Abstract
Dissection of the internal carotid artery (ICA) accounts for 5% to 25% of ischemic strokes in young adults. We report a case of spontaneous recanalization of a traumatic ICA dissection in which carotid duplex (CDU) and transcranial color-coded duplex ultrasound (TCCD) were used. A 47-year-old male presented with intermittent episodes of headache, blurry vision, anisocoria, and loss of taste sensation following a whiplash injury while body surfing.
Magnetic resonance angiogram (MRA) of the neck revealed absent flow in the cavernous ICA and a clot at the skull base. Carotid duplex, used to further evaluate flow, demonstrated reverberating color Doppler and spectrum signal. A TCCD showed ICA occlusion and smaller-caliber intracranial ICA. The patient reported for follow-up after 1 month on anticoagulation therapy. Upon his return, CDU and TCCD were normal and the ICA showed normal color and spectrum signals. Computed tomography angiogram confirmed ultrasound findings of a dramatic improvement of ICA patency. Additionally, the patient reported that his headaches had resolved.
Extracranial CDU and TCCD are useful for monitoring patient progress in cases of spontaneous recanalization following carotid artery dissection. These inexpensive and noninvasive imaging modalities proved to be critical in the initial and follow-up evaluations of the extracranial and intracranial vascular system, providing a strong alternative to expensive magnetic resonance imaging and invasive angiograms and offering more hemodynamic information than “static” MRA.
Keywords: transcranial color-coded duplex ultrasound, TCCD, internal carotid artery dissection, carotid duplex
INTRODUCTION
The ongoing improvement of neuroimaging techniques has made it increasingly possible to recognize the frequency of cervical carotid artery dissection. Although the reported incidence of internal carotid artery (ICA) dissection is 2.5 to 3 per 100,000 patients per year,1,2 the true incidence may be higher since some cases may be asymptomatic or present with only minor symptoms. Carotid artery dissection is responsible for 2.5% to 5% of all ischemic strokes and 5% to 25% of strokes in young patients.1,3,4 In the late 1970s, Fisher et al. recognized the clinical and radiological features of dissection syndromes.4 Dissections may occur due to direct forceful or even minor trauma of the neck. If there are no detectable underlying reasons for the dissection, it is diagnosed as spontaneous, although other intrinsic or environmental risk factors may exist.5 Internal carotid artery dissection results in carotid territory ischemia, which typically presents with unilateral headache, facial or neck pain, Horner syndrome, pulsatile tinnitus, retinal ischemic symptoms, different types of aphasia, and occasionally cranial nerve palsy.6
Early recognition and management is critical in preventing ischemic cerebrovascular complications, but clinical diagnosis can be challenging in these patients. Initial and follow-up evaluation of the extracranial and intracranial vascular systems can be performed with carotid duplex ultrasound (CDU) and the more recently available transcranial color-coded duplex ultrasound (TCCD).7 Traditionally, patients have been subject to repeat angiography or repeat contrast-enhanced computed tomography (CT)/magnetic resonance imaging (MRI) scanning. TCCD is an effective tool that is noninvasive and less expensive than MRI and eliminates the radiation exposure associated with CT.
Here we report a case of spontaneous recanalization of a traumatic ICA dissection in which CDU and TCCD proved to be valuable tools in diagnosis and management.
CASE REPORT
A 47-year-old male presented to Houston Methodist Hospital with intermittent episodes of headache, blurry vision, anisocoria, and loss of taste sensation following a whiplash injury that he sustained while body surfing. Within a day of the accident, the patient began to experience pressure on the right side of his face and behind the right eye and soreness in his neck. Two days after the accident, he developed flashes of light in both eyes that persisted when his eyes were closed. Four days after the accident, anisocoria prompted the patient to see an ophthalmologist, who determined that symptoms were not due to an eye-related issue. A CT scan did not reveal any bleeding. The patient then experienced acute loss of taste in the anterior tongue 1 week after the injury. After neurological investigation, the patient underwent an MRI with contrast of the brain, orbit, and neck as well as magnetic resonance angiogram (MRA) of the head and neck. The MRA neck image revealed absent flow in the cavernous internal carotid artery (ICA) and a clot at the skull base (Figures 1, 2 A, 3 A). Carotid duplex showed a reverberating color Doppler and spectrum, and TCCD showed ICA occlusion and smaller-caliber intracranial ICA (Figures 2 B, 4). A thrombus was noted in the ICA at the dissection site. The patient was subsequently treated with warfarin and enoxaparin.
Figure 1.

Internal carotid artery occlusion on neck magnetic resonance angiography (arrow).
Figure 2.
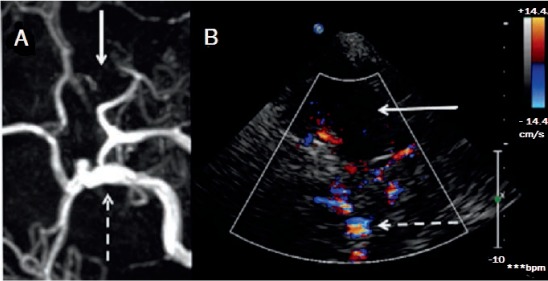
Right internal carotid artery (ICA) occlusion (A) on magnetic resonance angiography and (B) on transcranial color-coded Doppler. Arrow: absent ICA
Figure 3.
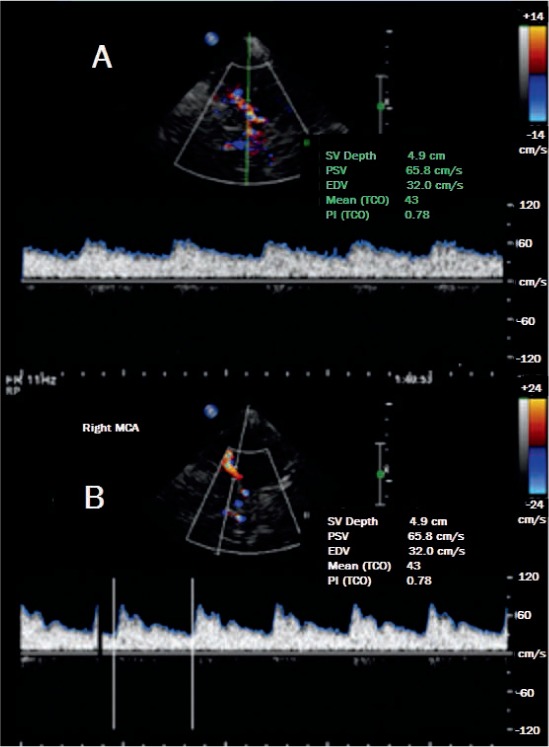
(A) Blunted middle cerebral artery signal at 49-mm depth (baseline on 8.09.2012) and (B) normal waveform with straight systolic upstroke (post-recanalization on 9.04.2012).
Figure 4.
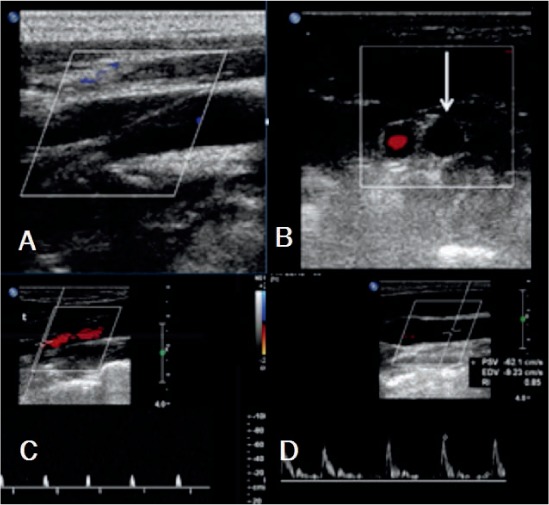
(A) Right internal carotid artery (ICA) occlusion longitudinal view, (B) cross-sectional view (white arrow: absent color Doppler signal of the ICA), (C) ICA spectra waveform (high-resistance spikes to/from waveforms in the ICA), and (D) high-resistance waveform in the common carotid artery.
Upon his follow-up visit after 1 month on anticoagulation therapy, the patient reported resolution of both his headaches and neurological signs. CDU and TCCD were normal and ICA showed normal color and spectrum signals (Figures 3 B, 5, 6). Computer tomography angiogram confirmed the ultrasound findings (Figure 7). The dramatic improvement of ICA patency, confirmed via CDU and TCCD, correlated with resolution of the patient's symptoms.
Figure 5.
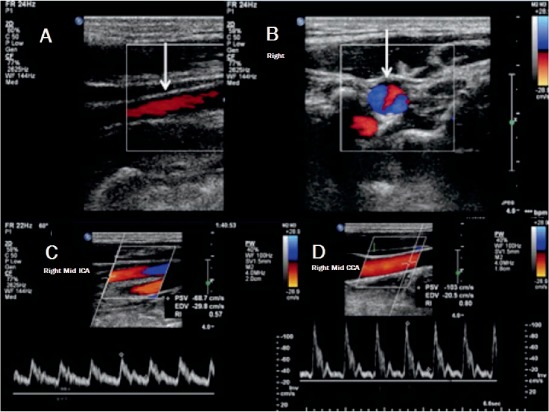
(A) Internal carotid artery (ICA) recanalization longitudinal view (color Doppler signal present in ICA), (B) cross-sectional view (color Doppler signal present in ICA), (C) ICA spectra waveform (low-resistance waveform in the ICA), and (D) common carotid artery normal waveform.
Figure 6.
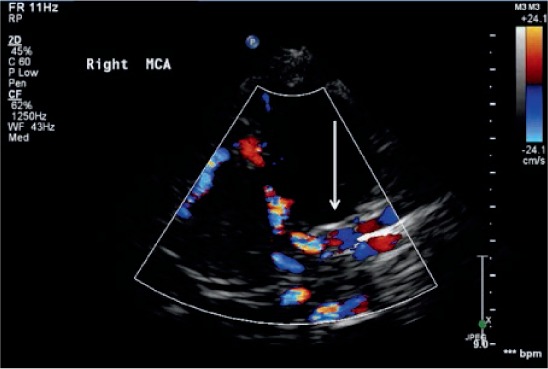
Recanalized right internal carotid artery (arrow) on transcranial color-coded Doppler.
Figure 7.
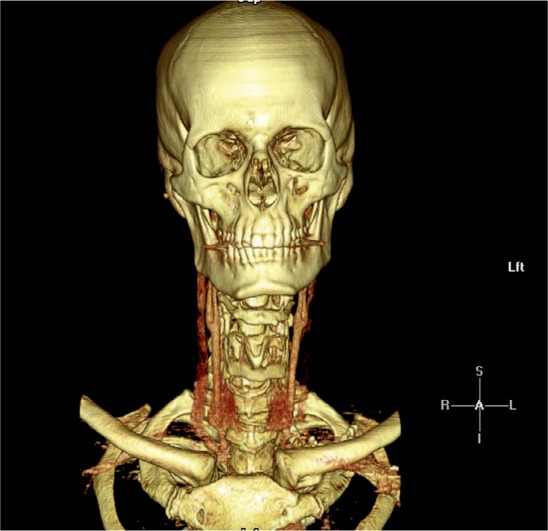
Recanalization on computed tomography angiogram.
DISCUSSION
Carotid dissection can be managed safety and inexpensively with an ultrasound-only strategy using TCCD and CDU. Additionally, both modalities are effective tools for facilitating the diagnosis of carotid dissection. Many carotid artery dissections heal spontaneously. Follow-up studies have reported recanalization of occlusions in 33% to 50% of patients.1,5 In a prospective observational study, Nedeltchev et al. found that 160 out of 268 patients (60%) experienced complete recanalization of spontaneous carotid artery dissection. The likelihood of achieving complete recanalization within 1-, 3-, 6-, or 12-month follow-up was 15.7% at 1 month, 50.4% at 3 months, and 59.7% at 6 and 12 months; however, recanalization after 12 months was rare.8 Patients with mild and local symptoms have a much more favorable prognosis and higher frequency of complete recanalization.1,5
The goal of management is to limit neurological deficits by reducing the risk of thromboembolic complications. Treatment choices include thrombolysis, anticoagulation or antiplatelet therapy, and endovascular interventions. In the absence of randomized clinical trial data, treatment decisions must be made on a case-by-case basis.4,9–11 The risk of a recurrent dissection is considered to be relatively rare, at about 2% within the first month and 1% annually; however, this data was challenged by Beletsky at al. in a prospective study that indicated a reoccurrence rate as high as 10.4%.2
Follow-up noninvasive imaging includes extracranial carotid duplex and TCCD examination to monitor patient progress and document healing of the dissection before stopping anticoagulant therapy. These inexpensive and noninvasive modalities are viable alternatives to invasive angiogram and provide more hemodynamic information than “static” MRA.
While TCCD and CDU have many positive features compared to MRI and CT angiography, there are some pertinent drawbacks. The equipment and expertise required for MRI and CT angiography are more widely available than for TCCD and CDU, which could limit use of the latter. Additionally, MRI and CT angiography allow visualization of the entire carotid artery segment, whereas TCCD and CDU use normal signals above and below the blind spot and the skull base to infer normal flow. Although these drawbacks should be considered, they should not negate the advantages of TCCD and CDU when these modalities are available.
CONCLUSION
Early imaging with carotid duplex and transcranial color-coded duplex ultrasound can be valuable in diagnosing and managing carotid dissection. The benefits of these therapies are 3-fold: they are less expensive than MRI, less invasive than angiography, and entail less radiation exposure than CT. While equipment and skilled operators for TCCD and CDU may be less abundant than the technology and personnel required for MRI and CT, these modalities should be considered as viable alternatives for evaluating carotid dissection when they are available. This strategy is economical and minimizes contrast and radiation exposure while providing evaluation of the cervical and intracranial carotid arteries.
Acknowledgments
We would like to thank Nyla Ismail, Ph.D., for critically reviewing this manuscript.
Footnotes
Conflict of Interest Disclosure:
The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1. Patel RR, Adam R, Maldjian C, Lincoln CM, Yuen A, Arneja A.. Cervical carotid artery dissection: current review of diagnosis and treatment. Cardiol Rev. 2012. May-Jun; 20 3: 145– 52. [DOI] [PubMed] [Google Scholar]
- 2. Beletsky V, Nadareishvili Z, Lynch J, . et al. Cervical arterial dissection: time for a therapeutic trial? Stroke. 2003. December; 34 12: 2856– 60. [DOI] [PubMed] [Google Scholar]
- 3. Mattioni A, Paciaroni M, Sarchielli P, Murasecco D, Pelliccioli GP, Calabresi P.. Multiple cranial nerve palsies in a patient with internal carotid artery dissection. Eur Neurol. 2007; 58 2: 125– 7. [DOI] [PubMed] [Google Scholar]
- 4. Thanvi B, Munshi SK, Dawson SL, Robinson TG.. Carotid and vertebral artery dissection syndromes. Postgrad Med J. 2005. June; 81 956: 383– 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009. July; 8 7: 668– 78. [DOI] [PubMed] [Google Scholar]
- 6. Baumgartner RW, Bogousslavsky J. Clinical manifestations of carotid dissection. Front Neurol Neurosci. 2005; 20: 70– 6. [DOI] [PubMed] [Google Scholar]
- 7. Srinivasan J, Newell DW, Sturzenegger M, Mayberg MR, Winn HR.. Transcranial Doppler in the evaluation of internal carotid artery dissection. Stroke. 1996. July; 27 7: 1226– 30. [DOI] [PubMed] [Google Scholar]
- 8. Nedeltchev K, Bickel S, Arnold M, . et al. R2-recanalization of spontaneous carotid artery dissection. Stroke. 2009. February; 40 2: 499– 504. [DOI] [PubMed] [Google Scholar]
- 9. Redekop GJ. Extracranial carotid and vertebral artery dissection: a review. Can J Neurol Sci. 2008. May; 35 2: 146– 52. [DOI] [PubMed] [Google Scholar]
- 10. Lyrer P, Engelter S. Antithrombotic drugs for carotid artery dissection. Cochrane Database Syst Rev. 2010. October 6; 10: CD000255. [DOI] [PubMed] [Google Scholar]
- 11. Machet A, Fonseca AC, Oppenheim C, . et al. Does anticoagulation promote mural hematoma growth or delayed occlusion in spontaneous cervical artery dissections? Cerebrovasc Dis. 2013; 35 2: 175– 81. [DOI] [PubMed] [Google Scholar]


