Abstract
Objectives
The aims of this meta-analysis were to examine intervention methods of qualitatively, well-designed studies from the past 10 years for treating visuo-spatial neglect (VSN) in patients who had suffered a stroke, and to evaluate the combined effects of intervention.
Methods
Studies published between 2008 and 2017 on the theme of VSN were collected from PubMed, CINAHL, and MEDLINE, representative academic databases and search engines. The PEDro scale was used for evaluating the quality of methodology. The sample size, mean, and standard deviation of identified studies were used for meta-analysis.
Results
Eight studies were selected for analysis. The PEDro scores of the selected studies were ≥ 7, with 237 subjects analyzed. The results of intervention were classified into “mental function” and “activity and participation” based on the International Classification of Functioning, Disability and Health. The analyzed effect sizes for combined outcomes, mental function and, activity and participation, were 0.728 (medium effect size), 0.850 (large effect size), and 0.536 (medium effect size), respectively.
Conclusion
Intervention methods for treating VSN had a short-term effect on cognitive function (visual perception). In particular, non-invasive brain stimulation therapy showed a large effect size for VSN treatment.
Keywords: brain, meta-analysis, stroke, therapeutic, visual perception
Introduction
Visuo-spatial neglect (VSN) is a common symptom associated with unilateral brain damage and has been frequently observed in individuals with right hemisphere brain injury [1]. In acute stroke, VSN occurred in 43% of patients with right hemisphere damage and 17% of patients with left hemisphere damage [1]. It has also been reported that VSN remained after 3 months in 17% of right hemisphere stroke victims, and 5% of left hemisphere stroke victims [2].
The VSN symptoms that remain after a stroke make it hard for patients to recognize objects on the side they are paralyzed, and be independent in daily life [3]. Furthermore, stoke rehabilitation studies show that patients with VSN-associated symptoms have a slower physical recovery than those patients whose stroke was not accompanied with VSN symptoms [4, 5].
Various interventions have been employed to treat VSN of individuals who have suffered a stroke. Previous studies have used individual behavioral training, assistive devices, sensory stimulation, brain stimulation, virtual reality, and drug therapy [6]. Individual behavioral training included interventions to improve the awareness and attention of the neglect side, voluntary trunk rotation, limb activation (LA), constraint-induced therapy, and smooth pursuit eye movement training [7–10]. Ipsilateral eye patching and prism adaptation training (PAT) were implemented as an assistive device of intervention for the neglect symptoms [11, 12]. Neck muscle vibration and galvanic-vestibular stimulation (GVS) were used as sensory stimulation [13, 14]. Noninvasive brain stimulation therapies included transcranial direct current stimulation (tDCS), repetitive transcranial magnetic stimulation (rTMS), and theta-burst stimulation (TBS) [15–17]. Currently, as technology evolves, virtual reality and medication have been used to treat VSN [18, 19]. It is clear that numerous treatment interventions have been developed over time to treat VSN of stroke victims.
In stroke rehabilitation, it is necessary to examine the interventions currently being applied and to assess which VSN treatments are effective. Therefore, the aims of this study were to investigate the treatment methods of VSN applied to patients in well-designed, qualitative studies from the past 10 years, and to analyze the effects of those interventions using meta-analysis. To do this trial outcomes were classified into “mental function” and “activity and participation” according to the domains of the International Classification of Functioning and Disability and Health (ICF) [20].
Materials and Methods
1. Research design
This meta-analysis targeted randomized, controlled, clinical trials that provided VSN treatments to stroke patients. Various types of VSN treatment methods were considered as independent variables. The outcomes extracted as dependent variables of each study were classified into “mental function” and “activity and participation” according to the domains of the ICF.
2. Literature search
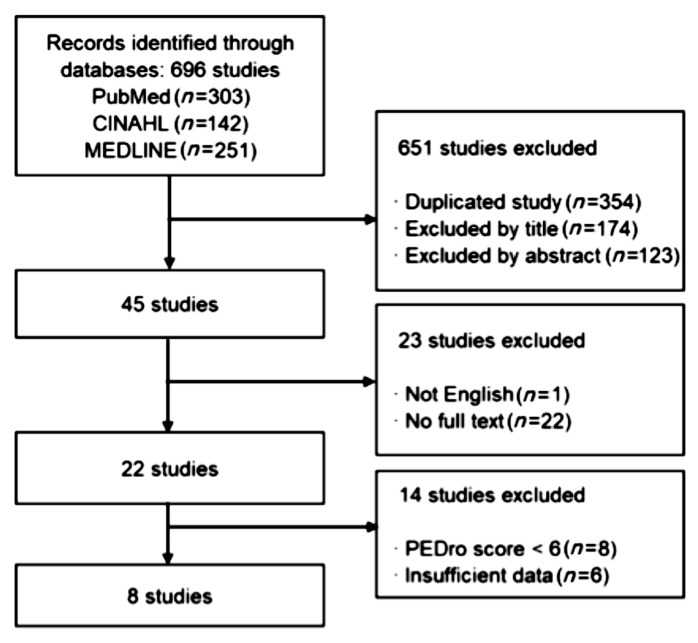
This study targeted trials published in international journals in English between January 2008 and September 2017. Three representative academic databases and search engines (i.e., PubMed, CINAHL, and MEDLINE) were used to find appropriate literature. Medical subject heading (MeSH) and keywords were used as the search strategies to collect appropriate literature: specifically, the syntax of (neglect OR inattention) AND (rehabilitation OR therapy OR intervention) AND stroke (MeSH) was used. Two researchers conducted the selection process for searched and collected studies independently and the discrepancy was compromised through discussion. As a result, 8 publications were used for the study (Figure 1).
Figure 1.
Inclusion and exclusion research flow diagram to identify studies for meta-analyses.
3. Criteria for selection
The following criteria were applied to select publications for final analysis; (1) the study measured mental function, activity and participation levels using a standardized evaluations and reported at least 1 outcome; (2) the study was an experimental study, not animal study, case study, review, or systematic literature review; (3) the study was a randomized controlled clinical trial; (4) the study provided a mean, standard deviation, and number of subjects in order to calculate effect size; (5) the study used intervention for treating VSN; (6) the study ensured homogeneity between the control group and the treatment group, and subjects were individual stroke victims; (7) the study had a PEDro score ≥ 6; (8) the study was published in English; and (9) the studies original text was available in full.
4. PEDro scale for assessment of quality of methodology
Two researchers estimated the PEDro scale independently to rate the quality of methodology of the studies. If the estimated PEDro scores were not in agreement, the final PEDro scores were agreed after consultation between the researchers. The PEDro scale has 10 items that can be used to analyze the internal validity of a publication, and a publication can be classified into 10 grades. Grades 9 and 10 were classified as very high quality studies, Grades 6, 7, and 8, were considered high quality studies, Grades 4 and 5 were seen as fair quality studies and Grades ≤ 3 were classified as studies of poor quality. [21]. This meta-analysis study only used publications of studies classified as very high or high quality.
5. Characteristics of included studies
8 studies were selected and analyzed for the study. There were 237 subjects analyzed; 117 subjects in the treatment group and 120 subjects in the control group. All subjects were acute stroke patients diagnosed within 6 months of onset.
VSN treatments were divided into several types; intervention combining rTMS, intervention merging right hemi-field eye patching (RHEP), computer-based cognitive training (CBT), intervention linking limb activation and sensory cuing (SC), TBS, PAT, GVS, and visuo-motor feedback training (VFT), a new intervention method.
Studies were classified by measurement outcomes to calculate the effect size. There were 8 studies testing the visual perception of the “mental function” domain, and 7 studies evaluating behaviors and activities of daily living (ADL) in the “activity and participation” domain. All analyzed publications were randomized, controlled, clinical trials with PEDro scores of ≥ 7 (Table 1).
Table 1.
Characteristics of selected studies included for meta-analyses.
| No | Study | Exp/Con(n) | Onset duration | Age (M±SD) | Intervention | Time of intervention | Outcome measure (Classification) | PEDro score |
|---|---|---|---|---|---|---|---|---|
| 1 | Aparicio-Lopez et al. (2016) [22] | 13 15 |
85.3±67.3* D 80.3±39.7* D |
50.5±7.6 45.7±8.1 |
CBT+RHEP CBT |
1 Hs 2–5 Ss/W total 15 Ss | BCT FCO LBT (MF) BTT CBS RT (A&P) |
7 |
| 2 | Cha & Kim (2016) [23] | 15 15 |
4.1±1.1* M 3.9±0.8* M |
64.1±12.1 63.3±12.2 |
CRT+rTMS CRT+sham |
50 Ms 5 Ss/W 4 Ws | AT LBT (MF) BBT (A&P) |
9 |
| 3 | Fong et al. (2013) [24] | 19 16 |
24.3±18.5* D 22.3±12.0* D |
66.2±14.8 68.6±10.6 |
CR+LA/SC CR+LA |
3 Hs 5 Ss/W 3 Ws | BIT-CT (MF) BIT-DT FIM (A&P) |
7 |
| 4 | Fu et al. (2015) [25] | 10 10 |
50.3±33.3* D 34.9±14.6* D |
55.1±14.0 59.5±12.7 |
CRT+cTBS CRT+sham |
30 Ms 3 Ss/W 2 Ws | LBT SCT (MF) | 8 |
| 5 | Mizuno et al. (2011) [26] | 15 19 |
67.1±18.4* D 64.4±20.9* D |
66.0±11.5 66.6±7.7 |
CRT+PAT CRT+ATnoP |
20 Ms 2 Ss/D 5 Ds/W 2 Ws | BIT-C (MF) BIT-B CBS (A&P) |
9 |
| 6 | Rossit et al. (2017) [27] | 9 10 |
3.1±0.9* M 3.2±0.5* M |
65.9±2.8 64.9±2.5 |
VFT VTnoF |
6–8 Rep/S 12 Ss for 2 Ws | BIT BaT (MF) SIS-ADL/SP (A&P) |
8 |
| 7 | Wilkinson et al. (2014) [28] | 16 15 |
94(39–534)† D 68(39–229)† D |
65.7±8.7 66.9±10.6 |
VST+GVS VST+sham |
10 Ss for 4 Ws | BIT (MF) BI (A&P) |
7 |
| 8 | Yang et al. (2016) [29] | 20 20 |
37.5±26.0* D 42.5±30.6* D |
54.6±11.8 58.7±12.7 |
CRT+rTMS CRT |
45 Ms 5 Ss/W 2 Ws | BIT-C (MF) CBS MBI (A&P) |
8 |
Mean±Standard Deviation,
Median (Interquartile Range)
A&P=activity and participation; AT=Albert Test; ATnoP=adaptation training without prism; Bat= alloons Test; BBT=Box and Block Test; BCT=Bell Cancelation Test; BI=Barthel Index; BIT=Behavioral Inattention Test; BIT-B=Behavioral Test; BIT-C=Conventional Test; BIT-CT=Cancellation Task; BIT-DT=Drawing Task; BTT=Baking Tray Task; CBS=Catherine Bergego Scale; CBT=computer-based cognitive rehabilitation; CG=control group; CRT=conventional rehabilitation therapy; cTBS=continuous theta-burst stimulation; D=days; EG=experimental group; FCO=Figure Copying of Ogden; FIM=Functional Independence Measure; GVS=galvanic vestibular stimulation; Hs=hours; LA= limb activation; LBT=Line Bisection Test; M=months; MBI=Modified Barthel Index; MF=mental function; Ms=minutes; PAT=prism adaptation training; Rep=repetition; RHEP=right hemi-field eye patching; RT=reading task; rTMS=repetitive transcranial magnetic stimulation; S(s)=session(s); SC=sensory cueing with wristwatch vibration device; SCT=Star Cancellation Test; SIS-ADL/SP=Stroke Impact Scale-Activities of Daily Living/Social Participation; VFT=visuomotor feedback training; VTnoF=visuomotor training without feedback; W(s)=week(s).
6. Quantitative analysis
A quantitative, meta-analysis was conducted to examine the integrated effect size, statistical homogeneity, and publishing bias of the selected studies. Comprehensive Meta-Analysis 3.0 was used for the analysis.
Q-value was used for evaluating the homogeneity of effect sizes. It was determined that the heterogeneity of effect size between studies was small when statistical significance of the Q-value was p ≥ 0.1. However, determining the heterogeneity between studies with Q-value, and deciding the effect model do not have a robust statistical basis. Therefore, this study determined the heterogeneity of effect size through Q-value and selected the fixed effect model or the random effect model when considering the study design, participants, intervention methods, and the temporal difference in measuring variables [30].
The number of study participants, mean, standard deviation, and statistical t- and p-values were used to estimate the combined effect size of the analyzed papers. The dependent variables used to calculate the effect size were analyzed by calculating the effect size combined with mental function and that with, activity and participation. The effect size was interpreted as a small effect size, a medium effect size, and a large effect size when Cohen’s d was < 0.4, 0.4 to 0.7, and ≥ 0.8, respectively, according to Cohen’s criteria [31]. The combined effect size and confidence interval were visualized through the forest plot.
Funnel plots and fail-safe number values were used to test publication bias. The funnel plot was used to evaluate if the points were symmetrically and evenly distributed on both sides around the effect size. When fail-safe number value was small and p > 0.05, it was considered that publication bias existed [32].
Results
1. Quantitative analysis
Statistical heterogeneity
Q-value was used to test the homogeneity of analyzed studies. It was found that the Q-value for the effect size of combined outcomes was 26.213 (df = 7, p 0.000). That of mental function was 25.768 (df = 7, p 0.001) and that of activity and participation was 9.073 (df = 6, p 0.169). The calculated Q-values indicated that the heterogeneity of combined outcomes and mental function effect sizes were high, and that of activity and participation effect sizes were low. However, the random effect model was selected because the homogeneity of the study design and subjects could not be guaranteed, and the effects were measured by various methods such as score, time, and length (Table 2).
Table 2.
Statistical heterogeneity.
| Studies | T2 | Q | df | p | |
|---|---|---|---|---|---|
| CO | 8 | 0.221 | 26.213 | 7 | 0.000 |
| MF | 8 | 0.430 | 25.768 | 7 | 0.001 |
| A&P | 7 | 0.071 | 9.073 | 6 | 0.169 |
A&P=activity and participation; CO=combined outcomes; MF=mental function.
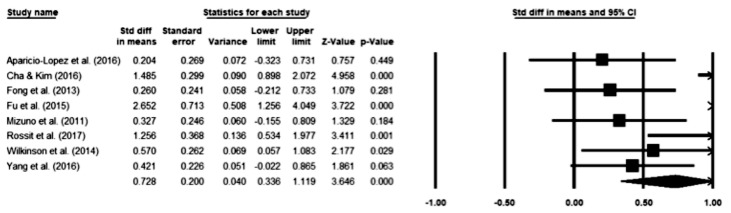
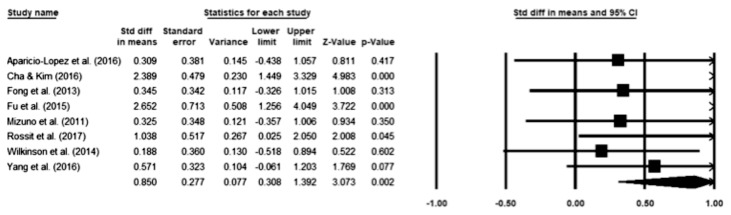
Effect on combined outcomes and mental function
There were 117 study participants in the experimental group and 120 in the control group to analyze the effect of VSN treatments on the combined outcomes and mental function. The effect size was 0.728 (95% CI 0.336 to 1.119), indicating a medium effect size (Figure 2). Analysis of mental function showed that the effect size was 0.850 (95% CI 0.308 to 1.392), indicating a large effect size (Figure 3).
Figure 2.
Effect of intervention for visuo-spatial neglect on combined outcomes.
Figure 3.
Effect of intervention for visuo-spatial neglect on mental function.
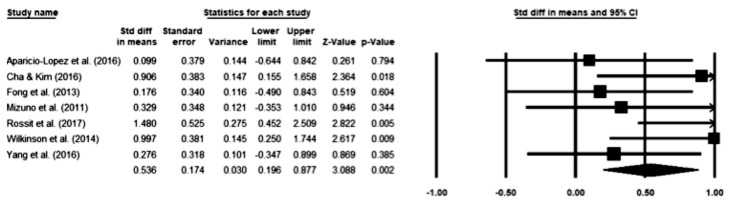
Effect on activity and participation
There were 107 study participants in the experimental group, and 110 in the control group to determine the effect of VSN treatments on, activity and participation. The effect size was 0.536 (95% CI 0.196 – 0.877), indicating a medium effect size (Figure 4).
Figure 4.
Effect of intervention for visuo-spatial neglect on activity and participation.
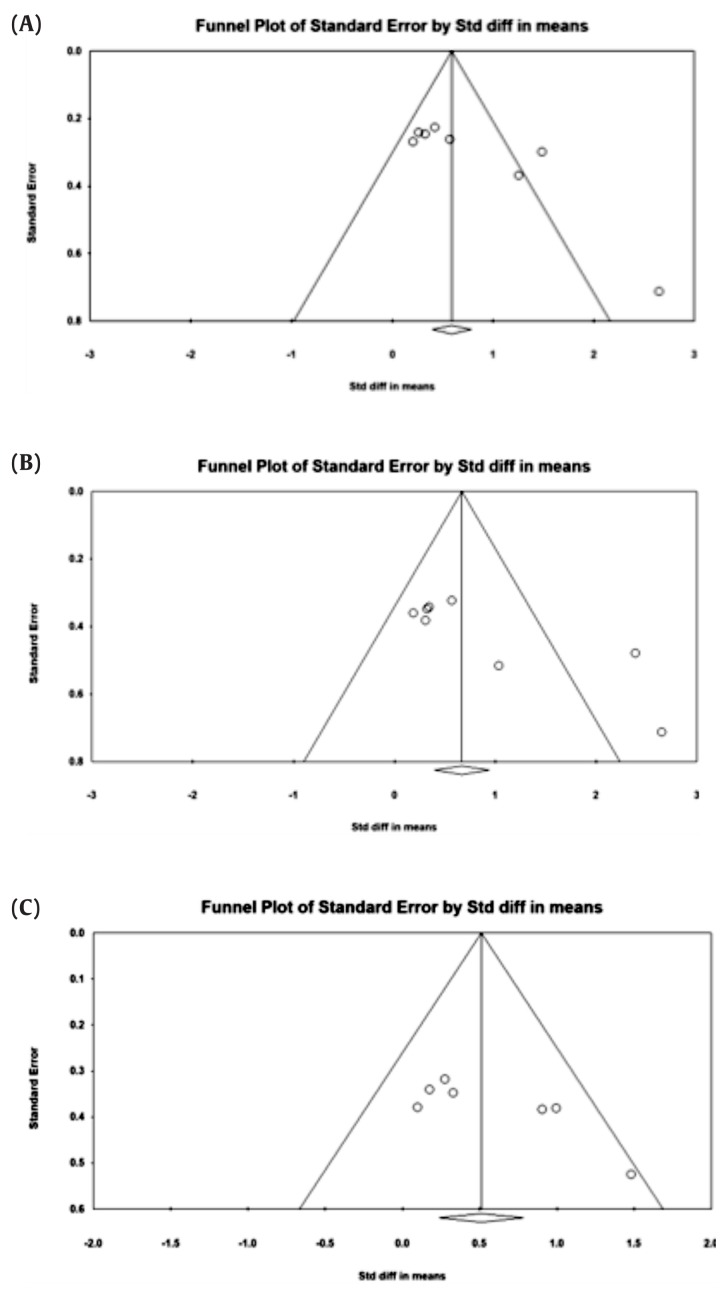
2. Publication bias
The publication bias was examined using funnel plots and fail-safe numbers. In the 8 studies used to analyze the effect sizes of combined outcomes and mental function, the fail-safe numbers were high at 89 (p < 0.05) and 57 (p < 0.05), respectively. However, the points in the funnel plot were widely spread and were not symmetrical. Therefore, publication bias can’t be ruled out. Seven studies evaluating the effect size of activity and participation distributed in the area of the funnel plot, had values that were symmetrical and the fail-safe number was 22 (p < 0.05). Therefore, it can be interpreted that there is no publication bias for these 7 studies (Figure 5).
Figure 5.
Funnel plots of outcomes (A) combined outcomes, (B) mental function, and (C) activity and participation.
Discussion
In this study, dependent variables were classified into “mental function” and “activity and participation” for analysis. The effect size of mental function was 0.850, indicating a large effect size and that of activity and participation was 0.536, a medium effect size. Even if the similar interventions were provided for similar participants, there was a difference in the effect sizes between mental function and, activity and participation [23, 29]. This finding could be due to the duration of an intervention, and the characteristics of outcome measurements. First, the duration of analyzed studies’ interventions was mostly a short period between 2 and 4 weeks, and mental function outcome measurements were mainly pencil and paper works, that could be sensitive to immediate effects [33]. On the other hand, the outcome measurements classified as activity and participation may not be sensitive to short-term effects because they reflected changes in behavior. Second, the outcome measurements of mental function directly reflect changes in behavior, because test scales such as time and distance were sensitive items, while that of activity and participation was on an ordinal scale reflecting the results of a pattern of activity. Lastly, it could be possible that participation in complex activities was limited because selected study subjects were all acute or subacute stroke patients diagnosed within 6 months from onset and insight of earlier symptoms is generally poor due to the characteristics of early VSN symptoms [22].
The analyzed studies offered various interventions to treat VSN. Amongst them, we paid attention to the immediate effects of non-invasive brain stimulation; rTMS and cTBS. It was noteworthy that the effect size of non-invasive brain stimulation therapy was large. The effect size was especially large for mental function [23, 25, 29]. This result supported a previous study showing that the non-invasive brain stimulation caused neurological changes by reducing the interhemispheric imbalance of the brains of patients with acute stroke and this had a positive effect on recovery of simple visual perception activities [16]. However, the possibility of neurological spontaneous recovery could not be ruled out because most of the patients were acute or subacute stroke victims.
This study highlighted the effectiveness of VFT which has been neglected in the rehabilitation field [27]. However, it showed large effect sizes in both mental function and, activity and participation even though the selected study had only a 2 week intervention period. It was noteworthy that other interventions showed a large effect size although only in the fragmentary visual perception test, whilst VFT revealed a large effect size in the behavioral test and the daily activity test. It may be possible that patients could learn how to correct errors if continuous feedback is received and a learned strategy may have changed the level of activity and participation consistently, even though it was a short period of time [34].
The limitation of this study was the absence of analysis of individual intervention because there were only a few selected studies for each VSN intervention treatment and only the short-term effects of treatment were analyzed. Therefore, future meta-analyses will need to examine the detailed therapeutic effects of each intervention and analyze both long-term and short-term effects.
In summary, the results of this analysis showed that the effects of interventions for treating VSN on mental function had a large effect size and those on activity and participation had a medium effect size. The effect on the combined outcomes could be interpreted as a medium effect size. In particular, non-invasive brain stimulation amongst various interventions was more effective for short-term VSN treatment.
Footnotes
Conflicts of Interest
No potential conflicts of interest relevant to this article was reported.
References
- 1.Cassidy TP, Lewis S, Gray CS. Recovery from visuospatial neglect in stroke patients. J Neurol, Neurosurg Psychiatry. 1998;64(4):555–7. doi: 10.1136/jnnp.64.4.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ringman JM, Saver JL, Woolson RF, Clarke WR, Adams HP. Frequency, risk factors, anatomy, and course of unilateral neglect in an acute stroke cohort. Neurology. 2004;63(3):468–74. doi: 10.1212/01.WNL.0000133011.10689.CE. [DOI] [PubMed] [Google Scholar]
- 3.Baylis GC, Baylis LL, Gore CL. Visual neglect can be object-based or scene-based depending on task representation. Cortex. 2004;40(2):237–46. doi: 10.1016/S0010-9452(08)70119-9. [DOI] [PubMed] [Google Scholar]
- 4.Katz N, Hartman-Maeir A, Ring H, Soroker N. Functional disability and rehabilitation outcome in right hemisphere damaged patients with and without unilateral spatial neglect. Arch Phys Med Rehabil. 1999;80(4):379–84. doi: 10.1016/S0003-9993(99)90273-3. [DOI] [PubMed] [Google Scholar]
- 5.Gillen R, Tennen H, McKee T. Unilateral spatial neglect: relation to rehabilitation outcomes in patients with right hemisphere stroke. Arch Phys Med Rehabil. 2005;86(4):763–7. doi: 10.1016/j.apmr.2004.10.029. [DOI] [PubMed] [Google Scholar]
- 6.Paci M, Matulli G, Baccini M, Rinaldi LA, Baldassi S. Reported quality of randomized controlled trials in neglect rehabilitation. Neurol Sci. 2010;31(2):159–63. doi: 10.1007/s10072-009-0198-4. [DOI] [PubMed] [Google Scholar]
- 7.Fong KN, Chan MK, Ng PP, et al. The effect of voluntary trunk rotation and half-field eye-patching for patients with unilateral neglect in stroke: a randomized controlled trial. Clin Rehabil. 2007;21(8):729–41. doi: 10.1177/0269215507076391. [DOI] [PubMed] [Google Scholar]
- 8.Eskes GA, Butler B, McDonald A, Harrison ER, Phillips SJ. Limb activation effects in hemispatial neglect. Arch Phys Med Rehabil. 2003;84(3):323–8. doi: 10.1053/apmr.2003.50012. [DOI] [PubMed] [Google Scholar]
- 9.Page SJ, Sisto S, Johnston MV, Levine P. Modified constraint-induced therapy after subacute stroke: a preliminary study. Neurorehabil Neural Repair. 2002;16(3):290–5. doi: 10.1177/154596830201600307. [DOI] [PubMed] [Google Scholar]
- 10.Kerkhoff G, Reinhart S, Ziegler W, Artinger F, Marquardt C, Keller I. Smooth pursuit eye movement training promotes recovery from auditory and visual neglect: a randomized controlled study. Neurorehabil Neural Repair. 2013;27(9):789–98. doi: 10.1177/1545968313491012. [DOI] [PubMed] [Google Scholar]
- 11.Tsang MH, Sze KH, Fong KN. Occupational therapy treatment with right half-field eye-patching for patients with subacute stroke and unilateral neglect: a randomised controlled trial. Disabil Rehabil. 2009;31(8):630–7. doi: 10.1080/09638280802240621. [DOI] [PubMed] [Google Scholar]
- 12.Serino A, Barbiani M, Rinaldesi ML, Ladavas E. Effectiveness of prism adaptation in neglect rehabilitation: a controlled trial study. Stroke. 2009;40(4):1392–8. doi: 10.1161/STROKEAHA.108.530485. [DOI] [PubMed] [Google Scholar]
- 13.Schindler I, Kerkhoff G, Karnath HO, Keller I, Goldenberg G. Neck muscle vibration induces lasting recovery in spatial neglect. J Neurol Neurosurg Psychiatry. 2002;73(4):412–9. doi: 10.1136/jnnp.73.4.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kerkhoff G, Hildebrandt H, Reinhart S, Kardinal M, Dimova V, Utz KS. A long-lasting improvement of tactile extinction after galvanic vestibular stimulation: two Sham-stimulation controlled case studies. Neuropsychologia. 2011;49(2):186–95. doi: 10.1016/j.neuropsychologia.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 15.Utz KS, Dimova V, Oppenlander K, Kerkhoff G. Electrified minds: transcranial direct current stimulation (tDCS) and galvanic vestibular stimulation (GVS) as methods of non-invasive brain stimulation in neuropsychology--a review of current data and future implications. Neuropsychologia. 2010;48(10):2789–810. doi: 10.1016/j.neuropsychologia.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Cazzoli D, Muri RM, Hess CW, Nyffeler T. Treatment of hemispatial neglect by means of rTMS--a review. Restor Neurol Neurosci. 2010;28(4):499–510. doi: 10.3233/RNN-2010-0560. [DOI] [PubMed] [Google Scholar]
- 17.Koch G, Bonni S, Giacobbe V, et al. Theta-burst stimulation of the left hemisphere accelerates recovery of hemispatial neglect. Neurology. 2012;78(1):24–30. doi: 10.1212/WNL.0b013e31823ed08f. [DOI] [PubMed] [Google Scholar]
- 18.Kim YM, Chun MH, Yun GJ, Song YJ, Young HE. The effect of virtual reality training on unilateral spatial neglect in stroke patients. Ann Rehabil Med. 2011;35(3):309–15. doi: 10.5535/arm.2011.35.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gorgoraptis N, Mah YH, Machner B, Singh-Curry V, Malhotra P, Hadji-Michael M, et al. The effects of the dopamine agonist rotigotine on hemispatial neglect following stroke. Brain. 2012;135(Pt 8):2478–91. doi: 10.1093/brain/aws154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. The Rejected Body: Feminist Philosophical Reflections on Disability. Geneva: World Health Organization; 2010. World Health Organization International Classification of Functioning, Disability and Health; pp. 19–22. [Google Scholar]
- 21.Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro) Aust J Physiother. 2002;48(1):43–9. doi: 10.1016/S0004-9514(14)60281-6. [DOI] [PubMed] [Google Scholar]
- 22.Aparicio-Lopez C, Garcia-Molina A, Garcia-Fernandez J, et al. Combination treatment in the rehabilitation of visuo-spatial neglect. Psicothema. 2016;28(2):143–9. doi: 10.7334/psicothema2015.93. [DOI] [PubMed] [Google Scholar]
- 23.Cha HG, Kim MK. Effects of repetitive transcranial magnetic stimulation on arm function and decreasing unilateral spatial neglect in subacute stroke: a randomized controlled trial. Clin Rehabil. 2016;30(7):649–56. doi: 10.1177/0269215515598817. [DOI] [PubMed] [Google Scholar]
- 24.Fong KN, Yang NY, Chan MK, et al. Combined effects of sensory cueing and limb activation on unilateral neglect in subacute left hemiplegic stroke patients: a randomized controlled pilot study. Clin Rehabil. 2013;27(7):628–37. doi: 10.1177/0269215512471959. [DOI] [PubMed] [Google Scholar]
- 25.Fu W, Song W, Zhang Y, Yang Y, Huo S, Zhang R, Wang M. Long-term effects of continuous theta-burst stimulation in visuospatial neglect. J Int Med Res. 2015;43(2):196–203. doi: 10.1177/0300060513498663. [DOI] [PubMed] [Google Scholar]
- 26.Mizuno K, Tsuji T, Takebayashi T, Fujiwara T, Hase K, Liu M. Prism adaptation therapy enhances rehabilitation of stroke patients with unilateral spatial neglect: a randomized, controlled trial. Neurorehabil Neural Repair. 2011;25(8):711–20. doi: 10.1177/1545968311407516. [DOI] [PubMed] [Google Scholar]
- 27.Rossit S, Benwell CSY, Szymanek L, et al. Efficacy of home-based visuomotor feedback training in stroke patients with chronic hemispatial neglect. Neuropsychol Rehabil. 2017:1–22. doi: 10.1080/09602011.2016.1273119. [DOI] [PubMed] [Google Scholar]
- 28.Wilkinson D, Zubko O, Sakel M, Coulton S, Higgins T, Pullicino P. Galvanic vestibular stimulation in hemi-spatial neglect. Front Integr Neurosci. 2014;8:4. doi: 10.3389/fnint.2014.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yang NY, Fong KN, Li-Tsang CW, Zhou D. Effects of repetitive transcranial magnetic stimulation combined with sensory cueing on unilateral neglect in subacute patients with right hemispheric stroke: A randomized controlled study. Clin Rehabil. 2017;31(9):1154–63. doi: 10.1177/0269215516679712. [DOI] [PubMed] [Google Scholar]
- 30.Borenstein M, Hedges LV, Higgins J, Rothstein HR. References: Wiley Online Library. 2009. [Google Scholar]
- 31.Cohen J. Statistical power for the social sciences. Hillsdale, NJ: Laurence Erlbaum and Associates; 1988. pp. 98–101. [Google Scholar]
- 32.Rosenthal R, Rubin DB. Comparing effect sizes of independent studies. Psychol Bull. 1982;92(2):500. doi: 10.1037/0033-2909.92.2.500. [DOI] [Google Scholar]
- 33.Bowen A, Hazelton C, Pollock A, Lincoln NB. Cognitive rehabilitation for spatial neglect following stroke. Cochrane Database Syst Rev. 2013 Jul 1;(7):CD003586. doi: 10.1002/14651858.CD003586.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Harvey M, Hood B, North A, Robertson IH. The effects of visuomotor feedback training on the recovery of hemispatial neglect symptoms: assessment of a 2-week and follow-up intervention. Neuropsychologia. 2003;41(8):886–93. doi: 10.1016/S0028-3932(03)00003-4. [DOI] [PubMed] [Google Scholar]