Abstract
Objective:
Current literature indicates that the presence of clinical pharmacists in hospitals results in improved patient care, rational drug therapy, and treatment costs. This study assessed the clinical pharmacy services in the intensive care unit (ICU) of a tertiary hospital at Tabriz University of Medical Sciences, Iran.
Methods:
During a 9-month cross-sectional study (2014–2015), the clinical pharmacy interventions in 27 sessions and educational activities for patients and health-care professionals were randomly assessed based on the Australian guideline and standard of practice for clinical pharmacy. The interventions of clinical pharmacist were evaluated in terms of their clinical importance.
Findings:
In this study, a total of 832 interventions on 242 patients were performed by the clinical pharmacist, and approximately 93.6% of the interventions were approved by the attending physician. Most interventions concerned adding a new medication to a drug regimen or switching to a needed new medication. Each patient received an average of three interventions. The clinical pharmacist provided drug information to employees and medical staff in 108 of the total 832 interventions (13%). Medical residents who were surveyed indicated that the quality of education, research, and patient care was improved by the attendance of a clinical pharmacist.
Conclusion:
The results of this study show that the collaboration of a clinical pharmacist with the medical staff of an ICU can improve pharmacotherapy approach and increase the quality of education.
KEYWORDS: Clinical pharmacist, critical care, intensive care unit, pharmacotherapy
INTRODUCTION
Before introducing pharmaceutical care services, physicians were responsible for managing patients' medications and their medical care. With the promotion of health-care services and complexity of drug therapy, the role of the clinical pharmacist has been felt more than before.[1] Therefore, by adding pharmaceutical services to patient care and by changing the professional activity of pharmacists from drug-focused to patient-oriented care, clinical pharmacists in hospitals were assigned to monitor pharmacotherapy regimens, participate in patient care, and cooperate in educating the staff and evaluating care.[2]
The American College of Clinical Pharmacy defines clinical pharmacists as practitioners who provide comprehensive “medication management” and related care for patients in all health-care settings (www.accp.com/standards).[3] “Medication management” is a significant term which implies and summarizes the clinical pharmacist's role in patient care. It applies to issues related to the indication, use and administration, and therapeutic goals of drug use, adverse drug events, drug interactions, and the monitoring of medications. Because of the complexity of drug therapy and the critical nature of patients in intensive care units (ICUs), the attendance of a clinical pharmacist in this setting is an important issue.[4,5]
Errors concerning medications are more probable and more harmful in ICUs than in non-ICU settings.[6] Studies have reported that the interventions of clinical pharmacists have resulted in a rational drug therapy and improved patient care and treatment costs.[7,8,9] Further training for clinical pharmacists, such as residency and fellowship programs, would enable them to become specialists in various areas of patient care, such as intensive care. All these efforts will improve the status of clinical pharmacists in providing clinical services. However, there is no agreement on what types of clinical pharmacy services should be consistently provided to patients or to what extent a clinical pharmacist has authority.
In 2010, clinical pharmacy services at Tabriz University of Medical Sciences were started for the first time with the involvement of a clinical pharmacy specialist in the ICU of a main referral, university-affiliated hospital by establishing independent pharmacotherapy rounds with medical residents and pharmacy interns, to have therapeutic and educational interventions.
The current study aimed to describe the clinical pharmacy services in the intensive care setting of the largest medical university in northwest of Iran.
METHODS
In a descriptive and cross-sectional study conducted in the trauma ICU of Shohada University Hospital which is affiliated with Tabriz University of Medical Sciences, all the clinical pharmacists' interventions and services were randomly evaluated during a 9-month period (November 2014–July 2015). The study protocol was approved by the Clinical Research Ethics Committee of Tabriz University of Medical Sciences, Iran (IRB # 2015-07-117).
A clinical pharmacist expert in critical care pharmacotherapy works there as a clinical assistant professor, performing clinical and educational activities in the trauma ICU of the medical center. The clinical pharmacist visited ICU patients accompanied by a pharmacist and medical interns and residents 2 days per week. The demographic data of patients were recorded in detail, including age, gender, patient's medical history, and medication information (drugs used and their dosage forms), and any pharmacological interventions or recommendations by the clinical pharmacist were also recorded.
Clinical pharmacist interventions were classified into nine categories as defined below:
Drug discontinuation: Stopping the administration of medicine to prevent or eliminate adverse drug reactions or drug interactions or because of lack of indication or efficacy
Adding a new drug or changing one: Adding or substituting a new drug to improve the pharmacotherapy approach
Changing the dose, frequency of administration, and duration of administration: Adjusting drug doses in patients with renal insufficiency
Changing the dosage forms, for example, changing furosemide from tablet form to injection form in patients with severe edema (gut absorption of furosemide in edematous patients is disturbed because of gut edema) and changing pantoprazole from injection form to tablet form in patients who were not NPO
Applying laboratory parameters to monitor medication, for example, performing liver function tests for patients who received rifampin
Preventing and managing side effects and drug interactions and reviewing and removing unwanted drug effects, for example, replacing tizanidine with baclofen in patients who received systemic ciprofloxacin
Therapeutic drug monitoring, for example, checking digoxin plasma levels and calculating appropriate doses, especially in patients with renal dysfunction
Investigating the stability of drugs and drug incompatibility and checking the stability or compatibility, especially when added in serums, for example, haloperidol was added to dextrose serum 5% instead of normal saline because of the better compatibly when used as a continuous infusion to control delirium in the ICU
Helping patients adhere to drug therapy or reducing nursing workload, for example, substituting salbutamol (albuterol) and ipratropium sprays with a combination of salbutamol plus ipratropium spray (Combivent®).
After each pharmacotherapy round and patients' visit by the clinical pharmacy specialist, the physician in charge of the ICU reviewed and decided whether to accept or reject the proposed drug-related medical orders of the clinical pharmacist. The acceptance rate for clinical pharmacist's interventions was recorded.
During a 9 month from 72 workdays, all clinical pharmacists' interventions were recorded over 27 sessions. Clinical pharmacist was blinded to the days which his interventions were going to be recorded. Blindness of clinical pharmacist to the workdays which were going to be recorded was important to estimate his fair approach to patients' visits and prevent overestimation of his interventions. Using random numbers from 1 to 27 generated by a computer, 9 sessions were selected and the interventions of the 9 random sessions were judged, unbeknownst to the clinical pharmacist. The impact of the clinical pharmacist's interventions on the outcomes of therapy which were approved by the physician was evaluated based on the Australian guideline and standard of practice for clinical pharmacy practice[10] by two intensive care specialists independently whom were blinded to the result of each other's evaluation. The judgments of the two intensivists were compared with others, and the differences were evaluated in a joint session by them and a clinical pharmacist who had not participated in patient care process during the study period in the same ICU. After discussion, the votes of the three specialists were integrated into one single agreement and recorded as insignificant, minor, moderate, major, and lifesaving.
Because of the important role of education in university hospitals, the training of pharmacy and medical interns and residents is one of the main activities of a clinical pharmacist in addition to providing pharmaceutical care. After each pharmacotherapy round, classes on pharmacotherapy subjects in the field of critical care were held for clinical residents and pharmacy and medical interns. The physician in charge of the ward surveyed residents about the quality of education and importance of clinical pharmacist attendance in the ICU's medical rounds. The survey consisted of five questions which students answered by selecting one of these options: I agree, I fairly agree, I have no idea, I fairly disagree, or I disagree.
Continuous quantitative data were reported as mean ± standard deviation (SD). Categorical variables were expressed as percentages. Descriptive statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS), version 16 (SPSS Inc., Chicago, IL, USA, 2007).
RESULTS
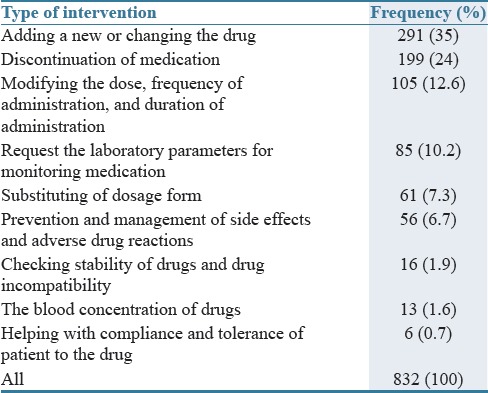
Over a 9-month period (2014–2015), the activities of the trauma ICU's clinical pharmacy specialist were recorded for 27 randomly chosen days. In this period, 242 patients were visited and 832 interventions were recorded for patients by the clinical pharmacist. From 242 patients, 172 (71.1%) were male and 70 (28.9%) were female. The mean (±SD) age of patients was 61.5 ± 21.1 years. The average (±SD) number of interventions by the clinical pharmacist was 3.4 ± 2.7 interventions per patient. The average new drug additions to the patients' drug regimens were 9.5 ± 4.8 per workday of the clinical pharmacist, for each patient, with a mean (±SD) of 1.1 ± 1.7. The frequency of clinical pharmacist interventions is presented in Table 1. The clinical pharmacist spent 119.3 ± 45.4 min per day on patient visits. The average time assigned to each clinical intervention was 14.4 ± 5.7 and 75 ± 12 min and was allocated for each class on pharmacotherapy subjects in the field of critical care for the pharmacy students and medical students and residents.
Table 1.
Frequency of interventions proposed by the clinical pharmacist for the study patients
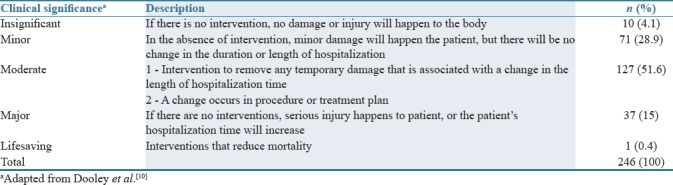
The intensivist in charge of the ICU approved 778 (93.5%) of the 832 interventions. The impact of the clinical pharmacist's interventions on the outcome of therapy which were reviewed by two intensivists as evaluators and one clinical pharmacist as coordinator is presented in Table 2.
Table 2.
Impact of the clinical pharmacist’s interventions on the outcome therapy in the study patients
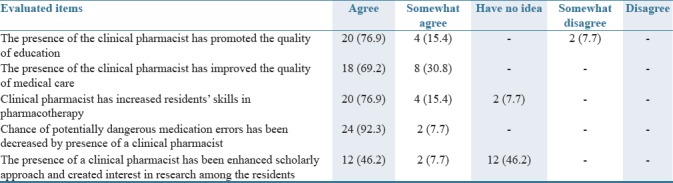
The results of the survey of 26 medical residents regarding the quality of education and importance of clinical pharmacist attendance in the ICU are shown in Table 3. They indicated that the quality of education, research, and patient care was improved by the attendance of a clinical pharmacist.
Table 3.
The feedback of medical students about the quality of education and the importance of clinical pharmacist’s attendance in the intensive care unit’s medical rounds
DISCUSSION
Although only 10% of hospitalized patients are admitted to the ICU, over 30% of hospital costs are allocated for patients needing acute care.[11] It seems that patients admitted to ICUs are prone to a higher risk of medication-related problems because of the higher numbers of prescribed medications, intensity of the work environment, presence of critical illness, and increased use of high-risk medications. Thus, the American College of Critical Care Medicine defined clinical roles and tried to introduce the best practice model in ICUs for any service which is involved in a multidisciplinary critical care setting.[12] That study aimed to define the best model based on the ability of each specialty involved in ICU patient care to minimize mortality and optimize efficiency. The authors classified pharmacotherapy services into three models. In one model, pharmacists check out drug orders retrospectively but usually do not actively attend in the ward. In the second model, pharmacists are involved in an intensive care satellite pharmacy in order to dispensing medications, as well as evaluating drug prescriptions, and taking part in ICU rounds to provide drug information. In this model, patients are visited by the pharmacy service based on a written consultation request from the physician in charge or a verbal request during clinical rounds. Thus, clinical pharmacists do not visit patients regularly. In the third model, pharmacists are exclusively assigned to direct patient care responsibilities, including attending actively in ward rounds and prospectively evaluating pharmacotherapy approaches for each patient. In this setting, the hospital demands the maximum responsibility of the clinical pharmacist and his active practice. It seems that the third model of clinical pharmacist intervention in specialized wards such as the critical care setting is the best one for the clinical pharmacist practice. The present study was based on the third model for clinical pharmacist practice. Adding a new drug and changing or omitting an inappropriate drug from a patient's drug list comprised around 60% of clinical pharmacist interventions, which may show the efficiency of the practice. The mean number of interventions for each patient was 3.
Dashti-Khavidaki et al. conducted a similar study in the infectious diseases and nephrology wards of an educational hospital in Tehran, Iran, in 2009. Most of the interventions concerned drug discontinuation and ordering changes with a frequency of 297 (22.7%) interventions, followed by adding a new drug to the regimen with a frequency of 272 (20.8%) interventions and replacing one medication with other with a frequency of 98 (7.5%) interventions. In this study, each patient had an average of 1.3 interventions.[13] In another study conducted by Hisham et al., the most common interventions at drug level (475 interventions during 1 year) were changing dose, frequency, and duration (73%) followed by stopping or adding a new drug to the regimen and changing one drug to another (20%).[14]
As previously mentioned, ICU patients need more pharmacological care due to their critical conditions and pharmacodynamic and pharmacokinetic changes because multiple system organ incompetence can modify the absorption, distribution, metabolism, and extraction of drugs.[5] Thus, patients with a critical illness exhibit specific pharmacological challenges for the physician. In this regards, it seems that the interventions of a clinical pharmacist in our study be more than other settings. Similar to the current results, in their 3-month study in the ICU at St. Joseph's Hospital in Hamilton, Canada, Montazeri and Cook[15] found that a clinical pharmacist made 10.7 ± 5.0 interventions per workday and spent almost 102 min on interventions.
In the present study, the physician in charge approved 93.6% of the clinical pharmacist interventions. The results from most of the similar studies conducted in different hospital units indicate that the acceptance rate of interventions has been reported at >90%.[8,13,16,17] In the third model suggested for clinical pharmacist practice, which is mentioned above, the active involvement of a clinical pharmacist in patient treatment is demanded. For high-risk patients, like those who are critically ill, routine pharmacotherapy visits should be established to consider the patients' rights to receive pharmaceutical care. In this setting, the acceptance rate of clinical pharmacist interventions by physicians would not be the main subject, but physicians should be responsible in any cases where the pharmacist's advice is rejected. The majority of interventions (51.6%) were categorized as moderately important. The rate of total important interventions (moderate, major, and lifesaving) in the current study was 67%, which is similar to the results obtained by Dooley et al. in their study of eight major government-funded acute care teaching hospitals in Australia (64.4%).[18] However, this value was higher in this study than in another study conducted in nephrology and infectious units (67% vs. 48.9%).[13] This finding may be due to the critical condition of ICU patients who need more pharmaceutical interventions.
According to this study, most clinical residents who participated in the survey believed that the presence of a clinical pharmacist has positive impacts on the education, research, and treatment. Previously, the effects of participation by a clinical pharmacist on education and evaluation of patient care in an ICU were shown.[4]
The current study may have some limitations as well. First, the cost-effectiveness of the clinical pharmacist interventions is not identified, and the second one, the time duration of the study and sample size were short and small. Finally, the efficacy of clinical pharmacist's educational teachings on the patients' outcome of therapy was not studied. Evaluation of the effectiveness of clinical pharmacists' interventions on patients' outcome would be suggested in future large prospective studies.
The results of this study show that the collaboration of a specialized clinical pharmacist with the medical staff in a trauma ICU can help to improve patient outcomes and increase the quality of education and medical staff satisfaction. However, studies with a larger size are needed to confirm this result.
AUTHORS' CONTRIBUTION
A.M: Participated in its design and coordination and helped to draft the manuscript, A.K: Collecting and recording data, K.S: Data gathering and helped to draft the manuscript, T.EM: Literature review, editing manuscript, H.H: Participated in the design of the study and performed the statistical analysis and helped to draft the manuscript. All authors read and approved the final manuscript.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bates DW, Cullen DJ, Laird N, Petersen LA, Small SD, Servi D, et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE prevention study group. JAMA. 1995;274:29–34. [PubMed] [Google Scholar]
- 2.Kaboli PJ, Hoth AB, McClimon BJ, Schnipper JL. Clinical pharmacists and inpatient medical care: A systematic review. Arch Intern Med. 2006;166:955–64. doi: 10.1001/archinte.166.9.955. [DOI] [PubMed] [Google Scholar]
- 3.Standards of Practice for Clinical Pharmacists. American College of Clinical Pharmacy. [Last accessed on 2018 Feb 21]. Available from: https://www.accp.com/docs/positions/guidelines/standardsofpractice.pdf .
- 4.Bond CA, Raehl CL, Patry R. Evidence-based core clinical pharmacy services in United States hospitals in 2020: Services and staffing. Pharmacotherapy. 2004;24:427–40. doi: 10.1592/phco.24.5.427.33358. [DOI] [PubMed] [Google Scholar]
- 5.Rudis MI, Brandl KM. Position paper on critical care pharmacy services. Society of critical care medicine and American College of Clinical Pharmacy task force on critical care pharmacy services. Crit Care Med. 2000;28:3746–50. doi: 10.1097/00003246-200011000-00037. [DOI] [PubMed] [Google Scholar]
- 6.Latif A, Rawat N, Pustavoitau A, Pronovost PJ, Pham JC. National study on the distribution, causes, and consequences of voluntarily reported medication errors between the ICU and non-ICU settings. Crit Care Med. 2013;41:389–98. doi: 10.1097/CCM.0b013e318274156a. [DOI] [PubMed] [Google Scholar]
- 7.Gallagher J, Byrne S, Woods N, Lynch D, McCarthy S. Cost-outcome description of clinical pharmacist interventions in a university teaching hospital. BMC Health Serv Res. 2014;14:177. doi: 10.1186/1472-6963-14-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kopp BJ, Mrsan M, Erstad BL, Duby JJ. Cost implications of and potential adverse events prevented by interventions of a critical care pharmacist. Am J Health Syst Pharm. 2007;64:2483–7. doi: 10.2146/ajhp060674. [DOI] [PubMed] [Google Scholar]
- 9.Schumock GT, Butler MG, Meek PD, Vermeulen LC, Arondekar BV, Bauman JL, et al. Evidence of the economic benefit of clinical pharmacy services: 1996-2000. Pharmacotherapy. 2003;23:113–32. doi: 10.1592/phco.23.1.113.31910. [DOI] [PubMed] [Google Scholar]
- 10.Dooley M, Bogovic A, Carroll M, Cuell S, Galbraith K, Matthews H. SHPA standards of practice for clinical pharmacy. J Pharm Pract Res. 2005;35:122–46. [Google Scholar]
- 11.Coopersmith CM, Wunsch H, Fink MP, Linde-Zwirble WT, Olsen KM, Sommers MS, et al. Acomparison of critical care research funding and the financial burden of critical illness in the United States. Crit Care Med. 2012;40:1072–9. doi: 10.1097/CCM.0b013e31823c8d03. [DOI] [PubMed] [Google Scholar]
- 12.Brilli RJ, Spevetz A, Branson RD, Campbell GM, Cohen H, Dasta JF, et al. Critical care delivery in the Intensive Care Unit: Defining clinical roles and the best practice model. Crit Care Med. 2001;29:2007–19. doi: 10.1097/00003246-200110000-00026. [DOI] [PubMed] [Google Scholar]
- 13.Dashti-Khavidaki S, Khalili H, Hamishekar H, Shahverdi S. Clinical pharmacy services in an Iranian teaching hospital: A descriptive study. Pharm World Sci. 2009;31:696–700. doi: 10.1007/s11096-009-9336-6. [DOI] [PubMed] [Google Scholar]
- 14.Hisham M, Sivakumar MN, Veerasekar G. Impact of clinical pharmacist in an Indian Intensive Care Unit. Indian J Crit Care Med. 2016;20:78–83. doi: 10.4103/0972-5229.175931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Montazeri M, Cook DJ. Impact of a clinical pharmacist in a multidisciplinary Intensive Care Unit. Crit Care Med. 1994;22:1044–8. doi: 10.1097/00003246-199406000-00027. [DOI] [PubMed] [Google Scholar]
- 16.Kim JM, Park SJ, Sohn YM, Lee YM, Yang CS, Gwak HS, et al. Development of clinical pharmacy services for Intensive Care Units in Korea. Springerplus. 2014;3:34. doi: 10.1186/2193-1801-3-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leape LL, Cullen DJ, Clapp MD, Burdick E, Demonaco HJ, Erickson JI, et al. Pharmacist participation on physician rounds and adverse drug events in the Intensive Care Unit. JAMA. 1999;282:267–70. doi: 10.1001/jama.282.3.267. [DOI] [PubMed] [Google Scholar]
- 18.Dooley MJ, Allen KM, Doecke CJ, Galbraith KJ, Taylor GR, Bright J, et al. Aprospective multicentre study of pharmacist initiated changes to drug therapy and patient management in acute care government funded hospitals. Br J Clin Pharmacol. 2004;57:513–21. doi: 10.1046/j.1365-2125.2003.02029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


