Abstract
Background:
Normal sagittal cervical alignment has been associated with improved outcome after anterior cervical discectomy and fusion (ACDF).
Objective:
The aim of this study is to identify alterations of cervical sagittal balance parameters after single-level ACDF and assess correlations with postoperative functionality.
Methods:
A retrospective chart review was performed between January 2010 and January 2014 to identify adult patients with no previous cervical spine surgery who underwent ACDF at any one level between C2 and C7 for the single-level degenerative disease. Tumor, infection, and trauma cases were excluded from the study. For the included cases, the following data were recorded preoperatively and 6 months–1 year after surgery: sagittal balance-marker measurements of the C1–C2 angle, C2–C7 angle, C7 slope, segmental angle at the operated level, and sagittal vertical axis (SVA) distance between C2 and C7, as well as the neck disability index and visual analog scale of pain.
Results:
The present study included 47 patients (average age: 51.2 years; range: 28–86 years). A moderate negative correlation between a smaller C2–C7 angle and the presence of right arm pain before treatment was found (P = 0.0281). Postoperatively, functionality scores significantly improved in all patients. C1–C2 angle increased with statistical significance (P = 0.0255). C2–C7 angle, segmental angle, C7 slope, and SVA C2–C7 distance did not change with statistical significance after surgery. C7 slope significantly correlated with overall cervical sagittal balance (P < 0.05).
Conclusions:
Single-level ACDF significantly increases upper cervical lordosis (C1–C2) without significantly changing lower cervical lordosis (C2–C7). The C7 slope is a significant marker of overall cervical sagittal alignment (P < 0.05).
Keywords: Anterior spine, cervical myelopathy, degenerative disease, radiculopathy, sagittal alignment, sagittal balance
INTRODUCTION
Degenerative cervical pathologies such as spondylosis and spondylolisthesis are caused mainly by disc degeneration, hypertrophic facet joints, and rotational forces in the cervical spine. Symptoms such as cervical pain, deteriorating function, and in severe cases of the degenerative disease, loss of forward gaze, are signs of significant changes in cervical lordosis.[1] Usually, these degenerative changes indicate the presence of cervical spondylotic myelopathy and cervical kyphosis.[2,3,4,5,6] Cervical spondylotic myelopathy has a strong correlation with cervical sagittal alignment as dynamic magnetic resonance imaging studies have proven.[7,8] In addition, cervical kyphosis may develop after multilevel laminectomies and in conjunction with diagnoses of infection, trauma, degenerative disorders, and tumors.[9] Other factors such as decreased bone density, disc pathologies, and thoracolumbar sagittal imbalance may be related to the appearance of cervical kyphotic changes.[10,11,12,13,14,15,16,17] The appearance of disorders in cervical alignment is an important element in recognizing defects in global spine imbalances.[13] Cervical imbalance causes morphological changes in the spinal cord that lead to microvasculopathy, neuronal degeneration, and impairment of function.[18]
Anterior cervical discectomy and fusion (ACDF) is a routinely performed surgical procedure for the treatment of benign structural anomalies of the cervical spine such as disk protrusions, cervical spondylosis, foraminal stenosis, and bony abnormalities. During the last decade, the study of cervical sagittal balance became highlighted as it links functionality and surgical outcome.[3,5,6,19,20,21,22,23,24,25,26] Cervical sagittal balance measurements include several radiological parameters; among these are C2–C7 lordosis, C1–C2 lordosis, sagittal vertical axis (SVA), segmental sagittal alignment at the operated level, and C7 and T1 slope.[5,10,11,14,20,24,25,27,28,29,30,31,32,33,34,35,36,37] The T1 slope is correlated with overall spine sagittal balance, including cervical spine balance.[27,29,38]
The aim of our retrospective study was to record the changes that single-level ACDF induces in the cervical sagittal alignment of patients with cervical radiculopathy or cervical myelopathy resulting from degenerative disc disease. In addition, we tried to relate these cervical sagittal alignment changes to patient-reported functional outcome scores, including the visual analog scale (VAS) and neck disability index (NDI). This comparison could provide valuable clinical information regarding the manifestations of cervical sagittal imbalance in patients treated for cervical myelopathy and/or radiculopathy with single-level ACDF.
METHODS
Population, setting
This retrospective chart review was conducted after obtaining the Institutional Review Board approval. The approval included a Health Insurance Portability and Accountability Act waiver of patient authorization owing to the retrospective nature of and use of de-identified data in this study. We included adult patients (>18-year-old) who underwent single-level ACDF for cervical radiculopathy and/or myelopathy for the first time between January 2010 and January 2014. All operations were right-sided Smith-Robinson approaches, performed at either of our two affiliated hospitals.
Surgeons used a polyetheretherketone (PEEK) anterior interbody cage with an allograft and an anterior plate in all procedures. VAS and NDI scores, as well as neutral standing cervical X-rays from before and at 6–12 months after surgery were available for these patients. Trauma, infection, and tumor cases were excluded from the study.
Data collection
Data collected included demographics and body mass index (BMI). In addition data collection included were preoperative and postoperative neurological examination findings and the Health-Related Quality of Life (HRQoL) scores for the VAS and NDI. Measurements were obtained of cervical sagittal alignment markers from each patient's pre-operative and post-operative standing cervical X-ray studies, including C7 slope, C1–C2 cervical lordosis (C1–C2 angle), C2–C7 cervical lordosis (C2–C7 angle), C2–C7 SVA (the horizontal distance between the plumb line of C2 and C7), and segmental angle (the angle between the inferior endplate of the upper vertebrae and the superior endplate of the next lower vertebrae, forming the disc space). Fusion status and surgical complications were also reviewed and recorded from medical records, X-rays performed during follow-up visits, and cervical spine CT scans obtained at 1 year after surgery.
Radiological measurements
All radiographic measurements were made using the picture archiving and communication system (Synapse, Fujifilm, Valhalla, New York). To ensure reproducibility and consistency of cervical sagittal alignment parameters, only standing neutral cervical X-rays were used before surgery and 6–12 months after surgery. Furthermore, by extending our measurements out for this length of time after surgery, we managed to achieve NDI and VAS scores that were not negatively affected by immediate postoperative pain.
We measured the lordosis between the C1 and C2 vertebrae, which reflects lordosis of the upper cervical spine, and between the C2 and C7 vertebrae, which reflects lower cervical lordosis. The C1–C2 lordosis measurement was performed by drawing the first-line parallel to the inferior endplate of C2 and the second line from the anterior tubercle of C1 to the posterior margin of the spinous process [Figure 1]. C2–C7 lordosis was measured by drawing a line parallel to the inferior endplate of C2 and a second-line parallel to the inferior endplate of C7. Perpendicular lines were then drawn at right angles to each of the previous two lines (Cobb technique).
Figure 1.
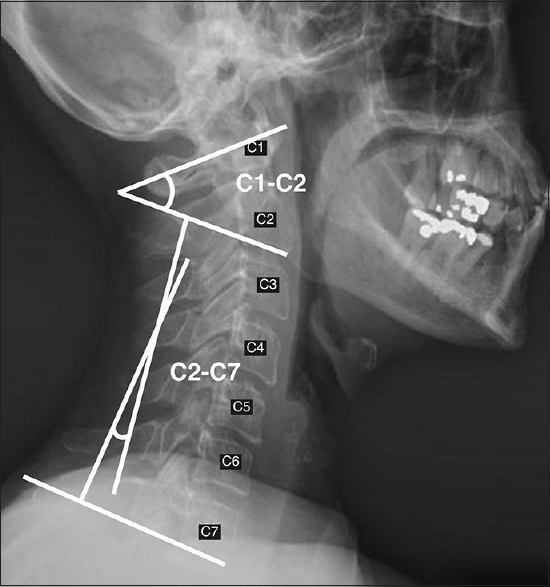
Lateral cervical spine X-ray. C1–C2 (upper cervical lordosis) and C2–C7 (lower cervical lordosis-by Cobb technique) angles are indicated
The angle formed between the perpendicular lines represented the cervical lordosis angle of C2–C7 [Figure 1]. The functional segmental angle was measured by drawing lines from the superior and inferior vertebral body to the level where the fusion was performed [Figure 2]. The C7 slope was calculated by measuring the angle formed by the horizontal line to the C7 vertebra and the parallel line to the superior endplate of the C7 vertebra [Figure 3]. The cervical SVA was measured as the horizontal distance between the plumb line of the C2 and C7 vertebrae [Figure 4]. All measurements were performed by two of the coauthors.
Figure 2.
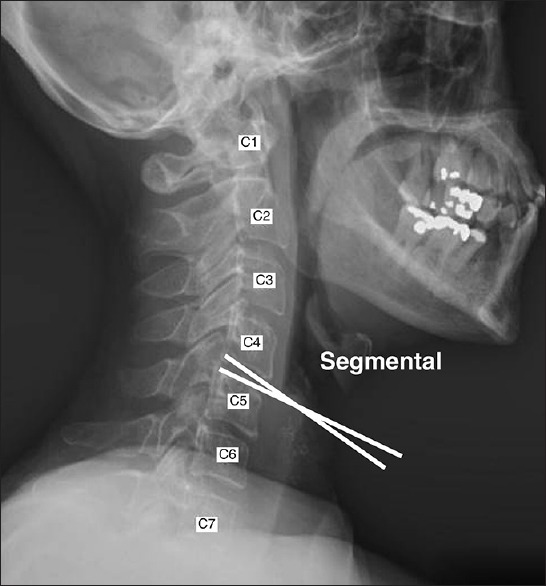
Lateral cervical spine X-ray. Formation of the segmental angle is indicated by parallel lines to the endplates of the involved vertebrae
Figure 3.

Lateral cervical spine X-ray. Formation of the C7 slope is indicated by the horizontal line at that level and the line that is parallel to the C7 superior endplate
Figure 4.

Lateral cervical spine X-ray. The sagittal vertical axis is calculated as the distance between the gravity centers of the C2 and C7 vertebrae
Lordosis angles were thought to be negative and kyphosis angles were thought to be positive in all our performed measurements (C1–C2, C2–C7, and segmental angle). C2–C7 angles were classified as Lordotic angles: <-10, Neutral: -10-0, kyphotic >0 according to the value of C2– C7 sagittal cervical alignment. Segmental angle values were categorized into lordotic (segmental angle < 0), neutral (segmental angle = 0), and kyphotic (segmental angle > 0).
Statistical analysis
The SAS® statistical package (version 9.3; SAS Institute, Cary, North Carolina, USA) was used for the statistical analysis. Radiographic measures and normal distribution of HRQoL scores were determined using the Shapiro–Wilk test. The paired t-test (for normally distributed data) or the Wilcoxon signed-rank test (for abnormally distributed data) was used to compare the distributions of the variables before and after treatment. When the value of P < 0.05, the distribution of the variable was significantly different before and after treatment. Correlation between radiographic measures and HRQoL scores before and after treatment and changes before and after treatment was evaluated using Spearman correlation coefficient. When the P < 0.05, it was concluded that the correlation was statistically significant. Correlations and changes between angles before and after treatment were evaluated using Spearman correlation coefficient. When the P < 0.05, the correlation was considered statistically significant.
RESULTS
Descriptive data
A total of 47 patients were included in this study. The average age of these patients was 51.2 ± 14.9 years (standard deviation [SD]), (range: 28–86 years); 27 (57.5%) were women. The average BMI was 28.9 ± 5.5 (SD), ranging from 20.40 to 42.00 [Table 1]. Nineteen (40.4%) patients had cervical myelopathy, and 28 (59.6%) had cervical degenerative disc disease. Eleven patients (23.4%) were operated on at the C3–C4 level, five patients (10.6%) at the C4–C5 level, 21 patients (44.7%) at the C5–C6 level, and 10 patients (21.3%) at the C6–C7 level. According to our data, the average follow-up period was 212 ± 56 days.
Table 1.
Summary statistics of health-related quality of life scale scores
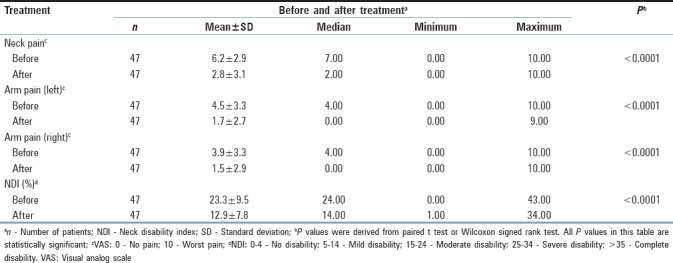
The HRQoL scores, including VAS for neck and arm pain and NDI, significantly changed after treatment [Table 1]. The mean value for VAS neck pain was 6.2 preoperatively and decreased to 2.8 after surgery (P< 0.0001). The mean value for VAS right arm pain decreased from 3.9 to 1.5 and for left arm pain from 4.5 to 1.7 (P< 0.001). The preoperative mean value for NDI was 23.3 and was reduced postoperatively to 12.9 (P< 0.0001) showing improvement from moderate-to-mild disability. There was a moderate negative correlation (−0.32046) between the C2–C7 angle and the presence of VAS right arm pain (P = 0.0281) before treatment [Figure 5]. There was no statistical correlation between these variables after treatment.
Figure 5.
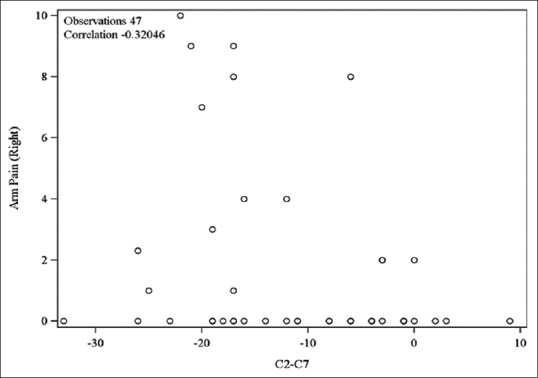
Scatter plot of the moderate negative correlation (P = 0.0281) between the presence of right arm pain and a smaller C2–C7 angle before treatment in 33 of 47 patients (14 patients did not have right arm pain, i.e., pain score of 0)
Overall lordosis and sagittal balance changes
According to our data, the cervical spine was lordotic in 30 patients, neutral in 16, and kyphotic in 1 before surgery. Approximately 6 months to 1 year after the procedure, the cervical spine was lordotic in 25 patients, neutral in 19, and kyphotic in 3. Preoperatively, the segmental angle was lordotic in 41 patients, neutral in 2, and kyphotic in 4. After the ACDF procedure, there were 44 patients with a lordotic segmental angle, 1 with a neutral segmental angle, and 2 with a kyphotic segmental angle.
The C1–C2 angle was significantly changed 6 months to 1 year after the surgical procedure [Table 2]. The mean preoperative C1–C2 value was −34.6°; after surgery, the mean value was-36.3° (P = 0.0255). Pre- and post-operative mean values for the C2–C7 angle were −13.6 and −11.0, respectively, which translates to a minor reduction in lordosis. The mean value of the segmental angle was −2.8 before surgery and −4.8 after surgery. C7 slope also changed from a mean of −26.70 to −27.7; although, this change was insignificant (P< 0.3143). There was a minimal change in SVA mean values, from 2.90 preoperatively to 3.0 postoperatively.
Table 2.
Summary statistics of radiographic measures before and after treatmenta
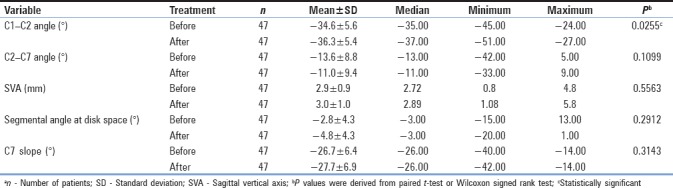
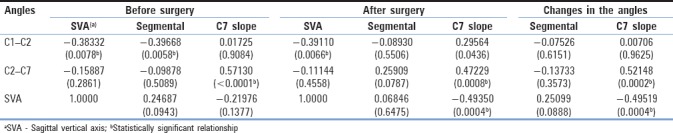
Statistical analysis also revealed a moderate negative correlation between the C1 and C2 angle and the SVA (r = 0.38332) as well as a moderate negative correlation between the C1 and C2 angle and the segmental angle before surgery (r = 0.39688) [Table 3]. Furthermore, the preoperative C2–C7 angle was associated with the preoperative C7 slope with a moderate positive correlation (r = 0.5713) [Table 3]. After surgery, C7 slope was associated with overall cervical lordosis (C1–C2 and C2–C7) with a moderate positive correlation (r[C1–C2]0.29564, r[C2–C7]0.47229) as well as with the SVA distance with a moderate negative correlation (r = 0.49350) [Table 3]. Regarding the existence of correlations between postoperative changes of the studied angles, statistical analysis showed a moderate negative correlation between C7 slope and SVA distance (r = 0.49519) and a moderate positive correlation between C7 slope and the C2–C7 angle (r = 0.52148) [Table 3].
Table 3.
Correlation coefficients and changes in angles before and after surgery
DISCUSSION
Key results and interpretation
Cervical sagittal alignment has not been studied as extensively as alignment in conjunction with thoracolumbar deformities. There are several variations of normal cervical sagittal balance in the literature.[10] In general, the C1–C2 angle is the parameter that is most representative of cervical sagittal lordosis and is responsible for 75% of cervical sagittal balance overall.[10,29,39,40] In addition, the segmental angle has variations depending on the involved level, as Hardacker et al. noted in their study of asymptomatic adult volunteers.[39] Furthermore, cervical sagittal balance is influenced by age, according to the study of Gore et al. in asymptomatic men and women.[41]
In this study, C7 slope proved to be of great importance as a marker of cervical sagittal alignment as it was linked to C2–C7 angle measurements before and after treatment. The C7 slope was also significantly related to upper cervical lordosis (C1–C2 level) as well as the SVA after treatment. Moreover, changes in C7 slope were significantly associated with changes in both C2–C7 angle and SVA. This finding is also documented in other studies. According to Núñez-Pereira et al., C7 slope is a useful marker not only for occipitocervical alignment but also for overall sagittal alignment.[28]
Several studies have attempted to correlate functional outcome scores such as NDI, Short Form-36 physical component summary scores, and modified Japanese Orthopedic Association scores with postoperative cervical sagittal balance.[3,5,6,13,20,21,22,35,42,43,44] According to these studies, changes of cervical sagittal alignment subsequent to a cervical spine procedure may have a positive or a negative influence on functionality. We used the NDI and VAS pain scale for the clinical evaluation of our patients because this was a retrospective study and these were the forms that our patients routinely completed.
Investigators of recent studies of single- level ACDF did not find a significant relationship between functional outcome scores and segmental and/or cervical sagittal alignment expressed by the C2–C7 angle. Faldini et al. performed a prospective study regarding the efficacy of the PEEK anatomical cervical cage and allograft bone in single-level ACDF.[45] They found that cervical lordosis increased 6 months after surgery from −15.8° to −20.9°; and at 1 year after surgery, it dropped to −18.5°. They did not find any correlation with functional outcome scores. In their comparison study regarding the effect of lordotic or parallel cage use after ACDF on functionality and cervical sagittal balance, Villavicencio et al. concluded that the maintenance or improvement of segmental lordosis may be linked to better functional outcome scores.[43] Another significant parameter of cervical sagittal balance is SVA, which has been associated with reduced functionality expressed by the NDI score when it exceeds 4 cm.[5]
In this study, the C1–C2 angle was significantly changed 6 months to 1 year after the surgical procedure. There was a reduction in C2–C7 lordosis 6 months to 1 year after surgery, although it was statistically insignificant. Moreover, SVA, C2–C7, and segmental angle were changed after surgery but not significantly. The increase in C1–C2 upper cervical lordosis could be explained by the existence of a negative correlation to C2–C7 lordosis, as documented in the literature.[28] Furthermore, Kim et al. concluded that ACDF can provoke changes in alignment of the operative level as well as indirect changes in the upper cervical sagittal alignment expressed by regional slope angles.[46] The C2–C7 cervical lordosis was reduced in our patients, although this change was not statistically significant. In addition, the segmental angle increased to more lordotic values resulting in better functional outcome scores.
With respect to functionality outcome scores in our patients, there was a correlation between the presence of right arm pain and C2–C7 lordosis before treatment. Patients with smaller overall C2–C7 lordosis had more pain in their right arm than the rest of the patients. This is an indication that restoration of overall lordosis should be one of the goals for spine surgeons to improve the functional outcome scores of their patients.
Limitations
The study has limitations. It has a retrospective design and a small number of patients.
CONCLUSIONS
In this study, we found that the ACDF procedure improved patient functionality significantly. Furthermore, upper cervical lordosis, represented by the C1–C2 angle, was affected significantly. On the contrary, lower cervical lordosis did not change significantly; although, it decreased. Furthermore, we found that C7 slope was a major marker of overall cervical alignment, as supported by other studies. Regarding functionality after the ACDF procedure, restoration of local and regional cervical lordosis has a significant impact on the neck and arm pain.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Matsunaga S, Sakou T, Sunahara N, Oonishi T, Maeda S, Nakanisi K, et al. Biomechanical analysis of buckling alignment of the cervical spine.Predictive value for subaxial subluxation after occipitocervical fusion. Spine (Phila Pa 1976) 1997;22:765–71. doi: 10.1097/00007632-199704010-00011. [DOI] [PubMed] [Google Scholar]
- 2.Steinmetz MP, Stewart TJ, Kager CD, Benzel EC, Vaccaro AR. Cervical deformity correction. Neurosurg. 2007;60:S90–7. doi: 10.1227/01.NEU.0000215553.49728.B0. [DOI] [PubMed] [Google Scholar]
- 3.Uchida K, Nakajima H, Sato R, Yayama T, Mwaka ES, Kobayashi S, et al. Cervical spondylotic myelopathy associated with kyphosis or sagittal sigmoid alignment: Outcome after anterior or posterior decompression. J Neurosurg Spine. 2009;11:521–8. doi: 10.3171/2009.2.SPINE08385. [DOI] [PubMed] [Google Scholar]
- 4.Yoshimoto H, Ito M, Abumi K, Kotani Y, Shono Y, Takada T, et al. Aretrospective radiographic analysis of subaxial sagittal alignment after posterior C1-C2 fusion. Spine (Phila Pa 1976) 2004;29:175–81. doi: 10.1097/01.BRS.0000107225.97653.CA. [DOI] [PubMed] [Google Scholar]
- 5.Tang JA, Scheer JK, Smith JS, Deviren V, Bess S, Hart RA, et al. The impact of standing regional cervical sagittal alignment on outcomes in posterior cervical fusion surgery. Neurosurg. 2012;71:662–9. doi: 10.1227/NEU.0b013e31826100c9. [DOI] [PubMed] [Google Scholar]
- 6.Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ. Anterior correction of cervical kyphotic deformity: Effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg. 2004;100:13–9. doi: 10.3171/spi.2004.100.1.0013. [DOI] [PubMed] [Google Scholar]
- 7.Roussouly P, Labelle H, Rouissi J, Bodin A. Pre- and post-operative sagittal balance in idiopathic scoliosis: A comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J. 2013;22(Suppl 2):S203–15. doi: 10.1007/s00586-012-2571-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hwang SW, Samdani AF, Tantorski M, Cahill P, Nydick J, Fine A, et al. Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: An effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine. 2011;15:491–6. doi: 10.3171/2011.6.SPINE1012. [DOI] [PubMed] [Google Scholar]
- 9.Matsunaga S, Onishi T, Sakou T. Significance of occipitoaxial angle in subaxial lesion after occipitocervical fusion. Spine (Phila Pa 1976) 2001;26:161–5. doi: 10.1097/00007632-200101150-00010. [DOI] [PubMed] [Google Scholar]
- 10.Scheer JK, Tang JA, Smith JS, Acosta FL, Jr, Protopsaltis TS, Blondel B, et al. Cervical spine alignment, sagittal deformity, and clinical implications: A review. J Neurosurg Spine. 2013;19:141–59. doi: 10.3171/2013.4.SPINE12838. [DOI] [PubMed] [Google Scholar]
- 11.Maeda T, Arizono T, Saito T, Iwamoto Y. Cervical alignment, range of motion, and instability after cervical laminoplasty. Clin Orthop Relat Res. 2002;401:132–8. doi: 10.1097/00003086-200208000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Iizuka H, Nakajima T, Iizuka Y, Sorimachi Y, Ara T, Nishinome M, et al. Cervical malalignment after laminoplasty: Relationship to deep extensor musculature of the cervical spine and neurological outcome. J Neurosurg Spine. 2007;7:610–4. doi: 10.3171/SPI-07/12/610. [DOI] [PubMed] [Google Scholar]
- 13.Smith JS, Shaffrey CI, Lafage V, Blondel B, Schwab F, Hostin R, et al. Spontaneous improvement of cervical alignment after correction of global sagittal balance following pedicle subtraction osteotomy. J Neurosurg Spine. 2012;17:300–7. doi: 10.3171/2012.6.SPINE1250. [DOI] [PubMed] [Google Scholar]
- 14.Guo Q, Ni B, Yang J, Liu K, Sun Z, Zhou F, et al. Relation between alignments of upper and subaxial cervical spine: A radiological study. Arch Orthop Trauma Surg. 2011;131:857–62. doi: 10.1007/s00402-011-1265-x. [DOI] [PubMed] [Google Scholar]
- 15.Roussouly P, Pinheiro-Franco JL. Sagittal parameters of the spine: Biomechanical approach. Eur Spine J. 2011;20(Suppl 5):578–85. doi: 10.1007/s00586-011-1924-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ilharreborde B, Vidal C, Skalli W, Mazda K. Sagittal alignment of the cervical spine in adolescent idiopathic scoliosis treated by posteromedial translation. Eur Spine J. 2013;22:330–7. doi: 10.1007/s00586-012-2493-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Protopsaltis TS, Scheer JK, Terran JS, Smith JS, Hamilton DK, Kim HJ, et al. How the neck affects the back: Changes in regional cervical sagittal alignment correlate to HRQOL improvement in adult thoracolumbar deformity patients at 2-year follow-up. J Neurosurg Spine. 2015;23:153–8. doi: 10.3171/2014.11.SPINE1441. [DOI] [PubMed] [Google Scholar]
- 18.Le Huec JC, Charosky S, Barrey C, Rigal J, Aunoble S. Sagittal imbalance cascade for simple degenerative spine and consequences: Algorithm of decision for appropriate treatment. Eur Spine J. 2011;20(Suppl 5):699–703. doi: 10.1007/s00586-011-1938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fehlings MG, Gray R. Importance of sagittal balance in determining the outcome of anterior versus posterior surgery for cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11:518–9. doi: 10.3171/2009.5.SPINE09182. [DOI] [PubMed] [Google Scholar]
- 20.Roguski M, Benzel EC, Curran JN, Magge SN, Bisson EF, Krishnaney AA, et al. Postoperative cervical sagittal imbalance negatively affects outcomes after surgery for cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2014;39:2070–7. doi: 10.1097/BRS.0000000000000641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C. Cervical spondylotic myelopathy: Surgical results and factors affecting prognosis. Neurosurg. 1998;43:43–9. doi: 10.1097/00006123-199807000-00028. [DOI] [PubMed] [Google Scholar]
- 22.Cabraja M, Abbushi A, Koeppen D, Kroppenstedt S, Woiciechowsky C. Comparison between anterior and posterior decompression with instrumentation for cervical spondylotic myelopathy: Sagittal alignment and clinical outcome. Neurosurg Focus. 2010;28:E15. doi: 10.3171/2010.1.FOCUS09253. [DOI] [PubMed] [Google Scholar]
- 23.Kim SW, Hai DM, Sundaram S, Kim YC, Park MS, Paik SH, et al. Is cervical lordosis relevant in laminoplasty? Spine J. 2013;13:914–21. doi: 10.1016/j.spinee.2013.02.032. [DOI] [PubMed] [Google Scholar]
- 24.Kim SW, Shin JH, Arbatin JJ, Park MS, Chung YK, McAfee PC, et al. Effects of a cervical disc prosthesis on maintaining sagittal alignment of the functional spinal unit and overall sagittal balance of the cervical spine. Eur Spine J. 2008;17:20–9. doi: 10.1007/s00586-007-0459-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K, et al. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976) 1993;18:2167–73. doi: 10.1097/00007632-199311000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech. 2004;17:79–85. doi: 10.1097/00024720-200404000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Knott PT, Mardjetko SM, Techy F. The use of the T1 sagittal angle in predicting overall sagittal balance of the spine. Spine J. 2010;10:994–8. doi: 10.1016/j.spinee.2010.08.031. [DOI] [PubMed] [Google Scholar]
- 28.Núñez-Pereira S, Hitzl W, Bullmann V, Meier O, Koller H. Sagittal balance of the cervical spine: An analysis of occipitocervical and spinopelvic interdependence, with C-7 slope as a marker of cervical and spinopelvic alignment. J Neurosurg Spine. 2015;23:16–23. doi: 10.3171/2014.11.SPINE14368. [DOI] [PubMed] [Google Scholar]
- 29.Lee SH, Kim KT, Seo EM, Suk KS, Kwack YH, Son ES, et al. The influence of thoracic inlet alignment on the craniocervical sagittal balance in asymptomatic adults. J Spinal Disord Tech. 2012;25:E41–7. doi: 10.1097/BSD.0b013e3182396301. [DOI] [PubMed] [Google Scholar]
- 30.Park JH, Cho CB, Song JH, Kim SW, Ha Y, Oh JK, et al. T1 slope and cervical sagittal alignment on cervical CT radiographs of asymptomatic persons. J Korean Neurosurg Soc. 2013;53:356–9. doi: 10.3340/jkns.2013.53.6.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jun HS, Chang IB, Song JH, Kim TH, Park MS, Kim SW, et al. Is it possible to evaluate the parameters of cervical sagittal alignment on cervical computed tomographic scans? Spine (Phila Pa 1976) 2014;39:E630–6. doi: 10.1097/BRS.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 32.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B, et al. Cobb method or harrison posterior tangent method: Which to choose for lateral cervical radiographic analysis. Spine (Phila Pa 1976) 2000;25:2072–8. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 33.Gangnet N, Pomero V, Dumas R, Skalli W, Vital JM. Variability of the spine and pelvis location with respect to the gravity line: A three-dimensional stereoradiographic study using a force platform. Surg Radiol Anat. 2003;25:424–33. doi: 10.1007/s00276-003-0154-6. [DOI] [PubMed] [Google Scholar]
- 34.Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, et al. Standing balance and sagittal plane spinal deformity: Analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–8. doi: 10.1097/BRS.0b013e31817886a2. [DOI] [PubMed] [Google Scholar]
- 35.Ames CP, Blondel B, Scheer JK, Schwab FJ, Le Huec JC, Massicotte EM, et al. Cervical radiographical alignment: Comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38:S149–60. doi: 10.1097/BRS.0b013e3182a7f449. [DOI] [PubMed] [Google Scholar]
- 36.Kim TH, Lee SY, Kim YC, Park MS, Kim SW. T1 slope as a predictor of kyphotic alignment change after laminoplasty in patients with cervical myelopathy. Spine (Phila Pa 1976) 2013;38:E992–7. doi: 10.1097/BRS.0b013e3182972e1b. [DOI] [PubMed] [Google Scholar]
- 37.Cho JH, Ha JK, Kim DG, Song KY, Kim YT, Hwang CJ, et al. Does preoperative T1 slope affect radiological and functional outcomes after cervical laminoplasty? Spine (Phila Pa 1976) 2014;39:E1575–81. doi: 10.1097/BRS.0000000000000614. [DOI] [PubMed] [Google Scholar]
- 38.Lee SH, Son ES, Seo EM, Suk KS, Kim KT. Factors determining cervical spine sagittal balance in asymptomatic adults: Correlation with spinopelvic balance and thoracic inlet alignment. Spine J. 2015;15:705–12. doi: 10.1016/j.spinee.2013.06.059. [DOI] [PubMed] [Google Scholar]
- 39.Hardacker JW, Shuford RF, Capicotto PN, Pryor PW. Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine (Phila Pa 1976) 1997;22:1472–80. doi: 10.1097/00007632-199707010-00009. [DOI] [PubMed] [Google Scholar]
- 40.Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size. A prospective controlled clinical study. Spine (Phila Pa 1976) 1994;19:1611–8. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 41.Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 1986;11:521–4. doi: 10.1097/00007632-198607000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Smith JS, Lafage V, Ryan DJ, Shaffrey CI, Schwab FJ, Patel AA, et al. Association of myelopathy scores with cervical sagittal balance and normalized spinal cord volume: Analysis of 56 preoperative cases from the AOSpine North America myelopathy study. Spine (Phila Pa 1976) 2013;38:S161–70. doi: 10.1097/BRS.0b013e3182a7eb9e. [DOI] [PubMed] [Google Scholar]
- 43.Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, et al. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurg. 2011;68:1309–16. doi: 10.1227/NEU.0b013e31820b51f3. [DOI] [PubMed] [Google Scholar]
- 44.Guérin P, Obeid I, Gille O, Bourghli A, Luc S, Pointillart V, et al. Sagittal alignment after single cervical disc arthroplasty. J Spinal Disord Tech. 2012;25:10–6. doi: 10.1097/BSD.0b013e31820f916c. [DOI] [PubMed] [Google Scholar]
- 45.Faldini C, Chehrassan M, Miscione MT, Acri F, d’Amato M, Pungetti C, et al. Single-level anterior cervical discectomy and interbody fusion using PEEK anatomical cervical cage and allograft bone. J Orthop Traumatol. 2011;12:201–5. doi: 10.1007/s10195-011-0169-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim JT, Lee HJ, Choi DY, Shin MH, Hong JT. Sequential alignment change of the cervical spine after anterior cervical discectomy and fusion in the lower cervical spine. Eur Spine J. 2016;25:2223–32. doi: 10.1007/s00586-016-4401-z. [DOI] [PubMed] [Google Scholar]


