Abstract
Background:
Performing cervical laminoplasty after wide laminectomy may be technically demanding. The unique technique of cervical lift-up laminoplasty using titanium basket plates was applied for the reconstruction of cervical laminae after wide laminectomy for the resection of intradural tumors.
Materials and Methods:
This technical study included 14 cases that could be followed periodically for at least 6 months after surgery. Participants were 8 male and 6 female, with a mean age of 41.6 years (range, 13–71 years). Tumors were intramedullary in 11 cases and extramedullary in 3 cases. After resection of intradural tumors, custom-designed titanium baskets were fitted to expand the spinal canal. Combining baskets of different sizes are also possible for each side at one level. A mixture of hydroxyapatite granules and collagen was packed into the basket. The reconstructed posterior laminae were secured using titanium mini plates. The fascia of the paravertebral muscles was sutured to the spino-ligamentous complex to further stabilize the posterior elements of the cervical spine.
Results:
No wounds or implant problems requiring revision surgery were recognized. Imaging analysis demonstrated no significant change in C2–C7 angle cervical range of motion between before and after surgery, suggesting sequential spinal stability at the base of the laminae.
Conclusions:
This technical note suggests that cervical lift-up laminoplasty with titanium basket plates appears practical and useful as a procedure to reconstruct cervical laminae after wide laminectomy.
Keywords: Cervical spine, laminoplasty, lift-up, spinal intramedullary tumor, titanium basket
INTRODUCTION
Cervical laminoplasty is commonly performed for posterior cervical decompression. A variety of procedures have been developed to obtain a reconstruction of posterior cervical elements.[1,2,3,4,5,6,7,8,9,10,11] Cervical laminoplasty appears effective on the maintenance of spinal curvature and range of motion (ROM) even long after surgery although the efficacy of this method has remained contentious.[12,13,14] However, performing cervical laminoplasty after wide laminectomy for intradural procedures such as resection of intradural tumors may be technically demanding.
We have developed a unique method of cervical laminoplasty using a hydroxyapatite (HA) block, in what we term “lift-up laminoplasty,” and have reported the advantages in the previous publications.[3,6,15] Here, we modified our technique of cervical lift-up laminoplasty to use titanium basket plates and created an integrated laminoplasty of the cervical spine. The mixture of HA granules and collagen was packed into the basket to be integrated with the lamina edge. The procedure is not particularly complicated and appears easier. We applied this technique for the reconstruction of cervical laminae after the resection of intradural tumors and examined the postoperative imaging results for cervical curvature and ROM.
MATERIALS AND METHODS
Patient population
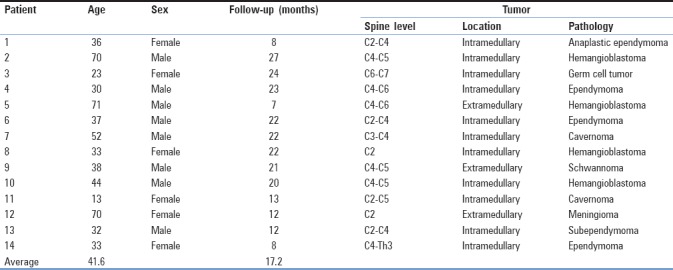
Cervical lift-up laminoplasty with titanium basket plates was introduced in our institute in September 2014 and was applied for the reconstruction of cervical laminae after the resection of intradural tumors. This study of cervical lift-up laminoplasty with titanium basket plates included 14 cases that could be followed periodically for at least 6 months after surgery. Participants were 8 male and 6 female, with a mean age of 41.6 years (range, 13–71 years). Tumors were intramedullary in 11 cases and extramedullary in three cases. Recurrent cases were excluded from this study. Patient characteristics are summarized in Table 1.
Table 1.
Patient characteristics
Surgical technique
The surgical technique for lift-up laminoplasty of the cervical spine has been described previously.[3,6,15] Briefly, after standard exposure of the posterior cervical spine with preservation of the spino-ligamentous complex, osteotomy of the laminae was carried out by transecting the laminae using a high-speed drill. The yellow ligaments were sharply dissected at the upper and lower level of the laminotomy, and the laminae removed en bloc. Additional resection of the lamina edge or posterior foraminotomy was performed in selected cases. After resection of intradural tumors, custom-designed titanium baskets (AMMTEC, Tokyo, Japan) were fitted to expand the spinal canal. The minimum size of a basket is 8 mm long. The width of a basket is 3 mm for the C3–C7 subaxial spine or 4 mm for C2. Combining baskets of different sizes are also possible for each side at one level. A mixture of HA granules and collagen (Refit; HOYA Technosurgical Corporation, Tokyo, Japan) was packed into the basket. The reconstructed posterior laminae were secured using titanium mini plates [Figure 1]. The fascia of the paravertebral muscles was sutured to the spino-ligamentous complex to further stabilize the posterior elements of the cervical spine. A soft collar was applied several weeks after surgery. No other external orthosis was applied after surgery.
Figure 1.
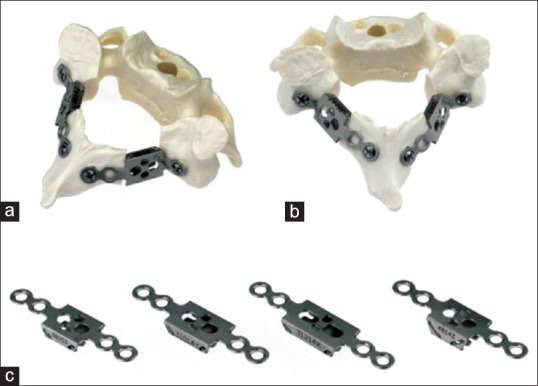
Photograph showing the cervical lift-up laminoplasty with titanium basket plates using a plastic model of the spine (a and b). Basket plates are titanium-6 aluminum-4 vanadium extra-low interstitial alloy consisting of a box-shaped cage available in different sizes (c)
Image analysis
All patients underwent comprehensive evaluations before and after surgery and completed a minimum 6 months of follow-up after surgery. Radiological evaluations included the C2–C7 angle of spinal curvature and ROM of the cervical spine on plain radiography and osseous integrity on computed tomography.[16,17] All radiological evaluations were performed using a computerized medical records system (EGMAIN-EX).
Statistical analysis
All data are expressed as means ± standard deviation. JMP version 9.0 Software (SAS Institute, Cary, NC, USA) was used for all statistical analyses in the present study. The paired t-test was used to assess differences in C2–C7 angle of spinal curvature and ROM of the cervical spine between before and after surgery.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of clinical data were followed in the present study. This comprehensive analysis of surgery-related outcomes was approved by the Institutional Ethics Committee. Informed consent for the use of titanium basket plates was obtained from the patient before surgery.
RESULTS
In the 14 patients, a total of 32 cervical laminae were reconstructed after resection of intradural tumors. Mean operation time including resection of the tumor was 473 min (range, 250–637 min). Mean estimated blood loss including the resection of the tumor was 261 ml (range, 40–700 ml). No wound or implant problems requiring revision surgery were encountered.
Cervical spine curvature before surgery was lordotic in 12 patients, straight in 0, S-shaped in 1, and kyphotic in 1. Postoperative image analysis demonstrated that cervical spine curvature after surgery remained lordotic in 12 patients, straight in 0, S-shaped in 0, and became kyphotic in 2. Average C2–C7 angle did not change significantly after surgery. Average neck ROM between flexion and extension was 40.9° before surgery and remained 46.8° after surgery [Figure 2]. The data from image analysis are summarized in Table 2. Image analysis using computed tomography suggested sequential spinal stability at the base of the laminae [Figure 3].
Figure 2.
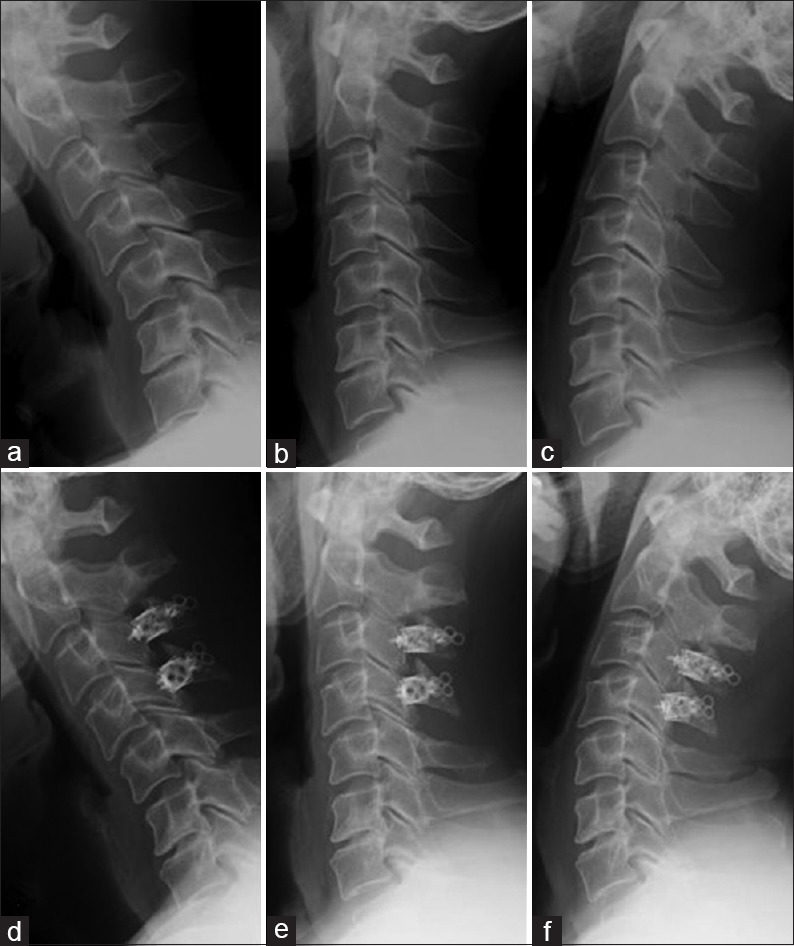
Lateral radiographs of the cervical spine (Patient 7) showing maintenance of C2–C7 angle and range of neck motion from before surgery (a-c) to after surgery (d-f)
Table 2.
Summary of image analysis
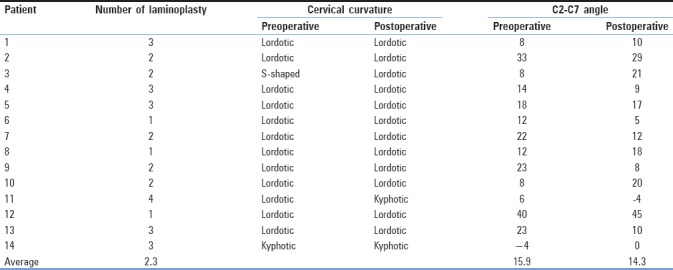
Figure 3.
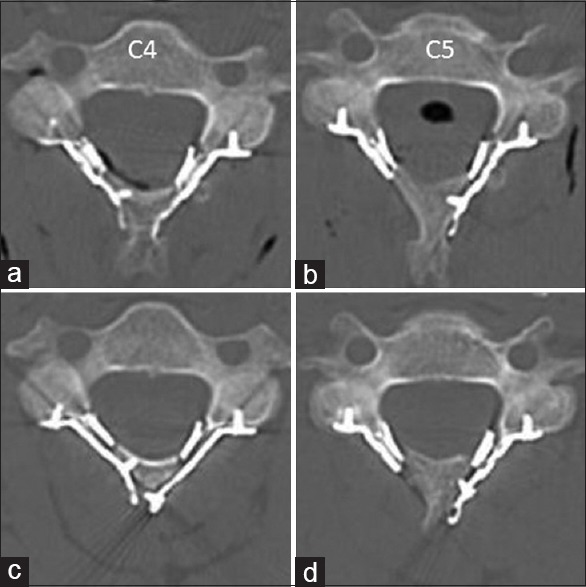
Image analysis using computed tomography (Patient 10) suggesting sequential osseous stability at the base of the laminae. (a and b): Early after surgery; (c and d): 6 months after surgery
Illustrative case 1
A 36-year-old woman was admitted with acute deterioration of a left-sided motor-weakness. Functional assessment before surgery suggested Grade 5 in the modified McCormick functional schema.[18,19] Magnetic resonance imaging (MRI) before surgery demonstrated the existence of intramedullary tumor at the C1–C4 level [Figure 4a]. Surgical verification revealed the anaplastic nature of the tumor, and partial resection was accomplished without trouble. Pathological examination of the tumor led to a diagnosis of intramedullary anaplastic ependymoma. Cervical lift-up laminoplasty with titanium basket plates for C2–C4 was completed [Figure 4b and d]. The patient underwent postoperative treatment with local radiation and chemotherapy [Figure 4c]. The postoperative course was uneventful, and functional assessment early after surgery suggested Grade 4 of the modified McCormick functional schema. During follow-up, image analysis demonstrated the maintenance of cervical curvature.
Figure 4.

Illustrative case (Patient 1). (a and b): Before surgery; (c and d): After surgery and radiation
Illustrative case 2
A 23-year-old woman was admitted with acute deterioration of tetraparesis. Functional assessment before surgery suggested Grade 5 of the modified McCormick functional schema. MRI before surgery demonstrated an intramedullary tumor at the C6–C7 level with extensive intramedullary signal change [Figure 5a]. Surgical verification revealed the anaplastic nature of the tumor, and partial resection of the tumor was accomplished without trouble. Pathological examination led to the diagnosis of intramedullary germ cell tumor. Cervical lift-up laminoplasty with titanium basket plates of C6–C7 was completed [Figure 5b and d]. The patient underwent postoperative radiotherapy of the whole brain and spine and chemotherapy [Figure 5c]. The postoperative course was uneventful, and functional assessment early after surgery suggested Grade 4 of the modified McCormick functional schema. During follow-up, image analysis demonstrated the improvement of the cervical curvature.
Figure 5.
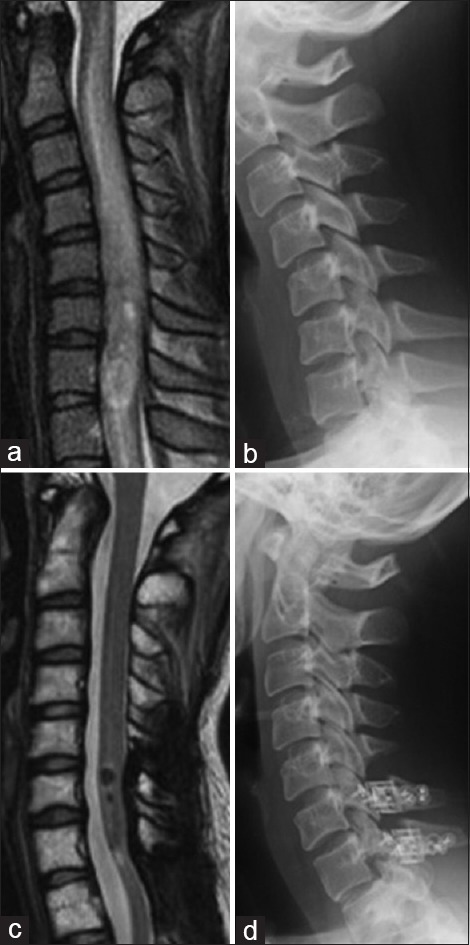
Illustrative case (Patient 3). (a and b): Before surgery; (c and d): After surgery and radiation
DISCUSSION
Although a variety of technical modifications are available for cervical laminoplasty, such as unilateral open-door, bilateral open-door, HA spacer or titanium plate, and screws,[1,2,3,4,5,6,7,8,9,10,11] these procedures may not be entirely suitable for the reconstruction of cervical laminae after resection of an intradural tumor. Wide laminectomy is helpful for surgeons to secure a sufficient working space for intradural procedure but may result in spinal deformity, instability, or aggravation of neck ROM.[20,21,22,23] Our previous reports described our lift-up technique of cervical laminoplasty using HA block.[3,6,15] Resected laminae were completely secured in the original position using HA block and titanium plates after wide laminectomy. The advantages of cervical lift-up laminoplasty are the provision of a wide space for intradural procedures and reconstruction of posterior osseous elements of the cervical spine. The degree of lift-up can be modified by changing the size of the HA block. Furthermore, expansive duraplasty was easily secured with the reconstructed laminae.[15] On the other hand, the procedure is not necessarily simple or easy, and the structure may be complex.
This technical note suggested that cervical lift-up laminoplasty with titanium basket plates can be applied easily and safely after resection of intradural tumors. Reconstructed laminae were assumed to be stable during follow-up, even after postoperative local radiation. Cervical alignment and ROM were well maintained after surgery. As Tani et al. reported, titanium basket plates offer some advantages.[10] The titanium basket plates are universally applicable to both uni- and bi-lateral open-door laminoplasty, not only to lift-up laminoplasty. The malleability of the metal allows the basket to be altered to fit with the laminae. Finally, a lower chance of implant failure such as crack formation associated with HA spacers can be noted. Minimal artifacts on postoperative MRI and computed tomography may be another advantage because the basket consists of a thin titanium alloy.
As mentioned above, we started performing this procedure in September 2014, and the number of cases in which we performed the procedure and the follow-up period was quite limited. Longer-term results for bony fusion and deformity in the postoperative period are thus needed. We will, therefore, continue using this procedure and accumulating and evaluating the results. Furthermore, biomechanical stability of the reconstructed laminae also needs to be carefully examined. This preliminary study, although quite short and including only a small number of cases, suggested that cervical lift-up laminoplasty with titanium basket plates may be clinically practical and represents a valid choice for reconstructing cervical laminae after wide laminectomy.
CONCLUSIONS
The technique of cervical lift-up laminoplasty using titanium basket plates was modified to create an integrated laminoplasty of the cervical spine after resection of intradural tumors. This preliminary analysis suggested that cervical spine curvature and average C2–C7 angle were not markedly changed after surgery. Neck ROM between flexion and extension was maintained from before surgery to after surgery. Image analysis using computed tomography suggested sequential osseous stability at the base of the laminae. Cervical lift-up laminoplasty with titanium basket plates appears practical and useful as a procedure to reconstruct the cervical laminae after wide laminectomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Kawai S, Sunago K, Doi K, Saika M, Taguchi T. Cervical laminoplasty (Hattori's method). Procedure and follow-up results. Spine (Phila Pa 1976) 1988;13:1245–50. [PubMed] [Google Scholar]
- 2.Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, et al. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976) 2001;26:479–87. doi: 10.1097/00007632-200103010-00010. [DOI] [PubMed] [Google Scholar]
- 3.Goto T, Ohata K, Takami T, Nishikawa M, Tsuyuguchi N, Morino M, et al. Hydroxyapatite laminar spacers and titanium miniplates in cervical laminoplasty. J Neurosurg. 2002;97:323–9. doi: 10.3171/spi.2002.97.3.0323. [DOI] [PubMed] [Google Scholar]
- 4.Takayasu M, Takagi T, Nishizawa T, Osuka K, Nakajima T, Yoshida J, et al. Bilateral open-door cervical expansive laminoplasty with hydroxyapatite spacers and titanium screws. J Neurosurg. 2002;96(1 Suppl):22–8. doi: 10.3171/spi.2002.96.1.0022. [DOI] [PubMed] [Google Scholar]
- 5.Tani S, Isoshima A, Nagashima Y, Tomohiko Numoto R, Abe T. Laminoplasty with preservation of posterior cervical elements: Surgical technique. Neurosurgery. 2002;50:97–101. doi: 10.1097/00006123-200201000-00017. [DOI] [PubMed] [Google Scholar]
- 6.Takami T, Ohata K, Goto T, Nishikawa M, Nishio A, Tsuyuguchi N, et al. Lift-up laminoplasty for myelopathy caused by ossification of the posterior longitudinal ligament of the cervical spine. Neurol India. 2004;52:59–63. [PubMed] [Google Scholar]
- 7.Kihara S, Umebayashi T, Hoshimaru M. Technical improvements and results of open-door expansive laminoplasty with hydroxyapatite implants for cervical myelopathy. Neurosurgery. 2005;57(4 Suppl):348–56. doi: 10.1227/01.neu.0000176646.88909.82. [DOI] [PubMed] [Google Scholar]
- 8.Chiba K, Ogawa Y, Ishii K, Takaishi H, Nakamura M, Maruiwa H, et al. Long-term results of expansive open-door laminoplasty for cervical myelopathy – Average 14-year follow-up study. Spine (Phila Pa 1976) 2006;31:2998–3005. doi: 10.1097/01.brs.0000250307.78987.6b. [DOI] [PubMed] [Google Scholar]
- 9.Kim P, Murata H, Kurokawa R, Takaishi Y, Asakuno K, Kawamoto T, et al. Myoarchitectonic spinolaminoplasty: Efficacy in reconstituting the cervical musculature and preserving biomechanical function. J Neurosurg Spine. 2007;7:293–304. doi: 10.3171/SPI-07/09/293. [DOI] [PubMed] [Google Scholar]
- 10.Tani S, Suetsua F, Mizuno J, Uchikado H, Nagashima H, Akiyama M, et al. New titanium spacer for cervical laminoplasty: Initial clinical experience. Technical note. Neurol Med Chir (Tokyo) 2010;50:1132–6. doi: 10.2176/nmc.50.1132. [DOI] [PubMed] [Google Scholar]
- 11.Kurokawa R, Kim P. Cervical laminoplasty: The history and the future. Neurol Med Chir (Tokyo) 2015;55:529–39. doi: 10.2176/nmc.ra.2014-0387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heller JG, Edwards CC, 2nd, Murakami H, Rodts GE. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: An independent matched cohort analysis. Spine (Phila Pa 1976) 2001;26:1330–6. doi: 10.1097/00007632-200106150-00013. [DOI] [PubMed] [Google Scholar]
- 13.Ratliff JK, Cooper PR. Cervical laminoplasty: A critical review. J Neurosurg. 2003;98:230–8. doi: 10.3171/spi.2003.98.3.0230. [DOI] [PubMed] [Google Scholar]
- 14.Duetzmann S, Cole T, Ratliff JK. Cervical laminoplasty developments and trends, 2003-2013: A systematic review. J Neurosurg Spine. 2015;23:24–34. doi: 10.3171/2014.11.SPINE14427. [DOI] [PubMed] [Google Scholar]
- 15.Goto T, Ohata K, Takami T, Nishikawa M, Nishio A, Morino M, et al. Prevention of postoperative posterior tethering of spinal cord after resection of ependymoma. J Neurosurg. 2003;99:181–7. doi: 10.3171/spi.2003.99.2.0181. [DOI] [PubMed] [Google Scholar]
- 16.Takeshita K, Murakami M, Kobayashi A, Nakamura C. Relationship between cervical curvature index (Ishihara) and cervical spine angle (C2–7) J Orthop Sci. 2001;6:223–6. doi: 10.1007/s007760100038. [DOI] [PubMed] [Google Scholar]
- 17.Scheer JK, Tang JA, Smith JS, Acosta FL, Jr, Protopsaltis TS, Blondel B, et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg Spine. 2013;19:141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 18.McCormick PC, Torres R, Post KD, Stein BM. Intramedullary ependymoma of the spinal cord. J Neurosurg. 1990;72:523–32. doi: 10.3171/jns.1990.72.4.0523. [DOI] [PubMed] [Google Scholar]
- 19.Takami T, Naito K, Yamagata T, Kawahara S, Ohata K. Surgical outcomes of posterolateral sulcus approach for spinal intramedullary tumors: Tumor resection and functional preservation. World Neurosurg. 2017 doi: 10.1016/j.wneu.2017.08.127. pii: S1878-8750(17)31428-6. [DOI] [PubMed] [Google Scholar]
- 20.Inoue A, Ikata T, Katoh S. Spinal deformity following surgery for spinal cord tumors and tumorous lesions: Analysis based on an assessment of the spinal functional curve. Spinal Cord. 1996;34:536–42. doi: 10.1038/sc.1996.97. [DOI] [PubMed] [Google Scholar]
- 21.Asazuma T, Nakamura M, Matsumoto M, Chibo K, Toyama Y. Postoperative changes of spinal curvature and range of motion in adult patients with cervical spinal cord tumors: Analysis of 51 cases and review of the literature. J Spinal Disord Tech. 2004;17:178–82. doi: 10.1097/00024720-200406000-00003. [DOI] [PubMed] [Google Scholar]
- 22.Fassett DR, Clark R, Brockmeyer DL, Schmidt MH. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006;20:E2. [PubMed] [Google Scholar]
- 23.Joaquim AF, Riew KD. Management of cervical spine deformity after intradural tumor resection. Neurosurg Focus. 2015;39:E13. doi: 10.3171/2015.5.FOCUS15134. [DOI] [PubMed] [Google Scholar]


