Abstract
Objective
This study examined the mediating role of body dissatisfaction between body mass index (BMI) and subsequent disordered eating (e.g. dieting and restricting/purging) among early adolescent African American girls.
Study Design
Participants included 701 African American girls in 6th and 7th grades in urban schools serving low-income communities, mean age 12.15 (SD=0.72) years. Participants were assessed at baseline and approximately 6 months later. Objectively measured height and weight were used to calculate BMI z-score. Participants completed questionnaires on body size dissatisfaction and recent dieting and restricting/purging behaviors.
Results
At baseline, 51.5% of participants were overweight/obese, and 60.4% expressed body dissatisfaction and a desire to be smaller. Path analytic analyses revealed change in body dissatisfaction significantly mediated the relation between initial BMI z-score and increases in dieting behaviors (B = 0.924, SE=0.280, p=.001) but not restricting/purging behaviors (p =.05).
Conclusions
Body dissatisfaction explains some associations between excess body weight and subsequent disordered eating symptoms among early adolescent, African American girls. Body dissatisfaction, identified by screening, may be an indicator of further negative consequences, including disordered eating behaviors.
Keywords: disordered eating, African American adolescents, body dissatisfaction, overweight, obesity, early adolescent girls
Introduction
Clinical eating pathology has been estimated to affect one in eight young women, and even subclinical disordered eating is associated with functional impairment and distress (Stice, Becker, & Yokum, 2013). Unhealthy eating attitudes and disordered eating behaviors are relatively widespread, with a national survey reporting that 21.8% of girls engaged in disordered eating behaviors within the last 30 days (Pisetsky, May Chao, Dierker, May, & Striegel-Moore, 2008). Disordered eating behaviors and obesity are recognized predictors of clinically diagnosable eating disorders (Russell-Mayhew, McVey, Bardick, & Ireland, 2012).
Driven by a desire to be thinner, overweight girls engage in more disordered eating behaviors (e.g., fasting or skipping meals or vomiting) than their normal weight peers (Olvera et al., 2015; Tanofsky-Kraff et al., 2004). They may refuse to eat for periods of time and may have an intense fear of gaining weight (Olvera et al., 2015; Tanofsky-Kraff et al., 2004). Also, they may engage in binge eating episodes (defined as eating a larger amount of food than most people eat in a discrete period of time), feeling embarrassed or disgusted by the amount of food eaten, and feeling out of control (American Psychiatric Association, 2013). Bucchianeri and colleagues found that, for females, body dissatisfaction increased between middle and high school, and increased further during the transition to young adulthood (Bucchianeri, Arikian, Hannan, Eisenberg, & Neumark-Sztainer, 2013), suggesting that early adolescence is a critical time period to intervene and prevent future consequences of body dissatisfaction. In the United States, the prevalence of overweight/obesity is high, particularly among adolescent African-American girls (42.5%) (Ogden, Carroll, Kit, & Flegal, 2014; Ogden et al., 2016). This evidence taken together suggests that the high prevalence of overweight/obesity among African American girls may put them at risk for both body dissatisfaction and disordered eating (Austin et al., 2011).
Historically, most studies of disordered eating (e.g., dieting, restricting/purging symptoms) and body dissatisfaction (e.g., the inconsistency between perceived and ideal body size) (Silberstein, Striegel-Moore, Timko, & Rodin, 1988) were conducted among middle to upper-class White girls (DeLeel, Hughes, Miller, Hipwell, & Theodore, 2009; Grabe & Hyde, 2006). The prevailing view in American popular culture and the psychological literature is that African American girls experience less body dissatisfaction than White girls (Bucchianeri et al., 2016; Mastria, 2002; Smolak & Striegel-Moore, 2001). However, stereotypes suggesting that minority adolescents are buffered from the negative consequences of body dissatisfaction may preclude ethnic-minority youth from seeking eating disordered treatment or participating in research (Mastria, 2002). Much of what is known about body dissatisfaction is based largely on cross sectional, college age, majority White samples (Grabe & Hyde, 2006). Therefore, there is a need to examine body dissatisfaction longitudinally specifically among African American youth.
One longitudinal study found that that BMI was differentially related to subsequent body dissatisfaction among African American youth, but did not examine effects specifically among African American girls due to limited sample size (Sutter, Nishina, & Adams, 2015). Furthermore, in a longitudinal sample of White Spanish youth, body dissatisfaction mediated the relation between gender and later disordered eating, with girls showing a significantly stronger relation between body dissatisfaction and disordered eating than boys (Ferreiro, Seoane, & Senra, 2014). BMI was not considered in this study.
Longitudinal studies that examine the mechanisms linking body size (measured objectively), body dissatisfaction, and disordered eating are needed urgently among early adolescent African American girls to determine whether the associations reported among White girls generalize to girls of other races or ethnicities (Bucchianeri et al., 2016; Witherspoon, Latta, Wang, & Black, 2013). To address this gap, we tested the hypothesis that association between baseline BMI and disordered eating behaviors 6 months later is mediated by body dissatisfaction among a sample of African American, early adolescent girls.
Material and Methods
Participants, Design, and Procedures
The current study is a secondary analysis of data from a study designed to test an intervention. Participants in the current analysis were 701 African American middle school girls participating in a multi-level, school-based program to promote health and prevent obesity conducted with 6th and 7th grade girls in 22 schools in a large urban public school system. School inclusion criteria were >75% of students eligible for free and reduced priced meals (FARMs) and >70% of students African American. Adolescent girls in grade 6 or 7 with no chronic illness or health condition that would interfere with participation in a physical education class were recruited to participate through mailings or in-person during lunch shifts and at school-sponsored events. A total of 1,076 students (out of a total pool of 1,804) were screened and eligible, and 789 students were randomized to participate in: 1) a small-group health promotion intervention focused on healthy nutrition and physical habits (intervention) or 2) an intervention on stress reduction (control). Of the 789 students randomized, 701 were African American.
Students were evaluated at baseline (Time 1) and at the conclusion of the interventions (6 months following baseline, Time 2) during the fall and spring semesters. Data collection occurred in multiple waves between the years 2009–2013. At each evaluation, height and weight were measured, and participants completed questionnaires regarding physical activity, diet, eating behaviors, and psychological well-being. Assessments were conducted after school using audio enhanced computer-administered questionnaires. Informed consent (caregiver) and assent (youth) were obtained from all participants prior to the start of the study. This study was approved by Institutional Review Boards at both the university and the public school system where the study took place.
Measures
Weight status
Body Mass Index (BMI) was calculated from weight and height, measured twice by trained staff using standardized procedures. If weight or height differed, a third measure was taken and the two closest measures were averaged. Weight was measured in kilograms to the nearest tenth using standard scales (TANITA 300GS, Tanita Corp., Tokyo, Japan). Height was measured by a portable stadiometer (Shorr Productions, Olney, Maryland) in centimeters to the nearest tenth. BMI-for-age percentiles and z-scores were based on sex-specific- CDC 2000 growth standards (Kuczmarski et al., 2002). Weight status was defined as: underweight (BMI-for-age < 5th percentile, normal: BMI-for-age < 85th percentile; overweight: BMI-for-age ≥85th and <95th percentile; obese: BMI-for-age ≥95th percentile (Ogden et al., 2016).
Body dissatisfaction
Body dissatisfaction was measured using culturally adapted, age- and sex-specific, 9-point silhouette scale (Pulvers et al., 2004; Yepes, Viswanathan, Bovet, & Maurer, 2015). Participants responded to two questions: (1) “Select the body size that looks most like you?” (perceived body size); (2) “Select the body size that you would like to be” (ideal body size). Body size dissatisfaction was calculated as the difference between the perceived and the ideal silhouettes. Answers were then dichotomized into wanting to be at least one size smaller categorized as “dissatisfied” and not wanting to be smaller categorized as “not-dissatisfied.”
Disordered eating
The Children’s version of the Eating Attitudes Test (ChEAT) (Maloney, McGuire, & Daniels, 1988) is a 26-item scale rated on a scale from 1 (always) to 6 (never) that assesses 4 subscales: dieting, restricting/purging, food preoccupation, and oral control (Smolak & Levine, 1994). Scores are recoded so that higher scores indicate more disordered eating symptoms. This measure has been used to assess disordered eating among African American girls ages 9 and older (DeLeel et al., 2009), with good reliability (Cronbach’s alpha=0.87) (Smolak & Levine, 1994) and has shown adequate reliability among African American girls (alpha = .74) (Vander Wal & Thomas, 2004). For the current study, mean scores on the dieting (Cronbach’s alpha=0.78) and restricting/purging (Cronbach’s alpha=0.72) subscales were examined. Subscale includes questions such as “I have been dieting” and “I think a lot about wanting to be thinner.” The restriction/purging scale is comprised of questions including “I stay away from eating when I am hungry” and “I have the urge to vomit or throw up after eating” and is thought to represent a closely connected cycle of restriction and purging (Smolak & Levine, 1994).
Data Analysis
To test the hypothesis that body dissatisfaction mediates the association between BMI and subsequent disordered eating, a unified path analysis was conducted in Mplus 8.0 (Muthén & Muthén, 2012). BMI z-score at Time 1, body dissatisfaction at Time 2 (controlling for Time 1 body dissatisfaction) and disordered eating symptoms (dieting and restricting/purging subscales) at Time 2 (controlling for baseline rates), were used in the model to ensure temporal sequence. Probit regression was conducted for the outcome of body dissatisfaction and censored-normal linear regression for disordered eating symptoms. Regressions predicting disordered eating at Time 2 included interventions status, and Time 1 disordered eating symptoms as covariates. In regressions predicting body dissatisfaction, intervention and Time 1 body dissatisfaction were included as covariates. The significance of the indirect effect was determined with Sobel’s test (Sobel, 1982). Model fit was assessed with Chi-square test of model fit (p >.05), the root mean square error (RMSEA) and the weighted root mean residual (WRMR). RMSEA values below 0.5 and WRMR values below 0.9 are indicative of good model fit (MacCallum, Browne, & Sugawara, 1996; Muthén & Muthén, 2012). In recognition of the varying racial views of body dissatisfaction (Bucchianeri et al., 2016), only African American girls were included in the current analyses (n = 701). Variance-adjusted weighted least squares (WLSMV) estimation was used for adjustments to the standard errors for non-normality. Finally, 11.8% of data were missing, and missing data imputation was conducted using HotDeck (Myers, 2011). Significance was set at p < 0.05.
Results
Sample Description
Participants were a mean age of 12.15 years at baseline. Sample means are presented in Table 1. On the ChEAT, 38.5% of the sample endorsed fear of being overweight, and 14% endorsed staying away from eating when hungry. Other endorsements included: 3.2% vomit after eating, 6.8% feel very guilty after eating, 6.9% like the stomach to be empty, 3.2% urge to vomit after eating, and 9.4% stay away from foods like bread, potatoes, and rice. MANOVA results revealed that intervention condition was not related to variables of interest (i.e., restricting/purging behaviors, body dissatisfaction, dieting behaviors, BMI z-score) in the current study F(21,1638)=1.23, p=.21.
Table 1.
Sample Characteristics
| Time 1 M (SD)/% |
Time 2 M (SD)/% |
|
|---|---|---|
| Age (years) | 12.15 (0.72) | |
| Body Mass Index z-score | 1.02 (1.03) | |
| Under weight (< 5th%) | 1% | |
| Normal (≥5th% to <85th%) | 47.4% | |
| Overweight (≥85th% to <95th %) | 19.8% | |
| Obese (≥95th% and above) | 31.7% | |
| Dieting Behaviors | 5.42 (5.98) | 6.18 (6.79) |
| Restricting/Purging Behaviors | 1.51 (3.05) | 2.12 (4.22) |
| Body Dissatisfaction (% wants to be smaller) | 60.4% | 58.6% |
Time 1=Baseline
Time 2=Post-intervention follow-up
Initial Correlations
Correlations are presented in Table 2. BMI z-score, body dissatisfaction, dieting behaviors and restricting/purging behaviors were all significantly correlated across both time periods. Age was not significantly related to any variables of interest.
Table 2.
Correlations between the study variables of interest
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | |
|---|---|---|---|---|---|---|---|
| 1. Dieting Behaviors Time 2 | - | ||||||
| 2. Restricting/Purging Behaviors Time 2 | .813** | - | |||||
| 3. Dieting Behaviors Time 1 | .498** | .369** | - | ||||
| 4. Restricting/Purging Behaviors Time 1 | .407** | .415** | .795** | - | |||
| 5. Body Dissatisfaction Time1 1 | .222** | .079 | .323** | .218** | - | ||
| 6. Body Dissatisfaction Time1 2 | .228** | .097* | .226** | .162** | .560** | - | |
| 7. BMI z-score | .235** | .079 | .335** | .244** | .604** | .603** | - |
| 8. Age | .000 | −.030 | −.019 | −.027 | −.020 | −.011 | −.030 |
p <.05,
p <.01
Dummy coded in reference to “satisfied/does not want to be smaller”
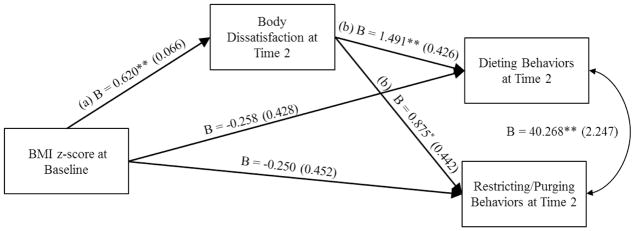
Mediation model
Dieting behaviors
A unified path analytic mediation model was conducted predicting dieting behaviors. The path model provided a good fit for the data χ2(5)= 5.77, p=0.33 (RMSEA=0.015, WRMR=0.506). Individual path estimates are presented in Figure 1. There was a significant association between BMI z-score at baseline and subsequent body dissatisfaction at Time 2 (path a: B=0.620, SE=0.066, p<.001). There was a significant association between body dissatisfaction and dieting behaviors at Time 2 (controlling for baseline dieting) (dieting path b: B=1.491, SE=0.426, p<.001). There was a significant association between body dissatisfaction and restricting/purging behaviors at Time 2 (controlling for baseline restricting/purging) (restricting/purging path b: B=0.875, SE=0.442, p=.048). A test of the indirect effect (a × b) was significant for dieting behaviors (B =0.924, SE=0.280, p=.001), indicating that body dissatisfaction significantly mediated the relation between BMI z-score at Time 1 and subsequent increases in dieting behaviors at Time 2. The indirect effect for restricting/purging was not significant (B =0.543, SE=0.281, p=.053).
Figure 1.
Body dissatisfaction as a mediator of the relationship between BMI z-score and dieting and restricting/purging behaviors. (n = 701)
Note: Unstandardized B weights and (standard errors) are presented along each path.
*p = .048 **p <.01
All Time 2 variables control for baseline estimates
‘a’ and ‘b’ paths are identified by the corresponding lowercase letters in brackets.
Discussion
This study examined body dissatisfaction as a mechanism linking body size (BMI z-score) to subsequent disordered eating behaviors among early adolescent, African American girls. The indirect effect of BMI z-score through body dissatisfaction was supported on subsequent dieting behaviors, but not on subsequent restricting/purging behaviors.
Results concerning dieting are in contrast to research by Epperson et al. (2014) which found that body image mediated the association between body size and dieting for White, but not African American 5th graders. However, a majority of studies concerning disordered eating among school age children (including Epperson et al. (2014)) use cross-sectional data which implies high risk of bias and no consideration of temporal relationships (Larsen, Strandberg-Larsen, Micali, & Andersen, 2015). The current study meets temporal assumptions by utilizing longitudinal data and adjusting for Time 1 variables, thereby strengthening the case for a mediational relation (Maxwell & Cole, 2007).
The lack of support for a mediated relation between BMI and subsequent restricting/purging behavior through body dissatisfaction may be at least partially attributed to the low rate of restricted/purging (3.2), which is less than rates from other samples (Evans, Tovée, Boothroyd, & Drewett, 2013) and to omitted variables in the model, such as negative affect. Stice (Stice, 2001) proposes a dual-pathway model of eating pathology whereby the interaction between body dissatisfaction and negative affect predicts purging symptoms. Future studies should include measures of mood and affect to explore this relationship among African American youth.
A larger body size has been shown to be more acceptable among African American girls, compared to White girls (e.g., Padgett & Biro, 2003). However, the current study finds body dissatisfaction is associated with BMI z-score among African American girls. Furthermore, increase in body dissatisfaction was associated with increases in disordered eating behaviors over 6 months. These findings are in line with recent research showing that BMI is linked with elevated body size dissatisfaction in children across race and ethnicity (Olvera et al., 2015), and may reflect national awareness and campaigns to prevent excess body weight, together with high rates of obesity among African American girls (Ogden et al., 2014; Ogden et al., 2016). Along with increases in overall obesity rates, there has been an increase in extreme obesity (BMI >99th percentile) among African American females (12.7%; Ogden et al., 2016). This change in conjunction with evidence from the current study may suggest that African American girls experience body size dissatisfaction and disordered eating more frequently than previously reported. Recently, Lebow, Sim, and Kransdorf (2015) suggested that adolescents with a history of overweight or obesity represent a substantial portion of treatment-seeking adolescents with restrictive eating disorders. Overweight youth may be at particular risk for disordered eating problems that go untreated due to disbelief from others that they are truly restricting their intake and may even be praised for unhealthy weight loss (Neumark-Sztainer, 2015). Regardless of weight status, sustainable healthy eating and physical activity patterns, should be encouraged and supported, whereas “going on a diet” should be discouraged (Neumark-Sztainer, 2015).
The finding that increases in body dissatisfaction mediate the link between BMI and increases in dieting behaviors among early adolescent girls represents an opportunity to prevent disordered eating by intervening early to build positive body image. This strategy is particularly relevant, given that body dissatisfaction appears to increase with age (Bucchianeri et al., 2013). Positive body image may be a protective factor against disordered eating for African American youth. Sutter, Nishina, and Adams (2015) found that only when African American youth were dissatisfied with their body did their self-worth decrease, regardless of objective weight. Findings from the present study, in conjunction with emerging literature (Bucchianeri et al., 2013; Sutter et al., 2015) highlight the associations between body dissatisfaction and disordered eating, and underscore the importance of addressing body dissatisfaction among all youth, regardless of body size or race/ethnicity. Interventions to address body dissatisfaction have been shown to be effective (Hart, Cornell, Damiano, & Paxton, 2015).
Several limitations should be considered when interpreting results from the current study. The current study examined disordered eating behaviors, not the presence of a formally diagnosed eating disorder. Unhealthy dieting behaviors were self-reported, which may lead to either under or over-reporting of actual behavior. Adolescents may distort the frequency of weight control behaviors symptoms due to the sensitive nature of the questions. However, examination of within-person change and the use of computer-administered questionnaires in a private location ideally minimized this risk. The body dissatisfaction measure used did not allow for the assessment of severity of body dissatisfaction or degree of distress. Body image is a multidimensional construct comprised of cognitive-affective, perceptual, and behavioral domains. Body dissatisfaction reflects the cognitive-affective component of the broader body image construct (Karazsia, Murnen, & Tylka, 2017) including perceived pressure for thinness and thin-ideal internalization (Stice & Shaw, 2002). Future research should utilize multimethod techniques to comprehensively assess the predictors and consequences of body dissatisfaction. Lastly, the current study utilized data from a larger intervention. Although intervention did not focus on weight or body size, and final models adjusted for intervention, it is impossible to preclude the possibility of indirect effects.
Strengths of the current study include the use of objectively measured BMI. Previous work has used self-reported weight (Lebow et al., 2015), which underestimates BMI (Himes, Hannan, Wall, & Neumark-Sztainer, 2005). Additionally, this study used longitudinal data to test a path analysis with a relatively large sample of understudied youth. This approach addresses a call for such path analyses put forth by Goldschmidt and colleagues (Goldschmidt, Aspen, Sinton, Tanofsky-Kraff, & Wilfley, 2008) as well as the call from Padgett (Padgett & Biro, 2003) for longitudinal studies that examine relations between body dissatisfaction and BMI in African American girls.
In light of the current results, practitioners might be encouraged to screen youth for body dissatisfaction which may be an indicator of further negative consequences including disordered eating behaviors. The false notion that African American youth are accepting of excess weight may reduce health care practitioners’ willingness to inquire on such topics, leading to deleterious long-term health consequences (Allen et al., 2016). Given national health objectives to reduce rates of obesity, effective providers and health policy professionals should strive to understand attitudes and behaviors related to body weight, image and healthy lifestyles and intervene with youth for health promotion and behavior change.
Highlights.
Overweight is linked to disordered eating behaviors and body dissatisfaction
African American girls are at high risk for overweight
Body dissatisfaction mediated the relation between weight and disordered dieting
Body dissatisfaction did not mediate the relation between weight and purging behavior
Acknowledgments
We thank the students, caregivers, teachers, and principals, who helped make the Challenge! Program a success.
Footnotes
No reprints requested.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allen D, Belcher HM, Young A, Gibson LW, Colantuoni E, Trent M. BMI, body image, emotional well-being and qeight-control behaviors in urban african american adolescents. International journal of child health and nutrition. 2016;5(3):55–104. [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®) American Psychiatric Pub; 2013. [Google Scholar]
- Austin SB, Spadano-Gasbarro J, Greaney ML, Richmond TK, Feldman HA, Osganian SK, … Peterson KE. Disordered weight control behaviors in early adolescent boys and girls of color: an under-recognized factor in the epidemic of childhood overweight. Journal of Adolescent Health. 2011;48(1):109–112. doi: 10.1016/j.jadohealth.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucchianeri MM, Arikian AJ, Hannan PJ, Eisenberg ME, Neumark-Sztainer D. Body dissatisfaction from adolescence to young adulthood: Findings from a 10-year longitudinal study. Body image. 2013;10(1):1–7. doi: 10.1016/j.bodyim.2012.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucchianeri MM, Fernandes N, Loth K, Hannan PJ, Eisenberg ME, Neumark-Sztainer D. Body dissatisfaction: Do associations with disordered eating and psychological well-being differ across race/ethnicity in adolescent girls and boys? Cultural Diversity and Ethnic Minority Psychology. 2016;22(1):137–146. doi: 10.1037/cdp0000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeLeel ML, Hughes TL, Miller JA, Hipwell A, Theodore LA. Prevalence of eating disturbance and body image dissatisfaction in young girls: An examination of the variance across racial and socioeconomic groups. Psychology in the Schools. 2009;46(8):767–775. doi: 10.1002/pits.20415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epperson AE, Song AV, Wallander JL, Markham C, Cuccaro P, Elliott MN, Schuster MA. Associations among body size, body image perceptions, and weight loss attempts among African American, Latino, and White youth: A test of a mediational model. Journal of pediatric psychology. 2014;39(4):394–404. doi: 10.1093/jpepsy/jst096. [DOI] [PubMed] [Google Scholar]
- Evans EH, Tovée MJ, Boothroyd LG, Drewett RF. Body dissatisfaction and disordered eating attitudes in 7-to 11-year-old girls: Testing a sociocultural model. Body image. 2013;10(1):8–15. doi: 10.1016/j.bodyim.2012.10.001. [DOI] [PubMed] [Google Scholar]
- Ferreiro F, Seoane G, Senra C. Toward understanding the role of body dissatisfaction in the gender differences in depressive symptoms and disordered eating: a longitudinal study during adolescence. Journal of adolescence. 2014;37(1):73–84. doi: 10.1016/j.adolescence.2013.10.013. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Aspen VP, Sinton MM, Tanofsky-Kraff M, Wilfley DE. Disordered eating attitudes and behaviors in overweight youth. Obesity. 2008;16(2):257–264. doi: 10.1038/oby.2007.48. [DOI] [PubMed] [Google Scholar]
- Grabe S, Hyde JS. Ethnicity and body dissatisfaction among women in the United States: a meta-analysis. Psychological bulletin. 2006;132(4):622–640. doi: 10.1037/0033-2909.132.4.622. [DOI] [PubMed] [Google Scholar]
- Hart LM, Cornell C, Damiano SR, Paxton SJ. Parents and prevention: a systematic review of interventions involving parents that aim to prevent body dissatisfaction or eating disorders. International Journal of Eating Disorders. 2015;48(2):157–169. doi: 10.1002/eat.22284. [DOI] [PubMed] [Google Scholar]
- Himes JH, Hannan P, Wall M, Neumark-Sztainer D. Factors associated with errors in self-reports of stature, weight, and body mass index in Minnesota adolescents. Annals of epidemiology. 2005;15(4):272–278. doi: 10.1016/j.annepidem.2004.08.010. [DOI] [PubMed] [Google Scholar]
- Karazsia BT, Murnen SK, Tylka TL. Is body dissatisfaction changing across time? A cross-temporal meta-analysis. Psychological bulletin. 2017;143(3):293. doi: 10.1037/bul0000081. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, Grummer-Strawn LM, Flegal KM, Mei Z, … Johnson CL. 2000 CDC Growth Charts for the United States: methods and development. Vital and health statistics. Series 11, Data from the national health survey. 2002;(246):1–190. [PubMed] [Google Scholar]
- Larsen PS, Strandberg-Larsen K, Micali N, Andersen AMN. Parental and child characteristics related to early-onset disordered eating: A systematic review. Harvard review of psychiatry. 2015;23(6):395–412. doi: 10.1097/HRP.0000000000000073. [DOI] [PubMed] [Google Scholar]
- Lebow J, Sim LA, Kransdorf LN. Prevalence of a history of overweight and obesity in adolescents with restrictive eating disorders. Journal of Adolescent Health. 2015;56(1):19–24. doi: 10.1016/j.jadohealth.2014.06.005. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological methods. 1996;1(2):130. [Google Scholar]
- Maloney MJ, McGuire J, Daniels SR. Reliability testing of a children’s version of the Eating Attitude Test. Journal of the American Academy of Child & Adolescent Psychiatry. 1988;27(5):541–543. doi: 10.1097/00004583-198809000-00004. [DOI] [PubMed] [Google Scholar]
- Mastria MR. Ethnicity and eating disorders. Psychoanalysis & Psychotherapy. 2002;19(1):59–77. [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 2012. [Google Scholar]
- Myers TA. Goodbye, listwise deletion: Presenting hot deck imputation as an easy and effective tool for handling missing data. Communication Methods and Measures. 2011;5(4):297–310. [Google Scholar]
- Neumark-Sztainer D. Higher weight status and restrictive eating disorders: An overlooked concern. The Journal of Adolescent Health. 2015;56(1):1–2. doi: 10.1016/j.jadohealth.2014.10.261. [DOI] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011–2012. Jama. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM. Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. Jama. 2016;315(21):2292–2299. doi: 10.1001/jama.2016.6361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olvera N, McCarley K, Matthews-Ewald MR, Fisher F, Jones M, Flynn EG. Pathways for disordered eating behaviors in minority girls the role of adiposity, peer weight-related teasing, and desire to be thinner. The Journal of Early Adolescence. 2015;36:1–20. [Google Scholar]
- Padgett J, Biro FM. Different shapes in different cultures: body dissatisfaction, overweight, and obesity in African-American and Caucasian females. Journal of pediatric and adolescent gynecology. 2003;16(6):349–354. doi: 10.1016/j.jpag.2003.09.007. [DOI] [PubMed] [Google Scholar]
- Pisetsky EM, May Chao Y, Dierker LC, May AM, Striegel-Moore RH. Disordered eating and substance use in high-school students: Results from the Youth Risk Behavior Surveillance System. International Journal of Eating Disorders. 2008;41(5):464–470. doi: 10.1002/eat.20520. [DOI] [PubMed] [Google Scholar]
- Pulvers KM, Lee RE, Kaur H, Mayo MS, Fitzgibbon ML, Jeffries SK, … Ahluwalia JS. Development of a culturally relevant body image instrument among urban African Americans. Obesity Research. 2004;12(10):1641–1651. doi: 10.1038/oby.2004.204. [DOI] [PubMed] [Google Scholar]
- Russell-Mayhew S, McVey G, Bardick A, Ireland A. Mental health, wellness, and childhood overweight/obesity. Journal of Obesity. 2012;2012:1–9. doi: 10.1155/2012/281801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silberstein L, Striegel-Moore R, Timko C, Rodin J. Behavioural and psychological implications of the thin standard of bodily attractiveness for women. International Journal of Eating Disorders. 1988;5:907–916. [Google Scholar]
- Smolak L, Levine MP. Psychometric properties of the children’s eating attitudes test. International Journal of Eating Disorders. 1994;16(3):275–282. doi: 10.1002/1098-108x(199411)16:3<275::aid-eat2260160308>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Smolak L, Striegel-Moore RH. Challenging the myth of the golden girl: Ethnicity and eating disorders. Washington, DC, US: American Psychological Association; 2001. [Google Scholar]
- Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological methodology. 1982;13(1982):290–312. [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. Journal of abnormal psychology. 2001;110(1):124. doi: 10.1037//0021-843x.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Becker CB, Yokum S. Eating disorder prevention: Current evidence-base and future directions. International Journal of Eating Disorders. 2013;46(5):478–485. doi: 10.1002/eat.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw HE. Role of body dissatisfaction in the onset and maintenance of eating pathology: A synthesis of research findings. Journal of psychosomatic research. 2002;53(5):985–993. doi: 10.1016/s0022-3999(02)00488-9. [DOI] [PubMed] [Google Scholar]
- Sutter C, Nishina A, Adams RE. How you look versus how you feel: Associations between BMI z-score, body dissatisfaction, peer victimization, and self-worth for African American and white adolescents. Journal of adolescence. 2015;43:20–28. doi: 10.1016/j.adolescence.2015.05.002. [DOI] [PubMed] [Google Scholar]
- Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. Journal of consulting and clinical psychology. 2004;72(1):53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vander Wal JS, Thomas N. Predictors of body image dissatisfaction and disturbed eating attitudes and behaviors in African American and Hispanic girls. Eating Behaviors. 2004;5(4):291–301. doi: 10.1016/j.eatbeh.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Witherspoon D, Latta L, Wang Y, Black MM. Do depression, self-esteem, body-esteem, and eating attitudes vary by BMI among African American adolescents? Journal of pediatric psychology. 2013;38(10):1112–1120. doi: 10.1093/jpepsy/jst055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yepes M, Viswanathan B, Bovet P, Maurer J. Validity of silhouette showcards as a measure of body size and obesity in a population in the African region: A practical research tool for general-purpose surveys. Population health metrics. 2015;13(1):1–9. doi: 10.1186/s12963-015-0069-6. [DOI] [PMC free article] [PubMed] [Google Scholar]