Abstract
Asthma morbidity and mortality is higher among older school-age children and early adolescents than other age groups across the lifespan. NIH recommended expanding asthma education to schools and community settings to meet cognitive outcomes that have an impact on morbidity and mortality. Guided by the acceptance of asthma model, an evidence-guided, comprehensive school-based academic health education and counseling program, Staying Healthy—Asthma Responsible & Prepared™ (SHARP), was developed. The program complements existing school curricula by integrating biology, psychology, and sociology content with related spelling, math, and reading and writing assignments. Feasibility, benefits, and efficacy have been established. We compared the effectiveness of SHARP to a non-academic program, Open Airways for Schools, in improving asthma knowledge and reasoning about symptom management. A two-group, cluster-randomized, single-blinded design was used with a sample of 205 students in grades 4–5 with asthma and their caregivers. Schools were matched prior to randomization. The unit of analysis was the student. Certified elementary school teachers delivered the programs during instructional time. Data were collected from student/caregiver dyads at baseline and at 1, 12, and 24 months after the intervention. In multilevel modeling, students enrolled in the academic SHARP program demonstrated significant (p<.001) improvement in asthma knowledge and reasoning over students enrolled in the non-academic program. Knowledge advantages were retained at 24 months. Findings support delivery in schools of the SHARP academic health education program for students with asthma.
Keywords: asthma knowledge, asthma reasoning, self-care, school-based, randomized clinical trial, comparative effectiveness, children, adolescents
More than 7 million children under age 18 years are currently diagnosed with asthma, and each year approximately 4 million children experience exacerbations of asthma symptoms (Akinbami, Moorman, & Liu, 2011). The National Guidelines for the Diagnosis and Management of Asthma (National Heart, Lung, & Blood Institute [NHLBI], 2007) specify that a successful management program includes educating students with asthma and their caregivers about the condition, and doing so beyond health care offices and clinics, in schools and community settings. In response, the Staying Healthy-Asthma Responsible & Prepared™ (SHARP) program, an academic asthma health education and counseling program, was developed for older school-age students with asthma, their family caregivers, and members of their social networks.
The SHARP Program: Background
SHARP (Kintner & Sikorskii, 2009; Kintner et al., 2012; Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015) is based on the acceptance of asthma model (AAM) that was developed through a series of qualitative and quantitative studies (Kintner, 1996, 1997, 2004, 2007) from an ecological approach (Bronfenbrenner, 1979) within a lifespan development perspective (Lerner, 1978, 1986; Santrock, 2010; Sugarman, 1986). In this model, education and counseling programs enhance a student’s knowledge of asthma (Kintner, 1996); reasoning about asthma symptom management, defined as introspective thinking through which situations are examined and options are considered (Kintner, 1997; Kintner, Cook, Hull, & Meeder, 2013); psychosocial acceptance of asthma and beliefs about the nature of asthma; and use of effective self-care behaviors. Knowledge of asthma is the foundation that enables students to reason about asthma symptom management, and that in turn influences psychosocial and behavioral factors that decrease asthma severity and improve condition control, use of healthcare services, school attendance, and quality of life outcomes, including participation in various life activities. The schematic integration of SHARP into the AAM is described (Kintner & Sikorskii, 2009) and depicted (Kintner et al., 2012) elsewhere.
SHARP targets older school-age students with asthma because children aged 9–14 years (a) experience higher amounts of morbidity and mortality than other age groups across the lifespan and (b) are on the cusp of a personal growth trajectory, when they are shifting from relying on their parents to taking more personal responsibility for managing their asthma as they transition from elementary to middle or junior high school.
Nurse specialists in pediatric asthma and psychiatric/mental health counseling developed the program in collaboration with school personnel (e.g., school nurses, administrators, principals, counselors, and teachers) and asthma coalition members (e.g., physicians, respiratory therapists, public health educators, parents of children with asthma, pharmacists, and community partners). To facilitate adoption by schools, SHARP was designed to meet academic benchmarks for grades 4–7 and performance-based assessment activity consistent with grade 5 (Michigan Department of Education [MDE], 2006) by incorporating grade-appropriate spelling words, math problems, and reading and writing assignments. In addition, SHARP was designed to complement existing school curricula by integrating biology, psychology, and sociology content consistent with assessment outcomes focused on the Healthy Lungs for Life program (MDE, 2006). SHARP has two components: a school-based component for students and a community-based component for members of the students’ social network (Kintner & Sikorskii, 2009; Kintner et al., 2012). The school component is the focus of this paper.
Evaluation of SHARP to Date
Feasibility, benefits (Kintner et al., 2012), and efficacy (Kintner & Sikorskii, 2009) of SHARP have been established. Its effectiveness for psychosocial, behavioral, and quality of life outcomes compared to a well-established non-academic asthma education program, Open Airways for Schools (OAS; Clark et al., 2004; Evans et al., 1987), has been reported elsewhere (Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015).
The purpose of this paper is to report the effectiveness of SHARP compared to OAS for improving cognitive outcomes of asthma knowledge and reasoning about asthma symptom management. The research question was: What is the effectiveness of SHARP compared to OAS for improving cognitive outcomes of asthma knowledge and reasoning about asthma symptoms management in fourth- and fifth-grade students with asthma at 1, 12, and 24 months post-intervention? Compared to grade 4–5 students enrolled in elementary schools who received OAS, students in schools who received SHARP were hypothesized to have a greater increase in (a) knowledge of asthma and (b) logical reasoning abilities for managing acute exacerbation of asthma symptoms.
Methods
Design
A two-group prospective cluster-randomized single-blinded design conducted with two cohorts was implemented, with randomization occurring by school. In the cluster-randomized design, randomization to intervention was at the level of the group, in this case the school, while data were analyzed at the level of the individual, in this case the student. This approach takes into account the potential for greater similarity of participants within groups that share geographic, demographic, or organizational characteristics by accounting for shared variance. Evaluators were blinded to program allocation.
Human Subjects Protections
The study was in full compliance with the Helsinki Declaration, Health Insurance Portability and Accountability Act (HIPAA), and Family Education Rights and Privacy Act (FERPA). Prior to data collection, human subjects approval was obtained through two university institutional review boards (IRBs) and the target school district.
All research team members (i.e., the principal investigator, co-investigator, and research associate; study consultants, statisticians, and research assistants; and the site coordinators overseeing day-to-day management of the study; participant coordinators responsible for tracking and monitoring student/caregiver dyads over time; recruiters who were subcontracted employees of the school district; evaluators responsible for data collection; and school teachers responsible for delivery of the programs) were (a) certified in the protection of human subjects, HIPAA, and FERPA, (b) trained in study protocols and procedures consistent with their position descriptions, including recruitment, enrollment, data collection and management, program delivery, quality assurance, and evaluation, and (c) had references and criminal background checks.
De-identified data files were labeled using coded identification numbers. All participant-signed documents were stored separately from the data. No unanticipated events were reported.
Sample Size
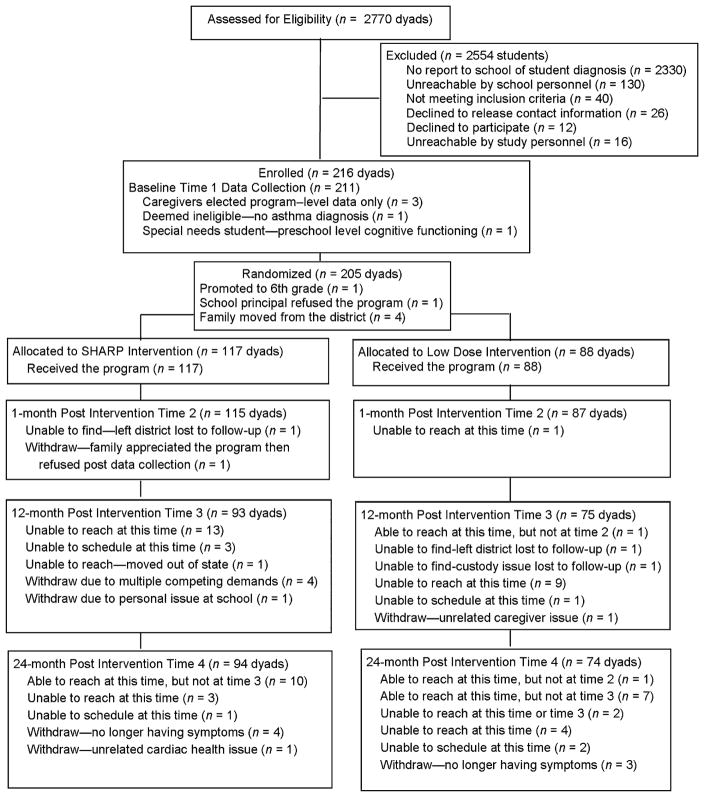
The partner district provided 23 elementary schools for participation. To identify the sample size needed to demonstrate significant effects, a priori power analysis was conducted based on public enrollment data for each school and the estimated 10% incidence/prevalence of asthma in the target community. We calculated minimum detectable effect size (Cohen, 1988; Murray, 1998; Raudenbush, 1997), the smallest impact of the intervention that can be detected with statistical power of at least .80 and level of significance alpha .05 for two-tailed tests, based on previous studies (Horner, 1998; Kintner & Sikorskii, 2009; Kintner et al., 2012). The results of the multi-level power analysis indicated that a post-attrition sample size of six students per school, or 138 dyads, at 24 months post-program would be sufficient across all measures. Based on our previous studies (Kintner & Sikorskii, 2009; Kintner et al., 2012), we set the retention rate low, at 67% over 34 months. This required sampling a minimum of nine students per school, or 207 dyads, to allow for potential striation. Eligibility, screening, enrollment, randomization, participation, and follow-up numbers are shown in a CONSORT chart (see Fig. 1).
FIGURE 1.
The CONSORT E-flowchart for caregiver/student dyad participants.
Group Assignment
The 23 schools were matched prior to randomization based on school-level public data, specifically enrollment numbers, standardized reading and math scores, free/reduced lunch eligibility, and the proportion of racial/ethnic group enrollment. The gmatch macro (Kosanke & Bergstralh, 2004), which implements the greedy matching algorithm as a multivariate distance measure, was used to match similar pairs of schools. Then, one in each pair was randomly assigned to the SHARP or OAS group. Twelve schools were assigned to the treatment group and 11 schools to the control group.
Student Eligibility and Recruitment
Eligibility
Participating schools were located in a diverse, primarily minority, moderately sized, medically under-served, and low socioeconomic inner-city community. Two cohorts of student/caregiver dyads were recruited in fall 2009 and 2010, and programs were delivered in spring 2010 and 2011.
A convenience sampling method was used to recruit students who met inclusion criteria. Student eligibility criteria included (a) a diagnosis of asthma, documented by asthma action plans on file in the schools that had been completed by healthcare providers (further documentation of diagnosis in self-report or chart reviews was not sought), (b) availability to participate in scheduled classes or make-up sessions, and (c) verbal and written assent and parent written informed consent to participate in the study. Caregiver eligibility criteria included (a) being a caregiver of a student with asthma, (b) ability to understand English, and (c) expressed availability to participate in study-related activities. Caregivers included biological parents, extended family members, or foster parents with knowledge of the student, the student’s health history, and current health status.
Recruitment
Notification packets prepared by the research team were mailed to caregivers of all fourth-grade students in May of 2009 and all third-and fourth grade students in May of 2010, alerting all families in the district of the study according to school policy so as not to target any one subset of the district’s population (i.e., students with asthma action plans on file with the school). Notification packets included a letter of introduction, a study brochure, an asthma screening tool, and two examples of an asthma action plan.
Recruitment packets with cover letters, colorful brochures, response forms, and postage-prepaid envelopes were mailed from the school district to caregivers of all fifth-grade students in September 2009, and all fourth- and fifth-grade students in September 2010, inviting participation. Families interested in learning about the study were asked to contact the research team. Two weeks after the recruitment letters were mailed in the fall, a school counselor who served as a paid trained recruiter made follow-up phone calls during evening and weekend hours, extending invitations to caregivers of students with asthma action plans on file.
Enrollment
Information on 205 families who were eligible, expressed interest, and agreed to be contacted was shared by the district with the research team’s participant coordinator. The participant coordinator arranged appointments for study enrollment and baseline data collection at a day, time, and location convenient for the dyads and evaluators. She began the consent process with the initial contact by verbally informing potential participants of the purpose and nature of the study and requirements, their responsibilities, and risks and benefits.
At the baseline visit, project evaluators were responsible for reading the consent and assent forms aloud, answering questions, and obtaining informed written caregiver consent and student assent. Throughout the study, students and caregivers were informed and reminded that their decision about study participation would not affect access to school-based supports or services. Only students enrolled in the study participated in the programs.
Interventions
Staying Healthy–Asthma Responsible & Prepared™ (SHARP)
Students enrolled in schools randomized to SHARP received ten 50-minute workbook-guided school sessions (Kintner & Sikorskii, 2009; Kintner et al., 2012). Detailed descriptions of the program’s curriculum and specifics on program delivery of the program are presented elsewhere (Kintner & Sikorskii, 2009; Kintner et al., 2012; Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015).
Open Airways for Schools (OAS)
Students enrolled in schools randomized to OAS received six 50-minute school lessons and took home handouts. Detailed descriptions of the program’s curriculum and specifics on program delivery of the program are presented elsewhere (Clark et al., 2004; Evans et al., 1987). Written permission from the American Lung Association was obtained to allow the program to be used in the control schools.
Teachers
Ten recently retired certified elementary school teachers, identified by the district, were hired, randomly assigned to SHARP or OAS, and trained to deliver their respective program in schools during instructional time. Retired teachers were recruited because they often seek to maintain connections with the schools, students, and caregivers. Certified elementary school teachers are educated to instruct students in diverse subject matter using a variety of techniques and methods. Teachers were trained and supervised by nurse specialists in pediatric asthma and psychiatric/mental health counseling (Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015).
Teacher training provided background on the study’s clinical problem, purpose, aims, significance, and relevance as well as preliminary work, theoretical framework, design and methods, timelines, future directions, and roles and responsibilities of the position. Teachers were responsible for implementing all school-related components of the study according to protocols, including delivering all sessions of their assigned program to students enrolled in the study and participating in evaluation procedures and quality assurance reviews. All procedures from pre-session organization through post-session review for each program were described in detail, including protocols for ensuring participant confidentiality.
Although five teachers had some personal or family experience with asthma, overall teacher knowledge of the condition was limited. Teachers in both treatment groups were provided with general asthma health information including (a) the anatomy, physiology, and pathology of asthma; (b) symptoms indicating severity of condition and episodes; (c) stimuli that could lead to exacerbation of symptoms; (d) medications used to control or relieve symptoms; (e) health promotion, risk reduction/prevention, and episode management behaviors; (f) early adolescent thoughts, feelings, and beliefs about asthma; (g) older school-age student reasoning about managing asthma situations; and (h) quality of life as evidenced by unrestricted participation in life activities.
Teachers in each treatment group were presented with the overall purpose and specific aims of their program (SHARP or OAS). The purpose, outcome learning objectives, content outlines, teaching and learning activities, materials and supplies, and evaluation methods for each of sessions were outlined, explored, and reviewed. Lectures, discussion, role-play, and hands-on demonstrations were used to facilitate processing of content. Teachers practiced demonstrations and trainers provided feedback until consistency was displayed and teachers expressed comfort with the content. Program-specific communication that fostered responsive and collaborative interactions between the teachers and research team members was maintained using restricted-access discussion forums located on the study’s password- and firewall-protected website. Program-specific weekly meetings with teachers and trainers were conducted so teachers could reflect on delivered sessions and prepare for upcoming sessions.
Fidelity
Teachers completed attendance and participation forms for each student to document dosage. All students received all content of their respective programs delivered according to written policies and procedures. Standardized checklists were also completed by teachers following each class session to ensure delivery according to detailed protocols. All interactions between teachers and students were digitally audio-recorded. Individual teachers and designated team members completed fidelity checklists using the audio-recorded files to monitor adherence to written policies and procedures and to minimize experimental drift. Designated team members reviewed attendance and participation forms and session and fidelity checklists for quality assurance.
Data Collection
Data were collected from participants using audio-linked, password-protected electronic databases loaded on password-protected and encrypted laptop computers. Pairs of evaluators, blinded to treatment condition, collected data at baseline and at 1, 12, and 24 months post-program from dyads in their home. A 75-page evaluator training manual was developed and used to standardize data collection. Training included role expectations, qualifications, requirements, and responsibilities. Procedures for (a) securing data safety and personal and participant safety and confidentiality and (b) monitoring and reporting potential unanticipated events were highlighted. Training was implemented using lectures, discussions, role-play, and hands-on learning activities. Feedback and support were offered with frequent reference to the training manual. Ongoing communication between research team members was maintained using a restricted-access discussion forum located on the study’s website. Timely announcements, comments, concerns, issues, and questions posted to the discussion forum fostered responsive and collaborative interactions.
The scope of the study required that evaluators conduct at least three data collection sessions per week over a 12-week period. The participant coordinator telephoned 24 hours before scheduled appointments to confirm meeting times, remind families that sessions would be audio-recorded, and share the first names of the evaluators. The designated evaluator telephoned 1 hour before the scheduled appointment to reconfirm the session. The participant coordinator telephoned participants 24 hours after the meeting to confirm that data were collected without incident and that participants had received their monetary awards. Evaluators were compensated at a flat rate per session.
Data were collected through electronic audio-linked surveys completed by the student and caregiver individually with the support of one of the evaluators. All data collection sessions were audio-recorded with two digital recorders, one for each respondent, for quality monitoring and assurance. Before leaving the collection site, caregiver and student response options were reviewed for completeness, accuracy, and consistency, and a standardized checklist was completed by the evaluators to confirm that protocol was followed. At each data collection time point, both students and caregivers were offered a cash award (Kintner et al., 2012) of $15 each ($30/dyad) to acknowledge their time and effort in completing surveys. At baseline, caregivers completed all five surveys in 0:16–2:19 hours:minutes (M =1:06, SD =0:24), with variation partially due to survey skip patterns (i.e., reporting environmental and food allergies and use of healthcare services information), and students completed their five surveys in 0:40–3:12 hours:minutes (M =1:32, SD=0:22), with breaks based on individual attention span and reading ability.
Outcome Measures
Self-report measures were used. Internal consistency reliability, stability, construct validity, readability, and age appropriateness were considered when selecting instruments. Caregivers completed the General Health History Survey (Kintner, 1996, 2009) and four additional instruments not reported here. Students completed the Knowledge of Asthma Survey (Kintner, 1996), the Reasoning about Asthma Scenarios (Kintner et al., 2013), and three additional instruments not reported here.
General health history survey (GHHS)
Completed by the caregiver, this 39-item instrument was used to collect demographic and asthma-related information (Kintner, 1996, 2004, 2007, 2009). Three items contained in the survey were used to compute the family’s socioeconomic status (Nam & Powers, 1983)
Knowledge of asthma survey (KAS)
This survey, titled “What I Know about Asthma,” is an 18-item fill-in-the-blank/multiple-choice quiz measuring level of knowledge about asthma. Six objectives were specified as the basis for the survey. Students with asthma and their caregivers should be able to: (a) name 10 anatomical parts of the respiratory system, (b) describe the physiology of asthma, (c) distinguish symptoms of respiratory distress, (d) discuss stimuli (triggers) to symptom exacerbation, (e) contrast five classifications of medications used to effectively treat asthma, and (f) assess the use of self-care techniques used to manage symptoms.
The items test knowledge of facts related to anatomy and physiology, signs and symptoms, stimuli or triggers, medical treatments, and asthma self-management techniques (Kintner, 1996, 2004, 2007; Kintner & Sikorskii, 2009; Kintner et al., 2012). For the single fill-in-the-blank item naming 10 parts of the respiratory system, a composite score is computed by multiplying the correct number of identified body parts by .30; scores range from 0 to 3. For items 2 through 18, each correct multiple-choice response is awarded one point; total scores range from 0 to 17. The composite fill-in-the blank score and the multiple-choice score are summed to compute a total score (range 0–20). Stability and validity are reported elsewhere (Kintner & Sikorskii, 2009; Kintner et al., 2012).
Reasoning about asthma scenarios (RAA)
This four-scenario information processing survey completed by students, titled “What I Would Do,” was used to measure reasoning abilities for managing asthma symptoms (Kintner et al., 2013). Students are directed to read each scenario and then respond to eight questions by circling the most appropriate response option(s). Scoring captures logical reasoning for each student within each of the four scenarios or items. Predetermined scores are provided by scenario for each response option to questions 1–4 and 6–8. Students receive 0 points for less logical responses, 1 point for more logical responses, and 2 points for most logical responses. First, mean scores for responses to questions 1–4 and 6–8 are computed and then a composite mean score rounded to the third decimal point for each scenario is computed. Finally, a grand mean score for the four-scenario scale is computed. Scores are considered continuous and can range from 0.000 to 2.000, with higher scores reflecting increased logical reasoning abilities. Internal consistency reliability assessed using Cronbach’s alpha coefficient for this sample was .80. Factor analysis confirmed strong loadings of .69–.86 on a single factor accounting for 60% of the explained variance.
Data Analysis
Immediately following data collection, all data entry and quality monitoring files were labeled and uploaded to a restricted-access drop box located on a firewall-protected, dedicated server. File transfer was accomplished using a data encryption system in combination with high-assurance identification numbers and passwords. All data entry files were merged into one relational systems file at the primary site. Raw data were downloaded into SPSS for analysis.
SPSS for Windows 19 (IBM SPSS, 2010) was used for computing descriptive statistics. We tested for differences by group in individual, family, and school characteristics at baseline to uncover potential sources of bias due to randomization at the school level using parametric and non-parametric tests for cross-group comparisons.
Missing data
Data for all covariates were complete, with the exception of school writing proficiency (9.76%) and severity of asthma (2.93%). The cognitive outcome of asthma knowledge had 1.46% missing data at baseline, 2.93% at post-test, 19.02% at 1-year follow-up, and 18.54% at 2-year follow-up. The cognitive outcome of reasoning about asthma had 1.46% missing data at baseline, 4.39% at post-test, 19.02% at 1-year follow-up, and 18.54% at 2-year follow-up.
Multiple imputation was used to account for missing data, following best-practice recommendations (Graham, 2009). Inferential statistics derived from multiple imputed data sets produce valid inferential statistics by replacing missing data with plausible values in multiple data sets and then combining results from analyses across all imputed data sets. Inferential tests incorporate within and between variability in the model parameter’s standard errors. Imputation was performed using the R Amelia package (Honaker & King, 2010), which uses longitudinal information to impute plausible values for missing data, using a bootstrapping approach to simulate uncertainty in imputed values. We established 20 data sets in which missing data were replaced with imputed values and identically analyzed. After analyzing individual data sets, parameter estimates and standard errors were combined using Rubin’s formulas (Rubin, 1987). All continuous variables were mean-centered prior to data imputation to aid in the interpretation of model coefficients.
Multilevel models
Multilevel models were fit using the R lme4 package (Bates, Maechler, & Bolker, 2013; Gelman & Hill, 2007). Models contained two levels: time points and participants. All models contained a random intercept for participant, thus accounting for the non-independence of observations. We followed longitudinal model-building recommendations (Singer & Willett, 2003). Several viable unconditional growth models (i.e., models with time variables and no other independent variables) were fit and then compared using the Akaike information criterion (AIC), following guidelines from Burnham and Anderson (2002), to determine which model was the best representation of longitudinal change for each outcome. After establishing the best unconditional growth model, person-level variables (e.g., intervention condition) were added to the model.
Unconditional growth models
For each outcome, a piecewise model was developed in two phases. The piecewise model allowed us to address the following: (a) was there an overall pre-post change regardless of treatment condition (i.e., pre-post change), (b) did the pre-post change differ across conditions (i.e., SHARP x pre-post change), (c) was there a difference by condition at post-test (i.e., SHARP main effect), (d) was there an overall change in the outcome after the intervention regardless of condition (i.e., post change), and (e) did post-intervention change differ across conditions (i.e., SHARP x post change).
The first time period was pre- to post-intervention change (henceforth referred to as pre-post change), which accounted for change between the pre-test assessment and the post-test assessment. All models included a pre-post change parameter, which represented change across all study participants irrespective of condition, as well as an interaction between pre-post change and condition, which represented differential pre-post change across conditions (e.g., SHARP participants’ knowledge increased more than did that of Open Airway participants).
The second time period represented change over time across the three post-test assessments, hereafter referred to as post change. Because the second period included multiple time points, we evaluated several models of change, including no change, linear change, log-linear change, and quadratic change, and compared AIC values to determine the best unconditional growth model for each outcome. For outcomes for which the no-change model was the best fit, we did not include a second time parameter because the outcome was equivalent across the three follow-up points.
If a no-change model was selected for the second time period, the SHARP main effect represented the average differences in the outcome across all follow-up assessments. The linear, log-linear, and quadratic change models included an interaction between SHARP and the putative time parameter, which, if significant, indicated differential change in the outcome by condition across the follow-up period.
Models with covariates
After the longitudinal model was established, we simultaneously entered all covariates, a variable indicating SHARP participation that was dummy-coded so that SHARP participants were coded 1 and OAS participants were coded 0, and interactions between SHARP participation and time terms. The outcome at baseline, SHARP participation (v. OAS participation), pre-post change, SHARP participation x pre-post change, post change if applicable, and SHARP participation x post change if applicable were included in all covariate models.
The following covariates were included in all models (dummy-coded variables include the comparison group in parentheses): female (v. male), age of student, fifth grade (v. fourth grade), African American (v. non-Hispanic White), Hispanic (v. non-Hispanic White), time since diagnosis, stimuli of allergies, stimuli of exercise, prescribed long-acting bronchodilator, prescribed inhaled steroid, family socioeconomic status, school reading proficient overall percentage, school writing proficient overall percentage, school math proficient overall percentage, and severity of asthma.
We computed simple slope contrasts (Bauer & Curran, 2005) at each assessment point to compare SHARP and OAS participants, which aided our interpretation of SHARP x time interaction effects. Contrasts were computed using simple slope comparisons using the R Contrast package (Kuhn, Weston, Wing, & Forester, 2011) for the 20 imputed data sets, and parameters were combined in manner described above. Effect sizes at each assessment point were derived by dividing the difference between the estimated means of treatment groups by the baseline standard deviation, which produces an effect size (dGMA-raw) in a longitudinal change model that is equivalent to traditional effect sizes, such as Cohen’s d (Feingold, 2009).
Results
Sample Description
The sample consisted of 205 grade 4–5 students ages 9–12 years (M =10.02, SD =.70) diagnosed with asthma and their caregivers. Males accounted for 60%. Students were primarily Black (43%), mixed Black and White (13%), and non-Hispanic White (23%), and were from single-parent households (69%) with lower (59%) to low-middle (34%) socioeconomic status. Severity of asthma ranged from mild intermittent (55%) to moderate persistent (37%) and severe persistent (8%), with 77% prescribed oral steroids at some point in their lives, 59% prescribed daily controller medications, 42% prescribed inhaled steroids, 71% reporting one or more urgent care visits for exacerbation of asthma symptoms, and 36% requiring one or more hospitalizations
When surveyed at the 24-month follow-up, caregivers (n =168) were primarily female (88%) ranging in age from 19 to 69 years (M =39, SD =8) and consisted of biological parents (88%), grandparents (6%), legal guardians (4%), step-parents (2%), and extended family members (2%). School-level proficiency in reading was 68–95% (M =85.16, SD =5.25), writing 10–50% (M =39.91, SD =8.27), and math 67–95% (M =86.51, SD =5.80).
Predictors of Asthma Knowledge and Reasoning
Asthma knowledge
We observed a main effect for the pre-post (t[184]=5.28, p<.001) change in asthma knowledge, indicating an average increase from pre- to post-intervention for all participants in both groups. A main effect for months (t[160] =3.14, p=.002) demonstrated an increase in asthma knowledge across post-test assessments for participants in both groups. The SHARP main effect was significant (t[169]=4.34, p<.001), indicating that SHARP participants exhibited higher levels of asthma knowledge at post-test. The SHARP participation x pre-post interaction also was significant (t[180]=4.15, p<.001), indicating that the SHARP participants exhibited a greater increase between pre- and post-test assessments than OAS participants. The SHARP participation x month interaction was not significant (t[170]=−1.57, p=.118), indicating that the higher level of asthma knowledge among SHARP participants at post-test was maintained throughout the follow-up assessments. This was borne out in the contrasts at each assessment: SHARP and OAS participants did not differ at pre-test (t[186]=−1.01, p=.315, dGMA-raw =−0.15), but SHARP participants exhibited higher levels of asthma knowledge at post-test (t[169]=4.34, p<.001, dGMA-raw = 0.61), 1-year follow-up (t[162] =4.47, p<.001, dGMA-raw = 0.46), and 2-year follow-up (t[162]=2.11, p=.036, dGMA-raw = 0.30).
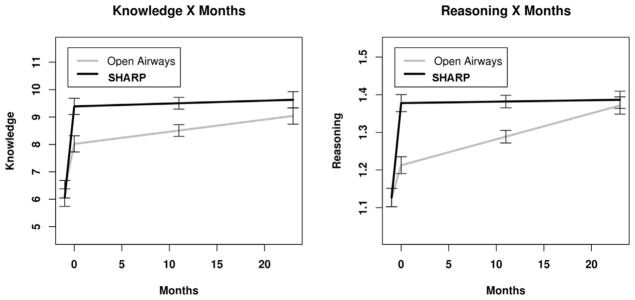
Means and standard deviations for the SHARP and OAS participants are presented in Table 1. Parameter estimates for asthma knowledge are presented in Table 2. Fitted values for the model with standard errors of the difference for simple slope estimates of SHARP versus OAS participants at each assessment point are displayed in Figure 2.
Table 1.
Knowledge and Reasoning Scores for Open Airways and SHARP Participants at Each Assessment
| Outcome | Pretest
|
1-Month Posttest
|
12-Month Follow-Up
|
24-Month Follow-Up
|
||||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | M | SD | |
| Knowledge | ||||||||
| Open airways | 6.31 | 2.13 | 7.85 | 2.34 | 8.47 | 2.48 | 9.00 | 2.51 |
| SHARP | 6.09 | 2.27 | 9.41 | 2.79 | 9.47 | 2.85 | 9.70 | 2.89 |
| Reasoning | ||||||||
| Open airways | 1.12 | 0.20 | 1.21 | 0.20 | 1.29 | 0.21 | 1.36 | 0.21 |
| SHARP | 1.13 | 0.19 | 1.40 | 0.21 | 1.37 | 0.21 | 1.40 | 0.21 |
Note. SHARP, Staying Healthy–Asthma Responsible & Prepared™; M, mean; SD, standard deviation.
Table 2.
Parameter Estimates for Models of Effects of Covariates, SHARP, and OAS on Asthma Knowledge and Reasoning
| Parameter | Asthma Knowledge
|
Asthma Reasoning
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | df | t | p | B | SE | df | t | p | |
| Intercept | 5.33 | 0.51 | 159 | 10.47 | <.001 | 0.51 | 0.06 | 159 | 8.41 | <.001 |
| Baseline cognitive | 0.48 | 0.05 | 162 | 10.48 | <.001 | 0.60 | 0.04 | 152 | 13.85 | <.001 |
| Female | 0.07 | 0.20 | 173 | 0.34 | .736 | 0.01 | 0.02 | 168 | 0.74 | .460 |
| Age of student | −0.21 | 0.20 | 155 | −1.05 | .297 | −0.02 | 0.02 | 132 | −1.48 | .141 |
| Fifth grade | 0.72 | 0.29 | 153 | 2.45 | .015 | 0.03 | 0.02 | 153 | 1.39 | .167 |
| African American | −0.32 | 0.22 | 162 | −1.49 | .138 | −0.02 | 0.02 | 146 | −1.12 | .264 |
| Hispanic | 0.48 | 0.33 | 173 | 1.44 | .151 | 0.00 | 0.03 | 157 | 0.16 | .877 |
| Time since diagnosis | 0.04 | 0.04 | 162 | 0.90 | .368 | 0.00 | 0.00 | 131 | 0.58 | .564 |
| Stimuli of allergies | −1.10 | 0.28 | 158 | −3.97 | <.001 | 0.01 | 0.02 | 172 | 0.62 | .538 |
| Stimuli of exercise | 0.16 | 0.24 | 147 | 0.66 | .510 | 0.00 | 0.02 | 161 | 0.16 | .872 |
| Prescribed long-acting bronchodilator | 0.15 | 0.27 | 170 | 0.56 | .574 | −0.01 | 0.02 | 131 | −0.52 | .606 |
| Prescribed inhaled steroid | 0.01 | 0.22 | 167 | 0.06 | .950 | 0.02 | 0.02 | 161 | 0.91 | .366 |
| Family socioeconomic status | 0.01 | 0.01 | 150 | 1.46 | .147 | 0.00 | 0.00 | 157 | 0.38 | .701 |
| Reading proficient % overall | 0.06 | 0.03 | 162 | 2.06 | .041 | 0.00 | 0.00 | 156 | 0.31 | .754 |
| Writing proficient % overall | 0.00 | 0.02 | 121 | 0.19 | .851 | 0.00 | 0.00 | 94 | 0.64 | .525 |
| Math proficient % overall | −0.05 | 0.03 | 151 | −1.87 | .064 | −0.00 | 0.00 | 158 | −0.26 | .794 |
| Severity of asthma | 0.10 | 0.06 | 155 | 1.62 | .107 | −0.00 | 0.00 | 156 | −0.03 | .979 |
| SHARP participation | 1.34 | 0.31 | 169 | 4.34 | <.001 | 0.16 | 0.02 | 165 | 6.88 | <.001 |
| Pre-post | 1.59 | 0.30 | 184 | 5.28 | <.001 | 0.09 | 0.02 | 177 | 3.85 | <.001 |
| SHARP participation X pre-post | 1.66 | 0.40 | 180 | 4.15 | <.001 | 0.16 | 0.03 | 176 | 5.34 | <.001 |
| Months | 0.04 | 0.01 | 160 | 3.14 | .002 | 0.01 | 0.00 | 157 | 6.10 | <.001 |
| SHARP participation X month | −0.03 | 0.02 | 170 | −1.57 | .118 | −0.01 | 0.00 | 150 | −4.18 | <.001 |
Note. SHARP, Staying Healthy–Asthma Responsible & Prepared™; OAS, Open Airways for Schools; SE, standard error.
FIGURE 2.
Fitted asthma knowledge and reasoning values for SHARP and open airways participants with ±one standard error of the difference for simple slope estimates of SHARP versus open airways participantsat each assessment point.
Reasoning about asthma symptom management
We observed a main effect for the pre-post (t[177] =3.85, p <.001) change in reasoning about asthma symptom management, indicating an average increase from pre- to post-test for all participants in both groups, and a main effect for months (t[157] =6.10, p <.001), indicating that there was an increase in reasoning across post-test assessments for all participants. The SHARP main effect was significant (t[165] =6.88, p <.001), indicating that SHARP participants exhibited higher levels of reasoning at post-test. The SHARP participation x pre-post interaction was significant (t[176] =5.34, p <.001), indicating that the SHARP participants exhibited a greater increase between pre- and post-test assessments than OAS participants. The SHARP participation x month interaction also was significant (t[150] =−4.18, p <.001), indicating that the reasoning advantage that SHARP participants exhibited over OAS participants at post-test decreased across the follow-up assessments. This can be seen in the contrasts at each assessment: SHARP and OAS participants did not differ at pre-test (t[184] =0.01, p =.993, dGMA-raw = 0.00), SHARP participants exhibited higher levels of reasoning at post-test (t[165] =6.88, p <.001, dGMA-raw = 0.86) and at 1-year follow-up (t[162] =5.51, p < .001, dGMA-raw = 0.51), but not at 2-year follow-up (t[147] =1.00, p =.317, dGMA-raw = 0.13). Parameter estimates for reasoning on asthma management are presented in Table 2. Fitted values for the model with standard errors of the difference for simple slope estimates of SHARP versus OAS participants at each assessment point are displayed in Figure 2.
Discussion
Multi-level modeling was used to describe the trajectory of intra-personal patterns of change in knowledge and reasoning over time: specifically, the initial state (intercept), rate of change (slope), and stability (residual). Students in the academic health education and counseling SHARP program experienced steep increases in knowledge of asthma and reasoning about symptom management that were sustained over time with moderate to large effect sizes, whereas students in the non-academic OAS program demonstrated an expected pre- to 1-month post-program increase that slowly continued to increase over time with age and, presumably, opportunistic learning. In addition, students who received SHARP had a sustained advantage in knowledge, although not in reasoning, over the ensuing 24 months.
Delivered by trained, certified elementary school teachers in schools during instructional time, the academic SHARP program demonstrated superior effectiveness over the non-academic OAS program at post-test. Whereas differences between the groups on reasoning decreased over time, as students who received the non-academic program gradually gained in symptom management reasoning to equal students who received SHARP, differences between groups for asthma knowledge remained significant for all follow-up time points. The findings suggest that the SHARP approach to enhancing students’ knowledge about asthma is effective and worthy of dissemination.
Limitations
Historical events, using community members as evaluators, and generalizability of findings were potential limitations. The economic crisis in Michigan from 2008 to 2013 had an impact on the study’s implementation. In 2007, prior to the study, school administrators classified more than 70% of families as mobile and unreachable, and during implementation of the study, the target population of primarily low-income, inner-city, minority families became more mobile and even less reachable. Students moved from one caregiver to another and beyond state lines. In the US and state censuses, the population decreased by 5%, and the unemployment rate increased to 16%. Half of the schools in the district were closed, principals were responsible for supervising more than one school, and senior school teachers and junior faculty were downsized. As a result, tracking participants over time and distance was exceedingly challenging and required diligence. However, because of the combined efforts of our participant coordinator and a school counselor who served as our liaison to the district, attrition was limited to 17% over the three years.
Threats to design validity (Edgren et al., 2005; Fawcett et al., 2008) were considered when making decisions about evaluators responsible for data collection. We chose to use a community-based participatory research approach (Christopher, Watts, McCormick, & Young, 2008; Jones & Wells, 2007; MacQueen et al., 2001; Uyeda, Bogart, Hawes-Dawson, & Schuster, 2009) to build trust and encourage active participation between community members and investigators. Evaluators, recruited from the community, included multi-lingual male and female professionals (i.e., respiratory therapists, registered nurses, physicians, social workers, counselors, psychologists, pharmacists, school teachers, and school and hospital administrators) of diverse race and ethnic backgrounds. They were selected based on personal professionalism, availability, responsibility, trustworthiness, commitment, and trainability. Prior to joining the research team, many of the evaluators were familiar with asthma management. Concerned that the evaluators would share their knowledge of asthma with the study participants, evaluators were directed not to intervene should participants ask questions about asthma, and scripted prompts were used to reassure families that questions would be addressed during delivery of the program but not during data collection. By using professionals from the community, high-quality data were collected safely and efficiently, and confidentiality was maintained.
The study was funded to target low-income, inner-city, medically underserved, racially, and ethnically diverse students with asthma enrolled in fourth and fifth grades. The programs were delivered in English to students in an English-language academic environment. Larger sample sizes from more diverse communities are needed to fully confirm generalizability of findings.
Implications for Clinical Practice
Advantages of the school setting
Asthma education delivered during high-stress and time-limited offices/clinic visits, emergency/urgent care, and overnight hospital stays relies primarily on provision of simple pamphlets that lack the depth and breadth of information required to manage an ongoing, life-long, and potentially life threatening condition. SHARP uses a collaborative and interdisciplinary team of health care professionals, educators, and community partners to extend and expand education of students with asthma and their families beyond health offices and clinics to schools and community settings (Kintner & Sikorskii, 2009; Kintner et al., 2012; Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015). Our findings indicate that school-based programs have the potential to extend the duration of involvement and expand the depth and breadth of content required to effectively manage asthma. In addition, schools are a key delivery system for the target age group because: (a) students spend the majority of their waking hours in school, making it a critical place to access and intervene with families, (b) the traditional setting for student learning is in schools during school hours, and (c) students actively engaged in the learning process in school settings are more inclined to absorb, process, and retain content. Moreover, schools provide a logical place to deliver counseling interventions because students reported that many of the psychosocial issues they encountered were associated with school situations and activities (Kintner, 1997).
Overcoming resistance to use of class time
Approved by the curriculum committees of the target school district, SHARP was readily accepted and welcomed as an academic program to be delivered in schools during instructional time. However, some school administrators, principals, and teachers familiar with OAS were resistant to approving the non-academic OAS program for delivery during instructional time (Bruzzese, Evans, & Kattan, 2009). They wanted instructional time to be dedicated to academic programs. In negotiations, we stressed the importance of equitable delivery of both programs for purposes of evaluation with school personnel. As the study was initiated, however, and school personnel were provided the names of students with asthma enrolled in the study, principals, office staff, and teachers realized that they were unaware that many of the students had asthma; the school staff readily connected the asthma diagnoses with school absenteeism. Further support for the SHARP program was obtained when classroom teachers informally quizzed SHARP students about what they were learning and were impressed by what the students shared. School personnel developed a new understanding that health is essential for learning as a result of this study and requested additional information and training in asthma management.
School teachers as interventionists
Historically, brief presentations on asthma have been provided in schools and community settings, not by teachers but by physicians, school nurses, respiratory therapists, trained health educators, social workers, pharmacists, parents of children with health conditions, and community members (Ahmad & Grimes, 2011; Clark et al., 2004; Findley et al., 2011; Magzamen, Patel, Davis, Edelstein, & Tager, 2008). In addition, asthma health education programs for schools were designed for early elementary students as non-academic, “pull out” programs to be delivered by facilitators who may or may not have had professional health or formal training as educators (Ahmad & Grimes, 2011; Bruzzese, Markman, Appel, & Webber, 2001; Bruzzese et al., 2011; Coffman, Cabana, & Yelin, 2009; Clark et al., 2004, 2010; Evans, Clark, Levison, Levin, & Mellins, 2001; Evans et al., 1987; Horner, 1998; Kaplan et al., 1986). These earlier programs were not explicitly designed to meet academic requirements.
In this study, recently retired certified elementary school teachers identified by the district delivered the programs. These teachers possessed a passion for teaching children and the keen ability to capture students’ attention and keep them focused and engaged. They were readily accepted by district administrators and board members; school principals, office staff, and support personnel; and regular classroom and specialized teachers as well as students and their family members. Because they were familiar with the district and school environment (e.g., access and resources), routines (e.g., announcements and assemblies), emergency processes (e.g., fire or smoke alarms, weather alerts, and lockdowns drills), and unanticipated changes in the academic schedule (e.g., special events and field trips), they were able to negotiate and navigate school-related, politically dynamic situations.
The certified elementary teachers possessed a comprehensive perspective on the overall district-wide core curricula and were able to determine how well programs met grade-level content, benchmarks, and assessment criteria. They expected to follow standardized curricula with purpose statements, outcome learning objectives, content outlines, teaching/learning activities, and assessment methods. They were able to facilitate the academic (i.e., spelling, math, reading, science, and writing) as well as counseling (i.e., personal sharing, interpersonal discussions, and creative expressions) aspects of the SHARP program. As trained and experienced instructors, they were able to structure individual class sessions. Because they understood the developmental needs and issues of older school-age students, the teachers were also able to efficiently manage dynamic classroom settings. Teachers supported student processing of content by introducing new information, providing clear and concise summaries, and meaningfully applying content to students’ life experiences. Teachers were able to foster each student’s unique cognitive and learning abilities as well as address diverse psychological, social, and behavioral issues as they arose.
Teachers randomized to deliver SHARP were initially challenged with asthma-specific content and required clarification and mentoring from school nurses, whereas those teachers randomized to deliver OAS continually struggled to avoid augmenting the program with academic teaching and learning activities. After delivering the programs, when both programs were shared with all teachers, teachers unanimously stated their preference for the academic SHARP program.
Application for Theory Development
Findings of this study support relationships posed in the acceptance of asthma model. Providing students with foundational knowledge of asthma and advancing reasoning abilities for managing asthma symptoms has the potential to influence psychosocial acceptance of the condition, beliefs about the nature of asthma, and use of effective asthma health behaviors. In turn, these behaviors and beliefs have the potential to affect morbidity and mortality outcomes of students as they transition from elementary to middle or junior high school and begin to assume increasing responsibility for self-management of their condition.
Foundations for Health Policy
Understanding that health is essential for learning, the findings of this study provide evidence that supports requiring delivery of developmentally appropriate self-management health education and counseling programs to children and adolescents living with chronic conditions. Further, they support adapting universal rules and regulations to support student self-management of chronic conditions in schools.
Recommendations for Future Research
Feasibility and benefits (Kintner et al., 2012), efficacy (Kintner & Sikorskii, 2009), and effectiveness (e.g., Kintner, Cook, Marti, Allen et al., 2015; Kintner, Cook, Marti, Gomes et al., 2015) of the English version of SHARP have been confirmed in preparation for a planned dissemination and implementation study. In these studies, investigators systematically examine processes and factors that lead to widespread use of a program and are associated with successful integration and adaptation of a program within particular settings such as schools and communities (Rabin et al., 2008). In the planned study, we will evaluate the degree of fidelity with which the core components of the original intervention were transported to more diverse real world settings. In further study, we specifically will address issues of complexity, adoption, sustainability, and cost-effectiveness. Larger and more diverse schools systems are needed to evaluate SHARP’s community-wide impact on use of healthcare services and school absenteeism over time.
In summary, scientific knowledge has been advanced through the validation of the effectiveness of the SHARP theory-based, evidence-guided, and developmentally appropriate comprehensive school-based academic asthma health education and counseling program. This effective program has been tested and was welcomed by school administrators and healthcare professionals for older school-age students with asthma.
Acknowledgments
This study was funded by the National Institutes of Health, R01 NR010544 Comparison of Asthma Programs for Schools, and The University of Texas at Austin School of Nursing Ed and Molly Smith Centennial Fellowship in Nursing. The authors acknowledge caregiver-student dyads who actively participated in the study, school personnel and school teachers responsible for delivering the program, and evaluators responsible for collecting data from participants.
Contributor Information
Eileen Kintner, Associate Professor, School of Nursing, D0100, The University of Texas at Austin, 1700 Red River Street, NUR 3.446, Austin, TX 78701-1499.
Gwendolyn Cook, Research Associate, Comparison of Asthma Programs for Schools, The University of Texas at Austin School of Nursing, Austin, TX.
C. Nathan Marti, Statistician, Division of Statistics and Scientific Computation, The University of Texas at Austin, Austin, TX.
Debbie Stoddard, Site Coordinator, University Outreach and Engagement, Michigan State University, East Lansing, MI.
Melissa Gomes, Licensed School Counselor, C. W. Otto Middle School, Lansing, MI.
Phyllis Harmon, Administrative Research Assistant, Comparison of Asthma Programs for Schools, The University of Texas at Austin School of Nursing, Austin, TX.
Laurie A. Van Egeren, Director, Community Evaluation and Research Collaborative, Co-Director, National Collaborative for the Study of University Engagement, University Outreach and Engagement, Michigan State University, East Lansing, MI
References
- Ahmad E, Grimes DE. The effects of self-management education for school-age children on asthma morbidity: A systematic review. The Journal of School Nursing. 2011;27:282–292. doi: 10.1177/1059840511403003. [DOI] [PubMed] [Google Scholar]
- Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005–2009. National Health Statistics Reports. 2011;32:1–14. [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B. lme4: Linear mixed-effects models using S4 classes. 2013 Retrieved from http://CRAN.R-project.org/package=lme4.
- Bauer DJ, Curran PJ. Probing interactions in fixed and multilevel regression: Inferential and graphical techniques. Multivariate Behavioral Research. 2005;40:373–400. doi: 10.1207/s15327906mbr4003_5. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Bruzzese JM, Markman LB, Appel D, Webber M. An evaluation of Open Airways for Schools: Using college students as instructors. Journal of Asthma. 2001;38:337–342. doi: 10.1081/jas-100000261. [DOI] [PubMed] [Google Scholar]
- Bruzzese JM, Sheares BJ, Vincent EJ, Du Y, Sadeghi H, Levison MJ, … Evans D. Effects of a school-based intervention for urban adolescents with asthma. A controlled trial. American Journal of Respiratory and Critical Care Medicine. 2011;183:998–1006. doi: 10.1164/rccm.201003-0429OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruzzese JM, Evans D, Kattan M. School-based asthma programs. Journal of Allergy & Clinical Immunology. 2009;124:195–200. doi: 10.1016/j.jaci.2009.05.040. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multi-model inference: A practical information-theoretic approach. New York, NY: Springer; 2002. [Google Scholar]
- Christopher S, Watts V, McCormick AK, Young S. Building and maintaining trust in a community-based participatory research partnership. American Journal of Public Health. 2008;98:1398–1406. doi: 10.2105/AJPH.2007.125757. AJPH. 2007.125757 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school-based asthma program on symptoms, parent management, grades, and absenteeism. Chest. 2004;125:1674–1679. doi: 10.1378/chest.125.5.1674. [DOI] [PubMed] [Google Scholar]
- Clark NM, Shah S, Dodge JA, Thomas LJ, Andridge RR, Little RJ. An evaluation of asthma interventions for preteen students. Journal of School Health. 2010;80:80–87. doi: 10.1111/j.1746-1561.2009.00469.x. JOSH469 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffman JM, Cabana MD, Yelin EH. Do school-based asthma education programs improve self-management and health outcomes? Pediatrics. 2009;124:729–742. doi: 10.1542/peds.2008-2085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. New York, NY: Academic Press; 1988. [Google Scholar]
- Edgren KK, Parker EA, Israel BA, Lewis TC, Salinas MA, Robins TG, … Hill YR. Community involvement in the conduct of a health education intervention and research project: Community action against asthma. Health Promotion Practice. 2005;6:263–269. doi: 10.1177/1524839903260696. [DOI] [PubMed] [Google Scholar]
- Evans D, Clark NM, Feldman CH, Rips J, Kaplan D, Levison MJ, … Mellins RB. A school health education program for children with asthma aged 8–11 years. Health Education Quarterly. 1987;14:267–279. doi: 10.1177/109019818701400302. [DOI] [PubMed] [Google Scholar]
- Evans D, Clark NM, Levison MJ, Levin B, Mellins RB. Can children teach their parents about asthma? Health Education & Behavior. 2001;28:500–511. doi: 10.1177/109019810102800409. [DOI] [PubMed] [Google Scholar]
- Fawcett SB, Boothroyd R, Schultz J, Francisco V, Carson V, Bremby R. Building capacity for participatory evaluation within community initiatives. Journal of Prevention and Intervention in the Community. 2008;26(2):21–36. doi: 10.1300/J005v26n02_03. [DOI] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Findley S, Thomas G, Madera-Reese R, McLeod N, Kintala S, Andres Martinez R, … Herman E. A community-based strategy for improving asthma management and outcomes for preschoolers. Journal of Urban Health. 2011;88(Suppl 1):85–99. doi: 10.1007/s11524-010-9479-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelman A, Hill J. Data analysis using regression and multilevel/hierarchical models. New York, NY: Cambridge University Press; 2007. [Google Scholar]
- Graham JW. Missing data analysis: Making it work in the real world. Annual Review of Psychology. 2009;60:549–576. doi: 10.1146/annurev.psych.58.110405.085530. [DOI] [PubMed] [Google Scholar]
- Honaker J, King G. What to do about missing values in time-series cross-section data. American Journal of Political Science. 2010;54:561–581. doi: 10.1111/j.1540-5907.2010.00447.x. [DOI] [Google Scholar]
- Horner SD. Using the Open Airways curriculum to improve self-care for third grade children with asthma. Journal of School Health. 1998;68:329–333. doi: 10.1111/j.1746-1561.1998.tb00595.x. [DOI] [PubMed] [Google Scholar]
- IBM SPSS. IBM SPSS 19.0 for Windows. Armonk, NY: IBM Company; 2010. [Google Scholar]
- Jones L, Wells K. Strategies for academic and clinician engagement in community-participatory partnered research. JAMA. 2007;297:407–410. doi: 10.1001/jama.297.4.407. 297/4/407 [pii] [DOI] [PubMed] [Google Scholar]
- Kaplan DL, Rips JL, Clark NM, Evans D, Wasilewski Y, Feldman CH. Transferring a clinic-based health education program for children with asthma to a school setting. Journal of School Health. 1986;56:267–271. doi: 10.1111/j.1746-1561.1986.tb05748.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. PhD dissertation. The University of Arizona; 1996. Testing of the school-aged child and adolescent acceptance of asthma model. Retrieved from http://hdl.handle.net/10150/282275. [Google Scholar]
- Kintner EK. Adolescent process of coming to accept asthma: A phenomenological study. Journal of Asthma. 1997;34:547–561. doi: 10.3109/02770909709055399. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Lack of relationship between acceptance and knowledge of asthma in school-age children and early adolescents. Journal for Specialists in Pediatric Nursing: JSPN. 2004;9:5–14. doi: 10.1111/j.1088-145x.2004.00005.x. [DOI] [PubMed] [Google Scholar]
- Kintner EK. Testing the acceptance of asthma model with children and adolescents. Western Journal of Nursing Research. 2007;29:410–431. doi: 10.1177/0193945907299657. [DOI] [PubMed] [Google Scholar]
- Kintner EK, Sikorskii A. Randomized clinical trial of a school-based academic and counseling program for older school-age students. Nursing Research. 2009;58:321–331. doi: 10.1097/NNR.0b013e3181b4b60e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Allen A, Meeder L, Bumpus J, Lewis K. Feasibility and benefits of a school-based academic and counseling program for older school-age students. Research in Nursing & Health. 2012;35:507–517. doi: 10.1002/nur.21490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Hull L, Meeder L. Development and evaluation of an instrument to measure reasoning about managing asthma in older school-age children and adolescents. Journal of Nursing Measurement. 2013;21:360–377. doi: 10.1891/1061-3749.21.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Marti CN, Allen A, Stoddard D, Harmon P, … Van Egeren LA. Effectiveness of a school-and community-based academic asthma health education program on use of effective asthma self-care behaviors in older school age students. Journal for Specialists in Pediatric Nursing. 2015;20:62–75. doi: 10.1111/jspn.12099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Marti CN, Gomes M, Meeder L, Van Egeren LA. Effectiveness of a school-based academic asthma education and counseling program on fostering acceptance of asthma in older school age students with asthma. Journal for Specialists in Pediatric Nursing. 2015;20:49–61. doi: 10.1111/jspn.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosanke J, Bergstralh E. gmatch. Mayo Clinic; 2004. Retrieved from http://www.mayo.edu/research/documents/gmatchsas/DOC-10027248. [Google Scholar]
- Kuhn M, Weston S, Wing J, Forester J. Contrast: A collection of contrast methods. 2011 Retrieved from http://CRAN.R-project.org/package=contrast.
- Lerner RM. Nature, nuture, and dynamic interactionism. Human Development. 1978;21:1–20. [Google Scholar]
- Lerner RM. Concepts and theories of human development. 2. New York, NY: PN McGraw-Hill; 1986. [Google Scholar]
- MacQueen KM, McLellan E, Metzger DS, Kegeles S, Strauss R, Scotti RP, Trotter RT. What is community? An evidence-based definition for participatory public health. American Journal of Public Health. 2001;91:1929–1938. doi: 10.2105/ajph.91.12.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magzamen S, Patel B, Davis A, Edelstein J, Tager IB. Kickin’ asthma: School-based asthma education in an urban community. Journal of School Health. 2008;78:655–665. doi: 10.1111/j.1746-1561.2008.00362.x. [DOI] [PubMed] [Google Scholar]
- Michigan Department of Education. Michigan model assessment activity grade five: Healthy advocacy. 2006 Retrieved from https://www.michigan.gov/documents/Sample_Assessment_Rubric_-_Grade_5_92970_7.pdf.
- Murray DM. Design and analysis of group-randomized trials. New York, NY: Oxford University Press; 1998. [Google Scholar]
- Nam CB, Powers MG. The socioeconomic approach to status measurement. Houston, TX: Cap & Gown Press; 1983. [Google Scholar]
- National Heart, Lung, and Blood Insititute (NHLBI. National Institutes of Health, National Heart, Lung, and Blood Institute Expert Panel Report 3: Guidelines for diagnosis and management of asthma. Bethesda, MD: US Department of Health and Human Services; 2007. Retrieved from http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. [Google Scholar]
- Rabin BA, Brownson RC, Haire-Joshu D, Kreuter MW, Weaver NL. A glossary for dissemination and implementation research in health. Journal of Public Health Management Practice. 2008;14:117–123. doi: 10.1097/01.PHH.0000311888.06252.bb. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW. Statistical analysis and optimal design for cluster randomized trials. Psychological Methods. 1997;2(2):173–185. doi: 10.1037/1082-989x.5.2.199. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York, NY: John Wiley & Sons, Inc; 1987. [Google Scholar]
- Santrock JW. A topical approach to lifespan development. 5. Boston, MA: McGraw-Hill; 2010. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Sugarman L. Life-span development concepts, theories, and interventions. New York, NY: Routledge; 1986. [Google Scholar]
- Uyeda K, Bogart LM, Hawes-Dawson J, Schuster MA. Development and implementation of a school-based obesity prevention intervention: Lessons learned from community-based participatory research. Progress in Community Health Partnerships. 2009;3:249–255. doi: 10.1353/cpr.0.008. S1557055×09300108 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]