Abstract
The Global Appraisal of Individual Needs (GAIN)1 is a 1–2 hour standardized biopsychosocial that integrates clinical and research assessment for people presenting to substance abuse treatment. The GAIN – Short Screener (GSS) is 3–5 minute screener to quickly identify those who would have a disorder based on the full 60–120 minute GAIN and triage the problem and kind of intervention they are likely to need along four dimensions (internalizing disorders, externalizing disorders, substance disorders, and crime/violence). Data were collected from 6,177 adolescents and 1,805 adults as part of 77 studies in three dozen locations around the United States that used the GAIN. For both adolescents and adults the 20-item total disorder screener (TDScr) and its four 5-item sub-screeners (internalizing disorders, externalizing disorders, substance disorders, and crime/violence) has good internal consistency (alpha of .96 on total screener), is highly correlated (r = .84 to .94) with the 123-item longer scales in the full GAIN. The GSS also does well in terms of its receiver operator characteristics (90% or more under the curve in all analyses) and has clinical decision-making cut points with excellent sensitivity (90% or more) for identifying people with a disorder and excellent specificity (92% or more) for correctly ruling out people who did not have a disorder. The GSS has good potential as an efficient screener for identifying people with co-occurring disorders across multiple systems and routing them to the right services and more detailed assessments.
Among people in the community with psychiatric and substance disorders, multiple co-occurring diagnoses are the norm.2–7 Co-occurrence of psychiatric disorders, substance use disorders, and crime/violence are an even more prominent characteristic of those entering the addiction treatment, mental health services, and the criminal/juvenile justice system.6,8–16 Individuals with multiple co-occurring problems are more likely to experience problems with treatment and medication adherence, shorter lengths of stay, administrative discharges, functional status, community adjustment, quality of life, and worse outcomes following treatment for their substance use disorder.17–24
Unfortunately, it is estimated that one- to two-thirds of people with serious disorders do not access treatment and most of those who are un- or under-treated are young males with poor education.25 Among people with substance use disorders, less than 1 in 5 adults and 1 in 10 adolescents enter treatment.26 While research suggests that 70 to 80% of people entering substance abuse treatment have one or more co-occurring psychiatric disorders only 16% of adults and 28% of adolescents have a co-occurring disorder documented in their intake assessments.27–28 This has led to calls to introduce standardized assessment of co-occurring disorders among people presenting to mental health, substance abuse, welfare and justice systems.29–32 The problem is that such assessments often take hours of client and staff time that press limited public resources. Thus, there is a need to develop and evaluate a short initial screener to (1) identify who has a disorder and rule out those who do not, (2) make an initial approximation of the type of problems and severity, and (3) guide referral to further assessment and treatment.
There are hundreds of diagnoses (each with multiple specifiers) identified in the Diagnostic and Statistical Manual Version IV text revised (DSM-IV-TR).33 Studies in general population34–37 and clinical samples,38–39 however, demonstrate the existence of three primary dimensions along which the prevalence of the more common mental disorders vary: (1) internalizing disorders (e.g., depression, anxiety, somatic disorder, traumatic distress, suicide), (2) externalizing disorders (e.g., attention deficit, hyperactivity, conduct and other impulse control disorders), and (3) substance use disorders (e.g., abuse, dependence, other substance induced health or psychiatric problems). While externalizing disorders typically onset in childhood, there is increasing recognition that they extend well into adulthood and are related to substance use severity.5,39–43 Among substance users and people in the juvenile/criminal justice system there is often a fourth dimension, crime and violence (e.g., interpersonal violence, drug related crime, property crime, interpersonal crime).38,44–46 While each disorder/problem is unique, those that vary along the same dimensions often share more etiology (e.g., age of onset, course), consequence, treatment, and outcomes with each other than with disorders in other dimensions. Methodologically, grouping symptoms and disorders into these four statistical dimensions increases the efficiency and accuracy of a screener.
The full Global Appraisal of Individual Needs (GAIN)1 is a standardized biopsychosocial that integrates clinical and research assessment for people presenting to substance abuse or other behavioral health treatment. It asks about symptoms from DSM-IV-TR that can be used to generate dimensional symptom count measures or categorical diagnostic impressions of specific disorders in the four main dimensions of interest here (i.e., internalizing, externalizing, substance, and crime/violence). While well received (it is currently in use by over 400 agencies across the U.S., Canada, and Mexico), it typically takes 2–3 months of training and feedback to get a staff person certified on GAIN administration and then takes 90 to 120 minutes per patient/staff person to actually administer. For many situations, this involves more resources, more control of programs/staff than is feasible over a large spread out system, and is substantively too extensive an assessment for a client coming in on a generic referral. Even if we pulled out just the 123 main diagnostic questions from the GAIN, this would still be 8 pages long and take 20–30 minutes. This is often still too long for use as a screener in settings like school, workplace, internet based health risk assessments, welfare, or justice systems where it may only be one of several components, there is limited time or limited staff resources. Thus, there was a need to develop a GAIN-Short Screener (GSS) that could be (a) easily trained, (b) used in 5 minutes or less to identify people who have a disorder and rule out people who do not, and (c) provide guidance for referral to further assessment and treatment. Consistent with the full GAIN, the GSS is designed to (a) be valid for both adolescent and adult populations, (b) provide measures of severity overall and in the four main dimensions of emotional/behavioral problems (internalizing, externalizing, substance, crime/violence), and (c) triage these dimensions to provide guides to support clinical decision making about diagnosis and treatment needs.
The aims of this paper are to (1) describe the development of the 20-item GSS (2) validate its use as a dimensional measure and (3) identify the optimal clinical cut points for clinical decision making about the likelihood of a disorder or crime/violence problem. For each aim we examine the GSS’s use for both adolescents and adults, as a measure of total severity, and as a measure within each of the four main dimensions of emotional/behavioral problems (internalizing, externalizing, substance, crime/violence) measured by the full GAIN.
METHODS
Data Source
The data are from the 77 studies in three dozen locations around the United States that used the GAIN.1 Over two thirds of these studies were conducted by independent investigators. They were funded by a wide range of organizations (e.g., the Center for Substance Abuse Treatment, National Institute on Alcohol Abuse and Alcoholism, National Institute on Drug Abuse, Robert Wood Johnson Foundation and Interventions Foundation) and conducted in a variety of institutional settings, including across adolescent and adult levels of care, student assistance programs, criminal and juvenile justice agencies, mental health agencies, and child protective service and family service agencies. All data were collected as part of general clinical practice or specific research studies under their respective voluntary consent procedures and were subsequently de-identified.
Sample Characteristics
The pooled data are based on GAIN interviews with 6,177 adolescents (age 10–17) and 1,805 adults (age 18–69). Table 1 shows the demographic and clinical characteristics of the sample by adolescent (average age 16) and adults (average age 34). The adolescents were significantly more likely than adults to be male and involved in the justice system, but less likely to be African American or entering residential treatment. Clinically, adolescents had slightly more total past-year symptoms on the GAIN’s General Individual Severity Scale and had a different pattern of symptoms as compared to adults; on average, adolescents reported significantly fewer past-year symptoms on the Internal Mental Distress Scale (internalizing disorder symptoms) and Substance Problem Scale (abuse/dependence/induced symptoms) and significantly more past-year symptoms than adults on the Behavior Complexity Scale (externalizing disorder symptoms) and Crime/Violence Scale. The bottom half of the table shows the difference in the patterns using the items to create diagnostic/categorical groups. Adolescents were significantly less likely than adults to meet criteria for internalizing disorders and substance dependence; adolescents were more likely to meet criteria for substance abuse, externalizing disorders, and crime/violence problems.
TABLE 1.
Sample Characteristics Based on Full GAIN Assessment by Agea
| Characteristic | Adolescent (n = 6,177) | Adult (n = 1,805) |
|---|---|---|
| Age – Mean (SD) | 16 (1.5) | 34 (9.1) |
| Male (%) | 73 | 49 |
| Race-Ethnicity: African American (%) | 17 | 52 |
| Caucasian (%) | 48 | 40 |
| Hispanic (%) | 14 | 3 |
| Mixed/Other (%) | 21 | 5 |
| Current Involvement in Juvenile/Criminal Justice System | 71 | 52 |
| Residential Treatment | 34 | 56 |
| General Individual Severity Scale (GISS) – Mean (SD)b | 37 (22.9) | 35 (23.6) |
| Internal Mental Distress Scale (IMDS) – Mean (SD) | 10 (9.1) | 13 (11.1) |
| Behavior Complexity Scale (BCS) – Mean (SD) | 12 (8.3) | 8 (8.6) |
| Substance Problem Scale (SPS) – Mean (SD) | 8 (4.9) | 10 (5.0) |
| Crime/Violence Scale (CVS) – Mean (SD) | 8 (6.2) | 4 (4.8) |
| Any Past Year Disorderc (%) | 94 | 94 |
| Any Past Year Internalizing Disorder (%) | 56 | 68 |
| Depression (%) | 37 | 53 |
| Anxiety (%) | 21 | 44 |
| Traumatic Distressd (%) | 42 | 50 |
| Suicidale (%) | 16 | 20 |
| Any Past Year Externalizing Disorder (%) | 66 | 40 |
| Attention Deficit/Hyperactivity Disorder (%) | 48 | 33 |
| Conduct Disorder (%) | 58 | 30 |
| Any Past Year Substance Use Disorder (%) | 86 | 90 |
| Dependence (%) | 56 | 76 |
| Abuse (%) | 29 | 13 |
| Any Past Year Crime/Violence Problems (%) | 66 | 41 |
| High Physical Conflictf (%) | 22 | 11 |
| Mod/High General Crimeg (%) | 64 | 37 |
All differences by age are significant at p < .05 level using a Wilcoxon Rank order test for continuous measures and Chi-square test for nominal variables.
Total symptom count which includes all of the symptoms in the four scales listed below.
Includes any of the diagnoses listed under the four domains below.
Includes Post Traumatic Distress, Acute Traumatic Distress and traumatic distress associated with Child Maltreatment / Interpersonal Violence that may be complex and both in the past and ongoing.
Any suicidal thoughts, plans, means or attempts.
Physical violence towards others based on the GAIN’S variation of the Conflict Tactic Scale.
Any illegal activities across the FBI’s Uniform Crime Report categories beyond simple possession/use.
The GAIN Family of Measures
The participant characteristics, dimensional measures and clinical diagnoses/problems were all based on participant self report to in-person interviews with the GAIN.1 The full GAIN is a 90- to 120-minute standardized biopsychosocial measure that integrates clinical and research assessment into one comprehensive structured interview with eight main sections (background, substance use, physical health, risk behaviors, mental health, environment, legal, and vocational). The full GAIN has 103 scales and indices to assess problems, measure change and document service utilization. The GAIN incorporates DSM-IV-TR33 symptoms for common disorders (discussed further below), American Society of Addiction Medicine’s (ASAM),47 Patient Placement Criteria for the Treatment of Substance-Related Disorders, Joint Commission on Accreditation of Healthcare Organization (JCAHO)48 epidemiological questions from the National Household Survey on Drug Abuse (NHSDA),49 and items which have been economically valued for benefit cost analysis with adults and adolescents by Dr. Michael French over the past decade.50–51 The GAIN’s main scales have demonstrated excellent to good internal consistency (alpha over .90 on main scales, .70 on subscales), and test-retest reliability (Rho over .70 on problem counts, Kappa over .60 on categorical measures). GAIN measures have been validated with time line follow-back methods, urine tests, collateral reports, treatment records, and blind psychiatric diagnosis (Rho of .70 or more; Kappa of .60 or more).24,38,52–57 The GAIN has also been applied to predict substance use relapse and recidivism to crime up to 30 months later.58–59 A more detailed list of studies, copies of the actual GAIN instruments/items (full and short screener), and the syntax for creating the scales and diagnostic group variables are publicly available at www.chestnut.org/li/gain.
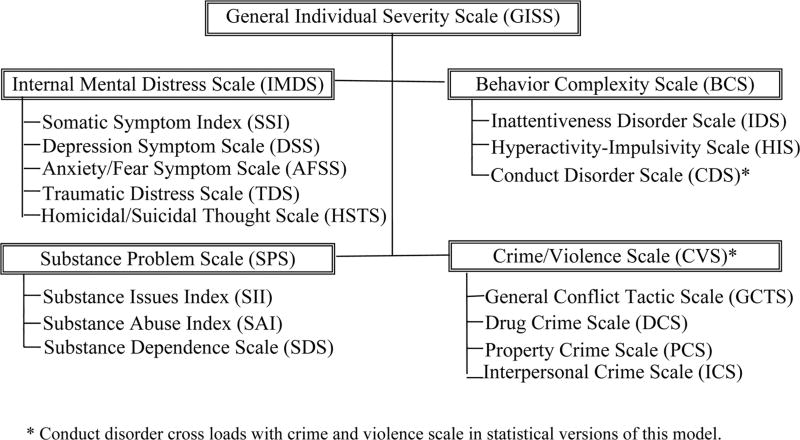
The GAIN Model of Emotional/Behavioral Problems
Figure 1 shows the substantive-statistical model of emotional and behavioral problems on which the full GAIN is based. It presumes that there is an underlying second order factor of multi-morbidity that can be represented by a total symptom count called General Individual Severity Scale (GISS; 123 items, alpha of .97 in adolescents and .97 in adolescent). These symptoms can be divided into four main dimensions represented by the:
The Internal Mental Distress Scale (IMDS; 43 items, alpha of 0.94 with adolescents and .96 with adults), which is a count of past-year symptoms related to internalizing disorders, including somatic, anxiety, depression, traumatic stress and suicide thoughts; it is based on the DSM-IV-TR (APA),33 the Hopkins Symptom Checklist 90 (HSCL-90),60–61 the Mississippi Scale of Post Traumatic Stress Disorder (PTSD)62–65 and common screening items for suicide risk (homicidal thoughts, suicidal thoughts, plans, means, attempts).
The Behavior Complexity Scale (BCS; 33 items, alpha of 0.94 with adolescents and .96 with adults), which is a count of past-year symptoms related to externalizing disorders, including attention deficit, hyperactivity/impulsivity, and conduct disorder; it is based on the DSM-IV-TR (APA)33 symptoms/disorders that are most common in adolescents but still persist into adulthood are correlated with substance use severity.39
The Substance Problem Scale (SPS; 16 items, alpha of 0.90 with adolescents and .92 with adults), which is a count of past-year symptoms related to any alcohol or drug use disorders, including abuse, dependence, substance induced health and psychiatric problems; it is based on the DSM-IV-TR (APA)33 and is associated with increased odds of internalizing and externalizing disorders.39
Crime/Violence Scale (CVS; 31 items, alpha of 0.90 with adolescents and .89 with adults), which is a count of increasingly violent strategies used for resolving interpersonal conflict in the past year and the types of drug related, property, and interpersonal crimes the respondent has committed; it is based on the Conflict Tactic Scale introduced in the Family Violence Survey66 and lay versions of the Federal Bureau of Investigations67 uniform crime report (UCR) categories introduced in the 1995 NHSDA49 and predicts future crime and violence.58–59
FIGURE 1.
GAIN Model of Emotional and Behavioral Problems
Under each of these four dimensions, there are 15 specific subscales that relate to a given type of diagnosis or problem (e.g., depression, conduct disorder, dependence, property crime) that can be important for deciding the most appropriate clinical intervention. For the purpose of the screener, however, we have focused on the fact that symptoms/disorders within the same dimension tend to be more highly correlated (e.g., depression and anxiety are more related than depression and violent crime).
Confirmatory factor analysis of the model in Figure 1 suggests that it closely fits the actual data with two caveats. First, there is a further loading between Crime/Violence and Conduct Disorder. Second, though structurally similar, adolescent and adult models fit better when their coefficients are calculated separately in terms of both confirmatory fit index (CFI; .83 constrained to the same coefficients across age vs. .92 if coefficients are allowed to vary by age) and Root Mean Square Error of Approximation (RMSEA; .08 constrained to the same vs. .06 if allowed to vary by age). Hu and Bentler68 suggest CFI should be over .9 and RMSEA under .6, so in this paper we have analyzed adult and adolescent data separately.
Development of the GAIN-Short Screener (GSS) Measures
As noted above, the GSS was developed to quickly identify who is likely to have an internalizing, externalizing, substance use or crime/violence diagnosis overall and to triage them by the kinds of emotional/behavioral health interventions that are likely to be appropriate. To be clear, it presumes that once you get people to the right program, a full GAIN or other more detailed assessment would be done there. Thus, this is a screener in the traditional sense, not a replacement for a detailed assessment.
We developed a 20-item GSS using 5 items for each of the four factors in Figure 1. Within each factor we selected at least one item from each of the subscales in the factor. The initial selection of items was based on the highest item-total correlation with the rest of the sub-scale and scale. A Rasch69 analysis with Winsteps70 was then applied to determine the relative item severity on the latent dimension represented by the four respective dimensions of Figure 1. For each dimension, we then constructed a chart with Rasch severity on the x-axis and the cumulative percent with a diagnosis on the y-axis. Using the resulting S-curve, we identified the transitional range of diagnostic uncertainty. Below this range, less than 10% of the patients had a diagnosis in this dimension; above this range over 90% of the patients had a diagnosis in this dimension. To achieve a high correlation between the screener and the full dimensional measure, we then adjusted the selection of items to make sure that the five items were spread as evenly as possible across this range of diagnostic uncertainty. (This technique was actually borrowed from a computer adaptive testing procedure developed by Riley and colleagues71 that has been used with the GAIN’s Substance Problem Scale.) The above process was done separately for adolescents and adults. The item that worked the best on average in both was used. The final 20-item version has a Total Disorder Screener (TDScr) with four 5-item subset screeners that correspond to the model in Figure 1 (Internalizing Disorder Screener (IDScr), Externalizing Disorder Screener (EDScr), Substance Disorder Screener (SDScr) and Crime/Violence Screener (CVScr). While the GSS (and all GAIN measures) are copyrighted and there is a license fee of $100, there is no per use fee, it has open syntax for scoring, and is available on line to preview for free (http://www.chestnut.org/LI/gain/GAIN_SS/index.html).
Validation Procedures
The 20 items in the GSS will be used to predict the dimensional and/or categorical values from the 123 diagnostic items in the full GAIN. For this analysis, if a single item was missing on any GSS or full GAIN measure, it would be replaced based on the average value for the relevant subscale or screener. Individual items were missing in less than 2% of the cases.
The GSS dimensional measures were validated based on a confirmatory factor analysis, a comparison of the Pearson correlation matrix between the full and screener scales, internal consistency based on Cronbach’s alpha and a measure “efficiency” as defined in equation (1).
| (1) |
Thus, efficiency goes down (good) the fewer items that are used and up (bad) the less the screener is correlated with the full scale. To verify that each sub-screener has discriminant validity, we compared the correlation of the sub-screener with the full GAIN scale that it was drawn from with the average correlation of the sub-screener with the other three GAIN dimensional scales.
The GSS cut points were validated based on sensitivity (the percentage of people with disorders on the full GAIN correctly identified by the GSS), specificity (percentage of people without a disorder on the full GAIN correctly excluded by the GSS) and the percentage of area under the curve (AUC) in a Receiver Operating Characteristics (ROC) analysis plotting the sensitivity (y-axis) against 1-specificity (x-axis). The optimal cut point is the one closest to or above 90% sensitivity, 90% specificity and 90% under the curve in the upper left corner (with values of 80% being good and 70% being fair). These analyses were done separately for adolescents and adults for the total screener and each of the four 5-item sub-screeners.
RESULTS
Validation of Dimensional Measures
Table 2 compares the GAIN Short Screener (GSS) measures in columns with the full GAIN measures in rows. The 20-item Total Disorder Screener represents only 17% of the 123 items in the full GAIN’s General Individual Severity Scale. While this made it less internally consistent (Cronbach’s alpha of .89 vs. .97), the GSS Total Disorder Screener was still highly correlated with the full GAIN’s General Individual Severity Scale (.94 for both adolescents and adults) and very efficient (efficiency = .17 for both, where lower than 1 is good). The four sub-screeners followed a similar pattern ranging from an 88% reduction in items (43 to 5) for internalizing disorders to a 68% reduction (16 to 5) for substance use disorders. This generally reduced the alpha from the excellent (.89 to .97) to moderate (.72 to .87) range with one major exception – the Crime/Violence Scale alpha for adults dropped from .89 to .65. The four sub-screeners, however, were still highly correlated with their respective longer version (Diagonal correlation of .84 to .90). Thus, the total and four sub-screeners reduced the number of items with minimal loss of information and are more efficient.
TABLE 2.
Internal consistency, efficiency and correlations of GAIN-SS with GAIN-I
| Correlationsa
|
|||||||
|---|---|---|---|---|---|---|---|
| Full GAIN-I Scale | GAIN-I No. of Items |
GAIN-I Cronbach’s Alpha |
Total Disorder Screener (TDScr)b |
Internalizing Disorder Screener (IDScr) |
Externalizing Disorder Screener (EDScr) |
Substance Disorder Screener (SDScr) |
Crime/ Violence Screener (CVScr) |
| Adolescent (n = 6,177) | |||||||
| General Individual Severity Scale (GISS)c | 123 | 0.97 | 0.94 | 0.73 | 0.77 | 0.66 | 0.68 |
| Internal Mental Distress Scale (IMDS) | 43 | 0.94 | 0.74 | 0.89 | 0.53 | 0.44 | 0.38 |
| Behavior Complexity Scale (BCS) | 33 | 0.94 | 0.81 | 0.52 | 0.88 | 0.49 | 0.55 |
| Substance Problem Scale (SPS) | 16 | 0.90 | 0.77 | 0.46 | 0.46 | 0.92 | 0.49 |
| Crime/Violence Scale (CVS) | 31 | 0.90 | 0.72 | 0.33 | 0.55 | 0.43 | 0.86 |
| GAIN-SS Number of items | 20 | 5 | 5 | 5 | 5 | ||
| GAIN-SS Cronbach’s Alpha | 0.87 | 0.74 | 0.76 | 0.76 | 0.72 | ||
| GAIN-SS Efficiencyd | 0.17 | 0.13 | 0.17 | 0.34 | 0.19 | ||
| Average non-diagonal Re | 0.44 | 0.51 | 0.45 | 0.47 | |||
| Adults (n = 1,805) | |||||||
| General Individual Severity Scale (GISS)c | 123 | 0.97 | 0.94 | 0.80 | 0.81 | 0.64 | 0.52 |
| Internal Mental Distress Scale (IMDS) | 43 | 0.96 | 0.79 | 0.90 | 0.62 | 0.46 | 0.27 |
| Behavior Complexity Scale (BCS) | 33 | 0.96 | 0.80 | 0.60 | 0.90 | 0.44 | 0.40 |
| Substance Problem Scale (SPS) | 16 | 0.92 | 0.75 | 0.47 | 0.43 | 0.93 | 0.36 |
| Crime/Violence Scale (CVS) | 31 | 0.89 | 0.62 | 0.31 | 0.49 | 0.35 | 0.84 |
| GAIN-SS Number of items | 20 | 5 | 5 | 5 | 5 | ||
| GAIN-SS Cronbach’s Alpha | 0.87 | 0.79 | 0.81 | 0.78 | 0.65 | ||
| GAIN-SS Efficiencyd | 0.17 | 0.13 | 0.17 | 0.33 | 0.19 | ||
| Average non-diagonal Re | 0.46 | 0.51 | 0.42 | 0.34 | |||
All correlations are significant, p < .001.
The Total Disorder Screener includes all the items in the four screeners to the right.
The General Individual Severity Scale includes all of the items in the four scales below it.
Efficiency = (# of screener items/# of full scale items). *1/(diagonal correlation).
The average correlation of the (sub) screener with the three (non-diagonal) full GAIN scales in the column.
To test the ability of the four sub-screeners to differentiate the types of problems we also examined their discriminant validity and overall structure (Table 2). The diagonal correlation with the scale that the screener items were drawn from was 1.7 to 2.5 times larger than the correlation of each screener with the other three scales from the full GAIN for the internalizing disorder screener (.89 diagonal vs. .44 average non diagonal for adolescents and .90 vs. .46 for adults), externalizing disorder screener (.88 vs. .51 for adolescents and .90 vs. .51 for adults), substance disorder screener (.92 vs. .45 for adolescents and .93 vs. .42 for adults) and crime/violence screener (.86 vs. .47 for adolescents and .84 vs. .34 for adults).
A confirmatory factor analysis of the structure of the GSS shows that it is also consistent with the regular GAIN model in Figure 1 after allowing adolescents and adults to vary and the cross loading of conduct disorder items with crime/violence. The confirmatory factor analysis was slightly worse than the full-scale version in terms of the confirmatory fit index (CFI; .87 for GSS vs. .92 for the full GAIN, where up is good) and slightly better in terms of Root Mean Square Error of Approximation (RMSEA; .05 for GSS vs. .06 for the full GAIN, where down is good). This suggests that each of the sub-screeners has good discriminant validity and that the total structure is consistent with the model used with the full GAIN.
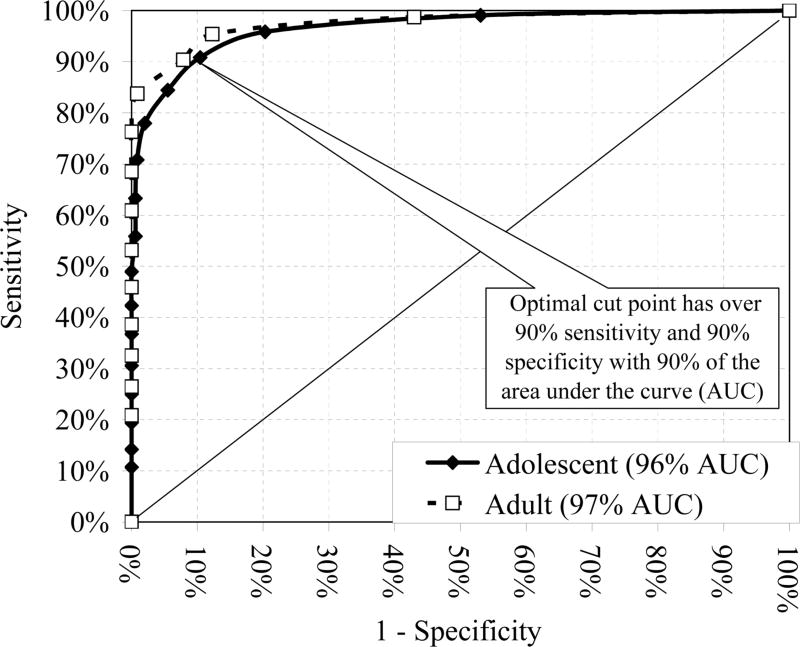
Optimization and Validation of Cut Points
Table 3 gives the sensitivity, specificity, and area under the curve for cut points of 1, 2, and 3 or more symptoms on the total and each of the four sub-screeners relative to respective diagnoses for that dimension. For the Total Disorder Screener it takes a cut point of 3 or more to get a balance of 90% + sensitivity and 90% + specificity. Figure 2 shows this graphically with the results of the Receiver Operator Characteristics (ROC) analysis. The Total Disorder Screener was very well behaved, with 96% of area under the curve for adolescents and 97% for adults. These differences were not significantly different by age (X2(1) = 3.2, n.s.d.). For both adolescents and adults, 3 or more past-year symptoms on the GSS is the closest to the optimal point of 90% sensitivity and specificity).
TABLE 3.
Sensitivity, specificity, and area under the curve (AUC) between GAIN-SS cut points and self-reported GAIN-I diagnoses by agea
| Adolescent (n = 6,177)
|
Adult (n = 1,805)
|
||||||
|---|---|---|---|---|---|---|---|
| Screener | Cut off | % Sensitivity |
% Specificity |
% AUC |
% Sensitivity |
% Specificity |
% AUC |
| Total Disorder Screener (TDScr)b | > = 1 | 99 | 47 | 99 | 57 | ||
| > = 2 | 96 | 80 | 96 | 95 | 88 | 97 | |
| > = 3 | 91 | 90 | 90 | 92 | |||
| Internalizing Disorder Screener (IDScr)c | > = 1 | 94 | 71 | 97 | 74 | 96* | |
| > = 2 | 77 | 95 | 92 | 87 | 94 | ||
| > = 3 | 55 | 99 | 71 | 100 | |||
| Externalizing Disorder Screener (EDScr)d | > = 1 | 98 | 75 | 97 | 81 | ||
| > = 2 | 86 | 88 | 94 | 85 | 93 | 95* | |
| > = 3 | 66 | 96 | 66 | 98 | |||
| Substance Disorder Screener (SDScr)e | > = 1 | 96 | 73 | 97 | 73 | ||
| > = 2 | 86 | 93 | 95 | 91 | 96 | 97* | |
| > = 3 | 68 | 100 | 80 | 100 | |||
| Crime/Violence Screener (CVScr)f | > = 1 | 94 | 76 | 91 | 87 | ||
| > = 2 | 70 | 99 | 93 | 52 | 100 | 92 | |
| > = 3 | 49 | 99 | 28 | 100 | |||
Sensitivity is the percent of people with a diagnosis on the GAIN-I correctly identified by screener at a given cut point or above; specificity is the percent of people without the diagnosis correctly rejected by the screener at a given cut point or above; and AUC is the area under the curve formed by 1-specificity on the x-axis and sensitivity on the y-axis (see Figure 1 & 2).
These AUC are all significantly different by age at p < .05.
Relative to detecting any of the disorders listed below.
Relative to detecting any internalizing disorder (Depression, Anxiety, Trauma, Suicide Ideation) on the full GAIN.
Relative to detecting any externalizing disorder (Attention Deficit, Hyperactivity, Impulse Control, Conduct) on the full GAIN.
Relative to detecting any substance use disorder (Abuse, Dependence) on the full GAIN.
Relative to detecting any crime/violence problem (high interpersonal conflict, any drug, property, or interpersonal/violent crime).
FIGURE 2.
Receiver Operator Characteristics (ROC) of the GSS Total Disorder Screener (TDScr) Relative to the Full GAIN
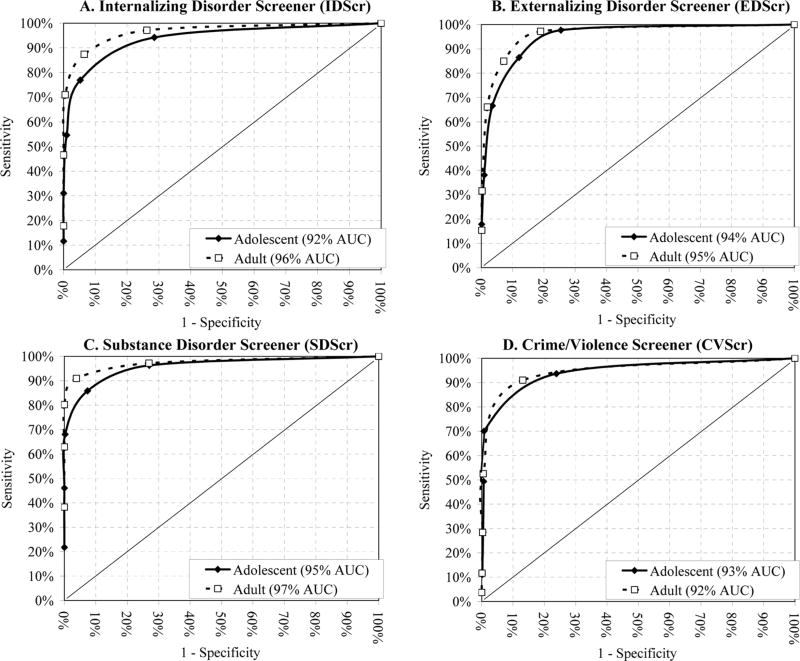
All four of the sub-screeners have 92% or more of their area under the curve for both adolescents and adults. However, as illustrated in Table 3 and Figure 3, there is generally no one optimal cut point on the sub-screeners with 90% + sensitivity and specificity. The one exception is the Substance Disorders Screener that meets this criterion at the 2 + cut-point for adults only. In the absence of a single optimal cut point, it is possible to triage the score into three groups: 0 (unlikely), 1–2 (possible), and 3–5 (probable) for which the lower cut point (1 +) has 90% sensitivity and the upper cut point (3 +) has 90% specificity. Comparisons of the ROC curves by ages suggest that the GSS worked slightly better for adults than adolescent on the Internalizing Disorder Screener (X2(1)) = 45.0, p < .0001), Externalizing Disorder Screener (X2(1)) = 5.4, p < .05), and the Substance Disorder Screener (X2(1)) = 18.2, p <. 0001).
FIGURE 3.
ROC of the GAIN Short Screener (GSS) Subscales Relative to the Full GAIN
DISCUSSION
Reprise
In this study we described the development of the 20-item GAIN-Short Screener (GSS) and validated its ability to serve as an efficient tool for reliably assessing psychopathology and crime/violence as a dimensional measure and as a screener to identify people who are likely to have diagnoses and require clinical services. While it would not be sufficient to render a specific diagnosis, the GSS appears capable of quickly identifying who has a possible or probable diagnosis/problem and triaging the problem into four dimensions of severity: internalizing disorders, externalizing disorder, substance disorders, and crime/violence problems.
Recommended Cut Points
Based on these analyses we recommend that the total and four sub-screeners be triaged into three groups for clinical decision making:
Low (0), who are unlikely to need services;
Moderate (1–2), who have a possible diagnosis and are likely to benefit from a brief intervention; and
High (3 or more) who have a high probability of a diagnosis and need more formal assessment and intervention (either directly or through referral).
These same ranges apply to the total and sub-screeners. As shown in the results section, moderate or above (1+) will have 90% or more sensitivity within a sub-screener and high will have 90% or more specificity. A manual is available on line to further support placement and treatment planning based on these cut points.72
In practice, most clinicians will want to look for a score of 3 or more on the Total Disorder Screener and then assume that services are needed in each of the four domains with scores of 1 or more. Thus, if you reported 5 symptoms − 3 on the Externalizing Disorder Screener and 2 on the Substance Disorder Screener, you would meet criteria for needing services and be referred to a program(s) to meet your externalizing and substance disorder needs. One very important caveat: this is just a screener based on self-reports. Clinicians should still be encouraged to combine it with other information (e.g., from a parent, spouse, probation officer, supervisor, records) and/or to override it on individual cases where they suspect other problems. It is designed to be a tool to facilitate clinical judgment, not override it.
Strengths and Limitations
This paper has several strengths including a large/diverse sample, being based on a full instrument that has a formal measurement model, and advanced statistical analyses. There are, however, some notable limitations of this paper that should be acknowledged. First, the analysis is based entirely on self-reported data. Second, the comparisons are between a part and whole scale collected at the exact same time. If there were alternative data available and/or more elapsed time, the comparisons would presumably come out lower. We are currently working with several treatment, school, workplace, mental health, justice and welfare programs to collect such data and hope to report those findings in the near future. Third, while GSS is an efficient screener to identify who is likely to have a disorder in a given area and might need further assessment, more information will typically need to be collected later to make a full diagnosis.
Next Steps
Because of its efficiency and ease of implementation (minimal training and 2 pages per administration), the GSS also has the potential to help with policy and program planning. This is important for the increasing number of federal, state and local initiatives to mandate or encourage standardized screening across a wide range of systems. This might include school, workplace, welfare and justice system that are increasingly interested in early identification and intervention related to behavioral health issues. The GSS can be used as a simple form of needs assessment to help guide program planning and the purchase of further training or technical assistance. For program evaluation, this simple measure can also be used to “predict” the number of people with each diagnosis or types of services needed and to evaluate/manage penetration and referral rates. It may also prove useful as a short measure of change that could be used to track reductions in symptoms in each of the four dimensions. Use of the GSS in these other settings and applications, however, still needs to be evaluated.
Conclusion
In conclusion, it is important to recognize that assessment costs money and staff/client time. Rather than one size fits all, we have consistently advocated a more progressive approach to assessment - screening general populations, a brief assessment for targeted populations and full assessment for more complicated/multi-morbid populations. We believe that the GAIN Short Screener (GSS) has great potential to serve as both a cost-effective front door screener to identify people with co-occurring disorders across multiple systems and route them to the right services and more detailed assessments.
Acknowledgments
The development of this paper was supported by the Center for Substance Abuse Treatment (CSAT), Substance Abuse and Mental Health Services Administration (SAMHSA) via Westat under contract 270–2003–00006 to Dr. Dennis at Chestnut Health Systems in Bloomington, Illinois using data provided by the following grants and contracts from CSAT (TI11320, TI11324, TI11317, TI11321, TI11323, TI11874, TI11424, TI11894, TI11871, TI11433, TI11423, TI11432, TI11422, TI11892, TI11888, TI013313, TI013309, TI013344, TI013354, TI013356, TI013305, TI013340, TI130022, TI03345, TI012208, TI013323, TI14376, TI14261, TI14189, TI14252, TI14315, TI14283, TI14267, TI14188, TI14103, TI14272, TI14090, TI14271, TI14355, TI14196, TI14214, TI14254, TI14311, TI15678, TI15670, TI15486, TI15511, TI15433, TI15479, TI15682, TI15483, TI15674, TI15467, TI15686, TI15481, TI15461, TI15475, TI15413, TI15562, TI15514, TI15672, TI15478, TI15447, TI15545, TI15671, TI11320, TI12541, TI00567; Contract 207–98–7047, Contract 277–00–6500), the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (R01 AA 10368), the National Institute on Drug Abuse (NIDA) (R37 DA11323; R01 DA 018183), the Illinois Criminal Justice Information Authority (95-DB-VX-0017), the Illinois Office of Alcoholism and Substance Abuse (PI 00567), the Interventions Foundation’s Drug Outcome Monitoring Study (DOMS), and the Robert Wood Johnson Foundation’s Reclaiming Futures (45054, 45059, 45060, 45053, 047266).
Footnotes
The opinions are those of the author and do not reflect official positions of the contributing project directors or government.
References
- 1.Dennis ML, Titus JC, White M, et al. Global Appraisal of Individual Needs (GAIN): Administration Guide for the GAIN and Related Measures. Version 5 ed. Bloomington, IL: Chestnut Health Systems; 2003. [Accessed April 6, 2006]. Available at: www.chestnut.org/li/gain. [Google Scholar]
- 2.Angst J, Sellaro R, Ries MK. Multimorbidity of psychiatric disorders as an indicator of clinical severity. European Archives of Psychiatry and Clinical Neuroscience. 2002;252:147–154. doi: 10.1007/s00406-002-0357-6. [DOI] [PubMed] [Google Scholar]
- 3.Kandel DB, Johnson JG, Bird HR, et al. Psychiatric comorbidity among adolescents with substance use disorders: Findings from the MECA study. J Am Acad Child Adolesc Psychiatry. 1999;38:693–699. doi: 10.1097/00004583-199906000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Nelson CB, McGonagle KA, et al. The epidemiology of co-occurring addictive and mental disorders: Implications for prevention and service utilization. Am J OrthoPsychiatry. 1996;66:17–31. doi: 10.1037/h0080151. [DOI] [PubMed] [Google Scholar]
- 5.Kessler RC, Chiu WT, Dernier O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krueger RF, Markon KE. Reinterpreting Comorbidity: A Model-Based Approach to Understanding and Classifying Psychopathology. Annu Revof Clin Psychology. 2006;2:111–113. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- 8.Crowley TJ, Riggs PD. Adolescent substance use disorder with conduct disorder and comorbid conditions. In: Rahdert ER, Czechowicz D, editors. Adolescent Drug Abuse: Clinical Assessment and Therapeutic Interventions. Rockville, MD: National Institute on Drug Abuse; 1995. pp. 49–111. [PubMed] [Google Scholar]
- 9.Diamond G, Panichelli-Mindel SM, Shera D, et al. Psychiatric syndromes in adolescents seeking outpatient treatment for marijuana with abuse and dependency in outpatient treatment. J Child Adoles Subst Abuse. 2006;15:37–54. [Google Scholar]
- 10.Eronen M, Angermeyer MC. The psychiatric epidemiology of violent behaviour. Social Psychiatry and Psychiatc Epidemiol. 1998;33(S1):S13–S23. doi: 10.1007/s001270050205. [DOI] [PubMed] [Google Scholar]
- 11.Gretton HM, Hare RD, Catchpole REH. Psychopathy and offending from adolescence to adulthood: A 10-year follow-up. J Consult Clin Psychol. 2004;72:636–645. doi: 10.1037/0022-006X.72.4.636. [DOI] [PubMed] [Google Scholar]
- 12.Mueser KT, Yarnold PR, Levinson DF, et al. Prevalence of substance abuse in schizophrenia: Demographic and clinical correlates. Schizophr Bull. 1990;16:31–56. doi: 10.1093/schbul/16.1.31. [DOI] [PubMed] [Google Scholar]
- 13.Latimer WW, Stone AL, Voight A, et al. Gender differences in psychiatric comorbidity among adolescents with substance use disorders. Exp Clin Psychopharmacology. 2002;10:310–315. doi: 10.1037//1064-1297.10.3.310. [DOI] [PubMed] [Google Scholar]
- 14.Loeber R, Farrington DP, Stouthamer-Loeber M, et al. Male mental health problems, psychopathy, and personality traits: Key findings from the first 14 years of the Pittsburgh Youth Study. Clin Child Fam Psychol Rev. 2001;4:273–297. doi: 10.1023/a:1013574903810. [DOI] [PubMed] [Google Scholar]
- 15.Ross HE, Glaser FB, Germanson T. The prevalence of psychiatric disorders in patients with alcohol and other drug problems. Arc Gen Psychiatry. 1988;45:1023–1031. doi: 10.1001/archpsyc.1988.01800350057008. [DOI] [PubMed] [Google Scholar]
- 16.Skeem JL, Mulvey EP. Psychopathy and community violence among civil psychiatric patients: Results from the MacArthur Violence Risk Assessment Study. Journal of Consult Clin Psych. 2001;69:358–374. [PubMed] [Google Scholar]
- 17.Brooner RK, King VL, Kidorf M, et al. Psychiatric and substance use comorbidity among treatment-seeking opioid abusers. Arch Gen Psychiatry. 1997;54:71–80. doi: 10.1001/archpsyc.1997.01830130077015. [DOI] [PubMed] [Google Scholar]
- 18.Cornelius JR, Maisto SA, Martin CS, et al. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav. 2004;29:1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- 19.McLellan AT, Luborsky L, Woody GE, et al. Prediction response to alcohol and drug abuse treatments. Arch Gen Psychiatry. 1983;40:620–628. doi: 10.1001/archpsyc.1983.04390010030004. [DOI] [PubMed] [Google Scholar]
- 20.Mueser KT, Drake RE, Miles KM. The course and treatment of substance use disorder in persons with severe mental illness. In: Onken LS, Blaine JD, Genser S, Horton AM, editors. Treatment of Drug-Dependent Individuals with Comorbid Mental Disorders. National Institute on Drug Abuse; 1997. [Google Scholar]
- 21.Hien DA, Nunes E, Levin FR, et al. Posttraumatic stress disorder and short-term outcome in early methadone treatment. J Subst Abuse Treat. 2000;19:31–37. doi: 10.1016/s0740-5472(99)00088-4. [DOI] [PubMed] [Google Scholar]
- 22.Project MATCH Research Group. Project MATCH secondary a priori hypotheses. Addiction. 1997;92:1671–1698. [PubMed] [Google Scholar]
- 23.Rounsaville BJ, Kosten TR, Weissman MM, et al. Prognostic significance of psychiatric disorders in treated opiate addicts. Arch Gen Psychiatry. 1986;43:739–745. doi: 10.1001/archpsyc.1986.01800080025004. [DOI] [PubMed] [Google Scholar]
- 24.Shane P, Jasiukaitis P, Green RS. Treatment outcomes among adolescents with substance abuse problems: The relationship between comorbidities and post-treatment substance involvement. Eval Prog Plann. 2003;26:393–402. [Google Scholar]
- 25.Bijl RV, de Graaf R, Hiripi E, et al. The Prevalence of Treated and Untreated Mental Disorders in Five Countries. Health Afs. 2003;22:122–133. doi: 10.1377/hlthaff.22.3.122. [DOI] [PubMed] [Google Scholar]
- 26.Clark HW, Horton AM, Jr, Dennis ML, et al. Moving from research to practice just in time: The treatment of cannabis use disorders comes of age. Addiction. 2002;97:S1–S3. doi: 10.1046/j.1360-0443.97.s01.11.x. [DOI] [PubMed] [Google Scholar]
- 27.Drug and Alcohol Services Information System (DASIS) Admissions with Co-Occurring Disorders: 1995 and 2001. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; [Accessed April 20, 2006]. Available at: http://www.oas.samhsa.gov/2k4/dualTX/dualTX.htm. [Google Scholar]
- 28.Drug and Alcohol Services Information System (DASIS) Adolescents with Co-Occurring Psychiatric Disorders: 2003. Rockville, MD: Office of Applied Studies, Substance Abuse and Mental Health Services Administration; [Accessed April 20, 2006]. Available at: http://www.oas.samhsa.gov/2k5/youthMH/youthMH.htm. [Google Scholar]
- 29.Center for Substance Abuse Treatment. Substance Abuse Treatment for Persons With Co-Occurring Disorders. Treatment Improvement Protocol (TIP) Series 42. DHHS Publication No. (SMA) 05-3992. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2005. [PubMed] [Google Scholar]
- 30.Center for Substance Abuse Treatment. Assessment and Treatment of Patients with Coexisting Mental Illness and Alcohol and Other Drug Abuse. Rockville, MD: Substance Abuse and Mental Health Services Administration; 1994. [PubMed] [Google Scholar]
- 31.Substance Abuse and Mental Health Services Administration. Report to Congress on the Prevention and Treatment of Co-Occurring Substance Abuse Disorders and Mental Disorders. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2002. [Google Scholar]
- 32.Weisner C, McLellan T, Barthwell A, et al. Report of the Blue Ribbon Task Force on Health Services Research at the National Institute on Drug Abuse. Rockville, MD: National Institute on Drug Abuse; 2004. [Google Scholar]
- 33.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR). 4th – text revision ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 34.Achenbach TM, Edelbrock CS. The classification of child psycho-pathology: A review and analysis of empirical efforts. Psychol Bull. 1978;85:1275–1301. [PubMed] [Google Scholar]
- 35.Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- 36.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): A longitudinal-epidemiological Study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 37.Vollebergh W, Iedema J, Bijl RV, et al. The structure and stability of common mental disorders: The NEMESIS study. Arch Gen Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- 38.Dennis ML, Dawud-Noursi S, Muck RD, et al. The need for developing and evaluating adolescent treatment models. In: Stevens SJ, Morral AR, editors. Adolescent Substance Abuse Treatment in the United States: Exemplary Models from a National Evaluation Study. Binghamton, NY: Haworth Press; 2003. pp. 3–34. [Google Scholar]
- 39.Chan YF, Dennis ML, Funk RR. Prevalence and comorbidity of major mental disorders among adolescents and adults presenting to substance abuse treatment. Journal of Substance Abuse Treatment. doi: 10.1016/j.jsat.2006.12.031. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: Results from the National Comorbidity Survey Replication. American Journal of Psychiatry. 2006;163:716–723. doi: 10.1176/appi.ajp.163.4.716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levin FR, Evans SM, Kleber HD. Prevalence of adult attention-deficit hyperactivity disorder among cocaine abusers seeking treatment. Drug and Alcohol Dependence. 1998;52:15–25. doi: 10.1016/s0376-8716(98)00049-0. [DOI] [PubMed] [Google Scholar]
- 42.Wender PH, Wolf LE, Wasserstein J. Adults with ADHD: An overview. Annals of New York Academy of Science. 2001;931:1–16. [PubMed] [Google Scholar]
- 43.Wilson JJ, Levin FR. Attention Deficit Hyperactivity Disorder (ADHD) and substance use disorders. Current Psychiatry Reports. 2001;3:497–506. doi: 10.1007/s11920-001-0044-8. [DOI] [PubMed] [Google Scholar]
- 44.Hare RD, Neumann CS. Structural models of psychopathy. Curr Psychiatry Rep. 2005;7:57–64. doi: 10.1007/s11920-005-0026-3. [DOI] [PubMed] [Google Scholar]
- 45.Walters GD, Chlumsky ML. The lifestyle criminality screening form and antisocial personality disorder: Predicting release outcome in a state prison sample. Behav Sci Law. 1993;11:111–115. doi: 10.1002/bsl.2370110109. [DOI] [PubMed] [Google Scholar]
- 46.Walters GD. Predicting criminal justice outcomes with the Psychopathy Checklist and Lifestyle Criminality Screening Form: A meta-analytic comparison. Behav Sci Law. 2003;21:89–102. doi: 10.1002/bsl.519. [DOI] [PubMed] [Google Scholar]
- 47.American Society of Addiction Medicine (ASAM) Patient placement criteria for the treatment for substance-related disorders (2nd ed.) Chevy Chase, MD: American Society of Addiction Medicine; 2001. [Google Scholar]
- 48.Joint Commission on Accreditation of Healthcare Organizations. (JCAHO) Accreditation manual for mental health, chemical dependency, and mental retardation/developmental disabilities services: Standards (Vol. 1) Oakbrook Terrace, IL: Author; 1995. [Google Scholar]
- 49.Office of Applied Studies, Substance Abuse and Mental Health Services Administration. Preliminary Estimates from the 1995 National Household Survey on Drug Abuse. Rockville, MD: Author; 1996. Advance Report. [Google Scholar]
- 50.French MT, Bradley CJ, Calingaert B, et al. Cost analysis of training and employment services in methadone treatment. Eval Prog Plann. 1994;17:107–120. [Google Scholar]
- 51.French MT, Roebuck MC, Dennis ML, et al. Outpatient marijuana treatment for adolescents: Economic evaluation of a multisite field experiment. Eval Rev. 2003;27:421–459. doi: 10.1177/0193841X03254349. [DOI] [PubMed] [Google Scholar]
- 52.Dennis ML, Titus JC, Diamond G, et al. The Cannabis Youth Treatment (CYT) experiment: Rationale, study design, and analysis plans. Addiction. 2002;97:S16–S34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- 53.Dennis ML, Godley SH, Diamond G, et al. Main findings of The Cannabis Youth Treatment randomized field experiment. J Sub Abuse Treat. 2004;27:197–213. doi: 10.1016/j.jsat.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 54.Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Eval Prog Plann. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Godley MD, Godley SH, Dennis ML, et al. Preliminary outcomes from the assertive continuing care experiment for adolescents discharged from residential treatment. J Subst Abuse Treat. 2002;23:21–32. doi: 10.1016/s0740-5472(02)00230-1. [DOI] [PubMed] [Google Scholar]
- 56.Lennox RD, Dennis ML, Scott CK, et al. Combining psychometric and biometric measures of substance use. Drug Alcohol Depend. 2006;83:95–103. doi: 10.1016/j.drugalcdep.2005.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lennox RD, Dennis ML, Ives M, et al. The Construct and Predictive Validity of Different Approaches to Combining Urine and Self-Reported Drug Use Measures among Adolescents in Substance Abuse Treatment. Am J Addict. 2006;15(Suppl. 1):92–101. doi: 10.1080/10550490601006089. [DOI] [PubMed] [Google Scholar]
- 58.White M. Predicting violence in juvenile offenders: The interaction of individual, social, and environmental influences. Offender Subst Abuse Rep. 2005:83–90. [Google Scholar]
- 59.White MK, Funk R, White W, et al. Predicting violent behavior in adolescent cannabis users: The GAIN-CVI. Offender Subst Abuse Rep. 2003;3:67–69. [Google Scholar]
- 60.Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale-Preliminary report. Psychopharmaco Bull. 1973;9:13–28. [PubMed] [Google Scholar]
- 61.Lipman RS, Covi L, Shapiro AK. The Hopkins Symptom Checklist (HSCL): factors derived from the HSCL-90. J Affect Dis. 1979;1:9–24. doi: 10.1016/0165-0327(79)90021-1. [DOI] [PubMed] [Google Scholar]
- 62.King DW, King LA, Fairbank JA, Surface CR, et al. Enhancing the precision of the Mississippi Scale for Combat-Related Posttraumatic Stress Disorder: An application of item response theory. Psychological Assessment. 1993;5:457–471. [Google Scholar]
- 63.Kulka RA, Schlenger WE, Fairbank JA, et al. Assessment of Posttraumatic Stress Disorder in the community: Prospects and pitfalls from recent studies of Vietnam Veterans. Psychol Assess. 1991;3:547–560. [Google Scholar]
- 64.Scott CK, Sonis J, Creamer M, Dennis ML. Maximizing follow-up in longitudinal studies of traumatized populations. Journal of Traumatic Stress. doi: 10.1002/jts.20186. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Stevens SJ, Murphy BS, McKnight K. Traumatic stress and gender differences in relationship to substance abuse, mental health, physical health, and HIV risk behavior in a sample of adolescents enrolled in drug treatment. Child Maltreatment. 2003;8:46–57. doi: 10.1177/1077559502239611. [DOI] [PubMed] [Google Scholar]
- 66.Strauss MA. Conflict tactic scale. In: Strauss MA, Gelles RJ, editors. Physical Violence in American Families: Risk Factors and Adaptations to Violence in 8,145 Families. Durham, NH: University of New Hampshire; 1990. [Google Scholar]
- 67.Federal Bureau of Investigations. 1993 Uniform Crime Reports. Washington DC: [Accessed May 23, 2006]. Available at: http://www.fbi.gov/ucr. [Google Scholar]
- 68.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struc Equation Model. 1999;6:1–55. [Google Scholar]
- 69.Rasch G. Probabilistic models for some intelligence and attainment tests. Copenhagen, Denmark: Paedogogiske Institut; 1960. [Google Scholar]
- 70.Linacre JM. Winsteps computer program. Chicago: MESA Press; 2002. [Google Scholar]
- 71.Riley BB, Conrad KJ, Bezruczko N, et al. Relative precision, efficiency and construct validity of different starting and stopping rules for a computerized adaptive test: The GAIN substance problem scale. J Appl Measur. In press. [PMC free article] [PubMed] [Google Scholar]
- 72.Dennis M, Feeny T. GAIN Short Screener (GSS) Summary Guidelines for Administration and Scoring. Bloomington, IL: Chestnut Health Systems; 2006. [Accessed August 8, 2006]. Available at: from http://www.chestnut.org/LI/gain/GAIN_SS/index.html. [Google Scholar]