Abstract
Background:
Complementary and alternative medicine is a rapidly growing area of biomedical inquiry. Yoga has emerged in the forefront of holistic medical care due to its long history of linking physical, mental, and spiritual well-being. Research in yoga therapy (YT) has associated improved cardiovascular and quality of life (QoL) outcomes for the special needs of heart failure (HF) patients.
Aim:
The aim of this study is to review yoga intervention studies on HF patients, discuss proposed mechanisms, and examine yoga's effect on physiological systems that have potential benefits for HF patients. Second, to recommend future research directions to find the most effective delivery methods of yoga to medically stable HF patients.
Methods:
The authors conducted a systematic review of the medical literature for RCTs involving HF patients as participants in yoga interventions and for studies utilizing mechanistic theories of stretch and new technologies. We examined physical intensity, mechanistic theories, and the use of the latest technologies.
Conclusions:
Based on the review, there is a need to further explore yoga mechanisms and research options for the delivery of YT. Software apps as exergames developed for use at home and community activity centers may minimize health disparities and increase QoL for HF patients.
Keywords: Complementary medicine, exercise adherence, heart failure, quality of life, yoga therapy
Introduction
Hatha yoga is a generic term for the practice of the physical yoga postures, (asanas), breathing techniques (pranayama), and meditation (dhyana) intended to improve health by balancing strength, breath, and flexibility.[1] The physical postures of yoga have evolved into many different styles and levels of exertion ranging from a focus on body alignment,[2] to rigorous forms that combine several postures in a dynamic series.[3] Yoga may provide overall and specific benefits that lower cardiac risk factors for cardiovascular disease and metabolic syndrome.[4,5] Currently, hundreds of medical centers in the United States offer yoga classes to their community members and patients with heart disease.[6] Medical reasons for yoga's widespread appeal may include its adaptability to a wide range of physical fitness levels, lower physiological stress reactivity,[7] and its association with weight loss.[8,9]
The treatment and survival of heart disease patients have been improving due to advancements in the medical specialty of cardiology, according to a recent report from the American Heart Association.[10] This positive outcome has led to significant increases in the number of patients who survive and live with heart failure (HF). Regarding HF and exercise, patients are encouraged to engage in exercise within the limits of their disease, which is a recent change in management. The large and increasing incidence of HF [11] leads to the investigation of yoga as an adjunct therapy.[12] Current therapies fail to reverse exercise intolerance, fatigue, and other well-known symptoms of HF, thus encouraging the investigation of a systems biology or integrative medicine approach involving either mind and body methodologies or alternative therapies for HF management.[13] In addition, yoga as a treatment modality for the HF patient may lead to a decrease in symptoms and improved quality of life (QoL) because of gains in muscle strength, improved endurance, flexibility, and decreased anxiety.
The effects of yoga for HF patients are just beginning to emerge in randomized clinical trials (RCTs). Initial findings include a reduction of inflammatory markers, blood pressure, pain, and a decrease in implantable cardioverter defibrillator firings. Moving forward, linking ancient therapeutic practices with medical device platforms using smart and connected technologies has the potential to advance yoga therapies toward hard-to-reach populations, aimed at reducing health disparities and improving QoL in the treatment of HF patients.
Therefore, we intend to review relevant yoga research interventions, discuss proposed mechanisms, and examine yoga's effect on physiological systems that have potential benefits for HF patients (e.g. pulmonary, vascular, and inflammatory) and recommend future research directions.
Methods
The authors conducted a systematic review of the medical literature. The initial search was conducted utilizing PubMed databases online, according to the PRISMA 2009 checklist for systematic reviews.[14] Search terms were, HF and Yoga (n = 17), Peripheral Stretch Mechanisms (n = 171), and Yoga Cardiovascular (n = 248). All studies were screened for randomization and topic relevance, leaving five studies that met the criteria of an RCT of yoga, conducted with HF patients as subjects. We also included studies on yoga's cardiovascular and metabolic requirements and stretch theory. The search included research after 1995, up to September 2016.
Metabolic demand of yoga and heart failure
Kinesiologists measure energy expenditure utilizing stationary [Figure 1] and portable metabolic systems.[19] Studies of yoga have highlighted the wide range of metabolic energy expenditure found across the many styles of yoga. It is critical to consider the energy requirements of any activity before making recommendations to deconditioned HF patients. We found no research in the database that examined the metabolic cost of Hatha yoga postures with cardiac or HF patients as subjects.
Figure 1.

Measurement of metabolic consumption during a yoga posture
Few studies have measured the energy cost of yoga in healthy adults, utilizing a variety of protocols. The first published investigation found, compared the metabolic equivalents (METs) of a 32-min Hatha yoga routine to a 32-min treadmill walk at 4.0 mph.[15] Ten subjects 38–47 years of age, achieved an energy expenditure of 4.1 METs for a yoga routine, compared with 5.4 METs required for treadmill walking. A similar study [16] measured the oxygen requirements of a more dynamic yoga sequence (Ashtanga Vinyasa style) and reported a metabolic demand of 6.7 METs. They also found a poor correlation (r = 0.05) between heart rate (HR) response during yoga its relationship to oxygen consumption based on a maximal treadmill test. The authors suggest that the nonlinear relationship is due to the anaerobic and isometric muscle action components of yoga.
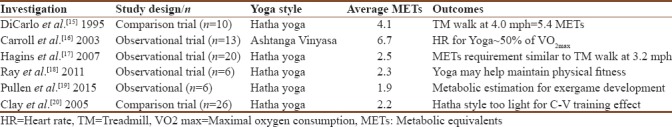
Clearly, metabolic requirements of yoga vary considerably based on the various forms of yoga practiced and the fitness level of the practitioner. This metabolic variation led to the question of the safety of yoga for the HF patient and further investigation of the literature. Table 1 presents the MET requirements of a variety of yoga styles conducted on healthy practitioners found in the scientific literature.[17,18,19,20] No studies were found that measured the metabolic intensity of yoga on HF patients directly, making recommendations unfounded from a scientific perspective. However, it is prudent to recommend that the less vigorous styles of yoga are of reasonable intensity for the HF patient who would participate in a yoga therapy (YT) program.
Table 1.
Metabolic equivalents for yoga (original)
Randomized controlled trials of YT and relaxation training in hypertensive individuals and cardiac patients have demonstrated significant reductions of systolic and diastolic blood pressure.[4,21] In a recent meta-analysis of studies on yoga's effect on hypertension,[22] yoga was associated with significant reductions in blood pressure (≈4 mmHg, systolic and diastolic). Their subgroup analyses demonstrated greater reductions in blood pressure (≈8 mmHg, systolic; ≈6 mmHg, diastolic) for interventions that incorporated all of the basic elements of a yoga practice (postures, meditation, and breathing). The differences between the physiological effects of yoga and standard exercise, however, were not significant. This raises the question: what are the differences between yoga and aerobic exercise and what are their effects on the downregulation of the hypothalamic–pituitary axis and the sympathetic nervous system.[23,24] To optimize the effects of exercise on endothelial function and peak oxygen consumption, aerobic interval training may yield greater benefits than moderate continuous aerobic exercise.[25] The exploration of exactly which combination and type of yoga protocol will yield the greatest benefits to HF patients remains. The future investigation could determine the most efficacious exercise prescription that combines yoga and traditional exercise dosing for HF patients.[26]
Mechanisms of yoga
Scientific analysis of the mechanisms of yoga and its effects on physiological systems are beginning to emerging in the medical literature. In-depth yoga review studies examine the role of yoga on health.[27,28] Innes et al.[28] pooled 70 studies that met specific inclusion criteria between 1970 and 2004. These studies were concerned with the role of yoga and the reduction of insulin resistance, metabolic syndrome, and cardiovascular diseases. One mechanism of yoga hypothesized to improve the cardiovascular risk profile is that the physical postures or breathing exercises exert a massaging effect that stimulates the vagal nerve.
The underlying physiology by which the practice of YT can improve cardiovascular disease-related outcomes may involve parasympathetic activation and extracellular factor release stimulation as in Figure 2. It is undetermined if newly synthesized or dislodged adhering factors released from the stretch or mechanical conditioning cause the observed measurement outcomes. Yoga effects could stem from three mechanisms: vagal nerve stimulation, reduction in perceived stress, and musculoskeletal stimulation. By massaging the vagal nerve directly, yoga may promote parasympathetic activation thus leading to decreased HR, blood pressure, improved HR variability (HRV), and similar metabolic and psychological benefits resulting in an improved outcome. Yoga has also been associated with decreased levels of depression,[29] improved quality and quantity of sleep,[30] improved metabolic syndrome risk,[31] and weight reduction in the form of reduced visceral fat.[8,32]
Figure 2.
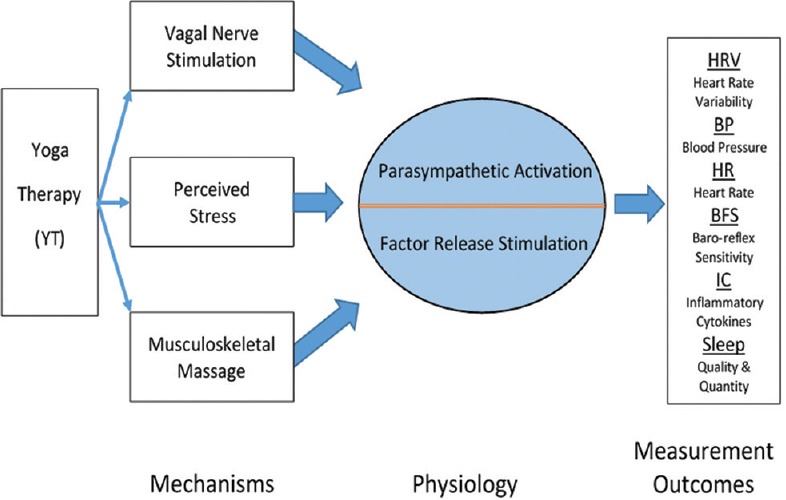
Yoga intervention may lower cardiovascular risk by acting through physiologic pathways of activation and stimulation. Yoga effects nerve stimulation, stress reactivity, musculoskeletal, and hormonal systems
The third mechanism for yoga's physiologic effects, labeled as musculoskeletal massage in Figure 2, was examined for a mechanical effect of stretching on inflammation-regulating molecules within affected connective tissue.[33] Stretch-induced molecules identified as inflammation pro-resolving mediators in a rodent model were reported.[34] Recently, circulating muscle-specific miRNAs increased in blood samples obtained following prolonged aerobic exercise in humans,[35] and after stretching in animal models.[34] A growing body of evidence demonstrates that exosomes can act as intercellular communication packets carrying factors such as receptors, transmembrane proteins, kinases, mRNA, miRNA, long noncoding RNA, DNA, and lipids.[36]
Collectively, these anthropometric, psychological, and metabolic changes may lead to improved coagulation and inflammatory profiles. Yoga, therefore, may promote increased fibrinolysis, decreased free-radical production, decreased oxidative stress, and improved endothelial function.[37] Understanding that atherosclerosis is an inflammatory process and cardiovascular events are in part dependent on endothelial function, the literature supports that yoga can reduce progression while improving management and clinical endpoints of atherosclerosis, hypertension, cardiovascular disease, and risk factor reduction.[38,39]
Brachial artery reactivity improved after a 6-week yoga pilot study on patients with coronary artery disease (CAD) or at high risk for CAD.[40] Impaired endothelial function is one of the mechanisms related to an increased risk of MI. Interestingly, the yoga intervention significantly improved brachial artery reactivity in the participants that had known CAD and had little association with the high-risk group. Santos et al.[41] studied the underlying mechanisms of blunted vasodilatation in HF patients and concluded that sympathetic activation modulated the blunted muscle endothelium-mediated vasodilatation during mental stress. The combination of the previous two studies, with the inclusion of yoga treatment, could further elucidate the role of yoga on sympathetic downregulation mechanisms.
Additional physiological mechanisms of yoga that have been the subject of scientific inquiry are improvement in baroreflex sensitivity,[42] increased HRV,[43] and decreased catecholamine response to hypoxia and hypercapnia.[44] Krishna et al. reported that a 12-week yoga intervention significantly improved parasympathetic activity, decreased sympathetic stimulation, and reduced N-terminal pro-B-type natriuretic peptide in New York Heart Association Class I and II HF patients in conjunction with standard medical therapy.[45,46] Tyagi et al.[5] concluded that yoga practitioners have greater metabolic variability compared to nonyoga practitioners and metabolic syndrome patients, due to reduced oxygen requirements during resting conditions and more rapid poststress recovery.
Yoga research with heart failure patients
Yoga as a therapeutic alternative or adjunct to traditional exercise programs is not included in the recommendations of highly respected organizations that publish management guidelines for HF patients. For example, the 2013 Canadian Cardiovascular Society HF Management Guidelines Update is silent in this area.[47] Currently, all stable HF patients are candidates for cardiac rehabilitation programs to improve exercise tolerance and QoL.[48,49,50] This represents a relatively recent development in cardiac care based on the positive results of the HF-ACTION study. Medicare now supports cardiac rehabilitation coverage for HF patients.[51] There are no multicenter clinical trials to study the best practices of YT for HF at present.
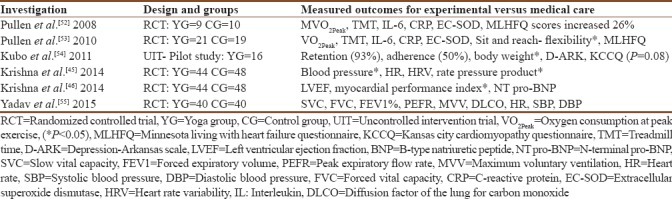
Our group [52,53] examined the effect of yoga on stable HF outpatients randomized to either yoga treatment or to standard medical care. These studies consisted of 60-min, bi-weekly yoga classes led by a qualified yoga instructor at a hospital-based Vascular Research Laboratory. At a hospital that served predominantly indigent patients, researchers utilized a pre-post-test format over an 8-week trial period. The measurements included the HF patients' exercise capacity, QoL, flexibility, and inflammatory biomarkers. Significant improvement of all biomarkers (interleukin-6, C-reactive protein, and extracellular superoxide dismutase) and functional capacity occurred in the yoga group after 8-week of yoga training as compared to the control group.
Kubo et al.[54] conducted a feasibility study to examine recruitment, retention, adherence, QoL, depression, and body weight for a multiethnic population of HF patients who attended supervised yoga sessions twice a week for 8 weeks. Significant reduction in weight and severity of depression was found. They concluded that HF patients can incorporate yoga into their lives and that it may help with disease management and symptoms.
More recently, randomized control studies (RCT) have been published that examined a variety of cardiac, pulmonary function, and QoL parameters with yoga and HF patients as subjects.[45,46,51,52,55] Yadav et al.[55] conducted a 3-month RCT of yoga postures, breathing, and relaxation exercises. Forced vital capacity increased 24%, from 1.6 to 2.1 for the yoga group. Systolic blood pressure decreased 11%, from 143 to 127 mmHg. Both measurements from pre- to post-test were statistically significant improvements for the yoga participants. Recently, a randomized trial by Hassanpour Dehkordi and Khaledi Far [56] utilized echocardiography to measure left ventricular diameter and ejection fraction in HF patients before and after 24 weeks of aerobic exercise training. They reported a significant improvement in left ventricular diameter and ejection fraction in the experimental group in comparison to the control group at the end of the experimental period. A similar design using a yoga intervention to determine how yoga effects left ventricular diameter and ejection fraction. Table 2 summarizes the studies that have published RCT of yoga and several physiological variables that have improved significantly in HF patients.
Table 2.
Yoga studies with heart failure patients as subjects (original)
Exercise adherence
For any exercise program to be beneficial, patients must participate and comply with the program. Corvera-Tindel et al.[57] examined factors influencing noncompliance in a 12-week home walking program. They found higher comorbidities, longer duration of HF, lower hostility, and lower BMI were predictive of noncompliance. They also concluded that noncompliant HF patients might benefit from individualized exercise prescriptions.
The logistics and practical aspects of attending a formal cardiac rehabilitation program prevent many patients from complying with a physician's recommendation or referral to attend a hospital-based cardiac rehabilitation program. Financial, social, and family issues are among some of the obstacles to attending cardiac rehabilitation. Cooper et al.[58] examined cardiac rehabilitation attendance and patients' beliefs toward attending cardiac rehabilitation programs. Patient beliefs accounted for 65% of the variance found. Four barriers differed significantly between attendees and nonattenders identified as, perceived necessity, exercise concerns, practical barriers, and personal suitability. In a similar study, interviews of postmyocardial infarction patients were thematically analyzed, which led to discovering that the determinants of cardiac rehabilitation relevance and adherence were influenced by financial, family, and social situations regardless of the encouragement they received toward attending the program. The researchers concluded that it would be unrealistic to anticipate 100% attendance in any cardiac rehabilitation program. A large segment of the HF patient population will not be able to attend a hospital-based cardiac rehabilitation program. A home-based alternative seems reasonable if a qualified health-care professional prescribes the exercise plan. Follow-up visits to the office or limited cardiac rehabilitation visits for adjustments and feedback would help reinforce adherence.
Home-based walking programs are reasonably safe for HF patients and facilitate adherence.[59] The number of steps walked at home, measured by pedometers worn by HF patients (n = 84), were found to predict survival better than a laboratory-based exercise test.[60] This study examined the relationship between daily activity levels and long-term prognosis. Pedometer-measured steps have also predicted exercise adherence and mortality in HF patients.[61] The use of pedometers to study the activity level and exercise capability of HF patients, initially reported by Cowley et al.[62] correlated poorly with treadmill stress test performance. The second study found that cardiac output (CO) correlated significantly (P < 0.001) with customary activity as assessed by the number of daily steps.[63] Conversely, the relationship between treadmill stress test performance and CO was poor (P = 0.245). The authors concluded that CO is a reliable index for determining patients' exercise capacity when walking speed is self-directed, but not when undergoing laboratory treadmill tests.
The HEART camp trial protocol attempted to determine the efficacy of a behavioral exercise training intervention on long-term adherence to exercise in patients with HF.[64] Considering the previous studies, the addition of behavioral techniques, pedometers, and cell phone apps are worthy of further study and may prove to increase engagement and adherence of yoga and walking activities at home. Recent publications report on novel interventions that explore new ways to deliver yoga guidance in home settings, for example, tele-yoga and exergames.[65,66]
Practical recommendations for heart failure patients
Recommendations for clinicians who treat HF patients based on the author's experience with cardiac patients; and research with yoga, HF patients and cardiac rehabilitation. Once an HF patient is medically stable, beginner Hatha, or Iyengar style yoga classes are reasonable to recommend. Caution HF patients to avoid rigorous or continuous flow styles of yoga, yoga classes conducted in a heated room and to avoid breath-holding. A hallmark condition of HF patients is peripheral muscle atrophy with impaired regulation of autonomic functions that may interfere with body temperature regulation.[67] Most yoga postures are modifiable to various levels of strength, balance, and endurance. For example, balance postures performed next to a wall, chairs used for support and seated postures for patients that have difficulty getting up and down from the floor. Yoga props can extend one's reach during a yoga session. In our study, inversion postures were avoided, except the legs up the wall posture. Hemodynamic tolerance was monitored by obtaining HR and blood pressure while patients were in the pose (see the Yoga 4 Heart asana sequence for specific yoga postures and modifications utilized).[68] At present, clinical history, individual assessment, exercise capacity, and clinical experience are the best tools for guiding HF patients in yoga.
Mindfulness in yoga therapy
As mentioned in the introduction, the component of yoga called mindfulness or meditation is important to consider for its impact on YT outcomes. Meditative practices may involve focused attention where the practitioner directs consciousness on breathing, an object, or word phrase known as a mantra. This focus of attention can also involve greater awareness of thoughts and sensations known as mindfulness meditation.[69] Others have explored the rationale and physiology of meditation to exert a positive influence on the cardiovascular system. Described as a wakeful hypometabolic state,[70] meditation can exert significant influence on autonomic tone with parasympathetic activation.[71] The autonomic nervous system is a principal component of the mind–heart connection and is a fundamental link between thoughts and emotions and the heart.[72] The Support Education and Research in Chronic Heart Failure Study trial demonstrated promise for the role of mindfulness therapy in the treatment of HF.[73] The treatment group had significantly improved HF symptoms at 1 year compared to the control group. The treatment group also had significantly lower levels of anxiety and depression; an effect that was attenuated at 1 year. More recently, transcendental meditation was found to decrease mortality, myocardial infarction, or stroke in African-American patients with coronary heart disease.[74] Although the results appear promising, analysis of these studies, raise the importance of mindfulness in therapeutic outcomes for HF patients. A limitation of this and many controlled studies on meditation is the potential effect of placebo, as no validated “sham meditation technique” exists.
Conclusions
Cardiac patients are encouraged to exercise and stay active for multiple benefits, including improvement of inflammatory markers and vascular reactivity. HF patients typically have comorbidities that prevent them from participating in traditional exercise programs and require individualized exercise prescription. The metabolic demand of yoga is flexible, ranging from chair based to continuous flow. Options for the delivery of yoga to HF patients may range from participation in a cardiac rehabilitation facility or a supervised home-based program using smart and connected technology, encouraging a sense of mastery and connection. Published research to date supports that yoga is a safe and effective addition to the management of HF patients and their QoL. The effects of yoga, either in conjunction with or as an alternative to traditional exercise management requires further investigation. We recommend multicenter, long-term studies designed to specify the type, amount and delivery of yoga to maximize the benefits and substantiate recommendations.
Smart and connected technologies to augment yoga-based therapeutic intervention for clinic or home settings could benefit hard-to-reach populations. Efforts using 3D room sensors such as Microsoft Kinect for qualitative analysis of yoga and Tai Chi postures [19] could lead to wide-scale adoption through inexpensive channels. These low-cost hardware/software smartphones or gaming platforms could assess therapeutic outcomes such as compliance to ideal postures, respiration, or energy expenditure. These applications can engage multiple participants for motivation and adherence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The content is solely the responsibility of the authors and does not necessarily represent official views of their respective institutions.
References
- 1.Hatha Yoga (n.d.) In Medical Dictionary Online. [Last accessed on 2017 Aug 12]. Available from: http://www.medical.dictionary.thefreedictionary.com/hatha+yoga.
- 2.Iyengar BK. Light on Yoga. New York: Shocken Books; 1979. [Google Scholar]
- 3.Birch BB. Power Yoga. New York: Fireside; 1995. [Google Scholar]
- 4.Chu P, Gotink RA, Yeh GY, Goldie SJ, Hunink MG. The effectiveness of yoga in modifying risk factors for cardiovascular disease and metabolic syndrome: A systematic review and meta-analysis of randomized controlled trials. Eur J Prev Cardiol. 2016;23:291–307. doi: 10.1177/2047487314562741. [DOI] [PubMed] [Google Scholar]
- 5.Tyagi A, Cohen M, Reece J, Telles S. An explorative study of metabolic responses to mental stress and yoga practices in yoga practitioners, non-yoga practitioners and individuals with metabolic syndrome. BMC Complement Altern Med. 2014;14:445. doi: 10.1186/1472-6882-14-445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cramer H, Lauche R, Haller H, Dobos G, Michalsen A. A systematic review of yoga for heart disease. Eur J Prev Cardiol. 2015;22:284–95. doi: 10.1177/2047487314523132. [DOI] [PubMed] [Google Scholar]
- 7.Madanmohan, Udupa K, Bhavanani AB, Krishnamurthy N, Pal GK. Modulation of cold pressor-induced stress by shavasan in normal adult volunteers. Indian J Physiol Pharmacol. 2002;46:307–12. [PubMed] [Google Scholar]
- 8.Kristal AR, Littman AJ, Benitez D, White E. Yoga practice is associated with attenuated weight gain in healthy, middle-aged men and women. Altern Ther Health Med. 2005;11:28–33. [PubMed] [Google Scholar]
- 9.Rioux JG, Ritenbaugh C. Narrative review of yoga intervention clinical trials including weight-related outcomes. Altern Ther Health Med. 2013;19:32–46. [PubMed] [Google Scholar]
- 10.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics - 2015 update: A report from the American heart association. Circulation. 2015;131:e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 11.Roger VL, Weston SA, Redfield MM, Hellermann-Homan JP, Killian J, Yawn BP, et al. Trends in heart failure incidence and survival in a community - Based population. JAMA. 2004;292:344–50. doi: 10.1001/jama.292.3.344. [DOI] [PubMed] [Google Scholar]
- 12.Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM, et al. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med. 2006;355:251–9. doi: 10.1056/NEJMoa052256. [DOI] [PubMed] [Google Scholar]
- 13.Nohria A, Lewis E, Stevenson LW. Medical management of advanced heart failure. JAMA. 2002;287:628–40. doi: 10.1001/jama.287.5.628. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.DiCarlo LJ, Sparling PB, Hinson BT, Snow TK, Roskoph LB. Cardiovascular, metabolic, and perceptual responses to hatha yoga standing poses. Med Exerc Nutr Health. 1995;4:107–12. [Google Scholar]
- 16.Carroll J, Blansit A, Otto RM, Wygand JW. The metabolic requirements of Vinyasa Yoga. Med Sci Sports Exerc. 2003;35:S155. [Google Scholar]
- 17.Hagins M, Moore W, Rundle A. Does practicing hatha yoga satisfy recommendations for intensity of physical activity which improves and maintains health and cardiovascular fitness? BMC Complement Altern Med. 2007;7:40. doi: 10.1186/1472-6882-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray US, Pathak A, Tomer OS. Hatha yoga practices: Energy expenditure, respiratory changes and intensity of exercise. Evid Based Complement Alternat Med 2011. 2011:241294. doi: 10.1093/ecam/neq046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pullen PR, Ogbesor A, Seffens W. Kinect acquisition of skeleton body positions during yoga and tai chi for exergame development. Med Sci Sports Exerc. 2015;47:162. [Google Scholar]
- 20.Clay CC, Lloyd LK, Walker JL, Sharp KR, Pankey RB. The metabolic cost of hatha yoga. J Strength Cond Res. 2005;19:604–10. doi: 10.1519/15144.1. [DOI] [PubMed] [Google Scholar]
- 21.Niranjan M, Bhagyalakshmi K, Ganaraja, Prabha AM, Ramesh B. Effects of yoga and supervised integrated exercise on heart rate variability and blood pressure in hypertensive patients. J Chin Clin Med. 2009;4:139–43. [Google Scholar]
- 22.Hagins M, States R, Selfe T, Innes K. Effectiveness of yoga for hypertension: Systematic review and meta-analysis. Evid Based Complement Alternat Med 2013. 2013:649836. doi: 10.1155/2013/649836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Innes KE, Vincent HK, Taylor AG. Chronic stress and insulin resistance-related indices of cardiovascular disease risk, part 2: A potential role for mind-body therapies. Altern Ther Health Med. 2007;13:44–51. [PubMed] [Google Scholar]
- 24.Benson H, Rosner BA, Marzetta BR, Klemchuk HM. Decreased blood-pressure in pharmacologically treated hypertensive patients who regularly elicited the relaxation response. Lancet. 1974;1:289–91. doi: 10.1016/s0140-6736(74)92596-3. [DOI] [PubMed] [Google Scholar]
- 25.Wisløff U, Støylen A, Loennechen JP, Bruvold M, Rognmo Ø, Haram PM, et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation. 2007;115:3086–94. doi: 10.1161/CIRCULATIONAHA.106.675041. [DOI] [PubMed] [Google Scholar]
- 26.Cook-Cottone C. Dosage as a critical variable in yoga therapy research. Int J Yoga Therap. 2013;23:11–2. [PubMed] [Google Scholar]
- 27.Jayasinghe SR. Yoga in cardiac health (a review) Eur J Cardiovasc Prev Rehabil. 2004;11:369–75. doi: 10.1097/01.hjr.0000206329.26038.cc. [DOI] [PubMed] [Google Scholar]
- 28.Innes KE, Bourguignon C, Taylor AG. Risk indices associated with the insulin resistance syndrome, cardiovascular disease, and possible protection with yoga: A systematic review. J Am Board Fam Pract. 2005;18:491–519. doi: 10.3122/jabfm.18.6.491. [DOI] [PubMed] [Google Scholar]
- 29.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: A systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–83. doi: 10.1002/da.22166. [DOI] [PubMed] [Google Scholar]
- 30.Halpern J, Cohen M, Kennedy G, Reece J, Cahan C, Baharav A, et al. Yoga for improving sleep quality and quality of life for older adults. Altern Ther Health Med. 2014;20:37–46. [PubMed] [Google Scholar]
- 31.Lau C, Yu R, Woo J. Effects of a 12-week hatha yoga intervention on metabolic risk and quality of life in Hong Kong Chinese adults with and without metabolic syndrome. PLoS One. 2015;10:e0130731. doi: 10.1371/journal.pone.0130731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McDermott KA, Rao MR, Nagarathna R, Murphy EJ, Burke A, Nagendra RH, et al. A yoga intervention for type 2 diabetes risk reduction: A pilot randomized controlled trial. BMC Complement Altern Med. 2014;14:212. doi: 10.1186/1472-6882-14-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berrueta L, Muskaj I, Olenich S, Butler T, Badger GJ, Colas RA, et al. Stretching impacts inflammation resolution in connective tissue. J Cell Physiol. 2016;231:1621–7. doi: 10.1002/jcp.25263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Corey SM, Vizzard MA, Bouffard NA, Badger GJ, Langevin HM. Stretching of the back improves gait, mechanical sensitivity and connective tissue inflammation in a rodent model. PLoS One. 2012;7:e29831. doi: 10.1371/journal.pone.0029831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Guescini M, Canonico B, Lucertini F, Maggio S, Annibalini G, Barbieri E, et al. Muscle releases alpha-sarcoglycan positive extracellular vesicles carrying miRNAs in the bloodstream. PLoS One. 2015;10:e0125094. doi: 10.1371/journal.pone.0125094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Emanueli C, Shearn AI, Angelini GD, Sahoo S. Exosomes and exosomal miRNAs in cardiovascular protection and repair. Vascul Pharmacol. 2015;71:24–30. doi: 10.1016/j.vph.2015.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sinha S, Singh SN, Monga YP, Ray US. Improvement of glutathione and total antioxidant status with yoga. J Altern Complement Med. 2007;13:1085–90. doi: 10.1089/acm.2007.0567. [DOI] [PubMed] [Google Scholar]
- 38.Shore R, Foster C, Pein R, Seebach E. Comparison of blood pressure lowering interventions. J Cardiopulm Rehabil. 2002;22:361–3. [Google Scholar]
- 39.Murugesan R, Govindarajulu N, Bera TK. Effect of selected yogic practices on the management of hypertension. Indian J Physiol Pharmacol. 2000;44:207–10. [PubMed] [Google Scholar]
- 40.Sivasankaran S, Pollard-Quintner S, Sachdeva R, Pugeda J, Hoq SM, Zarich SW, et al. The effect of a six-week program of yoga and meditation on brachial artery reactivity: Do psychosocial interventions affect vascular tone? Clin Cardiol. 2006;29:393–8. doi: 10.1002/clc.4960290905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Santos AC, Alves MJ, Rondon MU, Barretto AC, Middlekauff HR, Negrão CE, et al. Sympathetic activation restrains endothelium-mediated muscle vasodilatation in heart failure patients. Am J Physiol Heart Circ Physiol. 2005;289:H593–9. doi: 10.1152/ajpheart.01240.2004. [DOI] [PubMed] [Google Scholar]
- 42.Bernardi L, Porta C, Spicuzza L, Bellwon J, Spadacini G, Frey AW, et al. Slow breathing increases arterial baroreflex sensitivity in patients with chronic heart failure. Circulation. 2002;105:143–5. doi: 10.1161/hc0202.103311. [DOI] [PubMed] [Google Scholar]
- 43.Madanmohan, Bhavanani AB, Prakash ES, Kamath MG, Amudhan J. Effect of six weeks of shavasan training on spectral measures of short-term heart rate variability in young healthy volunteers. Indian J Physiol Pharmacol. 2004;48:370–3. [PubMed] [Google Scholar]
- 44.Spicuzza L, Gabutti A, Porta C, Montano N, Bernardi L. Yoga and chemoreflex response to hypoxia and hypercapnia. Lancet. 2000;356:1495–6. doi: 10.1016/S0140-6736(00)02881-6. [DOI] [PubMed] [Google Scholar]
- 45.Krishna BH, Pal P, Pal GK, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. Effect of yoga therapy on heart rate, blood pressure and cardiac autonomic function in heart failure. J Clin Diagn Res. 2014;8:14–6. doi: 10.7860/JCDR/2014/7844.3983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Krishna BH, Pal P, Pal G, Balachander J, Jayasettiaseelon E, Sreekanth Y, et al. A randomized controlled trial to study the effect of yoga therapy on cardiac function and N terminal pro BNP in heart failure. Integr Med Insights. 2014;9:1–6. doi: 10.4137/IMI.S13939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Canadian Cardiovascular Society Heart Failure Management Primary Panel. Moe GW, Ezekowitz JA, O'Meara E, Howlett JG, Fremes SE, et al. The 2013 Canadian Cardiovascular Society Heart Failure Management Guidelines Update: Focus on rehabilitation and exercise and surgical coronary revascularization. Can J Cardiol. 2014;30:249–63. doi: 10.1016/j.cjca.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 48.Flynn KE, Lin L, Moe GW, Howlett JG, Fine LJ, Spertus JA, et al. Relationships between changes in patient-reported health status and functional capacity in outpatients with heart failure. Am Heart J. 2012;163:88–94. doi: 10.1016/j.ahj.2011.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wenger NK. Quality of life: Can it and should it be assessed in patients with heart failure? Cardiology. 1989;76:391–8. doi: 10.1159/000174523. [DOI] [PubMed] [Google Scholar]
- 50.Tyni-Lenné R, Gordon A, Sylvén C. Improved quality of life in chronic heart failure patients following local endurance training with leg muscles. J Card Fail. 1996;2:111–7. doi: 10.1016/s1071-9164(96)80029-7. [DOI] [PubMed] [Google Scholar]
- 51.O'Connor CM, Whellan DJ, Lee KL, Keteyian SJ, Cooper LS, Ellis SJ, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301:1439–50. doi: 10.1001/jama.2009.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Pullen PR, Nagamia SH, Mehta PK, Thompson WR, Benardot D, Hammoud R, et al. Effects of yoga on inflammation and exercise capacity in patients with chronic heart failure. J Card Fail. 2008;14:407–13. doi: 10.1016/j.cardfail.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 53.Pullen PR, Thompson WR, Benardot D, Brandon LJ, Mehta PK, Rifai L, et al. Benefits of yoga for African American heart failure patients. Med Sci Sports Exerc. 2010;42:651–7. doi: 10.1249/MSS.0b013e3181bf24c4. [DOI] [PubMed] [Google Scholar]
- 54.Kubo A, Hung YY, Ritterman J. Yoga for heart failure patients: A feasibility pilot study with a multiethnic population. Int J Yoga Therap. 2011;21:77–83. [PubMed] [Google Scholar]
- 55.Yadav A, Singh S, Singh K, Pai P. Effect of yoga regimen on lung functions including diffusion capacity in coronary artery disease patients: A randomized controlled study. Int J Yoga. 2015;8:62–7. doi: 10.4103/0973-6131.146067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hassanpour Dehkordi A, Khaledi Far A. Effect of exercise training on the quality of life and echocardiography parameter of systolic function in patients with chronic heart failure: A randomized trial. Asian J Sports Med. 2015;6:e22643. doi: 10.5812/asjsm.22643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Corvera-Tindel T, Doering LV, Gomez T, Dracup K. Predictors of noncompliance to exercise training in heart failure. J Cardiovasc Nurs. 2004;19:269–77. doi: 10.1097/00005082-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 58.Cooper AF, Weinman J, Hankins M, Jackson G, Horne R. Assessing patients' beliefs about cardiac rehabilitation as a basis for predicting attendance after acute myocardial infarction. Heart. 2007;93:53–8. doi: 10.1136/hrt.2005.081299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Duncan KA, Pozehl B. Staying on course: The effects of an adherence facilitation intervention on home exercise participation. Prog Cardiovasc Nurs. 2002;17:59–65. doi: 10.1111/j.0889-7204.2002.01229.x. [DOI] [PubMed] [Google Scholar]
- 60.Walsh JT, Charlesworth A, Andrews R, Hawkins M, Cowley AJ. Relation of daily activity levels in patients with chronic heart failure to long-term prognosis. Am J Cardiol. 1997;79:1364–9. doi: 10.1016/s0002-9149(97)00141-0. [DOI] [PubMed] [Google Scholar]
- 61.Evangelista LS, Dracup K, Erickson V, McCarthy WJ, Hamilton MA, Fonarow GC, et al. Validity of pedometers for measuring exercise adherence in heart failure patients. J Card Fail. 2005;11:366–71. doi: 10.1016/j.cardfail.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 62.Cowley AJ, Fullwood L, Stainer K, Hampton JR. Exercise tolerance in patients with heart failure – How should it be measured? Eur Heart J. 1991;12:50–4. doi: 10.1093/oxfordjournals.eurheartj.a059824. [DOI] [PubMed] [Google Scholar]
- 63.Cowley AJ, Fullwood LJ, Muller AF, Stainer K, Skene AM, Hampton JR, et al. Exercise capability in heart failure: Is cardiac output important after all? Lancet. 1991;337:771–3. doi: 10.1016/0140-6736(91)91381-4. [DOI] [PubMed] [Google Scholar]
- 64.Pozehl BJ, Duncan K, Hertzog M, McGuire R, Norman JF, Artinian NT, et al. Study of adherence to exercise in heart failure: The HEART camp trial protocol. BMC Cardiovasc Disord. 2014;14:172. doi: 10.1186/1471-2261-14-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Selman L, McDermott K, Donesky D, Citron T, Howie-Esquivel J. Appropriateness and acceptability of a Tele-Yoga intervention for people with heart failure and chronic obstructive pulmonary disease: Qualitative findings from a controlled pilot study. BMC Complement Altern Med. 2015;15:21. doi: 10.1186/s12906-015-0540-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Seffens WS, Pullen PR. Exergame development study of Kinect for yoga postures. International Association of Yoga Therapy, IYAT Symposium on Yoga Research. 2014. [Last accessed on 2017 Aug 12]. Available from: https://www.c.ymcdn.com/sites/www.iayt.org/resource/resmgr/docs_syr2015/syr2014.
- 67.Benda NM, Eijsvogels TM, Van Dijk AP, Bellersen L, Thijssen DH, Hopman MT, et al. Altered core and skin temperature responses to endurance exercise in heart failure patients and healthy controls. Eur J Prev Cardiol. 2016;23:137–44. doi: 10.1177/2047487315574281. [DOI] [PubMed] [Google Scholar]
- 68.Pullen PR. The Benefits of Yoga Therapy for Heart Failure Patients [Dissertation]. Appendix B. Atlanta (GA): Georgia State University; 2009. [Last accessed on 2017 Aug 12]. Available from: http://www.scholarworks.gsu.edu/kin_health_diss/2/. [Google Scholar]
- 69.Olex S, Newberg MD, Andrew B, Figueredo MD, Vincent M. Meditation: Should a cardiologist care? Cardiology Faculty Papers Paper 29. 2013. [Last accessed on 2017 Aug 12]. Available from: http://www.jdc.jefferson.edu/cardiologyfp/29 .
- 70.Jevning R, Wallace RK, Beidebach M. The physiology of meditation: A review. A wakeful hypometabolic integrated response. Neurosci Biobehav Rev. 1992;16:415–24. doi: 10.1016/s0149-7634(05)80210-6. [DOI] [PubMed] [Google Scholar]
- 71.Young JD, Taylor E. Meditation as a voluntary hypometabolic state of biological estivation. News Physiol Sci. 1998;13:149–53. doi: 10.1152/physiologyonline.1998.13.3.149. [DOI] [PubMed] [Google Scholar]
- 72.Emani S, Binkley PF. Mind-body medicine in chronic heart failure: A translational science challenge. Circ Heart Fail. 2010;3:715–25. doi: 10.1161/CIRCHEARTFAILURE.110.951509. [DOI] [PubMed] [Google Scholar]
- 73.Sullivan MJ, Wood L, Terry J, Brantley J, Charles A, McGee V, et al. The Support, Education, and Research in Chronic Heart failure study (SEARCH): A mindfulness-based psychoeducational intervention improves depression and clinical symptoms in patients with chronic heart failure. Am Heart J. 2009;157:84–90. doi: 10.1016/j.ahj.2008.08.033. [DOI] [PubMed] [Google Scholar]
- 74.Schneider RH, Grim CE, Rainforth MV, Kotchen T, Nidich SI, Gaylord-King C, et al. Stress reduction in the secondary prevention of cardiovascular disease: Randomized, controlled trial of transcendental meditation and health education in blacks. Circ Cardiovasc Qual Outcomes. 2012;5:750–8. doi: 10.1161/CIRCOUTCOMES.112.967406. [DOI] [PMC free article] [PubMed] [Google Scholar]


