Abstract
Study Design:
Retrospective cohort study.
Objective:
Type III odontoid fractures are classically treated nonoperatively, yet, the current literature on Type III odontoid fractures includes fractures of multiple etiologies and fracture morphologies. We hypothesize that a subgroup of complex, Type III fractures caused by high-energy mechanisms are more likely to fail nonoperative treatment.
Materials and Methods:
Acute Type III odontoid fractures were identified at a single institution from 2008 to 2015. Fractures were categorized as high- or low-energy fracture with high-energy fractures defined as those with lateral mass comminution (>50%) or secondary fracture lines into the pars interarticularis or vertebral body. Patients were treated in either a hard collar orthosis or halo vest and were followed for fracture union and stability.
Results:
One hundred and twenty-five Type III odontoid fractures were identified with 51% classified as complex fractures. Thirty-three patients met the inclusion and exclusion criteria including 15 patients treated in a halo vest and 18 in a hard collar orthosis. Mean follow-up was 32 (±44) weeks. Seven patients demonstrated progressive displacement of either 2 mm of translation or 5° of angulation and underwent delayed surgical stabilization. Two additional patients required delayed surgery for nonunion and myelopathy. Initial fracture displacement and angulation were not correlative with final outcome. No statistical advantage of halo vest versus hard collar orthosis was observed.
Conclusions:
Complex Type III odontoid fractures are distinctly different from low-energy injuries. In the current study, 21% of patients were unsuccessfully treated nonoperatively with external immobilization and required surgery. For complex Type III fractures, we recommend initial conservative treatment, while maintaining close monitoring throughout patient recovery and fracture union.
Keywords: Axis, C2, cervical, odontoid, trauma
INTRODUCTION
The incidence of odontoid fractures varies between age groups and is generally believed to account for approximately 20% of all cervical spine injuries.[1,2] The great majority of odontoid fractures occur in the elderly population from a low-energy mechanism with a smaller contribution from high-energy accidents in the young.[3,4]
The Anderson and D'Alonzo classification is the most commonly utilized classification system.[1] Type I fractures occur at the proximal tip of the dens from an avulsion injury. Type II fractures occur at the junction of the dens and the C2 vertebral body. Type III fractures extend into the vertebral body and account of 39% of all odontoid fractures.[5] In general, the Type III fracture is believed to have high healing potential due to large fracture surface area through cancellous bone.[6] Current studies recommend nonsurgical management of Type III odontoid fractures with union rates of 85%–100% with external immobilization.[5,7,8,9,10,11]
A considerable amount of heterogeneity exists among Type III fractures. High-energy fractures with comminution of the lateral mass and secondary fracture lines extending into the pars interarticularis or vertebral body have historically been studied together with low-energy simple fractures in the elderly. The purpose of this study is to separately evaluate treatment outcomes of complex Type III fractures with external immobilization (halo vest and hard collar orthosis).
MATERIALS AND METHODS
A single-institution, retrospective cohort study was conducted to evaluate the outcome of conservative treatment of complex Type III odontoid fractures. Acute C2 (axis) fractures were identified from International Statistical Classification of Diseases-9 coding from 2008 to 2015. Institutional review board approval was obtained. Fracture morphology was delineated by computed tomography (CT) and classified according to the definition of Type III fracture according to Anderson and D'Alonzo.[1] Information regarding patient characteristics including age, mechanism of injury, neurologic status, and other associated injuries (spine, chest, and abdomen) were recorded for all patients with acute Type III odontoid fractures.
Type III odontoid fractures were divided into two categories. Fractures with lateral mass comminution >50% or with secondary fractures lines into the pars interarticularis or vertebral body were classified as “complex fractures” [Figure 1]. All other Type III fractures were classified as simple fractures [Figure 2]. Inclusion criteria for the study were complex Type III fractures that were treated nonoperatively in either a hard collar orthosis (Aspen Collar®) or halo vest. Patients that underwent early surgery without a trial of nonoperative management or those lost to follow-up were not included in this study.
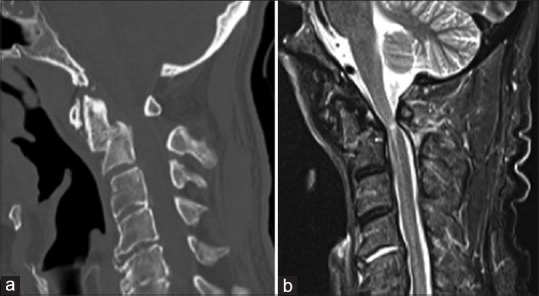
Figure 1.
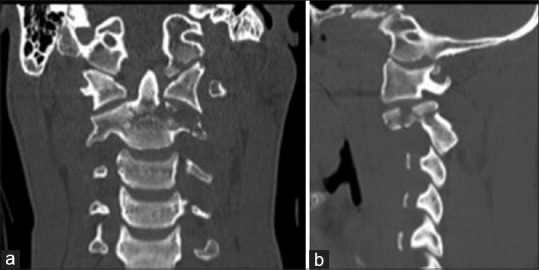
Example of a complex Type III fracture with comminution of the left lateral mass extending into the pars interarticularis. (a) coronal (b) left parasagittal computed tomography
Figure 2.
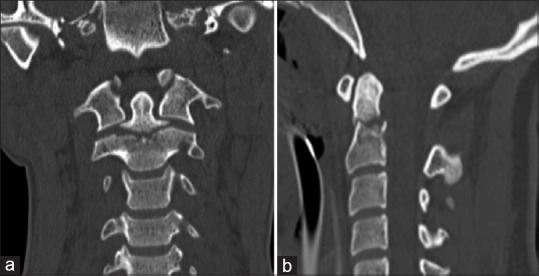
Example of simple Type III odontoid fracture with extension into bilateral superior articular facets. (a) coronal (b) mid-sagittal computed tomography
Patients were treated by both orthopedic and neurological surgeons based on the preferences of the treating surgeon. All patients in the study were followed at periodic intervals (1–4 weeks) after discharge from the hospital with upright anteroposterior and lateral radiographs. Fracture deformity was measured off initial CT scans and on final follow-up radiographs with notation of displacement and angulation by two authors. The mean value of displacement and angulation was utilized for analysis. Displacement was defined as the anterior translation of the odontoid fracture fragment in relation to the C2 or C3 vertebral body. Any significant worsening of alignment or displacement prompted recommendations for surgical fusion.
Fracture stability and union were determined independently by two different authors at the time of discontinuation of immobilization. Stability was defined as the absence of nonphysiologic motion of C1–C2 on dynamic imaging with atlantodens interval >3 mm.[12] Union was defined as bridging bony consolidation on CT or bony healing of the fracture lines on X-rays in addition to the lack of motion at the fracture site on dynamic radiographs. The maintenance of reduction was defined as <2 mm of change in displacement or 5° of angulation in comparison to initial CT scan.
Univariate descriptive statistics of the study sample were summarized. Participants were characterized by the type of Type III odontoid fracture (simple/complex), and Chi-square and t-tests/Kruskal–Wallis tests were performed as appropriate to compare the two groups. Type III complex odontoid fracture participants were further categorized into two groups, based on treatment received (halo/hard collar) and other inclusion criteria mentioned in the methods section above. These two groups were compared using Chi-square and Kruskal–Wallis tests as appropriate. All statistical analyses were performed in SAS 9.4 (SAS Institute, Inc., Cary, NC) and level of significance (α) was set at 0.05 (two-sided).
RESULTS
A total of 125 acute Type III odontoid fractures were identified at our institution between 2008 and 2015 [Table 1]. Sixty-one fractures were classified as simple [Figure 2], and 64 met the criteria for complex fractures [Figure 1]. Patient's characteristics are displayed in Table 1. The average age of presentation of all Type III odontoid fractures was 55.9 years (±22.3). Simple fractures had a lower mean age (51.1 ± 22.4) than complex fractures (56.9 ± 22.4).
Table 1.
Characteristics of patient by fracture type
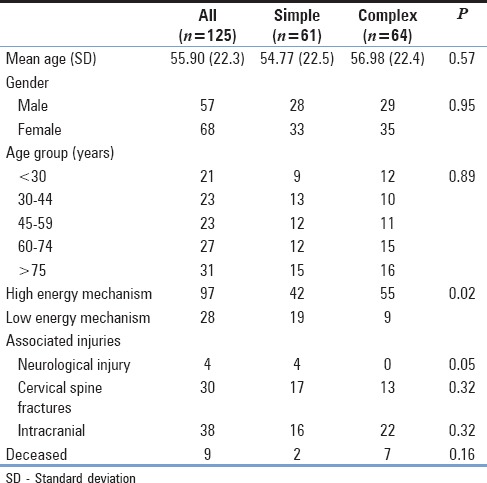
Fifty-five (86%) of the complex fractures occurred secondary to high-energy blunt trauma; whereas, nearly one-third (19/61) of simple fractures occurred secondary to falls from standing. Of patients younger than age 60, 66 of 68 (97%) occurred secondary to high-energy blunt trauma; whereas, only 52% (30 of 57) patients >60 years of age occurred from high-energy mechanisms. Neurological injury was seen in four patients each with simple fractures extending into the superior articular facet.
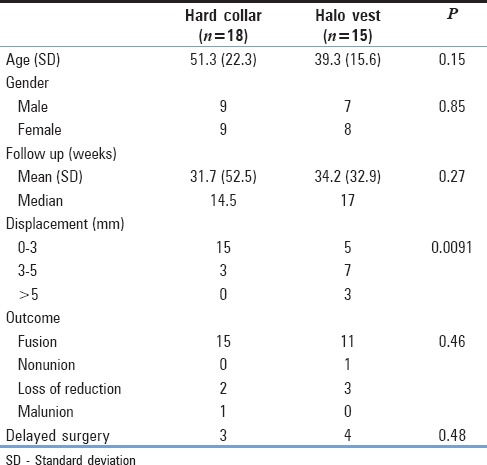
Of the 64 complex fractures, 33 met the inclusion and exclusion criteria for the study. Eight patients were excluded due to limited outpatient follow-up and seven patients due to death. An additional 16 were not included due to early surgery. Average follow-up for the cohort was 32 weeks (±44) with a median of 16 weeks. A relative equal distribution of treatment in halo vest (n = 15) and hard collar orthosis (n = 18) was seen at discharge from the hospital [Table 2].
Table 2.
Study cohort patient and fracture characteristics according to treatment
Twenty-six patients (78.7%) progressed to fracture union without loss of reduction or change in alignment. One patient removed his hard collar before recommendation and returned to clinic months later with myelopathy secondary to a malunion [Figure 3].
Figure 3.
Malunion of complex Type III fracture in a patient with poor compliance with hard collar orthosis. Patient return to clinic 9 months after injury with spinal cord compression and clinical examination consistent with myelopathy. (a) mid-sagittal computed tomography (b) mid-sagittal T2 magnetic resonance imaging
Seven patients (21%) underwent late surgery as outlined in Table 3. Two patients treated with a hard collar orthosis demonstrated a progressive loss of reduction and underwent posterior fusion. A third patient treated in a collar underwent a C1 laminectomy for myelopathy as described above. Four patients treated in a halo underwent late surgery (posterior fusion) with three occurring due to progressive displacement and one who showed no signs of healing at 8 weeks.
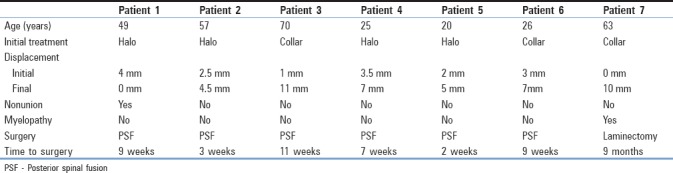
Table 3.
Characteristics of patients requiring secondary surgery
DISCUSSION
In 1972, Anderson and D’Alonzo modified Schazkter's classification of odontoid fractures extending the scheme to include those that involved the vertebral body (Type III fractures).[1,13] In clinical practice, the Type III fracture encompasses a heterogeneous collection of morphologically different fractures of varying etiologies and patient demographics. At trauma centers, a complex, high-energy subtype exists that radiographically fits the definition of Type III odontoid fracture but of unknown clinical context. The current study was designed to further investigate complex Type III fractures and evaluate radiographic treatment outcomes.
Fractures with >50% comminution of the lateral mass or secondary fracture lines extending into the vertebral body or pars interarticularis were classified as complex. Biomechanically, complex fractures exhibit the same deforming forces as all odontoid fractures with additional instability in the rotatory or coronal plane. In the current study, 51% of Type III fractures met our criteria as complex fractures. These patients were of similar age to all odontoid fractures (56.9 vs. 55.9 years) but were commonly associated (86%) with high-energy blunt trauma (P = 0.02).
While a Cochrane review revealed that no quality trials existed to guide treatment of odontoid fractures,[14] Type III odontoid fractures are universally treated nonoperatively.[15] With rigid external immobilization, high success rates have been shown in the treatment of Type III odontoid fractures.[5,7,8,9,10,11] In 1989, Hadley et al. treated 48 patients with either halo or sternal-occipital-mandibular immobilization (SOMI) brace with all progressing to the union.[11] Greene et al. retrospectively reviewed 77 Type III fractures with 69 managed in halo or SOMI with a 1.4% nonunion rate.[5]
Analysis of complex fractures shows an overall 21% failure rate with nonoperative management requiring delayed surgery. A majority of these patients (7/9) demonstrated progressive displacement of either 2 mm of translation or 5° of angulation and underwent delayed surgical stabilization. In addition, one patient in our study had poor compliance with hard collar orthosis and developed a malunion prompting decompression for myelopathy 9 months after injury [Figure 3]. The relationship between odontoid fractures and delayed myelopathy has been well documented in the literature.[16,17,18] However, most authors cite myelopathy secondary instability from a nonunion and not a malunion as seen with our patient.
To date, no standard of care exists for optimal immobilization technique in Type III odontoid fractures. Clinically, both Patel and Polin both showed no statistical advantage of halo vest compared to hard collar in their case series of 15 and 18 patients, respectively.[8,9] With increased knowledge of morbidity and mortality associated with the halo vest,[19] nationwide inpatient sample data from 2000 to 2010 suggests treatment of C2 fractures in halo vest has decreased 25% to 10.4%.[20] Our results suggest a higher yet nonstatistically significant rate of failure (P = 0.48) of the halo vest (26.6%) versus hard collar orthosis (11.1%). However, we caution against interpreting the results as a superiority of the halo vest as the two treatment groups were not alike [Table 2]. The halo vest was utilized in more displaced fracture (P = 0.009) and in younger patients (P = 0.15). In addition, one-third of complex fractures had accompanying intracranial pathology that at times precludes halo vest placement.
In the current study, no variables were identified that were predictive of failure with nonoperative treatment. Both initial fracture displacement and angulation did not correlate with fracture union. All six patients who underwent delayed fusion surgery ranged in initial displacement between 0 mm and 4 mm. The three patients with severe displacement (>5 mm) on presentation all progressed to union and stability on dynamic imaging. Our results contradict recommendations by Ryken et al., and Fujii et al., suggesting operative treatment of fractures with displacement >5 mm.[15,21]
The authors of the current study advocate conservative treatment of Type III odontoid fractures regardless of fracture morphology or displacement. As our data suggest, a small percentage of fractures cannot be adequately treated with external immobilization and will require fusion surgery.[22] Nonetheless, a trial of nonoperative management should be attempted with close monitoring. If instability is detected or patient progresses to a nonunion, delayed surgery can be conducted with efficacious outcomes.[23]
Limitations in the study largely lie in its retrospective, nonrandomized design. Individual treatment of each fracture may reflect the bias of the treating surgeon. As a primarily radiographic study, clinical outcomes were not analyzed.
CONCLUSIONS
Type III odontoid fractures can occur following high-energy trauma. These are distinctly different than low energy injuries. In our study, 21% of complex Type III odontoid fractures could not be adequately treated with external immobilization and required fusion surgery. We recommend conservative treatment of all Type III fractures while maintaining close monitoring throughout patient recovery and fracture union.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis 1974. J Bone Joint Surg Am. 2004;86-A:2081. [PubMed] [Google Scholar]
- 2.Clark CR, White AA., 3rd Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340–8. [PubMed] [Google Scholar]
- 3.Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(Suppl 2):B54–64. doi: 10.1016/j.injury.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 4.Butler JS, Dolan RT, Burbridge M, Hurson CJ, O’Byrne JM, McCormack D, et al. The long-term functional outcome of type II odontoid fractures managed non-operatively. Eur Spine J. 2010;19:1635–42. doi: 10.1007/s00586-010-1391-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntag VK, et al. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976) 1997;22:1843–52. doi: 10.1097/00007632-199708150-00009. [DOI] [PubMed] [Google Scholar]
- 6.Hanssen AD, Cabanela ME. Fractures of the dens in adult patients. J Trauma. 1987;27:928–34. doi: 10.1097/00005373-198708000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Müller EJ, Schwinnen I, Fischer K, Wick M, Muhr G. Non-rigid immobilisation of odontoid fractures. Eur Spine J. 2003;12:522–5. doi: 10.1007/s00586-003-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polin RS, Szabo T, Bogaev CA, Replogle RE, Jane JA. Nonoperative management of types II and III odontoid fractures: The philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450–6. doi: 10.1097/00006123-199603000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Patel A, Zakaria R, Al-Mahfoudh R, Clark S, Barrett C, Sarsam Z, et al. Conservative management of type II and III odontoid fractures in the elderly at a regional spine centre: A prospective and retrospective cohort study. Br J Neurosurg. 2015;29:249–53. doi: 10.3109/02688697.2014.958055. [DOI] [PubMed] [Google Scholar]
- 10.Govender S, Grootboom M. Fractures of the dens – The results of non-rigid immobilization. Injury. 1988;19:165–7. doi: 10.1016/0020-1383(88)90007-1. [DOI] [PubMed] [Google Scholar]
- 11.Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: A review of 229 cases. J Neurosurg. 1989;71(5 Pt 1):642–7. doi: 10.3171/jns.1989.71.5.0642. [DOI] [PubMed] [Google Scholar]
- 12.Yang SY, Boniello AJ, Poorman CE, Chang AL, Wang S, Passias PG, et al. Areview of the diagnosis and treatment of atlantoaxial dislocations. Global Spine J. 2014;4:197–210. doi: 10.1055/s-0034-1376371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schatzker J, Rorabeck CH, Waddell JP. Fractures of the dens (odontoid process). An analysis of thirty-seven cases. J Bone Joint Surg Br. 1971;53:392–405. [PubMed] [Google Scholar]
- 14.Shears E, Armitstead CP. Surgical versus conservative management for odontoid fractures. Cochrane Database Syst Rev. 2008;4:CD005078. doi: 10.1002/14651858.CD005078.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryken TC, Hadley MN, Aarabi B, Dhall SS, Gelb DE, Hurlbert RJ, et al. Management of isolated fractures of the axis in adults. Neurosurgery. 2013;72(Suppl 2):132–50. doi: 10.1227/NEU.0b013e318276ee40. [DOI] [PubMed] [Google Scholar]
- 16.Sherk HH. Fractures of the atlas and odontoid process. Orthop Clin North Am. 1978;9:973–84. [PubMed] [Google Scholar]
- 17.Bohlman HH. Acute fractures and dislocations of the cervical spine. An analysis of three hundred hospitalized patients and review of the literature. J Bone Joint Surg Am. 1979;61:1119–42. [PubMed] [Google Scholar]
- 18.Moskovich R, Crockard HA. Myelopathy due to hypertrophic nonunion of the dens: Case report. J Trauma. 1990;30:222–5. doi: 10.1097/00005373-199002000-00017. [DOI] [PubMed] [Google Scholar]
- 19.Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: A death sentence? J Trauma. 2005;59:350–6. doi: 10.1097/01.ta.0000174671.07664.7c. [DOI] [PubMed] [Google Scholar]
- 20.Daniels AH, Arthur M, Esmende SM, Vigneswaran H, Palumbo MA. Incidence and cost of treating axis fractures in the United States from 2000 to 2010. Spine (Phila Pa 1976) 2014;39:1498–505. doi: 10.1097/BRS.0000000000000417. [DOI] [PubMed] [Google Scholar]
- 21.Fujii E, Kobayashi K, Hirabayashi K. Treatment in fractures of the odontoid process. Spine (Phila Pa 1976) 1988;13:604–9. [PubMed] [Google Scholar]
- 22.Goel A, Jain S, Shah A, Patil A, Vutha R, Ranjan S, et al. Atlantoaxial Fixation for Odontoid Fracture: Analysis of 124 Surgically Treated Cases. World Neurosurg. 2018;110:558–67. doi: 10.1016/j.wneu.2017.08.192. [DOI] [PubMed] [Google Scholar]
- 23.Smith JS, Kepler CK, Kopjar B, Harrop JS, Arnold P, Chapman JR, et al. Effect of type II odontoid fracture nonunion on outcome among elderly patients treated without surgery: Based on the AOSpine North America geriatric odontoid fracture study. Spine (Phila Pa 1976) 2013;38:2240–6. doi: 10.1097/BRS.0000000000000009. [DOI] [PubMed] [Google Scholar]


