Dear Editor,
A 24-year-old female presented with palpable, painful nodules, which had appeared three weeks prior, on both calves. Laboratory tests showed no abnormalities. Magnetic resonance imaging (MRI) revealed oval lesions showing high signal intensity in short-tau inversion-recovery (STIR) sequences, with enhancement after gadolinium infusion, in the ventral portion of the muscles, together with oval lesions in the bones that showed low signal intensity in T1-weighted sequences and high signal intensity in STIR sequences (Figures 1 and 2). The diagnostic hypothesis was musculoskeletal sarcoidosis, which was confirmed by biopsy. After treatment with corticosteroids, there was regression of the symptoms and of the lesions seen on the MRI scans.
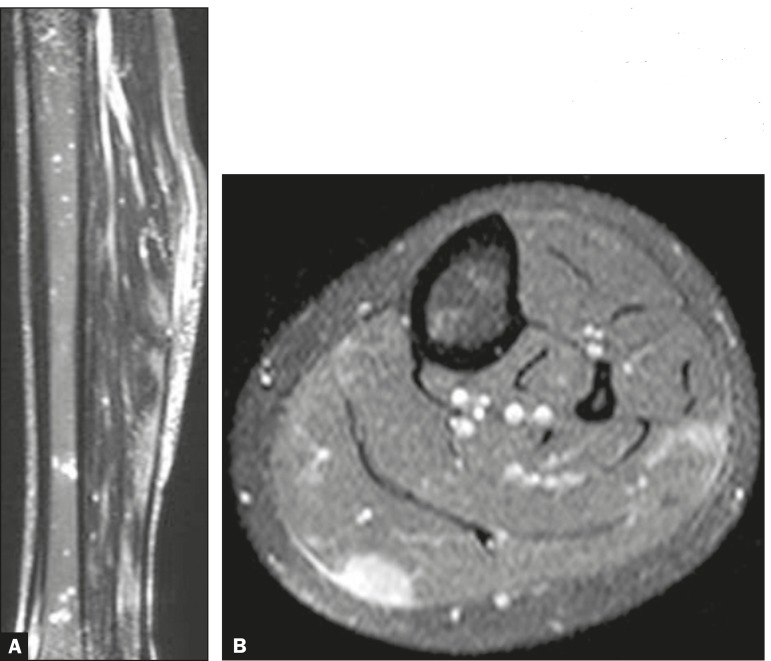
Figure 1.
A: Non-contrast-enhanced STIR sequence showing nodules of high signal intensity, in the muscle and in the bone. B: Contrast-enhanced, fat-saturated T1-weighted sequence showing enhancement of the nodule to be biopsied.
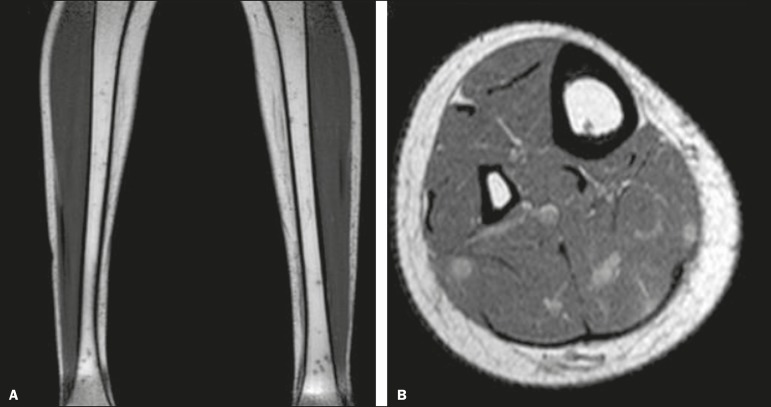
Figure 2.
A: Non-contrast-enhanced T1-weighted sequence showing nodules of low signal intensity in the bone. B: Contrast-enhanced T1-weighted sequence showing enhancement of the nodules in the muscle.
Sarcoidosis is a systemic disease of unknown cause(1), which causes inflammatory granulomas in organs and tissues(2), affecting more women than men(3). Musculoskeletal sarcoidosis is a rare condition, first reported by Licharew in 1908(4), that has two forms of clinical presentation(2,5): nodular and myopathic. The nodular form often involves the extremities, especially the legs(1), giving rise to solitary or multiple nodules(2). The most common sign is a painless or only slightly painful mass(1,2). The myopathic form involves the muscles in a symmetric, diffuse manner and does not form masses, manifesting as slowly progressive myalgia, with weakness, and atrophy(2), as well as resulting in high levels of creatine phosphokinase(1).
Although joint involvement is common in musculoskeletal sarcoidosis, the presence of muscle and bone lesions is not; it is believed that such lesions are indicative of a chronic and prolonged disease course(6). Symptomatic muscle involvement occurs in 1.4% of the known cases of sarcoidosis(2,7), compared with 1.0-13.0% (estimated mean, 5.0%) for symptomatic skeletal involvement(1).
Because of the excellent tissue contrast provided by MRI, it can reveal musculoskeletal changes that are not visible on X-rays, as well as allowing the identification of the lesions that are most suitable for biopsy(1,8-11). On MRI, nodular sarcoidosis has a characteristic appearance that can facilitate its accurate diagnosis-it typically consists of central areas of fibrosis that show low signal intensity in all sequences, together with peripheral areas of granulomas that show high signal intensity in T2weighted sequences and contrast enhancement(1,6)-findings collectively known as a "black star". In myopathic sarcoidosis, the MRI findings are nonspecific-the affected muscle shows an increase in signal intensity in T2-weighted sequences(6), also showing atrophy and fatty replacement in some cases(1).
The differential diagnosis of musculoskeletal sarcoidosis includes other benign and malignant mesenchymal masses, such as tophi, pannus formations, and xanthomas(1). In 50-80% of sarcoidosis patients, a biopsy reveals granuloma formation in muscle tissue. However, in most cases, the patient shows no signs or symptoms of the disease(1).
REFERENCES
- 1.Moore SL, Teirstein AE. Musculoskeletal sarcoidosis spectrum of appearances at MRI. Radiographics. 2003;23:1389–1399. doi: 10.1148/rg.236025172. [DOI] [PubMed] [Google Scholar]
- 2.Otake S. Sarcoidosis involving skeletal muscle imaging findings and relative value of imaging procedures. AJR Am J Roentgenol. 1994;162:369–375. doi: 10.2214/ajr.162.2.8310929. [DOI] [PubMed] [Google Scholar]
- 3.Hennessy TW, Ballard DJ, DeRemee RA. The influence of diagnostic access bias on the epidemiology of sarcoidosis a populationbased study in Rochester, Minnesota, 1935-1984. J Clin Epidemiol. 1988;41:565–570. doi: 10.1016/0895-4356(88)90060-1. [DOI] [PubMed] [Google Scholar]
- 4.Licharew A. Moskauer venerologische und dermatologische Gesellschaft. Dermatol Zentralbl. 1908;11:235–235. [Google Scholar]
- 5.Hinterbuchner CN, Hinterbuchner LP. Myopathic syndrome in muscular sarcoidosis. Brain. 1964;87:355–366. doi: 10.1093/brain/87.2.355. [DOI] [PubMed] [Google Scholar]
- 6.Koyama T, Ueda H, Togashi K. Radiologic manifestations of sarcoidosis in various organs. Radiographics. 2004;24:87–104. doi: 10.1148/rg.241035076. [DOI] [PubMed] [Google Scholar]
- 7.Mayock RL, Bertrand P, Morrison CE. Manifestations of sarcoidosis Analysis of 145 patients, with a review of nine series selected from the literature. Am J Med. 1963;35:67–89. doi: 10.1016/0002-9343(63)90165-7. [DOI] [PubMed] [Google Scholar]
- 8.Chagas-Neto FA, Nogueira-Barbosa MH, Lorenzato MM. Diagnostic performance of 3D TSE MRI versus 2D TSE MRI of the knee at 1 5 T, with prompt arthroscopic correlation, in the detection of meniscal and cruciate ligament tears. Radiol Bras. 2016;49:69–74. doi: 10.1590/0100-3984.2015.0042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simão MN, Vinson EN, Spritzer CE. Magnetic resonance imaging evaluation of meniscoid superior labrum normal variant or superior labral tear. Radiol Bras. 2016;49:220–224. doi: 10.1590/0100-3984.2015.0083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sá Neto JL, Simão MN, Crema MD. Diagnostic performance of magnetic resonance imaging in the assessment of periosteal reactions in bone sarcomas using conventional radiography as the reference. Radiol Bras. 2017;50:176–181. doi: 10.1590/0100-3984.2015.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loures FB, Carrara RJ, Góes RFA. Anthropometric study of the knee in patients with osteoarthritis intraoperative measurement versus magnetic resonance imaging. Radiol Bras. 2017;50:170–175. doi: 10.1590/0100-3984.2016.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]