| Bivalirudin | 105 (21) | 87 (39) | 18 (7) | <0.0001 |
| Coronary angiography | 477 (95) | 222 (99) | 255 (92) | 0.001 |
| Multivessel disease | 281 (59) | 125 (56) | 156 (61) | 0.30 |
| PCI | 356 (75) | 201 (90) | 155 (61) | <0.0001 |
| IABP | 7 (1.4) | 6 (2.7) | 1 (0.4) | 0.03 |
| CABG | 31 (6) | 7 (3) | 24 (9) | 0.01 |
CABG, coronary artery by-pass grafting; eGFR, estimated glomerular filtration rate (MDRD formula); EF, left ventricular ejection fraction; IABP, intra-aortic balloon pump; LMWH, low molecular weight heparin; MI, myocardial infarction; NSTE-ACS, non-ST-elevation acute coronary syndrome; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction; TIA, transient ischemic attack; UFH, unfractioned heparin.
Clinical management and antithrombotic strategy (Table 1)
Oral antiplatelet therapy was prescribed as follows: 488 (97%) patients received aspirin and 470 (94%) received a P2Y12 inhibitor. A total of 31 patients (6%) were treated with aspirin alone or did not receive any antiplatelet treatment. Of the patients treated with DAPT, 230 were on clopidogrel and 240 were on prasugrel or ticagrelor. DAPT was used more often in STEMI than in NSTE-ACS patients. Clopidogrel was the most often second antiplatelet agent used both in STEMI (40%) and in NSTE-ACS (51%) subgroups. Clopidogrel and ticagrelor were significantly more often used in NSTE-ACS patients in contrast to prasugrel which was more often used in STEMI patients. Glycoprotein IIb/IIIa inhibitors and bivalirudin were used more often in STEMI patients, while fondaparinux was used in 100 patients (20%), mostly with NSTE-ACS. The majority of patients (95%) underwent coronary angiography and multivessel coronary disease (MVD) was diagnosed in 59% of cases. PCI was performed in 356 patients (75%), significantly more often in the STEMI group. A radial arterial access was used in 56% of cases.
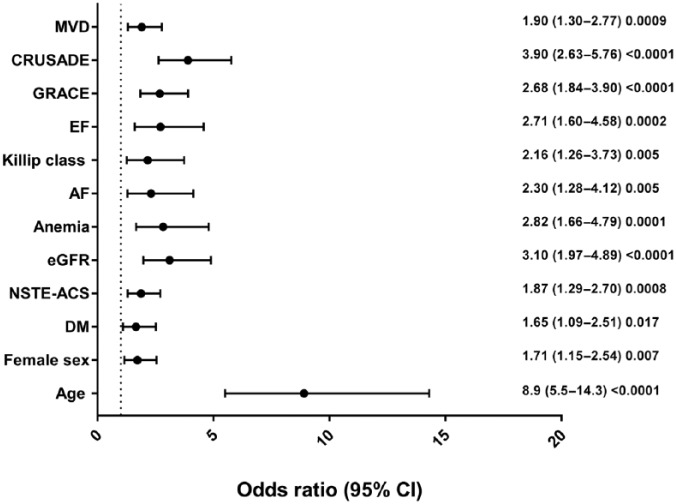
Clinical characteristics associated with clopidogrel prescription
Table 2 summarizes the clinical characteristics of patients according to the P2Y12 therapy prescribed (clopidogrel versus novel P2Y12 inhibitors). Patients treated with clopidogrel were significantly older, with an age ⩾75 years in 53% of cases versus only 11% in patients treated with prasugrel or ticagrelor. They were more frequently females, had a higher prevalence of diabetes, anemia and stage III or higher renal failure. They presented at admission a worse Killip class and a worse in-hospital left ventricular systolic function. Finally, they had more often a NSTE-ACS diagnosis and underwent less often to coronary angiography and PCI, although presenting with a higher prevalence of MVD. In summary, comparing the P2Y12 inhibitors therapy subgroups, clopidogrel patients correspond to a higher risk population for both in-hospital ischemic and hemorrhagic events. In fact, they showed GRACE and CRUSADE risk scores values significantly higher than prasugrel or ticagrelor-treated patients. At the univariable logistic regression analysis some clopidogrel use predictors emerged (Figure 1): advanced age, female sex, diabetes mellitus, renal failure, anemia, atrial fibrillation, MVD, NSTE-ACS presentation, worse Killip class, lower ejection fraction and higher GRACE and CRUSADE risk scores were associated with its prescription.
Table 2.
Clinical characteristics of patients according to P2Y12 inhibitor therapy prescribed. Values are presented as median (interquartile range) or n (%).
| Clopidogrel n = 230 | Prasugrel/Ticagrelor n = 240 | p value | |
|---|---|---|---|
| Age (years) | 75 (65–81) | 61 (53–70) | <0.0001 |
| Age ⩾ 75 years | 122 (53) | 27 (11) | <0.0001 |
| Female | 86 (37) | 62 (26) | 0.007 |
| Diabetes mellitus | 71 (31) | 51 (21) | 0.02 |
| STEMI | 89 (39) | 130 (54) | 0.001 |
| NSTE-ACS | 141 (61) | 110 (46) | 0.001 |
| eGFR < 60 ml/min/m2 | 78 (34) | 34 (14) | <0.0001 |
| Anemia | 53 (23) | 23 (10) | <0.0001 |
| EF (%) | 53 (41–58) | 55 (48–59) | 0.001 |
| Killip class ⩾ 2 | 43 (19) | 23 (10) | 0.005 |
| Atrial fibrillation | 38 (16) | 19 (8) | 0.005 |
| Acute pulmonary edema | 10 (4.3) | 4 (1.7) | 0.10 |
| Cardiogenic shock | 7 (3) | 4 (1.7) | 0.37 |
| Cardiac arrest | 2 (1) | 9 (4) | 0.06 |
| GRACE risk score | 150 (126–177) | 125 (103–150) | <0.0001 |
| CRUSADE risk score | 35 (23–44) | 19 (10–30) | <0.0001 |
| Coronary angiography | 218 (95) | 236 (98) | 0.04 |
| Multivessel disease | 146 (67) | 121 (51) | 0.001 |
| PCI | 153 (70) | 196 (83) | 0.001 |
| IABP | 5 (2.2) | 2 (0.8) | 0.27 |
eGFR, estimated glomerular filtration rate (MDRD formula); EF, left ventricular ejection fraction; IABP, intra-aortic balloon pump; NSTE-ACS, non-ST-elevation acute coronary syndrome; PCI, percutaneous coronary intervention; STEMI, ST-elevation myocardial infarction.
Figure 1.
Clinical characteristics associated with clopidogrel prescription on univariable logistic regression analysis.
Age, age ⩾ 75 years; AF, atrial fibrillation; CI, confidence interval; CRUSADE, CRUSADE risk score > 30; DM, diabetes mellitus; EF, left ventricular ejection fraction ⩽ 40%; eGFR, estimated glomerular filtration rate (MDRD formula) < 60 ml/min/m2; GRACE, GRACE risk score > 140; Killip class, Killip class ⩾ 2; MVD, multivessel coronary disease; NSTE-ACS, non-ST-elevation acute coronary syndrome.
In-hospital adverse events and their relationship with clopidogrel use
Table 3 summarizes the in-hospital major adverse events according to the P2Y12 therapy prescribed (clopidogrel versus novel P2Y12 inhibitors). In the whole population, the composite incidence of ReMI and UPR was 7%, 32 patients (6.4%) underwent a BARC type 2 or 3 bleeding, 11 (2.2%) a BARC type 3 bleeding, and mortality was 2.6%. Patients treated with clopidogrel presented a significantly higher mortality (4.8%) than patients treated with prasugrel or ticagrelor (0.4%) and a borderline significant higher incidence of overall bleedings, while no significant differences were found regarding ReMI/UPR and BARC type 3 bleedings. In order to further analyze the association of clopidogrel use with mortality and overall bleedings, we performed a stepwise multivariable logistic regression analysis including along with clopidogrel prescription all the variables significantly associated with its use. What we found is that only female sex, the presence of anemia and a Killip class at admission ⩾ 2 were independently associated with mortality (Figure 2), while only a moderate or higher risk CRUSADE value was independently associated with overall bleedings.
Table 3.
In-hospital adverse events according to P2Y12 inhibitor therapy prescribed. Values are presented as n (%).
| Clopidogrel n = 230 | Prasugrel/Ticagrelor n = 240 | p value | |
|---|---|---|---|
| ReMI/UPR | 9 (4) | 11 (5) | 0.82 |
| Overall bleedings | 20 (8.7) | 10 (4.2) | 0.06 |
| BARC 3 bleedings | 6 (2.6) | 5 (2.1) | 0.76 |
| Death | 11 (4.8) | 1 (0.4) | 0.002 |
BARC, Bleeding Academic Research Consortium; ReMI, myocardial infarction/re-infarction; UPR, urgent percutaneous revascularization.
Figure 2.
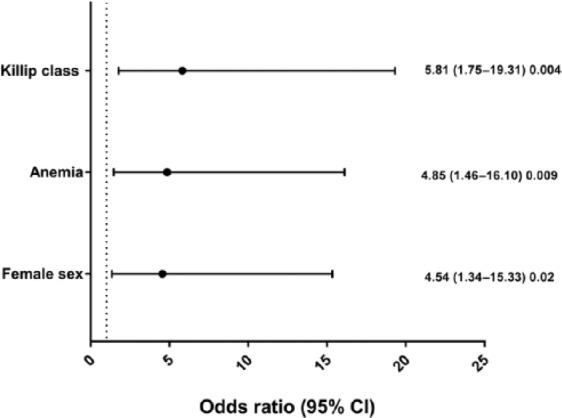
Clinical characteristics independently associated with in-hospital death on multivariable stepwise logistic regression analysis.
CI, confidence interval; Killip class, Killip class ⩾ 2.
Discussion
The main results of the present study can be summarized as follows: (i) clopidogrel has been the most frequently used second antiplatelet agent, accounting for nearly half of the prescriptions in the overall population; (ii) clinical variables associated with its use identify patients at higher risk for adverse events; and (iii) this is probably the reason for the higher in-hospital mortality observed in clopidogrel-treated patients.
Although the last European Society of Cardiology (ESC) and ACC/AHA Guidelines for the management of patients with STEMI and NSTE-ACS17–20 recommend prasugrel and ticagrelor over clopidogrel as the first choice drugs for double platelet inhibition according to the results of the TRITON-TIMI 38 and of the PLATelet inhibition and patient Outcomes (PLATO) trials showing the superiority of the two new P2Y12 inhibitors in reducing MACE in ACS patients,9,10 clopidogrel is still widely used in the clinical practice, as highlighted by several international registries.11,21–26
In our study clopidogrel was used in 46% of the overall population, and in particular in 40% of STEMI patients and in 51% of NSTE-ACS patients. When compared with previous studies, our prescription rate of clopidogrel in NSTE-ACS patients is similar to that observed in the AMIS-PLUS21 and in the SCAAR22 registries. Considering STEMI patients in AMIS-PLUS,21 SCAAR22 and MULTIPRAC23 registries, however, where clopidogrel was the first choice second antiplatelet agent in 47.8%, 51.3% and 54.4%, our clopidogrel use appears to be lower (40%), with a high new P2Y12 inhibitors prescription rate (58%), in particular of prasugrel (35%). These data, in a similar way as the results of the GReek AntiPlatelet rEgistry (GRAPE) registry,26 seem to suggest a trend toward a more adherent application of international guideline indications.
Besides the still wide prescription of clopidogrel, these registries highlight the patients’ clinical characteristics associated with clopidogrel utilization in daily clinical practice. In particular, NSTE-ACS diagnosis and age appear to be two important factors favoring clopidogrel prescription.11,21,22,24–26 This probably reflects the special warnings for prasugrel utilization in elderly patients9 and the less definite results obtained by its use in NSTE-ACS population9,27 and the reluctance of ticagrelor utilization in the aged patients because of the higher bleeding risk in this population, despite the favorable results obtained in the elderly substudy of the PLATO trial.28 According to the aforementioned observations, in our study both advanced age and NSTE-ACS diagnosis were associated with clopidogrel utilization. Patients taking clopidogrel had a median age of 75 years and more than half of them had an age ⩾ 75 years versus only 11% of those taking the new P2Y12 inhibitors. Moreover, at the univariable logistic regression analysis, other clopidogrel use predictors emerged in our study, such as female sex, diabetes mellitus, chronic renal impairment, atrial fibrillation, anemia, worse Killip class and left ventricular function and coronary multivessel disease. In essence, our clopidogrel-treated patients represent a globally higher risk population, both regarding ischemic and bleeding events, as highlighted by the significantly higher values of GRACE and CRUSADE risk scores associated with clopidogrel prescription. This means that in daily practice we face the clinical paradox that patients at higher risk of MACE are treated with the less efficacious P2Y12 inhibitor.24 On the other hand, since baseline clinical characteristic contribute to the risk of MACE, the outcome data related to the various P2Y12 inhibitors may be confounded in this setting. In this regard, interesting observations can be drawn from the results of the Platelet Inhibition Registry in ACS EvalUation Study (PIRAEUS),12,13 that aimed to integrate the wide array of data generated by individual registries on the efficacy and safety of P2Y12 inhibitors in ACS. In summary, the various observational studies showed the superiority of both prasugrel and ticagrelor over clopidogrel in terms of MACE and mortality reduction, while more difficult was the comparison regarding bleeding events, because of the different bleeding definitions used in the various registries. At most, a trend toward more bleedings in clopidogrel-treated patients was observed. In contrast to these data, however, two other observational registries24,25 did not show any beneficial effect of prasugrel or ticagrelor over clopidogrel regarding MACE and in-hospital or long-term mortality.
In our study, overall in-hospital mortality was 2.6% and overall bleedings were 6.4%. In accordance with the most of registries, we observed a significantly higher in-hospital mortality in clopidogrel-treated patients (4.8%) than in patients treated with prasugrel or ticagrelor (0.4%), while no significant differences were found regarding recurrent ischemic events or urgent revascularization. Finally, a no significant trend toward a higher incidence of overall bleedings in clopidogrel cohort patients was present.
In order to better understand the real relationship between clopidogrel utilization and in-hospital mortality observed in our population, we performed multivariable logistic regression analysis, including along with clopidogrel prescription all the clinical variable associated with its utilization. What we obtained is that clopidogrel is not independently associated with in-hospital mortality, but only female sex, a high Killip class and anemia at admission are independently associated with it. Moreover, as far as bleeding events are concerned, only an at least moderate CRUSADE score value was independently associated with overall bleeding events, confirming the predictive role of this risk model.
These data indicate that in the daily clinical practice a safety-oriented approach prevails when treating patients at high risk because of advanced age and several comorbidities and that the baseline clinical characteristics represent the main negative prognostic factor.
The present study has some limitations. The first one is the relatively limited sample size and the consequent small number of events that may influence the statistic results. A second limitation is that this is a single-institution experience and this might reduce the generalizability of our findings to other populations. However, we think that our population, although relatively small, is a well-balanced mix of ACS patients. As a matter of fact, it represents a contemporary population of ACS, being almost equally subdivided in STEMI and NSTE-ACS patients managed according to current clinical practice.
Conclusion
In our unselected ACS patient population, clopidogrel has been widely prescribed and patients treated with clopidogrel showed a higher in-hospital mortality and a trend toward more bleeding events. However, clinical variables associated with its use identify a population at high risk for adverse events and clopidogrel per se does not seem independently associated with higher in-hospital mortality.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Diego Castini, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Via A. di Rudinì 8, 20142 Milan, Italy.
Simone Persampieri, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Sara Cazzaniga, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Giulia Ferrante, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Marco Centola, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Stefano Lucreziotti, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Diego Salerno-Uriarte, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Carlo Sponzilli, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
Stefano Carugo, Division of Cardiology, San Paolo Hospital, Department of Health Sciences, University of Milan, Italy.
References
- 1. Mehta SR, Yusuf S, Peters R, et al. ; Clopidogrel in Unstable angina to prevent Recurrent Events trial (CURE) Investigators. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001; 358: 527–533. [DOI] [PubMed] [Google Scholar]
- 2. Peters R, Mehta SR, Fox KA, et al. ; Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) Trial Investigators. Effects of aspirin dose when used alone or in combination with clopidogrel in patients with acute coronary syndromes: observations from the Clopidogrel in Unstable angina to prevent Recurrent Events (CURE) study. Circulation 2003; 108: 1682–1687. [DOI] [PubMed] [Google Scholar]
- 3. Mehta SR, Tanguay JF, Eikelboom JW, et al. Double-dose versus standard-dose clopidogrel and high-dose versus low-dose aspirin in individuals undergoing percutaneous coronary intervention for acute coronary syndromes (CURRENT-OASIS 7): a randomized factorial trial. Lancet 2010; 376: 1233–1243. [DOI] [PubMed] [Google Scholar]
- 4. Angiolillo DJ. The evolution of antiplatelet therapy in the treatment of acute coronary syndromes: from aspirin to the present day. Drugs 2012; 72: 2087–2101. [DOI] [PubMed] [Google Scholar]
- 5. Patrono C, Bachmann F, Baigent C, et al. Expert consensus document on the use of antiplatelet agents. The task force on the use of antiplatelet agents in patients with atherosclerotic cardiovascular disease of the European Society of Cardiology. Eur Heart J 2004; 25: 166–181. [DOI] [PubMed] [Google Scholar]
- 6. Kereiakes DJ, Yeh RW, Massaro JM, et al. Antiplatelet therapy duration following bare metal or drug eluting stents: the dual antiplatelet therapy randomized clinical trial. JAMA 2015; 313: 1113–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gurbel PA, Blinden KP, Hiatt BL, et al. Clopidogrel for coronary stenting: response variability, drug resistance, and the effect of pretreatment platelet reactivity. Circulation 2003; 107: 2908–2913. [DOI] [PubMed] [Google Scholar]
- 8. Mega JL, Simon T, Collet JP, et al. Reduced-function CYP2C19 genotype and risk of adverse clinical outcomes among patients treated with clopidogrel predominantly for PCI: a meta-analysis. JAMA 2010; 304: 1821–1830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wiviott SD, Braunwald E, McCabe CH, et al. ; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007; 357: 2001–2015. [DOI] [PubMed] [Google Scholar]
- 10. Wallentin L, Becker RC, Budaj A, et al. ; PLATelet inhibition and patient Outcomes (PLATO) investigators. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2009; 361: 1045–1057. [DOI] [PubMed] [Google Scholar]
- 11. De Luca L, Leonardi S, Cavallini C, et al. ; EYESHOT Investigators. Contemporary antithrombotic strategies in patients with acute coronary syndrome admitted to cardiac care units in Italy: the EYESHOT Study. Eur Heart J Acute Cardiovasc Care 2015; 4: 441–452. [DOI] [PubMed] [Google Scholar]
- 12. Zeymer U, Widimsky P, Danchin N, et al. ; PIRAEUS group. P2Y12 receptor inhibitors in patients with non-ST elevation acute coronary syndrome in the real world: use, patient selection, and outcomes from contemporary European registries. Eur Heart J Cardiovasc Pharmacother 2016; 2: 229–243. [DOI] [PubMed] [Google Scholar]
- 13. Danchin N, Lettino M, Zeymer U, et al. ; PIRAEUS group. Use, patient selection and outcomes of P2Y12 receptor inhibitor treatment in patients STEMI based on contemporary European registries. Eur Heart J Cardiovasc Pharmacother 2016; 2: 152–167. [DOI] [PubMed] [Google Scholar]
- 14. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med 2003; 163: 2345–2353. [DOI] [PubMed] [Google Scholar]
- 15. Subherwal S, Bach RG, Chen AY, et al. Baseline risk of major bleeding in non-ST-segment-elevation myocardial infarction: the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress Adverse outcome with Early implementation of the ACC/AHA Guidelines) Bleeding Score. Circulation 2009; 119: 1873–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus from the Bleeding Academic Research Consortium. Circulation 2011; 123: 2736–2747. [DOI] [PubMed] [Google Scholar]
- 17. Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016; 37: 267–315. [DOI] [PubMed] [Google Scholar]
- 18. Steg PG, James SK, Atar D, et al. ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012; 33: 2569–2619. [DOI] [PubMed] [Google Scholar]
- 19. Amsterdam EA, Wenger NK, Brindis R, et al. 2014 AHA/ACC guideline for the management of patients with non–ST-Elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2014; 130: e344–e426. [DOI] [PubMed] [Google Scholar]
- 20. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: executive summary: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013; 61: 485–510. [DOI] [PubMed] [Google Scholar]
- 21. Kurz DJ, Radovanovic D, Seifert B, et al. Comparison of prasugrel and clopidogrel-treated patients with acute coronary syndrome undergoing percutaneous coronary intervention: a propensity score-matched analysis of the Acute Myocardial Infarction in Switzerland (AMIS)-Plus Registry. Eur Heart J Acute Cardiovasc Care 2016; 5: 13–22. [DOI] [PubMed] [Google Scholar]
- 22. Damman P, Varenhorst C, Koul S, et al. Treatment patterns and outcomes in patients undergoing percutaneous coronary intervention treated with prasugrel or clopidogrel (from the Swedish Coronary Angiography and Angioplasty Registry [SCAAR]). Am J Cardiol 2014; 113: 64–69. [DOI] [PubMed] [Google Scholar]
- 23. Clemmensen P, Grieco N, Ince H, et al. MULTInational non-interventional study of patients with ST-segment elevation myocardial infarction treated with PRimary Angioplasty and Concomitant use of upstream antiplatelet therapy with prasugrel or clopidogrel—the European MULTIPRAC Registry. Eur Heart J Acute Cardiovasc Care 2015; 4: 220–229. [DOI] [PubMed] [Google Scholar]
- 24. Yudi MB, Clark DJ, Farouque O, et al. Clopidogrel, prasugrel or ticagrelor in patients with acute coronary syndromes undergoing percutaneous coronary intervention. Intern Med J 2016; 46: 559–565. [DOI] [PubMed] [Google Scholar]
- 25. Park KH, Jeong MH, Ahn Y, et al. Comparison of short-term clinical outcomes between ticagrelor versus clopidogrel in patients with acute myocardial infarction undergoing successful revascularization: from Korea Acute Myocardial Infarction Registry-National Institute of Health. Int J Cardiol 2016; 215: 193–200. [DOI] [PubMed] [Google Scholar]
- 26. Alexopoulos D, Goudevenos JA, Xanthopoulou I, et al. Implementation of contemporary oral antiplatelet treatment guidelines in patients with acute coronary syndrome undergoing percutaneous coronary intervention: a report from the GReek AntiPlatelet rEgistry (GRAPE). Int J Cardiol 2013; 168: 5329–5335. [DOI] [PubMed] [Google Scholar]
- 27. Roe MT, Armstrong PW, Fox KAA, et al. Prasugrel versus clopidogrel for acute coronary syndromes without revascularization. N Engl J Med 2012; 367: 1297–1309. [DOI] [PubMed] [Google Scholar]
- 28. Husted S, James S, Becker R, et al. Ticagrelor versus clopidogrel in elderly patients with acute coronary syndromes: a substudy from the prospective randomized PLATelet inhibition and patient Outcomes (PLATO) trial. Circ Cardiovasc Qual Outcomes 2012; 5: 680–688. [DOI] [PubMed] [Google Scholar]