Abstract
Patients with congenital heart disease have improved survival rates, and most patients are now expected to survive into adulthood. This improved survival has resulted in increasing numbers of women with congenital heart disease who are of childbearing age. This patient population requires specialized advice on contraception and pregnancy risk. Understanding the unique challenges this population presents is key to providing appropriate care.
Keywords: congenital heart disease, pregnancy, pregnancy risk, CARPREG score, tetralogy of Fallot
INTRODUCTION
Long-term survival rates of infants born with congenital heart disease continue to improve, allowing the vast majority of patients with access to current surgical and medical technologies to reach adulthood. In most cases, however, this improved survival does not imply a cure of congenital heart disease but, rather, enhanced palliation. These maturing patients experience sequelae of their heart disease and repair that often requires medical, pharmacologic, and repeat surgical intervention. Women with congenital heart disease experience unique challenges across the spectrum of the reproductive health cycle, not only with pregnancy and delivery. Being aware and informed regarding these challenges is necessary for adult cardiologists to provide appropriate care for this distinctive patient population.
CONGENITAL HEART DISEASE EFFECTS ON DEVELOPMENT, MENSES, AND FERTILITY
Women with congenital heart disease experience psychosocial as well as medical concerns during adolescence and young adulthood that may impact their reproductive health. Dissatisfaction with physical appearance related to scars; difficulty with intrapersonal relationships; and concerns about fertility, inheritability of congenital heart disease, and possible negative effects on cardiac health related to pregnancy have all been demonstrated to negatively affect overall sexual health.1 Importantly, the majority of patients rated the information provided by their physician regarding sexuality and congenital heart disease as suboptimal,1 which underscores the importance of providing information on these issues to patients and their families starting at an early age. Recognizing the psychological impact of congenital heart disease and integrating life coaching and counseling into the care of these patients may improve overall quality of life.
Menarche in women with congenital heart disease has been shown to be delayed, with the longest delay noted in cyanotic women.2 After menarche, women with cyanotic congenital heart disease are more likely to have dysfunctional uterine bleeding, which may represent a chronic anovulatory state, dysfunction of the hypothalamic-pituitary-ovarian axis, or abnormal uterine hemostasis.2,3 Menorrhagia may also be a complication for women required to use long-term anticoagulants. Careful evaluation and treatment of these menstrual irregularities is indicated to prevent complications that include iron deficiency anemia and the long-term concerns associated with chronic anovulation.2
CONTRACEPTION
In-depth knowledge of contraceptive methods, including pharmacology, implementation, and interaction with cardiac physiology is necessary to provide appropriate counseling to the patient and cooperative care with gynecology colleagues. Women who have a cardiac condition that leads to a prohibitive risk of pregnancy should be counseled regarding permanent contraceptive methods or long-acting reversible contraception. Microinsert hysteroscopic sterilization is shown to be a safe and effective method for permanent contraception in women with severe cardiac disease, avoiding the risk associated with general anesthesia for surgical tubal ligation.4 Estrogen-containing contraception is contraindicated in women with cyanotic congenital heart disease and should not be a first-line therapy for women with mechanical valves or single ventricle circulation. Both intrauterine devices (IUDs) that elute progestin as well as progestin implants provide long-term contraception with the advantage of inherent compliance. These methods may also help with menorrhagia associated with cyanotic congenital heart disease or with anticoagulation use. While theoretical concern for IUD-associated endocarditis has been raised, there is no compelling data to suggest that IUD use in women with congenital heart disease is associated with higher rates of endocarditis.
PRE-CONCEPTION COUNSELING
All women with congenital heart disease who desire pregnancy should be provided with expert pre-conception counseling regarding risks of cardiac complications during pregnancy, risk of cardiac disease in the offspring, risk of fetal morbidity and mortality, and long-term cardiac sequelae related to the hemodynamic stressors of pregnancy. Most women with congenital heart disease can complete a pregnancy, though women with the Eisenmenger complex, significant congestive heart failure, severe obstructive lesions, and connective tissue disorders with a risk of aortic dissection should be counseled against becoming pregnant. Appropriate risk assessment in individual patients requires a comprehensive understanding of the patient's anatomy and hemodynamics and how the marked physiologic changes of pregnancy and delivery will affect her.
Several risk stratification models are available to delineate maternal risk in women with congenital heart disease. The CARPREG5 risk predictor model can be applied to women with congenital heart disease but was developed after prospectively studying women with both acquired and congenital heart disease. In this model, there are four predictors of primary cardiac events during pregnancy (Table 1). One point is assigned for each risk factor present. The risk of a cardiac event during pregnancy is estimated at 5%, 27%, and 75% for a pregnancy with 0, 1, or > 1 point, respectively.5 Although this approach to risk prediction is straightforward and can be very helpful during pre-conception counseling, it may provide a less accurate risk assessment for mothers with congenital heart disease as many conditions affecting these women, such as right heart dysfunction, are not addressed. Application of the CARPREG score in a cohort of women with congenital heart disease did indeed demonstrate that severe pulmonary valve regurgitation and/or sub-pulmonary ventricular systolic dysfunction are important additional risk predictors that should be added to the model.6 More recently, the ZAHARA study7 evaluated pregnancy complications in women with congenital heart disease and demonstrated additional risk factors in predicting cardiac complications during pregnancy (Table 2). The expected rates of cardiac complications based on these factors are shown in Table 3.
Table 1.
Predictors of primary cardiac events during pregnancy (CARPREG study). Adapted from Siu S et al.5

Table 2.
Predictors of cardiac complication during pregnancy and associated points for risk calculation (ZAHARA study). Adapted from Drethen W et al.7
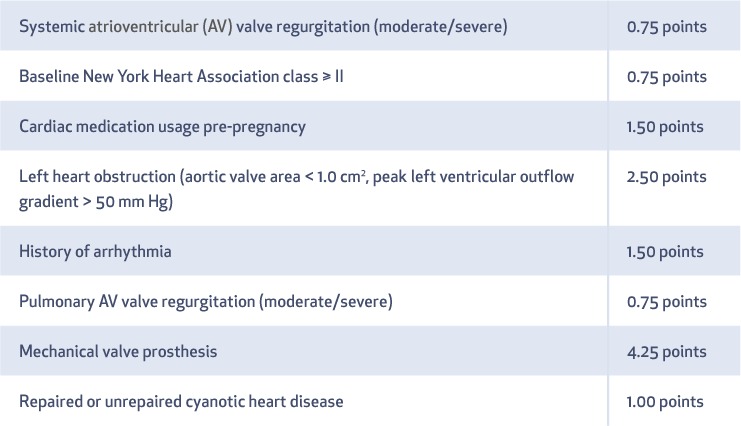
Table 3.
Cardiac complications during completed pregnancies as calculated by the ZAHARA risk score. Adapted from Drethen W et al.7

The World Health Organization (WHO) has stratified risk of cardiac complication into four classes, with recommendations on follow-up during pregnancy based on this risk strata (Table 4).8 After assessing the risk of cardiac complication during pregnancy, the physician should review management strategies with the patient to address these potential complications. If the patient requires anticoagulation during pregnancy, options for anticoagulation regimens should be reviewed during the pre-conception visit.
Table 4.
Modified World Health Organization Classification of Maternal Cardiovascular Risk. Adapted from the European Society of Cardiology Guidelines on the Management of Cardiovascular Diseases during Pregnancy.8

Pregnancies complicated by maternal congenital heart disease result in higher rates of neonatal complications than those in the general population, as prematurity, fetal demise, and fetal growth restriction are all potentially related to the inability to increase cardiac output to meet the demands of pregnancy. This hypothesis is supported by a prospective study that demonstrated an increased rate of neonatal complications in pregnancies where maternal cardiac output declined as gestation advanced or third-trimester umbilical artery Doppler flows were abnormal.9 The CARPREG and ZAHARA studies also examined maternal factors that predicted adverse neonatal outcomes, and many of these factors—including maternal congestive heart failure, cyanosis, outflow tract obstruction, and tobacco use—would potentially limit cardiac output and oxygen content delivery to the placental circulation.5,7 Maternal use of cardiac medications and anticoagulation also results in risk to the fetus, including teratogenicity, fetal growth restriction, and hemorrhage. All cardiac medications prescribed must be evaluated and a decision made as to which drugs to continue throughout pregnancy. A good understanding of the FDA schema for classifying the risk of drugs during pregnancy and breastfeeding is imperative. Many cardiac medications are classified as risk unknown (C), risk proven (D), or risk contraindicated (X) but may still be used if the benefit to the mother outweighs the potential risks. All statins, angiotensin converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs) should be discontinued. Nitrates and hydralazine can be substituted for ACE inhibitors and ARBs in women with systolic heart failure.
The offspring of patients with congenital heart disease have an increased risk of having congenital heart disease. The risk is variable, as the genetic mechanisms resulting in cardiac defects are heterogeneous in most forms of congenital heart disease.10 The overall risk in offspring was found to be 4.1% in the British collaborative study of patients with congenital heart disease.11 Women with conotruncal defects should have testing for 22q11 microdeletion, as offspring of patients with this microdeletion will have a 50% chance of inheriting the microdeletion and a markedly increased risk of congenital heart defects. It is appropriate to obtain screening fetal echocardiography in most cases when parental congenital heart disease is present.
PREGNANCY AND DELIVERY MANAGEMENT
Mothers with congenital heart disease are best managed with a multidisciplinary team of caregivers, including maternal fetal medicine specialists, anesthesiologists, neonatologists, and cardiologists. Cardiology follow-up during pregnancy is determined by the patient's cardiovascular risk as outlined in the WHO stratification (Table 4). Delivery in a tertiary care center is recommended for mothers at high risk of cardiac decompensation. The preferred method of delivery in most women with congenital heart disease is vaginal delivery, with Cesarean delivery reserved for obstetrical indications, mothers with decompensated heart failure, and mothers who are anticoagulated with a vitamin K antagonist. Cesarean delivery may be the best option in mothers with pulmonary hypertension and severe obstructive valvular lesions. The cardiac output demands of labor can be tempered with good anesthesia/analgesia, and most mothers benefit from epidural anesthesia. For women in whom excessive Valsalva is a concern, labor can be completed using a forceps-assisted delivery without maternal pushing. Postpartum attention to thromboembolic prophylaxis and fluid management is critical.
LESION-SPECIFIC MANAGEMENT AND OUTCOMES
Most women with atrial septal defect (ASD) and/or partial anomalous pulmonary venous return (PAPVR) can complete a pregnancy with low morbidity, excluding those who have a significant increase in pulmonary vascular resistance. Women with repaired ASD or PAPVR are classified as WHO group I, and those unrepaired are considered WHO group II. Closure of ASD during pregnancy should not be performed unless the mother has a significant change in cardiovascular status. While pregnancy is a hypercoagulable state, therapeutic anticoagulation is not routinely indicated during gestation to prevent paradoxical emboli. Recognized cardiac complications in this patient population include arrhythmia, preeclampsia, fetal mortality, and fetal growth restriction in mothers with unrepaired ASD, especially if the maternal age was > 30 years or the patient had a prior history of arrhythmia.12 During labor and delivery, air filters should be used on all intravenous lines to prevent air emboli.
Women with unrepaired ventricular septal defects (VSD) generally fall into two categories: small restrictive defects with no significant hemodynamic consequences or large defects with significant elevation in pulmonary vascular resistance (the Eisenmenger syndrome). Women with repaired VSD are classified as WHO group I, whereas those with small, restrictive VSD are classified as WHO group II. Women with Eisenmenger syndrome are classified as WHO group IV, in which pregnancy is contraindicated. The ZAHARA investigators demonstrated that compared to women with unrepaired VSD, those with repaired VSD were at higher risk of preterm labor and of having infants who were small for their gestational age; this may reflect some degree of cardiac compromise in those women who had VSDs large enough to require surgical intervention.13 Women with unrepaired VSD demonstrated a higher incidence of preeclampsia compared to the general population.13
Women with coarctation of the aorta may have cardiac complications during pregnancy even after repair of the coarctation. Potential complications include pregnancy-induced hypertension, preeclampsia, ascending aorta dilatation, and aortic dissection or rupture. A review of cases from the Mayo Clinic demonstrated that 30% of women with coarctation had hypertension during pregnancy, with 73% of them having a hemodynamically significant native or residual coarctation.14 Appropriate monitoring and treatment of blood pressure is indicated during pregnancy.
Tetralogy of Fallot has been successfully repaired since the late 1950s. As a result, it is now the most common lesion among previously cyanotic women who are considering pregnancy. Pregnancy after tetralogy of Fallot repair is usually well tolerated; however, concerning issues in this patient population include pulmonary valve regurgitation, right heart dysfunction, arrhythmia, and increased pulmonary vascular resistance in those women who initially had a systemic-to-pulmonary-artery shunt for palliation. Women with tetralogy of Fallot should undergo cardiology monitoring at least each trimester. Women with right ventricular systolic or diastolic dysfunction are at increased risk of volume overload during the first week postpartum, so earlier follow-up with a cardiologist is indicated in the postpartum period.
Women with more complex forms of congenital heart disease, including Ebstein anomaly, complete transposition of the great arteries (status post atrial or arterial switch operation), congenitally corrected transposition of the great arteries, and single ventricle circulation (status post Fontan palliation) have all been reported to have successful pregnancies but with increased risk to both mother and fetus. This patient population requires subspecialty management from pre-conception to postpartum.
CONCLUSION
Women with congenital heart disease that may complicate pregnancy are a growing population. Although most women can have a successful pregnancy, even those with complex anatomy, success is dependent on accurate pre-conception counseling and meticulous multidisciplinary management during pregnancy, delivery, and the postpartum period.
KEY POINTS
Most women with congenital heart disease can have a successful pregnancy but may require multidisciplinary care.
Vaginal delivery is the preferred method of delivery for most women with congenital heart disease.
Women with even “simple” congenital heart disease benefit from pre-conception counseling regarding risks of pregnancy.
Footnotes
Conflict of Interest Disclosure:
The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1. Opić P, Roos-Hesselink JW, Cuypers JA, . et al. Sexual functioning is impaired in adults with congenital heart disease. Int J Cardiol. 2013. October 9; 168 4: 3872– 7. [DOI] [PubMed] [Google Scholar]
- 2. Canobbio MM, Perloff J, Rapkin A.. Gynecological health of females with congenital heart disease. Int J Cardiol. 2005. February 28; 98 3: 379– 87. [DOI] [PubMed] [Google Scholar]
- 3. Canobbio M, Rapkin AJ, Perloff JK, Lin A, Child JS.. Menstrual patterns in women with congenital heart disease. Pediatr Cardiol. 1995. Jan-Feb; 16 1: 12– 5. [DOI] [PubMed] [Google Scholar]
- 4. Famuyide AO, Hopkins MR, El-Nashar SA, . et al. Hysteroscopic sterilization in women with severe cardiac disease: experience at a tertiary center. Mayo Clin Proc. 2008. April; 83 4: 431– 8. [DOI] [PubMed] [Google Scholar]
- 5. Siu SC, Sermer M, Colman JM, . et al .; Cardiac Disease in Pregnancy (CARPREG) Investigators Prospective multicenter study of pregnancy outcomes in women with heart disease. Circulation. 2001. July 31; 104 5: 515– 21. [DOI] [PubMed] [Google Scholar]
- 6. Khairy P, Ouyang DW, Fernandes SM, Lee-Parritz A, Economy KE, Landzberg MJ.. Pregnancy outcomes in women with congenital heart disease. Circulation. 2006. January 31; 113 4: 517– 24. [DOI] [PubMed] [Google Scholar]
- 7. Drenthen W, Boersma E, Balci A, . et al .; ZAHARA Investigators Predictors of pregnancy complications in women with congenital heart disease. Eur Heart J. 2010. September; 31 17: 2124– 32. [DOI] [PubMed] [Google Scholar]
- 8. Regitz-Zagrosek V, Lundqvist CB, Borghi C, . et al .; ESC Committee for Practice Guidelines ESC Guidelines on the management of cardiovascular diseases during pregnancy: the Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011. December; 32 24: 3147– 97. [DOI] [PubMed] [Google Scholar]
- 9. Wald RM, Silversides CK, Kingdom J, . et al. Maternal Cardiac Output and Fetal Doppler Predict Adverse Neonatal Outcomes in Pregnant Women With Heart Disease. J Am Heart Assoc. 2015. November 23; 4 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zaidi S, Brueckner M. Genetics and Genomics of Cogenital Heart Disease. Circ Res. 2017. March 17; 120 6: 923– 40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Burn J, Brennan P, Little J, . et al. Recurrence risks in offspring of adults with major heart defects: results from first cohort of British collaborative study. Lancet. 1998. January 31; 351 9099: 311– 6. [DOI] [PubMed] [Google Scholar]
- 12. Yap SC, Drenthen W, Meijboom FJ, . et al .; ZAHARA investigators Comparison of pregnancy outcomes in women with repaired versus unrepaired atrial septal defect. BJOG. 2009. November; 116 12: 1593– 601. [DOI] [PubMed] [Google Scholar]
- 13. Yap SC, Drenthen W, Pieper PG, . et al .; ZAHARA investigators Pregnancy outcome in women with repaired versus unrepaired isolated ventricular septal defect. BJOG. 2010. May; 117 6: 683– 9. [DOI] [PubMed] [Google Scholar]
- 14. Beauchesne LM, Connolly HM, Ammash NM, Warnes CA.. Coarctation of the aorta: outcome of pregnancy. J Am Coll Cardiol. 2001. November 15; 38 6: 1728– 33. [DOI] [PubMed] [Google Scholar]


