Summary
The present study examined whether work stressors contribute to sleep problems and depressive symptoms over the course of deployment (i.e., predeployment, postdeployment, and 6-month reintegration) among U.S. Navy members. Specifically, we examined whether depressive symptoms or sleep quality mediate the relationships between work stressors and these outcomes. Participants were 101 U.S. Navy members who experienced an 8-month deployment after Operational Enduring Freedom/Operation Iraqi Freedom. Using piecewise latent growth models, we found that increased work stressors was linked to increased depressive symptoms and decreased sleep quality across all three deployment stages. Further, increases in work stressors from pre- to postdeployment contributed to poorer sleep quality postdeployment via increasing depressive symptoms. Moreover, sleep quality mediated the association between increases in work stressors and increases in depressive symptoms from pre- to post-deployment. These effects were maintained from postdeployment through the 6-month reintegration. Although preliminary, our results suggest that changes in work stressors may have small, but significant implications for both depressive symptoms and quality of sleep over time and a bi-directional relationship persists between sleep quality and depression across deployment. Strategies that target both stress and sleep could address both precipitating and perpetuating factors that affect sleep and depressive symptoms.
Keywords: work stressors, depressive symptoms, sleep quality, military members, deployment
Introduction
Extensive research has shown that military members are at risk for insufficient sleep and poor sleep quality (RAND Corporation, 2015). Further, poor sleep is exacerbated during deployment (Seelig et al, 2010) and sleep disturbance may last for years after deployment (RAND Corporation, 2015). Among U.S. Navy members who took part in a recent cross-sectional study, prior deployment was associated with greater sleep-related daytime impairments (RAND Corporation, 2015). Further, sleep problems are associated with depression among redeployed soldiers (Luxton et al., 2011) and veterans (Swinkels et al., 2013). Despite the increase in work demands associated with deployment, and documented difficulty related to sleep (RAND Corporation, 2015) and depressive symptoms (Mustillo et al., 2015) among military members, the association between work stressors, sleep quality, and depressive symptoms over the course of deployment has received little attention.
Work Stressors, Depressive Symptoms, and Sleep Quality
A large literature has established a complex reciprocal relationship between a range of stress concepts and depression (Liu & Alloy, 2010). The adverse effects of stress on sleep are also well-established (Kim & Dimsdale, 2007). As related to occupational stressors, perceived work-related stressors may increase the risk of depression (Bonde, 2008), job stress is associated with poor sleep (Knudsen et al., 2007), and better sleep is associated with better work performance and less psychological distress (Barber et al., 2013). Among military personnel, recent research has found that work stressors are associated with problematic alcohol use via depressive symptoms (Kelley et al., in press) and poor sleep quality (Bravo et al., 2017). However, how work stressors, depressive symptoms, and sleep quality interrelate across deployment has not been examined.
Associations between sleep and depression are also well established, but causal relationships between these constructs are less clear. Sleep disturbance has been historically conceptualized as a symptom of depression, with both insomnia and hypersomnia being essential features of the disorder. However, research has underscored the bidirectional nature of these conditions, and growing empirical evidence supports the premise that sleep disturbance plays a causal role in the development of depression (Franzen & Buysse, 2008). For example, in a study of more than 15,000 U.S. military service members deployed since 9/11, predeployment insomnia symptoms were associated with increased odds of new onset of depression at post-deployment (Gehrman et al., 2013). When these findings were discussed in the context of the larger literature, the authors propose that insomnia may increase vulnerability to mental health disorders and/or result in a reduced capacity to deal with stress. In contrast, in a longitudinal study of Norwegians that examined associations between difficulty initiating sleep and depression from adolescence to adulthood, depressive symptoms were more predictive of future difficulty initiating sleep than was difficulty initiating sleep for predicting depressive symptoms across a 10-year period (Hayley et al., 2015). Thus, while the bidirectional nature of sleep and depression is supported, ongoing longitudinal research is needed to better understand the association and how level of stress may impact this relationship.
Present Study
To our knowledge, prior research has not previously examined longitudinal relationships between work stressors, sleep and depression concurrently, especially among military personnel. Examining U.S. Navy members across a single deployment presents a unique opportunity to assess these constructs with minimal external influences due to living in the same physical environment with comparable living situations across an identical time period. For the present study, we constructed piecewise latent growth models (LGM) to capture the growth or decay of relationships between variables from the previous time point (i.e., postdeployment to six-month reintegration). In other words, we chose a multi-slope LGM approach to examine this potential growth or decay of relationships after deployment and at 6-month reintegration given that sleep quality and depressive symptoms would likely be reactive to each other and work stressors in real time. Taken together, we tested two independent piecewise latent growth models to examine whether depression or sleep quality mediate the relationships between work stressors and these outcomes across deployment and to determine the relative magnitude of these effects. In light of the contradictory findings on longitudinal relationships between sleep and depression discussed above (Gehrman et al., 2013; Hayley et al., 2015), we did not hypothesize about what we expected to find in terms of mediation. As such, our analyses are considered exploratory.
Participants/Procedure
Participants were 101 U.S. Navy members assigned to an Arleigh Burke-class destroyer stationed in southeastern Virginia, who were assessed approximately 6 weeks prior to deployment (predeployment, n=101; spring 2013), approximately 6 weeks after the ship’s return (i.e., postdeployment, n=60; winter 2015) and 6 months after the ship’s return (reintegration, n=46; summer 2015). Among Navy members, 71.3% (n=72) were men, 64.4% (n=65) were White, and 100% had completed at least a GED/high school degree or some college. Further, the average age of participants was 28.34 (SD=5.99, Range=19–44) and average years in the Navy was 7.41 (SD=6.06, Range=less than 1 year to 21 years). See Kelley et al. (in press) for additional information regarding recruitment, demographics, and incentives. IRB approval was obtained prior to data collection and participants gave consent to participate.
Measures
Across all deployment stages, participants completed the same battery of measures. For all measures, composite scores were created by averaging or summing items and reverse-coding items when appropriate such that higher scores indicate higher levels of the construct.
Work stressors
Work stressors was assessed using the Command Stress Assessment (CSA; Chavez & Patrissi, 2012). We examined a 6-item subscale from the CSA that assesses workplace or command stress; measured on a 4-point response scale (0=a lot, 3=none at all). Participants were instructed to indicate how much stress they experienced from each of the following during the past 30 days: unpredictability of operations or job duties; communication within my organization; competing taskings from the chain of command; increase in my work load; working long hours; and conflicts between my professional duties and family responsibilities.
Depressive symptoms
Depressive symptoms was assessed using the Short Form of the Center for Epidemiologic Studies Depression Scale (CESD-10; Kohout et al., 1993). The CESD-10 assesses current depressive symptoms; measured on a 4-point response scale (0=rarely or none of the time/less than 1 day, 3=most or all of the time/5–7days). Participants were instructed to indicate how often they have felt a certain way during the past week (e.g., “I felt depressed”, “I felt sad”). Given that sleep quality was being modeled as a predictor and criterion of depressive symptoms, we removed an item that focused on sleep patterns (i.e., “My sleep was restless”).
Sleep Quality
In an attempt to develop a brief measure of sleep that would capture key sleep problems and reduce participant burden, four items were drawn from the Pittsburgh Sleep Quality Index (Buysse et al., 1989) and the Medical Outcomes Study sleep measure (Hays et al., 2005) and measured on a 5-point response scale. These items assessed sleep quality (“How would you rate your quality of sleep?”), sleepiness (“How often do you feel tired, fatigued, or sleepy during the daytime?), satisfaction (“How satisfied are you with your sleep?”), and trouble (“How often have you trouble falling asleep, staying asleep, or waking up too early?”). The response code for the sleepiness and trouble items were (1) never, to (5) very often; (1) very poor, to (5) very good for quality of sleep; and (1) very dissatisfied, to (5) very satisfied for sleep satisfaction. All four items loaded well onto a latent factor of sleep quality (Bravo et al., 2017).
Statistical Analyses
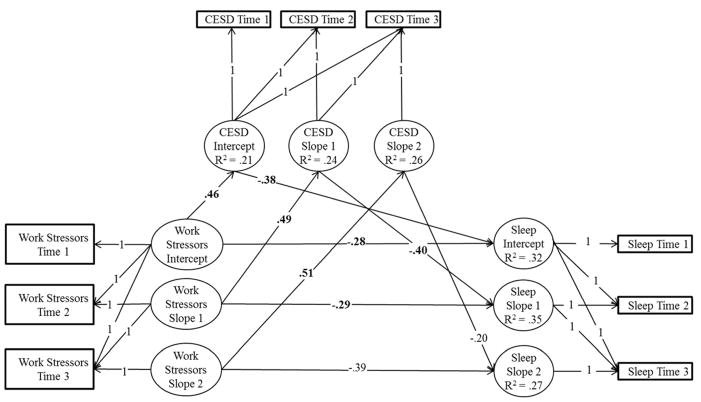
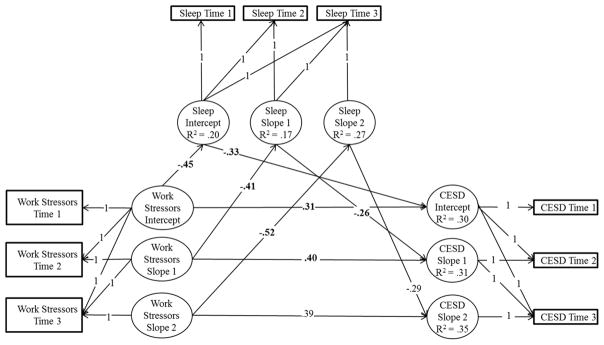
To test the proposed models, analyses were conducted in Mplus, version 7.2. (Muthén & Muthén, 1998–2015). In model 1 (see Figure 1), the structural paths assessed if work stressors influenced depressive symptoms (intercept) or its growth over time (slopes 1 and 2), and in turn if depressive symptoms influenced sleep quality (intercept) or its growth over time (slopes 1 and 2). Work stressors and depressive symptoms growth predicted sleep quality for the same period (e.g., depressive symptoms slope 1’s influence on sleep quality slope 1). In model 2 (see Figure 2), the structural paths assessed if work stressors influenced sleep quality (intercept) or its growth over time (slopes 1 and 2), and in turn if sleep quality influenced depressive symptoms (intercept) or its growth over time (slopes 1 and 2). Work stressors and sleep quality growth predicted depressive symptoms for the same period.
Figure 1.
Standardized results of the parallel-process latent growth model for work stressors, depressive symptoms, and sleep quality (N=101). Significant effects are in bold typeface for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. Factor loadings were set to 1 for the intercept to reflect predeployment levels for each construct. Factor loadings were set to 0, 1, and 1 for predeployment, postdeployment, and 6-month reintegration, respectively, for slope 1 to capture growth from predeployment to postdeployment, and were set to 0, 0, and 1 for slope 2 to capture growth from postdeployment to 6-month reintegration. Loadings constrained to 0 for the intercept and slope factors, correlations among errors, and disturbances are not displayed for clarity. CESD=10-item Center for Epidemiological Studies Depression Scale; Sleep=Sleep Quality.
Figure 2.
Standardized results of the parallel-process latent growth model for work stressors, sleep quality, and depressive symptoms (N=101). Significant effects are in bold typeface for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. Factor loadings were set to 1 for the intercept to reflect predeployment levels for each construct. Factor loadings were set to 0, 1, and 1 for predeployment, postdeployment, and 6-month reintegration, respectively, for slope 1 to capture growth from predeployment to postdeployment, and were set to 0, 0, and 1 for slope 2 to capture growth from postdeployment to 6-month reintegration. Loadings constrained to 0 for the intercept and slope factors, correlations among errors, and disturbances are not displayed for clarity. CESD=10-item Center for Epidemiological Studies Depression Scale; Sleep=Sleep Quality.
We examined the total, direct, and indirect effects of each predictor variable on outcomes using bias-corrected bootstrapped estimates based on 10,000 bootstrapped samples, which provides a powerful test of mediation (Fritz et al., 2007). Given that sample sizes approaching 100 are preferred for growth models (including parallel process latent growth models; Curran et al., 2010), missing data were handled using full information maximum likelihood, which has been found to be more efficient and has less bias than alternative procedures in structural equation models (Newman, 2014), including longitudinal models (Newman, 2003). Statistical significance was concluded if the 95% confidence intervals did not contain zero.
Results
All bivariate correlations, descriptive statistics, and Cronbach’s alphas among study variables across deployment stages (i.e., predeployment, postdeployment, and 6-month reintegration) are summarized in Table 1. Across all three deployment stages, more work stress was linked to higher depressive symptoms and lower sleep quality. Further, higher depressive symptoms were associated with lower sleep quality across deployment stages. To examine depressive symptoms and sleep quality as statistical mediators, we turn to the specific paths in the independent piecewise latent growth mediation models. It is important to note that all models were additionally conducted including gender, age, and years in the Navy as covariates; however, results were consistent across models (i.e., direct and indirect effects did not statistically change) and for simplicity only the models without these covariates are presented.
Table 1.
Descriptive statistics and correlations among all observed variables within the parallel-process latent growth models
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | M | SD | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Work Stressors Time 1 | .82 | 10.47 | 4.17 | ||||||||
| 2. Work Stressors Time 2 | .34 | .86 | 9.93 | 4.45 | |||||||
| 3. Work Stressors Time 3 | .09 | .31 | .89 | 10.56 | 5.00 | ||||||
| 4. CESD Time 1 | .45 | .33 | .02 | .87 | 9.35 | 6.09 | |||||
| 5. CESD Time 2 | .18 | .61 | .15 | .49 | .89 | 8.06 | 6.47 | ||||
| 6. CESD Time 3 | .07 | .26 | .41 | .57 | .56 | .87 | 9.19 | 6.31 | |||
| 7. Sleep Quality Time 1 | −.44 | −.37 | −.10 | −.49 | −.30 | −.35 | .75 | 9.99 | 2.52 | ||
| 8. Sleep Quality Time 2 | −.26 | −.58 | −.16 | −.32 | −.56 | −.23 | .60 | .87 | 11.00 | 3.11 | |
| 9. Sleep Quality Time 3 | −.04 | −.34 | −.43 | −.21 | −.43 | −.50 | .53 | .63 | .87 | 10.19 | 3.10 |
Note. Significant correlations are bolded for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. Cronbach’s alphas are underlined and shown on the diagonals. CESD=10-item Center for Epidemiological Studies Depression Scale. Time 1=predeployment; Time 2=postdeployment; Time 3=6-month reintegration.
Depressive Symptoms as a Mediator
Specific indirect and direct model effects are summarized in Table 2. The values represented in the top section of Table 2 represent the means (for work stressors) and intercepts (for depressive symptoms and sleep quality) for the latent growth model variables, which are interpreted as growth observed if the values of the associated predictors are zero. As seen in Table 2, if there is no change in work stressors, depressive symptoms growth to Time 2 (i.e., postdeployment) and growth to Time 3 (i.e., 6-month reintegration) is not significant. In other words, there is no significant change in depressive symptoms scores across time if there is no change in work stressors. Further, there is no significant change in sleep quality scores across time if there is no change in work stressors and depressive symptoms (see top of Table 2).
Table 2.
Parallel-process latent growth model of work stressors, depressive symptoms, and sleep quality with regression
| Means and Intercepts | b | β | 95% CI |
|---|---|---|---|
| Work Stressors Intercept | 10.46 | 2.51 | 9.58, 11.27 |
| Work Stressors Slope 1 | −0.46 | −0.09 | −1.64, 0.79 |
| Work Stressors Slope 2 | 0.52 | 0.09 | −1.36, 2.07 |
| CESD Intercept | 2.32 | 0.38 | −0.33, 5.00 |
| CESD Slope 1 | −1.29 | −0.20 | −2.80, 0.14 |
| CESD Slope 2 | 1.48 | 0.25 | −0.08, 3.06 |
| Sleep Quality Intercept | 13.31 | 5.16 | 11.96, 14.49 |
| Sleep Quality Slope 1 | 0.62 | 0.23 | −0.001, 1.21 |
| Sleep Quality Slope 2 | −0.45 | −0.17 | −1.18, 0.21 |
|
| |||
| Direct Effects | b | B | 95% CI |
|
| |||
| Work Stressors Intercept → CESD Intercept | 0.67 | 0.46 | 0.41, 0.94 |
| Work Stressors Slope 1 → CESD Slope 1 | 0.63 | 0.49 | 0.24, 1.01 |
| Work Stressors Slope 2 → CESD Slope 2 | 0.54 | 0.51 | 0.19, 0.79 |
| CESD Intercept → Sleep Quality Intercept | −0.16 | −0.38 | −0.23, −0.08 |
| CESD Slope 1 → Sleep Quality Slope 1 | −0.17 | −0.40 | −0.25, −0.08 |
| CESD Slope 2 → Sleep Quality Slope 2 | −0.09 | −0.20 | −0.26, 0.04 |
| Work Stressors Intercept → Sleep Quality Intercept | −0.18 | −0.28 | −0.29, −0.05 |
| Work Stressors Slope 1 → Sleep Quality Slope 1 | −0.15 | −0.29 | −0.26, −0.06 |
| Work Stressors Slope 2 → Sleep Quality Slope 2 | −0.19 | −0.39 | −0.37, 0.01 |
|
| |||
| Indirect Effects | b | β | 95% CI |
|
| |||
| Work Stressors Intercept → CESD Intercept → Sleep Quality Intercept | −0.11 | −0.17 | −0.18, −0.05 |
| Work Stressors Slope 1 → CESD Slope 1 → Sleep Quality Slope 1 | −0.11 | −0.20 | −0.20, −0.04 |
| Work Stressors Slope 2 → CESD Slope 2 → Sleep Quality Slope 2 | −0.05 | −0.10 | −0.17, 0.01 |
Note. Significant effects are in bold typeface for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. CESD=10-item Center for Epidemiological Studies Depression Scale. Slope 1 reflects growth from predeployment to postdeployment. Slope 2 reflects growth from postdeployment to 6-month reintegration. Note that the top section of the table displays means for exogenous variables (i.e., work stressors latent growth models) and intercepts for endogenous variables (i.e., depressive symptoms and sleep quality latent growth models).
At predeployment, higher work stressors was associated with higher depressive symptoms (β=.46), which in turn was associated with poorer sleep quality (β=−.38). As could be expected by these direct effects (see Figure 1), depressive symptoms mediated the relationship between work stressors and sleep quality at predeployment (indirect β=−.17) accounting for 37.81% of the total effect of work stressors on sleep quality. However, there was still a significant direct association between work stressors and poor sleep quality (β=−.28). At postdeployment (i.e., slope 1), increases in work stressors significantly predicted increases in depressive symptoms (β=.49). Further, increases in depressive symptoms did significantly predict decreases in sleep quality at postdeployment (β=−.40). As expected, there was a significant indirect effect (indirect β=−.15) suggesting that increases in work stressors significantly impacts (i.e., decreases) sleep quality postdeployment via increasing depressive symptoms. Depressive symptoms accounted for 40.77% of the total effect of work stressors on sleep quality; although there was still a significant direct association between work stressors and poor sleep quality (β=−.29). The indirect effect for slope 2 is not significant, indicating that these effects are maintained (i.e., not growth or decay) from postdeployment through the 6-month reintegration (see Table 2).
Sleep Quality as a Mediator
Specific indirect and direct model effects are summarized in Table 3. If there is no change in work stressors, sleep quality growth to Time 2 is significant indicating that sleep quality improves if there no change in work stressors from predeployment to postdeployment. However, sleep quality growth to Time 3 (i.e., 6-month reintegration) significantly decreases if there is no change in work stressors from postdeployment to 6-month integration. Further, there is no significant change in depressive symptoms scores across time if there is no change in work stressors and sleep quality (see top of Table 3).
Table 3.
Parallel-process latent growth model of work stressors, sleep quality, and depressive symptoms with regression
| Means and Intercepts | b | β | 95% CI |
|---|---|---|---|
| Work Stressors Intercept | 10.47 | 2.51 | 9.60, 11.30 |
| Work Stressors Slope 1 | −0.46 | −0.09 | −1.65, 0.80 |
| Work Stressors Slope 2 | 0.50 | 0.09 | −1.36, 2.05 |
| Sleep Quality Intercept | 12.82 | 5.06 | 11.57, 13.94 |
| Sleep Quality Slope 1 | 0.82 | 0.32 | 0.21, 1.42 |
| Sleep Quality Slope 2 | −0.70 | −0.27 | −1.41, −0.08 |
| CESD Intercept | 12.39 | 2.05 | 6.00, 18.16 |
| CESD Slope 1 | −0.33 | −0.05 | −1.69, 1.14 |
| CESD Slope 2 | 0.68 | 0.11 | −0.64, 2.25 |
|
| |||
| Direct Effects | b | β | 95% CI |
|
| |||
| Work Stressors Intercept → Sleep Quality Intercept | −0.27 | −0.45 | −0.37, −0.17 |
| Work Stressors Slope 1 → Sleep Quality Slope 1 | −0.21 | −0.41 | −0.31, −0.07 |
| Work Stressors Slope 2 → Sleep Quality Slope 2 | −0.25 | −0.52 | −0.43, −0.08 |
| Sleep Quality Intercept → CESD Intercept | −0.78 | −0.33 | −1.16, −0.35 |
| Sleep Quality Slope 1 → CESD Slope 1 | −0.65 | −0.26 | −1.13, −0.09 |
| Sleep Quality Slope 2 → CESD Slope 2 | −0.67 | −0.29 | −1.23, 0.11 |
| Work Stressors Intercept → CESD Intercept | 0.45 | 0.31 | 0.20, 0.72 |
| Work Stressors Slope 1 → CESD Slope 1 | 0.51 | 0.40 | 0.22, 0.79 |
| Work Stressors Slope 2 → CESD Slope 2 | 0.41 | 0.39 | −0.03, 0.70 |
|
| |||
| Indirect Effects | b | β | 95% CI |
|
| |||
| Work Stressors Intercept → Sleep Quality Intercept → CESD Intercept | 0.21 | 0.15 | 0.09, 0.37 |
| Work Stressors Slope 1 → Sleep Quality Slope 1 → CESD Slope 1 | 0.14 | 0.10 | 0.03, 0.31 |
| Work Stressors Slope 2 → Sleep Quality Slope 2 → CESD Slope 2 | 0.16 | 0.15 | 0.03, 0.36 |
Note. Significant effects are in bold typeface for emphasis and were determined by a 95% bias-corrected bootstrapped confidence interval (based on 10,000 bootstrapped samples) that does not contain zero. CESD=10-item Center for Epidemiological Studies Depression Scale. Slope 1 reflects growth from predeployment to postdeployment. Slope 2 reflects growth from postdeployment to 6-month reintegration. Note that the top section of the table displays means for exogenous variables (i.e., work stressors latent growth models) and intercepts for endogenous variables (i.e., sleep quality and depressive symptoms latent growth models).
At predeployment, higher work stressors was associated with poorer sleep quality (β=−.45), which in turn was associated with higher depressive symptoms (β=−.33). As could be expected by these direct effects (see Figure 2), sleep quality mediated the relationship between work stressors and depressive symptoms at predeployment (indirect β=.15) accounting for 31.78% of the total effect of work stressors on depressive symptoms. However, there was still a significant direct association between work stressors and depressive symptoms (β=.31). At postdeployment (i.e., slope 1), increases in work stressors significantly predicted poorer sleep quality (β=−.41). Further, poorer sleep quality did significantly predict increases in depressive symptoms at postdeployment (β=−.26). As expected, there was a significant indirect effect (indirect β=−.10) suggesting that increases in work stressors significantly impacts (i.e., increases) depressive symptoms postdeployment via decreasing sleep quality. Sleep quality accounted for 21.06% of the total effect of work stressors on depressive symptoms; although there was still a significant direct association between work stressors and depressive symptoms (β=−.41). The indirect effect for slope 2 is significant; however, caution must be taken given the non-significant direct path between sleep quality and depressive symptoms (see Table 3).
Discussion
In the present study, we examined how work stressors were associated with sleep quality and depressive symptoms over the course of U.S. Navy deployment. Consistent with the bi-directional nature of sleep quality and depression described in prior studies, our findings suggest that poorer sleep quality might be a mechanism through which work stress results in increased depressive symptoms, and that increased depressive symptoms might be a mechanism through which work stress results in poorer sleep quality. Interestingly, we also found that a consistent level of work stress from postdeployment to six-month reintegration was associated with a decrease in sleep quality. This finding is consistent with prior research showing an increase in psychiatric difficulties with increasing time since deployment (Milliken et al., 2007).
Taken together, our findings are consistent with previous research linking higher stress with poorer sleep among U.S. Navy members (Chavez & Patrissi, 2012) and negative deployment experiences with increased levels of depressive symptoms (Welsh et al., 2015). The link between depressive symptoms and decreased sleep quality has been well articulated in previous literature (Franzen & Buysse, 2008). However, the underlying mechanism for this link has been debated. Impaired sleep and depression are likely to interact in such a way as to not only facilitate the onset of the other condition, but may also interact to sustain the other condition. For example, chronic sleep disturbance can impair functioning across a range of life domains, including occupational (Kucharczyk et al., 2012) and interpersonal functioning (Beattie et al., 2015); and impaired functioning across these life domains is likely to exacerbate poor mood and dysfunctional cognitions (McKnight & Kashdan, 2009). Similarly, depressed individuals often engage in sleep behaviors that work against optimal sleep. For example, they often use their sleep environments as a venue for disengagement from life (Manber et al., 2008), and their inactivity and limited light exposure has adverse implications for circadian regulation (Germain & Kupfer, 2008).
The two-process model of sleep regulation (Borbély & Wirz-Justice, 1982), focused on circadian and homeostatic sleep processes, is a particularly relevant theoretical framework for examining our findings. U.S. Navy members routinely experience both sleep deprivation (Harrison et al, 2017) and circadian misalignment (Skornyakov, et al, 2017), and prior research has demonstrated clear relationships between these circadian and homeostatic sleep processes and depression. Reduced slow wave sleep activity in depression is hypothesized to result from impairments in sleep homeostasis (Borbély & Wirz-Justice, 1982), and circadian rhythm dysregulation is common among those with mood disorders (Rumble, White, & Benca, 2015). In a recent reappraisal of the two-process model of sleep, Borbély and colleagues (2016) integrated recent evidence of synergistic effects between the two sleep processes. Studies demonstrating this synergistic effect were focused on the acute effects of disrupted sleep (Landsness et al, 2011). However, military personnel experience sustained periods of sleep disruption, including both sleep deprivation and circadian dysregulation. Future research should consider the possibility of synergistic effects of circadian and homeostatic sleep processes when examining the sequelae of work stressors on sleep and depression among military service members.
Clinical Implications
Given the high demands and unique circumstances around active duty service in the U.S. Navy, service members are at risk of developing chronic sleep issues. In accordance with the 3Ps Model of Insomnia (Spielman et al., 1987), military service members are subject to numerous precipitating factors for the onset of insomnia (Bramoweth & Germain, 2013). In particular, U.S. Navy members experience tight sleep quarters, have irregular and alternating shifts with no weekends and few days off during a long deployment, have high levels of caffeine intake, and experience increases in hypervigilance/hyperarousal due to the nature of their mission. Each of these precipitating factors sets the stage for changes in both behaviors and cognitions (perpetuating factors) that promote sustained sleep difficulties. Therefore, prevention strategies that target U.S. Navy ship operations (e.g., more consistent, shorter shifts) and/or teach Navy members techniques that bring on an earlier onset of sleep (e.g., self-guided relaxation or meditative exercises) could help foster better quality of sleep, which may in turn reduce negative outcomes (e.g., depression).
With regards to treatment, in a stepped care approach (Espie, 2009) the degree of symptomology (both depressive and sleep) would dictate level of care required. Given the treatment engagement difficulties among active duty service members, creative self-directed approaches may be best suited for U.S. Navy members. In a recent RAND study (2015), recommendations for sleep treatment have been proposed to include mobile and web-based interventions as well as telehealth communication to assist those with more complex or severe symptoms. Other recommendations included CAM (Complementary and Alternative Medicine) treatments, such as yoga and meditation, which have shown promise in assisting with symptoms of depression and sleep difficulties in military populations (RAND Corporation, 2015).
Limitations
Several limitations should be noted. Only 61% of those who completed the predeployment survey completed the postdeployment and/or 6-month postdeployment survey. We do not know whether crewmembers who declined to participate at the postdeployment and 6-month postdeployment surveys were no longer assigned to the ship and did not receive the survey reminders or if they chose not to participate. However, there were no significant demographic differences between those who participated in the postdeployment surveys versus those that did not. Beyond the small sample size, all participants were assigned to a single ship. Although collecting data from a single ship reduces the number of external environmental factors that may affect our studied relationships, we are limited in our generalizability and our results should not be construed as representative of all U.S. Navy members or even those assigned to ship duty. Despite the study limitations, the high work demands experienced by current U.S. Navy members, the prospective nature of the study, and the importance of these issues may offset these concerns. At the same time, future research should attempt to replicate these findings with larger samples and to test more complex models (e.g., multi-group models comparing these models across different job roles).
Conclusions
Across all three deployment stages (i.e., predeployment, postdeployment, and 6-month reintegration), work stressors was associated with higher/increased depressive symptoms and lower/decreased sleep quality. At predployment, sleep quality mediated the association between work stressors and depressive symptoms, and depressive symptoms mediated the association between work stressors and sleep quality at predeployment. Depressive symptoms mediated the association between increases in work stressors and decreases in sleep quality from pre- to postdeployment, and these effects were maintained from predeployment to 6-month postdeployment reintegration. Comparably, sleep quality mediated the association between increases in work stressors and increases in depressive symptoms from pre- to post-deployment. These effects were also maintained from postdeployment through the 6-month reintegration. Although our results should be considered preliminary, they suggest that changes in work stressors may have small, but significant implications for both depressive symptoms and quality of sleep over time and a bi-directional relationship persists between sleep quality and depression across deployment. Our preliminary findings draw further attention to the need to address work stressors and techniques to reduce depressive symptoms and increase sleep quality among current U.S. Navy members.
Acknowledgments
Funding: This work was conducted at Old Dominion University and was supported by a grant from the American Psychological Association Society for Military Psychology (Division 19) to MLK. AJB is supported by a training grant (T32-AA018108) from the National Institute on Alcohol Abuse and Alcoholism (NIAAA). CSU is supported by a Veterans Affairs Research Career Development Award (CDA-09-218).
Footnotes
Author Contributions
Dr. Bravo conceptualized the research questions, conducted the analyses, drafted the statistical analyses and results sections, and created the tables and figures. Dr. Kelley designed/conducted the study and wrote parts of the introduction and discussion sections. Dr. Swinkels assisted with interpretation of the data and drafted parts of the discussion section. Dr. Ulmer drafted parts of the introduction and discussion sections. All authors contributed to and approved of the final manuscript.
Conflict of Interest: All of the authors do not have any conflict of interest that could inappropriately influence, or be perceived to influence, our work.
References
- Barber L, Grawitch MJ, Munz DC. Are better sleepers more engaged workers? A self-regulatory approach to sleep hygiene and work engagement. Stress Health. 2013;29:307–316. doi: 10.1002/smi.2468. [DOI] [PubMed] [Google Scholar]
- Beattie L, Kyle SD, Espie CA, Biello SM. Social interactions, emotion and sleep: A systematic review and research agenda. Sleep Med Rev. 2015;24:83–100. doi: 10.1016/j.smrv.2014.12.005. [DOI] [PubMed] [Google Scholar]
- Bonde JPE. Psychosocial factors at work and risk of depression: A systematic review of the epidemiological evidence. Occup Environ Med. 2008;65:438–445. doi: 10.1136/oem.2007.038430. [DOI] [PubMed] [Google Scholar]
- Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: A reappraisal. J Sleep Res. 2016;25:131–43. doi: 10.1111/jsr.12371. [DOI] [PubMed] [Google Scholar]
- Borbély AA, Wirz-Justice A. Sleep, sleep deprivation and depression. A hypothesis derived from a model of sleep regulation. Hum Neurobiol. 1982;1:205–210. [PubMed] [Google Scholar]
- Bramoweth AD, Germain A. Deployment-related insomnia in military personnel and veterans. Curr Psychiatry Rep. 2013;15:1–8. doi: 10.1007/s11920-013-0401-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bravo AJ, Kelley ML, Hollis BF. Work stressors, sleep quality, and alcohol-related problems across deployment: A parallel process latent growth modeling approach among Navy members. Stress Health. 2017 doi: 10.1002/smi.2712. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Chavez B, Patrissi G. The Command Stress Assessment. 2012 Retrieved from 2012PC-Chavez-Patrissi-Command_Stress_Assessment.pdf.
- Curran PJ, Obeidat K, Losardo D. Twelve frequently asked questions about growth curve modeling. J Cogn Dev. 2010;11:121–136. doi: 10.1080/15248371003699969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espie CA. “Stepped care”: A health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep. 2009;32:1549–1558. doi: 10.1093/sleep/32.12.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzen PL, Buysse DJ. Sleep disturbances and depression: Risk relationships for subsequent depression and therapeutic implications. Dialogues Clin Neurosci. 2008;10:473–481. doi: 10.31887/DCNS.2008.10.4/plfranzen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz MS, MacKinnon DP. Required sample size to detect mediated effect. Psychol Sci. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gehrman P, Seelig AD, Jacobson IG, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. 2013;36:1009–1018. doi: 10.5665/sleep.2798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Germain A, Kupfer DJ. Circadian rhythm disturbances in depression. Hum Psychopharmacol. 2008;23:571–585. doi: 10.1002/hup.964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayley AC, Skogen JC, Sivertsen B, et al. Symptoms of depression and difficulty initiating sleep from early adolescence to early adulthood: A longitudinal study. Sleep. 2015;38:1599–1606. doi: 10.5665/sleep.5056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison E, Glickman GL, Beckerley S, Taylor MK. Self-reported sleep during US Navy operations and the impact of deployment-related factors. Mil Med. 2017;182:189–194. doi: 10.7205/MILMED-D-16-00078. [DOI] [PubMed] [Google Scholar]
- Hays RD, Martin SA, Sesti AM, Spritzer KL. Psychometric properties of the medical outcomes study sleep measure. Sleep Med. 2005;6:41–44. doi: 10.1016/j.sleep.2004.07.006. [DOI] [PubMed] [Google Scholar]
- Kelley ML, Bravo AJ, Hollis BF. Work stressors, depressive symptoms, and hazardous alcohol use among Navy members: Do work stressors contribute to hazardous drinking across deployment? Mil Psychol. in press. [Google Scholar]
- Kim EJ, Dimsdale JE. The effect of psychosocial stress on sleep: A review of polysomnographic evidence. Behav Sleep Med. 2007;5:256–278. doi: 10.1080/15402000701557383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen HK, Ducharme LJ, Roman PM. Job stress and poor sleep quality: Data from an American sample of full-time workers. Soc Sci Med. 2007;64:1997–2007. doi: 10.1016/j.socscimed.2007.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D Depression Symptoms Index. J of Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- Kucharczyk ER, Morgan K, Hall AP. The occupational impact of sleep quality and insomnia symptoms. Sleep Med Rev. 2012;16:547–559. doi: 10.1016/j.smrv.2012.01.005. [DOI] [PubMed] [Google Scholar]
- Landsness EC, Goldstein MR, Peterson MJ, Tononi G, Benca RM. Antidepressant effects of selective slow wave sleep deprivation in major depression: A high-density EEG investigation. J Psychiatr Res. 2011;45:1019–1026. doi: 10.1016/j.jpsychires.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu RT, Alloy LB. Stress generation in depression: A systematic review of the empirical literature and recommendations for future study. Clin Psychol Rev. 2010;30:582–593. doi: 10.1016/j.cpr.2010.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luxton DD, Greenburg D, Ryan J, Niven A, Wheeler G, Mysliwiec V. Prevalence and impact of short sleep duration in redeployed OIF soldiers. Sleep. 2011;34:1189–1195. doi: 10.5665/SLEEP.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manber R, Edinger JD, Gress JL, San Pedro-Salcedo MG, Kuo TF, Kalista T. Cognitive behavioral therapy for insomnia enhances depression outcome in patients with comorbid major depressive disorder and insomnia. Sleep. 2008;31:489–495. doi: 10.1093/sleep/31.4.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKnight PE, Kashdan TB. The importance of functional impairment to mental health outcomes: A case for reassessing our goals in depression treatment research. Clin Psychol Rev. 2009;29:243–259. doi: 10.1016/j.cpr.2009.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298:2141–2148. doi: 10.1001/jama.298.18.2141. [DOI] [PubMed] [Google Scholar]
- Mustillo SA, Kysar-Moon A, Douglas SR, et al. Overview of depression, post-traumatic stress disorder, and alcohol misuse among active duty service members returning from Iraq and Afghanistan, self-report and diagnosis. Mil Med. 2015;180:419–427. doi: 10.7205/MILMED-D-14-00335. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Muthén and Muthén; Los Angeles: 1998–2015. [Google Scholar]
- Newman DA. Longitudinal modeling with randomly and systematically missing data: A simulation of ad hoc, maximum likelihood, and multiple imputation techniques. Organ Res Methods. 2003;6:328–362. [Google Scholar]
- Newman DA. Missing data: Five practical guidelines. Organ Res Methods. 2014;17:372–411. [Google Scholar]
- RAND Corporation. Sleep in the military: Promoting healthy sleep among U.S. servicemembers. RAND Corporation; Santa Monica: 2015. [PMC free article] [PubMed] [Google Scholar]
- Rumble ME, White KH, Benca RM. Sleep disturbances in mood disorders. Psychiatr Clin N AM. 2015;38:743–759. doi: 10.1016/j.psc.2015.07.006. [DOI] [PubMed] [Google Scholar]
- Seelig AD, Jacobson IG, Smith B, et al. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep. 2010;33:1615–1622. doi: 10.1093/sleep/33.12.1615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skornyakov E, Shattuck NL, Winser MA, et al. Sleep and performance in simulated Navy watch schedules. Accid Anal Prev. 2017;99:422–427. doi: 10.1016/j.aap.2015.11.021. [DOI] [PubMed] [Google Scholar]
- Spielman AJ, Caruso LS, Glovinsky PB. A behavioral perspective on insomnia treatment. Psychiatr Clin North Am. 1987;10:541–553. [PubMed] [Google Scholar]
- Swinkels CM, Ulmer CS, Beckham JC, Buse N, Calhoun PS VA Mid-Atlantic MIRECC Registry Workgroup. The associations of sleep duration, mental health, and health risk behaviors among U.S. Afghanistan/Iraq Era Veterans. Sleep. 2013;36:1019–25. doi: 10.5665/sleep.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh JA, Olson J, Perkins DF, Travis WJ, Ormsby L. The role of natural support systems in the post-deployment adjustment of active duty military personnel. Am J Community Psychol. 2015;56:69–78. doi: 10.1007/s10464-015-9726-y. [DOI] [PubMed] [Google Scholar]