Abstract
The relevance of gene mutations leading to heart diseases and hence heart failure has become evident. The risk for and the course of heart failure depends on genomic variants and mutations underlying the so‐called genetic predisposition. Genetic contribution to heart failure is highly heterogenous and complex. For any patient with a likely inherited heart failure syndrome, genetic counselling is recommended and important. In the last few years, novel sequencing technologies (named next‐generation sequencing – NGS) have dramatically improved the availability of molecular testing, the efficiency of genetic analyses, and moreover reduced the cost for genetic testing. Due to this development, genetic testing has become increasingly accessible and NGS‐based sequencing is now applied in clinical routine diagnostics. One of the most common reasons of heart failure are cardiomyopathies such as the dilated or the hypertrophic cardiomyopathy. Nearly 100 disease‐associated genes have been identified for cardiomyopathies. The knowledge of a pathogenic mutation can be used for genetic counselling, risk and prognosis determination, therapy guidance and hence for a more effective treatment. Besides, family cascade screening for a known familial, pathogenic mutation can lead to an early diagnosis in affected individuals. At that timepoint, a preventative intervention could be used to avoid or delay disease onset or delay disease progression. Understanding the cellular basis of genetic heart failure syndromes in more detail may provide new insights into the molecular biology of physiological and impaired cardiac (cell) function. As our understanding of the molecular and genetic pathophysiology of heart failure will increase, this might help to identify novel therapeutic targets and may lead to the development of new and specific treatment options in patients with heart failure.
Keywords: cardiomyopathy, DCM, HCM, heart failure, cardiogenetics
Introduction
Heart failure is a continuously growing public health problem. Presently, almost 40 million people are affected by heart failure worldwide.1, 2, 3 In developed countries, the prevalence of heart failure is approximately 1–2% of the adult population.4, 5 Because of the ageing of our population in general, it is increasing in prevalence.6 Despite substantial improvements in medical treatments that delay onset and prolong life with heart failure, morbidity and mortality for this disease remain extremely high. Heart failure is associated with cognitive impairment, reduced exercise tolerance, and multiorgan impairment, which all reduce quality of life tremendously, particularly in the multimorbid older population. Besides, healthcare costs for heart failure are enormous as it is one of the main reasons leading to hospitalization among adults.
Heart failure is a clinical syndrome characterized by typical patient symptoms and physical examination findings caused by impaired ventricular function. Its treatment can be challenging as the term encompasses diverse underlying aetiologies. A broad range of cardiac diseases, inherited disorders, and systematic diseases can result in heart failure.3 The situation is even more complex, as heart failure can have mixed aetiologies, which mutually do not exclude each other. Heart failure itself represents a final common pathway in response to genetic and/or environmental influences.
Prevention of heart failure by identifying and treating risk factors and subclinical precursors currently represents a big challenge. Increasing evidence suggests that risk and course of heart failure depend on genetic predisposition. Recently, the involvement of mutations in various genes leading to heart diseases and hence heart failure has become clearer. Accurate and comprehensive genetic testing strategies might be a powerful tool to identify patients at risk and to treat heart failure in these patients more effectively. With genetic testing, patients at risk for heart failure could be identified before overt disease is present. At that timepoint, a preventative intervention could be used to avoid or delay disease onset or progression.
Familial (genetic) predisposition for heart failure
Susceptibility to heart failure often has a genetic and therefore heritable component. In the Framingham Offspring Study, parental heart failure was associated with asymptomatic left ventricular dysfunction and an increased risk for overt heart failure in the offspring.7 This study clearly demonstrated the importance of familial (genetic) factors as determinants of heart failure. In another large nationwide Swedish population study, the relevance of genetic factors as independent risk factors for heart failure was also shown: The risk for heart failure even increased in individuals having more than one sibling affected with heart failure.8 Moreover, this situation was associated with early onset of heart failure.
In children with heart failure, a familial origin is frequently identified.9, 10 In unselected adult heart failure populations, prevalence of heart failure caused by (monogenic) cardiomyopathies is probably lower compared with that in paediatric populations.
Genetic contribution to heart failure is heterogeneous and sometimes complex. At one end of the disease spectrum, there are familial monogenic heart failure syndromes with monogenic causative gene mutations with high penetrance. Mainly, they are inherited in an autosomal‐dominant way, less commonly in a recessive, mitochondrial, or X‐linked inheritance pattern. At the other end, heart failure susceptibility might be influenced by more common, but less penetrant, genetic variants. In that case, the cumulative effect of common variants interacts with environmental factors and determines heart failure susceptibility, and heart failure should be considered as a multifactorial disease.
A definition of (genetic) cardiomyopathies
One of the most common causes of heart failure are cardiomyopathies. In 2006, the American Heart Association described cardiomyopathies as a heterogeneous group of myocardial diseases that are predominantly genetic and associated with mechanical and/or electrical dysfunction.11 Two years later, the European Society of Cardiology provided their own classification of cardiomyopathies and defined them as ‘a myocardial disorder in which the heart muscle is structurally and functionally abnormal, in the absence of coronary artery disease, hypertension, valvular disease and congenital heart disease sufficient to cause the observed myocardial abnormality’.12 Based on specific morphological and functional phenotypes, cardiomyopathies can be clinically divided into five groups: dilated cardiomyopathy (DCM), hypertrophic cardiomyopathy (HCM), restrictive cardiomyopathy (RCM), arrhythmogenic right ventricular cardiomyopathy (ARVC), and unclassified cardiomyopathies such as the left ventricular non‐compaction cardiomyopathy (Figure 1 ). These five entities can be further subdivided into familial (genetic) and non‐familial (non‐genetic) forms. In 2013, the World Heart Federation concluded that ‘a substantial increase in the knowledge of the genetic basis of cardiomyopathy called for a standardized, universally acceptable classification/nosology system that integrates phenotype description as well as genetic information’.13 Therefore, the so‐called MOGE(S) nosology system was proposed, which describes cardiomyopathies not only according to the morphofunctional phenotype (M) but also according to organ involvement (O), genetic inheritance pattern (G), aetiological annotation (E) including genetic defect or underlying disease/substrate, and functional status (S) of the disease. This classification system offers a better flexibility in categorizing overlapping genetic and phenotypic syndromes.
Figure 1.
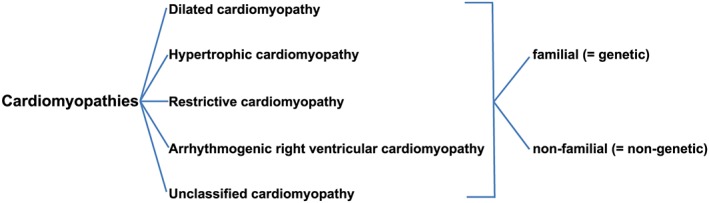
Classification of cardiomyopathies. Cardiomyopathies can be classified into five groups according to different morphological and functional criteria. Figure adapted from Elliot et al.12
Genetic diagnostics and genetic terminology in heart failure
A clear distinction between acquired and inherited heart failure syndromes remains challenging. Examination of heart failure patients should include an inquiry of the occurrence of sudden cardiac death and other heart failure symptoms among their family members. This should help to determine potential genetic causes of the disease and to identify other persons in the family being at risk for heart failure. Genetic counselling is strongly recommended for any patient with a cardiomyopathy, unless an acquired cause of the cardiomyopathy is clearly demonstrated. In the case of a potential genetic component, genetic testing should be considered for these individuals. In the current heart failure guidelines of the European Society of Cardiology, genetic testing ‘is recommended when the prevalence of detectable mutations is sufficiently high and consistent to justify routine targeted genetic screening’.14 Cardiogenetic counselling should be exclusively performed by someone with enough knowledge and expertise of the specific psychological, social, and medical implications of a cardiogenetic diagnosis.
In the last years, next‐generation sequencing (NGS) has dramatically improved and revolutionized genetic testing, leading to a high efficiency, and has reduced the cost of genetic analyses.15 Because of this technological development, genetic testing has become increasingly accessible and is nowadays applied in clinical routine diagnostics.
NGS‐based genetic testing of all disease‐associated genes can produce different results. First of all, a pathogenic mutation can be identified in a given gene, and the causative nature of the mutation can be determined by human geneticists in accordance with interpretation guidelines. Sometimes, identified variants can only be described as ‘variants of uncertain significance’. These are often sequence changes that are not commonly detected in the population, but for which there exist only few supporting cues that these variants might be pathogenic. In addition, genetic testing might show only so‐called benign polymorphisms, which are relatively frequent variants (frequencies >0.1–1% are not likely to cause a disease) and are not considered as being disease causing. Many of the identified disease‐causing mutations are rare and frequently ‘private’, that is, specific to an individual (and his or her family). Detailed clinical phenotyping of patients and their families is crucial, as it allows uncovering of familial segregations, family members at risk, reduced penetrance of specific mutations, or de novo occurrence of dominant mutations.
Different inheritance patterns are described for heart failure syndromes. Autosomal‐dominant inheritance is the predominant form of transmission. However, autosomal‐recessive, X‐linked, or mitochondrial inheritance are also found. In addition, dominant mutations can also occur de novo in patients having a risk of 50% to be inherited to their offspring.16
Each cardiomyopathy phenotype can be caused by mutations in one of the numerous different genes described (i.e. genetic heterogeneity). However, even mutations in the same disease‐associated gene can cause a distinct quantitative variability in the expression of the cardiomyopathy phenotype (i.e. phenotypic heterogeneity). Interestingly, different mutations within a specific gene might cause different functional effects and thereby produce different phenotypes. Variable expressivity and penetrance imply that factors beyond the single pathogenic mutations (i.e. genetic, epigenetic, or environmental modifiers) might influence the phenotype.
In addition, it is suggested that patients with inherited heart failure might also carry more than one pathogenic mutation. Cardiomyopathies attributable to compound heterozygosity (two mutations in the same gene, autosomal‐recessive inheritance) or digenic inheritance (two mutations in different genes) are found in heart failure patients, particularly in diseases known to be associated with a low penetrance. Oligogenic inheritance might be one explanation for the, sometimes observed, tremendous variations in disease penetrance in individual families but has not yet been genetically proven. Even in monogenic disease, multiple other loci are likely to act as modifiers of the disease phenotype.
Genetic cardiomyopathies and their associated genes
In the last decades, nearly 100 genes whose mutations cause different forms of cardiomyopathies have been identified.17 Most of these genes are associated with DCM and HCM, fewer with RCM and ARVC. Selected common genes whose mutations can cause cardiomyopathies are also shown in Table 1.
Table 1.
Selected genes associated with cardiomyopathies
| Cardiomyopathy form | Gene | Chromosome | Protein name |
|---|---|---|---|
| Dilated cardiomyopathy | LMNA | 1 | Lamin A/C |
| MYH7 | 14 | Beta myosin heavy chain | |
| TTN | 2 | Titin | |
| TNNT2 | 1 | Troponin T | |
| Hypertrophic cardiomyopathy | MYBPC3 | 11 | Cardiac myosin binding protein C |
| MYH7 | 14 | Beta myosin heavy chain | |
| TNNI3 | 19 | Troponin I | |
| TNNT2 | 1 | Troponin T | |
| TPM1 | 15 | Alpha‐tropomyosin | |
| MYL3 | 3 | Myosin light chain 3 | |
| Restrictive cardiomyopathy | DES | 2 | Desmin |
| MYH7 | 14 | Beta myosin heavy chain | |
| TNNI3 | 19 | Troponin I | |
| Arrhythmogenic right ventricular cardiomyopathy | DSC2 | 18 | Desmocollin |
| DSG2 | 18 | Desmoglein 2 | |
| DSP | 6 | Desmoplakin | |
| JUP | 17 | Plakoglobin | |
| PKP2 | 12 | Plakophilin 2 |
DCM is characterized by the presence of a left ventricular or biventricular dilatation and systolic impairment in the absence of abnormal loading conditions. It is the second most common aetiology for heart failure with reduced ejection fraction. DCM is a complex disorder with different genetic variants and environmental factors that determine disease onset and course. The familial form (due to single‐gene mutations) of DCM has an estimated prevalence of approximately 1:2500, although this might be underestimated.18, 19 DCM is most often autosomal‐dominantly inherited, and it is genetically highly heterogeneous.20, 21 Genes associated with DCM primarily encode for structural proteins in the cardiomyocyte sarcomere, cytoskeleton, and nuclear envelope and also for membrane ion channels and desmosomes.22 Of note, mutations in the genes MYH7 encoding beta myosin heavy chain, TNNT2 encoding troponin T, TTN encoding titin, and LMNA encoding a nuclear envelope protein are frequent causes of familial DCM.22 TTN is the gene with the most exons in the human genome, and mutations are suggested to be most frequent with approximately 25%,23, 24 but it has to be taken into consideration that many of the described disease‐causing mutations in TTN might just be variants of unclear significance.
HCM is characterized by an abnormal left ventricular wall thickening and mass. It is the most common hereditary cardiac disease with a prevalence of 1:500.25 HCM is a frequent cause of sudden cardiac death in young and asymptomatic individuals. Most HCM cases are inherited in an autosomal‐dominant manner with variable expressivity and age‐related penetrance. By now, in more than 60% of all HCM patients, the specific genetic cause of the disease can be identified by NGS‐based sequencing strategies. Nearly 70% of all HCM mutations can be found in the sarcomere genes MYH7 and MYBPC3 (encoding for cardiac myosin binding protein C).16 Further common mutations are localized in TNNT2 and in the genes for troponin I (TNNI3), alpha‐tropomyosin (TPM1), or myosin light chain 3 (MYL3).26
RCM is characterized by a rigid ventricular wall. The resulting impaired cardiac muscle relaxation leads to a decreased ventricular filling. Diagnosis of RCM is really difficult, as the heart seems more or less morphologically normal. Overall, prognosis of RCM is very bad. RCM is one of the most seldom cardiac diseases.27 Familial forms are caused by gene mutations affecting sarcomeric and cytoskeletal proteins as well as intermediate filaments.28 The inheritance pattern is normally autosomal dominant, but most RCM cases are based on a de novo mutation. Among others, mutations in TNNI3, in MYH7, and in the gene for desmin (DES) are described.28
ARVC is a progressive heart muscle disorder associated with structural and functional abnormalities mainly of the right ventricle, as its cardiomyocytes are replaced by fatty tissue and fibrosis. Besides, a biventricular and left‐dominated form also exist. ARVC is a frequent cause of sudden cardiac death in young adults and athletes. It is inherited in most cases in an autosomal‐dominant pattern and has a prevalence of 1:2000–1:5000.19 In approximately 50% of all cases, ARVC is caused by mutations in genes encoding for desmosomal proteins. Especially, mutations in the plakophilin 2 (PKP2) gene are frequent.29 Besides, common mutations can be found in the genes for desmoplakin (DSP), plakoglobin (JUP), desmoglein 2 (DSG2), and desmocollin (DSC2).19, 30
Other inherited cardiomyopathy forms triggering heart failure can be due to metabolic or mitochondrial diseases. Mutations in proteins involved in fat or carbohydrate metabolism or mitochondrial biogenesis cause these diseases. Most of them are associated with an unexplained left ventricular hypertrophy imitating a phenotype reminding of HCM, DCM, or RCM. However, the genetic cause of these diseases cannot be found in the genes described for cardiomyopathies. They are so‐called phenocopies with totally different pathophysiologies, extracardiac manifestations, and therapies. An example of such a phenocopy is Fabry disease, a lysosomal storage disease caused by a mutation in the gene GLA encoding for α‐galactosidase A.31
Clinical consequences of genetic findings in heart failure patients
Identification of a pathogenic mutation has important and different implications. The information can be used for accurate genetic counselling, for therapy guidance, and for family cascade screening and thus early diagnosis in affected individuals. Therefore, genetic findings in patients with heart failure are recommended and have concrete clinical aspects and consequences.
A couple of mutations in specific genes are associated with a poor prognosis and an increased risk for sudden cardiac death. If such a mutation is discovered in a patient, the threshold for recommending an implantable cardiac defibrillator to a patient should be decreased. LMNA mutation carriers have an increased occurrence of malignant (potentially life‐threatening) ventricular arrhythmias and sudden cardiac death.32 Other examples are TNNT2 33 and DES 34 mutation carriers, who also present with a high arrhythmia risk. In these patients, decisions regarding the primary prophylactic implantation of an implantable cardiac defibrillator should take genetic aspects into account.
Genetic cascade screening of asymptomatic family members in inherited heart failure can also have direct medical implications. Many patients have a long preclinical phase with few or even no symptoms. Before clear clinical heart failure symptoms are apparent, patients can present with asymptomatic structural or functional cardiac abnormalities. These might be potential precursors of heart failure syndromes. After identification of a pathogenic mutation in asymptomatic family members, these so‐called genotype‐positive phenotype‐negative patients should undergo early risk stratification. Depending on the mutation, preventative measures, such as avoidance of competitive sport,35 or an early start of cardioprotective medication can positively influence the disease course, thereby delaying cardiac decompensation or remodelling and preventing sudden cardiac death.
Finally, understanding the cellular basis of genetic heart failure in more detail may provide new insights into the biology of normal and impaired cardiac (cell) functions. This might help to identify novel therapeutic targets for heart failure and may lead to the development of new and specific treatment options in inherited cardiomyopathies.
Conclusions
Prevention and treatment of heart failure by identifying its genetic (and environmental) determinants is of high importance. On the one hand, heart failure can be caused by mutations in different disease‐associated genes. On the other hand, a complex interaction between genetic and environmental factors can also trigger heart failure. A clear genetic diagnosis can positively influence patient treatment and, thereby, improve prognosis. Furthermore, comprehensive genetic testing facilitates early identification of additional family members at risk for heart failure. Besides, understanding the pathogenesis of genetically induced heart failure at its molecular level may lead to the development of specific individual heart failure therapies in the future.
Conflict of interest
None declared.
Czepluch, F. S. , Wollnik, B. , and Hasenfuß, G. (2018) Genetic determinants of heart failure: facts and numbers. ESC Heart Failure, 5: 211–217. doi: 10.1002/ehf2.12267.
References
- 1. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol 2011; 8: 30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker‐Collo S, Barrero LH, Bartels DH, Basáñez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Bin Abdulhak A, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan‐Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere‐Derry J, Danaei G, Davis A, De Leo D, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz‐Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Franklin R, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gosselin R, Grainger R, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Ma J, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina‐Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi‐Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez‐Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA 3rd, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez‐Riera L, Sanman E, Schwebel DC, Scott JG, Segui‐Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh PH, Zaidi AK, Zheng ZJ, Zonies D, Lopez AD, Murray CJ, AlMazroa MA, Memish ZA. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012; 380: 2163–2196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ziaeian B, Fonarow GC. Epidemiology and aetiology of heart failure. Nat Rev Cardiol 2016; 13: 368–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Cowie MR, Mosterd A, Wood DA, Deckers JW, Poole‐Wilson PA, Sutton GC, Grobbee DE. The epidemiology of heart failure. Eur Heart J 1997; 18: 208–225. [DOI] [PubMed] [Google Scholar]
- 5. Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJV, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WHW, Tsai EJ, Wilkoff BL. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013; 128: e240–e327. [DOI] [PubMed] [Google Scholar]
- 6. Braunwald E. The war against heart failure: the Lancet lecture. Lancet 2015; 385: 812–824. [DOI] [PubMed] [Google Scholar]
- 7. Lee DS, Pencina MJ, Benjamin EJ, Wang TJ, Levy D, O'Donnell CJ, Nam BH, Larson MG, D'Agostino RB, Vasan RS. Association of parental heart failure with risk of heart failure in offspring. N Engl J Med 2006; 355: 138–147. [DOI] [PubMed] [Google Scholar]
- 8. Lindgren MP, Smith JG, Li X, Sundquist J, Sundquist K, Zoller B. Sibling risk of hospitalization for heart failure—a nationwide study. Int J Cardiol 2016; 223: 379–384. [DOI] [PubMed] [Google Scholar]
- 9. Towbin JA, Lowe AM, Colan SD, Sleeper LA, Orav EJ, Clunie S, Messere J, Cox GF, Lurie PR, Hsu D, Canter C, Wilkinson JD, Lipshultz SE. Incidence, causes, and outcomes of dilated cardiomyopathy in children. JAMA 2006; 296: 1867–1876. [DOI] [PubMed] [Google Scholar]
- 10. Monserrat L, Hermida M, Bouzas B, Mosquera I, Mahon N, Peteiro J, Alvarez N, Penas‐Lado M, Crespo M, Castro‐Beiras A. Familial dilated cardiomyopathy in patients transplanted for idiopathic dilated cardiomyopathy. Rev Esp Cardiol 2002; 55: 725–732. [DOI] [PubMed] [Google Scholar]
- 11. Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation 2006; 113: 1807–1816. [DOI] [PubMed] [Google Scholar]
- 12. Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, Kühl U, Maisch B, McKenna WJ, Monserrat L, Pankuweit S, Rapezzi C, Seferovic P, Tavazzi L, Keren A. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2008; 29: 270–276. [DOI] [PubMed] [Google Scholar]
- 13. Arbustini E, Narula N, Tavazzi L, Serio A, Grasso M, Favalli V, Bellazzi R, Tajik JA, Bonow RO, Fuster V, Narula J. The MOGE(S) classification of cardiomyopathy for clinicians. J Am Coll Cardiol 2014; 64: 304–318. [DOI] [PubMed] [Google Scholar]
- 14. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37: 2129–2200. [DOI] [PubMed] [Google Scholar]
- 15. Punetha J, Hoffman EP. Short read (next‐generation) sequencing: a tutorial with cardiomyopathy diagnostics as an exemplar. Circ Cardiovasc Genet 2013; 6: 427–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ku CS, Tan EK, Cooper DN. From the periphery to centre stage: de novo single nucleotide variants play a key role in human genetic disease. J Med Genet 2013; 50: 203–211. [DOI] [PubMed] [Google Scholar]
- 17. McNally EM, Barefield DY, Puckelwartz MJ. The genetic landscape of cardiomyopathy and its role in heart failure. Cell Metab 2015; 21: 174–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hershberger RE, Lindenfeld J, Mestroni L, Seidman CE, Taylor MR, Towbin JA. Genetic evaluation of cardiomyopathy—a Heart Failure Society of America practice guideline. J Card Fail 2009; 15: 83–97. [DOI] [PubMed] [Google Scholar]
- 19. Schulze‐Bahr E, Klaassen S, Abdul‐Khaliq H, Schunkert H. Molecular diagnostics of cardiovascular diseases. Expert consensus statement by the German Cardiac Society (DGK) and the German Society of Pediatric Cardiology (DGPK). Kardiologe 2015; 9: 213–243. [Google Scholar]
- 20. Li X, Zhang P. Genetic determinants of myocardial dysfunction. J Med Genet 2017; 54: 1–10. [DOI] [PubMed] [Google Scholar]
- 21. Haas J, Frese KS, Peil B, Kloos W, Keller A, Nietsch R, Feng Z, Müller S, Kayvanpour E, Vogel B, Sedaghat‐Hamedani F, Lim WK, Zhao X, Fradkin D, Köhler D, Fischer S, Franke J, Marquart S, Barb I, Li DT, Amr A, Ehlermann P, Mereles D, Weis T, Hassel S, Kremer A, King V, Wirsz E, Isnard R, Komajda M, Serio A, Grasso M, Syrris P, Wicks E, Plagnol V, Lopes L, Gadgaard T, Eiskjær H, Jørgensen M, Garcia‐Giustiniani D, Ortiz‐Genga M, Crespo‐Leiro MG, Deprez RH, Christiaans I, van Rijsingen IA, Wilde AA, Waldenstrom A, Bolognesi M, Bellazzi R, Mörner S, Bermejo JL, Monserrat L, Villard E, Mogensen J, Pinto YM, Charron P, Elliott P, Arbustini E, Katus HA, Meder B. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur Heart J 2015; 36: 1123–1135a. [DOI] [PubMed] [Google Scholar]
- 22. Tayal U, Prasad S, Cook S. Genetics and genomics of dilated cardiomyopathy and systolic heart failure. Genome Med 2017; 9: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Herman DS, Lam L, Taylor MR, Wang L, Teekakirikul P, Christodoulou D, Conner L, DePalma SR, McDonough B, Sparks E, Teodorescu DL, Cirino AL, Banner NR, Pennell DJ, Graw S, Merlo M, Di Lenarda A, Sinagra G, Bos JM, Ackerman MJ, Mitchell RN, Murry CE, Lakdawala NK, Ho CY, Barton PJ, Cook SA, Mestroni L, Seidman JG, Seidman CE. Truncations of titin causing dilated cardiomyopathy. N Engl J Med 2012; 366: 619–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Walsh R, Buchan R, Wilk A, John S, Felkin LE, Thomson KL, Chiaw TH, Loong CCW, Pua CJ, Raphael C, Prasad S, Barton PJ, Funke B, Watkins H, Ware JS, Cook SA. Defining the genetic architecture of hypertrophic cardiomyopathy: re‐evaluating the role of non‐sarcomeric genes. Eur Heart J 2017; 38: 3461–3468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Richard P, Charron P, Carrier L, Ledeuil C, Cheav T, Pichereau C, Benaiche A, Isnard R, Dubourg O, Burban M, Gueffet JP, Millaire A, Desnos M, Schwartz K, Hainque B, Komajda M. Hypertrophic cardiomyopathy: distribution of disease genes, spectrum of mutations, and implications for a molecular diagnosis strategy. Circulation 2003; 107: 2227–2232. [DOI] [PubMed] [Google Scholar]
- 26. Roma‐Rodrigues C, Fernandes AR. Genetics of hypertrophic cardiomyopathy: advances and pitfalls in molecular diagnosis and therapy. Appl Clin Genet 2014; 7: 195–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kostareva A, Kiselev A, Gudkova A, Frishman G, Ruepp A, Frishman D, Smolina N, Tarnovskaya S, Nilsson D, Zlotina A, Khodyuchenko T, Vershinina T, Pervunina T, Klyushina A, Kozlenok A, Sjoberg G, Golovljova I, Sejersen T, Shlyakhto E. Genetic spectrum of idiopathic restrictive cardiomyopathy uncovered by next‐generation sequencing. PLoS One 2016; 11: e0163362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Towbin JA. Inherited cardiomyopathies. Circ J 2014; 78: 2347–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. van der Smagt JJ, van der Zwaag PA, van Tintelen JP, Cox MG, Wilde AA, van Langen IM, Ummels A, Hennekam FA, Dooijes D, Gerbens F, Bikker H, Hauer RN, Doevendans PA. Clinical and genetic characterization of patients with arrhythmogenic right ventricular dysplasia/cardiomyopathy caused by a plakophilin‐2 splice mutation. Cardiology 2012; 123: 181–189. [DOI] [PubMed] [Google Scholar]
- 30. Pinamonti B, Brun F, Mestroni L, Sinagra G. Arrhythmogenic right ventricular cardiomyopathy: from genetics to diagnostic and therapeutic challenges. World J Cardiol 2014; 6: 1234–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Nagueh SF. Anderson‐Fabry disease and other lysosomal storage disorders. Circulation 2014; 130: 1081–1090. [DOI] [PubMed] [Google Scholar]
- 32. van Rijsingen IA, Arbustini E, Elliott PM, Mogensen J, Hermans‐van Ast JF, van der Kooi AJ, van Tintelen JP, van den Berg MP, Pilotto A, Pasotti M, Jenkins S, Rowland C, Aslam U, Wilde AA, Perrot A, Pankuweit S, Zwinderman AH, Charron P, Pinto YM. Risk factors for malignant ventricular arrhythmias in lamin a/c mutation carriers a European cohort study. J Am Coll Cardiol 2012; 59: 493–500. [DOI] [PubMed] [Google Scholar]
- 33. Watkins H, McKenna WJ, Thierfelder L, Suk HJ, Anan R, O'Donoghue A, Spirito P, Matsumori A, Moravec CS, Seidman JG, Seidman CE. Mutations in the genes for cardiac troponin T and alpha‐tropomyosin in hypertrophic cardiomyopathy. N Engl J Med 1995; 332: 1058–1064. [DOI] [PubMed] [Google Scholar]
- 34. van Spaendonck‐Zwarts KY, van Hessem L, Jongbloed JD, de Walle HE, Capetanaki Y, van der Kooi AJ, van Langen IM, van den Berg MP, van Tintelen JP. Desmin‐related myopathy. Clin Genet 2010; 80: 354–366. [DOI] [PubMed] [Google Scholar]
- 35. Elliott PM, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, Hagege AA, Lafont A, Limongelli G, Mahrholdt H, McKenna WJ, Mogensen J, Nihoyannopoulos P, Nistri S, Pieper PG, Pieske B, Rapezzi C, Rutten FH, Tillmanns C, Watkins H. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J 2014; 35: 2733–2779. [DOI] [PubMed] [Google Scholar]


