Abstract
Objective
Vital signs are critical markers of illness severity in the Emergency Department (ED). Providers need to understand the abnormal vital signs in older adults that are problematic. We hypothesized that in patients age ≥ 65 years discharged from the ED, there are abnormal vital signs that are associated with an admission to an inpatient bed within 7 days of discharge.
Methods
We conducted a retrospective cohort study using data from a regional integrated health system of members age ≥ 65 years during the years 2009–2010. We used univariate contingency tables to assess the relationship between hospital admission within 7 days of discharge and vital sign (including systolic blood pressure, heart rate, body temperature, and pulse oximetry (Sp02) values measured closest to discharge) using standard thresholds for abnormal and thresholds derived from the study data‥
Results
Of 104,025 ED discharges, 4,638 (4.5%) were followed by inpatient admission within 7-days. Vital signs had a greater odds of admission beyond a single cut-off. The vital signs with at least twice the odds of admission were systolic blood pressure ≤ 97 mmHg (OR 2.02, 95% CI 1.57–2.60), heart rate ≥ 101 bpm (OR 2.00 95% CI 1.75–2.29), body temperature ≥99.2 degrees Fahrenheit (OR 2.14, 95% CI 1.90–2.41), and pulse oximetry ≤ 92 Sp02 (OR 2.04, 95% CI 1.55–2.68). Patients with two vital sign abnormalities per the analysis had the highest odds of admission. A majority of patients discharged with abnormal vital signs per the analysis were not admitted within 7 days of ED discharge.
Conclusion
While we found a majority of patients discharged with abnormal vital signs as defined by the analysis, not to be admitted after discharge, we identified vital signs associated with at least twice the odds of admission.
INTRODUCTION
Vital signs are an important component of the emergency department (ED) encounter.1–3 However, despite their “vital” nature and their importance to the clinical encounter, little is known as to the value of abnormal vital signs that may predict poor outcomes after discharge. As ED encounters often lack follow-up, understanding which abnormal vital signs are associated with short-term admissions after discharge can help clinicians better manage patients.
Numerous attempts have been made to study vital signs: to electronically monitor vital signs4–6, determine their association with clinical markers such as pain,7 as well as assess their relationship with clinical outcomes.1–3,8–13 Yet prior literature has found conflicting results when evaluating vital signs in critical patients. In trauma patients presenting to the hospital, abnormal standard initial vital signs can determine the presence of critical illness.1,3,8 Whereas in patients presenting to the ED triage area11 or overcoming surgical procedures such as bowel resection,8 vital signs were not found to be helpful in determining disease course.
To our knowledge, there are no prior studies evaluating the link between ED vital signs to outcomes after discharge due to a lack of consistent event capture methods. As the elderly have the highest rates of admissions after discharge,14 we evaluated 104,025 ED visits of patients age ≥ 65 years to any of 13 hospitals in an integrated health system over a 2 year span (2009–2010) to determine the association between ED vital signs closest to discharge and an inpatient admission within 7 days of discharge.
METHODS
Study Design
We conducted a multisite retrospective cohort study of ED visits. This study was approved by the IRBs of Kaiser Permanente Southern California and the University of California, Los Angeles.
Setting
We analyzed clinical data from Kaiser Permanente Southern California (KPSC), an integrated health system that provides comprehensive care to over 3.5 million members at 14 medical centers and 197 offices throughout Southern California. There were 13 health system EDs in operation during the study period. All members have very similar health care benefits, including coverage of emergency services both within and outside the health system. Members of the health plan are generally representative of the population of Southern California, which is a racially and socioeconomically diverse region.15 Approximately 7% of all members enroll through Medicaid and 10% through Medicare.
Selection of Participants
Study participants were members of KPSC with at least 1 ED visit and discharge to a non-acute care facility from January 1st 2009 to December 31st 2010. A subject had to be a member of the health plan at the time of the ED visit; however, no minimum enrollment history was required. We restricted analyses to adults age ≥65 as this population has the greatest rates of admission after discharge.14 A discharge to a non-acute care facility included a facility such as home, nursing facility, or rehabilitation facility that did not contain 24 hour physician surveillance. If participants had multiple ED visits, then only the first visit was analyzed.
Patients who “left without being seen” by a health provider were excluded. Transfers to observation status from the ED were also excluded as encounters in this setting could resemble an inpatient admission. We excluded patients receiving hospice care as including these patients would bias the sample because the goal of this care is to provide palliative services rather than prolong life. Patients who were transferred to and from other hospitals were also excluded. The small number (<0.1%) of visit records that had potentially erroneous day and time entries resulting in either negative or excessively long ED lengths-of-stay (>48 hours), were also dropped from the analysis.
Data Sources
The electronic health record (termed KP HealthConnect) contains records of all member visits to health plan EDs during the study period. This system contains past history, mode of arrival, vital signs, staff notes, orders, diagnoses, and test results. Standardized data fields from ED visits provide time-stamps for patient registration, triage, assignment to provider, and disposition order (discharge to home, a care facility, or an inpatient bed). KP HealthConnect was also used to identify the International Classification of Disease (ICD-9-CM) diagnosis code associated with the ED visit.
Outcome Measures
The primary outcome was an inpatient admission within 7-days of discharge from the ED. The inpatient admission could be to a general inpatient bed or to an Intensive Care Unit (ICU) bed. The admission could be either to a KPSC or non-KPSC hospital bed. Observation care was not included as an outcome. We chose the 7-day period based on results that indicated the highest percentage of admissions occur within 7 days and also because of its clinical relevance, implications for health policy decisions, and use in previous studies.16–18 Information regarding admissions and the type of admission (inpatient ward bed, ICU, etc.) after discharge was obtained through Kaiser billing data.
Vital Signs
The four vital signs of systolic blood pressure (SBP), heart rate (HR), body temperature (TEMP), and pulse oximetry (PO) were taken from the electronic record. As opposed to being recorded on the same record, whether at the same time or at different times, these vital signs are recorded separately for each patient encounter. Respiratory rate was not included as prior literature has found that it has questionable reliability and may not be accurately recorded.19,20 For 96% of encounters, patients had at least one set of the four vital signs taken for each visit. For patients with visits with more than one measure for a given vital sign, the vital sign closest to discharge was chosen for the analysis. For extreme values of the vital signs that were not compatible with life and most likely a coding error, the vital sign was coded as missing: systolic blood pressure < 50 or > 300, heart rate < 25 or >225, body temperature <70 or > 105, and pulse oximetry < 30.
Data Analysis
We first summarized the outcome as a function of a set of continuous and categorical vital signs and variables (age, gender, race/ethnicity, Emergency Severity Index, Charlson Comorbidy index, discharge diagnosis, and ED shift). We tabulated the number of patients with admission after discharge who had abnormal vital signs per standard ranges21,22 and per our analysis, defined by the study team as having at least twice the odds (OR > 2.0) of admission after discharge‥ We generated an odds ratio (OR) of the outcome (admission after discharge), positive predictive value (PPV), negative predictive value (NPV), sensitivity, and specificity. For all vital sign ranges, we noted that only one extreme, or cut-off, was associated with increased admission after discharge.
All data management and analysis was performed with SAS 9.3 (SAS Institute, Cary, NC).
RESULTS
Characteristics of the Study Cohort
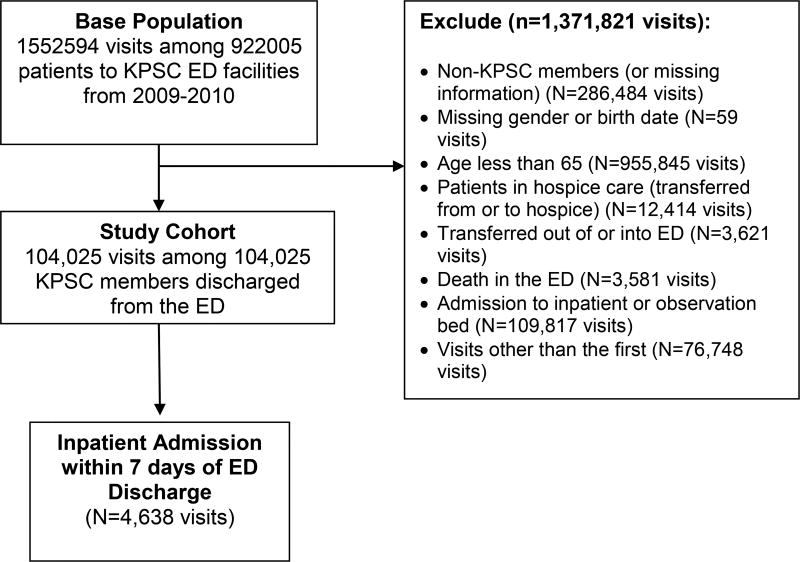
The study cohort included 104,025 health plan member visits of patients age ≥ 65 years who were discharged from a KPSC ED between 1/1/2009 and 12/31/2010 (Figure 1). The mean age was 75.3 years (SD 7.6). The frequency of an inpatient admission within 7-days of ED discharge was 4.5%. The percent of patients with multiple measures for each vital sign was: systolic blood pressure (76.6%), heart rate (76.0%), body temperature (34.3%), and pulse oximetry (69.4%). Half a percent had no vital sign recorded and these records were not included in the analysis.
Figure 1.
Flow Diagram of Study Cohort
Table 1 presents characteristics of the full cohort and the percent of patients with admission. Patients with older age, male gender, white ethnicity, lower (worse) emergency severity index, and higher Charlson comorbidity indexes had a higher percent of admission within 7 days of ED discharge. The top 6 discharge diagnosis categories of patients with the highest percent of admission were Mental Illness, Heart Disease, Neoplasms, Renal Disease, Diseases of the Blood, and non-infectious lung disease.
Table I.
Characteristics of the Discharged Cohort
| Total ED Discharges (N=104,025) |
Admitted within 7 days N=4,638 (row %) |
p value* | |
|---|---|---|---|
| Age | |||
| 65–69 | 29,538 | 1024 (3.5%) | <0.0001 |
| 70–74 | 23,743 | 1006 (4.2%) | |
| 75–79 | 20,564 | 945 (4.6%) | |
| 80–84 | 15,593 | 780 (5%) | |
| 85+ | 14,587 | 883 (6.1%) | |
| GENDER | 0.0008 | ||
| F | 59,517 | 2543 (4.3%) | |
| M | 44,508 | 2095 (4.7%) | |
| Race/ethnicity | <0.0001 | ||
| Asian/PI | 8,354 | 319 (3.8%) | |
| Black | 14,349 | 585 (4.1%) | |
| Hispanic | 22,963 | 920 (4%) | |
| Other | 2,307 | 23 (1%) | |
| White | 56,052 | 2791 (5%) | |
| Emergency severity index | <0.0001 | ||
| 1,2 | 3,614 | 277 (7.7%) | |
| 3 | 70,192 | 3713 (5.3%) | |
| 4,5 | 29,871 | 623 (2.1%) | |
| Charlson comorbidity score | <0.0001 | ||
| 0 | 20,335 | 449 (2.2%) | |
| 1 | 18,176 | 515 (2.8%) | |
| 2 | 14,901 | 554 (3.7%) | |
| 3 | 13,369 | 590 (4.4%) | |
| 4 | 10,276 | 533 (5.2%) | |
| 5 | 7,621 | 448 (5.9%) | |
| 6 | 6,441 | 441 (6.8%) | |
| 7+ | 12,906 | 1108 (8.6%) | |
| Discharge Diagnoses (Top 6) | <0.0001 | ||
| Mental Illness | 1833 | 300 (16.4%) | |
| Heart Disease | 196 | 31 (15.8%) | |
| Neoplasms | 234 | 32 (13.7%) | |
| Renal Disease | 52 | 6 (11.5%) | |
| Diseases of the Blood | 513 | 53 (10.3%) | |
| Non-infectious Lung Disease | 145 | 14 (9.7%) | |
| Shift | <0.0001 | ||
| 8am – 4pm | 55,299 | 2307 (4.2%) | |
| 4pm – 12am | 35,106 | 1681 (4.8%) | |
| 12am – 8am | 13,620 | 650 (4.8%) |
p-values are from univariate logistic regression models. There was no missing information for age, gender, race/ethnicity, Charlson comorbidity index, and shift. The missing rate for all other variables in this table was less than 1%.
Main Results
Table 2 presents the standard vital sign ranges, the numbers of patients by vital sign ranges with admission after discharge, and the following metrics: odds ratio of admission after discharge (OR), positive predictive value (PPV), negative predictive value (NPV), sensitivity (Sn) and specificity (Sp). The ranges of values with the greatest rate of admission after discharge were: systolic blood pressure 50–89 mmHg (14.3%), heart rate ≥100 bpm (7.9%), body temperature ≥ 100.4 degrees Fahrenheit (11.2%), and pulse oximetry ≤ 94 Sp02 (7.3%). Of all the standard vital sign cut offs, a systolic blood pressure < 90 mmHg had the greatest odds of admission after discharge (OR 3.59. 95% CI 1.62–8.01) but was rarely observed. All the standard vital signs had a high NPV (96%) which means that if patients are discharged in the normal range (for example, a systolic blood pressure ≥ 90 mmHg) they have at least a 96% chance of not being admitted after discharge. The low positive predictive value of all vital signs is a result of the low number of outcomes following admission.
Table 2.
Standard Vital Signs and Counts of Discharged Cohort
| Total ED Discharges (N=104,025) |
Admitted within 7 days N=4,638 (row %) |
OR (95% CI) |
PPV | NPV | Sn | Sp | |
|---|---|---|---|---|---|---|---|
| Systolic BP, mmHg | |||||||
| 50–89 | 49 | 7 (14.3%) | 3.59 (1.62–8.01) | 0.14 | 0.96 | 0.002 | 1.000 |
| 90–139 | 56388 | 2778 (4.9%) | |||||
| ≥ 140 | 46935 | 1799 (3.8%) | |||||
| Heart rate, bpm | |||||||
| 25–59 | 11541 | 347 (3%) | |||||
| 60–99 | 88219 | 3947 (4.5%) | |||||
| ≥ 100 | 3703 | 294 (7.9%) | 1.92 (1,70–2,17) | 0.08 | 0,96 | 0.064 | 0.966 |
| Body Temperature, Degrees Fahrenheit | |||||||
| 70–94.9 | 63 | 3 (4.8%) | |||||
| 95.0–100.3 | 101864 | 4476 (4.4%) | |||||
| ≥100.4 | 490 | 55 (11.2%) | 2.75 (2.08–3.65) | 0.11 | 0.96 | 0.012 | 0.996 |
| Pulse oximetry, Sp02 | |||||||
| ≤94 | 3584 | 262(7.3%) | |||||
| ≥95 | 96678 | 4,237 (4.4%) | 1.72(1.51–1.96) | 0.07 | 0.96 | 0.058 | 0.965 |
The vital signs missing information are as follows: SBP 0.6%, heart rate 0.5%, temperature 1.5%, pulse oximetry 3.6%. P-values are generated from univariate logistic regression. Odds ratios are based on the referent category of the opposite range of the vital sign, for example for systolic blood pressure, the odds ratio presented is for having a systolic blood pressure of <90 mmHg as compared to a systolic blood pressure of ≥ 90 mmHg
Table 3 includes the abnormal vital sign ranges per the analysis and percent with admission after discharge. The abnormal vital signs per the analysis with at least a 2.0 odds of admission after discharge are: systolic blood pressure ≤ 97 mmHg (OR 2.02, 95% CI 1.57–2.60), heart rate ≥ 101 bpm (2.00, 95% CI 1.75–2.29), body temperature ≥ 99.2 degrees Fahrenheit (2.14, 95% CI 1.90–2/41), and pulse oximetry reading ≤ 92 Sp02 (OR 2.04, 95% CI 1.55–2.68). Similar to the standard vital sign measures, the high NPV of these values means that if patients are discharged with vital signs in the normal range, the probability of not getting admitted after discharge is 96%. The low PPV is a result of the low number of outcomes.
Table 3.
Abnormal Vital Signs of Discharged Cohort Per the Analysis
| Total ED Discharges N =104025 |
Admitted within 7 days (row %) N=4638 (4.5%) |
OR (95% CI) | PPV | NPV | Sn | Sp | |
|---|---|---|---|---|---|---|---|
| Systolic BP, mmHg | |||||||
| ≤97* | 787 | 67 (8.5%) | 2.02 (1.57–2.60) | 0.09 | 0.96 | 0.015 | 0.993 |
| ≥98 | 10285 | 4517(4.4%) | |||||
| Heart rate, bpm | |||||||
| 25–100 | 100462 | 4339 (4.3%) | |||||
| ≥101* | 3001 | 249 (8.3%) | 2.00 (1.75–2.29) | 0.08 | 0.96 | 0.054 | 0.972 |
| Body Temperature, Degrees Fahrenheit | |||||||
| 70–99.1 | 98826 | 4221 (4.3%) | |||||
| ≥99.2* | 3591 | 313 (8.7%) | 2.14 (1.90–2.41) | 0.09 | 0.96 | 0.069 | 0.967 |
| Pulse oximetry, Sp02 | |||||||
| ≤92* | 655 | 57 (8.7%) | 2.04 (1.55–2.68) | 0.09 | 0.96 | 0.013 | 0.994 |
| ≥93 | 99607 | 4442 (4.5%) |
The vital signs missing information are as follows: SBP 0.6%, heart rate 0.5%, body temperature 1.5%, pulse oximetry 3.6%
Abnormal vital signs per the analysis defined as with a greater than 2.0 odds of admission after discharge
Table 4a shows the numbers of patients with a given number of abnormal vital signs per the analysis (as identified in table 3) and the percent that experienced an admission. There were no patients in this discharged cohort that had 4 abnormal vital signs per the analysis. Patients with 2 or 3 abnormal vital signs per the analysis had the greatest percent of admission. Table 4b presents the Odds ratio of admission after discharge, PPV, NPV, sensitivity (Sn), and specificity (Sp) of the following number of abnormal vital signs per the analysis: 1,2,or 3 (0 referent), 2 or 3 (0 or 1 referent), 3 (0,1, or 2 referent).
Table 4.
| a: Abnormal Vital Signs of Discharged Cohort and rate of 7-Day Admission Following ED Discharge | ||
|---|---|---|
| Number of Abnormal Vital Signs |
Total ED Discharges N=104025 |
Admitted within 7 days N = 4638 (row %) |
| 0 | 96027 | 3968 (4.1) |
| 1 | 6968 | 560 (8.0) |
| 2 | 506 | 60 (11.7) |
| 3 | 18 | 2 (11.1) |
| 4 | 0 | 0 |
| b: Metrics of Discharged Patients with Abnormal Vital Signs and Odds of 7-Day Admission Following ED Discharge | |||||
|---|---|---|---|---|---|
| Number of Abnormal Vital Signs |
OR (95% CI) | PPV | NPV | Sn | Sp |
| 1,2,or 31 | 2.10 (1.92–2.31) | 0.08 | 0.96 | 0.136 | 0.931 |
| . 2 or 32 | 2.92 (2.24–3.82) | 0.12 | 0.96 | 0.014 | 0.995 |
| . 33 | 2.70 (0.62–11.73) | 0.11 | 0.96 | 0.000 | 1.000 |
0.5% of patients discharged from EDs had no single vital sign recorded
The presented abnormal vital signs are based on the analysis. The vital signs missing information are as follows: SBP 0.6%, heart rate 0.5%, body temperature 1.5%, pulse oximetry 3.6%
Abnormal Vital Signs are determined by the analysis.
1,2, or 3 abnormal vital signs with referent 0 abnormal vital signs
2 or 3 abnormal vital signs with referent 0 or 1 abnormal vital signs
0 3 abnormal vital signs with referent 0,1, or 2 abnormal vital signs
DISCUSSION
We identified the standard vital sign ranges associated with an admission after discharge. In addition, we identified the abnormal vital signs that are associated with at least twice the odds of admission after discharge. All cut-offs were unilateral. While the numbers were low, we also found that patients with at least 2 abnormal vital signs per the analysis had the highest percent of admission after discharge.
Understanding the history of vital signs can help clarify their importance. Vital signs were first measured and discovered in different contexts until they were used consistently in all patient medical charts in the 1970s. Heart rate was first recorded in 2600 BC in China to reveal the nature of disease. Respiration was first observed by Hippocrates in the late 5th century BC as a marker of the physiologic state, Body temperature was first measured by a Greek mathematician and physicist in the 2nd century AD. In the 1700’s an English clergyman discovered blood pressure when he studied plants and animals.23 Pulse oximetry was first measured by a German physician in 1935 using a meter of red and green filters. 24
Systolic blood pressure readings in the emergency setting have been linked to various outcomes such as persistent epistaxis, stroke and change in mentation, as well as cardiac events. While both high blood pressure25–27 and low blood pressure28–30 have been associated with poor outcomes, we found patients with systolic blood pressure ≤ 97 mmHg to have at least twice the odds of experiencing an admission after discharge‥ We also found that for the standard cut off ranges, a systolic blood pressure < 90 bpm has close to 3.5 times the odds of admission after discharge, the highest odds of all vital signs. This finding is consistent with clinical judgement. As patients acquire an insult to their hemodynamic stability such as severe infection or acute blood loss, blood pressure can be negatively affected. We also found that the negative predictive value of this marker was high (96%) which suggests that if patients are discharged with a systolic blood pressure > 97 mmHg, the chance that they are not admitted after discharge is high (96%). The low positive predictive value of all vital signs was a marker of the low number of outcomes, admissions after discharge.
While heart rate has been assessed in the ED setting to evaluate the likelihood of predicting illness, such as developing sepsis31,32 or post-traumatic stress disorder33,34, no studies have linked ED heart rate measures to admissions shortly after discharge. We found that as heart rate increased, the more the odds of admission after discharge increased. Heart rate ≥ 100 bpm had a 1.9 odds of the outcome and the measure with at least twice the odds of admission was similar to the standard measure, ≥ 101 bpm . Prior studies have been similar in their findings and have found low heart rates to be cardioprotective in all adults and associated with a reduced odds of utilizing services and suffer poor outcomes.35,36 Our findings are consistent with clinical judgement and the body’s hemodynamic response in that an elevated heart rate can require additional consideration by the ED provider.
As clinically expected, we found a high body temperature to be associated with admission after discharge. Patients with a body temperature ≥ 99.2 degrees Fahrenheit had twice the odds of the outcome and patients with a “fever”, as defined by the standard cut off of 100.4 degrees Fahrenheit, had close to three times the odds of being admitted after discharge. Prior literature has found that older adults could have a reduced ability to regulate body temperature37 and our results of a lower body temperature cut off could describe this finding.
Pulse Oximetry was associated with twice the odds of the outcome when it was at a value of ≤ 92 Sp02. The literature has found similar results in that pulse oximetry reads at or below 92% can predict hypoxemia.38 This may be in part because of the hemoglobin dissociation curve. This “S” shaped curve starts to plummet at the low 90% range. It is important to note that while pulse oximetry can accurately detect blood oxygenation when compared to Arterial Blood Gas,38,39 it functions on the ability to detect modulation in transmitted light and thus various factors such as nail polish and ambient light40,41 or low perfusion39,42 could impact the accuracy of the readings.
We found a diagnosis of mental illness, heart disease, and neoplasms to have the highest odds of an admission after discharge. A diagnosis of mental illness includes dementia, mood disorders, depression, and substance-related disorders. Although this is a different study with a different population, our finding in this study are similar to our prior work in that we found cognitive impairment43 and chronic medical conditions44 to be associated with a poor outcome after ED discharge in older adults. Patients with mental illness possibly have a diagnosis masked by the mental illness or are suffering an impairment in mental judgment and are unable to follow ED after care instructions.
Our analysis identified vital sign cut offs that are associated with twice the odds of admission after discharge: systolic blood pressure ≤ 97 mmHg, heart rate ≥ 101 bpm , body temperature ≥99.2 degrees Fahrenheit, and pulse oximetry ≤ 92 Sp02 . Yet we also found that patients with these abnormalities have a high chance of not being admitted after discharge. Our findings suggest that while vital signs are an important component of the physical exam, patients discharged with both abnormal standard vital signs and abnormal vital signs per the analysis may not require an admission shortly after discharge. As in the 21st century a majority of ED visits are both tracked and recorded electronically, we suggest that ED providers recognize patients with the abnormal vital signs both per our analysis and standard measures, acknowledge and/or re-measure the vital signs, and consider arranging for closer outpatient follow-up.
Limitations
Our study has several potential limitations. First, despite the improved internal validity because of consistent event-capture methods, our results may not generalize to other settings. Although demographic characteristics of this elderly managed care population are similar to those of the surrounding population in southern California, our patient population may not match that of other regions. Furthermore, health plan members may have access to rapid outpatient evaluations that may not be available to the general population, potentially preventing an inpatient admission. Second, as there have been several analyses in the past evaluating death after ED discharge, this analysis did not evaluate outcomes of death.16,43 Also, the EDs at Kaiser Permanente Southern California do not represent the most overcrowded conditions (such as those seen at safety net hospitals)45 and the uninsured and underinsured are not represented in this study. In addition, the data used for this analysis are from 2009–2010 and practices in admission after discharge may have changed since that time frame. Finally, it is important to note that in most instances, patients with the highly abnormal vital signs were admitted directly from the emergency department to an inpatient bed and were therefore not included in the sample.
CONCLUSION
We identified the vital sign abnormalities in older adults that have an increased odds of admission after discharge. We also found that a majority of patients discharged with abnormal vital signs were not admitted. While an important component of the physical exam, vital signs may not have a high association with admission after discharge.
Supplementary Material
Acknowledgments
Funding and Support:
This research and Dr. Gabayan were supported by the National Institute of Health National Center for Research Resources National Center for Advancing Translational Science (NIH/NCRR/NCATS) University of California at Los Angeles Clinical and Translational Science Institute (UCLA CTSI). Dr. Gabayan is currently supported by the National Institute on Aging Grant for Early Medical/Surgical Specialists Transition to Aging Research Grant (GEMSSTAR R03AG047862-01). Dr. Sarkisian is currently supported by the National Institute on Aging (1K24AG047899-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The funding organizations did not have a role in the design and conduct of the study; management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author Contribution:
GZG conceived the study and also obtained funding. CAS, MKG , and SFD aided in the design of the study and supervised the conduct of the study. SCY managed the data. VYC and REW provided statistical advice and analyzed the data. GZG drafted the manuscript and all authors contributed substantially to its revision. GZG takes responsibility for the paper as a whole.
There are no potential conflicts of interest for all authors of this manuscript.
References
- 1.Barfod C, Lauritzen MM, Danker JK, et al. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department - a prospective cohort study. Scandinavian journal of trauma, resuscitation and emergency medicine. 2012;20:28. doi: 10.1186/1757-7241-20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yu JH, Weng YM, Chen KF, Chen SY, Lin CC. Triage vital signs predict in-hospital mortality among emergency department patients with acute poisoning: a case control study. BMC Health Serv Res. 2012;12:262–9. doi: 10.1186/1472-6963-12-262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rady MY, Smithline HA, Blake H, Nowak R, Rivers E. A comparison of the shock index and conventional vital signs to identify acute, critical illness in the emergency department. Ann Emerg Med. 1994;24:685–90. doi: 10.1016/s0196-0644(94)70279-9. [DOI] [PubMed] [Google Scholar]
- 4.Gutierrez MF, Cajiao A, Hidalgo JA, et al. A vital signs telemonitoring system - interoperability supported by a personal health record systema and a cloud service. Studies in health technology and informatics. 2014;200:124–30. [PubMed] [Google Scholar]
- 5.Costin H, Rotariu C, Alexa I, Andruseac G, Adochiei F, Ciobotariu R. A complex system for telemonitoring of medical vital signs. Revista medico-chirurgicala a Societatii de Medici si Naturalisti din Iasi. 2013;117:825–32. [PubMed] [Google Scholar]
- 6.Ansermino JM. Universal access to essential vital signs monitoring. Anesthesia and analgesia. 2013;117:883–90. doi: 10.1213/ANE.0b013e3182a1f22f. [DOI] [PubMed] [Google Scholar]
- 7.Marco CA, Plewa MC, Buderer N, Hymel G, Cooper J. Self-reported pain scores in the emergency department: lack of association with vital signs. Acad Emerg Med. 2006;13:974–9. doi: 10.1197/j.aem.2006.04.015. [DOI] [PubMed] [Google Scholar]
- 8.Erb L, Hyman NH, Osler T. Abnormal vital signs are common after bowel resection and do not predict anastomotic leak. J Am Coll Surg. 2014;218:1195–9. doi: 10.1016/j.jamcollsurg.2013.12.059. [DOI] [PubMed] [Google Scholar]
- 9.Subbe CP, Sabin J. Two ways to live, two ways to die? Not all patients at risk of deterioration in hospital are identified through abnormalities in vital signs. Resuscitation. 2014;85:456–7. doi: 10.1016/j.resuscitation.2014.01.023. [DOI] [PubMed] [Google Scholar]
- 10.Storm-Versloot MN, Verweij L, Lucas C, et al. Clinical relevance of routinely measured vital signs in hospitalized patients: a systematic review. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2014;46:39–49. doi: 10.1111/jnu.12048. [DOI] [PubMed] [Google Scholar]
- 11.Lamantia MA, Stewart PW, Platts-Mills TF, et al. Predictive value of initial triage vital signs for critically ill older adults. The western journal of emergency medicine. 2013;14:453–60. doi: 10.5811/westjem.2013.5.13411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kline JA, Corredor DM, Hogg MM, Hernandez J, Jones AE. Normalization of vital signs does not reduce the probability of acute pulmonary embolism in symptomatic emergency department patients. Acad Emerg Med. 2012;19:11–7. doi: 10.1111/j.1553-2712.2011.01253.x. [DOI] [PubMed] [Google Scholar]
- 13.Hong W, Earnest A, Sultana P, Koh Z, Shahidah N, Ong ME. How accurate are vital signs in predicting clinical outcomes in critically ill emergency department patients. European journal of emergency medicine : official journal of the European Society for Emergency Medicine. 2013;20:27–32. doi: 10.1097/MEJ.0b013e32834fdcf3. [DOI] [PubMed] [Google Scholar]
- 14.Gabayan GZ, Asch SM, Hsia RY, et al. Factors Associated With Short-Term Bounce-Back Admissions After Emergency Department Discharge. Ann Emerg Med. 2013 doi: 10.1016/j.annemergmed.2013.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corinna Koebnick P, MS, Langer-Gould M Annette M, PhD MDS, Gould M Michael K, MS, et al. Sociodemographic Characteristics of Members of a Large, Integrated Health Care System: Comparison with US Census Bureau Data. Perm J. 2012;16:37–41. doi: 10.7812/tpp/12-031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gabayan GZ, Derose SF, Asch SM, et al. Patterns and predictors of short-term death after emergency department discharge. Ann Emerg Med. 2011;58:551–8. e2. doi: 10.1016/j.annemergmed.2011.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sklar DP, Crandall CS, Loeliger E, Edmunds K, Paul I, Helitzer DL. Unanticipated death after discharge home from the emergency department. Ann Emerg Med. 2007;49:735–45. doi: 10.1016/j.annemergmed.2006.11.018. [DOI] [PubMed] [Google Scholar]
- 18.Guttmann A, Schull MJ, Vermeulen MJ, Stukel TA. Association between waiting times and short term mortality and hospital admission after departure from emergency department: population based cohort study from Ontario, Canada. BMJ. 2011;342:d2983. doi: 10.1136/bmj.d2983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krieger B, Feinerman D, Zaron A, Bizousky F. Continuous noninvasive monitoring of respiratory rate in critically ill patients. Chest. 1986;90:632–4. doi: 10.1378/chest.90.5.632. [DOI] [PubMed] [Google Scholar]
- 20.Semmes BJ, Tobin MJ, Snyder JV, Grenvik A. Subjective and objective measurement of tidal volume in critically ill patients. Chest. 1985;87:577–9. doi: 10.1378/chest.87.5.577. [DOI] [PubMed] [Google Scholar]
- 21.Henry M, Seidel JWB, Dains Joyce E, Flynn John A, Solomon Barry S, Stewart Rosalyn W. Mosby's Guide to Physical Examination. Mosby Elsevier; [Google Scholar]
- 22.Pulse Oximetry Training Manual. WHO Press; 2011. [Google Scholar]
- 23.Stewart JV. Vital Signs and Resuscitation. Landes Bioscience; 2003. [Google Scholar]
- 24.Matthes K. Untersuchungen über die Sauerstoffsättigung des menschlichen Arterienblutes [Studies on the Oxygen Saturation of Arterial Human Blood. Naunyn-Schmiedeberg's Archives of Pharmacology. 1935;179:698–711. [Google Scholar]
- 25.Terakura M, Fujisaki R, Suda T, Sagawa T, Sakamoto T. Relationship between blood pressure and persistent epistaxis at the emergency department: a retrospective study. Journal of the American Society of Hypertension : JASH. 2012;6:291–5. doi: 10.1016/j.jash.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Irisawa T, Iwami T, Kitamura T, et al. An association between systolic blood pressure and stroke among patients with impaired consciousness in out-of-hospital emergency settings. BMC Emerg Med. 2013;13:24. doi: 10.1186/1471-227X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoon NS, Jeong MH, Ahn Y, et al. Impact of high-normal blood pressure measured in emergency room on adverse cardiac events in acute myocardial infarction. Korean circulation journal. 2012;42:304–10. doi: 10.4070/kcj.2012.42.5.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Duran L, Balci K, Kati C, Akdemir HU, Kocabicak E, Dogruel C. Has admission blood pressure any prognostic value in patients with subarachnoid hemorrhage: an emergency department experience. Journal of clinical hypertension (Greenwich, Conn) 2013;15:737–41. doi: 10.1111/jch.12177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lalezarzadeh F, Wisniewski P, Huynh K, Loza M, Gnanadev D. Evaluation of prehospital and emergency department systolic blood pressure as a predictor of in-hospital mortality. Am Surg. 2009;75:1009–14. doi: 10.1177/000313480907501032. [DOI] [PubMed] [Google Scholar]
- 30.Lipsky AM, Gausche-Hill M, Henneman PL, et al. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. J Trauma. 2006;61:1228–33. doi: 10.1097/01.ta.0000196694.52615.84. [DOI] [PubMed] [Google Scholar]
- 31.Chen WL, Kuo CD. Characteristics of heart rate variability can predict impending septic shock in emergency department patients with sepsis. Acad Emerg Med. 2007;14:392–7. doi: 10.1197/j.aem.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 32.Barnaby D, Ferrick K, Kaplan DT, Shah S, Bijur P, Gallagher EJ. Heart rate variability in emergency department patients with sepsis. Acad Emerg Med. 2002;9:661–70. doi: 10.1111/j.1553-2712.2002.tb02143.x. [DOI] [PubMed] [Google Scholar]
- 33.Zatzick DF, Russo J, Pitman RK, Rivara F, Jurkovich G, Roy-Byrne P. Reevaluating the association between emergency department heart rate and the development of posttraumatic stress disorder: A public health approach. Biological psychiatry. 2005;57:91–5. doi: 10.1016/j.biopsych.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 34.Shalev AY, Sahar T, Freedman S, et al. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Archives of general psychiatry. 1998;55:553–9. doi: 10.1001/archpsyc.55.6.553. [DOI] [PubMed] [Google Scholar]
- 35.Hsia J, Larson JC, Ockene JK, et al. Resting heart rate as a low tech predictor of coronary events in women: prospective cohort study. BMJ. 2009;338:b219. doi: 10.1136/bmj.b219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ho JE, Bittner V, Demicco DA, Breazna A, Deedwania PC, Waters DD. Usefulness of heart rate at rest as a predictor of mortality, hospitalization for heart failure, myocardial infarction, and stroke in patients with stable coronary heart disease (Data from the Treating to New Targets [TNT] trial) Am J Cardiol. 2010;105:905–11. doi: 10.1016/j.amjcard.2009.11.035. [DOI] [PubMed] [Google Scholar]
- 37.Roghmann MC, Warner J, Mackowiak PA. The relationship between age and fever magnitude. The American journal of the medical sciences. 2001;322:68–70. doi: 10.1097/00000441-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 38.Lee WW, Mayberry K, Crapo R, Jensen RL. The accuracy of pulse oximetry in the emergency department. Am J Emerg Med. 2000;18:427–31. doi: 10.1053/ajem.2000.7330. [DOI] [PubMed] [Google Scholar]
- 39.Van de Louw A, Cracco C, Cerf C, et al. Accuracy of pulse oximetry in the intensive care unit. Intensive care medicine. 2001;27:1606–13. doi: 10.1007/s001340101064. [DOI] [PubMed] [Google Scholar]
- 40.Hanowell L, Eisele JH, Jr, Downs D. Ambient light affects pulse oximeters. Anesthesiology. 1987;67:864–5. doi: 10.1097/00000542-198711000-00057. [DOI] [PubMed] [Google Scholar]
- 41.Cote CJ, Goldstein EA, Fuchsman WH, Hoaglin DC. The effect of nail polish on pulse oximetry. Anesthesia and analgesia. 1988;67:683–6. [PubMed] [Google Scholar]
- 42.Wilson BJ, Cowan HJ, Lord JA, Zuege DJ, Zygun DA. The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective cohort study. BMC Emerg Med. 2010;10:9. doi: 10.1186/1471-227X-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gabayan GZ, Gould MK, Weiss RE, et al. Poor Outcomes After Emergency Department Discharge of the Elderly: A Case-Control Study. Ann Emerg Med. 2016;68:43–51. e2. doi: 10.1016/j.annemergmed.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gabayan GZ, Sarkisian CA, Liang LJ, Sun BC. Predictors of admission after emergency department discharge in older adults. J Am Geriatr Soc. 2015;63:39–45. doi: 10.1111/jgs.13185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sun BC, Mohanty SA, Weiss R, et al. Effects of hospital closures and hospital characteristics on emergency department ambulance diversion, Los Angeles County, 1998 to 2004. Ann Emerg Med. 2006;47:309–16. doi: 10.1016/j.annemergmed.2005.12.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.