Abstract
Cancer continuously ranks among the top 10 leading causes of death in the United States. The burden of cancer is particularly elevated in the Commonwealth of Kentucky and its 54-county Appalachian region, where cancer is the leading cause of death. Kentucky’s high rates of cancer have been attributed to a wide range of socioeconomic, behavioral, environmental, and policy influences, resulting in numerous disparities. The present review specifically evaluates the burden of lung, colorectal, cervical, and head and neck cancers in Kentucky, along with resultant cancer control research and community outreach efforts conducted by the state’s only National Cancer Institute–designated cancer center using an adapted version of McLeroy’s Social-Ecological Model. Here, we categorize disparities and identify relevant intervention approaches based on their level of influence (ie, individual, community, and policy).
Keywords: Appalachia, cancer, disparities, Kentucky, Social-Ecological Model
Despite national, state, and local efforts focused on reducing cancer incidence and mortality in the United States, cancer continues to be the second leading cause of death.1,2 The burden of cancer is elevated significantly in the Commonwealth of Kentucky, where cancer is the leading cause of death.3 Nationally, Kentucky ranks first in all-site cancer incidence and mortality, part because of the high rates of cancer in its eastern 54-county Appalachian region as compared with the non-Appalachian counties in central and western Kentucky (Table 1).
Table 1.
Age-adjusted cancer incidence and mortality data for select cancers in the United States and Kentucky, 2010–2014
| National ranking | US | Kentucky | % Difference | Non-Appalachian Kentucky | Appalachian Kentucky | % Difference | |
|---|---|---|---|---|---|---|---|
| Age-adjusted cancer incidence rates per 100,000 population | |||||||
| All cancer sites | 1 | 452.1 | 521.1*** | 15.26 | 514.5 | 538.5*** | 4.66 |
| Lung | 1 | 61.2 | 95.3*** | 55.72 | 89.9 | 108.9*** | 21.13 |
| Colorectal | 1 | 39.8 | 50.0*** | 25.63 | 48.0 | 55.1*** | 14.79 |
| Larynx | 1 | 3.5 | 5.7*** | 62.86 | 5.1 | 7.2*** | 41.18 |
| Oral cavity | 1 | 11.5 | 14.1*** | 22.61 | 13.9 | 14.5 | 4.32 |
| Cervix | 8 | 7.6 | 8.7*** | 14.47 | 8.1 | 10.2** | 25.93 |
| Age-adjusted cancer mortality rates per 100,000 population | |||||||
| All cancer sites | 1 | 165.6 | 201.5*** | 21.68 | 191.8 | 226.1*** | 17.88 |
| Lung | 1 | 44.4 | 69.6*** | 56.76 | 64.4 | 82.4*** | 27.95 |
| Colorectal | 5 | 14.7 | 17.2*** | 17.01 | 16.0 | 20.2*** | 26.25 |
| Larynx | 3 | 1.0 | 1.5*** | 50.00 | 1.3 | 1.9*** | 46.15 |
| Oral cavity | 6 | 2.5 | 3.0*** | 20.00 | 3.0 | 3.1 | 3.33 |
| Cervix | 10 | 2.3 | 2.8*** | 21.74 | 2.6 | 3.3* | 26.92 |
P values for Kentucky are calculated against US P values. P values for Appalachian Kentucky are calculated against P values for non-Appalachian Kentucky. ASource: SEER*Stat, Kentucky Cancer Registry, and US Cancer Statistics. Source for state ranking: Centers for Disease Control and Prevention and US Cancer Statistics. Source for age-adjusted rates: NCI SEER*Stat, Kentucky Cancer Registry, and US Cancer Statistics. BA rate-ratio approach was used to test statistical difference between two age-adjusted rates. P values for Kentucky are calculated against US P values. P values for Appalachian Kentucky are calculated against P values for non-Appalachian Kentucky.C
P ≤ 0.05;
P ≤ 0.01;
P ≤ 0.001.
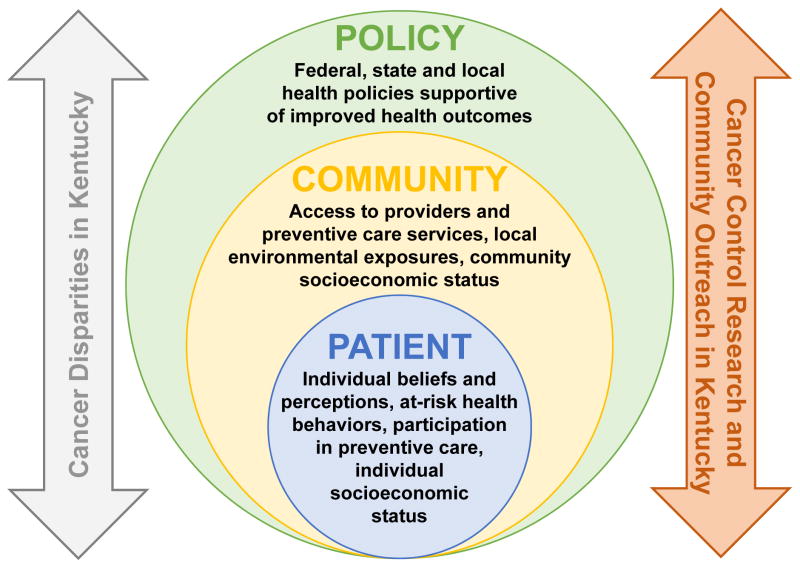
Kentucky’s high rates of cancer are attributed to myriad socioeconomic, behavioral, environmental, and policy influences, which can be described using an adapted version of McLeroy’s Social-Ecological Model (SEM). The SEM examines the interactions between and among individuals, their family and peer networks, and their community and local, state, and national policies, and determines the impact those interactions have on a person’s health status and resultant disparities.4,5 For example, using the SEM, an interaction can be observed between the distressed economic status (ie, employment, income, and poverty indicators in the lowest 10% of all US counties) of 69% of counties in Appalachian Kentucky,6 the significant number of health professional shortage areas throughout the region,7 the lower rates of Pap testing among Appalachian adult women, and the elevated cervical cancer mortality in the region.8
The present report uses the overarching tiers of influence in the SEM to frame cancer disparities in Kentucky and identifies areas for cancer control research and community outreach as undertaken by the state’s only National Cancer Institute (NCI)-designated cancer center, the University of Kentucky (UK) Markey Cancer Center (MCC; Fig.). The review focuses on lung, colorectal (CRC), cervical, and head and neck cancers (HNCs), which have been identified as cancers in Kentucky with high incidence and mortality (Table 1), but those that also are responsive to evidence-based prevention and screening interventions and health policy recommendations that lead to improvements in population health.
Fig.
McLeroy’s Social-Ecological Model.
Lung Cancer
Kentucky has the highest rates of lung cancer incidence and mortality nationwide. There is a 56% difference between lung cancer incidence in Kentucky and the United States and a 57% difference in mortality (Table 1).A As seen in Table 1, Appalachian residents have 5-year rates of lung cancer incidence and mortality that are higher than non-Appalachian residents.
Patient- and Community-Level Influences
As reported by NCI, the primary risk factors for lung cancer include exposure to tobacco smoke (firsthand or secondhand); a family history of lung cancer; human immunodeficiency virus infection; environmental exposure to radon and radiation; air pollution; and workplace exposure to substances such as asbestos, arsenic, and chromium.9 Approximately 80% to 90% of lung cancer cases are attributed to tobacco smoke.9
As noted in Table 2, 26% of adults in Kentucky and 30% of adults living in Appalachian Kentucky, respectively, are current smokers compared with 17% nationwide. Contributing to the high rates of smoking is a historical and cultural context of tobacco farming in Kentucky. For instance, the 2012 Census of Agriculture data found that Kentucky has the highest number of tobacco farms and the second highest total tobacco acreage nationwide.10
Table 2.
Select cancer risk factor prevalence data for the United States and Kentucky, 2014–2016
| US | Kentucky | Appalachian Kentucky | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Rate | 95% CL | KY | 95% CL | Rate | 95% CL | |
|
| ||||||
| Females aged 13–17 y who are up to date with HPV vaccinationa | 49.5 | 47.6–51.4 | 39.7 | 30.9–49.3 | — | — |
| Males aged 13–17 y who are up to date with HPV vaccinationa | 37.5 | 35.8–39.2 | 28.5 | 21.0–37.3 | — | — |
|
| ||||||
| Women aged ≥18 y who had a Pap test within the past 3 yb | 74.9 | 74.5–75.4 | 74.5 | 72.4–77.0 | 69.6 | 65.9–73.2 |
|
| ||||||
| Adults who are obese (BMI ≥30.0)c | 28.9 | 28.7–29.1 | 33.1 | 32.0–34.2 | 39.1 | 37.2–41.1 |
|
| ||||||
| Adults who are currently smokersc | 17.0 | 16.9–17.2 | 26.0 | 24.9–27.2 | 30.1 | 28.2–32.0 |
|
| ||||||
| Adults aged ≥50 y who have ever had a sigmoidoscopy or colonoscopyb | 68.9 | 68.5–69.2 | 69.6 | 67.8–71.4 | 63.2 | 60.4–66.2 |
|
| ||||||
| Adults aged ≥50 y who had a blood stool test within past 2 yb | 15.0 | 14.7–15.3 | 14.6 | 13.3–15.8 | 16.0 | 13.7–18.3 |
|
| ||||||
| Adults who reported heavy drinkingc | 5.8 | 5.7–5.9 | 5.7 | 5.0–6.3 | 3.8 | 2.9–4.7 |
BMI, body mass index; BRFSS, Behavioral Risk Factor Surveillance System; CL, confidence limit; HPV, human papillomavirus; KY, Kentucky.
National Immunization Survey-Teen, United States, 2016.
Data only available in 2014.
Rates were calculated by using all participants in 2014 and 2015 BRFSSs as denominator, all cases as numerator. Missing values were excluded when calculating rates.
Lung cancer screening rates are not reported on a state-by-state basis; however, in 2015, an estimated 6.8 million Americans were eligible for low-dose computed tomography screening based on their smoking status11 (ie, any individual between the ages of 55 and 80 who currently smokes or has smoked ≥30 packs of cigarettes per year [or within the past 15 years]12). A mere 3.9% of those individuals received a low-dose computed tomography screening.11 With national rates this low, it is unlikely that Kentucky lung cancer screening rates are near desirable levels among eligible candidates.
In addition to behavioral health risk, Kentuckians are exposed to high to moderate levels of radon,13 the second leading cause of lung cancer,14 because of the state’s unique limestone, shale, and dolomite geology and karst topography.15,16 Radon exposure, which is substantial in central Kentucky, is especially concerning in combination with the high levels of tobacco smoke exposure. Notably, 30 Kentucky counties are ranked as high potential radon zones (ie, radon exposure >4 pCi/L) and an additional 67 counties are ranked as moderate potential radon zones (ie, radon exposure between 2 and 4 pCi/L).13 Other environmental concerns include two major coal beds in eastern and western Kentucky containing high concentrations of heavy metals. The presence of multiple carcinogens (eg, arsenic, cadmium, chromium) in air, soil, and water is both naturally occurring and linked to mountaintop and other coal mining practices that may place residents at risk of lung cancer, among other malignancies.17,18 Additional research that is specific to lung cancer development and exposure to heavy metals via natural occurrence and industry practices in Kentucky is needed.
Policy-Level Influences
Kentucky’s low tobacco product tax, lack of a statewide smoking ban, lack of spending on tobacco prevention programs, and low minimum legal age to purchase cigarettes exacerbate its high rates of smoking. Nationally, the average excise tax on cigarettes is $1.71 per pack.19 Kentucky has the 43rd lowest excise tax nationwide, at $0.60 per pack.19 In fiscal year 2016, the state of Kentucky collected $302 million from the tobacco master settlement agreement; the Centers for Disease Control and Prevention (CDC) recommended Kentucky spend $56.4 million of the 2016 master settlement agreement revenue on tobacco prevention programs.20 Despite the CDC’s recommendation, Kentucky spent only $2.5 million (4.4% of the CDC’s recommendation) on tobacco prevention programs.20
Regarding smoke-free policies, as of October 1, 2017, only 26 communities in Kentucky have enacted comprehensive smoke-free policies (ie, smoking is banned in work/public places).21 Four communities have instituted smoking bans in public places, and 15 communities have smoke-free policies with significant exceptions (ie, specific places and tobacco products are excluded).21 With current legislation, only 32.7% of Kentucky’s workforce is protected from cigarette smoke in the workplace.22 States such as California and Hawaii have enacted legislation raising the minimum legal sale age (MLSA) for tobacco products to 21 years in an attempt to prevent youth from ever starting to smoke. In 2015, the Institute of Medicine released a report stating that raising the MLSA to 21 years reduces smoking rates by approximately 12% and reduces smoking-related deaths by approximately 10%.23 At the time of publication, the MLSA in Kentucky is 18 years.
One area of progress relates to state policy supporting tobacco cessation. Notably, Kentucky recently passed Senate Bill 89, which mandates insurance and Medicaid coverage for US Preventive Services Task Force–recommended tobacco cessation treatment interventions or programs.24
CRC
Despite notable increases in CRC screening and subsequent decreases in CRC incidence and mortality across the United States since the early 2000s, Kentucky continues to rank first nationwide for CRC incidence and fifth for CRC mortality (Table 1).B
Patient- and Community-Level Influences
As reported by the NCI, individuals are at an increased risk of developing CRC if they are older than 50 years, have a personal history of CRC or high-risk adenomas, have a personal history of inflammatory bowel disease, have a family history of CRC, have an inherited risk (eg, Lynch syndrome), drink three or more alcoholic drinks per day, are obese, or smoke.25 As noted earlier, Kentucky has significantly elevated smoking rates, and as presented in Table 2, one-third of Kentuckians are obese, with even higher rates in the Appalachian region of Kentucky (39%). Primary screening tools for CRC include colonoscopy, sigmoidoscopy, and blood stool tests such as fecal immunochemical tests (FIT).26 Behavioral Risk Factor Surveillance System (BRFSS) data suggest that 70% of Kentuckians older than age 50 received a CRC screening endoscopy examination (vs 69% nationally) in 201; however, only 63% of Appalachian Kentuckians older than 50 reported receiving a CRC screening endoscopy in 2014 (Table 2).
Barriers related to CRC screening are commonly cited by residents of Kentucky, including personal attitudes toward screening (eg, fear, discomfort, reticence), out-of-pocket costs, lack of provider recommendation and patient-centered communication, and lack of knowledge about screening examinations and to where to obtain a colonoscopy.27–29 In addition, patients have reported delays in treatment, which leads to them being less likely to seek treatment.30
Policy-Level Influences
Kentucky policymakers and advocacy organizations have been active in implementing policies to help support CRC screening, including the passage of KRS 304.17A-257 (which provided coverage of “complete CRC screening based on ACS [American Cancer Society] guidelines” as a health insurance benefit without a copay or deductible) and KRS 214.540-544 (which helped establish the Kentucky Colon Cancer Screening Program [KCCSP]).31 KCCSP receives CDC and state funding to provide free CRC screening tests to qualifying individuals. As a result of funding limitations, however, KCCSP cannot extend its program to the entire state; therefore, only 14 health departments provide free screenings, leaving more than half of the state’s counties without KCCSP services.
Cervical Cancer
Kentucky ranks eighth nationwide for invasive cervical cancer incidence and tenth for related mortality.C As presented in Table 1, there is a 14% difference between Kentucky’s incidence rates and those of the United States and a 22% difference in mortality. In addition, 5-year invasive cervical cancer incidence and mortality rates in Appalachian Kentucky are higher than those in non-Appalachian Kentucky.
Patient- and Community-Level Influences
According to the NCI, cervical cancer risk factors include human papillomavirus (HPV) infection, diethylstilbestrol exposure, cigarette smoking, immunosupression from human immunodeficiency virus, long-term oral contraceptive use, and being sexually active at a young age or having had many sexual partners.32 More important, almost all cervical cancer cases (>90%) are attributed to HPV, a sexually transmitted virus with an established preventive vaccine.33 Updated CDC immunization recommendations state that individuals 15 to 26 years of age should receive all three doses of the HPV vaccine, and younger adolescents 9 to 14 years old should receive two doses.34 As of 2016, only 40% of Kentucky adolescent girls are up to date with HPV vaccination requirements, compared with 50% nationally (Table 2). Similarly, only 29% of adolescent boys in Kentucky are up to date with HPV vaccination requirements compared with 38% nationally. Independent research studies have specifically identified low rates of HPV vaccination among adolescent girls 13 to 17 years old in Appalachia when compared with non-Appalachian adolescent girls.35 Adolescent girls and young adult women in Appalachia have citied similar barriers to HPV vaccination, including lack of parental approval, misinformation about the vaccine, lack of provider recommendation, transportation barriers, fatalistic beliefs, and lack of knowledge related to the link between HPV and cervical cancer.36–39
Pap smears and HPV testing are used to screen for cervical cancer based on age, prior test results, and time intervals.32 BRFSS data from 2014 suggest that Pap smear screening rates in Kentucky (75%) were similar to national screening rates (75%); however, Appalachian Kentucky screening rates are lower at 70% (Table 2). Moreover, follow-up care for abnormal Pap smears has been noted as being lower in Appalachian Kentucky.40 Fears related to what physicians may find upon further examination, privacy concerns, fear that the test will be painful, and transportation issues have been cited as barriers to receiving follow-up care.40
Policy-Level Influences
To increase vaccination rates among adolescents, Rhode Island, Virginia, and Washington, DC have enacted HPV vaccination mandates for school entry.41 As a result, these states and the District have seen an increase in vaccination rates either at or above the national average for males and females.42 Kentucky does not have a school-mandated HPV vaccination requirement, nor is HPV vaccination required to be reported in the state’s immunization registry. Related to screening, with Medicaid expansion, rates of cervical cancer screening in Kentucky increased by 88% among Medicaid enrollees from 2013 to 2014, however.43
HNCs
For the purposes of this review, HNCs are defined as cancer of the larynx and oral cavity. Kentucky ranks first for 5-year incidence rates for cancer of the larynx and oral cavity, respectively. In addition, Kentucky ranks third nationally for larynx cancer and sixth for oral cavity cancer mortality (Table 1).D
Patient- and Community-Level Influences
According to the NCI, tobacco and/or alcohol use, HPV infection, betel quid or gutka chewing, and a personal history of HNC have been linked to an increased risk of HNCs.44 As discussed earlier, Kentucky has high rates of smoking and low rates of HPV vaccination. BRFSS data from 2016 indicate that 13.6% of men in Kentucky currently use smokeless tobacco.45 Rates of heavy drinking in Kentucky and Appalachian Kentucky are lower than the national average (Table 2).E
Policy-Level Influences
Because of the overlapping risk factors between lung and cervical cancers and HNCs, there are shared policy-level interventions that can be implemented to reduce the burden of HNCs in Kentucky. As previously discussed, rates of smoking and limited HPV prevention in Kentucky are influenced by the lack of HPV school vaccination requirements, lower tobacco excise taxes, lower minimum legal age to purchase tobacco, and limited comprehensive smoking bans.
Discussion
Research has been published related to cancer disparities in Kentucky and Appalachia. A unique contribution of the present review, however, is the application of the tiers of influence found in the SEM to multiple cancers prevalent in Kentucky that are amenable to evidence-based prevention and screening strategies and health policy recommendations that have implications for improvements in population health. The review identified overarching themes and barriers to healthful living, including individual and communal beliefs and perceptions about cancer prevention and screening, increased at-risk health behaviors such as tobacco use and higher rates of obesity, lack of provider recommendation for guideline-recommended cancer screening and immunization, barriers to access to care, environmental exposures to carcinogens, and limited state health policies supporting positive health outcomes.
Another contribution of this review is the identification of areas of intervention through both cancer control research and community outreach as led by the state’s only NCI-designated cancer center, the UK MCC.46 The MCC specifically supports a clinical and research network, cancer control research studies, collaborative community programming, and policy initiatives addressing specific barriers and levels of influence addressed by the present review that may serve as a model for other cancer centers’ work in their respective communities.
For example, at the individual and community levels, the MCC Network collaborates with 24 community hospitals in Kentucky to deliver cutting-edge clinical trials, advanced cancer care and screening, community education, and training for healthcare professionals.47 The MCC Network supports the concept that high-quality cancer care should be delivered “close to home,” which helps to address issues related to distance and travel for rural residents and increases the capacity of local healthcare facilities and their providers. MCC researchers also have engaged with hundreds of individuals in Appalachian Kentucky through faith-placed cervical cancer screening and smoking cessation interventions delivered by lay health advisors.48,49 Multilevel interventions are delivered by the Kentucky LEADS (Lung Cancer. Education. Awareness. Detection. Survivorship.) Collaborative and the Terminate Lung Cancer study teams, both of which aim to increase healthcare providers’ implementation of high-quality lung cancer screening and tobacco cessation treatment, and raise community awareness of lung cancer screening services.50–52 Similarly, BREATHE (Bridging Research Efforts and Advocacy Toward Healthy Environments), a coalition of research programs including the Tobacco Policy Research Program, the Kentucky Center for Smoke-free Policy, and the Radon Policy Research Program, helps support smoke-free communities and worksites, radon control and mitigation, and smoking cessation activities in Kentucky.53–56
Related to CRC, the MCC has a long history of working with 15 local cancer coalitions across the state to implement multicomponent strategies such as academic detailing with primary care providers, engaging the faith community to promote CRC screening, using small and mass media to increase community demand for screening services, and supporting KCCSP. As a result, Kentucky has moved from 49th (34.7% in 2001) to 23rd (69.6% in 2014) among all states for guideline-adherent CRC endoscopy screening; the state CRC incidence rate has fallen by 24% and the mortality rate has decreased 30%. In complementary efforts to increase CRC endoscopy screening, MCC-based outreach staff are evaluating the impact of community-based distribution of FIT kits in Appalachian Kentucky and navigation of individuals to follow-up testing and treatment as appropriate, and MCC investigators are testing the impact of tailored health communication messages to promote annual adherence to FIT testing. As noted in Table 2, in 2014 Appalachian adults reported slightly higher blood stool testing rates compared with national and state estimates. Similar community-based efforts have been conducted with HPV vaccination, including partnerships with schools and health departments, with a focus on adherence to the full series36,57,58 and recruitment of women via free health clinics, community events, and health departments to self-collect a cervicovaginal swab, followed by HPV testing and navigation to Pap testing if needed.59,60
As a final example of MCC’s work in the community, given the presence of environmental carcinogens in Kentucky, the UK Center for Appalachian Research in Environmental Sciences has established a regionally focused research and community engagement infrastructure to foster innovative studies of environmental factors in chronic diseases such as cancer and community health disparities.61
Although this review is, to the best of our knowledge, novel in its purpose to identify and address specific cancer burdens in Kentucky as aligned with the primary levels of influence found in the SEM, there are noted limitations. The review is not exhaustive in its identification of disease risk factors, influences, and related interventions. Indeed, other causative factors such as the significant socioeconomic disparities present in Kentucky, residents’ genetic makeup, historical residential and occupational exposures, unique geology, and the extreme prevalence of tobacco use and obesity may explain any observed differences within Kentucky and between other areas of the United States. In addition, we did not explicitly address familial and peer influences or national health policies that may affect individuals’ health behaviors and outcomes. Last, we recognize that the MCC is just one entity among a host of dedicated organizations and stakeholders committed to reducing the incidence, morbidity, and mortality of cancer in Kentucky.
Conclusions
Kentucky’s high rates of cancer and continuous ranking in the top 10 for multiple cancer sites signify that there are tangible health concerns in the state. Addressing the disparities outlined in this review requires mounting a collaborative, multilevel effort that is centered on reducing individual and community-level health disparities, empowering the public and providers with cancer information and education, and improving health policy—all with the goal of reducing Kentucky’s significant cancer burden and improving quality of life among its constituents.
Key Points.
Cancer is the leading cause of death in Kentucky and incidence and mortality rates are higher than the national average.
Kentucky’s high rates of cancer are attributed to disparities in socioeconomic status, exposure to environmental factors, limited access to health care, geographic isolation, lower rates of health literacy, and at-risk health behaviors such as tobacco use.
McLeroy’s Social-Ecological Model can be applied to identify approaches that could reduce the incidence and mortality rates of some cancer types (eg, cervical, lung, colorectal, head and neck cancers) that are most responsive to prevention and screening interventions.
Acknowledgments
This manuscript was supported by services from the University of Kentucky Markey Cancer Center (UK MCC) Behavioral and Community-Based Research and Biostatistics and Bioinformatics Shared Resource Facilities (P30 CA177558).
N.L.V. has received compensation from the National Institutes of Health (grant no. P30 CA177558). R.V. has received compensation from the Centers for Disease Control and Prevention, the National Cancer Institute, the American Cancer Society, the Cancer Prevention Research Institute of Texas, and John Wiley & Sons. The remaining authors did not report any financial relationships or conflicts of interest.
We thank the UK MCC Research Communications Office for assistance with formatting and graphic design.
Footnotes
The sentences “Kentucky has the highest rates of lung cancer incidence and mortality nationwide. There is a 56% difference between lung cancer incidence in Kentucky and the United States and a 57% difference in mortality (Table 1).” require attribution. Please insert ref citations and add the full citations (as 8a, 8b, etc) to the refs list. Please also see the query for Table 1 itself.
The sentence “Despite notable increases in CRC screening and subsequent decreases in CRC incidence and mortality across the United States since the early 2000s, Kentucky continues to rank first nationwide for CRC incidence and fifth for CRC mortality (Table 1).” requires ref attribution. Please insert ref citations and add the full citations (as 24a) to the refs list. Please also see the query for Table 1 itself.
The sentences “Kentucky ranks eighth nationwide for invasive cervical cancer incidence and tenth for related mortality. As presented in Table 1, there is a 14% difference between Kentucky’s incidence rates and those of the United States and a 22% difference in mortality. In addition, 5-year invasive cervical cancer incidence and mortality rates in Appalachian Kentucky are higher than those in non-Appalachia Kentucky.” require reference attribution. Please insert ref citations and add the full citations (as 31a, 31b, etc) to the refs list. Please also see the query for Table 1 itself.
The sentences “Kentucky ranks first for 5-year incidence rates for cancer of the larynx and oral cavity, respectively. In addition, Kentucky ranks third nationally for larynx cancer and sixth for oral cavity cancer mortality (Table 1).” require reference attribution. Please insert ref citations and add the full citations (as 43a, 43b, etc) to the refs list. Please also see the query for Table 1 itself.
The sentence “Rates of heavy drinking in Kentucky and Appalachian Kentucky are lower than the national average (Table 2).” requires reference attribution. Please insert ref citations and add the full citations (as 45a) to the refs list. Please also see the query for Table 2 itself.
Please check the first sentence of the footnote for accuracy of editing.
These sources must be added to the refs list as full reference citations.
Please check the last 2 sentences of the main footnote for accuracy of editing.
To purchase a single copy of this article, visit sma.org/smj-home. To purchase larger reprint quantities, please contact Reprintsolutions@wolterskluwer.com.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66:7–30. doi: 10.3322/caac.21332. [DOI] [PubMed] [Google Scholar]
- 2.Byers T, Wender RC, Jemal A, et al. The American Cancer Society challenge goal to reduce US cancer mortality by 50% between 1990 and 2015: results and reflections. CA Cancer J Clin. 2016;66:359–369. doi: 10.3322/caac.21348. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. [Accessed October 4, 2017];Stats of the state of Kentucky. https://www.cdc.gov/nchs/pressroom/states/kentucky.htm.
- 4.McLeroy KR, Bibeau D, Steckler A, et al. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 5.Sallis JF, Owen N, Fisher EB. Ecological models of health behavior. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. San Francisco: Jossey-Bass; 2008. pp. 465–486. [Google Scholar]
- 6.Appalachian Regional Commission. [Accessed September 17, 2017];ARC-designated distressed counties, fiscal year 2017. https://www.arc.gov/program_areas/ARCDesignatedDistressedCountiesFiscalYear2017.asp.
- 7.Health Resources and Services Administration Data Warehouse. [Accessed September 17, 2017];Data by geography—Kentucky. https://datawarehouse.hrsa.gov/Tools/DataByGeographyResults.aspx?geoTyp=State&geoCd=21.
- 8.Freeman HP, Wingrove B. Excess Cervical Cancer Mortality: A Marker for Low Access to Health Care in Poor Communities. Rockville, MD: National Cancer Institute Center to Reduce Cancer Health Disparities; 2005. [Google Scholar]
- 9.National Cancer Institute. [Accessed October 4, 2017];Lung cancer prevention. https://www.cancer.gov/types/lung/patient/lung-prevention-pdq#section/_12.
- 10.Campaign for Tobacco-Free Kids. [Accessed October 4, 2017];Tobacco-growing states in the USA. https://www.tobaccofreekids.org/research/factsheets/pdf/0125.pdf. Published September 4, 2014.
- 11.Jemal A, Fedewa SA. Lung cancer screening with low-dose computed tomography in the United States-2010 to 2015. JAMA Oncol. 2017;3:1278–1281. doi: 10.1001/jamaoncol.2016.6416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.US Preventive Services Task Force. [Accessed October 4, 2017];Lung cancer: screening. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/lung-cancer-screening. Published December 2013.
- 13.Environmental Protection Agency. [Accessed October 4, 2017];EPA map of radon zones. https://www.epa.gov/radon/epa-map-radon-zones.
- 14.Centers for Disease Control and Prevention. [Accessed October 4, 2017];What we know about radon. https://www.cdc.gov/cancer/dcpc/prevention/policies_practices/radon/radon.htm. Updated September 27, 2017.
- 15.Kentucky Geological Survey. [Accessed October 4, 2017];Karst Land in Kentucky. https://www.uky.edu/KGS/water/general/karst/index.htm. Modified August 1, 2012.
- 16.Hahn EJ, Gokun Y, Andrews WM, Jr, et al. Radon potential, geologic formations, and lung cancer risk. Prev Med Rep. 2015;2:342–346. doi: 10.1016/j.pmedr.2015.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendryx M, O’Donnell K, Horn K. Lung cancer mortality is elevated in coal-mining areas of Appalachia. Lung Cancer. 2008;62:1–7. doi: 10.1016/j.lungcan.2008.02.004. [DOI] [PubMed] [Google Scholar]
- 18.Jenkins WD, Christian WJ, Mueller G, et al. Population cancer risks associated with coal mining: a systematic review. PLoS One. 2013;8:e71312. doi: 10.1371/journal.pone.0071312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Campaign for Tobacco-Free Kids. [Accessed October 4, 2017];State cigarette excise tax rates and rankings. https://www.tobaccofreekids.org/assets/factsheets/0097.pdf. Published 2017.
- 20.Campaign for Tobacco-Free Kids. [Accessed October 4, 2017];Broken promises to our children: a state-by-state look at the 1998 State Tobacco Settlement 17 years later. https://www.tobaccofreekids.org/microsites/statereport2016. Published 2015.
- 21.Kentucky Center for Smoke-Free Policy. [Accessed September 17, 2017];26 Kentucky communities with comprehensive smoke-free ordinances. http://www.uky.edu/breathe/sites/breathe.uky.edu/files/SFLawsRegsOCT2017.pdf. Published 2017.
- 22.Kentucky Center for Smoke-Free Policy. [Accessed October 4, 2017];Percent of the Kentucky population covered by 100% smoke-free workplace laws. Updated October 1, 2017. http://www.uky.edu/breathe/sites/breathe.uky.edu/files/PercentSmoke-FreeWorkplaceLawsorRegulationsOCT2017.pdf.
- 23.Institute of Medicine. Health Implications of Raising the Minimum Age for Purchasing Tobacco Products. Washington, DC: The National Academies Press; 2015. [PubMed] [Google Scholar]
- 24.Adams J, Alvarado R, Carroll D, et al. [Accessed October 5, 2017];Senate Bill 89 (BR 837) http://www.lrc.ky.gov/record/17RS/SB89.htm.
- 25.National Cancer Institute. [Accessed October 4, 2017];Colorectal cancer prevention (PDQ®)–patient version. https://www.cancer.gov/types/colorectal/patient/colorectal-prevention-pdq. Updated February 8, 2017.
- 26.American Cancer Society. [Accessed October 4, 2017];Colorectal cancer screening tests. https://www.cancer.org/cancer/colon-rectal-cancer/early-detection/screening-tests-used.html. Revised August 22, 2017.
- 27.Tucker T. [Accessed October 6, 2017];Understanding the colorectal cancer burden in Kentucky: environmental, behavioral and genetic risk factors. http://www.kycancerc.org/docsandpubs/KYColonCaBurden2013.ppt. Published October 3, 2013.
- 28.Knight JR, Kanotra S, Siameh S, et al. Understanding barriers to colorectal cancer screening in Kentucky. Prev Chronic Dis. 2015;12:E95. doi: 10.5888/pcd12.140586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bachman AS, Cohen EL, Collins T, et al. Identifying communication barriers to colorectal cancer screening adherence among Appalachian Kentuckians. Health Commun. 2017:1–9. doi: 10.1080/10410236.2017.1351274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Seiber EE, Camacho F, Zeeshan MF, et al. Disparities in colorectal cancer treatment delay within Appalachia—the role of forprofit hospitals. J Rural Health. 2015;31:382–391. doi: 10.1111/jrh.12122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kentucky Cancer Consortium. [Accessed September 17, 2017];Reducing barriers to colorectal cancer screening. http://www.kycancerc.org/policychange/coloncancerscreeningbarriers.php. Published 2017.
- 32.National Cancer Institute. [Accessed September 17, 2017];Cervical cancer prevention (PDQ®)–patient version. https://www.cancer.gov/types/cervical/patient/cervical-prevention-pdq. Updated September 21, 2017.
- 33.Centers for Disease Control and Prevention. [Accessed September 17, 2017];How many cancers are linked with HPV each year? http://www.cdc.gov/cancer/hpv/statistics/cases.htm. Updated March 3, 2017.
- 34.Meites E, Kempe A, Markowitz LE. Use of a 2-dose schedule for human papillomavirus vaccination—updated recommendations of the Advisory Committee on Immunization Practices. MMWR Morb Mortal Wkly Rep. 2016;65:1405–1408. doi: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- 35.Reiter PL, Katz ML, Paskett ED. HPV vaccination among adolescent females from Appalachia: implications for cervical cancer disparities. Cancer Epidemiol Biomarkers Prev. 2012;21:2220–2230. doi: 10.1158/1055-9965.EPI-12-0850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Vanderpool RC, Cohen E, Crosby RA, et al. “1-2-3 Pap” intervention improves HPV vaccine series completion among Appalachian women. J Commun. 2013;63:95–115. doi: 10.1111/jcom.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mills LA, Head KJ, Vanderpool RC. HPV vaccination among young adult women: a perspective from Appalachian Kentucky. Prev Chronic Dis. 2013;10:E17. doi: 10.5888/pcd10.120183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vanderpool RC, Dressler EV, Stradtman LR, et al. Fatalistic beliefs and completion of the HPV vaccination series among a sample of young Appalachian Kentucky women. J Rural Health. 2015;31:199–205. doi: 10.1111/jrh.12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oldach BR, Katz ML. Ohio Appalachia public health department personnel: human papillomavirus (HPV) vaccine availability, and acceptance and concerns among parents of male and female adolescents. J Community Health. 2012;37:1157–1163. doi: 10.1007/s10900-012-9613-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schoenberg N, Baltisberger J, Bardach S, et al. Perspectives on Pap test follow-up care among rural Appalachian women. Women Health. 2010;50:580–597. doi: 10.1080/03630242.2010.516702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Conference of State Legislatures. [Accessed November 13, 2016];HPV vaccine: state legislation and statutes. http://www.ncsl.org/research/health/hpv-vaccine-state-legislation-and-statutes.aspx.
- 42.Reagan-Steiner S, Yankey D, Jeyarajah J, et al. National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR Morb Mortal Wkly Rep. 2016;65:850–858. doi: 10.15585/mmwr.mm6533a4. [DOI] [PubMed] [Google Scholar]
- 43.Kentucky Center for Economic Policy. [Accessed September 17, 2017];Protecting Medicaid’s role in advancing a healthy Kentucky. http://kypolicy.org/dash/wp-content/uploads/2016/05/Medicaid-Advancing-a-Healthy-Kentucky.pdf. Published May 2016.
- 44.National Cancer Institute. [Accessed October 4, 2017];Oral cavity and oropharyngeal cancer prevention. https://www.cancer.gov/types/head-and-neck/patient/oral-prevention-pdq#section/_20.
- 45.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System Prevalence and trends data. [Accessed October 4, 2017];Kentucky: topic: smokeless tobacco. https://www.cdc.gov/brfss/brfssprevalence/index.html. Published 2016.
- 46.University of Kentucky HealthCare. [Accessed October 4, 2017];University of Kentucky Markey Cancer Center National Cancer Institute designation. https://ukhealthcare.uky.edu/markey-cancer-center/about/nci. Published 2017.
- 47.University of Kentucky Markey Cancer Center. [Accessed October 4, 2017];Markey Network. https://ukhealthcare.uky.edu/markey/network.
- 48.Schoenberg NE, Hatcher J, Dignan MB, et al. Faith moves mountains: an Appalachian cervical cancer prevention program. Am J Health Behav. 2009;33:627–638. doi: 10.5993/ajhb.33.6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Schoenberg NE, Studts CR, Shelton BJ, et al. A randomized controlled trial of a faith-placed, lay health advisor delivered smoking cessation intervention for rural residents. Prev Med Rep. 2016;3:317–323. doi: 10.1016/j.pmedr.2016.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cardarelli R, Reese D, Roper KL, et al. Terminate lung cancer (TLC) study—a mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in eastern Kentucky. Cancer Epidemiol. 2017;46:1–8. doi: 10.1016/j.canep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cardarelli R, Roper KL, Cardarelli K, et al. Identifying community perspectives for a lung cancer screening awareness campaign in Appalachia Kentucky: the Terminate Lung Cancer (TLC) Study. J Cancer Educ. 2017;32:125–134. doi: 10.1007/s13187-015-0914-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kentucky LEADS Collaborative. [Accessed December 12, 2016]; About. https://www.kentuckyleads.org/about.
- 53.Fallin A, Goodin A, Rayens MK, et al. Smoke-free policy implementation: theoretical and practical considerations. Policy Polit Nurs Pract. 2014;15:81–92. doi: 10.1177/1527154414562301. [DOI] [PubMed] [Google Scholar]
- 54.Hahn EJ, Rayens MK, Adkins S, et al. A controlled community-based trial to promote smoke-free policy in rural communities. J Rural Health. 2015;31:76–88. doi: 10.1111/jrh.12087. [DOI] [PubMed] [Google Scholar]
- 55.Pyles MK, Hahn EJ. Economic effects of smoke-free laws on rural and urban counties in Kentucky and Ohio. Nicotine Tob Res. 2012;14:111–115. doi: 10.1093/ntr/ntr123. [DOI] [PubMed] [Google Scholar]
- 56.Hahn EJ, Rayens MK, Kercsmar SE, et al. Dual home screening and tailored environmental feedback to reduce radon and secondhand smoke: an exploratory study. J Environ Health. 2014;76:156–161. [PubMed] [Google Scholar]
- 57.Cohen EL, Head KJ, McGladrey MJ, et al. Designing for dissemination: lessons in message design from “1-2-3 pap. Health Commun. 2015;30:196–207. doi: 10.1080/10410236.2014.974130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vanderpool RC, Breheny PJ, Tiller PA, et al. Implementation and evaluation of a school-based human papillomavirus vaccination program in rural Kentucky. Am J Prev Med. 2015;49:317–323. doi: 10.1016/j.amepre.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 59.Crosby RA, Hagensee ME, Vanderpool R, et al. Community-based screening for cervical cancer: a feasibility study of rural Appalachian women. Sex Transm Dis. 2015;42:607–611. doi: 10.1097/OLQ.0000000000000365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Vanderpool RC, Jones MG, Stradtman LR, et al. Self-collecting a cervico-vaginal specimen for cervical cancer screening: an exploratory study of acceptability among medically underserved women in rural Appalachia. Gynecol Oncol. 2014;132(Suppl 1):S21–S25. doi: 10.1016/j.ygyno.2013.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gregory A. [Accessed October 4, 2017];UK partners with community to answer environmental health questions through new research center. https://uknow.uky.edu/research/uk-partners-community-answer-environmental-health-questions-through-new-research-center. Published August 7, 2017.