Abstract
Ureteral stricture formation after ureteroscopic lithotripsy is a late complication that can lead to hydronephrosis and a subsequent risk of renal deterioration. The specific incidence is unknown, and the mechanism of stricture formation has not been completely explained. In this review, we summarize the current evidence regarding the incidence of this condition and discuss its pathogenesis. We then list preventive strategies to reduce the morbidity of ureteral strictures.
Keywords: Ureteroscopy, Ureteral stricture, Lithotripsy, Complications
1. Introduction
Due to technological developments in the past 2 decades, ureteroscopy has played an increasingly important role in the diagnosis and treatment of upper urinary diseases. According to a recent report, ureteroscopic lithotripsy (URL) has replaced shockwave lithotripsy (SWL) as the primary treatment modality for upper tract calculi in the United States [1].
However, with such wide application, the complications of URL should not be ignored [2], [3]. As one of the late complications of URL, ureteral stricture can lead to ureteral obstruction and progressive deterioration of renal function. In patients with “silent ureteral obstruction”, irreversible renal failure may occur if routine postoperative follow-ups are not conducted.
Our aim is to summarize the incidence, risk factors, etiology, and prevention strategies of ureteral stricture following URL.
2. Evidence acquisition
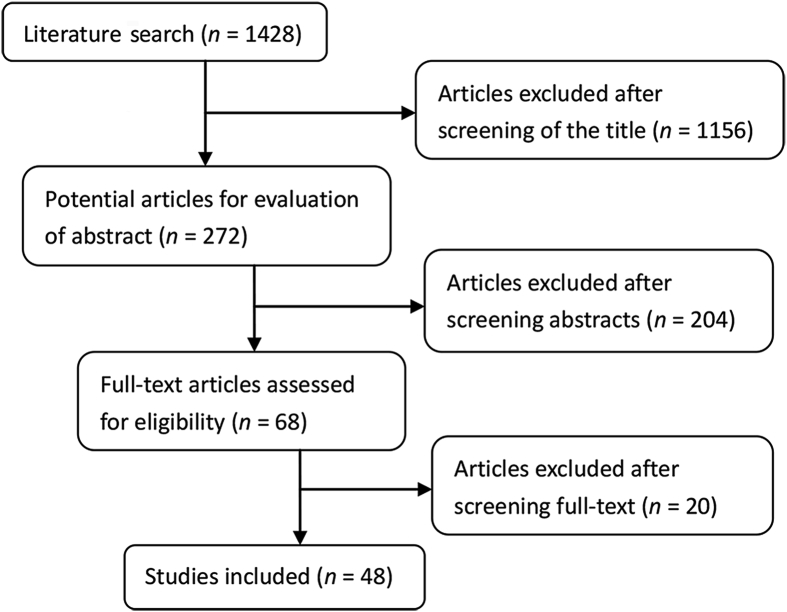
A literature search was performed using the PubMed from January 1970 to March 2017. The following terms and combinations of terms were searched: “ureteral stricture or ureteral stenosis” combined with the terms “ureteroscopy or ureteroscopic lithotripsy”, and “complications” combined with “ureteroscopy or ureteroscopic lithotripsy”. The review identified 1428 articles in total with the use of the above mentioned keywords in English. We excluded those articles if they did not corresponding with the aim of our review by reading title, abstracts and full-text screening. Finally, 48 studies were considered valuable for this review (Fig. 1). These articles include four reviews, five randomized controlled trials, five prospective studies, and 34 retrospective studies. The primary aim of the review is to report the incidence, pathogenesis and risk factors of ureteral strictures following ureteroscopy. The second aim is to introduce preventive measures for ureteral strictures.
Figure 1.
Flowchart for article selection of the review.
3. Incidence
There is significant variability in the reported incidence of ureteral stricture formation following URL. According to recent studies, the incidence of ureteral stricture following URL is 0.71% (0.30%–23.81%) (Table 1). In addition to the risk factors of stricture formation, the incidence of ureteral stricture is also influenced by the strategy of postoperative imaging follow-up. In some studies, the incidence of ureteral stenosis may be underestimated due to insufficient follow-up [4], [5].
Table 1.
Strictures after ureteroscopic treatment of ureter stones.
| Study | No. of patients | Age (year) | Stone size (mm)b | Stone location |
Impacted rate (%) | Type of ureteroscopy | Type of lithotripsy | Ureters cope size (Fr) | No. of stricture | Mean follow-up (month) | Incidence (%) | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Proximal | Middle | Distal | |||||||||||
| Roberts et al., 1998 [8]a | 21 | 41.6 | 10.3 | 3 | 8 | 10 | 100 | R | LL | 7–10 | 5 | 7.0 | 23.81 |
| Weizer et al., 2002 [9] | 241 | 47.2 | 3–35 | 56 | 111 | 74 | – | R/F | LL | – | 3 | 5.4 | 1.24 |
| Brito et al., 2006 [10]a | 42 | 23–72 | 5–20 | 9 | 12 | 21 | 100 | R | PL | 8.5 | 6 | 6.0 | 14.29 |
| El-Abd et al., 2014 [5] | 1950 | – | – | 789 | – | 1161 | – | R/F | LL/PL | 7.4–8.5 | 12 | 7.6 | 0.6 |
| Adiyat et al., 2009 [11] | 214 | 48.3 | 10.85 | 114 | 42 | 58 | 5.14 | R/F | LL | 6–7.5 | 3 | 14.5 | 1.40 |
| Binbay et al., 2011 [12]a | 80 | 39.9 | – | 12 | 21 | 47 | 100 | R | LL/PL | 8.5 | 1 | 15 | 1.25 |
| de la Rosette et al., 2014 [3] | 10 511 | 48.7 | – | 3101 | 2390 | 5020 | 27.2 | R/F | LL/PL/ UL/EL |
– | 36 | – | 0.30 |
| Li et al., 2015 [13] | 982 | 41.9 | 5–15 | – | 387 | 595 | – | R | LL/PL | 7.5 | 29 | 12 | 2.95 |
| Fam et al., 2015 [14] | 64 | – | – | 21 | 15 | 28 | 100 | R | LL | 6.5 | 5 | 7.0 | 7.81 |
| Combined | 14 105 | – | – | 4105 | 2986 | 7014 | – | – | – | – | 100 | 9.3 | 0.71 |
Series of patients with impacted stones; R, rigid ureteroscopy; F, flexible ureteroscopy; LL, laser lithotripsy; PL, pneumatic lithotripsy; UL, ultrasonic lithotripsy; EL, electrohydraulic lithotripsy; –,data deficient or not mentioned.
Data presented as mean or range.
With the development of equipment and accumulation of experience, the risk of ureteral injury and ureteral stricture has decreased dramatically. In a retrospective study, Elashry et al. [6] compared the outcomes of patients who underwent URL from 1991 to 1995 (Group 1) with patients who underwent this procedure from 1996 to 2005 (Group 2) in a single center. In the latter group, intraoperative perforation and avulsion decreased from 3.3% to 0.5% and from 1.3% to 0.1%, respectively. In addition, the incidences of ureteric stricture were 0.7% and 0.1% in Group 1 and Group 2, respectively (p = 0.007). Another study summarizing the 15-year experience of a urologist and showed a similar result [7].
4. Risk factors
According to previous reports, the incidence of ureteral stricture is high in patients with impacted stones. A retrospective study conducted in 1998 reported that the incidence of stricture formation following endoscopic treatment was nearly 24% [8]. Brito et al. [10] evaluated the outcomes of URL for impacted ureteral stones with a pneumatic lithotripter. Ureteral stricture was observed in 14.29% of patients (6/42) during the follow-up period. A more recent prospective study was conducted to evaluate the risk of ureteral stricture in patients with impacted stones after ureteroscopic treatment [14]. The incidence of ureteral stricture in this previous report was 7.8% of a total 64 patients. Xi et al. [15] compared the outcomes of URL and ureteroureterostomy for patients with impacted ureteral stones. Compared with the ureteroureterostomy group, a higher incidence of ureteral stricture was observed in the URL group (26.2% vs. 4.0%; p = 0.019). This result showed that the removal of the pathologic ureter with a polyp or stricture lesion might reduce the long-term risk of ureteral stricture for patients with impacted stones [15].
There is limited literature evaluating the risk of stricture formation in different parts of the ureter. In a global study of 9681 cases of URL, the incidence of ureteral stricture was 0.9% for proximal ureter locations, 1.1% for midureteral locations and 0.7% for distal ureter locations [16]. The difference between the three groups was not statistically significant. However, according to the study by Brito et al. [10], URL for proximal ureter stones was associated with a higher risk of perforation and ureteral stricture compared to distal or midureteral stones. In addition, the study by Schuster et al. [17] showed similar result. The intraoperative perforation rate after URL was 6.3% and 4.2% for proximal and distal stones, respectively. Another retrospective study also concluded that proximal ureteral stone was one of the significant factors for unfavorable results of semi-rigid ureteroscopy [18].
The ureteral access sheath (UAS) has been used worldwide for flexible-URL to enable multiple access points to the collecting system, to maintain low intrarenal pressure and to protect the scope [19], [20], [21]. Use of UAS has the advantages of minimizing the damage to ureter and improving the effectiveness of operation [22]. However, there is no consensus on whether the application of a UAS in flexible ureteroscopy increases the risk of ischemic injury and subsequent stricture. Lallas et al. [23] studied the potential risk of ischemia in porcine ureters, and the results showed that the ischemia is transient and is not enough to induce ischemic injuries. A study assessed the long-term incidence of ureteral stricture formation in patients receiving ureteroscopy with a UAS [24]. The incidence of ureteral stricture was 1.4% (1/71) which is similar to previously reported published stricture rates without the use of UAS and no evidence showed that the UAS is a contributing factor for stricture formation in the patient who developed this complication [24], [25]. Wang et al. [26] evaluated the influence of the use of a UAS on the outcomes of ureteroscopy in children. The intraoperative complication rate was higher in patients undergoing ureteroscopy with a UAS (15% vs. 2%, p = 0.02). Ureteral stricture was not observed with a median follow-up of 11 months. Traxer and Thomas [27] conducted a prospective study to evaluate the incidence and severity of ureteral injury caused by introducing a UAS. Ureteral injuries were observed in 46.5% of patients (167/359). Among these complications, severe ureteral injury involving the smooth muscle layers occurred in 13.3% of patients. The limitation of this study was that it lacked a long-term follow-up, which is important for evaluating the incidence of ureteral stricture. Therefore, a prospective multicenter study with long-term follow-up is needed to evaluate the impact of ureteral soft lens sheath on ureteral stenosis. A study suggests that a double-J tube should be placed in patients with impacted stones, intraoperative ureteral injuries and preoperative ureteral strictures after ureteroscopy with UAS [28]. The postoperative hydronephrosis was detected in 3 days after the operation in 54% (34/63) patients and no hydronephrosis was detected after a 2-month follow-up [28].
Holmium:yttrium-aluminum-garnet (Ho:YAG) lasers and pneumatic lithotripters are the most commonly used lithotripters for URL. Compared with the use of pneumatic lithotripters, Ho:YAG laser lithotripsy has the advantages of using a small caliber scope, causing minimal stone migration and producing smaller stone fragments. Binbay et al. [12] conducted a prospective study to compare the outcomes for the use of a pneumatic lithotripter or a Ho:YAG laser for the treatment of impacted ureteral stones. In their study, ureteral stricture was observed in 2.5% of patients in the pneumatic group, while no stricture was noted in the laser group after a >16-month follow-up. However, a recent meta-analysis reported the opposite conclusion in terms of risks of postoperative ureteral stricture [4]. A total of eight studies with 1555 patients were included, and the incidence of ureteral stricture following URL was higher in the laser group than in the pneumatic group (OR = 3.38, 95%CI: 1.56–7.31, p = 0.002). In this previous review, the number of postoperative ureteral stricture patients was much higher in one study than in the others (29 vs. 5), a factor which may have influenced the conclusion of the review.
A large-caliber ureteroscope increases the risk of ureteral injury following stricture formation. A retrospective study conducted in 1995 revealed that the use of conventional large rigid ureteroscopes was associated with a high ureteral injury rate [29]. In the large ureteroscope group, the rates of small mucosal lesions and full-thickness perforations were 24.5% and 11.2%, respectively. In the small ureteroscope group, the rates of mucosal lesions and perforations were 6.1% and 2%, respectively. Another study by Yaycioglu et al. [30] showed a similar result. Compared with a 10 Fr ureteroscope, a 7.5 Fr ureteroscope was associated with a better outcome in the treatment of ureteral stones. A retrospective study of 2461 patients investigated the outcomes of URL with different-caliber semi-rigid ureteroscopes [7]. A 10/10.5 Fr scope was used in Group 1, an 8.9/9.8 Fr scope in Group 2, and a 6/7.5 Fr scope in Group 3. According to modified Satava classification, the overall complication rates were 10.8%, 7.6%, and 6.9%, respectively (p = 0.01).
Other risk factors that are associated with an unfavorable result of URL include stone size and the experience of the urologist. A long-term study reported that the ureteral stricture rate is 4.4% with stone sizes larger than 2 cm; this is compared to 0.17% with stone sizes smaller than 2 cm (p < 0.001) [5]. Sugihara et al. [31] analyzed 12 372 cases to investigate the risk factors of severe adverse events after URL. Their results showed that high-volume centers were associated with lower complication rates, indicating that the experience of the surgeon plays a key role in minimizing the risk of ureteral injury.
5. Pathogenesis
The mechanism of ureteral stricture formation following URL may be multifactorial and is not fully understood. The contributing factors of postoperative ureteral stricture may include intraoperative ureteral injury and a long-term inflammation reaction caused by the stones. Eight studies discussed the pathogenesis of ureteral stricture in our included articles.
It is believed that the ureteral injuries during the procedure and the subsequent inflammation are key steps toward stricture formation [8], [14]. The injured mucosa produces a fibrinous exudate, which can lead to an inflammatory reaction and promote stricture formation. Previous reports have shown that ureteric perforation is associated with a high rate of ureteral stricture [8], [10], [14]. In the report by Roberts et al. [8], 80% of patients with postoperative ureteral stricture had intraoperative ureteral perforation, indicating that ureteral perforation at the site of the stone was the key risk factor for stricture formation. The study by Brito et al. [10] showed the overall incidence of ureteral stricture was 14.29% in patients with impacted ureteral calculi treated by pneumatic lithotripsy. However, the incidence of ureteral stricture was 75% in patients who experienced a perforation during the procedure. El-Abd et al. [5] reported that among 1980 patients who underwent ureteroscopy for ureteral calculi, ureteral stricture occurred in six of eight patients with an intraoperative ureteral perforation.
Impacted ureteral stones increase the risk of ureteral stricture in different ways. First, long-term irritation caused by the impacted stone can lead to the ureteral lesion. Yamaguchi et al. [32] reported that two types of microscopic lesions in ureteral lesions are associated with impacted stones. Type 1 lesions are edematous or cystic hemispheric lesions and appear microscopically as submucosal edema. Type 2 lesions were defined as having a villous appearance and appeared microscopically as being composed of columnar mesenchymal tissue. Endoscopic observation revealed inflammatory ureteral polyps and ureteral stricture in 30.9% and 17.0% of patients with ureteral impacted stones, respectively [33]. These lesions result in a susceptibility to fibrosis and stenosis. Second, epithelial hypertrophy and edema caused by impaction increase the frangibility of surrounding tissues. Limited working space caused by impaction increases the risk of perforation during the ureteroscopic lithotripsy process. Moreover, over the long term, stone impaction can cause urinary infection and urine extravasation, which can also lead to periureteral fibrosis [34].
In addition, ischemia, granuloma and fibrosis also play critical roles in the formation of strictures. Dretler and Young [35] found that “stone granulomas” caused by fragments of calculi embedded in the ureteral mucosa play an important role in the development of ureteral strictures. In the stone granuloma, macrophages and foreign body giant cells were found around embedded calcium oxalate crystal. Surrounding inflammation and fibrosis were also observed.
Postoperative scarring is usually caused by direct injury to the ureter during electrocoagulation, laser coagulation or resection. Although the tissue penetration of the Ho:YAG laser is only 0.4 mm, there remains a risk of stricture from scarring of the ureter. According to previous reports, the incidence of ureteral stricture ranged from 8.57% to 13.67% in patients who underwent endoscopic treatment of upper tract neoplasm by Ho:YAG laser [36], [37], [38]. The high incidence of ureteral stricture in these studies confirmed the relationship between stricture formation and the thermal effect of the Ho:YAG laser. According to a series studies, 55 of 1310 patients using Ho:YAG laser developed ureteral strictures with a 4.20% stricture rate. However, 14 of 1226 patients using pneumatic lithotripsy developed strictures with a stricture rate of 1.14% [4], [10], [12], [13], [39]. Thus, the Ho:YAG laser may have a higher incidence of postoperative ureteral stricture compared with the pneumatic lithotripter in the treatment of ureteral stones. Therefore, the thermal effect of Holmium lasers on ureteral mucosal injury should not be overlooked.
6. Diagnosis
Early diagnosis of postoperative ureteral stricture is important for the preservation of renal function. Routine postoperative radiographic imaging is recommended to detect silent ureteral obstructions. The incidence of postoperative ureteral stricture decreased dramatically with the evolution of ureteroscopy. Therefore, some urologists questioned the need for routine postoperative imaging after URL. In a retrospective study, Karod et al. [40] evaluated the necessity for radiologic evaluation after ureteroscopy by conducting routine radiologic follow-up in 189 patients undergoing ureteroscopy. In their series, 110 patients were asymptomatic after ureteroscopy at a median of 60 days follow-up. None of the asymptomatic patients exhibited ureteral obstruction on radiologic follow-up. In the 21 patients with flank pain, 13 patients were found to have ureteral obstruction on radiologic follow-up. Therefore, these authors suggested that routine postoperative imaging for the detection of obstruction is unnecessary for asymptomatic patients. However, another study by Weizer et al. [9] showed that silent ureteral obstruction developed in 2.9% of patients (7/241) at a mean of 5.4 months of follow-up. One of these patients required life-long hemodialysis for renal failure. Therefore, the authors advocated a routine 3-month postoperative radiographic surveillance for all patients to avoid the adverse effect of silent obstruction. Another retrospective study revealed that the negative and positive predictive values of pain for predicting obstruction were 83% and 75%, respectively [41]. A recent study showed that the incidences of symptomatic and asymptomatic obstruction following URL were 0.15% and 0.46%, respectively [5]. Therefore, a lack of symptoms is not a sufficient criterion to omit postoperative imaging given that the consequence of undiagnosed obstruction is very serious.
In addition to symptomatic patients, imaging follow-up should be conducted in complicated cases. Beiko et al. [39] evaluated the indications for upper tract imaging after ureteroscopic procedure. These authors concluded that routine radiographic surveillance should be conducted in patients with impacted stones, intraoperative ureteral injury, pre-existing renal function impairment, endoscopic evidence of stricture and postoperative flank pain or fever. El-Abd et al. [5] reported that intraoperative perforation and impacted stones of >2 cm were the highest risk factors for ureteral stricture. In their 12 patients with postoperative ureteral stricture, three were diagnosed at 13 months and one at 18 months after treatment. Therefore, these authors recommended that radiological follow-up should extend to 18 months in patients with intraoperative ureteric injury and in those with large impacted stones in the proximal ureter.
7. Preventive strategies
Prior to the interventions for upper urinary tract diseases, a comprehensive evaluation should be conducted that includes the history of treatments and imaging examinations. This evaluation should be performed to identify the patients with stricture-related high risk factors, such as impacted stones, former iatrogenic injuries, infection, and multiple lesions. For impacted stones, endoscopic and intraluminal sonographic technology can be used to identify submucosal calculi [42]. In addition, the incidence of ureteral injury can be largely decreased by preoperative Double-J stenting [27]. However, at present, preoperative assessments are not frequently recommended, and further prospective studies are required to clarify their utility.
Some practices are helpful for the prevention of ureteral lesions and subsequent stricture formation during ureteroscopic procedures. Firstly, a small rigid ureteroscope is useful. Compared with 8.5–11.5 Fr semi-rigid ureteroscope, the 4.5–6.5 Fr scope was associated with less mucosal injury (1.9% and 13.5%, p = 0.027) [43]. The need for active or passive dilation could be avoided with a 4.5 Fr ureteroscope, even in difficult-to-access ureters that cannot be accessed using conventional ureteroscopes [44]. Secondly, fluoroscopic imaging is mandatory in some challenging cases of URL. It is a longstanding principle that URL should be performed under fluoroscopic guidance. Recently, with the development of new instruments, some urologists omit fluoroscopy in the treatment of uncomplicated upper urinary stones [45], [46], [47]. However, in certain difficult circumstances, such as anatomic abnormalities and kinked ureters caused by impacted ureteral stones, fluoroscopic guidance is important to avoid ureteral lesion [45]. Thirdly, meticulous technique and patience also play important roles in minimizing the risk of ureteral injury. Introducing a guide wire or a ureteroscope with poor visualization can lead to submucosal passage or ureteral perforation.
It is important to minimize the risk of stone granuloma formation. It has been reported that calcium oxalate particles embedded in the ureteral wall may lead to a subsequent granulomatous response and stricture disease [35]. Great care should be taken to prevent the displacement of stone fragments into the ureteral wall. Firstly, the laser fiber tip should be maintained centrally on the stone to avoid thermal injury to the ureteral mucosa [48]. Secondly, in situ lithotripsy should be avoided if the stone fragments are attached to the ureteral wall. The edematous tissue surrounding the impacted stone is so fragile that the shockwave effect of the Holmium laser can push the stone fragments into ureteral wall. It is advisable to strip out the fragments from ureteral wall with a laser fiber, guide wire or the tip of the ureteroscope. Thirdly, if the working space is limited due to significant mucosal edema or polyps, it is recommended to transfer the fragments proximally to minimize the risk of ureteral injury [35]. Last but not least, the stone fragments should be kept away from the site of impaction and ureteral lesions by irrigation, thereby avoiding a subsequent inflammatory reaction.
8. Conclusion
With recent advances in ureteroscopic technology, the incidence of ureteral stricture has notably decreased. However, this complication cannot be overlooked because of its great danger to patients. Appropriate imaging examinations and renal function evaluation are necessary before a therapeutic schedule is decided upon. Preventive measures should be taken to reduce the occurrence of ureteral stricture, and regular follow-ups should be performed after ureteroscopy, thereby allowing for a timely intervention if a stricture is detected.
Conflicts of interest
The authors declare no conflict of interest.
Footnotes
Peer review under responsibility of Second Military Medical University.
References
- 1.Oberlin D.T., Flum A.S., Bachrach L., Matulewicz R.S., Flury S.C. Contemporary surgical trends in the management of upper tract calculi. J Urol. 2015;193:880–884. doi: 10.1016/j.juro.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Tepeler A., Resorlu B., Sahin T., Sarikaya S., Bayindir M., Oguz U. Categorization of intraoperative ureteroscopy complications using modified Satava classification system. World J Urol. 2014;32:131–136. doi: 10.1007/s00345-013-1054-y. [DOI] [PubMed] [Google Scholar]
- 3.de la Rosette J., Denstedt J., Geavlete P., Keeley F., Matsuda T., Pearle M. The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol. 2014;28:131–139. doi: 10.1089/end.2013.0436. [DOI] [PubMed] [Google Scholar]
- 4.Chen S., Zhou L., Wei T., Luo D., Jin T., Li H. Comparison of holmium: YAG laser and pneumatic lithotripsy in the treatment of ureteral stones: an update meta-analysis. Urol Int. 2017;98:125–133. doi: 10.1159/000448692. [DOI] [PubMed] [Google Scholar]
- 5.El-Abd A.S., Suliman M.G., Abo Farha M.O., Ramadan A.R., El-Tatawy H.H., El-Gamal O.M. The development of ureteric strictures after ureteroscopic treatment for ureteric calculi: a long-term study at two academic centres. Arab J Urol. 2014;12:168–172. doi: 10.1016/j.aju.2013.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elashry O.M., Elgamasy A.K., Sabaa M.A., Abo-Elenien M., Omar M.A., Eltatawy H.H. Ureteroscopic management of lower ureteric calculi: a 15-year single-centre experience. BJU Int. 2008;102:1010–1017. doi: 10.1111/j.1464-410X.2008.07747.x. [DOI] [PubMed] [Google Scholar]
- 7.Kilinc M.F., Doluoglu O.G., Karakan T., Dalkilic A., Sonmez N.C., Yuceturk C.N. The effect of ureteroscope size in the treatment of ureteral stone: 15-year experience of an endoscopist. Turk J Urol. 2016;42:64–69. doi: 10.5152/tud.2016.84594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Roberts W.W., Cadeddu J.A., Micali S., Kavoussi L.R., Moore R.G. Ureteral stricture formation after removal of impacted calculi. J Urol. 1998;159:723–726. [PubMed] [Google Scholar]
- 9.Weizer A.Z., Auge B.K., Silverstein A.D., Delvecchio F.C., Brizuela R.M., Dahm P. Routine postoperative imaging is important after ureteroscopic stone manipulation. J Urol. 2002;168:46–50. [PubMed] [Google Scholar]
- 10.Brito A.H., Mitre A.I., Srougi M. Ureteroscopic pneumatic lithotripsy of impacted ureteral calculi. Int Braz J Urol. 2006;32:295–299. doi: 10.1590/s1677-55382006000300006. [DOI] [PubMed] [Google Scholar]
- 11.Adiyat K.T., Meuleners R., Monga M. Selective postoperative imaging after ureteroscopy. Urology. 2009;73:490–493. doi: 10.1016/j.urology.2008.09.064. [discussion 493] [DOI] [PubMed] [Google Scholar]
- 12.Binbay M., Tepeler A., Singh A., Akman T., Tekinaslan E., Sarilar O. Evaluation of pneumatic versus holmium:YAG laser lithotripsy for impacted ureteral stones. Int Urol Nephrol. 2011;43:989–995. doi: 10.1007/s11255-011-9951-8. [DOI] [PubMed] [Google Scholar]
- 13.Li L., Pan Y., Weng Z., Bao W., Yu Z., Wang F. A prospective randomized trial comparing pneumatic lithotripsy and holmium laser for management of middle and distal ureteral calculi. J Endourol. 2015;29:883–887. doi: 10.1089/end.2014.0856. [DOI] [PubMed] [Google Scholar]
- 14.Fam X.I., Singam P., Ho C.C., Sridharan R., Hod R., Bahadzor B. Ureteral stricture formation after ureteroscope treatment of impacted calculi: a prospective study. Korean J Urol. 2015;56:63–67. doi: 10.4111/kju.2015.56.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xi Q., Wang S., Ye Z., Liu J. Combined removal of stones with resection of concurrent pathologic ureter may be a preferred treatment for impacted ureteral stones with stricture lesions. J Endourol. 2009;23:243–247. doi: 10.1089/end.2008.0507. [DOI] [PubMed] [Google Scholar]
- 16.Perez Castro E., Osther P.J., Jinga V., Razvi H., Stravodimos K.G., Parikh K. Differences in ureteroscopic stone treatment and outcomes for distal, mid-, proximal, or multiple ureteral locations: the Clinical Research Office of the Endourological Society ureteroscopy global study. Eur Urol. 2014;66:102–109. doi: 10.1016/j.eururo.2014.01.011. [DOI] [PubMed] [Google Scholar]
- 17.Schuster T.G., Hollenbeck B.K., Faerber G.J., Wolf J.S., Jr. Complications of ureteroscopy: analysis of predictive factors. J Urol. 2001;166:538–540. doi: 10.1016/s0022-5347(05)65978-2. [DOI] [PubMed] [Google Scholar]
- 18.El-Nahas A.R., El-Tabey N.A., Eraky I., Shoma A.M., El-Hefnawy A.S., El-Assmy A.M. Semirigid ureteroscopy for ureteral stones: a multivariate analysis of unfavorable results. J Urol. 2009;181:1158–1162. doi: 10.1016/j.juro.2008.10.167. [DOI] [PubMed] [Google Scholar]
- 19.Breda A., Territo A., Lopez-Martinez J.M. Benefits and risks of ureteral access sheaths for retrograde renal access. Curr Opin Urol. 2016;26:70–75. doi: 10.1097/MOU.0000000000000233. [DOI] [PubMed] [Google Scholar]
- 20.De S., Sarkissian C., Torricelli F.C., Brown R., Monga M. New ureteral access sheaths: a double standard. Urology. 2015;85:757–763. doi: 10.1016/j.urology.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Torricelli F.C., De S., Hinck B., Noble M., Monga M. Flexible ureteroscopy with a ureteral access sheath: when to stent? Urology. 2014;83:278–281. doi: 10.1016/j.urology.2013.10.002. [DOI] [PubMed] [Google Scholar]
- 22.Kaplan A.G., Lipkin M.E., Scales C.D., Jr., Preminger G.M. Use of ureteral access sheaths in ureteroscopy. Nat Rev Urol. 2016;13:135–140. doi: 10.1038/nrurol.2015.271. [DOI] [PubMed] [Google Scholar]
- 23.Lallas C.D., Auge B.K., Raj G.V., Santa-Cruz R., Madden J.F., Preminger G.M. Laser Doppler flowmetric determination of ureteral blood flow after ureteral access sheath placement. J Endourol. 2002;16:583–590. doi: 10.1089/089277902320913288. [DOI] [PubMed] [Google Scholar]
- 24.Delvecchio F.C., Auge B.K., Brizuela R.M., Weizer A.Z., Silverstein A.D., Lallas C.D. Assessment of stricture formation with the ureteral access sheath. Urology. 2003;61:518–522. doi: 10.1016/s0090-4295(02)02433-0. [DOI] [PubMed] [Google Scholar]
- 25.Abdel-Razzak O.M., Bagley D.H. Clinical experience with flexible ureteropyeloscopy. J Urol. 1992;148:1788–1792. doi: 10.1016/s0022-5347(17)37030-1. [DOI] [PubMed] [Google Scholar]
- 26.Wang H.H., Huang L., Routh J.C., Kokorowski P., Cilento B.G., Jr., Nelson C.P. Use of the ureteral access sheath during ureteroscopy in children. J Urol. 2011;186(4 Suppl.):1728–1733. doi: 10.1016/j.juro.2011.03.072. [DOI] [PubMed] [Google Scholar]
- 27.Traxer O., Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal surgery. J Urol. 2013;189:580–584. doi: 10.1016/j.juro.2012.08.197. [DOI] [PubMed] [Google Scholar]
- 28.Kawahara T., Ito H., Terao H., Kakizoe M., Kato Y., Uemura H. Early ureteral catheter removal after ureteroscopic lithotripsy using ureteral access sheath. Urolithiasis. 2013;41:31–35. doi: 10.1007/s00240-012-0518-7. [DOI] [PubMed] [Google Scholar]
- 29.Francesca F., Scattoni V., Nava L., Pompa P., Grasso M., Rigatti P. Failures and complications of transurethral ureteroscopy in 297 cases: conventional rigid instruments vs. small caliber semirigid ureteroscopes. Eur Urol. 1995;28:112–115. doi: 10.1159/000475032. [DOI] [PubMed] [Google Scholar]
- 30.Yaycioglu O., Guvel S., Kilinc F., Egilmez T., Ozkardes H. Results with 7.5F versus 10F rigid ureteroscopes in treatment of ureteral calculi. Urology. 2004;64:643–646. doi: 10.1016/j.urology.2004.05.050. [discussion 646–647] [DOI] [PubMed] [Google Scholar]
- 31.Sugihara T., Yasunaga H., Horiguchi H., Nishimatsu H., Kume H., Ohe K. A nomogram predicting severe adverse events after ureteroscopic lithotripsy: 12 372 patients in a Japanese national series. BJU Int. 2013;111:459–466. doi: 10.1111/j.1464-410X.2012.11594.x. [DOI] [PubMed] [Google Scholar]
- 32.Yamaguchi K., Minei S., Yamazaki T., Kaya H., Okada K. Characterization of ureteral lesions associated with impacted stones. Int J Urol. 1999;6:281–285. doi: 10.1046/j.1442-2042.1999.00067.x. [DOI] [PubMed] [Google Scholar]
- 33.Mugiya S., Ito T., Maruyama S., Hadano S., Nagae H. Endoscopic features of impacted ureteral stones. J Urol. 2004;171:89–91. doi: 10.1097/01.ju.0000100960.08768.81. [DOI] [PubMed] [Google Scholar]
- 34.Mitchinson M.J., Bird D.R. Urinary leakage and retroperitoneal fibrosis. J Urol. 1971;105:56–58. doi: 10.1016/s0022-5347(17)61458-7. [DOI] [PubMed] [Google Scholar]
- 35.Dretler S.P., Young R.H. Stone granuloma: a cause of ureteral stricture. J Urol. 1993;150:1800–1802. doi: 10.1016/s0022-5347(17)35899-8. [DOI] [PubMed] [Google Scholar]
- 36.Suh R.S., Faerber G.J., Wolf J.S., Jr. Predictive factors for applicability and success with endoscopic treatment of upper tract urothelial carcinoma. J Urol. 2003;170:2209–2216. doi: 10.1097/01.ju.0000097327.20188.c1. [DOI] [PubMed] [Google Scholar]
- 37.Chen G.L., Bagley D.H. Ureteroscopic surgery for upper tract transitional-cell carcinoma: complications and management. J Endourol. 2001;15:399–404. doi: 10.1089/089277901300189420. [discussion 409] [DOI] [PubMed] [Google Scholar]
- 38.Johnson G.B., Fraiman M., Grasso M. Broadening experience with the retrograde endoscopic management of upper urinary tract urothelial malignancies. BJU Int. 2005;95(Suppl. 2):110–113. doi: 10.1111/j.1464-410x.2005.05210.x. [DOI] [PubMed] [Google Scholar]
- 39.Beiko D.T., Beasley K.A., Koka P.K., Watterson J.D., Nott L., Denstedt J.D. Upper tract imaging after ureteroscopic holmium:YAG laser lithotripsy: when is it necessary? Can J Urol. 2003;10:2062–2067. [PubMed] [Google Scholar]
- 40.Karod J.W., Danella J., Mowad J.J. Routine radiologic surveillance for obstruction is not required in asymptomatic patients after ureteroscopy. J Endourol. 1999;13:433–436. doi: 10.1089/end.1999.13.433. [DOI] [PubMed] [Google Scholar]
- 41.Bugg C.E., Jr., El-Galley R., Kenney P.J., Burns J.R. Follow-up functional radiographic studies are not mandatory for all patients after ureteroscopy. Urology. 2002;59:662–667. doi: 10.1016/s0090-4295(02)01508-x. [DOI] [PubMed] [Google Scholar]
- 42.Grasso M., Liu J.B., Goldberg B., Bagley D.H. Submucosal calculi: endoscopic and intraluminal sonographic diagnosis and treatment options. J Urol. 1995;153:1384–1389. doi: 10.1016/s0022-5347(01)67409-3. [DOI] [PubMed] [Google Scholar]
- 43.Atis G., Arikan O., Gurbuz C., Yildirim A., Erol B., Pelit S. Comparison of different ureteroscope sizes in treating ureteral calculi in adult patients. Urology. 2013;82:1231–1235. doi: 10.1016/j.urology.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 44.Soylemez H., Yildirim K., Utangac M.M., Aydogan T.B., Ezer M., Atar M. A new alternative for difficult ureter in adult patients: No need to dilate ureter via a balloon or a stent with the aid of 4.5F semirigid ureteroscope. J Endourol. 2016;30:650–654. doi: 10.1089/end.2016.0118. [DOI] [PubMed] [Google Scholar]
- 45.Tepeler A., Armagan A., Akman T., Silay M.S., Akcay M., Basibuyuk I. Is fluoroscopic imaging mandatory for endoscopic treatment of ureteral stones? Urology. 2012;80:1002–1006. doi: 10.1016/j.urology.2012.02.082. [DOI] [PubMed] [Google Scholar]
- 46.Mandhani A., Chaudhury H., Gupta N., Singh H.K., Kapoor R., Kumar A. Is fluoroscopy essential for retrieval of lower ureteric stones? Urol Int. 2007;78:70–72. doi: 10.1159/000096938. [DOI] [PubMed] [Google Scholar]
- 47.Peng Y., Xu B., Zhang W., Li L., Liu M., Gao X. Retrograde intrarenal surgery for the treatment of renal stones: is fluoroscopy-free technique achievable? Urolithiasis. 2015;43:265–270. doi: 10.1007/s00240-015-0760-x. [DOI] [PubMed] [Google Scholar]
- 48.Giusti G., Proietti S., Villa L., Cloutier J., Rosso M., Gadda G.M. Current standard technique for modern flexible ureteroscopy: tips and tricks. Eur Urol. 2016;70:188–194. doi: 10.1016/j.eururo.2016.03.035. [DOI] [PubMed] [Google Scholar]