Abstract
Introduction
We examined trends in seven mutually exclusive tobacco product use patterns (T-PUPs) in nationally representative samples of U.S. youth over time and age.
Methods
We used time varying effect modeling on National Youth Tobacco Surveys, 1999–2014 (N = 38662, 9–17 years, M = 15.02). Regression coefficients were estimated as a non-parametric function of time. T-PUPs were cigarette only, non-cigarette combustible only, noncombustible only, non-cigarette combustible and noncombustible dual, cigarette and noncombustible dual, cigarette and non-cigarette combustible dual, and POLY (i.e. cigarettes, non-cigarette combustibles, and noncombustibles) use.
Results
Among youth tobacco users, cigarette only use was the predominant T-PUP from 1999 to 2010. After 2010 and 2013, non-cigarette combustible only (AOR 1.38, CI = 1.02–1.87) and noncombustible only (AOR 1.57, CI = 1.00–2.45) use became more prevalent than cigarette only use. In 2011, dual and POLY T-PUPs were on the rise although not significantly different from cigarette only use.
Cigarette only use was the predominant T-PUP among 11- to 17-year-old tobacco users. Non-cigarette combustible only (AOR 0.14, CI = 0.10–0.19), noncombustible only (AOR 0.01, CI = 0.008–0.02), non-cigarette combustible and noncombustible (AOR 0.01, CI = 0.01–0.03), cigarette and noncombustible (AOR 0.02, CI = 0.01–0.04), cigarette and non-cigarette combustible (AOR 0.32, CI = 0.24–0.43), and POLY (AOR 0.02, CI = 0.01–0.04) use were less prevalent than cigarette only use at age 17.
Conclusions
Non-cigarette, dual, and POLY T-PUPs are rising among youth tobacco users. Screening for all tobacco use and delivering treatment during pediatrician visits should be standard clinical practice.
Implications
Tracking trends in tobacco product use patterns (T-PUPs) over time and age is necessary to achieve Healthy People 2020 goal of reducing tobacco use among youth. Trends over time show a rise of non-cigarette T-PUPs especially noncombustible products but cigarette only use remains the most prevalent among 11- to 17-year-old tobacco users. The recent extension of FDA’s regulatory jurisdiction over all tobacco products (e.g. e-cigarettes, hookah) is a step toward comprehensive tobacco control especially among youth. Public health practitioners should extend prevention and cessation efforts among youth to T-PUPs beyond exclusive cigarette smoking.
Introduction
Reducing tobacco use among youth is an objective of Healthy People 2020.1 Defined as tobacco-containing products made for human consumption,2 tobacco products were largely exempt from health regulations prior to 2009 unless health claims were made.3 The Food and Drug Administration (FDA) has regulated cigarettes, roll-your-own cigarettes, and smokeless tobacco since 2009 under the Family Smoking Prevention and Tobacco Control Act.3 FDA’s authority extended to all tobacco products (i.e. cigarettes, all cigars, pipe tobacco, e-cigarettes, hookah, dissolvable tobacco, smokeless tobacco, roll-your-own, and any other products that meet the definition of a tobacco product under the Tobacco Control Act) in 2016.3
Sensitivity to low levels of nicotine puts youth at higher risk of nicotine dependency, heavy and continued cigarette use into adulthood compared to adults.4,5 Youth who use non-cigarette tobacco products exhibit similar levels of nicotine dependence as cigarette smokers.6 Further, youth who use multiple tobacco products are at greater risks of nicotine dependency and detrimental health and social outcomes compared to users of single tobacco products.7
National surveillance data show that youth cigarette smoking has declined. Among U.S. 8th, 10th, and 12th graders, past 30-day cigarette use dropped from 20.7% in 1991 to 7.0% in 2015.8 However, any tobacco use climbed from 20.4% in 20129 to 24.6% in 201410 among high-school students, which could be attributed to use of non-cigarette combustible and noncombustible tobacco products. Among U.S. youth, use of large cigars was at 4.2%, flavored little cigars at 7.1%, regular little cigars at 4.9%, smokeless tobacco at 4.7%, and e-cigarettes at 13.2% in 2015.8 In 2014, use of any two or more tobacco products was at 3.1% and 12.7% among U.S. middle- and high-school students, respectively.11
Much is known about trends in youth cigarette use and age of onset.12 Conversely, little is known about trends in non-cigarette tobacco products, dual, and polytobacco use. Additionally, no study to date has identified ages at which youth adopt these use patterns. This is due to limitations in current literature on youth tobacco use. Typically, studies have focused on single tobacco products (e.g. water pipe)13 or inconsistently defined dual and polytobacco use. For example, Arrazola and colleagues combined dual and polytobacco use into one broad pattern of two or more tobacco products use.11 Conversely, Lee and colleagues identified fine-grained dual and polytobacco patterns that reflected 11 different combinations of tobacco products use (e.g. hookah and cigarettes, two noncombustible products, three or more products).14
To capture the totality of youth tobacco use, El-Toukhy and Choi proposed a new classification of tobacco product use patterns (T-PUPs) based on number (i.e. single, dual, polytobacco) and categories (i.e., cigarette, non-cigarette combustible, noncombustible) of tobacco products used.15 The underlying premise of the T-PUPs model is to group users of tobacco product(s) that share a similar nicotine delivery mechanism. The seven T-PUPs are cigarettes only use, non-cigarette combustibles only use, noncombustibles only use, non-cigarette combustibles and noncombustibles dual use, cigarettes and noncombustibles dual use, cigarettes and non-cigarette combustibles dual use, and POLY use (i.e. cigarettes, non-cigarette combustibles, noncombustibles). Cigarettes, although a combustible product, are a separate category because of their differential consumption rates16,17 and associated health risks18 than non-cigarette combustible products. Non-cigarette combustibles include cigars, cigarillos, little cigars, pipe, roll-your-own cigarettes, bidis, clove cigarettes, and hookah whereas noncombustibles include chewing tobacco, snuff, dip, snus, dissolvable tobacco, and e-cigarettes. Applying T-PUPs model to the 2012 National Youth Tobacco Survey (NYTS), we found that users who adopted certain T-PUPs differed in their demographic profile (e.g. gender, race, and ethnicity), and exposure and receptivity to pro-tobacco marketing.15
This paper aimed to examine the extent to which the prevalence of T-PUPs varied over time (1999–2014) and age (9–17 years old) among U.S. youth. We extend the literature in several ways. First, by examining seven mutually exclusive T-PUPs, we overcome limitations of existing literature, which excludes certain use patterns (e.g. exclusive non-cigarette use) and/or inconsistently classifies dual and polytobacco use.9,14 Second, by examining trends in T-PUPs from 1999 to 2014, we extend literature on non-cigarette tobacco products, which have documented use of non-cigarette products only in recent years. Third, by examining use patterns over age, we fill gaps in literature on age of use of non-cigarette tobacco products, dual, and polytobacco use. Finally, by examining all T-PUPs, we provide a comparative angle over time and age rather than examining individual T-PUPs in isolation.
Methods
Data Source
Initiated in 1999, NYTS is a multi-stage sample, self-administered, cross-sectional, nationally representative survey of tobacco knowledge, attitudes, and use among U.S. middle- and high-school students. A complete description of NYTS sampling procedures is available online.19 We used all available NYTS datasets from 1999 to 2014: 1999, 2000, 2002, 2004, 2006, 2009, 2011, 2012, 2013, and 2014.
We limited our analyses to 17 years old or younger tobacco users who reported any tobacco use in the past 30 days (N = 38662) despite being prohibited by law to purchase tobacco products until age 18.3,20,21 Sample size for individual survey years ranged from 2737 (in 2011) to 7667 (in 2000). Overall response rates ranged from 68.4% (in 2013) to 84.8% (in 2009). The study is a secondary data analysis on de-identified data, which is exempt from Institutional Review Board.
Measures
Past 30-day use of tobacco products was assessed (i.e. “During the past 30 days, on how many days did you use [tobacco product]?” or “During the past 30 days, have you used [tobacco product] on at least one day?”). We classified users into one T-PUP if they reported use of any product from a parent category for at least one day and no products from other parent categories based on all tobacco products assessed in any given survey year. T-PUPs were: cigarette only use, non-cigarette combustible only use (i.e. cigars, cigarillos, little cigars, pipe, roll-your-own cigarettes, bidis, clove cigarettes, hookah, water pipe), noncombustible only use (i.e. chewing tobacco, snuff, dip, snus, dissolvable tobacco, e-cigarettes), non-cigarette combustible and noncombustible dual use, cigarette and noncombustible dual use, cigarette and non-cigarette combustible dual use, and POLY use.15 We include e-cigarettes because they are regulated in the U.S. as a product that meets the definition of a tobacco product under the Tobacco Control Act.3 Use questions for all aforementioned products consistently appeared in NYTS from 1999 to 2014 except for roll-your-own cigarettes, hookah, snus, dissolvable tobacco, and e-cigarettes that were absent in 1999 to 2009 and roll-your-own cigarettes and clove cigarettes that were absent in 2014. Noteworthy is that dissolvable tobacco was introduced to the US market in 2001,22 whereas e-cigarettes23 and snus24 were introduced in 2006.
To illustrate our classification of users into T-PUPs, participants were (1) cigarette only users if they reported use of cigarettes, but no use of any non-cigarette combustibles or noncombustibles; (2) non-cigarette combustible exclusive users if they reported use of hookah, a non-cigarette combustible, but no use of cigarettes or any noncombustibles; (3) non-cigarette combustible and noncombustible dual users if they reported use of little cigars, a non-cigarette combustible, and e-cigarettes, a noncombustible, but no use of cigarettes; and (4) POLY users if they reported use of roll-your-own cigarettes, a non-cigarette combustible, e-cigarettes, a noncombustible, and cigarettes.
Information on gender, grade (middle school/high school), race and ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, non-Hispanic Asian, non-Hispanic other), and living with cigarette user (yes/no) were collected. Non-Hispanic other included American Indians, Alaska Natives, Native Hawaiians, and Pacific Islanders. Exposure to internet (“When you are using the internet, how often do you see ads for tobacco products?”) and in-store (“When you go to a convenience store, supermarket, or gas station, how often do you see ads for cigarettes and other tobacco products or items that have tobacco company names or pictures on them?”) tobacco advertising were dichotomized into “no” for responses “I don’t use the internet/ I never go to a convenience store, supermarket, or gas station” and “never see ads” and “yes” for responses “hardly ever or rarely see ads”, “most of the time”, “some of the time”, and “always”.
Data Analyses
Using SAS® version 9.3 (SAS Institute, Cary: NC), we conducted time varying effect modeling (TVEM)25 to examine prevalence of T-PUPs over two time metrics (i.e. chronological time and age). Chronological time reflects year of data collection (e.g. 1999) whereas age reflects age of participant captured by the question “how old are you?” TVEM is an extension of linear regression models where regression coefficients are estimated as a smooth function of time without prior assumptions regarding the shape of the relationship between variables. TVEM results are plotted in figures with 95% confidence intervals. Because TVEM produces an infinite number of data points, we highlight the highest or lowest points of TVEM irregular curves in the results section to represent model-estimated prevalence and adjusted odds ratios. However, the highest/lowest points of a TVEM curve reflect traditional time-invariant regression coefficients whereas the TVEM curve in its entirety reflects time-varying modeling of the outcome.
First, we estimated intercept-only models for each T-PUP where t-pup is tobacco product use pattern (e.g. non-cigarette combustible only use) and is the log odds of T-PUP at a given time (t).
Second, we examined the log odds of each T-PUP (slope function) compared to cigarette only use as a reference (coded 0). We used cigarette only use as the reference group because cigarettes are the most consumed tobacco product16 and are used by researchers and consumers as a reference for assessing perceived harmfulness of non-cigarette tobacco products.26,27 We adjusted for gender, grade, race and ethnicity, living with a cigarette user, and exposure to tobacco advertising on the internet and in stores. We specified these covariates as time-varying because their prevalence and/or associations with the outcome variable could vary over time. For example, self-reported exposure to tobacco advertising on the internet among youth in grades 6 through 12 increased from 2000 to 2004;28 point-of-sale expenditure ranged from $329.4 million in 199929 to $238.2 million in 2014 for cigarettes;30 use of tobacco products fluctuated over time;8–10 and T-PUPs users vary by race/ethnicity and gender.15 We included survey year as a covariate when examining T-PUPs over age. TVEM automatically excludes observations with missing data for the outcome or covariates. In our analyses, no missing data were present in the intercept-only models whereas missing data ranged from 6.8% to 7.7% in the T-PUPs log odds models.
Results
Weighted sample characteristics appear in Table 1. The sample was 57.7% male; 64.3% non-Hispanic White, 12.5% non-Hispanic Black, 19.7% Hispanic, 1.5% non-Hispanic Asian, and 1.7% non-Hispanic other; and 73.3% high-school students. Mean age was 15.02 years.
Table 1.
Weighted Sample Characteristics
| Year | 1999 (n = 3313) | 2000 (n = 7667) | 2002 (n = 4457) | 2004 (n = 4483) | 2006 (n = 3933) | 2009 (n = 3257) | 2011 (n = 2737) | 2012 (n = 3202) | 2013 (n = 2453) | 2014 (n = 3160) |
|---|---|---|---|---|---|---|---|---|---|---|
| % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | % (95% CI) | |
| Gender | ||||||||||
| Female | 45.5 (43.1–47.9) | 43.1 (41.4–44.8) | 43.8 (41.7–46.0) | 46.7 (44.6–48.8) | 44.2 (41.5–46.9) | 39.1 (36.4–41.7) | 38.7 (36.2–41.2) | 39.2 (36.9–41.5) | 41.3 (38.3–44.3) | 43.4 (40.6–46.1) |
| Male | 54.4 (52.0–56.8) | 56.8 (55.1–58.5) | 56.1 (53.9–58.2) | 53.2 (51.1–55.3) | 55.7 (53.0–58.4) | 60.8 (58.2–63.5) | 61.2 (58.7–63.7) | 60.7 (58.4–63.0) | 58.6 (55.6–61.6) | 56.5 (53.8–59.3) |
| Age* | 14.80 (14.74–14.86) | 15.05 (15.02–15.09) | 14.90 (14.85–14.95) | 14.83 (14.78–14.87) | 15.01 (14.96–15.06) | 15.21 (15.15–15.27) | 14.99 (14.93–15.06) | 15.24 (15.18–15.29) | 15.23 (15.16–15.30) | 15.11 (15.05–15.17) |
| Race/Ethnicity | ||||||||||
| Non-Hispanic White | 66.1 (60.4–71.8) | 69.7 (65.1–74.3) | 69.3 (65.1–73.5) | 71.8 (67.6–76.1) | 71.7 (66.9–76.5) | 64.2 (56.0–72.4) | 60.7 (54.6–66.8) | 58.2 (53.1–63.3) | 56.5 (49.8–63.2) | 58.8 (53.0–64.6) |
| Non-Hispanic Black | 15.2 (10.0–20.5) | 14.2 (10.7–17.6) | 12.5 (10.0–15.0) | 11.6 (9.0–14.3) | 10.9 (7.4–14.4) | 10.6 (7.8–13.4) | 13.6 (10.3–16.8) | 14.5 (10.1–18.9) | 15.2 (11.1–19.4) | 11.8 (8.4–15.3) |
| Hispanic | 14.7 (11.9–17.4) | 11.5 (8.8–14.2) | 13.1 (10.4–15.7) | 13.7 (10.2–17.1) | 14.5 (11.3–17.7) | 21.5 (14.8–28.1) | 22.8 (17.4–28.2) | 24.3 (20.2–28.5) | 24.8 (19.3–30.2) | 26.1 (21.2–31.1) |
| Non-Hispanic Asian | 1.5 (0.8–2.2) | 1.8 (1.3–2.3) | 1.7 (1.1–2.3) | 1.4 (0.9–1.9) | 1.1 (0.6–1.5) | 1.6 (0.9–2.4) | 1.2 (0.6–1.7) | 1.4 (0.6–2.2) | 1.8 (1.0–2.7) | 1.8 (1.1–2.5) |
| Non-Hispanic Other | 2.3 (1.7–3.0) | 2.6 (1.8–3.4) | 3.2 (2.5–3.8) | 1.3 (0.9–1.6) | 1.6 (1.0–2.1) | 1.8 (1.3–2.4) | 1.5 (0.8–2.3) | 1.3 (1.0–1.7) | 1.4 (0.9–1.9) | 1.1 (0.8–1.5) |
| School | ||||||||||
| Middle School | 25.5 (20.3–30.7) | 31.4 (27.5–35.3) | 33.5 (27.9–39.1) | 31.6 (26.9–36.3) | 27.6 (22.4–32.8) | 24.2 (18.9–29.5) | 24.1 (19.6–28.7) | 22.9 (19.4–26.5) | 22.7 (18.6–26.7) | 23.6 (18.4–28.8) |
| High School | 74.4 (69.2–79.6) | 68.5 (64.6–72.4) | 66.4 (60.8–72.0) | 68.3 (63.6–73.0) | 72.3 (67.1–77.5) | 75.7 (70.4–81.0) | 75.8 (71.2–80.3) | 77.0 (73.4–80.5) | 77.2 (73.2–81.3) | 76.3 (71.1–81.5) |
| Living with cigarette user | ||||||||||
| No | 40.0 (36.8–43.1) | 42.2 (39.9–44.5) | 41.1 (38.7–43.5) | 41.9 (38.9–44.9) | 42.1 (38.9–45.3) | 46.9 (43.2–50.6) | 51.0 (47.8–54.1) | 53.6 (50.5–56.6) | 53.0 (49.2–56.8) | 57.0 (53.4–60.7) |
| Yes | 59.6 (56.8–63.1 | 57.7 (55.4–60.0) | 58.8 (56.4–61.2) | 58.0 (55.0–61.0) | 57.8 (54.6–61.0) | 53.0 (49.3–56.7) | 48.9 (45.8–52.1) | 46.3 (43.3–49.4) | 46.9 (43.1–50.7) | 42.9 (39.2–46.5) |
| Exposure to internet ads | ||||||||||
| No | 53.1 (51.2–55.0) | 43.0 (41.2–44.9) | 31.5 (29.4–33.5) | 28.5 (26.6–30.5) | 25.4 (23.8–27.0) | 21.4 (19.5–23.4) | 22.9 (20.7–25.0) | 19.5 (17.8–21.3) | 21.7 (19.3–24.0) | 16.9 (14.8–19.0) |
| Yes | 46.8 (44.9–48.7) | 56.9 (55.0–58.7) | 68.4 (66.4–70.5) | 71.4 (69.4–73.3) | 74.5 (72.9–76.1) | 78.5 (76.5–80.4) | 77.0 (74.9–79.2) | 80.4 (78.6–82.1) | 78.2 (75.9–80.6) | 83.0 (80.9–85.1) |
| Exposure to in-store ads | ||||||||||
| No | 7.0 (5.6–8.3) | 6.7 (5.9–7.6) | 6.3 (4.8–7.8) | 8.1 (6.7–9.4) | 8.4 (7.1–9.6) | 10.0 (7.4–12.6) | 7.7 (6.0–9.3) | 11.3 (9.4–13.2) | 11.5 (9.4–13.7) | 7.9 (6.2–9.6) |
| Yes | 92.9 (91.6–94.3) | 93.2 (92.3–94.0) | 93.6 (92.1–95.1) | 91.8 (90.5–93.2) | 91.5 (90.3–92.8) | 89.9 (87.3–92.5) | 92.2 (90.6–93.9) | 88.6 (86.7–90.5) | 88.4 (86.2–90.5) | 92.0 (90.3–93.7) |
| Tobacco use patterns | ||||||||||
| Cigarette only use | 35.1 (32.1–38.1) | 38.3 (36.5–40.1) | 40.0 (37.4–42.6) | 38.3 (35.8–40.7) | 35.5 (33.1–37.8) | 32.5 (28.6–36.3) | 17.7 (15.9–19.4) | 14.9 (13.2–16.6) | 12.3 (10.6–14.0) | 6.9 (5.4–8.3) |
| Non-cigarette combustible only use | 15.2 (12.8–17.6) | 14.8 (13.4–16.3) | 15.3 (13.6–17.0) | 15.8 (13.9–17.7) | 16.5 (14.1–18.9) | 19.7 (16.9–22.5) | 24.5 (20.9–28.2) | 26.6 (23.9–29.3) | 31.8 (28.0–35.6) | 20.9 (17.1–24.7) |
| Noncombustible only use | 4.3 (3.2–5.3) | 4.9 (4.0–5.9) | 5.8 (4.7–6.8) | 5.2 (4.0–6.3) | 7.8 (5.7–9.8) | 7.9 (5.7–10.1) | 10.2 (8.0–12.4) | 10.4 (8.2–12.6) | 10.9 (8.7–13.1) | 30.2 (26.6–33.7) |
| Any dual use | 37.4 (35.2–39.7) | 33.2 (31.9–34.5) | 30.4 (28.6–32.2) | 31.9 (29.8–34.0) | 30.0 (28.3–31.7) | 29.3 (26.5–32.0) | 32.6 (30.3–34.8) | 30.4 (28.0–32.8) | 29.6 (27.5–31.7) | 26.4 (24.2–28.6) |
| POLY use | 7.7 (6.7–8.7) | 8.5 (7.3–9.7) | 8.2 (7.1–9.2) | 8.6 (7.5–9.7) | 10.0 (8.4–11.6) | 10.4 (8.6–12.3) | 14.8 (12.9–16.6) | 17.5 (15.1–19.8) | 15.1 (12.9–17.3) | 15.5 (13.7–17.3) |
| Dual use sub-patterns | ||||||||||
| Non-cigarette combustible & noncombustible | 2.8 (2.1–3.6) | 3.6 (3.1–4.1) | 3.8 (3.0–4.6) | 4.7 (3.7–5.6) | 3.6 (2.9–4.4) | 4.8 (3.5–6.2) | 4.9 (3.8–6.0) | 6.5 (5.3–7.7) | 8.2 (6.8–9.5) | 14.0 (12.2–15.7) |
| Cigarette & noncombustible | 3.8 (2.3–5.2) | 2.8 (2.2–3.4) | 3.5 (2.6–4.3) | 2.7 (1.8–3.7) | 3.1 (1.9–4.4) | 3.9 (2.6–5.2) | 5.7 (4.3–7.1) | 5.3 (4.3–6.3) | 5.2 (3.7–6.6) | 7.3 (6.1–8.5) |
| Cigarette & non- cigarette combustible | 30.7 (28.1–33.3) | 26.6 (25.0–28.3) | 23.1 (21.1–25.0) | 24.4 (22.4–26.4) | 23.1 (21.1–25.1) | 20.4 (18.5–22.3) | 21.8 (20.2–23.5) | 18.5 (16.5–20.6) | 16.2 (14.1–18.3) | 5.0 (3.7–6.4) |
N = 38662 tobacco users who reported any past 30-day tobacco use, ages 17 or younger.
n = unweighted N.
95% CI: 95% confidence intervals.
*Cells represent mean and 95% confidence intervals.
Cigarette only use (n = 11192), non-cigarette combustible only use (n = 7898), noncombustible only use (n = 3172), any dual use (n = 12340), POLY use (n = 4060), non-cigarette combustible and noncombustible dual use (n = 2046), cigarette and noncombustible dual use (n = 1390), cigarette and non-cigarette combustible dual use (n = 8904).
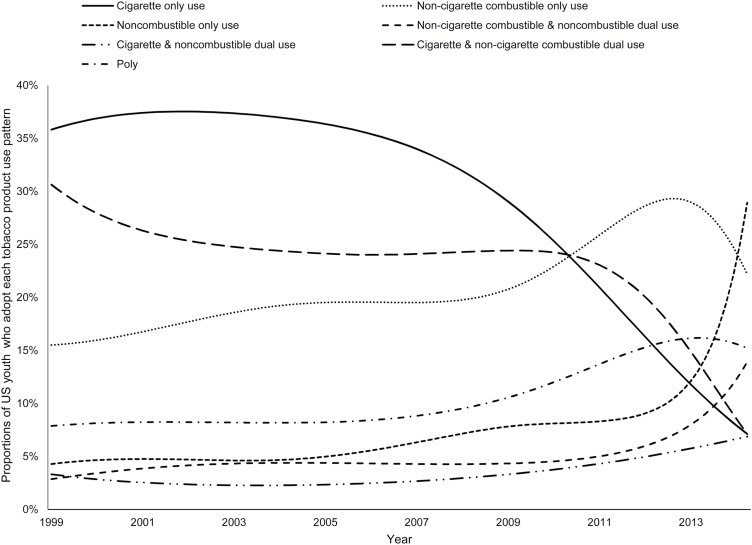
Figure 1 shows unadjusted descriptive trends in T-PUPs among youth tobacco users ages 17 and younger from 1999 to 2014. Past 30-day cigarette only use, cigarette and non-cigarette combustible dual use, and non-cigarette combustible only use were the three most prevalent T-PUPs from 1999 to 2010 among 9- to 17-year-old tobacco users. Of youth tobacco users, an estimated 36% and 20% were cigarette only users and 30% and 22% were cigarette and non-cigarette combustible dual users in 1999 and 2010, respectively. After 2010, both T-PUPs showed a downward trend falling to an estimated 8% in 2014 among youth tobacco users. Non-cigarette combustible only use exhibited an upward trend from 1999 to 2012 estimated at 15% and 29%, respectively, after which it declined to 22% in 2014 among tobacco users. Conversely, POLY, noncombustible only use, non-cigarette combustible and noncombustible dual use, and cigarette and noncombustible dual use showed an upward trend among 9- to 17-year-old tobacco users. Estimated proportions were 7% for POLY, 4% for noncombustible only use, 3% for cigarette and non-cigarette noncombustible dual use, and 2% for non-cigarette combustible and noncombustible dual use in 1999 among youth tobacco users. By 2014, POLY, noncombustible only use, non-cigarette combustible and noncombustible dual use, and cigarette and noncombustible dual use were estimated at 15%, 28%, 13%, and 7%, respectively, among youth tobacco users.
Figure 1.
Proportions of tobacco product use patterns among US youth tobacco users, 1999–2014. N = 38662 tobacco users who reported any past 30-day tobacco use, ages 17 or younger.
Supplementary figure 1 shows the adjusted odds ratios of T-PUPs compared to cigarette only use among tobacco users over time, 1999 to 2014. Compared to cigarette only use, non-cigarette combustible only use and noncombustible only use were more prevalent starting in 2010 (AOR 1.38, CI = 1.02–1.87) (Supplementary Figure 1a) and 2013 (AOR 1.78, CI = 1.11–2.84) (Supplementary Figure 1b). All other T-PUPs remained less prevalent than cigarette only use among youth tobacco users: non-cigarette combustible and noncombustible dual use (lowest AOR 0.04, CI = 0.02–0.09 in 1999) (Supplementary Figure 1c), cigarette and noncombustible dual use (lowest AOR 0.01, CI = 0.008–0.03 in 2004) (Supplementary Figure 1d), cigarette and non-cigarette combustible dual use (lowest AOR 0.21, CI = 0.16–0.28 in 2001) (Supplementary Figure 1e), and POLY (lowest AOR 0.07, CI = 0.05–0.10 in 2002) (Supplementary Figure 1f). In 2014, prevalence of dual (i.e. non-cigarette combustible and noncombustible, cigarette and noncombustible, cigarette and non-cigarette combustible) and POLY became statistically indistinguishable from cigarette only use.
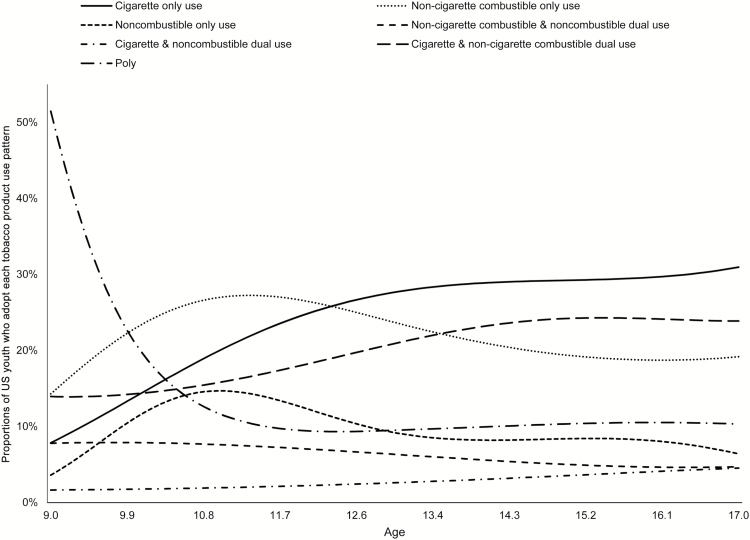
Figure 2 shows unadjusted descriptive trends in T-PUPs by age, 9 to 17 years old, among tobacco users. Past 30-day cigarette only use was the most prevalent T-PUP among 12.5- to 17-year-old tobacco users with estimated proportions of 26% and 30%, respectively. The second and third most prevalent T-PUPs among 14- to 17-year-old tobacco users were cigarette and non-cigarette combustible dual use (23% estimated proportion throughout ages 14 to 17) and non-cigarette combustible only use (estimated to be 21% at age 14 and 19% at age 17). Among nine-year-old tobacco users, POLY (51%), non-cigarette combustible only use (22%), cigarette and non-cigarette combustible dual use (14%), cigarette only use (13%), and non-cigarette combustible and noncombustible dual use (7%) were estimated to be the most prevalent T-PUPs.
Figure 2.
Proportions of tobacco product use patterns among US youth tobacco users by age (9–17 years), 1999–2014. N = 38662 tobacco users who reported any past 30-day tobacco use, ages 17 or younger.
Supplementary Figure 2 shows the adjusted odds ratios odds ratios of T-PUPs compared to cigarette only use by age. T-PUPs did not significantly differ from cigarette only use among 9- to 10-year-old tobacco users. Further, cigarette only use remained the most prevalent T-PUP across ages 11 to 17. Non-cigarette combustible only use (AOR 0.14, CI = 0.10–0.19) (Supplementary Figure 2a), noncombustible only use (AOR 0.01, CI = 0.008–0.02) (Supplementary Figure 2b), non-cigarette combustible and noncombustible dual use (AOR 0.01, CI = 0.01–0.03) (Supplementary Figure 2c), cigarette and noncombustible dual use (AOR 0.02, CI = 0.01–0.04) (Supplementary Figure 2d), cigarette and non-cigarette combustible dual use (AOR 0.32, CI = 0.24–0.43) (Supplementary Figure 2e), and POLY (AOR 0.02, CI = 0.01–0.04) (Supplementary Figure 2f) were less prevalent compared to cigarette only use at age 17.
To accommodate the introduction of new tobacco products starting 2010, we examined prevalence of T-PUPs over age for two periods 1999–2009 and 2011–2014. The year 2010 marked the national launch of Marlboro snus, 2012 marked Lorillard’s acquisition of Blu, and 2013 marked the launch of Mark Ten and Vuse. Odds ratio figures for 1999–2009 mirrored those of the overall sample (Supplementary Figures 1a–f). No significant differences were detected in prevalence of each T-PUP compared to cigarette only use for 2011–2014.
Discussion
This paper is the first to document trends in seven mutually exclusive T-PUPs over time (1999 to 2014) and age (9 to 17) using nationally representative samples.15 Three results emerged: First, cigarette only use was most prevalent T-PUP from 1999 to 2010 and among youth tobacco users ages 11 to 17. Second, starting in 2010 and 2013, non-cigarette combustible only use and noncombustible only use were more prevalent compared to cigarette only use among youth tobacco users. Third, starting in 2011, there was an upward trend of cigarette and noncombustible dual use, non-cigarette combustible and noncombustible dual use, and POLY among youth tobacco users, patterns that involve non-cigarette combustible and/or noncombustible products either solely or in combination with cigarettes.
Our results corroborate available evidence, which demonstrate the accuracy of T-PUPs model as a classification tool. Our downward trend of cigarette only use is consistent with evidence that shows past 30-day smoking has declined from 20.7% in 1991 to 7.0% in 2015 among U.S. youth.8 Further, the introduction of new non-cigarette tobacco products may explain the upward trend of non-cigarette combustible only and noncombustible only T-PUPs. Examples include the launch of Blu, Mark Ten, and Vuse e-cigarettes in 2012–201331 and an estimated 300 hookah cafés in the U.S. since 2000.32 Consequently, use of e-cigarettes and hookah among youth increased from 3.3% and 4.1% in 2011 to 6.8% and 5.4% in 2012, respectively.33
Non-cigarette combustible only use and noncombustible only use were the only T-PUPs estimated to be more prevalent than cigarette only use starting in 2010 and 2013 among youth tobacco users. While today’s youth grew up in an anti-cigarette smoking environment,34 non-cigarette tobacco products enjoy several features that appeal to them. For example, non-cigarette products come in youth-oriented flavors (e.g. candy, fruit),35,36 which overcome youth aversion to tobacco smoke and encourage experimentation. Data show that 32.2% of 10–14 year-olds and 59.3% of 15–17 year-olds use flavored product when they first tried tobacco products.16 Youth perceive new tobacco products (e.g. e-cigarettes) to be less harmful and more socially appealing than traditional cigarettes.37 Finally, tobacco companies are heavily marketing non-cigarette tobacco products such as e-cigarettes and smokeless tobacco to youth.38,39
Three T-PUPs (cigarette and noncombustible dual use, non-cigarette combustible and noncombustible dual use, and POLY) showed an upward trend starting in 2011 among youth tobacco users. Common across these patterns are noncombustible tobacco products. Further, these patterns are exclusively dual and polytobacco use. These results suggest future shifts in T-PUPs among youth where use of non-cigarette tobacco products becomes more prevalent than cigarettes. These results are consistent with previous studies that show use of multiple tobacco products is prevalent among youth.11,15 Although these T-PUPs are yet to be significantly more prevalent than cigarette only use, this upward trend is alarming. For example, individuals who use both cigarettes and smokeless tobacco have higher exposure to nicotine and tobacco-specific nitrosamine than those who only smoke cigarettes.40 Additionally, early exposure to nicotine is associated with negative health (e.g. nicotine dependency, addiction, use of illicit drugs),5,12,41 cognitive (e.g. degraded cognitive performance),42,43 psychological (e.g. anxiety, depression),41,44,45 and social (e.g. poor academic performance) outcomes.12 However, evidence is insufficient on short- and long-term effects of non-cigarette tobacco products.46–48 Moreover, evidence is scarce on the combined effects of cigarette and non-cigarette tobacco products among dual and polytobacco youth users on individual and population health. Research is needed to further understand the risks of dual and polytobacco use especially among youth.
Our results on T-PUPs by age show that cigarette only use remains the most prevalent T-PUP among tobacco users ages 11 to 17. This corroborates existing literature that shows cigarettes remain the main tobacco product used with or without other products.16 Interestingly, we find that among tobacco users 9 to 10 years old, no T-PUP emerges as significantly more or less prevalent than cigarette only use. This suggests that youth experiment early on with various tobacco products. In support, Soneji and colleagues (2014) identified types of tobacco products that youth ages 10 to14 first tried. Although cigarettes were most common (79.5%), youth have tried dip (9.1%); chewing tobacco (3.8%); cigars or cigarillos, large or premium cigars, filtered cigars, and hookah (1.5% each); and snuff and snus (0.8% each).16
As per recommendations of The American Academy of Pediatrics, pediatricians should screen for all tobacco use and deliver treatments during annual health visits49 when 62% to 83% of adolescents ages 14 to 17 have preventive health care visits.50 Educational campaigns51,52 and in-school interventions53 targeting parents and youth are also necessary to curb tobacco use. Tracking prevalence of T-PUPs over time and age by gender, race and ethnicity, and education should be a priority.15 Surveillance reports should also include data on intensity and frequency of use of all tobacco products to better capture use behaviors and their effects on individual and population health. Finally, research is needed to establish health risks associated with each T-PUP with appropriate biomarkers that capture harmful components of tobacco products. These steps will ensure better understanding of shifts in T-PUPs among youth and inform regulations and policies for tobacco control.48
With a multitude of emerging tobacco products (e.g. e-cigarettes), the T-PUPs model affords a parsimonious way to monitor tobacco use in seven categories while retaining the underlying differential characteristics of products that share a combustion method.15 Further, the model affords a standardized categorization of tobacco use, especially dual and polytobacco use, which have been inconsistently defined in the literature.11,14 The tradeoff for the use of T-PUPs is the loss of fine-grained data on individual tobacco products.15 Health agencies should decide on the level of granularity needed for different surveillance purposes.
Limitations
We cannot generalize results beyond in-school middle- and high-school students. Although data are self-reported, studies show the validity of self-report tobacco use data against biological markers.54 Further, the results are based on past 30-day tobacco use, which might produce estimates different from those based on other use definitions and questions (e.g., every day, some days, not at all).55 For example, results based on past 30-day use might overestimate current use prevalence because of experimentation with tobacco products rather than habitual use. E-cigarette question was not specific and, thus, participants might have reported their use of nicotine or non-nicotine products. However, studies showed traceable amounts of nicotine in some nicotine-free labeled products.56,57 Data on intensity/frequency of use were not available for all tobacco products. The cross-sectional nature of NYTS prevented us from understanding transitions between T-PUPs at the individual level.
Questions on use of roll-your-own cigarettes, hookah, snus, dissolvable tobacco, and e-cigarettes were absent in NYTS 1999 to 2009. Further, questions on use of roll-your-own and clove cigarettes were absent in NYTS 2014. NYTS methodology does not provide a rationale for excluding certain tobacco products at any given year after their introduction to the U.S. market. We controlled only for variables that consistently appeared in NYTS across years (e.g. living with a cigarette user). We did not control for variables that were completely absent (e.g. socio-economic status) or inconsistently present (e.g. exposure to tobacco magazine advertising) in NYTS. Results on tobacco use among youth 11 years old and younger should be interpreted with caution. Small sample size of participants ages 9 (n = 291), 10 (n = 35), and 11 (n = 511) might explain wide confidence intervals in T-PUPs by age (See Supplementary Table 1). Finally, the current version of TVEM macro does not allow for weighted analyses.
In conclusion, cigarette only use was most prevalent T-PUP till 2010 and remains the most prevalent among 11 to 17-year-old tobacco users. However, there is a rise in non-cigarette T-PUPs especially those exclusive to or in combination with noncombustible products. With an increasing number of available tobacco products, T-PUPs is a parsimonious model to survey exclusive patterns of tobacco use in an effort to extend public health efforts to all tobacco products and ultimately reduce tobacco use among youth.1
Supplementary Material
Supplementary data are available at Nicotine and Tobacco Research online.
Funding
The effort of Drs. Sherine El-Toukhy, Melanie Sabado, and Kelvin Choi was supported by the Division of Intramural Research of the National Institutes of Health, National Institute on Minority Health and Health Disparities. The funding source had no role to play in study conceptualization or data analysis.
Declaration of Interests
The authors have no conflicts of interest relevant to this article to disclose.
Disclaimer
The opinions expressed in this manuscript are the authors’ and do not represent those of the U.S. Department of Health and Human Services, the National Institutes of Health, or the National Institute on Minority Health and Health Disparities.
Authors’ contributions
Dr. El-Toukhy conceptualized the study, carried out the main analyses, and drafted the manuscript. Dr. Sabado prepared the dataset and carried out the initial analyses. Dr. Choi supervised data analyses and reviewed the manuscript. All authors interpreted the results and approved the final manuscript as submitted.
Supplementary Material
References
- 1. Healthy People. Tobacco use 2016. https://www.healthypeople.gov/2020/topics-objectives/topic/tobacco-use/objectives Accessed April 11, 2016.
- 2. Public Law 111–31. Family smoking prevention and tobacco control and federal retirement reform 2009. https://www.gpo.gov/fdsys/pkg/PLAW-111publ31/pdf/PLAW-111publ31.pdf. Accessed January 30, 2017.
- 3. Tobacco Control Legal Consortium. Federal regulation of tobacco: A summary 2009. http://publichealthlawcenter.org/sites/default/files/resources/tclc-fda-summary.pdf. Accessed January 30, 2017.
- 4. U.S. Department of Health and Human Services. Preventing tobacco use among youth and young adults: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2012. [Google Scholar]
- 5. U.S. Department of Health and Human Services. How tobacco smoke causes disease: The biology and behavioral basis for smoking-attributable disease. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2010. [Google Scholar]
- 6. DiFranza JR, Sweet M, Savageau JA, Ursprung WW. The assessment of tobacco dependence in young users of smokeless tobacco. Tob Control. 2012;21(5):471–476. [DOI] [PubMed] [Google Scholar]
- 7. Simon TR, Sussman S, Dent CW, Burton D, Flay BR. Correlates of exclusive or combined use of cigarettes and smokeless tobacco among male adolescents. Addict Behav. 1993;18(6):623–634. [DOI] [PubMed] [Google Scholar]
- 8. Johnston LD, O’Malley PM, Miech RA, Bachman JG, Schulenberg JE.. Monitoring the Future national survey results on drug use, 1975–2015: Overview, key findings on adolescent drug use. Ann Arbor: Institute for Social Research, The University of Michigan; 2016. [Google Scholar]
- 9. Arrazola RA, Kuiper NM, Dube SR. Patterns of current use of tobacco products among U.S. high school students for 2000–2012—findings from the National Youth Tobacco Survey. J. Adolesc. Health. 2014;54(1):54–60.e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention. Youth and tobacco use. 2016 http://www.cdc.gov/tobacco/data_statistics/fact_sheets/youth_data/tobacco_use/ Accessed April 11, 2016.
- 11. Arrazola RA, Singh T, Corey CG et al. ; Centers for Disease Control and Prevention (CDC). Tobacco use among middle and high school students - United States, 2011-2014. MMWR Morb Mortal Wkly Rep. 2015;64(14):381–385. [PMC free article] [PubMed] [Google Scholar]
- 12. U.S. Department of Health and Human Services. The health consequences of smoking - 50 years of progress: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 13. Barnett TE, Curbow BA, Weitz JR, Johnson TM, Smith-Simone SY. Water pipe tobacco smoking among middle and high school students. Am J Public Health. 2009;99(11):2014–2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee YO, Hebert CJ, Nonnemaker JM, Kim AE. Youth tobacco product use in the United States. Pediatrics. 2015;135(3):409–415. [DOI] [PubMed] [Google Scholar]
- 15. El-Toukhy S, Choi K. A risk-continuum categorization of product use among US youth tobacco users. Nicotine Tob Res. 2016;18(7):1596–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Soneji S, Sargent J, Tanski S. Multiple tobacco product use among US adolescents and young adults. Tob Control. 2016;25(2):174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Arrazola RA, Neff LJ, Kennedy SM, Holder-Hayes E, Jones CD; Centers for Disease Control and Prevention (CDC) Tobacco use among middle and high school students–United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(45):1021–1026. [PMC free article] [PubMed] [Google Scholar]
- 18. Gray N, Henningfield JE, Benowitz NL et al. Toward a comprehensive long term nicotine policy. Tob Control. 2005;14(3):161–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Centers for Disease Control and Prevention. National Youth Tobacco Survey (NYTS) 2015. http://www.cdc.gov/tobacco/data_statistics/surveys/nyts/index.htm Accessed February 1, 2016.
- 20. Forster JL, Wolfson M. Youth access to tobacco: policies and politics. Annu Rev Public Health. 1998;19:203–235. [DOI] [PubMed] [Google Scholar]
- 21. Apollonio DE, Glantz SA. Minimum ages of legal access for tobacco in the United States From 1863 to 2015. Am J Public Health. 2016;106(7):1200–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dissolvable tobacco http://ecigarettereviewed.com/dissolvable-tobacco Accessed January 30, 2017.
- 23. A historical timeline of electronic cigarettes http://casaa.org/historical-timeline-of-electronic-cigarettes/ Accessed January 30, 2017.
- 24. Biener L, Bogen K. Receptivity to Taboka and Camel Snus in a U.S. test market. Nicotine Tob Res. 2009;11(10):1154–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. TVEM SAS, Macro suite [computer program]. Version 3.1.0.2015.
- 26. Trtchounian A, Williams M, Talbot P. Conventional and electronic cigarettes (e-cigarettes) have different smoking characteristics. Nicotine Tob Res. 2010;12(9):905–912. [DOI] [PubMed] [Google Scholar]
- 27. Ambrose BK, Rostron BL, Johnson SE et al. Perceptions of the relative harm of cigarettes and e-cigarettes among U.S. youth. Am J Prev Med. 2014;47(2 Suppl 1):S53–S60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Duke JC, Allen JA, Pederson LL, Mowery PD, Xiao H, Sargent JD. Reported exposure to pro-tobacco messages in the media: trends among youth in the United States, 2000-2004. Am J Health Promot. 2009;23(3):195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Federal Trade Commission. Federal Trade Commission cigarette report for 2000. 2002. http://escholarship.org/uc/item/9w16c3dc#page-1. Accessed January 19, 2017. [Google Scholar]
- 30. Federal Trade Commission. Federal Trade Commission cigarette report for 2014. 2016. https://www.ftc.gov/system/files/documents/reports/federal-trade-commission-cigarette-report-2014-federal-trade-commission-smokeless-tobacco-report/ftc_cigarette_report_2014.pdf. Accessed January 19, 2017. [Google Scholar]
- 31. Tobacco Tactics. E-cigarettes http://www.tobaccotactics.org/index.php/ E-cigarettes Accessed January 19, 2016.
- 32. Smokeshop. Hookah cafes on the rise 2004. http://www.smokeshopmag.com/0404/retail.htm Accessed May 9, 2016.
- 33. Lauterstein D, Hoshino R, Gordon T, Watkins BX, Weitzman M, Zelikoff J. The changing face of tobacco use among United States youth. Curr Drug Abuse Rev. 2014;7(1):29–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Soc Sci Med. 2008;67(3):420–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. King BA, Tynan MA, Dube SR, Arrazola R. Flavored-little-cigar and flavored-cigarette use among U.S. middle and high school students. J Adolesc Health. 2014;54(1):40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Wagoner KG, Cornacchione J, Wiseman KD, Teal R, Moracco KE, Sutfin E. E-cigarettes, hookah pens and vapes: adolescent and young adult perceptions of electronic nicotine delivery systems. Nicotine Tob Res. 2016;18(10):2006–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Grana RA, Ling PM. “Smoking revolution”: a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46(4):395–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. El-Toukhy SM, Choi K. Magazine hyped: trends in tobacco advertising and readership characteristics, 2010-2014. Prev Med. 2016;91:132–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rostron BL, Chang CM, van Bemmel DM, Xia Y, Blount BC. Nicotine and toxicant exposure among U.S. smokeless tobacco users: results from 1999 to 2012 National Health and Nutrition Examination Survey data. Cancer Epidemiol Biomarkers Prev. 2015;24(12):1829–1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122(2):125–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Fountain SB, Rowan JD, Kelley BM, Willey AR, Nolley EP. Adolescent exposure to nicotine impairs adult serial pattern learning in rats. Exp Brain Res. 2008;187(4):651–656. [DOI] [PubMed] [Google Scholar]
- 43. Counotte DS, Spijker S, Van de Burgwal LH et al. Long-lasting cognitive deficits resulting from adolescent nicotine exposure in rats. Neuropsychopharmacology. 2009;34(2):299–306. [DOI] [PubMed] [Google Scholar]
- 44. Slawecki CJ, Thorsell AK, El Khoury A, Mathé AA, Ehlers CL. Increased CRF-like and NPY-like immunoreactivity in adult rats exposed to nicotine during adolescence: relation to anxiety-like and depressive-like behavior. Neuropeptides. 2005;39(4):369–377. [DOI] [PubMed] [Google Scholar]
- 45. Goodman E, Capitman J. Depressive symptoms and cigarette smoking among teens. Pediatrics. 2000;106(4):748–755. [DOI] [PubMed] [Google Scholar]
- 46. Etter JF, Bullen C, Flouris AD, Laugesen M, Eissenberg T. Electronic nicotine delivery systems: a research agenda. Tob Control. 2011;20(3):243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Critchley JA, Unal B. Health effects associated with smokeless tobacco: a systematic review. Thorax. 2003;58(5):435–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. O’Connor RJ. Non-cigarette tobacco products: what have we learnt and where are we headed?Tob Control. 2012;21(2):181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Farber HJ, Groner J, Walley S, Nelson K; SECTION ON TOBACCO CONTROL Protecting children from tobacco, nicotine, and tobacco smoke. Pediatrics. 2015;136(5):e1439–e1467. [DOI] [PubMed] [Google Scholar]
- 50. Eugene O. Adolescent health care visits: opportunities for brief prevention messages. Eff Clin Pract. 1999;2(6):272–276. [PubMed] [Google Scholar]
- 51. Stephenson MT. Anti‐drug public service announcements targeting parents: an analysis and evaluation. Southern Journal of Communication. 2002;67(4):335–350. [Google Scholar]
- 52. Stephenson MT, Quick BL. Parent ads in the National Youth Anti-Drug Media Campaign. J Health Commun. 2005;10(8):701–710. [DOI] [PubMed] [Google Scholar]
- 53. U.S. Department of Health and Human Services. Reducing tobacco use: A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000. [Google Scholar]
- 54. Caraballo RS, Giovino GA, Pechacek TF. Self-reported cigarette smoking vs. serum cotinine among U.S. adolescents. Nicotine Tob Res. 2004;6(1):19–25. [DOI] [PubMed] [Google Scholar]
- 55. Ryan H, Trosclair A, Gfroerer J. Adult current smoking: differences in definitions and prevalence estimates—NHIS and NSDUH, 2008. J. Environ. Public Health. 2012;2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Trehy ML, Ye W, Hadwiger ME et al. Analysis of electronic cigarette cartridges, refill solutions, and smoke for nicotine and nicotine related impurities. J. Liq. Chromatogr. Rel. Technol. 2011;34(14):1442–1458. [Google Scholar]
- 57. U.S. Food and Drug Administration. Evaluation of e-cigarettes 2009 DPATR-FY-09-23. https://www.fda.gov/downloads/drugs/scienceresearch/ucm173250.pdf. Accessed January 30, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.