Abstract
Miltefosine, the only oral drug approved for the treatment of leishmaniasis—a parasitic disease transmitted by sandflies—is considered as a success story of research and development (R&D) by a public-private partnership (PPP). It epitomises the multiple market failures faced by a neglected disease drug: patients with low ability to pay, neglect by authorities and uncertain market size. Originally developed as an anticancer agent in the 1990s, the drug was registered in India in 2002 to treat the fatal visceral leishmaniasis. At the time, miltefosine was considered a breakthrough in the treatment, making it feasible to eliminate a regional disease. Today, access to miltefosine remains far from secure. The initial PPP agreement which includes access to the public sector is not enforced. The reality on the ground has been challenging: shortages due to inefficient supply chains, and use of a substandard product which led to a high number of treatment failures and deaths. Miltefosine received orphan drug status in the USA; when it was registered there in 2014, a priority review voucher (PRV) was awarded. The PRV, meant to facilitate drug development for neglected disease, was subsequently sold to another company for US$125 million without, to date, any apparent impact on drug access. At the heart of these concerns are questions on how to protect societal benefit of a drug developed with public investment, while clinicians worldwide struggle with its lack of affordability, limited availability and sustainability of access. This article analyses the reasons behind the postregistration access failure of miltefosine and provides the lessons learnt.
Keywords: leishmaniasis, health policy, public health, treatment
Summary box.
Miltefosine is a major therapeutic advance as the only oral drug for leishmaniasis. Its development showed that public-private partnership (PPP) is a viable model for promoting research and development (R&D) in neglected tropical diseases (NTDs).
However, access to miltefosine postlicensure is limited. Low availability and affordability have been key issues globally, despite an agreement between the manufacturer and public institution(s).
-
PPPs focusing on product development for neglected and other diseases thus should aim, beyond the registration of the product, on the following:
Mechanism(s) to enforce framework and legal agreements between partners need to improve.
Ensuring access downstream is imperative: any new NTD tools being developed should include a postmarketing or postregistration access plan.
Drug pricing structures should be transparent: manufacturers should not take advantage of a monopolistic situation to overcharge.
Priority review voucher as an incentive to enhance R&D for NTD needs fixing; applicants should seek regulatory approval and demonstrate appropriate access strategies.
Introduction
Miltefosine, the only oral drug approved for the treatment of leishmaniasis, is an example of successful research and development (R&D) for a neglected tropical disease (NTD) that fails to reach the people who need it. Leishmaniases (infectious diseases caused by multiple species of Leishmania protozoan parasites and transmitted by the Phlebotomine sandfly) result in 700 000 to 1 million new cases annually worldwide.1 More than 1.5 billion people are at risk in 97 endemic countries.2 The disease is associated with malnutrition and immunosuppression as well as with poverty, poor housing and population displacement.3–6 The visceral form (kala-azar or visceral leishmaniasis, VL) is fatal when untreated. VL is the cause of the second largest parasitic disease burden after malaria. Each year, the infection causes 50 000–90 000 cases and 20 000–30 000 deaths.7 Stigma and disability due to cutaneous lesions and mucocutaneous form—involving the destruction of mucosa of nasopharynx—are devastating.8 9 The Indian subcontinent, eastern Africa and Brazil in Latin America are regions enduring a high burden. Transmission can be human to human, but animals are reservoir hosts in zoonotic areas such as southern Europe.10 In the absence of vaccines and effective vector/reservoir control, diagnosis and treatment remain the cornerstone of public health programmes in most parts of the world.11
Treatment options for leishmaniasis are limited.12 Medicines for such a disease are not attractive targets for the profit-driven pharmaceutical industry to invest their R&D efforts because most of the patients are poor. This situation has been described as an example of market failure, a modern welfare economy concept, defined as inefficient outcomes in markets where standard assumptions (perfect competition, symmetrical information) are non-existent or violated, leading to a net society loss.13 14 In the context of pharmaceutical R&D, the term has been aptly used.15–17 The main incentive for the producers—the ability to sell products at high prices—does not apply to NTDs, and market challenges are further compounded by perceived lack of intellectual property rights protection in developing countries. For more than 50 years, VL was treated with a single regimen—injectable pentavalent antimonials—until alarming failure rates and drug resistance were shown in India.18 Other medicines for leishmaniasis (amphotericin B, paromomycin, pentamidine or liposomal amphotericin) are all parenteral, toxic or too expensive. Thus a new, better drug was sorely needed.12
In 1995, the Special Programme for Research and Training in Tropical Diseases at WHO (WHO/TDR) engaged in a public-private partnership (PPP) with a pharmaceutical company, Asta Medica19 for the clinical development of miltefosine. This development involved repurposing what was originally an anticancer compound.20 21 Clinical trials proved miltefosine administered orally was superior to antimonial injections. In 2002, India’s Central Drug Standard Control Organisation approved miltefosine (Impavido) as the first-line regimen for the treatment of VL.22 This therapeutic breakthrough was a major factor behind the launch in 2005 of a VL elimination initiative on the Indian subcontinent. Oral administration enabled more patients to be treated in primary care settings.23 24 Subsequently, miltefosine was registered in various countries for both VL and cutaneous leishmaniasis (CL) and was included in the WHO Model List of Essential Medicines (EML) in 2011.25 26
Nonetheless, access to miltefosine after it was approved—the postlicensure or postregistration phase—has been less of a success story. The medicine never became as affordable and widely available as originally anticipated. The price of miltefosine made the medicine unaffordable for the majority of patients, most of them poor and marginalised.27 Even when provided for free by the public health system in the Indian subcontinent, the supply of the drug never quite met the demand.28 The Bangladeshi VL elimination programme opted for a locally sourced, less expensive alternative product. However, this generic version was clinically ineffective, and on verification, the capsules lacked the active pharmaceutical ingredient.29
To this day the drug remains valuable as a partner drug in combination regimens to treat VL and for several other clinical indications, yet miltefosine is hardly available in countries where leishmaniasis burden is high. Widespread adoption of miltefosine was challenging, due to various reasons that this paper attempts to unravel.
Fifteen years ago, WHO/TDR made a substantial R&D investment with a clear goal to reach people in need of life-saving medicine, yet access to this medicine remains compromised. We analyse the lessons learnt in the context of R&D for NTDs, the postlicensure phase and recommend strategies moving forward to increase access to this drug.
The development of miltefosine for leishmaniasis: a PPP success story
Miltefosine (hexadecylphosphocholine) is the only oral drug currently registered for the treatment of leishmaniasis.30 Two research groups discovered the compound in the early 1980s: one in Germany investigating the antitumour activity and another in the UK working on anti-inflammatory properties.21 31 Dose-limiting gastrointestinal adverse events in several phase I and II studies32 33 resulted in the discontinuation of the drug’s development as an oral drug for the treatment of solid tumours.20 Its development as a topical formulation for treating cutaneous metastases of breast cancer continued though, and Miltex (Bayer, UK) has been marketed in Europe since 1992.34–36 In 1987, miltefosine’s antileishmaniasis activity in vitro and in vivo was described.37 Excellent oral bioavailability in mouse models was found, in addition to superiority as compared with intravenous pentavalent antimonials in these animals.38 These results established miltefosine as a development candidate for the treatment of human VL. A proof-of-concept study conducted in India39 provided encouraging data for further clinical studies.40–42
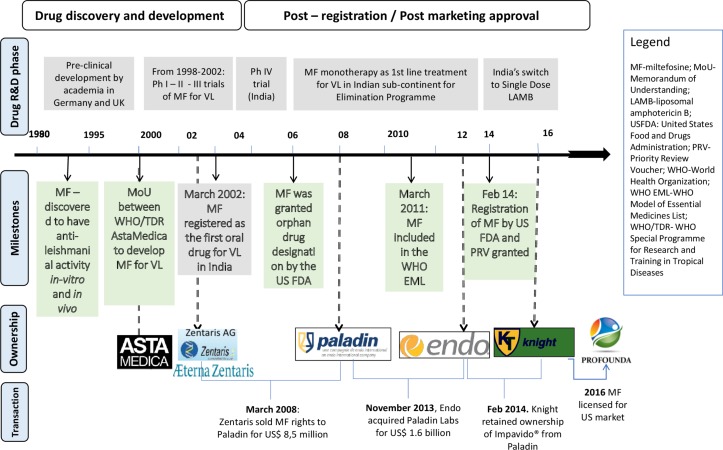
In 1995, WHO/TDR partnered with Asta Medica (later Zentaris, see figure 1), providing funding and expertise to further develop the drug for the treatment of VL.43 44 The motivation for the company in the partnership was linked to the potential market in South Asia, and substantial in-kind public input from WHO/TDR.45 Between 1996 to 2004, seven clinical trials were carried out for adults and children in India.39–42 46–49 A pivotal phase III study conducted on 398 adults demonstrated a cure rate of 94% (95% CI 91% to 97%) in the miltefosine arm. Phase IV studies involving 704 adults and 428 children were conducted in India and in Bangladesh (cure rates were of 82% overall50 and 72%, respectively51). Though trials involving miltefosine were still ongoing for CL52 53 and VL-HIV co-infection,54 in 2005—when the elimination initiative was launched—miltefosine was considered a game changer in the VL control strategy.22 46 55 The short time taken to bring the drug to market illustrates the efficiency of PPP in miltefosine’s R&D process: clinical trials started in 1996, and in 2002 the drug received approval to treat VL in India and in 2003 it was in the market (see figure 1). Oral administration (enabling straightforward management within primary care), gave rise to hopes for VL elimination.24 56
Figure 1.
Milestones in miltefosine’s journey. R&D, research and development; VL, visceral leishmaniasis.
However, implementation of miltefosine treatment faces certain challenges. Miltefosine’s reproductive toxicity requires women of childbearing age to avoid pregnancy during, and for at least 3 months after treatment.57 The required pretreatment pregnancy screening and contraceptive cover severely hindered roll-out through primary care services in resource-limited settings. Gastrointestinal problems are common adverse events: up to 62% patients report vomiting/diarrhoea, although self-limiting.31 40 47 When the drug is self-administered, even mild adverse events may compromise adherence to a full regimen. Transient elevation of hepatic transaminases and mild renal dysfunction affect up to 10%–15% of patients.50 In phase IV trials in India and Bangladesh enrolling ~1000 patients, each recorded one death possibly related to the gastrointestinal side effects of miltefosine.50 51 Adverse events are thus common and need to be managed accordingly.
The difficulty in complying with a twice daily, 1 month treatment course,58 and a long half-life,59 all concur to make miltefosine monotherapy vulnerable to emerging drug resistance. The potential for resistance became a major concern in India when the drug was sold in private pharmacies and patients resorted to shorter courses due to affordability issues. India, therefore, restricted miltefosine provision to the public sector from 2008 onwards.27 60 Preserving efficacy of this valuable drug is crucial, and approaches such as directly observed treatment (DOT) and miltefosine use in combination regimens were thus recommended.61 After being used as a monotherapy for over a decade, miltefosine effectiveness reportedly declined: in India, 7% of patients with VL on DOT relapsed within 6 months;62 and in Nepal, the relapse rate was 20% for patients within 12 months on a self-administration schedule.63 This high failure rate, at least in the paediatric populations, was partly attributed to drug underexposure in paediatric populations at the recommended dose.64 65
Meanwhile, other treatment regimens were developed for VL66–68 and in 2014 the single-dose liposomal amphotericin B was rolled out through the elimination initiative replacing miltefosine monotherapy.69 Nevertheless, miltefosine remains an important drug in leishmaniasis therapy, as a companion in combination regimens, or in VL/HIV co-infected patients who require rotating multiple regimens. The spectrum of indications for miltefosine increased over time, currently covering VL caused by Leishmania donovani and postkala-azar dermal leishmaniasis in Asia, CL caused by Leishmania Viannia (Leishmania braziliensis, Leishmania guyanensis, Leishmania panamensis) and mucocutaneous leishmaniasis (MCL) caused by L. braziliensis.69 70 For CL and MCL, miltefosine is a useful alternative for use in paediatric populations (>2 years old) where existing treatment regimens prove insufficient.71 72
Postlicensure access to miltefosine: the early years and current status
Registration
Miltefosine was initially registered in India and Germany. Later, it has been approved for treatment of VL in Nepal, and for both VL and CL in Argentina, Bangladesh, Bolivia, Colombia, Ecuador, Guatemala, Honduras, Mexico, Pakistan, Paraguay, Peru, Israel and the USA—though some licenses may have lapsed and not been renewed by the company. Miltefosine received an orphan drug designation in the European Union in 200273 and the USA in 2006.74 WHO included the drug in its EML in 2011,25 26 underlining its public health importance.
Cost
Affordability is a critical issue for medicines developed to treat a poverty-related disease. An economic analysis has shown that for miltefosine to be an effective public health tool, the drug should cost no more than US$50–60 per treatment.45 75 The initial agreements, in the form of a memorandum of understanding between WHO and Asta Medica in 1995 provided the framework to ensure availability and affordability of the drug (see figure 1). The company was allowed to market the drug in the private sector but had to make it available at a preferential price within the public sector in all developing countries, conditional on the free provision of the drug to patients. The agreements stated that this preferential price should allow the company to recover the production cost plus a modest mark-up, while setting the price for the private sector would remain under the company’s control.
But, as the negotiation for the preferential price took years, miltefosine was at first only available in the private pharmacies in India at a cost of US$150–200 per treatment.27 This price is three to four times higher than the preferential one and well beyond the means of the majority of patients with VL, who had to pay out of pocket. The situation improved when preferential pricing was put in place, and after miltefosine was restricted to the public sector in India. Based on the initial agreement, the price of an adult treatment varied between €45–54 (US$54–64) depending on order quantity, at the time set at minimum 75 000 capsules.76 In the 2004 application for inclusion in WHO EML, the price quoted by Zentaris (Asta Medica spin-off acquired by Aeterna in 2002, later became Aeterna Zentaris in 2004—see figure 1 for complete chronology of ownership changes) was €80–300 for full adult treatment, the former for use in developing countries and the latter for the private sector.77 However, the preferential price has gradually increased over time, and for a period, it was only applicable when buying a full batch or 200 000 capsules (equivalent to 3500 treatment courses), a challenge for control programmes in countries like Nepal or Bangladesh with lower case numbers. Paladin (the owner company in 2008–2014, see figure 1) expressed in its 2010 application to WHO EML that price would not be a barrier,25 yet the conditions that need to be met for the preferential price were often unclear. The pricing structure provided by the supplier was not transparent: between 2009 and 2014, the price obtained by a non- governmental organisation (NGO) operating in endemic countries reached €250. Currently, the preferential price, according to Knight Therapeutics, sits between US$120 and US$160 per course, although there is no longer an obligation for minimum quantity (see table 1).
Table 1.
Price for one full adult course of miltefosine treatment
| Price policy | Price per full course§ | Period covered | Remark |
| Preferential price for the public or non-for-profit sector in developing countries | €45–55 (US$54–64)* | 2002–2008 | Price varied based on quantity purchased; minimum order quantity (MOQ) was imposed |
| €80–110 (US$94–130) | 2009–2014 | ||
| €100–140 (US$117–164)† | 2016 onwards | No MOQ, but price still varied based on quantity | |
| Market price EU | €3000–12000 | 2012 | Direct order to the producer/distributor |
| Market price US | US$33000-51000‡ | 2016 |
*This is the original price aimed for in the agreement between WHO and Asta Medica (1995) and published officially in the latest WHO Control of Leishmaniasis guidelines (2010).
†Price quoted by Knight Therapeutics for purchase by non-profit organisations Médecins Sans Frontières (MSF).
‡For 28 caps (https://www.drugs.com/price-guide/impavido). With the recommended dose, in the USA a patient weighing >45 kg needs 50 mg thrice daily, total 84 capsules.
§One full adult course of miltefosine monotherapy uses one pack containing 56 caps. The recommended dose is 2.5 mg/kg daily for 28 days (roughly 50 mg capsule twice daily for adults weighing >25 kg).
In Europe, the drug is only registered in Germany with one course costs €3000–12 000 (US$3500–14 000).45 Several access initiatives had been in place: in 2003, the company agreed to supply miltefosine for treating leishmania under special conditions for NGOs through a German medical aid organisation.78 Compassionate access programmes also exist for special cases, for example, VL/HIV co-infected patients,79 although many clinicians may be unaware. In the USA, a full drug course is in the range of US$17 000 (for 28 capsules, while a patient weighing >45 kg would need 50 mg thrice daily, amounting to 84 capsules)80 which health insurance is unlikely to cover.81 When used for treating free-living amoebas such as Acanthamoeba keratitis, miltefosine costs have reached US$48 000.82
Availability
Table 2 gives an overview of the main availability issues by region. The situation is indeed diverse. In the Indian subcontinent, frequent shortages of miltefosine have been reported by healthcare providers.28 Small-scale donations made possible by Paladin (see figure 1) did not solve the underlying problems. Obstacles to securing supply include bureaucratic, rigid tender mechanisms for public procurement; inadequate delivery systems; lack of buffer stock and difficulties in forecasting demand, as well as the long production lead time at the manufacturer. The minimum order quantities that were imposed by the company to be eligible for preferential prices for public or not-for-profit sectors seem to play a role, nonetheless. Earlier requirements to purchase a minimum of a full batch were not always compatible with the needs of the procurers (eg, for second-line treatment or clinical trials). The requirement thus had led to oversupply and wastage as the shelf life is limited, while substantial amounts of miltefosine expired in the manufacturer’s warehouse and had to be destroyed. Moreover, the global availability of miltefosine has been mostly depending on a single source. The ownership rights have been retained by the private company and have been exchanged over the years through business mergers and acquisitions (see figure 1). The change of companies for miltefosine has led to delays in delivering the drug on time.
Table 2.
Overview of miltefosine access issues by region
| Region | Year first marketed/approved | Access issues | Supply and delivery |
| Asia27 75 108 | 2002 |
|
Through national VL control programme |
| Africa106 | NA* |
|
Usually brought in the country by NGOs or WHO |
| Europe31 78 | 2004 |
|
To be ordered directly from the company |
| North America31 86 97 | 2014 |
|
Available through CDC as an off-label treatment for PAM private market (producer price)* |
| Latin America53 110 | 2005 |
|
Through MoH in coordination with PAHO |
*Impavido is available in the USA since Knight Therapeutics provided licensing agreement to Profounda in 2015 (www.impavido.com).
CDC, Centres for Disease Control and Prevention; MoH, Ministry of Health; NGOs, non-governmental organisations; PAHO, Pan American Health Organization; PAM, primary amoebic meningoencephalitis; VL, visceral leishmaniasis.
Since 2016, Knight owns worldwide rights to Impavido (miltefosine) related to its sale and distribution in all countries other than the USA.83 84 There, it was initially available through the Centres for Disease Control and Prevention and since 2015 after being approved for leishmaniasis by FDA, through Knight’s licensee, Profounda (figure 1). Currently, to say that the drug is freely available in the global market is an overstatement. Entities that need miltefosine have to approach Knight directly and negotiate, with little scope of collective action. Even in the Indian subcontinent where miltefosine is no longer first-line treatment, the medicine is still sorely needed for an alternative regimen, used in combination with paromomycin or liposomal amphotericin B (AmBisome)—and for treatment of HIV/VL. There are no accurate data on how many patients were treated with miltefosine since it was registered for VL. However, from 2008 to 2014, 163 000 VL cases were reported in India alone.85 The majority of these patients were supposedly treated with miltefosine.
Miltefosine is considered as a valuable compound in the field of leishmaniasis and beyond, thus several trials are still ongoing. However, no change in the pricing structure is foreseeable in the near future. More frustratingly, the US$125 million earned by Knight for registering miltefosine in 2014 in the USA, did not have any impact on the problematic access in developing countries, despite advocacy efforts by the civic societies.86
What are the lessons?
Miltefosine represents a major therapeutic advance for the treatment of leishmaniasis, with possible use against other pathogens. The drug’s development is a clear success story of a partnership between WHO, a private company and strongly motivated clinical researchers in endemic countries that proved that drug development for neglected diseases by PPPs is a viable model (figure 1).87–89 However, to date, access to miltefosine is limited, even in a context where preferential pricing should apply, and the manufacturer still has a de facto monopoly of a drug as the only quality-assured source. Based on miltefosine’s development history, we present policy recommendations for the wider drug development context and eventually narrow the train of our focus on practical suggestions to improve access to miltefosine for leishmaniasis.
One of the main lessons learnt is that miltefosine’s availability has been affected by the multiple changes in the ownership rights (as shown in figure 1) which resulted in changing distribution or marketing licenses for different subsidiaries over time.90–92 The agreement between WHO/TDR and the initial company—drafted to ensure continuous supply at an affordable price for public health use— could not be enforced with the company’s later successors. The case for needing a stronger agreement to ensure access in the postapproval phase is compelling, especially with the expansion of the PPP model for drug development, through organisations like the Drugs for Neglected Diseases initiative, Medicine for Malaria Venture and other entities.
Product development partnerships should set goals beyond mere registration of an NTD drug in endemic countries.93 94 Pharmaceutical or biotech companies targeting neglected diseases seem to operate a niche business model,45 seeking profits from both public and private markets in tiered pricing mechanisms. Tiered or differential pricing structure has been argued as a rational way of funding drug or vaccine availability in endemic resource-poor countries if effective access is indeed provided.95 However, sustained access under preferential pricing may not spontaneously yield robust market mechanisms for demand. Underlying PPP agreements must, therefore, include detailed and transparent provisions for sustained access, including pricing structures and frameworks for monitoring and enforcement.93 96 The absence of these structures and frameworks was a critical factor in the miltefosine journey. Furthermore, deployment strategies for new NTD drugs should also include long-term pharmacovigilance and feasibility studies for various contexts.
Another lesson is that some current incentive mechanisms meant to enhance R&D for NTDs seem to defeat their purpose. In 2014, the US FDA approved miltefosine registration for leishmaniasis, and Knight Therapeutics—which had acquired the rights to the drug the same year—was granted a reward: the tropical disease priority review voucher (PRV).97 98 PRV is enacted since 2007 to facilitate the development of drugs for NTDs. If a sponsor achieves approval for a new chemical entity that constitutes a significant improvement for one of the listed tropical diseases, the sponsor receives a PRV which can be used for priority review of any subsequent new drug or biologic under development.99 100 The voucher is transferable, and its value has been estimated to be up to US$350 million101.
While the voucher is meant to stimulate R&D for NTD drugs, the overall impact of the programme has yet to be established.102 103 In the case of miltefosine, as a drug co-developed with public money and already licensed in key countries, the lucrative incentive seems misplaced.104 Knight Therapeutics subsequently sold its PRV to Gilead for US$125 million,105 yet no improvements in miltefosine pricing or access in global markets have been seen so far.86 We suggest that preconditions on PRVs should stipulate that applicants seek regulatory approval of the drug in endemic countries, and demonstrate appropriate access strategies.103 106
Miltefosine is not the only leishmaniasis drug produced by a single manufacturer. In the long run, competitors or generic producers might help to secure supply and to stabilise prices. Miltefosine is no longer under patent protection, but generic manufacturers would need time or support to enter the market. It is worth noting that shrinking sales volume, as the number of VL cases decreases following elimination efforts on the Indian subcontinent, may deter potential producers. Nevertheless, as this is the the only oral treatment with potential for additional clinical indications within larger disease groups, efforts to ensure there are more quality-assured producers should continue. The addition of miltefosine to WHO’s invitation of expressions of interest for NTD prequalifications in 2017, is a step in the right direction.107
Several areas need to be addressed to overcome key access barriers to miltefosine (see table 3). Reducing access barriers to a life-saving drug needs a strong and sustained political commitment from the public sector, governments and global actors alike, supported by coherent policies. International coordinated procurement by multilateral organisations or advance market commitments should be sought to ensure miltefosine’s availability in the short term. In this regard, ensuring sufficient buffer or rotating stock at the regional level seems reasonable, if all stakeholders can reach a consensus. More transparent manufacturing timelines could help to avoid shortages, along with the better consolidation of forecast and orders. In the longer run, miltefosine registration in endemic countries needs to be reviewed and pursued. The inaccessibility of miltefosine should not be taken for granted, thus advocacy must continue. The current monopolistic situation must be challenged, hence encouraging new potential producers to enter the market would be beneficial. Harmonised actions to protect access to an essential public health tool, such as miltefosine, must be provided by the global public policy.
Table 3.
Summary of miltefosine access barriers and strategies to address them
| Key area | Access barriers | Access strategy | Action(s) proposed |
| Governance and coordination | Lack of consolidated coordination to ensure miltefosine access among stakeholders in the public and private sectors | Identify effective leadership; ensure that partnerships developing drugs for NTDs include safeguards to access |
|
| Affordability | High product price | Lowering prices and ensure a healthy market (non-single supplier) |
|
| Availability | Inconsistent supply |
|
|
DNDi, Drugs for Neglected Diseases initiative; IDA, International Drug Association; KalaCORE, UKaid-funded consortium to tackle VL; MSF, Médecins Sans Frontières; NTD, neglected tropical disease; PDP, Product Development Partnership; WHO, World Health Organization.
Conclusion
The miltefosine story demonstrated the complexity of providing access to a promising NTD drug. Regrettably, apart from being a success story in R&D, the miltefosine journey embodies many flaws along the pathway from drug development to end user, and we observed issues of affordability and availability at global and country levels. Anticipated public health impact was hindered, as access barriers at different levels were not overcome. Strategies to expand access to an NTD drug thus must address affordability as a key obstacle, along with supply-side strategies that assure availability. Benefits of publicly funded medical research should be made broadly accessible to patients—neglect and imbalance should not be the end of the story.
Acknowledgments
The authors thank Els Torreele and Piero Olliaro for their critical reading of the manuscript, and Margriet den Boer, Koert Ritmeijer and Jose Postigo for their support. The authors also thank and Sarah Venis, Patricia Kahn, Kristien Cloots, Evelien Paessens; and Barbara Nasto for her expertise and enthusiasm.
Footnotes
Handling editor: Seye Abimbola
Contributors: TS, JP and MB conceived the paper. TS wrote the first draft. TS, JP, MB approved the final script.
Funding: This study has received funding from the European Union’s Horizon 2020 research and innovation programme under the Marie Sklodowska-Curie grant agreement No 642609.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1. Alvar J, Vélez ID, Bern C, et al. Leishmaniasis worldwide and global estimates of its incidence. PLoS One 2012;7:e35671 10.1371/journal.pone.0035671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Global leishmaniasis update, 2006–2015: a turning point in leishmaniasis surveillance. Wkly Epidemiol Rec 2017;92:557–72. [PubMed] [Google Scholar]
- 3. Murray HW, Berman JD, Davies CR, et al. Advances in leishmaniasis. Lancet 2005;366:1561–77. 10.1016/S0140-6736(05)67629-5 [DOI] [PubMed] [Google Scholar]
- 4. Diro E, Lynen L, Ritmeijer K, et al. Visceral leishmaniasis and HIV coinfection in East Africa. PLoS Negl Trop Dis 2014;8:e2869 10.1371/journal.pntd.0002869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Alvar J, Yactayo S, Bern C. Leishmaniasis and poverty. Trends Parasitol 2006;22:552–7. 10.1016/j.pt.2006.09.004 [DOI] [PubMed] [Google Scholar]
- 6. Harhay MO, Olliaro PL, Vaillant M, et al. Who is a typical patient with visceral leishmaniasis? Characterizing the demographic and nutritional profile of patients in Brazil, East Africa, and South Asia. Am J Trop Med Hyg 2011;84:543–50. 10.4269/ajtmh.2011.10-0321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. WHO. Leishmaniasis Fact Sheet. 2017. http://www.who.int/mediacentre/factsheets/fs375/en/ (cited 7 Jun 2017).
- 8. Hofstraat K, van Brakel WH. Social stigma towards neglected tropical diseases: a systematic review. Int Health 2016;8(Suppl 1):i53–70. 10.1093/inthealth/ihv071 [DOI] [PubMed] [Google Scholar]
- 9. Reithinger R, Dujardin JC, Louzir H, et al. Cutaneous leishmaniasis. Lancet Infect Dis 2007;7:581–96. 10.1016/S1473-3099(07)70209-8 [DOI] [PubMed] [Google Scholar]
- 10. Pigott DM, Bhatt S, Golding N, et al. Global distribution maps of the leishmaniases. Elife 2014;3:1–21. 10.7554/eLife.02851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chappuis F, Sundar S, Hailu A, et al. Visceral leishmaniasis: what are the needs for diagnosis, treatment and control? Nat Rev Microbiol 2007;5:873–82. 10.1038/nrmicro1748 [DOI] [PubMed] [Google Scholar]
- 12. den Boer M, Davidson RN. Treatment options for visceral leishmaniasis. Expert Rev Anti Infect Ther 2006;4:187–97. 10.1586/14787210.4.2.187 [DOI] [PubMed] [Google Scholar]
- 13. Bator FM. The anatomy of market failure. Q J Econ 1958;72:351–79. 10.2307/1882231 [DOI] [Google Scholar]
- 14. Kremer M. Pharmaceuticals and the developing world. J Econ Perspect 2002;16:67–90. 10.1257/089533002320950984 [DOI] [PubMed] [Google Scholar]
- 15. Pecoul B, Chirac P, Trouiller P, et al. Access to essential drugs in poor countries. Virtual Mentor 2000;2:361–7. 10.1001/virtualmentor.2000.2.7.jdsc1-0007 [DOI] [PubMed] [Google Scholar]
- 16. Trouiller P, Olliaro P, Torreele E, et al. Drug development for neglected diseases: a deficient market and a public-health policy failure. Lancet 2002;359:2188–94. 10.1016/S0140-6736(02)09096-7 [DOI] [PubMed] [Google Scholar]
- 17. Pedrique B, Strub-Wourgaft N, Some C, et al. The drug and vaccine landscape for neglected diseases (2000-11): a systematic assessment. Lancet Glob Health 2013;1:e371–9. 10.1016/S2214-109X(13)70078-0 [DOI] [PubMed] [Google Scholar]
- 18. Lira R, Sundar S, Makharia A, et al. Evidence that the high incidence of treatment failures in Indian kala-azar is due to the emergence of antimony-resistant strains of Leishmania donovani. J Infect Dis 1999;180:564–7. 10.1086/314896 [DOI] [PubMed] [Google Scholar]
- 19. Engel J. Miltefosine, the story of a successful partnership: disease endemic country - TDR - pharmaceutical industry (Zentaris). TDR News 2002;68:5. [Google Scholar]
- 20. Sindermann H, Engel J. Development of miltefosine as an oral treatment for leishmaniasis. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S17–20. 10.1016/j.trstmh.2006.02.010 [DOI] [PubMed] [Google Scholar]
- 21. Croft SL, Engel J. Miltefosine--discovery of the antileishmanial activity of phospholipid derivatives. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S4–S8. 10.1016/j.trstmh.2006.03.009 [DOI] [PubMed] [Google Scholar]
- 22. Ganguly N. Oral miltefosine may revolutionize treatment of visceral leishmaniasis. TDR News 2002:68:2. [Google Scholar]
- 23. Sundar S, Mondal D, Rijal S, et al. Implementation research to support the initiative on the elimination of kala azar from Bangladesh, India and Nepal--the challenges for diagnosis and treatment. Trop Med Int Health 2008;13:2–5. 10.1111/j.1365-3156.2007.01974.x [DOI] [PubMed] [Google Scholar]
- 24. Matlashewski G, Arana B, Kroeger A, et al. Visceral leishmaniasis: elimination with existing interventions. Lancet Infect Dis 2011;11:322–5. 10.1016/S1473-3099(10)70320-0 [DOI] [PubMed] [Google Scholar]
- 25. Paladin. Application for inclusion of miltefosine on who model list of essential medicines. 2010. http://www.who.int/selection_medicines/committees/expert/18/applications/Miltefosine_application.pdf (cited 13 Dec 2016).
- 26. WHO. 20th Model List of Essential Medicines: WHO. 2017. http://www.who.int/medicines/publications/essentialmedicines/20th_EML2017_FINAL_amendedAug2017.pdf?ua=1.
- 27. Sundar S, Murray HW. Availability of miltefosine for the treatment of kala-azar in India. Bull World Health Organ 2005;83:394–5. doi:/S0042-96862005000500018 [PMC free article] [PubMed] [Google Scholar]
- 28. Banjara MR, Hirve S, Siddiqui NA, et al. Visceral leishmaniasis clinical management in endemic districts of India, Nepal, and bangladesh. J Trop Med 2012;2012:1–8. 10.1155/2012/126093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Dorlo TP, Eggelte TA, Schoone GJ, et al. A poor-quality generic drug for the treatment of visceral leishmaniasis: a case report and appeal. PLoS Negl Trop Dis 2012;6:e1544 10.1371/journal.pntd.0001544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sundar S, Singh A. Recent developments and future prospects in the treatment of visceral leishmaniasis. Ther Adv Infect Dis 2016;3:98–109. 10.1177/2049936116646063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dorlo TP, Balasegaram M, Beijnen JH, et al. Miltefosine: a review of its pharmacology and therapeutic efficacy in the treatment of leishmaniasis. J Antimicrob Chemother 2012;67:2576–97. 10.1093/jac/dks275 [DOI] [PubMed] [Google Scholar]
- 32. Planting AST, Stoter G, Verweij J. Phase II study of daily oral miltefosine (hexadecylphosphocholine) in advanced colorectal cancer. Eur J Cancer 1993;29:518–9. 10.1016/S0959-8049(05)80142-X [DOI] [PubMed] [Google Scholar]
- 33. Verweij J, Gandia D, Planting AS, et al. Phase II study of oral miltefosine in patients with squamous cell head and neck cancer. Eur J Cancer 1993;29A:778–9. 10.1016/S0959-8049(05)80369-7 [DOI] [PubMed] [Google Scholar]
- 34. Smorenburg CH, Seynaeve C, Bontenbal M, et al. Phase II study of miltefosine 6% solution as topical treatment of skin metastases in breast cancer patients. Anticancer Drugs 2000;11:825–8. [DOI] [PubMed] [Google Scholar]
- 35. Ragnarsson-Olding B, Djureen-Mårtensson E, Månsson-Brahme E, et al. Loco-regional control of cutaneous metastases of malignant melanoma by treatment with miltefosine (Miltex®). Acta Oncol 2005;44:773–7. 10.1080/02841860500340340 [DOI] [PubMed] [Google Scholar]
- 36. Burk K, David M, Junge K, et al. Overview of the clinical development of miltefosine solution (Miltex) for the treatment of cutaneous breast cancer. Drugs Today 1994;30:59–72. [Google Scholar]
- 37. Croft SL, Neal RA, Pendergast W, et al. The activity of alkyl phosphorylcholines and related derivatives against Leishmania donovani. Biochem Pharmacol 1987;36:2633–6. 10.1016/0006-2952(87)90543-0 [DOI] [PubMed] [Google Scholar]
- 38. Kuhlencord A, Maniera T, Eibl H, et al. Hexadecylphosphocholine: oral treatment of visceral leishmaniasis in mice. Antimicrob Agents Chemother 1992;36:1630–4. 10.1128/AAC.36.8.1630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Sundar S, Rosenkaimer F, Makharia MK, et al. Trial of oral miltefosine for visceral leishmaniasis. Lancet 1998;352:1821–3. 10.1016/S0140-6736(98)04367-0 [DOI] [PubMed] [Google Scholar]
- 40. Jha TK, Sundar S, Thakur CP, et al. Miltefosine, an oral agent, for the treatment of Indian visceral leishmaniasis. N Engl J Med 1999;341:1795–800. 10.1056/NEJM199912093412403 [DOI] [PubMed] [Google Scholar]
- 41. Sundar S, Gupta LB, Makharia MK, et al. Oral treatment of visceral leishmaniasis with miltefosine. Ann Trop Med Parasitol 1999;93:589–97. 10.1080/00034983.1999.11813462 [DOI] [PubMed] [Google Scholar]
- 42. Sundar S, Makharia A, More DK, et al. Short-course of oral miltefosine for treatment of visceral leishmaniasis. Clin Infect Dis 2000;31:1110–3. 10.1086/318122 [DOI] [PubMed] [Google Scholar]
- 43. Gutteridge WE. TDR collaboration with the pharmaceutical industry. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S21–S25. 10.1016/j.trstmh.2006.02.013 [DOI] [PubMed] [Google Scholar]
- 44. Ridley RG. Product development pubilc private partnerships for disease of poverty. Are there more efficient alternatives? Are there limitations? IPPPH Meeting, London 15th-16th April. Geneva, Switzerland: Initiative on Public-Private Partnerships for Health, 2004. [Google Scholar]
- 45. Moran M, Ropars A-L, Guzman J, Dias J, Garrison C. The new landscape of neglected disease drug development: a pharmacetical r&d policy project. 2005. London: London School of Economics and Political Science, Wellcome Trust. [Google Scholar]
- 46. Sundar S, Jha TK, Thakur CP, et al. Oral miltefosine for the treatment of Indian visceral leishmaniasis. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S26–S33. 10.1016/j.trstmh.2006.02.011 [DOI] [PubMed] [Google Scholar]
- 47. Sundar S, Jha TK, Thakur CP, et al. Oral miltefosine for Indian visceral leishmaniasis. N Engl J Med 2002;347:1739–46. 10.1056/NEJMoa021556 [DOI] [PubMed] [Google Scholar]
- 48. Sundar S, Jha TK, Sindermann H, et al. Oral miltefosine treatment in children with mild to moderate Indian visceral leishmaniasis. Pediatr Infect Dis J 2003;22:434–8. 10.1097/01.inf.0000066877.72624.cb [DOI] [PubMed] [Google Scholar]
- 49. Bhattacharya SK, Jha TK, Sundar S, et al. Efficacy and tolerability of miltefosine for childhood visceral leishmaniasis in India. Clin Infect Dis 2004;38:217–21. 10.1086/380638 [DOI] [PubMed] [Google Scholar]
- 50. Bhattacharya SK, Sinha PK, Sundar S, et al. Phase 4 trial of miltefosine for the treatment of Indian visceral leishmaniasis. J Infect Dis 2007;196:591–8. 10.1086/519690 [DOI] [PubMed] [Google Scholar]
- 51. Rahman M, Ahmed BN, Faiz MA, et al. Phase IV trial of miltefosine in adults and children for treatment of visceral leishmaniasis (kala-azar) in Bangladesh. Am J Trop Med Hyg 2011;85:66–9. 10.4269/ajtmh.2011.10-0661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Soto J, Toledo J, Gutierrez P, et al. Treatment of American cutaneous leishmaniasis with miltefosine, an oral agent. Clin Infect Dis 2001;33:e57–61. 10.1086/322689 [DOI] [PubMed] [Google Scholar]
- 53. Soto J, Berman J. Treatment of New World cutaneous leishmaniasis with miltefosine. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S34–40. 10.1016/j.trstmh.2006.02.022 [DOI] [PubMed] [Google Scholar]
- 54. Ritmeijer K, Dejenie A, Assefa Y, et al. A comparison of miltefosine and sodium stibogluconate for treatment of visceral leishmaniasis in an Ethiopian population with high prevalence of HIV infection. Clin Infect Dis 2006;43:357–64. 10.1086/505217 [DOI] [PubMed] [Google Scholar]
- 55. Mondal D, Singh SP, Kumar N, et al. Visceral leishmaniasis elimination programme in India, Bangladesh, and Nepal: reshaping the case finding/case management strategy. PLoS Negl Trop Dis 2009;3:e355 10.1371/journal.pntd.0000355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Singh OP, Hasker E, Boelaert M, et al. Elimination of visceral leishmaniasis on the Indian subcontinent. Lancet Infect Dis 2016;16:e304–9. 10.1016/S1473-3099(16)30140-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Dorlo TP, Balasegaram M, Lima MA, et al. Translational pharmacokinetic modelling and simulation for the assessment of duration of contraceptive use after treatment with miltefosine. J Antimicrob Chemother 2012;67:1996–2004. 10.1093/jac/dks164 [DOI] [PubMed] [Google Scholar]
- 58. Uranw S, Ostyn B, Dorlo TP, et al. Adherence to miltefosine treatment for visceral leishmaniasis under routine conditions in Nepal. Trop Med Int Health 2013;18:179–87. 10.1111/tmi.12025 [DOI] [PubMed] [Google Scholar]
- 59. Dorlo TP, van Thiel PP, Huitema AD, et al. Pharmacokinetics of miltefosine in Old World cutaneous leishmaniasis patients. Antimicrob Agents Chemother 2008;52:2855–60. 10.1128/AAC.00014-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sundar S, Olliaro PL. Miltefosine in the treatment of leishmaniasis: Clinical evidence for informed clinical risk management. Ther Clin Risk Manag 2007;3:733–40. [PMC free article] [PubMed] [Google Scholar]
- 61. van Griensven J, Balasegaram M, Meheus F, et al. Combination therapy for visceral leishmaniasis. Lancet Infect Dis 2010;10:184–94. 10.1016/S1473-3099(10)70011-6 [DOI] [PubMed] [Google Scholar]
- 62. Sundar S, Singh A, Rai M, et al. Efficacy of miltefosine in the treatment of visceral leishmaniasis in India after a decade of use. Clin Infect Dis 2012;55:543–50. 10.1093/cid/cis474 [DOI] [PubMed] [Google Scholar]
- 63. Rijal S, Ostyn B, Uranw S, et al. Increasing failure of miltefosine in the treatment of Kala-azar in Nepal and the potential role of parasite drug resistance, reinfection, or noncompliance. Clin Infect Dis 2013;56:1530–8. 10.1093/cid/cit102 [DOI] [PubMed] [Google Scholar]
- 64. Ostyn B, Hasker E, Dorlo TP, et al. Failure of miltefosine treatment for visceral leishmaniasis in children and men in South-East Asia. PLoS One 2014;9:e100220 10.1371/journal.pone.0100220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Dorlo TP, Rijal S, Ostyn B, et al. Failure of miltefosine in visceral leishmaniasis is associated with low drug exposure. J Infect Dis 2014;210:146–53. 10.1093/infdis/jiu039 [DOI] [PubMed] [Google Scholar]
- 66. Sundar S, Rai M, Chakravarty J, et al. New treatment approach in Indian visceral leishmaniasis: single-dose liposomal amphotericin B followed by short-course oral miltefosine. Clin Infect Dis 2008;47:1000–6. 10.1086/591972 [DOI] [PubMed] [Google Scholar]
- 67. Sundar S, Sinha PK, Rai M, et al. Comparison of short-course multidrug treatment with standard therapy for visceral leishmaniasis in India: an open-label, non-inferiority, randomised controlled trial. Lancet 2011;377:477–86. 10.1016/S0140-6736(10)62050-8 [DOI] [PubMed] [Google Scholar]
- 68. Bern C, Adler-Moore J, Berenguer J, et al. Liposomal amphotericin B for the treatment of visceral leishmaniasis. Clin Infect Dis 2006;43:917–24. 10.1086/507530 [DOI] [PubMed] [Google Scholar]
- 69. WHO. Control of the leishmaniases: report of a meeting of the WHO Expert Committee on the Control of Leishmaniases, Geneva, 22–26 March 2010. World Health Organ Tech Rep Series No 949. Geneva, Switzerland, 2010:1–186. [Google Scholar]
- 70. Aronson N, Herwaldt BL, Libman M, et al. Diagnosis and treatment of leishmaniasis: clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Am J Trop Med Hyg 2017;96:24–45. 10.4269/ajtmh.16-84256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Rubiano LC, Miranda MC, Muvdi Arenas S, et al. Noninferiority of miltefosine versus meglumine antimoniate for cutaneous leishmaniasis in children. J Infect Dis 2012;205:684–92. 10.1093/infdis/jir816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Berger BA, Cossio A, Saravia NG, et al. Cost-effectiveness of meglumine antimoniate versus miltefosine caregiver DOT for the treatment of pediatric cutaneous leishmaniasis. PLoS Negl Trop Dis 2017;11:e0005459 10.1371/journal.pntd.0005459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. European Medicine Agency. European medicine agency orphan drug designation for miltefosine. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/orphans/2009/11/human_orphan_000280.jsp&murl=menus/medicines/medicines.jsp&mid=WC0b01ac058001d12b (cited 13 Jan 2017).
- 74. Food and Drugs Administration. Miltefosine orphan drug designation to treat leishmaniasis. 2006. https://www.accessdata.fda.gov/scripts/opdlisting/oopd/detailedIndex.cfm?cfgridkey=229406 (cited 27 Dec 2016).
- 75. den Boer M, Argaw D, Jannin J, et al. Leishmaniasis impact and treatment access. Clin Microbiol Infect 2011;17:1471–7. 10.1111/j.1469-0691.2011.03635.x [DOI] [PubMed] [Google Scholar]
- 76. Olliaro P, Sundar S. Anthropometrically derived dosing and drug costing calculations for treating visceral leishmaniasis in Bihar, India. Trop Med Int Health 2009;14:88–92. 10.1111/j.1365-3156.2008.02195.x [DOI] [PubMed] [Google Scholar]
- 77. Pietras M. Application for inclusion of miltefosine on WHO model list of essential medicines. http://www.who.int/selection_medicines/committees/expert/18/applications/Miltefosine_application.pdf (15 Dec 2016).
- 78. AdisInsight. Miltefosine. 2016. http://adis.springer.com/drugs/800001883 (cited 1 Apr 2017).
- 79. Nitin Kashyap U, Raghunandan H. Comparison of drug approval process in United States & Europe. J Pharm Sci Res 2013;5:131–6. [Google Scholar]
- 80. Drugs. Impavido prices, patient assistance programs. https://www.drugs.com/price-guide/impavido (cited 21 Aug 2017).
- 81. Murray HW. Leishmaniasis in the United States: treatment in 2012. Am J Trop Med Hyg 2012;86:434–40. 10.4269/ajtmh.2012.11-0682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. The STAT Team. Drug to combat brain-eating amoeba exists — but how to get it to patients? 2016. https://www.statnews.com/2016/09/16/amoeba-drug-miltefosine/ (cited 26 Apr 2017).
- 83. Blackwell R. Knight Therapeutics reacquires leishmaniasis drug Impavido - The Globe and Mail. https://www.theglobeandmail.com/report-on-business/knight-therapeutics-reacquires-leishmaniasis-drug-impavido/article29252299/ (cited 6 Jun 2017).
- 84. Knight Therapeutic Inc. Knight obtains impavido worldwide rights. http://www.gud-knight.com/en/knight-obtains-impavido-worldwide-rights (cited 10 Jun 2017).
- 85. National Vector Borne Disease Control Programme - Ministry of Health India. Kala Azar Situation in India. http://nvbdcp.gov.in/ka-cd.html (cited 9 Feb 2018).
- 86. DNDi. Patient Access to Miltefosine in Developing Countries Not Secure Despite Award of US FDA PRV Sold for USD 125 Million. 2014. http://www.dndi.org/2014/media-centre/press-releases/pr-miltefosine-prv/ (cited 2 Jan 2017).
- 87. Moran M. A breakthrough in R&D for neglected diseases: New ways to get the drugs we need. PLoS Med 2005;2:0828–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Grace C. Product development partnerships (PDPs): lessons from PDPs established to develop new health technologies for neglected diseases. London: UK Department of International Development, 2010. https://www.gov.uk/government/publications/product-development-partnerships-pdps-lessons-from-pdps-established-to-develop-new-health-technologies-for-neglected-diseases. [Google Scholar]
- 89. Nwaka S, Ridley RG. Virtual drug discovery and development for neglected diseases through public-private partnerships. Nat Rev Drug Discov 2003;2:919–28. 10.1038/nrd1230 [DOI] [PubMed] [Google Scholar]
- 90. Zentaris receives approval to market Impavido in Germany. http://archives.who.int/eml/expcom/expcom14/miltefosine/Attachment1-JuergenEngel_20041207eng.pdf (cited 11 Jan 2017).
- 91. Evaluategroup. Æterna zentaris receives first regulatory approval for impavido for parasitic skin disease. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=64808 (cited 11 Jan 2017).
- 92. Profounda, Inc. launches Impavido (miltefosine), the first and only oral Rx treatment for visceral, mucosal and cutaneous leishmaniasis, in the United States. http://www.prnewswire.com/news-releases/profounda-inc-launches-impavido-miltefosine-the-first-and-only-oral-rx-treatment-for-visceral-mucosal-and-cutaneous-leishmaniasis-in-the-united-states-300238867.html (cited 11 Jan 2017).
- 93. Drugs for Neglected Diseases Initiative. An innovative approach to r&d for neglected patients: ten years of experience & lessons learned by DNDi, 2014. [Google Scholar]
- 94. Frost LJ, Reich MR. Creating access to health technologies in poor countries. Health Aff 2009;28:962–73. 10.1377/hlthaff.28.4.962 [DOI] [PubMed] [Google Scholar]
- 95. Danzon PM, Towse A. Differential pricing for pharmaceuticals: reconciling access, R&D and patents. Int J Health Care Finance Econ 2003;3:183–205. [DOI] [PubMed] [Google Scholar]
- 96. DNDi. New report reviews the successful development of the antimalarial ASAQ. 2015. https://www.dndi.org/2015/media-centre/news-views-stories/news/asaq-lessons-learned/ (cited 22 Jun 2017).
- 97. Food and Drugs Administration. Miltefosine approval letter. 2014. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2014/204684Orig1s000Approv.pdf
- 98. Knight Therapeutics Inc Announces FDA approval for impavido® (miltefosine) for the treatment of visceral, mucosal and cutaneous leishmaniasis - awarded priority review voucher. http://www.gud-knight.com/en/knight-therapeutics-inc-announces-fda-approval-for-impavido-miltefosine-for-the-treatment-of-visceral-mucosal-and-cutaneous-leishmaniasis-awarded-priority-review-voucher (cited 2 Jan 2017).
- 99. Ridley DB, Grabowski HG, Moe JL. Developing drugs for developing countries. Health Aff 2006;25:313–24. 10.1377/hlthaff.25.2.313 [DOI] [PubMed] [Google Scholar]
- 100. Kesselheim AS. Drug development for neglected diseases - the trouble with FDA review vouchers. N Engl J Med 2008;359:1981–3. 10.1056/NEJMp0806684 [DOI] [PubMed] [Google Scholar]
- 101. Berman J, Radhakrishna T. The tropical disease priority review voucher: a game-changer for tropical disease products. Am J Trop Med Hyg 2017;96 10.4269/ajtmh.16-0099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Jain N, Hwang T, Franklin JM, et al. Association of the priority review voucher with neglected tropical disease drug and vaccine development. JAMA 2017;318:388 10.1001/jama.2017.7467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Ridley DB, Régnier SA. The commercial market for priority review vouchers. Health Aff 2016;35:776–83. 10.1377/hlthaff.2015.1314 [DOI] [PubMed] [Google Scholar]
- 104. Doshi P. US incentive scheme for neglected diseases: a good idea gone wrong? BMJ 2014;349:g4665–3. 10.1136/bmj.g4665 [DOI] [PubMed] [Google Scholar]
- 105. Marketwired. Knight sells priority review voucher to gilead. http://www.marketwired.com/press-release/knight-sells-priority-review-voucher-to-gilead-tsx-gud-1969777.htm (cited 2 Jan 2017).
- 106. Moran M, Strub-Wourgaft N, Guzman J, et al. Registering new drugs for low-income countries: the African challenge. PLoS Med 2011;8:e1000411–3. 10.1371/journal.pmed.1000411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. World Health Organization. FPPs & APIs Eligible for Prequalification (“EOIs”). 2017. https://extranet.who.int/prequal/sites/default/files/documents/EOI-NTD-v5.pdf
- 108. Berman J, Bryceson AD, Croft S, et al. Miltefosine: issues to be addressed in the future. Trans R Soc Trop Med Hyg 2006;100(Suppl 1):S41–S44. 10.1016/j.trstmh.2006.02.009 [DOI] [PubMed] [Google Scholar]
- 109. Solano-Gallego L, Miró G, Koutinas A, et al. LeishVet guidelines for the practical management of canine leishmaniosis. Parasit Vectors 2011;4:86 10.1186/1756-3305-4-86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Monge-Maillo B, López-Vélez R. Miltefosine for visceral and cutaneous leishmaniasis: drug characteristics and evidence-based treatment recommendations. Clin Infect Dis 2015;60:1398–404. 10.1093/cid/civ004 [DOI] [PubMed] [Google Scholar]
- 111. WHO. WHO aims to improve access to antileishmanial medicines in affected countries. 2016. http://www.who.int/neglected_diseases/news/improve_access_to_antileishmanial_medicines/en/ (cited 19 Jun 2017).