Abstract
Blunt trauma to the chest wall and rib fractures are remarkably frequent and are the basis of considerable morbidity and possible mortality. Surgical remedies for highly displaced rib fractures, especially in cases of flail chest, have been undertaken intermittently for more than 50 years. Rib-specific plating systems have started to be used in the last 10 years. These have ushered in the modern era of rib repair with chest wall stabilization (CWS) techniques that are safer, easier to perform, and more efficient. Recent consensus statements have sought to define the indications and contraindications, as well as the when, the how, and the technical details of CWS. Repair should be considered for patients who have three or more displaced rib fractures or a flail chest, whether or not mechanical ventilation is required. Additional candidates include patients who fail non-operative management irrespective of fracture pattern and those with rib fractures who need thoracic procedures for other reasons. Traditionally, unstable spine fracture and severe traumatic brain injury are definite contraindications. Pulmonary contusion’s role in the decision to perform CWS remains controversial. A range of rib-specific plating systems are now commercially available.
Keywords: Flail chest, chest wall stabilization (CWS), rib fracture, plating systems
Why chest wall stabilization (CWS)?
Chest wall trauma is common around the world. Approximately 500,000 patients present annually to emergency hospitals in the United States with an injury to their bony thorax, and more than one-third of these are hospitalized. Reported morbidity and mortality rates after chest wall injury vary widely, but clearly increase with age, number of rib fractures, and the presence of flail chest. Patients with flail chest often also present with significant pulmonary contusion, long-term pain, disability, and inability to maintain employment. In a study of 3,151 trauma patients (road traffic-motorbike) three or more rib fractures or any element of displacement was the most significant predictor for developing pulmonary complications. In contrast, those with fewer than three rib fractures, no displacement, and no initial lung or other organ injuries, could be managed safely as outpatients (1).
In the past two decades, there has been an exponential increase in interest in the surgical stabilization of rib fractures, with multiple authors showing improved outcomes compared with conventional management. The procedure is being used more and more In the United States by thoracic, trauma and orthopedic surgeons. Recent consensus statements have sought to define the indications, contraindications, timing, and technical details of CWS. As previously mentioned, patients who have three or more acutely displaced rib fractures or flail chest (two or more contiguous ribs fractured in two or more places) should be considered for repair whether or not mechanical ventilation is required. Other candidates include patients who fail optimal non-operative management irrespective of the pattern of fractures, and patients with rib fractures who need thoracic surgeries for other reasons (2).
As with any other procedure there is a specific learning curve for repairing a rib fracture. Those who are new to CWS should avoid the more difficult fractures at the extremes of exposure. Instead they should select patients with lateral fracture patterns. The incision length will be reduced with experience and confidence in sufficient exposure and reduction of fractures. The majority of rib repairs in the United States and Brazil are carried out by trauma or thoracic surgeons, but this varies between centers. Surgeons who are new to osteosynthesis should seek the help of an orthopedist in their initial endeavors. Treatment “algorithms” have been proposed based on a combination of clinical experience and identification of the most relevant risk factors based on an analysis of the available literature (3). The most notable challenge is to identify the right treatment for the right patient.
There is paucity of data regarding functional impairment and pain due to multiple rib fractures following trauma. Fagevik Olsén et al. in 2016, assessed respiratory and physical function, pain, range of movement, and kinesiophobia in patients with multiple rib fractures who had undergone stabilizing surgery and compared results with conservatively managed patients. According to the author’s opinion, the results must be interpreted with caution as the study population is small but they noticed a tendency for decreased pain, better thoracic range of motion and physical function in the group that was managed with surgery. If operative technique could become less invasive, the author believes that the benefit of surgery would be greater (4).
Traumatic flail chest injuries can be life-threatening and frequently involve prolonged invasive mechanical ventilation and admission to an intensive care unit (ICU). Recent research published by Kocher et al. evaluated the practicality and cost-effectiveness of surgical rib stabilization in patients who had flail chest with ventilator-dependent respiratory insufficiency. This retrospective study compared the usefulness of rib fixation in relation to predictors for prolonged ventilation, outcome and cost-effectiveness. A total of 61 consecutive flail chest patients underwent stabilization with a locking titanium plate fixation system. Sixty-two percent (n=38) of patients could be gradually taken off the ventilator within the first 72 post-operative hours. Furthermore, a cost study showed that a reduction of two days in the ICU could potentially offset the surgical rib fixation’s cost. The authors conclude that CWS in flail chest could potentially reduce the number of ventilator days, length of stay in ICU, and consequently, hospital costs for selected patients who have traumatic flail chest and need mechanical ventilation (5).
There remains considerable debate about the widespread application of rib fixation, as well as the quality and quantity of available data. In 2017, Farquhar et al. related that “although considerable enthusiasm surrounds surgical fixation of flail chest injuries, our analysis does not immediately validate its universal implementation, but rather encourages the use of modern, multidisciplinary, non-operative strategies. The function of rib fracture fixation in modern chest wall trauma management should ultimately be defined by prospective, randomized trials” (6).
In 2017, Uchida et al., evaluated the efficacy and indications of rib stabilization using a propensity score analysis of 187 patients with significant rib fractures. Ten patients from both the operative and non-operative groups were included. The surgically treated patients extubated significantly earlier than their non-operative counterparts. They experienced a shorter duration of continuous intravenous narcotic, and a significantly shorter ICU length of stay. The non-operative management group had a considerably higher incidence of pneumonia. They concluded that early rib fixation is a sufficiently acceptable procedure not only for flail chest but also for repair of severe multiple rib fractures (7).
In 2016, Pieracci et al. carried out a prospective, controlled evaluation of CWS as compared with optimal medical management for severe rib fracture patterns among critically-ill trauma patients in a 2-year clinical evaluation with at least one of the following rib fracture patterns: flail chest, 30% or greater hemithorax volume loss, three or more fractures with bicortical displacement, and experienced severe pain or respiratory failure even with optimal medical management. In 2013, all patients were managed with a non-operative approach. However, in 2014, all patients were managed operatively using univariate and multivariable analyses. This included seventy patients, with 35 in each group and most importantly there were no mortalities. In this evaluation, the authors concluded that CWS “as compared with the best medical management improved acute outcomes among a group of critically ill trauma patients with a variety of severe fracture patterns” (8).
When should CWS be performed?
There are a number of scoring systems to help the clinician to assess the seriousness of a rib injury. Usually they incorporate the number, pattern and laterality of fractures, together with the presence of other significant factors such as a flail segment and/or pulmonary contusion. Higher scores indicate worse outcomes. The optimization of pain control, pulmonary hygiene and ventilation strategies are important for this population, irrespective of whether surgical intervention is incorporated in their treatment.
The choice of when to perform surgical stabilization after blunt trauma to the chest is important. Many researchers support intervention within a few days of the initial trauma. Early fixation can potentially mitigate factors such as inflammation, severe hematoma, clotted hemothorax, empyema, rigidity with deformities of the chest wall, and early callous formation which can impede operative reduction of the fractures. The timing of surgery must be made in the context of the patients overall clinical condition. Occasionally surgery has to be postponed while other complications are dealt with.
Recent years have seen a paradigm shift among supporters of CWS toward earlier intervention, strongly supported by clinical experience (Table 1). The (often) predictable deterioration observed in patients with severe injuries to the chest wall managed non-operatively may be avoided by early CWS. To this end, most recently published series have described the operation intervention within72 hours of injury, and ideally within 24 hours of injury (9).
Table 1. Potential benefits of CWS.
| Shortened duration of mechanical ventilation |
| Decreased incidence of pneumonia |
| Decreased need for tracheostomy |
| Shortened ICU length of stay |
| Shortened hospital length of stay |
| Decreased mortality in patients with flail chest |
| Rapid return to work |
| Cost effectiveness |
| Decreased use of narcotics |
| Earlier mobilization |
CWS, chest wall stabilization; ICU, intensive care unit.
Rib fractures in the elderly are also common, carrying a significant morbidity and mortality risk. The impact of rib fractures in patients who are 65 years and older has been well documented and is associated with increasing pneumonia and mortality rates. According to Fitzgerald et al., rib plating in the older trauma population demonstrates a measurable decrease in mortality and respiratory complications, improves respiratory mechanics, and permits an accelerated return to a functioning state (10).
Singular attention has been paid to “flail chest” injury. This is usually described as two fractures in each of three or more consecutive ribs. These patients frequently experience hypoxemic respiratory failure associated with inefficient ventilatory mechanics, underlying pulmonary contusion and subsequent pneumonia. Even in the modern era mortality rates can reach 9–16% for these patients. For surviving patients, complications such as chronic pain in the chest wall and deformity that results in enduring disability and poor quality of life are also occur regularly. Although these outcomes are well documented, treatment alternatives are still not clearly defined (5).
In 2016, Coughlin et al. published a meta-analysis of the available randomized controlled trials. The objective was to compare the efficacy of the non-operative management approach, specifically utilizing a systematic search of the literature to find available controlled trials which compared clinical outcomes. Three randomized control trials, out of a total of 1,273 papers identified, reported the results of 123 patients with flail chest. Surgical stabilization was associated with a reduction of two-thirds in the incidence of pneumonia, and considerable reductions in the period of mechanical ventilation and ICU and overall lengths of stay. They concluded that: “surgical stabilization for a traumatic flail chest is associated with significant clinical benefits in this meta-analysis.” (11).
Another very important indication: chronic nonunion
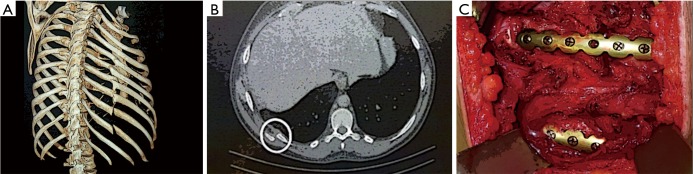
Chronic nonunion is defined as a lack of bone healing nine months after injury. Fractures that have not healed within 3 months have been defined as delayed union. It is estimated that between 5% and 10% of all rib fractures will present chronic nonunion and a majority of these will remain symptomatic. Purported risk factors are: smoking, alcohol, malnutrition, use of steroids, NSAIDs, diabetes, and vitamin D deficiency. Hallmark symptoms include: persistent pain and a clicking or motion sensation. Pain is frequently worsened by coughing, sneezing, contorting and exacerbated by lifting activities, exercise, and/or work. The results of surgical repair or rib resection are inconsistent but are the only modalities reported to provide relief for the symptoms (Figure 1).
Figure 1.
(A,B,C) Chronic nonunion of the 9th, 10th ribs and after fixation.
A small but finite percentage of rib fractures will result in nonunion. This happens because of the unique characteristics of the fracture or because of various poor healing factors of the subject. If a patient continues to present symptomology after 3 months, surgeons may look at operative management. Isolated resection of fibrous scar tissue from the nonunion site may be adequate in some cases but it may also be necessary to provide additional structural stability to the rib. This depends on the extent of the fracture pattern and resection. This objective can be obtained operatively with rib plating and interposition bone grafting to span gaps and promote bony union (12).
Little published data exist on the safety of early operative fixation in the setting of pulmonary contusion (Table 2). There is extensive clinical experience from multiple high volume centers that would suggest that it is safe and perhaps even desirable to offer these patients early CWS. Likewise, concomitant CWS and spine stabilization has been performed by this author with good results. Incomplete resuscitation and severe TBI remain absolute contraindications to early rib fixation.
Table 2. Traditional contraindications to CWS.
| Pulmonary contusion |
| Severe traumatic brain injury |
| Hemodynamic instability |
| Unstable spine or pelvis fractures |
CWS, chest wall stabilization.
How do we do CWS?
With established considerable improvements in the available materials and technique of CWS, most fractures are amenable to operative fixation. Many procedures which allow access to fractures that are difficult to reach have been described. These include percutaneous trocar access, hanging scapula retractors, step-ladder incisions and the use of 90° instruments (screwdriver and drill). Despite these procedures, certain rib fractures cannot be easily repaired. In particular, fractures of ribs 1 and 2 and those paraspinal rib fractures within 2 to 3 cm of the transverse process remain out of reach.
The first and second ribs, with little contribution to respiratory physiology, are unduly morbid and challenging to expose. Likewise, ribs 11 and 12, known as floating ribs, are not critical to respiration, and are not easily accessible with standard muscle sparing incisions. Therefore, the target ribs are 3 through 10. There is no apparent advantage to repairing “every other rib” to minimize dissection. Every attempt to “spare” or minimize muscle division should be made. Excellent exposure of most posterior and lateral rib fractures can be obtained through the auscultatory triangle.
Routine or selective use of video-assisted thoracoscopic surgery (VATS) in conjunction with rib fixation is commonly described. VATS is proven safe, and may add additional value by aiding with the precise identification of fractured sites. Also, VATS may help direct optimal placement of the incision to minimize length, minimize muscle division, allow for complete evacuation of hemothorax, facilitate optimal chest tube position, aid in fracture reduction, and rule out and repair diaphragm or pulmonary lacerations.
A totally thoracoscopic approach to rib fixation was recently demonstrated. This method allows visualization of all rib segments with the added advantage of minimal incisions. Although feasibility was demonstrated, the practical and widespread application of this technique will require further development of specialized equipment and training (13).
Operative techniques
Preparation
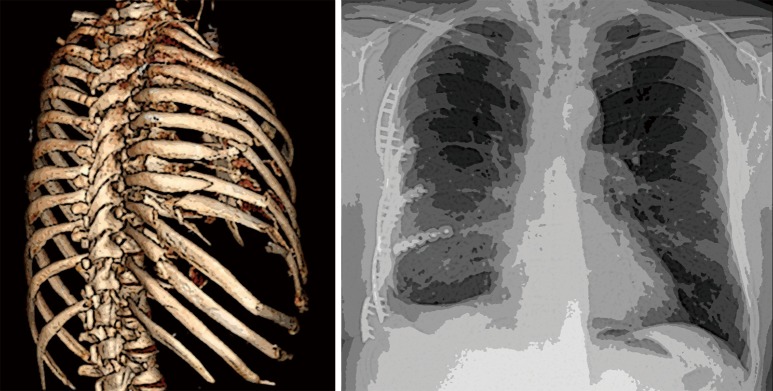
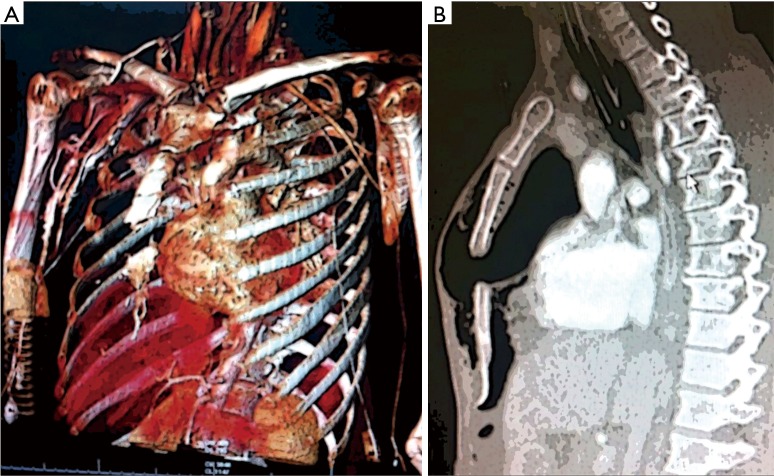
As soon as the trauma patient has been adequately revived, hemodynamic stability achieved, and a complete evaluation of all injuries concluded, a decision can be made to go ahead with the operative fixation of rib fractures, preferentially as mentioned before, during the first 72 hours. 3D images of the chest computer-assisted tomography (CT) scan are not absolutely necessary; however, they can be of great help in defining the real extent of fractures, the deformity and instability of the chest wall, and for planning incisions. Pre-operative optimization of the patient must include aggressive multi-modal pain control, pulmonary hygiene, and evaluation of pulmonary function. A pre-operative bronchoscopy can clear bronchial secretions and help in placing a double-lumen endotracheal tube, if one is necessary. Many surgeons routinely use VATS as we mentioned before (Figure 2).
Figure 2.
Preoperative CT scan and postoperative chest X-ray.
Operation
There is a number commercially available system for rib fixation, each with their unique advantages and shortcomings. The most commonly used systems employ plates secured to the outer rib surface, secured with bicortical screws. A minimum of twenty millimeters of visible healthy rib on either side of the fracture is necessary to secure sufficient fixation. Exposure of fractures is usually performed through a single well placed incision. A second incision can be made for additional exposure, particularly in those cases with multiple distinct fracture lines.
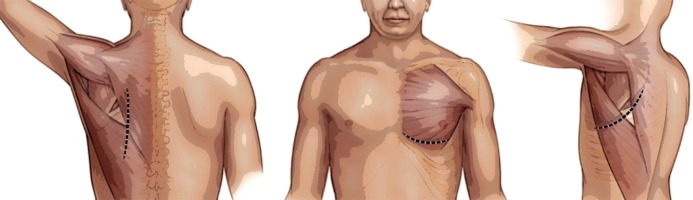
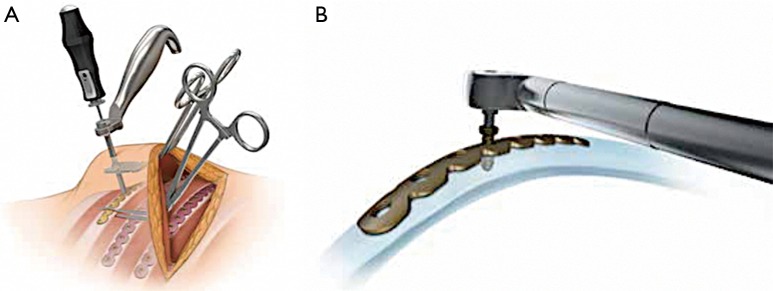
Lateral or posterior decubitus positioning allows access to most rib fractures. Supine position provides optimal exposure for anterior and antero-lateral fractures. Anterior fractures may be exposed through an oblique incision along the inframammary fold. Prone positioning with 90-degree abduction of the ipsilateral arm rotates the scapula laterally and optimizes exposure to posterior and subscapular fractures (Figure 3).
Figure 3.
Typical muscle sparing incisions (subscapular, inframammary and posterior vertical).
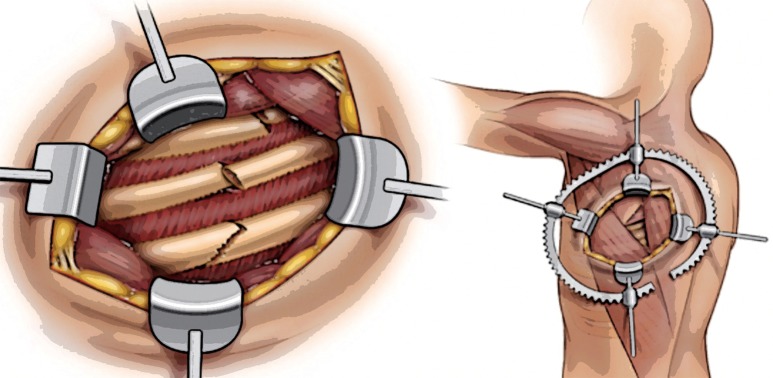
The correct placement of surgical incision(s) will keep incision length and soft-tissue trauma to a minimum. We, and others, have gradually adopted non-traditional incisions, for example oblique and vertical, and avoid muscle transection when possible. “Splitting” the latissimus dorsi (without dividing) is routine and allows excellent access to the majority of lateral and posterior fractures. One cannot over emphasize the utility of the triangle of auscultation, the exploitation of which provides widespread exposure to posterior, lateral, and subscapular fractures (Figure 4).
Figure 4.
Subscapular exposure through the triangle of auscultation.
Muscle-sparing incisions, which are designed to expose multiple ribs without dividing muscles, involve a shift away from traditional thoracic incisions, which are planned to provide exposure to extra and intra-pleural structures. Newer equipment, including right-angled drilling and screw driving systems, has greatly facilitated repair of rib fractures underneath overlying, intact myocutaneous flaps.
Access to the anterior fractures of the second and third rib may be gained via a small horizontal incision, with splitting of the fibers of the pectoralis muscles. Lateral fracture series may be accessed with the patient in the classical lateral decubitus position via a longitudinal incision between 7 and 9 cm long, placed along the anterior border of the latissimus dorsi. At this point care should be taken to avoid damage to the long thoracic nerve (14). Posterior fractures are usually the hardest to repair as they are adjacent to transverse processes, angulation of the rib, and subscapular location. These fractures may be approached with the subject in the prone position with the ipsilateral arm resting on a lowered table. Then, a longitudinal incision is made medial to the scapular tip.
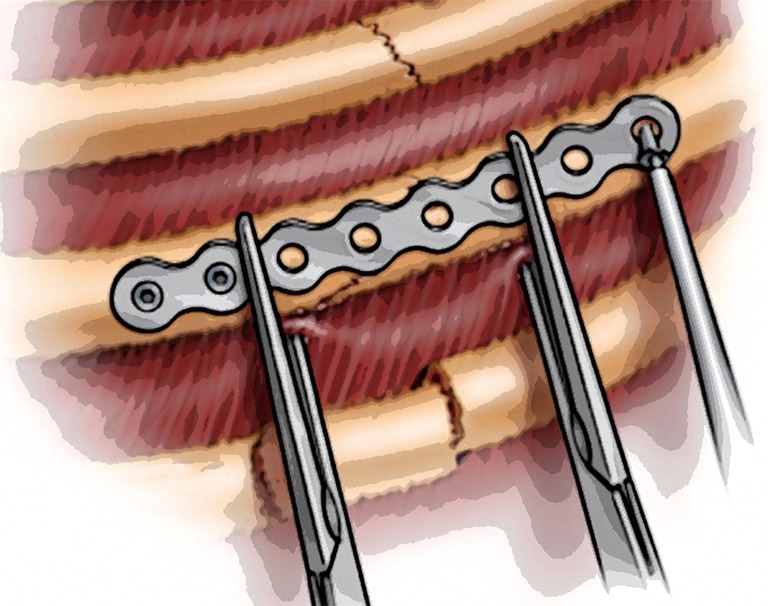
Following skin incision, some degree of sub-cutaneous flap development will provide access to multiple rib fractures. The fractures are commonly easily detectable through the musculature and must be exposed separately. The reduction is normally accomplished quite simply by lifting the depressed rib segment with a right-angle clamp or with a finger and the ends of the fracture can be “settled” in proper reduction. It’s also important to mention that reduction of multiple adjacent fractures in order before fixation helps to maintain the contour of the chest wall and help in placement of the systems. Clearing the rib of its anterior soft tissue envelope is required for 2.5 centimeters on both sides of the fracture to allow precise matching of the rib prosthesis to the rib surface. In our opinion it is very important to keep the periosteum intact, if possible. Aggressive over-exposure of the ends of the fractured rib is not necessary or even desirable (Figure 5).
Figure 5.
(A,B) Right-angle clamp and screw driving system.
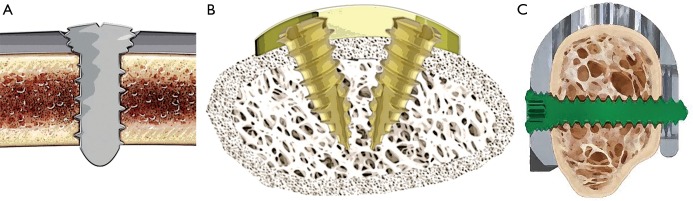
A range of rib-specific plating systems are currently available commercially. They have multiple design features in common; particularly a semi-rigid fixation with anterior plate positioning and locking screws. The flexible nature of ribs requires locking screws in order to minimize failure. In addition, these systems are low profile, are made of titanium, and can be easily shaped (Figure 6).
Figure 6.
(A,B,C) Bi-cortical, unicortical and u-plate rib fixation.
The thickness of ribs is variable (8–12 mm). Therefore, rib thickness should be measured with a caliper prior to plating to determine the optimal length for screws. Bi-cortical screw purchase of the rib is considered the standard and allows for dual point fixation. One newer system utilizes unicortical screws of 7 mm length. Another popular system incorporates a u-plate design which allows for screw purchase of the plate in front and in back of the rib. The surgeon will check the fracture line to ascertain the number of screw holes necessary for fixing the plate. One should aim for at least 2.5 cm of plate fixation on both sides of the fracture (Figure 7). The plate should be shaped to the precise contour of the surface of the anterior rib, without spaces and with minimal tension. For placement of screws, right-angle clamps or a plate holding forceps will hold the plate in position and the rib in reduction.
Figure 7.
Fracture reduction and plate application.
Rib shapes are variable and complex and exact matching of plates to ribs often requires bending and twisting in two or more planes. All of the systems currently available use “low profile” or right-angled drill and screwdriver instruments to allow fixing. The fractures at the limits of exposure the most difficult, i.e., those close to the spine or underneath the scapula. Trocar systems are available to further minimize the length of incisions when direct 90-degree access to the plates with standard instruments are required.
Minimized approaches allow sufficient stabilization of severe dislocated rib fractures without extensive dissection or division of the thoracic muscles. Shorter incisions are advantageous for the patient’s ultimate aesthetical appearance, but also to reduce the surgical trauma. The simple technique of increasing scapula mobility by keeping the arm in the sterile field provides the largest accessible surface of the rib cage. It is not necessary to repair every rib fracture. The stability of the chest wall increases with every rib stabilized and it is acceptable just to fix all rib fractures that are easily accessible through the guide incision. One should try to repair both fracture lines involved in a flail segment when it is technically feasible (15) (Figure 8).
Figure 8.
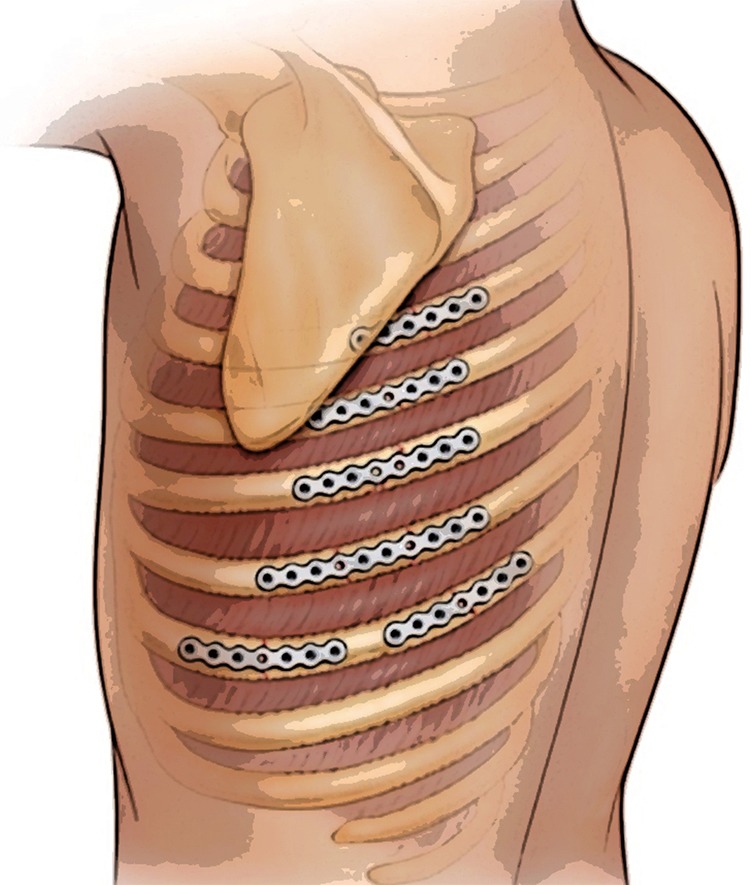
Various fracture and plate configurations.
Closure is simple with muscle sparing techniques. Absorbable sutures are used to close muscular “windows” in a running or interrupted pattern. The use of a closed suction drain in the sub-cutaneous space depends on host factors and surgeon preference. Chest tube placement is discretionary but highly recommended by these, and most authors. We use soft, fluted tubes with a diameter of 24 Fr or less.
This is the perfect opportunity to lavage the pleural space with 1–2 liters of warm saline preferentially with the concomitant use of video thoracic surgery. These authors use this video assisted or even a blind lavage technique with excellent results and the virtual elimination of retained hemothorax. To complete the procedure, there is an option of placing a regional analgesia catheter or intercostal rib blocks (16) (Figure 9).
Figure 9.
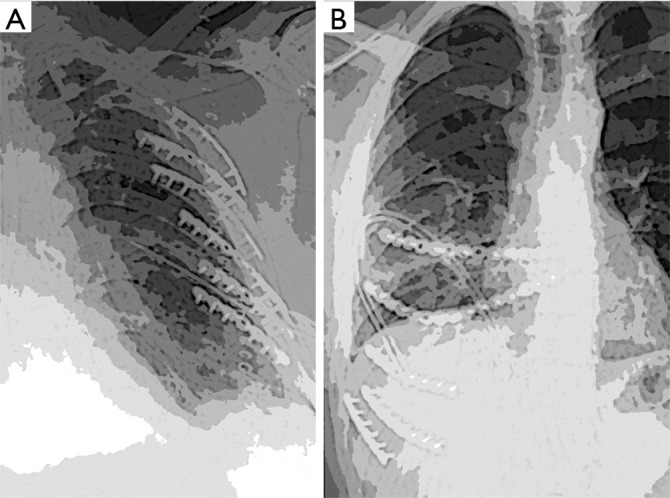
(A,B) Examples of post CWS chest radiographs. CWS, chest wall stabilization.
Sternal fractures are largely associated with deceleration injuries and blunt anterior chest trauma. Sternal trauma must be carefully evaluated by monitoring vital parameters. It is paramount that associated injuries are not included. Nonetheless, the routine admission of patients with isolated sternal fractures for observation is common in today’s practice and is often unnecessary.
Sternal fractures can occur in isolation or with associated injuries. The prognosis is very good for isolated sternal fractures, with the majority of patients experiencing a complete recovery within a number of weeks. Nevertheless, two-thirds of sternal fractures have concomitant injuries with a high mortality rate of between 25% and 45%. Chest wall injuries include simple rib fractures, sternoclavicular dislocation and flail chest. Pneumothorax, hemothorax, myocardial and pulmonary contusions, cardiac tamponade and injuries to the diaphragm and abdomen also occur frequently. There is considerable correlation between displaced or unstable sternal fractures and pulmonary injuries, pericardial effusions, spinal and rib fractures (Figure 10).
Figure 10.
(A,B) Complete sternal fracture with associated flail chest, hemo-pneumothorax.
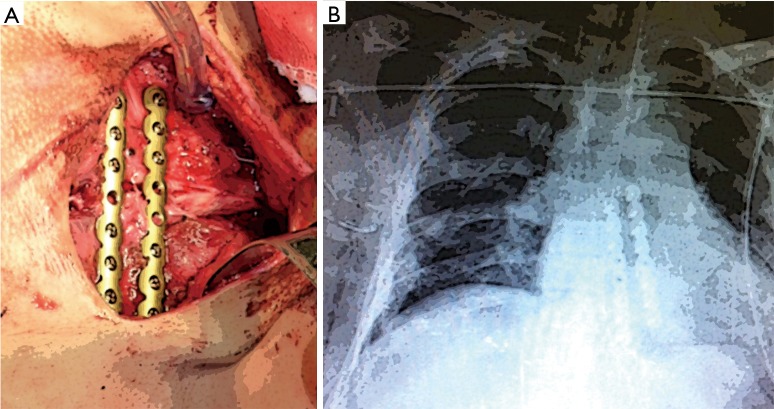
In this example of total sternal fracture, complicated by flail chest and bilateral hemo-pneumothorax, a direct approach to the fracture was undertaken promptly. Sternal fixation was accomplished with two parallel plates. In addition, bilateral thoracoscopy was performed for drainage of hemothorax. The plates provided stability to the sternum and resulted to a complete consolidation of the fracture in its anatomical position (Figure 11).
Figure 11.
(A,B) Two plate construct to stabilize sternum and resultant chest X-ray.
There are short and long-term complications associated with sternal fractures. Chest pain is the most common short term complication with an average duration of 8–12 weeks for all age groups with analgesia alone. Anxiety as a result of pain can impede ventilation, leaving the patient vulnerable to chest infection. Long term complications include non-union and mal-union. These present as painful pseudarthrosis and often prompt delayed surgical correction.
Final considerations and unanswered questions
Despite the increasing popularity of CWS, this operation is performed in less than 1% of flail chest cases (17). Lack of widespread adoption is likely due to unfamiliarity with the technique and nonexistence of subspecialty ownership. The benefit of CWS in non-flail chest fracture patterns is currently being addressed by the CWIS Non-flail trial. This is a multi-institutional study comparing the outcomes of patients with 3 or more displaced rib fractures randomized to rib fracture repair or non-operative management. (https://cwisociety.org/research/nonflailrct/) Clearly, patients with less impressive radiographic fracture arrangements may present with rebellious pain or respiratory deficiency. An example of this is a patient with severe pain localized, over one or two fractures, together with an uncomfortable “clicking” feeling and palpation. The utility of rib repair in these less dramatic fracture patterns remains unclear and unstudied.
A number of studies reported a reduction in duration of mechanical ventilation, length of ICU stays (LOS), LOS in hospital, pneumonia, pain, need for tracheostomy, and overall cost of operatively treated patients who suffered multiple rib fractures in comparison with non-operatively treated patients. Even though patient selection and the timing of the operation appear critical to a successful outcome, there is no consensus. Reduction in mortality has only been shown in a small number of studies. The majority of studies are retrospective cohort and case-control studies. Conservative treatment, which consists of respiratory assistance and pain control, remains the preferred treatment in the overwhelming majority of patients with multiple rib fractures. In some subjects, the operative fixation of fractured ribs within 72 post injury hours can lead to better outcomes. More randomized control trials are necessary to better determine which patients benefit from surgical fixation (18).
Many fractures occur within 2.5 cm of the transverse process. There would appear to be an inadequate length of proximal rib on which to fixate a plate or deploy an intramedullary strut. Whether these should or should not be repaired remains a vexing question. Anterior fractures and the need to anchor plates to sternum or costal cartilage are another challenge. Many advanced techniques have been described but represent FDA “off label” uses of the current fixation systems.
Another question that has garnered significant debate is the necessity of repairing all fractures in a flail chest pattern. Nickerson et al. in 2016, asked “Does partial flail chest stabilization, compared with complete flail chest stabilization, result in satisfactory outcomes for patients?” They considered aggressive measures to reach fractures that are hard to access to be unnecessary. They assessed 43 subjects who had undergone operative stabilization of flail chest (84% with 6-month follow-up) and found in conclusion that: “Despite these obvious limitations of the study, we plan to incorporate our results into the practice of rib fracture stabilization at our institution. We routinely avoid additional incisions, repairing only those fractures that are readily accessible through the primary incision. From our presented evidence, we suggest that additional incisions or aggressive maneuvers to access all fractures are unnecessary and unwarranted” (19).
A related question is the appropriateness of repairing alternating, or “every other” rib in a line of fractures to minimize soft tissue dissection and cost. Here we have only expert opinion to guide us. The majority of rib repair experts believe that this alternating approach is less than desirable and provides inadequate stabilization and pain relief. Fractures of the chest apex remain challenging to expose and repair. Ribs 1 and 2 contribute little to the respiratory bellows but can contribute significantly to chest wall deformity. In a similar manner, ribs 11–12, which are free floating and difficult to expose through index incisions, are not usually repaired.
Regarding the cost effectiveness of CWS, a number of investigators have found that speedy surgical rib stabilization in subjects with blunt trauma to the chest is more cost effective than non-operative treatment on its own. The higher cost of surgical intervention is likely to be counterbalanced by the lower cost of consequent care as rates of respiratory failure and pneumonia, length of ICU stays, and length of hospital stay are reduced. A recent published publication from Swart E et al, utilized a cost-effectiveness analysis, supported by systematic review and meta-analysis, on outcomes after operative fixation of flail chest injuries. They evaluated stays in ICU, LOS, pneumonia, need for tracheostomy and mortality. The results were subsequently applied to a decision-analysis model that compared the costs and outcomes of operative fixation against non-operative treatment. Their results support the conclusion that surgical fixation of rib fractures from flail chest injuries reduced time spent in ICU, pulmonary complications, LOS in hospital, and mortality. This resulted in better health care-related outcomes and was a cost-effective intervention (20).
Lastly, what is known about who will/should perform CWS? Presently, various surgical subspecialties play a part in rib stabilization. Orthopedic surgeons, trauma surgeons, and thoracic surgeons have all demonstrated passion and requisite aptitude for rib fixation. Each one brings specific knowledge to patient care and is essential in a highly functioning trauma unit. Trauma surgeons are often the attendants and have the most complete knowledge for management of poly-trauma patients, while orthopedic surgeons are most familiar with the instrumentation required for the fixation of fractures. Lastly, one can argue that thoracic surgeons are best informed about the anatomy of the chest wall and dealing with other intrathoracic pathology. Thoracic surgeons often delegate this care to others in reality. Thoracic surgeons must preserve an active interest in this area of specialty.
Two clinical studies deserve mention. Caragounis et al. in 2016, reviewed in a prospective study, the long-term (1 year) effects of CWS on 54 patients who had a median Injury Severity Score of 20 [9–66] and a median New Injury Severity Score of 34 [16–66], presented with multiple rib fractures and flail chest and had undergone surgical stabilization with plate fixation. Patients completed a standardized questionnaire relating to pain, local discomfort, shortness of breath, use of analgesics and health-related quality of life (EQ-5D-3 L). This was done at 6 weeks, 3 months, 6 months and 1 year. Lung function, breathing movements, range of motion and physical function were evaluated. This showed a steady improvement in issues related to pain, quality of life, mobility and disability (21).
Finally, in an effort to inform the debate regarding the added expense of surgical fixation to a disease process that has traditionally been allowed to heal without surgical intervention, Majercik et al. compared in-hospital outcomes, costs, and charges for CWS patients, with and without surgical fixation. They compared patients who were admitted with rib fractures between January 2009 and June 2013. A 2-to-1 propensity score matching methodology was used to find non-operated patients who were similar to CWS patients. The final results show that the hospital charges and costs for CWS patients are higher. In mechanically ventilated patients without head injury, the in-hospital outcomes are better, with no difference in hospital charges and costs. Additional prospective cost-effectiveness research will determine whether better quality of life and the ability to return to productive activity earlier offsets the increased costs of acute care episodes for CWS patients (22).
Author’s note
In March 2017, the Chest Wall Injury Society officially launched with the mission of optimizing operative and non-operative care for patients with chest wall injury. They are currently accepting membership for surgeons and other healthcare professionals that function as part of the healthcare team. Anyone interested is invited to review more information regarding research, education, and advocacy efforts online at www.cwisociety.org.
Acknowledgements
Special thanks to SarahAnn Whitbeck and Dr. Sarah Majercik for their editing and review.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Chien CY, Chen YH, Han ST, et al. The number of displaced rib fractures is more predictive for complications in chest trauma patients. Scand J Trauma Resusc Emerg Med 2017;25:19. 10.1186/s13049-017-0368-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pieracci FM, Majercik S, Ali-Osman F, et al. Consensus statement: Surgical stabilization of rib fractures rib fracture colloquium clinical practice guidelines. Injury 2017;48:307-21. 10.1016/j.injury.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 3.Bemelman M, de Kruijf MW, van Baal M, et al. Rib Fractures: To Fix or Not to Fix? An Evidence-Based Algorithm. Korean J Thorac Cardiovasc Surg 2017;50:229-34. 10.5090/kjtcs.2017.50.4.229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fagevik Olsén M, Slobo M, Klarin L, et al. Physical function and pain after surgical or conservative management of multiple rib fractures - a follow-up study. Scand J Trauma Resusc Emerg Med 2016;24:128. 10.1186/s13049-016-0322-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kocher GJ, Sharafi S, Azenha LF, et al. Chest wall stabilization in ventilator-dependent traumatic flail chest patients: who benefits? Eur J Cardiothorac Surg 2017;51:696-701. [DOI] [PubMed] [Google Scholar]
- 6.Farquhar J, Almarhabi Y, Slobogean G, et al. No benefit to surgical fixation of flail chest injuries compared with modern comprehensive management: results of a retrospective cohort study. Can J Surg 2016;59:299-303. Erratum in: Can J Surg 2017;60:7. 10.1503/cjs.000515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uchida K, Nishimura T, Takesada H, et al. Evaluation of efficacy and indications of surgical fixation for multiple rib fractures: a propensity-score matched analysis. Eur J Trauma Emerg Surg 2017;43:541-7. 10.1007/s00068-016-0687-0 [DOI] [PubMed] [Google Scholar]
- 8.Pieracci FM, Lin Y, Rodil M, et al. A prospective, controlled clinical evaluation of surgical stabilization of severe rib fractures. J Trauma Acute Care Surg 2016;80:187-94. 10.1097/TA.0000000000000925 [DOI] [PubMed] [Google Scholar]
- 9.Pieracci FM, Coleman J, Ali-Osman F, et al. A multicenter evaluation of the optimal timing of surgical stabilization of rib fractures. J Trauma Acute Care Surg 2018;84:1-10. 10.1097/TA.0000000000001729 [DOI] [PubMed] [Google Scholar]
- 10.Fitzgerald MT, Ashley DW, Abukhdeir H, et al. Rib fracture fixation in the 65 years and older population: A paradigm shift in management strategy at a Level I trauma center. J Trauma Acute Care Surg 2017;82:524-7. 10.1097/TA.0000000000001330 [DOI] [PubMed] [Google Scholar]
- 11.Coughlin TA, Ng JW, Rollins KE, et al. Management of rib fractures in traumatic flail chest: a meta-analysis of randomised controlled trials. Bone Joint J 2016;98-B:1119-25. 10.1302/0301-620X.98B8.37282 [DOI] [PubMed] [Google Scholar]
- 12.Kaplan DJ, Begly J, Tejwani N. Multiple Rib Nonunion: Open Reduction and Internal Fixation and Iliac Crest Bone Graft Aspirate. J Orthop Trauma 2017;31 Suppl 3:S34-5. 10.1097/BOT.0000000000000910 [DOI] [PubMed] [Google Scholar]
- 13.Pieracci FM, Johnson JL, Stovall RT, et al. Completely thoracoscopic, intra-pleural reduction and fixation of severe rib fractures. Trauma Case Rep 2015;1:39-43. 10.1016/j.tcr.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skedros JG, Mears CS, Langston TD, et al. Medial scapular winging associated with rib fractures and plating corrected with pectoralis major transfer. Int J Surg Case Rep 2014;5:750-3. 10.1016/j.ijscr.2014.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marasco S, Liew S, Edwards E, et al. Analysis of bone healing in flail chest injury: do we need to fix both fractures per rib? J Trauma Acute Care Surg 2014;77:452-8. 10.1097/TA.0000000000000375 [DOI] [PubMed] [Google Scholar]
- 16.Majercik S, Vijayakumar S, Olsen G, et al. Surgical stabilization of severe rib fractures decreases incidence of retained hemothorax and empyema. Am J Surg 2015;210:1112-6; discussion 1116-7. 10.1016/j.amjsurg.2015.08.008 [DOI] [PubMed] [Google Scholar]
- 17.Dehghan N, de Mestral C, McKee MD, et al. Flail chest injuries: a review of outcomes and treatment practices from the National Trauma Data Bank. J Trauma Acute Care Surg 2014;76:462-8. 10.1097/TA.0000000000000086 [DOI] [PubMed] [Google Scholar]
- 18.Majak P, Næss PA. Rib fractures in trauma patients: does operative fixation improve outcome? Curr Opin Crit Care 2016;22:572-7. 10.1097/MCC.0000000000000364 [DOI] [PubMed] [Google Scholar]
- 19.Nickerson TP, Thiels CA, Kim BD, et al. Outcomes of Complete Versus Partial Surgical Stabilization of Flail Chest. World J Surg 2016;40:236-41. 10.1007/s00268-015-3169-3 [DOI] [PubMed] [Google Scholar]
- 20.Swart E, Laratta J, Slobogean G, et al. Operative Treatment of Rib Fractures in Flail Chest Injuries: A Meta-analysis and Cost-Effectiveness Analysis. J Orthop Trauma 2017;31:64-70. 10.1097/BOT.0000000000000750 [DOI] [PubMed] [Google Scholar]
- 21.Caragounis EC, Fagevik Olsén M, Pazooki D, et al. Surgical treatment of multiple rib fractures and flail chest in trauma: a one-year follow-up study. World J Emerg Surg 2016;11:27. 10.1186/s13017-016-0085-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Majercik S, Wilson E, Gardner S, et al. In-hospital outcomes and costs of surgical stabilization versus nonoperative management of severe rib fractures. J Trauma Acute Care Surg 2015;79:533-8; discussion 538-9. 10.1097/TA.0000000000000820 [DOI] [PubMed] [Google Scholar]