SUMMARY
Inflammasome activation is critical for host defense against various microbial infections. Activation of the NLRC4 inflammasome requires detection of flagellin or type III secretion system (T3SS) components by NLR family apoptosis inhibitory proteins (NAIPs); yet how this pathway is regulated is unknown. Here we found that interferon regulatory factor 8 (IRF8) is required for optimal activation of the NLRC4 inflammasome in bone marrow-derived macrophages infected with Salmonella Typhimurium, Burkholderia thailandensis, or Pseudomonas aeruginosa but is dispensable for activation of the canonical and non-canonical NLRP3, AIM2, and Pyrin inflammasomes. IRF8 governs the transcription of Naips to allow detection of flagellin or T3SS proteins to mediate NLRC4 inflammasome activation. Furthermore, we found that IRF8 confers protection against bacterial infection in vivo, owing to its role in inflammasome-dependent cytokine production and pyroptosis. Altogether, our findings suggest that IRF8 is a critical regulator of NAIPs and NLRC4 inflammasome activation for defense against bacterial infection.
Keywords: NLRC4, inflammasome, IRF8, ICSBP, interferon regulatory factor, IRF, ALR, NLR, NAIP, caspase-1, PU.1, SPI1, Burkholderia, Pseudomonas, Salmonella, pathogen, type I interferon, infection, immunity, infectious diseases
Graphical Abstract
Optimal activation of the NLRC4 activation in response to pathogenic bacteria is dependent on the factor IRF8.

INTRODUCTION
Type I interferons (IFNs) are secreted polypeptides that govern a vast array of functions ranging from anti-viral immunity to cancer immunosurveillance. During microbial infection, IFNs are rapidly induced to launch a potent host response primarily achieved by induction of IFN–stimulated genes that mediate pathogen clearance (Ivashkiv and Donlin, 2014; Zitvogel et al., 2015). Multiple intersections exist between type I IFN signaling and inflammasome activation. Inflammasomes are molecular platforms that assemble upon sensing various intracellular stimuli to process caspase-1 into its active form, allowing production of mature IL-1β and IL-18 (Man and Kanneganti, 2015). Caspase-1 activation via the caspase-11–dependent non-canonical NLR family, pyrin domain containing 3 (NLRP3) inflammasome requires type I IFNs (Rathinam et al., 2012). Bone marrow–derived macrophages (BMDMs) from IFN α/β receptor (IFNAR) knockout mice have impaired caspase-11 induction (Rathinam et al., 2012) and processing (Broz et al., 2012) in response to Gram-negative bacteria. Moreover, type I IFNs are required for the activation of the Absent in melanoma 2 (AIM2) inflammasome in response to the facultative intracellular bacteria Francisella (Fernandes-Alnemri et al., 2010; Henry et al., 2007), mediated by IFN regulatory factor 1 (IRF1) (Man et al., 2015). Yet the role of type I IFNs and IRFs in regulating other inflammasomes, including NLR family CARD domain containing 4 (NLRC4) and Pyrin inflammasomes, requires further investigation.
IRFs are a family of transcription factors that were first identified to regulate type I IFNs and type I IFN–induced genes (Tamura et al., 2008). Pioneering studies addressed IRF1 as a regulator for type I IFN production, however, IFN-α and IFN-β levels were normal in IRF1-deficient mouse embryonic fibroblasts following viral infection (Fujita et al., 1989; Matsuyama et al., 1993). IRF3 and IRF7 are now recognized as the major transcription factors for virus-induced type I IFN production (Sato et al., 2000). IRF9 is a component of the transcriptional activator IFN-stimulated gene factor 3 (ISGF3) required for type I IFN signaling (Veals et al., 1992). IRF8, also known as IFN consensus sequence binding protein (ICSBP), participates in IFN induction in a context-dependent manner (Tailor et al., 2007). IRF1 and IRF8 are both basally present in macrophages and inducible by IFNs and LPS (Barber et al., 1995; Driggers et al., 1990; Harada et al., 1989; Lehtonen et al., 1997). They cooperatively promote transcription of genes important for macrophage function such as IL-12 and iNOS (Liu et al., 2004; Masumi et al., 2002; Wang et al., 2000; Xiong et al., 2003). Based on the interaction of these two IRFs (Bovolenta et al., 1994), their importance in cellular immunity, and the requirement of IRF1 for AIM2 inflammasome activation in F. novicida infection, we investigated whether IRF8 has a similar role in inflammasome activation.
The NLRC4 inflammasome relies on NLR family apoptosis inhibitory proteins (NAIPs) for sensing bacterial components in the cytosol (Zhao and Shao, 2015). C57BL/6 mice have multiple Naip genes which encode cytosolic receptors for NLRC4 inflammasome assembly (Zhao and Shao, 2015). Yeast two-hybrid and mouse genetic studies have established a ligand-specific role of NAIP proteins in NLRC4 inflammasome activation. NAIP1 and NAIP2 detect needle and rod proteins of the bacterial type 3 secretion system (T3SS), respectively, whereas NAIP5 and NAIP6 recognize flagellin (Kofoed and Vance, 2011; Rauch et al., 2016; Zhao et al., 2011, 2016). On the other hand, humans have a single NAIP that senses needle and flagellin (Kortmann et al., 2015; Yang et al., 2013). Although the specific ligands for NLRC4 inflammasome have been examined in detail, upstream regulators have remained unexplored.
Here, we discovered a novel role of IRF8 in optimal activation of the NLRC4 inflammasome. Our findings show that IRF8 is a transcriptional regulator of Naips that are prerequisite for NLRC4 inflammasome activation, ultimately contributing to host defense against bacterial pathogens.
RESULTS
IRF8 is dispensable for AIM2, NLRP3, and Pyrin inflammasome activation
The agent responsible for causing tularemia in humans, Francisella tularensis, uses multiple strategies to evade immune surveillance (Jones et al., 2012). Importantly, AIM2 detects the double-stranded DNA of the bacterium following its exposure in cytosol (Fernandes-Alnemri et al., 2010; Jones et al., 2010a). F. tularensis subspecies novicida (F. novicida) induced AIM2 inflammasome–dependent cleavage of pro-caspase-1 (p45) into active caspase-1 (p20) and subsequently produced mature cytokines IL-1β and IL-18, ultimately leading to cell death in unprimed wild-type (WT) BMDMs. Irf8−/− BMDMs were equally capable of cleaving caspase-1 as WT, producing IL-1β and IL-18, and pyroptosis following F. novicida infection, suggesting IRF8 had no role in AIM2 inflammasome activation (Figures 1A–1C and S1A). Because IRF8 is involved in the development of immune cells (Kurotaki and Tamura, 2016), we examined the macrophage markers F4/80 and CD11b. The enrichment of double-positive cell populations in Irf8−/− BMDMs was comparable to that in WT BMDMs, indicative of normal in vitro macrophage differentiation (Figure S2A). Our group previously demonstrated that IRF1 is required to induce GBP2 and GBP5, which mediate killing of F. novicida and liberation of bacterial DNA to induce AIM2 inflammasome activation (Man et al., 2015). In Irf8−/− BMDMs, the protein levels of GBP2 and GBP5 were similar to those of control (Figure S2B). IRF1 is dispensable for cytosolic poly(dA:dT)-mediated AIM2 inflammasome activation (Man et al., 2015). To investigate the requirement of IRF8 in response to poly(dA:dT), we transfected poly(dA:dT) into WT and Irf8−/− BMDMs. Caspase-1 activation, IL-18 levels, and cell death in poly(dA:dT)-transfected BMDMs from WT or Irf8−/− mice were comparable (Figures 1D–1F and S1B). Similarly, we did not observe a significant difference in canonical NLRP3 inflammasome (Figures 1G–1I and S1C) or non-canonical NLRP3 inflammasome activation (Figures 1J–1L and S1D). The levels of inflammasome-independent cytokines (IL-6, TNF, and KC) were largely unaffected by the absence of IRF8 (Figure S1).
Figure 1. IRF8 does not affect the activation of AIM2, NLRP3, or Pyrin inflammasomes.
(A) Immunoblot analysis of pro-caspase-1 (p45) and the cleaved caspase-1 (p20) in WT or mutant BMDMs left untreated/uninfected (Media) or infected with F. novicida (multiplicity of infection [MOI], 100) and collected after 20 h.
(B) Assessment of IL-18 release by enzyme-linked immunosorbent assay (ELISA) following F. novicida infection.
(C) Images of BMDMs under light microscopy after F. novicida infection. The arrows indicate pyroptotic cells.
(D–F) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs after transfection with poly(dA:dT).
(G–I) Immunoblot analysis of caspase-1, IL-18 release, and cell images of LPS-primed BMDMs stimulated with ATP.
(J–L) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs primed with LPS and followed by LPS transfection.
(M–O) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs following treatment of toxin from C. difficle AB+ strain.
Scale bars, 100 μm (C, F, I, L and O), NS, not significant; **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are representative of 3 (A, C, D, F, G, I, J, L, M, and O) or from 3 (B, E, H, K, and N) independent experiments (mean ± SEM).
Pyrin inflammasome activation is triggered by the inactivation of Rho GTPases, which can be caused by bacterial cytotoxins (Xu et al., 2014). Toxin from C. difficile AB+ strain induced Pyrin inflammasome activation that was not mediated by IRF8 (Figures 1M–1O). These results excluded the requirement of IRF8 for AIM2, NLRP3, and Pyrin inflammasome activation.
IRF8 is required for optimal NLRC4 inflammasome activation
The NLRC4 inflammasome is critical for determining the response to bacterial pathogens that have gained access to the cytosol. Salmonella, a Gram-negative bacteria whose primary route of infection in mice and humans is through the gastrointestinal tract, was one of the first microbes identified to activate the NLRC4 inflammasome (Mariathasan et al., 2004). Other bacterial species characterized to engage NLRC4 inflammasome are Pseudomonas aeruginosa, Burkholderia thailandensis, and Legionella pneumophila (Amer et al., 2006; Sutterwala et al., 2007; Zamboni et al., 2006; Zhao et al., 2011). We infected WT BMDMs with Salmonella enterica subspecies enterica serovar Typhimurium (S. Typhimurium), which resulted in robust caspase-1 activation (Figure 2A). Surprisingly, reduced caspase-1 activation was observed in infected Irf8−/− BMDMs (Figure 2A and S2C). IL-18 and IL-1β production was dampened, with fewer pyroptotic cells (Figures 2B, 2C and S3A). Collectively, all features of caspase-1 activation were attenuated in the absence of IRF8 in response to S. Typhimurium infection.
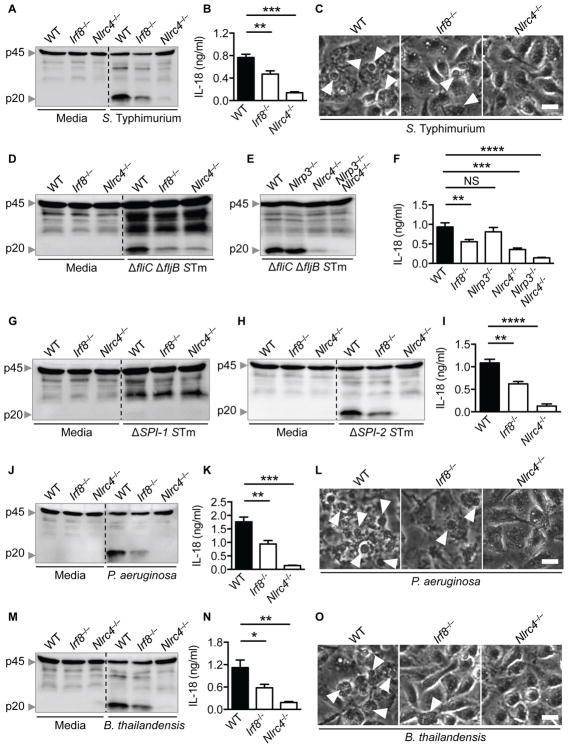
Figure 2. IRF8 is necessary for NLRC4 inflammasome activation induced by bacterial infection.
(A–C) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs that were infected with S. Typhimurium (MOI, 0.1) and collected after 4 h.
(D and E) Immunoblot analysis of caspase-1 in BMDMs that were infected with ΔfliCΔfljB S. Typhimurium (ΔfliCΔfljB) (MOI, 1) and collected after 4 h.
(F) Assessment of IL-18 levels in cell supernatants following ΔfliCΔfljB infection.
(G) Immunoblot analysis of caspase-1 in BMDMs that were infected with ΔSPI-1 S. Typhimurium (ΔSPI-1) (MOI, 1) and collected after 4 h.
(H) Immunoblot analysis of caspase-1 in BMDMs that were infected with ΔSPI-2 S. Typhimurium (ΔSPI-2) (MOI, 1) and collected after 4 h.
(I) Assessment of IL-18 levels in cell supernatants following ΔSPI-2 infection.
(J–L) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs after P. aeruginosa (MOI, 1) infection for 4 h.
(M–O) Immunoblot analysis of caspase-1, IL-18 release, and cell images of BMDMs after B. thailandensis (MOI, 1) infection for 4 h.
Scale bars, 100 μm (C, L and O), NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are representative of 3 (A, C, D, E, G, H, J, L, M, and O) or from 3 (B, F, I, K, and N) independent experiments (mean ± SEM).
Many pathogenic bacteria including Salmonella species harbor flagella and the evolutionarily related T3SS as important virulence mechanisms, which activate the NLRC4 inflammasome. Flagellin monomers form the filamentous flagellum that confers motility. The T3SS is composed of a basal body, connecting rod, and needle that altogether serves as a molecular syringe to inject various effector proteins into the host cytosol, inflicting intracellular perturbations beneficial to the invasion of the bacterium (Crowley et al., 2016; Fàbrega and Vila, 2013; Storek and Monack, 2015). Previous studies have utilized flagellin-mutant S. Typhimurium to delineate the specific role of flagellin in activating the NLRC4 inflammasome (Franchi et al., 2006; Miao et al., 2006). S. Typhimurium lacking flagellin proteins FliC and FljB (ΔfliCΔfljB) was still able to elicit caspase-1 activation and cell death in WT BMDMs that was largely dependent on NLRC4 (Figures 2D, S3B, and S3C). ΔfliCΔfljB can activate the NLRC4 inflammasome alternatively by T3SS (Zhao et al., 2011). Infection with ΔfliCΔfljB in Irf8−/− BMDMs revealed reduced caspase-1 activation and cell death, suggesting that IRF8 is necessary for T3SS-dependent NLRC4 inflammasome activation (Figures 2D, S3B, and S3C). The residual caspase-1 cleavage observed in cells lacking NLRC4 might be due to NLRP3 inflammasome activation (Broz et al., 2010; Man et al., 2014). To address this question, we infected Nlrp3−/−Nlrc4−/− BMDMs with ΔfliCΔfljB, which exhibited defective caspase-1 activation, IL-18 production, and cell death (Figures 2E, 2F, S3B, and S3C). There are two versions of Salmonella T3SS that are encoded separately by Salmonella pathogenicity island-1 (SPI-1) and SPI-2. SPI-1 T3SS is expressed to promote cell invasion in early stages of infection until Salmonella establishes its replicative niche in the phagocytic compartment Salmonella-containing vesicle (SCV), where it downregulates flagellin and SPI-1 T3SS expression and switches to SP1-2 T3SS (Crowley et al., 2016). SPI-1 was critical for inflammasome activation in response to S. Typhimurium because the ΔSPI-1 strain was unable to activate caspase-1 (Figure 2G). In contrast, ΔSPI-2 infection was able to induce NLRC4 inflammasome–mediated caspase-1 activation, IL-18 secretion, and pyroptosis in WT BMDMs, and to a lesser degree, in Irf8−/− BMDMs (Figures 2H, 2I, S3B, and S3C). These results suggest that IRF8 plays a role in NLRC4 inflammasome activation that is dependent on functional SPI-1 T3SS of Salmonella.
We further investigated the contribution of IRF8 to NLRC4 inflammasome activation by infecting BMDMs with other bacteria that engage the NLRC4 inflammasome. P. aeruginosa activated caspase-1 in WT BMDMs, leading to IL-18 and IL-1β secretion and pyroptotic cell death. Indeed, Irf8−/− BMDMs had less caspase-1 activation, IL-18 and IL-1β, and cell death than WT (Figures 2J–2L, S2D, and S3D). Consistently, the extent of NLRC4 inflammasome activity was reduced in Irf8−/− BMDMs after infection with B. thailandensis (Figures 2M–2O, S2E, and S3E). However, there was no defect in inflammasome-independent cytokine production upon these bacterial infections (Figures S3A, S3D, and S3E). IRF8 is constitutively expressed and its expression does not change significantly under conditions that induce expression of a variety of pro-inflammatory cytokines. (Figures S2F). Further supporting our observations, silencing Irf8 in BMDMs resulted in decreased caspase-1 cleavage compared to that of control siRNA-treated BMDMs infected with S. Typhimurium, but not in those infected with F. novicida (Figures S4A and S4B). In addition, caspase-1 activation in Irf8−/− BMDMs infected with S. Typhimurium was less than that of Irf8+/− BMDMs (Figures S4C and S4D). Altogether, our findings highlight the importance of IRF8 to enable recognition of bacterial components during infection for NLRC4 inflammasome activation.
IRF8 is required for expression of murine Naips
NAIPs belong to the NLR family of pattern recognition receptors (PRRs) and contain repeats of the inhibitor of apoptosis (IAP) domain also known as the Baculovirus inhibitor of apoptosis protein repeat (BIR) domain (Jones et al., 2016). Association of each NAIP with its specific bacterial protein drives assembly and activation of the NLRC4 inflammasome. In mice, the corresponding NAIPs and ligands are NAIP1 for the T3SS needle, NAIP2 for the T3SS inner rod, and NAIP5 and NAIP6 for flagellin (Zhao and Shao, 2015). Humans encode a single NAIP that has the highest sequence homology with murine NAIP1 and is able to recognize needle and flagellin (Kortmann et al., 2015; Yang et al., 2013). In our experiments with bacterial infection, we identified the requirement of IRF8 for optimal NLRC4 inflammasome activation (Figure 2). Following these observations, we performed microarray to examine possible differential regulation of innate immune sensors in WT and Irf8−/− BMDMs upon infection with S. Typhimurium. We found reduced expression of genes encoding for NAIP6, NAIP5, NAIP2, and NLRC4; all critical components of the NLRC4 inflammasome complex (Figure 3A).
Figure 3. IRF8 is a key factor in transcriptional regulation of NAIPs.
(A) Microarray analysis of the expression of pattern recognition receptor (PRR)–encoding genes 4 h after infection with S. Typhimurium (MOI, 0.1) in Irf8−/− BMDMs relative to that of WT.
(B) Interaction network visualizing the associations between IRF8, IRF4, SPI1, NLRC4, and NAIPs.
(C) Chromatin immunoprecipitation-sequencing (ChIP-seq) for IRF8 binding in Naip1, Naip2, Naip5, Naip6, and Nlrc4. Peaks indicate regions of DNA bound by IRF8.
(D) Real-time (RT)-PCR analysis of genes encoding NAIPs in BMDMs before (0 h) and after (1 h or 3 h) infection with S. Typhimurium, presented relative to levels of the gene encoding HPRT.
(E) RT-PCR analysis of genes encoding NAIP5 and NAIP6 in BMDMs before (0 h) and after (1 h or 3 h) transfection with 0.5 μg flagellin, presented relative to levels of the gene encoding HPRT.
(F) RT-PCR analysis of genes encoding NLRP3 and NLRC4 in untreated BMDMs, presented relative to levels of the gene encoding HPRT.
(G) ChIP-seq for IRF4 binding in Naip2 and Naip5.
(H) ChIP-seq for SPI1 binding in Naip1, Naip2, Naip5, and Naip6, shown as MACS2 called peaks.
NS, not significant; and **P < 0.01 (two-tailed t test). Data (D–F) are from 3 independent experiments (mean ± SEM).
To find the regulatory interactions involving the NLRC4 inflammasome, we first generated a network of interactions between IRF8 and NAIPs (not shown) where IRF8 physically interacted with IRF4. Interestingly, IRF4 has the greatest sequence homology with IRF8 and requires SPI1 (also known as PU.1) as a binding partner to govern transcriptional programs in the B-cell lineage (Yamagata et al., 1996). Our subsequent generation of an interaction network involving IRF4 and NAIPs revealed the co-expression between IRF8 and SPI1. Moreover, Irf8 was co-expressed with Naip2, Naip5, Naip6, and Nlrc4 but not with Naip1. The selected group of proteins exhibited clique-like properties, with each node being connected to most of the other nodes, suggesting a potential functional interaction (Figure 3B).
To address how NAIPs are being regulated by IRF8, we reanalyzed a published Chromatin immunoprecipitation-sequencing (ChIP-seq) dataset (Olsson et al., 2016). Sequences mapping to the promoter regions of Naip2, Naip5 and Naip6 were enriched, suggesting that their expression can be regulated by IRF8 transcription factor activity. We found no enrichment of sequences mapping to the Naip1 promoter. Although we did not find enrichment in the promoter region of Nlrc4, we identified an IRF8 binding site in the intronic region. Transcription factor binding in the introns have previously been reported to regulate transcription of target genes (Martone et al., 2003; Tokuhiro et al., 2003; Wei et al., 2006). IRF8 binding in the intron might be regulating Nlrc4 expression by increasing chromatin accessibility for other transcription factors (Figure 3C). Real-time PCR (RT-PCR) analysis confirmed that Naip1, Naip2, Naip5, and Naip6 had reduced gene expression in response to S. Typhimurium or flagellin transfection in Irf8−/− BMDMs relative to WT BMDMs (Figures 3D and 3E). Importantly, there was a basal defect in the transcription of all the Naips and Nlrc4, but not for the control gene Nlrp3 (Figures 3D–3F). Collectively, we show that IRF8 likely has binding sites in Naip promoters, contributing to the steady-state expression of Naips. IFN signaling is important for the regulation of IRF8 (Driggers et al., 1990). Therefore it might be possible that the molecules related to IFN production and signaling involve in the regulation of NAIPs. However we found similar gene expression of Naips and Nlrc4 in the BMDMs lacking IRF1, IRF3, IRF7, IRF3 and IRF7, IRF5, IRF9, IFNAR1, IFNAR2, STAT1, TRIF, MAVS, MDA5, cGAS, and STING, suggesting IRF8 specifically regulates Naips independent of IFN signaling (Figure S5). Our interaction map reveals a close network between IRF8, IRF4, and Ets family member SPI1 (Figure 3B). When we analyzed another published ChIP-seq dataset (Iwata et al., 2017), there was no enrichment of IRF4 binding to Naip2 or Naip5 promoters. (Figure 3G). In addition we checked for SPI1 binding sites (Langlais et al., 2016), where we found enrichment of SPI1 binding to Naip1, Naip2, Naip5, and Naip6 loci. This data suggests that SPI1 might work in conjunction with IRF8 for the transcriptional regulation of Naips (Figure 3H).
To validate IRF8 binding to Naip promoters found in the public ChIP analysis, we designed primer sets specific to the IRF8 consensus sequence at −590 and −390 on the promoter regions of Naip2 and Naip5, respectively, to perform targeted ChIP-PCR. The samples immunoprecipitated with IRF8 antibody but not the control IgG antibody yielded amplified PCR products, suggesting the recruitment of IRF8 onto the Naip2 and Naip5 promoters (Figure 4A). Next, to gain further insight into the molecular mechanism of IRF8-mediated transcription of Naips, we cloned the promoters of Naip2 or Naip5 into a luciferase reporter vector. Luciferase expression was significantly upregulated in cells that were co-transfected with IRF8 compared to those transfected with empty vectors, which suggested that IRF8 regulates mRNA abundance of Naip2 and Naip5 at the level of transcription (Figure 4B). Furthermore we sought to confirm the direct recruitment of IRF8 to Naip promoters. To this end, we performed electrophoretic mobility shift assay (EMSA) where we observed IRF8 binding to Naip2 and Naip5 promoters in nuclear extracts from WT BMDMs (Figure 4C). To determine whether the binding was specific to IRF8, we utilized competitive EMSA and antibody-mediated super shift assays. Non-labeled Naip2 or Naip5 oligonucleotides successfully competed with the labeled probes and addition of IRF8 antibody abolished the migration of the IRF8-Naip promoter complex into the membrane (Figure 4C). Together, these results establish that IRF8 directly binds to the promoters of Naip2 and Naip5 to regulate their expression. To further corroborate these findings, we reconstituted IRF8 in Irf8−/− BMDMs. Compared to untreated or control-transfected cells, reconstitution of IRF8 increased the expression of Naip1, Naip2, Naip5, and Naip6. (Figure 4D). All these findings mechanistically prove that IRF8 regulates Naips at the transcriptional level.
Figure 4. Transcriptional activity of IRF8 for Naips.
(A) ChIP for IRF8 followed by semi-quantitative PCR for Naip2 or Naip5 promoters were performed in BMDMs.
(B) Relative reporter luciferase activity for Naip2 or Naip5 promoters in IRF8 overexpressing cells, presented as fold change with respect to empty vector (EV) transfected cells. Data was normalized for transfection efficiency by normalizing firefly luciferase activity with renilla luciferase activity.
(C) Electrophoretic mobility shift assay was performed with Naip2 or Naip5 oligonucleotide probes incubated with nuclear protein extracts (NPE) from BMDMs.
(D) RT-PCR analysis of Naip1, Naip2, Naip5, Naip6, and Irf8 in Irf8−/− BMDMs transfected with control or Irf8 vectors, normalized to levels of Gapdh.
NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (two-tailed t test). Data are representative of 2 (A and C) or from 2 (B and D) independent experiments (mean ± SEM).
Furthermore we examined the role of IRF8 in the NLRC4 inflammasome response to bacterial flagellin and components of the T3SS apparatus. Flagellin treatment alone without the transfection agent DOTAP failed to induce processing of caspase-1. Intracellular delivery of flagellin led to caspase-1 activation in WT BMDMs but activation was greatly impaired in Irf8−/− BMDMs (Figures 5A and S4E). In line with these observations, inflammasome-dependent cytokines IL-18 and IL-1β were reduced whereas KC was unaffected by the absence of IRF8 (Figures 5B, S4F, and S4G). Correspondingly, BMDMs lacking IRF8 were compromised in their ability to undergo pyroptosis after flagellin transfection (Figures 5C and 5D). Because NAIP5 is the receptor for cytosolic flagellin recognition, we checked for inflammasome activation in Naip5−/− BMDMs transfected with flagellin. As expected, caspase-1 maturation and IL-18 production were diminished in cells lacking NAIP5 to a similar extent as seen in cells lacking NLRC4 (Figure S4H and S4I). Irf8−/− BMDMs also had decreased inflammasome activity in response to bacterial T3SS. Transfection of the needle protein PrgI or the rod protein PrgJ into Irf8−/− BMDMs resulted in reduced caspase-1 activation, IL-18 release, and cell death compared to that of WT (Figures 5E–J and S4J). These results demonstrate the significance of IRF8 for sterile NLRC4 inflammasome activation triggered by pure ligands of NAIPs.
Figure 5. NLRC4 inflammasome activation in response to isolated bacterial proteins is impaired in the absence of IRF8.
(A–D) BMDMs were treated with the liposomal agent DOTAP alone, transfected with 0.5 μg flagellin (DOTAP + Flgn), or treated with 0.5 μg flagellin (Flgn) alone.
(A) Immunoblot analysis of caspase-1.
(B) Assessment of IL-18 levels in cell supernatants.
(C) Microscopic analysis.
(D) Cell death was assessed by evaluating the release of lactate dehydrogenase (LDH).
(E–G) Immunoblot analysis of caspase-1, IL-18 release, and cell death in BMDMs transfected with PrgI (DOTAP + PrgI) or treated with PrgI alone.
(H–I) Immunoblot analysis of caspase-1, IL-18 release, and cell death in BMDMs transfected with PrgJ (DOTAP + PrgJ) or treated with PrgJ alone.
Scale bars, 100 μm (C), NS, not significant; *P < 0.05, **P < 0.01 and ***P < 0.001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are representative of 3 (A and C) or 2(E and H) or from 3 (B and D) or 2 (F, G, I, and J) independent experiments (mean ± SEM).
Requirement of IRF8 in host defense against S. Typhimurium and B. thailandensis
NLRC4 inflammasome activation is required for bacterial clearance in S. Typhimurium infected mice (Carvalho et al., 2012). To examine the in vivo relevance of IRF8 we infected mice intraperitoneally with S. Typhimurium and monitored body weight change and mortality during the course of infection. Compared to WT mice, Irf8−/− mice exhibited rapid weight loss between day 1 and day 2 which was similar to the degree of wasting in Nlrc4−/− mice. On the other hand Irf8+/− mice followed the trend of WT mice, showing a gradual decrease in body weight and successive recovery (Figure 6A). All Irf8−/− mice succumbed to infection within 4 days, while during the same time 100% of the Irf8+/− and WT mice were still alive. We continued monitoring until day 12 in which the accumulated mortality of Irf8+/− and WT mice was about 50%. The high susceptibility of Nlrc4−/− mice, as reported (Carvalho et al., 2012), was comparable to that of Irf8−/− mice (Figure 6B). The accelerated mortality of mice lacking IRF8 or NLRC4 highlights the importance of early innate immune responses to contain the pathogen which in turn greatly affects the outcome of the infection. Moreover, Irf8−/− mice were more susceptible to B. thailandensis infection. Within 4 days all Irf8−/− mice died, but more than 50% of WT mice survived (Figure S6A). Interestingly, Naip5−/− mice were more susceptible to S. Typhimurium infection than WT mice but still more resistant than Irf8−/− or Nlrc4−/− mice (Figure 6B). This intermediate phenotype suggests that other NAIPs also contribute to mount NLRC4 inflammasome activation in response to S. Typhimurium infection in vivo.
Figure 6. IRF8 confers protection against S. Typhimurium in vivo.
(A) Body weight of 8-week-old WT (n=13), Irf8−/− (n=7), Irf8+/− (n=6) and Nlrc4−/− (n=9) mice infected intraperitoneally with 103 CFU of S. Typhimurium.
(B) Survival of WT (n=13), Irf8−/− (n=7), Irf8+/− (n=6), Naip5−/− (n=9) and Nlrc4−/− mice (n=9) infected as (A).
(C and D) Bacterial burden in the spleen and liver of WT (n=20), Irf8−/− (n=15), Nlrc4−/− (n=15) and Naip5−/−(n=9) mice on day 3 after infection as (A).
(E and F) Analysis of IL-18 in the spleen and liver collected from WT (n=10), Irf8−/− (n=6), Nlrc4−/− (n=10) and Naip5−/− (n=6) mice on day 3 after infection as (A).
(G–L) RT-PCR analysis of genes encoding NAIPs, NLRC4, and IRF8 in the spleen collected from WT and Irf8−/− mice before infection (day 0) and after infection (day 3) as (A), presented relative to that of the gene encoding HPRT.
NS, not significant; *P < 0.05, ***P < 0.0001 and ****P < 0.0001 (log-rank test [B], ANOVA with Dunn’s multiple comparisons test [C–F], or Two-way ANOVA with Tukey’s multiple comparisons test [G–L]). Data are from 2 experiments.
The bacterial burden in the spleen and liver of Irf8−/− or Nlrc4−/− mice, but not Naip5−/− mice was greater than that of WT mice upon S. Typhimurium infection (Figures 6C and 6D). Similarly, Irf8−/− mice had increased bacterial burden in the lung, liver, and spleen after B. thailandensis infection compared to WT mice (Figure S6B). IL-18 levels in the spleen, liver, and serum of these mice were also assessed 3 days after S. Typhimurium infection, or 2 days after B. thailandensis infection. Less IL-18 was detected in the tissues and serum of Irf8−/− mice than in those of WT, reflecting defective inflammasome activation in response to infection in Irf8−/− mice (Figures 6E, 6F, and S6C). Furthermore we investigated the numbers of circulating blood cells from the peripheral blood of infected WT and Irf8−/− mice using an automated hematology analyzer. Relative to WT mice, Irf8−/− mice exhibited higher numbers of total white blood cells (WBCs), neutrophils, and lymphocytes 3 days after S. Typhimurium infection, whereas no significant differences were noted in the numbers of total monocytes, eosinophils, basophils, red blood cells (RBCs), or platelets (Figure S7A). Similarly, we found more circulating WBCs and neutrophils in Irf8−/− mice 2 days after B. thailandensis infection, suggesting that the susceptibility of IRF8-deficient mice to infection was not due to impaired immune cell production and circulation (Figure S7B). However, we observed more prominent recruitment of immune cells, which were largely composed of neutrophils, in the lungs of B. thailandensis infected WT mice than in the lungs of Irf8−/− mice (Figure S6D). This may be due to the decreased production of inflammasome dependent cytokines in IRF8-deficient mice.
The main effectors of inflammasome activation are the cytokines IL-1 and IL-18, and the recently identified pore-forming molecule gasdermin D (Kayagaki et al., 2015; Liu et al., 2016; Shi et al., 2015). We used the above S. Typhimurium infection model to further access the relative contribution of cytokine production and pyroptosis in host defense. The body weight of Il18−/−Il1r−/−, Gsdmd−/−, and Casp1−/− mice dropped significantly during the first few days of infection compared to WT mice (Figure 7A). In 4 days, all mice from the three knock-out genotypes succumbed to infection, without showing any significant difference between the groups (Figure 7B). In comparison to WT mice, the bacterial loads of Gsdmd−/− mice and Il18−/−Il1r−/−mice were greater, supporting the idea that inflammasome-dependent cytokines and cell death were both critical in mediating host defense against S. Typhimurium infection (Figure 7C).
Figure 7. Inflammasome-dependent cytokines and pyroptosis both contribute to protection against S. Typhimurium infection in vivo.
(A) Body weight of 8-week-old WT (n=13), Il18−/−Il1r−/− (n=4), Gsdmd−/− (n=9), Casp1−/− (n=7), and Irf8−/− (n=8) mice infected intraperitoneally with 103 CFU of S. Typhimurium.
(B) Survival of WT (n=13), Il18−/−Il1r−/− (n=4), Gsdmd−/− (n=9), Casp1−/− (n=7), and Irf8−/− (n=8) mice infected as (A).
(C) Bacterial burden in tissues. For spleen, WT (n=10), Il18−/−Il1r−/− (n=11), Gsdmd−/− (n=11), Casp1−/− (n=8), and Irf8−/− (n=7) mice; for liver, WT (n=10), Il18−/−Il1r−/− (n=12), Gsdmd−/− (n=11), Casp1−/− (n=7), and Irf8−/− (n=7) mice on day 3 after infection as (A).
NS, not significant; **P < 0.001 and ***P < 0.0001 (log-rank test [B] or ANOVA with Dunn’s multiple comparisons test [C]). Data are from 1 experiment.
Next, we examined Naip gene expression patterns in the spleen of WT and Irf8−/− mice before and after infection with S. Typhimurium. Irf8−/− mice had basally lower expression of Naip1, Naip5, Naip6, Nlrc4, but not Naip2 than WT mice (Figures 6G–6K). In WT mice we observed significant reduction in the gene expression of Naip1 and Naip5 after infection, which might be due to reduction in the levels of Irf8 (Figures 6G, 6I, and 6L). After infection, Naip1 and Naip6 gene expression remained lower in Irf8−/− mice compared to that of WT mice (Figures 6G and 6J). Similarly, we observed lower gene expression of Naip1, Naip5, and Naip6 in the spleen of Irf8−/− mice compared to those of WT mice after B. thailandensis infection (Figures S6E and S6G). However, in the lungs we observed decreased expression of Naip2 along with other Naips and Nlrc4 before and after B. thailandensis infection (Figures S6F and S6H). Thus, in the absence of IRF8, infected mice were not able to promote sufficient inflammasome activation due to the lack of Naips expression. These data display an important role for IRF8 in regulating the NLRC4-dependent clearance of S. Typhimurium and B. thailandensis.
DISCUSSION
We identified the novel role of IRF8 as an upstream regulator of NAIPs, ultimately contributing to NLRC4 inflammasome activity. Transcription of NAIPs was dependent on IRF8, but there was no significant induction of Naips in vitro and in vivo in response to infection. The residual expression of Naips and NLRC4 inflammasome activity in the absence of IRF8 imply that other factors may also contribute to the transcription of NAIPs. IRF8 is known to be recruited with other transcription factors owing to its weak DNA-binding activity. IRF, AP-1, and Ets family transcription factors interact with IRF8 to bind to specific composite elements allowing combinatorial control over numerous genes (Bovolenta et al., 1994; Eklund et al., 1998; Glasmacher et al., 2012). In our network analysis IRF8 is co-expressed with IRF4 and SPI1. ChIP-Seq analysis indicated that SPI1 but not IRF4 binds to the promoter regions of Naips. Therefore, it is also possible that SPI1 could function with IRF8 to regulate Naips expression and NLRC4 inflammasome activation. Whether IRF8 and SPI1 share common binding sites for Naips needs to be explored.
Due to the existence of compensatory mechanisms to combat infections, it is difficult to access the sole contribution of inflammasome activity. Nevertheless, the expulsion of bacteria-containing intestinal epithelial cells from S. Typhimurium-challenged mice well displays how the inflammasome promotes bacterial clearance. Mice lacking Nlrc4 or Naips have increased bacterial load locally and systemically (Sellin et al., 2014). Moreover IL-1 and IL-18, and gasdermin D mediated cell death directed by inflammasome activation were both important for host protection. Our in vivo data provide a striking example of how optimal NAIP/NLRC4 inflammasome activity, conferred by IRF8, is crucial for host survival. In addition to the regulation of inflammasome activation shown here, IRF8 also plays a critical role in development of cDC1s and pDCs (Sichien et al., 2016), which might also have contributed to the increased susceptibility of Irf8−/− mice to Salmonella and Burkholderia infections.
There was reduction of Naip2 in the lungs but not the spleen of mice lacking IRF8, implying that additional regulatory or compensatory mechanisms may exist to modulate Naip2 expression independently of IRF8 in certain cell types. Moreover the relative expression of Naips varies among different cell types (Yang et al., 2013). In addition, bacteria produce different amounts of single or multiple NAIP ligands of varying affinity. Because of this combination of host factors and pathogen factors, the degree of NLRC4 inflammasome activation in vivo is complex (Zhao and Shao, 2015). Altogether, our work on IRF8 provides new insights into the regulation of the NAIP/NLRC4 inflammasome. The relationship among IRFs, the IFN signaling pathway, and inflammasomes remains to be further explored.
STAR★METHODS
KEY RESOURCES TABLE
The table highlights the genetically modified organisms and strains, cell lines, reagents, software, and source data essential to reproduce results presented in the manuscript. Depending on the nature of the study, this may include standard laboratory materials (i.e., food chow for metabolism studies), but the Table is not meant to be comprehensive list of all materials and resources used (e.g., essential chemicals such as SDS, sucrose, or standard culture media don’t need to be listed in the Table). Items in the Table must also be reported in the Method Details section within the context of their use. The number of primers and RNA sequences that may be listed in the Table is restricted to no more than ten each. If there are more than ten primers or RNA sequences to report, please provide this information as a supplementary document and reference this file (e.g., See Table S1 for XX) in the Key Resources Table.
Please note that ALL references cited in the Key Resources Table must be included in the References list. Please report the information as follows:
REAGENT or RESOURCE: Provide full descriptive name of the item so that it can be identified and linked with its description in the manuscript (e.g., provide version number for software, host source for antibody, strain name). In the Experimental Models section, please include all models used in the paper and describe each line/strain as: model organism: name used for strain/line in paper: genotype. (i.e., Mouse: OXTRfl/fl: B6.129(SJL)-Oxtrtm1.1Wsy/J). In the Biological Samples section, please list all samples obtained from commercial sources or biological repositories. Please note that software mentioned in the Methods Details or Data and Software Availability section needs to be also included in the table. See the sample Table at the end of this document for examples of how to report reagents.
SOURCE: Report the company, manufacturer, or individual that provided the item or where the item can obtained (e.g., stock center or repository). For materials distributed by Addgene, please cite the article describing the plasmid and include “Addgene” as part of the identifier. If an item is from another lab, please include the name of the principal investigator and a citation if it has been previously published. If the material is being reported for the first time in the current paper, please indicate as “this paper.” For software, please provide the company name if it is commercially available or cite the paper in which it has been initially described.
-
IDENTIFIER: Include catalog numbers (entered in the column as “Cat#” followed by the number, e.g., Cat#3879S). Where available, please include unique entities such as RRIDs, Model Organism Database numbers, accession numbers, and PDB or CAS IDs. For antibodies, if applicable and available, please also include the lot number or clone identity. For software or data resources, please include the URL where the resource can be downloaded. Please ensure accuracy of the identifiers, as they are essential for generation of hyperlinks to external sources when available. Please see the Elsevier list of Data Repositories with automated bidirectional linking for details. When listing more than one identifier for the same item, use semicolons to separate them (e.g. Cat#3879S; RRID: AB_2255011). If an identifier is not available, please enter “N/A” in the column.
A NOTE ABOUT RRIDs: We highly recommend using RRIDs as the identifier (in particular for antibodies and organisms, but also for software tools and databases). For more details on how to obtain or generate an RRID for existing or newly generated resources, please visit the RII or search for RRIDs.
Please use the empty table that follows to organize the information in the sections defined by the subheading, skipping sections not relevant to your study. Please do not add subheadings. To add a row, place the cursor at the end of the row above where you would like to add the row, just outside the right border of the table. Then press the ENTER key to add the row. Please delete empty rows. Each entry must be on a separate row; do not list multiple items in a single table cell. Please see the sample table at the end of this document for examples of how reagents should be cited.
KEY RESOURCES TABLE.
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| Mouse monoclonal anti-caspase-1 | Adipogen | Cat#AG-20B-0042; RRID: AB_2490248 |
| Goat polyclonal anti-IRF8 | Santa Cruz Biotechnology | Cat#sc-6058; RRID:AB_649510 |
| Rabbit polyclonal anti-GBP2 | Proteintech | Cat#11854-1-AP; RRID: AB_2109336 |
| Rabbit polyclonal anti-GBP5 | Proteintech | Cat#13220-1-AP; RRID: AB_2109348 |
| Mouse monoclonal anti-β-actin | Proteintech | Cat#66009-1-Ig; RRID:AB_2687938 |
| HRP–conjugated anti-rabbit | Jackson Immuno Research Laboratories | Cat#111-035-047; RRID:AB_2337940 |
| HRP–conjugated anti-mouse | Jackson Immuno | Cat#315-035-047; |
| Research Laboratories | RRID:AB_2340068 | |
| HRP–conjugated anti-goat | Jackson Immuno | Cat#705-035-003; |
| Research Laboratories | RRID:AB_2340390 | |
| Rat monoclonal anti-CD11b | Affymetrix eBioscience | Cat#48-0112-82; RRID: AB_1582236 |
| Rat monoclonal anti-F4/80 | BioLegend | Cat#123109; RRID: AB_893498 |
| Rabbit monoclonal anti-IRF8 | Cell Signaling Technology | Cat#5628 RRID:AB_10828231 |
| Normal rabbit IgG | Cell Signaling Technology | Cat#2729 RRID:AB_1031062 |
| Bacterial and Virus Strains | ||
| Francisella novicida strain U112 | (Man et al., 2015) | N/A |
| Salmonella Typhimurium SL1344 | (Man et al., 2015) | N/A |
| Salmonella Typhimurium SL1344 ΔfliCΔfljB | (Man et al., 2015) | N/A |
| Salmonella Typhimurium SL1344 ΔSPI-1 | (Man et al., 2015) | N/A |
| Salmonella Typhimurium SL1344 ΔSPI-2 | (Broz et al., 2010) | N/A |
| Burkholderia thailandensis strain E264 | Dr. Joseph Mougous (Schwarz et al., 2010) | N/A |
| Pseudomonas aeruginosa strain PAO1 | Dr. Joseph Mougous (Hood et al., 2010) | N/A |
| Biological Samples | ||
| Chemicals, Peptides, and Recombinant Proteins | ||
| DMEM | ThermoFisher Scientific | Cat#11995-073 |
| MEM Non-Essential Amino Acids Solution | ThermoFisher Scientific | Cat#11140-050 |
| Fetal Bovine Serum | Biowest | Cat#S1620 |
| Penicillin and Streptomycin | ThermoFisher Scientific | Cat#15070-063 |
| BBL Trypticase Soy Broth | BD Biosciences | Cat#211768 |
| L-cysteine | ThermoFisher Scientific | Cat#BP376-100 |
| Luria-Bertani media | MP Biomedicals | Cat#3002-031 |
| BBL Trypticase Soy Broth | BD Biosciences | Cat#211768 |
| BBL brain heart infusion agar | BD Biosciences | Cat#211065 |
| PBS | ThermoFisher Scientific | Cat#14190-250 |
| Gentamicin | ThermoFisher Scientific | Cat#15750-060 |
| Ultrapure LPS from Salmonella minnesota R595 | InvivoGen | Cat#tlrl-smlps |
| ATP | Roche | Cat#10127531001 |
| Poly(dA:dT) | InvivoGen | Cat#tlrl-patn |
| Opti-MEM | ThermoFisher Scientific | Cat#31985-070 |
| Ultrapure flagellin from S. Typhimurium | InvivoGen | Cat#tlrl-epstfla-5 |
| Recombinant S. Typhimurium PrgI | Mybiosource | Cat#MBS1177087 |
| Recombinant S. Typhimurium PrgJ | Mybiosource | Cat#MBS2061410 |
| DOTAP Liposomal Transfection Reagent | Roche | Cat#11202375001 |
| Luminata Forte Western HRP Substrate | Millipore | Cat#WBLUF0500 |
| TRIzol | ThermoFisher Scientific | Cat#15596026 |
| SYBR Green | Applied Biosystems | Cat#4368706 |
| GenMute siRNA Transfection Reagent | SignaGen Laboratories | Cat#SL100568 |
| Protease inhibitor | Roche | Cat#11697498001 |
| Phosphatase inhibitor | Roche | Cat#04906837001 |
| FuGENE HD Transfection Reagent | Promega | Cat#E2311 |
| Neon Transfection System Kit | ThermoFisher Scientific | Cat#MPK10025 |
| Critical Commercial Assays | ||
| Xfect transfection kit | Clontech Laboratories, Inc | Cat#631318 |
| CytoTox 96 Non-Radioactive Cytotoxicity Assay | Promega | Cat#G1780 |
| High capacity cDNA Reverse Transcription kit | Applied Biosystems | Cat#4368814 |
| Ambion Wild-Type Expression kit | ThermoFisher Scientific | Cat# 4411973 |
| Affymetrix GeneChip Mouse Gene 2.0 ST Array | ThermoFisher Scientific | Cat#902119 |
| Multiplex ELISA kit | Millipore | Cat#MCYTOMAG-70K |
| IL-18 ELISA kit | Invitrogen | Cat#BMS618-3 |
| Light Shift Chemiluminescent EMSA kit | ThermoFisher Scientific | Cat#20148 |
| Dual-Luciferase Reporter Assay System | Promega | Cat#E1910 |
| Deposited Data | ||
| Microarray raw data | This paper | GEO: GSE110452 |
| Experimental Models: Cell Lines | ||
| HEK293T | ATCC#3216 | Cat# CRL-3216; RRID:CVCL_0063 |
| Experimental Models: Organisms/Strains | ||
| Irf8−/− mice | Jackson Laboratory | RRID:IMSR_JAX:018298 |
| Irf1−/− mice | (Matsuyama et al., 1993) | N/A |
| Nlrp3−/− mice | (Kanneganti et al., 2006) | N/A |
| Nlrc4−/− mice | (Franchi et al., 2006) | N/A |
| Nlrp3−/−Nlrc4−/− mice | This paper (Mice crossed in our facility) | N/A |
| Aim2−/− mice | (Jones et al., 2010) | N/A |
| Pyrin−/− mice | (Gorp et al., 2016) | N/A |
| Naip5−/− mice | Dr. Russell Vance (Lightfield et al., 2008) | N/A |
| Il18−/−Il1r−/− mice | (Glaccum et al., 1997; Takeda et al., 1998) (Mice crossed in our facility) | N/A |
| Gsdmd−/− mice | This paper (Generated in our facility) | N/A |
| Casp1−/− mice | (Man et al., 2017) | N/A |
| Casp11−/− mice | (Kayagaki et al., 2011) | N/A |
| Irf3−/− mice | (Sato et al., 2000) | N/A |
| Irf7−/− mice | (Honda et al., 2005) | N/A |
| Irf3−/− Irf7−/− mice | This paper (Mice crossed in our facility) | N/A |
| Irf9−/− mice | (Kimura et al., 1996) | N/A |
| Ifnar1−/− mice | (Müller et al., 1994) | N/A |
| Ifnar2−/− mice | (Fenner et al., 2006) | N/A |
| Stat1−/− mice | (Matsuyama et al., 1993) | N/A |
| Trif−/− mice | (Yamamoto et al., 2003) | N/A |
| Mavs1−/− mice | Dr. Michael Gale (Suthar et al., 2012) | N/A |
| Ifih1−/− (Mda5−/−) mice | (Kato et al., 2006) | N/A |
| Mb21d1−/− (Cgas−/−) mice | (Schoggins et al., 2014) | N/A |
| Tmem173−/− (Stinggt/gt) mice | (Sauer et al., 2011) | N/A |
| Oligonucleotides | ||
| siGENOME SMARTpool siRNA specific for the gene encoding mouse Irf8 | Dharmacon | Cat#M-040737-00 |
| RT-PCR Naip1 Forward: 5′ - TGCCCAGTATATCCAAGGCTA-3′ | This paper | N/A |
| RT-PCR Naip1 Reverse: 5′ - AGACGCTGTCGTTGCAGTAAG-3′ | This paper | N/A |
| RT-PCR Naip2 Forward: 5′ - TTTTGTGAATCCCTGGGTCA-3′ | This paper | N/A |
| RT-PCR Naip2 Reverse: 5′ - TGTAGAAAAGGCCTGCTTTGA-3′ | This paper | N/A |
| RT-PCR Naip5 Forward: 5′ - AAGGAGATGACCCCTGGAAG-3′ | This paper | N/A |
| RT-PCR Naip5 Reverse: 5′ - TGACCCAGGACTTCACAAAA-3′ | This paper | N/A |
| RT-PCR Naip6 Forward: 5′ - TTTTGTGAAGTCCTGGGTCAG-3′ | This paper | N/A |
| RT-PCR Naip6 Reverse: 5′ - CAATGTCCTTTTTGCCAGTG-3′ | This paper | N/A |
| RT-PCR Nlrc4 Forward: 5′ - CAGGTGGTCTGATTGACAGC-3′ | This paper | N/A |
| RT-PCR Nlrc4 Reverse: 5′ - CCCCAATGTCAGACAAATGA-3′ | This paper | N/A |
| RT-PCR Irf8 Forward: 5′ - GATCGAACAGATCGACAGCA-3′ | This paper | N/A |
| RT-PCR Irf8 Reverse: 5′ - GCTGGTTCAGCTTTGTCTCC-3′ | This paper | N/A |
| RT-PCR Nlrp3 Forward: 5′ - TGCAGAAGACTGACGTCTCC-3′ | This paper | N/A |
| RT-PCR Nlrp3 Reverse: 5′ - CGTACAGGCAGTAGAACAGTTC-3′ | This paper | N/A |
| RT-PCR Gapdh Forward: 5′ - CGTCCCGTAGACAAAATGGT-3′ | This paper | N/A |
| RT-PCR Gapdh Reverse: 5′ - TTGATGGCAACAATCTCCAC-3′ | This paper | N/A |
| RT-PCR Hprt Forward: 5′ - CTCATGGACTGATTATGGACAGGAC-3′ | This paper | N/A |
| RT-PCR Hprt Reverse: 5′ - GCAGGTCAGCAAAGAACTTATAGCC-3′ | This paper | N/A |
| ChIP-PCR Naip2 Forward: 5′ - TTTCAACCTTACTACACTTTCAATCAAATAGAA-3′ | This paper | N/A |
| ChIP-PCR Naip2 Reverse: 5′ - ATAGATAGATAGATATGGATATATAACC-3′ | This paper | N/A |
| ChIP-PCR Naip5 Forward: 5′ - AGTGCTGACACATTTGATGCCACCAATGCA-3′ | This paper | N/A |
| ChIP-PCR Naip5 Reverse: 5′ - GCCCCCTTGCTGCTGATGCTCTGTGACCAG-3′ | This paper | N/A |
| Recombinant DNA | ||
| pGL4.17[luc2/Neo] Vector | Promega | Cat#E6721 |
| pRL-TK-Renilla | Promega | Cat#E2241 |
| pCMV6-mIRF8 | Origene | Cat#MR206748 |
| pcDNA3.1 | Invitrogen | Cat#V79020 |
| Software and Algorithms | ||
| GraphPad Prism 6.0 | GraphPad Software, Inc. | http://www.graphpad.com |
| FlowJo software | FlowJo, LLC and Illumina, Inc | http://www.flowjo.com/ |
| Partek Genomics Suite version 6.6 | Partek | http://www.partek.com |
| Ingenuity Pathways Analysis software | Qiagen | https://www.qiagenbioinformatics.com/ |
| Cytoscape | (Shannon et al., 2003) | http://www.cytoscape.org/ |
| GeneMANIA Cytoscape plugin | (Mostafavi et al., 2008) | http://genemania.org/plugin |
| Gene Expression Omnibus (GEO) | (Edgar et al., 2002) | https://www.ncbi.nlm.nih.gov/geo/ |
| MACS2 | (Zhang et al., 2008) | |
| Tuxedo | (Trapnell et al., 2012) | |
| Integrative Genomics Viewer (IGV) | (Robinson et al., 2011) | http://software.broadinstitute.org/software/igv/ |
| DAVID bioinformatics database 50 | (Huang et al., 2009) | https://david.ncifcrf.gov/home.jsp |
| Other | ||
| PVDF Membrane | Millipore | Cat#IPVH00010 |
| Biodyne Nylon Membrane | ThermoFisher Scientific | Cat#77016 |
CONTACT FOR REAGENT AND RESOURCE SHARING
Further information and requests for reagents may be directed to, and will be fulfilled by the lead contact Thirumala-Devi Kanneganti (thirumala-devi.kanneganti@stjude.org).
EXPERIMENTAL MODELS AND SUBJECT DETAILS
Mice
Irf8−/− mice (Jackson Laboratory, 018298), Irf1−/− mice (Matsuyama et al., 1993), Nlrp3−/− mice (Kanneganti et al., 2006), Nlrc4−/− mice (Franchi et al., 2006), Nlrp3−/−Nlrc4−/− mice (generated by crossing Nlrp3−/− and Nlrc4−/− mice in our facility), Aim2−/− mice (Jones et al., 2010b), Pyrin−/− mice (Gorp et al., 2016), and Naip5−/− mice (kindly provided by Dr. R. Vance), Il18−/−Il1r−/− mice (generated by crossing Il18−/− and Il1r −/− mice in our facility), Gsdmd−/− mice (generated in our facility), Casp1−/− mice (Man et al., 2017), Casp11−/− mice (Kayagaki et al., 2011), Irf3−/− mice (Sato et al., 2000), Irf7−/− mice (Honda et al., 2005), Irf3−/− Irf7−/− mice (generated by crossing Irf3−/− and Irf7 −/− mice in our facility), Irf9−/− mice (Kimura et al., 1996), Ifnar1−/− mice (Müller et al., 1994), Ifnar2−/− mice (Fenner et al., 2006), Stat1−/− mice (Matsuyama et al., 1993), Trif−/− mice (Yamamoto et al., 2003), Mavs1−/− mice (Suthar et al., 2012), Ifih1−/− (Mda5−/−) mice (Kato et al., 2006), Mb21d1−/− (Cgas−/−) mice (Schoggins et al., 2014), and Tmem173−/− (Stinggt/gt) mice (Sauer et al., 2011) have been described. All mice were bred at St. Jude Children’s Research Hospital. Animal studies were conducted under protocols approved by St. Jude Children’s Research Hospital’s committee on the use and care of animals.
Bone Marrow-Derived Macrophages
Primary BMDMs were grown for 6 days in DMEM (ThermoFisher Scientific, 11995-073) supplemented with 1% non-essential amino acids (ThermoFisher Scientific, 11140-050), 10% FBS (Biowest, S1620), 30% medium conditioned by L929 mouse fibroblasts, and 1% penicillin and streptomycin (ThermoFisher Scientific, 15070-063). BMDMs in antibiotic-free medium were seeded onto 12-well plates at a density of 1 × 106 cells per well, followed by incubation overnight.
Bacterial Culture
F. novicida strain U112 was grown overnight under aerobic conditions at 37°C in BBL Trypticase Soy Broth (BD Biosciences, 211768) supplemented with 0.2% L-cysteine (ThermoFisher Scientific, BP376-100). Bacteria were subcultured (1:10) for 4 h at 37°C in fresh Trypticase Soy Broth supplemented with 0.2% L-cysteine and resuspended in PBS (ThermoFisher Scientific, 14190-250). Salmonella Typhimurium strain SL1344, isogenic mutants lacking SPI-1 (ΔSPI-1), isogenic mutants lacking SPI-2 (ΔSPI-2), isogenic mutants lacking fliC and fljB (ΔfliCΔfljB), Burkholderia thailandensis strain E264 (a gift from Dr. Joseph Mougous), and Pseudomonas aeruginosa strain PAO1 (a gift from Dr. Joseph Mougous) were inoculated into Luria-Bertani (LB) broth (MP Biomedicals, 3002-031) and incubated overnight under aerobic conditions at 37°C. S. Typhimurium SL1344, all isogenic mutants of S. Typhimurium SL1344, B. thailandensis strain E264, and P. aeruginosa strain PAO1 were subcultured (1:10) for 3 h at 37°C in fresh LB broth to generate bacteria grown to log phase. C. difficile strain r20291 AB− and AB+ strains were provided by Dr. N. Minton (Kuehne et al., 2014). Strains were streaked onto brain heart infusion agar (BD Biosciences, 211065) and incubated overnight at 37°C in an anaer obic chamber. Single colonies were inoculated into tryptone-yeast extract medium and grown overnight at 37°C anaerobically. C. difficile cultures for cell stimulation were prepared by collecting supernatant via centrifugation followed by sterilization through a 0.2 μm filter.
METHODS DETAILS
Stimulation of Bone Marrow–Derived Macrophages
For activation of the canonical NLRP3 inflammasome, BMDMs were primed for 4 h with 100 ng/mL ultrapure LPS from Salmonella minnesota R595 (InvivoGen, tlrl-smlps) and were stimulated for 45 min with 5 mM ATP (Roche, 10127531001). For transfection of DNA, each reaction consisted of 2 μg of poly(dA:dT) (InvivoGen, tlrl-patn) resuspended in PBS and mixed with 0.6 μL of Xfect polymer in Xfect reaction buffer (Clontech Laboratories, Inc, 631318). After 10 min, DNA complexes were added to BMDMs in Opti-MEM (ThermoFisher Scientific, 31985-070), followed by incubation for 5 h. For IRF8 expression, BMDMs were stimulated with 100 ng/mL ultrapure LPS for indicated times. For bacterial protein transfection, 0.1 μg, 0.5 μg, or 1 μg of ultrapure flagellin from Salmonella Typhimurium (InvivoGen, tlrl-epstfla-5); 1 μg of recombinant Salmonella Typhimurium PrgI (Mybiosource, MBS1177087); and 1 μg of recombinant Salmonella Typhimurium PrgJ (Mybiosource, MBS2061410) were resuspended in PBS and mixed with 20 μL of DOTAP (Roche, 11202375001) per reaction. The reaction mixture was incubated for 1 h and added to BMDMs in 500 μL Opti-MEM.
For bacterial infection, the following conditions were used: F. novicida at an MOI of 100 for 20 h of incubation (for activation of caspase-1) and an MOI of 50 for 2, 8, 16, or 24 h of incubation (for expression of IRF8, GBP2, and GBP5); S. Typhimurium at an MOI of 0.01, 0.1, or 1 for 4 h of incubation (for activation of caspase-1) and an MOI of 0.01 for indicated times (for expression of IRF8); ΔSPI-1 at an MOI of 1 for 4 h of incubation; ΔSPI-2 at an MOI of 1 for 4 h of incubation; ΔfliCΔfljB at an MOI of 1 for 4 h of incubation; B. thailandensis at an MOI of 0.5, 1, or 5 for 4 h of incubation (for activation of caspase-1) and an MOI of 1 for indicated times (for expression of IRF8); and P. aeruginosa at an MOI of 0.5, 1, or 5 for 4 h of incubation. 50 μg/ml gentamicin (ThermoFisher Scientific, 15750-060) was added after 8 h (F. novicida) post-infection to kill extracellular bacteria. Cell culture supernatants were collected for enzyme-linked immunosorbent assays (ELISAs). Levels of lactate dehydrogenase released by cells were measured by performing a CytoTox 96 non-radioactive cytotoxicity assay according to the manufacturer’s instructions (Promega, G1780).
Knockdown via small interfering RNA
BMDMs were transfected for 48 h with small interfering RNA (siRNA) from siGENOME smart pools by using the GenMute siRNA Transfection Reagent according to the manufacturer’s instructions (SignaGen Laboratories, SL100568). The siGENOME SMARTpool siRNA specific for mouse Irf8 (Dharmacon, M-040737-00) was used in the study. A control siRNA pool was also used. Transfected cells were infected with S. Typhimurium as described above.
Immunoblot analysis
BMDM cell lysates and culture supernatants were combined in caspase lysis buffer (containing protease inhibitors, phosphatase inhibitors, 10% NP-40, and 25mM DTT) and sample loading buffer (containing SDS and 2-mercaptoethanol) for immunoblot analysis of caspase-1. For immunoblot analysis of signaling, supernatants were removed and BMDMs were washed once with PBS, followed by lysis in RIPA buffer and sample loading buffer (containing SDS and 2-Mercaptoethanol). Proteins were separated by electrophoresis through 8–12% polyacrylamide gels. Following electrophoretic transfer of proteins onto PVDF membranes (Millipore, IPVH00010), nonspecific binding was blocked by incubation with 5% skim milk, then membranes were incubated with primary antibodies anti-caspase-1 (1:3,000 dilution; Adipogen, AG-20B-0042), anti-IRF8 (1:1,000 dilution; Santa Cruz Biotechnology, sc-6058), anti-GBP2 (1:1,000 dilution; Proteintech, 11854-1-AP), anti-GBP5 (1:1,000 dilution; Proteintech, 13220-1-AP), or anti-β-actin (1:10,000 dilution; Proteintech, 66009-1-IG). Membranes were then washed and incubated with the appropriate horseradish peroxidase (HRP)–conjugated secondary antibodies (1:5,000 dilution; Jackson Immuno Research Laboratories, anti-rabbit [111-035-047], anti-mouse [315-035-047], and anti-goat [705-035-003]) for 1 h. Proteins were visualized by using Luminata Forte Western HRP Substrate (Millipore, WBLUF0500).
Real-time (RT-PCR) analysis
For bacterial stimulation, the following conditions were used: S. Typhimurium at an MOI of 0.01; and for flagellin transfection, 0.1 μg of flagellin. RNA was extracted by using TRIzol (ThermoFisher Scientific, 15596026) according to the manufacturer’s instructions. The isolated RNA was reverse-transcribed into cDNA by using a First-Strand cDNA Synthesis Kit (Applied Biosystems, 4368814). Real-time quantitative PCR was performed on an ABI 7500 RT-PCR instrument by using 2X SYBR Green (Applied Biosystems, 4368706) and the appropriate primers. RT-PCR primer sequences are found in the Key Resources Table.
Cytokine analysis
Cytokines were measured by performing multiplex ELISA (Millipore, MCYTOMAG-70K) or ELISA for IL-18 (Invitrogen, BMS618-3) according to the manufacturer’s instructions.
Flow cytometry
The following monoclonal antibodies were used for flow cytometry cellular analyses: CD11b (M1/70; Affymetrix eBioscience, 48-0112-82) and F4/80 (BM8; BioLegend, 123109). The dilution factor used for these antibodies was 1:300. Flow cytometry data were acquired on a FACSCalibur flow cytometer (BD) and were analyzed by using FlowJo software (FlowJo, LLC and Illumina, Inc).
Microarray, Network analysis, and ChIP-seq
Transcripts were profiled for S. Typhimurium-infected BMDMs obtained from WT and Irf8−/− mice. Total RNA (100 ng) was converted into biotin-labeled cRNA by using an Ambion Wild-Type Expression kit (ThermoFisher Scientific, 4411973) and was hybridized to a Affymetrix GeneChip Mouse Gene 2.0 ST Array (ThermoFisher Scientific, 902119). After chips were stained and washed, array signals were normalized and transformed into log2 transcript expression values by using the robust multi-array average algorithm (Partek Genomics Suite version 6.6) 49. Differential expression was defined by application of a difference in expression of 0.5-fold (log2 signal) between conditions. Lists of differentially expressed transcripts were analyzed for ‘functional enrichment’ by using the DAVID bioinformatics database 50 (Huang et al., 2009) and Ingenuity Pathways Analysis software (Qiagen). An interaction network was generated by using the GeneMANIA Cytoscape plugin with default settings (Mostafavi et al., 2008). FASTQ files corresponding to input (GEO Accession number: GSM1721243), IRF8 ChIP (GEO Accession number: GSM1721244) (Olsson et al., 2016) were downloaded from the Sequence Read Archive database by using SRA toolkit. FASTQ files were uploaded to DNA Nexus (St. Jude Cloud), and sequence reads were mapped against the GRCm38/mm10 genome build. Bedgraph files corresponding to IRF4 ChIP-seq experiment were downloaded from GEO database (GEO Accession number: GSE85172) (Iwata et al., 2017). BED files containing the enrichment scores for SPI1 binding were also downloaded from GEO database (GEO Accession number: GSE77886) (Langlais et al., 2016). The result was visualized using Integrative Genomics Viewer (IGV) (Robinson et al., 2011).
ChIP-PCR
WT BMDMs were cross-linked with 1% paraformaldehyde for 10 min followed by glycin quenching. Samples were washed with ice cold PBS and scraped in PBS supplemented with protease inhibitors. Cell pellets were incubated with SDS lysis buffer for 10 min on ice followed by sonication using Covaris sonicator to obtain the desired fragment length (300 bps to 700 bps). An equal amount of DNA was used for IgG (control) (Cell Signaling Technology, 2729) and IRF8 (Cell Signaling Technology, 5628) immunoprecipitation. Immunoprecipitated DNA was eluted in elution buffer and amplified with primers for Naip2 and Naip5 (found in Key Resources Table).
Luciferase assay
The Naip2 and Naip5 promoter fragments nt −1kb to + 1kb, were amplified by PCR using mouse genomic DNA as a template and inserted into the KpnI and XhoI sites of the luciferase reporter plasmid pGL4.17 basic vector (Promega, E6721) yielding reporter constructs pGL4.17 Naip2 and pGL4.17 Naip5 respectively. HEK293T cells (ATCC, 3216) were co-transfected with the mixture of the indicated luciferase reporter plasmid and pRL-TK-Renilla luciferase (Promega, E2241) plasmid using FuGENE (Promega, E2311) according to manufacturer’s instructions. For inducing IRF8 expression, cells were transfected with pCMV6-mIRF8 vector (Origene, MR206748) and luciferase activity was quantified 48 h after transfection with the Dual-Luciferase Reporter Assay System (Promega, E1910) according to the manufacturer’s instructions. pcDNA3.1 (Invitrogen, V79020) was used as empty vector control.
Electrophoretic Mobility Shift Assay
Nuclear extracts from BMDMs were prepared using NP-40 lysis buffer. EMSA was performed using Light Shift Chemiluminescent EMSA kit (ThermoFisher Scientific, 20148). Analysis of IRF8 binding to predicted sites was performed using annealed biotin labeled oligonucleotide probes in a 20μl reaction mixture for 20 min at room temperature. Samples were run on a non-denaturing 5% polyacrylamide gel and transferred to a nylon membrane (ThermoFisher Scientific, 77016), cross-linked in UV. Probes are listed in Key Resources Table.
IRF8 complementation
Primary mouse BMDMs were transfected with the control pcDNA3.1 or pCMV6-mIRF8 vector (Origene, MR206748) by nucleofection (ThermoFisher Scientific, MPK10025) following the manufacturer’s instructions.
Animal infection
Frozen stocks of S. Typhimurium or B. thailandensis were prepared from LB–grown S. Typhimurium or B. thailandensis, quantified prior to infection, and diluted in PBS for infections. For S. Typhimurium infection, mice were injected intraperitoneally with 103 CFU in 200 μL PBS. For B. thailandensis infection, mice were lightly anesthetized with isoflurane and inoculated intranasally with 5 × 104 CFU in 50 μL PBS. After 3 days of S. Typhimurium or 2 days of B. thailandensis infection, lungs, liver, and spleen were collected and then homogenized for 2 min in PBS with metal beads by using a TissueLyser II apparatus (Qiagen). CFU values were quantified by plating lysates onto LB agar, followed by incubation overnight. No randomization or blinding was used. Formalin preserved lungs were processed and embedded in paraffin according to standard procedures. Sections (5 μm) were stained with H&E and examined.
QUANTIFICATION AND STATISTICAL ANALYSIS
Statistical analysis
GraphPad Prism 6.0 software was used for data analysis. Data are shown as mean ± SEM. Statistical significance was determined by t tests (two-tailed) for two groups or ANOVA (with Dunnett’s multiple comparisons test, Dunn’s multiple comparisons test, or Tukey’s multiple comparisons test) for three or more groups. Survival curves were compared with the log-rank test outcome. P values less than 0.05 were considered to be statistically significant.
DATA RESOURCES
Microarray
The dataset was deposited under the accession code GSE110452.
Supplementary Material
(A) Release of cytokines IL-1β, IL-6, TNF and LDH in BMDMs after infection with F. novicida (MOI, 100).
(B) Release of IL-6, TNF, KC and LDH in BMDMs transfected with poly(dA:dT).
(C) Release of IL-1β, IL-6, TNF and LDH in BMDMs primed with LPS and stimulated with ATP.
(D) Release of IL-6, TNF, KC and LDH in BMDMs primed with LPS and transfected with LPS.
NS, not significant; **P < 0.01 and ***P < 0.001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are from 3 independent experiments (mean ± SEM).
(A) Flow cytometric analysis of side-scattered light (SSC), forward-scattered light (FSC); and expression of F4/80 and CD11b of BMDMs generated from WT and Irf8−/− mice.
(B) Immunoblot analysis of IRF8, GBP2, GBP5, and β-actin (loading control) in BMDMs at various times after infection with F. novicida.
(C–E) Immunoblot analysis of caspase-1 in BMDMs that were infected with multiple MOIs of S. Typhimurium, P. aeruginosa, or B. thailandensis.
(F) Immunoblot analysis of IRF8 in BMDMs stimulated with LPS or infected with S. Typhimurium or B. thailandensis.
Data are representative of 2 independent experiments.
(A) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with S. Typhimurium (MOI, 0.1).
(B and C) Microscopic images and cell death analysis of BMDMs infected with ΔfliCΔfljB (MOI, 1) or ΔSPI-2 (MOI, 1).
(D) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with P. aeruginosa (MOI, 1).
(E) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with B. thailandensis (MOI, 1).
Scale bars, 100 μm (B), NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are representative of 3 (B) or from 3 (A and C–E) independent experiments (mean ± SEM).
(A) Immunoblot analysis of caspase-1 in WT BMDMs transfected with a control siRNA or Irf8 siRNA and then infected with S. Typhimurium (MOI, 0.1) for 4 h or F. novicida (MOI, 100) for 20 h. Nlrc4−/− (left) or Aim2−/− (right) BMDMs were used as controls.
(B) Relative expression of the gene encoding IRF8 in WT BMDMs transfected with a control siRNA or Irf8 siRNA.
(C) Immunoblot analysis of caspase-1 in BMDMs that were infected with S. Typhimurium (MOI, 0.1) and collected after 4 h.
(D) Microscopic images of BMDMs that were infected with S. Typhimurium (MOI, 0.1).
(E) Immunoblot analysis of caspase-1 in BMDMs that were transfected with different doses of flagellin.
(F and G) Release of IL-1β and KC in BMDMs treated with DOTAP, transfected with flagellin (DOTAP + Flgn), or treated with flagellin (Flgn).
(H and I) Immunoblot analysis of caspase-1 and assessment of IL-18 levels in BMDMs untreated or transfected with flagellin.
(J) Microscopic images of BMDMs transfected with PrgI (DOTAP + PrgI) or PrgJ (DOTAP + PrgJ).
Scale bars, 100 μm (D and J), NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are from 3 (F and G) or 2 (I) or representative of 2 (A–E, H, and J) independent experiments (mean ± SEM).
RT-PCR analysis of genes encoding NAIPs and NLRC4 in BMDMs, normalized to that of the gene encoding HPRT.
Data are from 2 independent experiments (mean ± SEM).
(A) Survival of 8-week-old WT (n=11) and Irf8−/− (n=7) mice infected intranasally with 5 × 104 CFU of B. thailandensis.
(B) Bacterial burden in the lungs, liver and spleen of WT (n=10) and Irf8−/− (n=9) mice on day 2 after infection as (A).
(C) Analysis of IL-18 in the lungs, liver, spleen, and serum collected from WT (n=10) and Irf8−/− (n=9) mice on day 2 after infection as (A).
(D) H&E staining of lungs collected from WT and Irf8−/− mice on day 2 after infection as (A).
(E–H) RT-PCR analysis of genes encoding NAIPs and NLRC4 in spleen and lungs collected from WT (n=10) and Irf8−/− (n=9) mice before (day 0) and after infection (day 2) as (A), presented relative to that of the gene encoding HPRT.
Scale bars, 250 μm (D), NS, not significant; *P < 0.05, **P < 0.001, ***P < 0.0001 and ****P < 0.0001 (log-rank test [A] or two-tailed t test [B and C] or Two-way ANOVA with Tukey’s multiple comparisons test [E–H]). Data are representative of 2 (D) or from 2 (A–C and E–H) independent experiments.
(A) Blood cell counts from peripheral blood of WT (n=10), Irf8−/− (n=6), and Nlrc4−/− (n=10) mice on day 3 after intraperitoneal infection with 103 CFU of S. Typhimurium.
(B) Blood cell counts from peripheral blood of WT (n=10) and Irf8−/− (n=9) mice on day 2 after intranasal infection with 5 × 104 CFU of B. thailandensis.
NS, not significant; *P < 0.05, **P < 0.01 and ***P < 0.001 (One-way ANOVA with Dunnett’s multiple comparisons test [A] or two-tailed t test [B]). Data are from 1 independent experiment.
HIGHLIGHTS.
IRF8 is required for the optimal activation of NLRC4 inflammasome.
The expression of Naip1, Naip2, Naip5, and Naip6 is dependent on IRF8.
IRF8 is dispensable for the activation of NLRP3, AIM2 and Pyrin inflammasomes.
Irf8−/− mice are susceptible to S. Typhimurium and B. thailandensis infection.
Acknowledgments
We thank A. Burton from St. Jude Children’s Research Hospital for technical support. We thank members of the Kanneganti laboratory for their comments and suggestions. Work from our laboratory is supported by the US National Institutes of Health (AI101935, AI124346, AR056296 and CA163507 to T.-D.K.), and the American Lebanese Syrian Associated Charities (to T.-D.K.)
Footnotes
DECLARATION OF INTERESTS
The authors declare no competing financial interests.
AUTHOR CONTRIBUTIONS
R.K., E.L., and T.-D.K. conceptualized the study; R.K., E.L., D.P., P.S., J.M., A.B. and R.K.S.M. designed the methodology; R.K., E.L., D.P., P.S., J.M., B.R.S., A.B., R.K.S.M., R.G. and Q.Z. performed the experiments; R.K., E.L., D.P., P.S., J.M., B.R.S., A.B., R.K.S.M and G.N. conducted the analysis; R.K., E.L., and T.-D.K. wrote the manuscript with input from all authors. T.-D.K. acquired the funding and provided overall supervision.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amer A, Franchi L, Kanneganti TD, Body-Malapel M, Özören N, Brady G, Meshinchi S, Jagirdar R, Gewirtz A, Akira S, et al. Regulation of Legionella Phagosome Maturation and Infection through Flagellin and Host Ipaf. J Biol Chem. 2006;281:35217–35223. doi: 10.1074/jbc.M604933200. [DOI] [PubMed] [Google Scholar]
- Barber SA, Fultz MJ, Salkowski CA, Vogel SN. Differential expression of interferon regulatory factor 1 (IRF-1), IRF-2, and interferon consensus sequence binding protein genes in lipopolysaccharide (LPS)-responsive and LPS-hyporesponsive macrophages. Infect Immun. 1995;63:601–608. doi: 10.1128/iai.63.2.601-608.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovolenta C, Driggers PH, Marks MS, Medin JA, Politis AD, Vogel SN, Levy DE, Sakaguchi K, Appella E, Coligan JE. Molecular interactions between interferon consensus sequence binding protein and members of the interferon regulatory factor family. Proc Natl Acad Sci U S A. 1994;91:5046–5050. doi: 10.1073/pnas.91.11.5046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broz P, Newton K, Lamkanfi M, Mariathasan S, Dixit VM, Monack DM. Redundant roles for inflammasome receptors NLRP3 and NLRC4 in host defense against Salmonella. J Exp Med. 2010;207:1745–1755. doi: 10.1084/jem.20100257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broz P, Ruby T, Belhocine K, Bouley DM, Kayagaki N, Dixit VM, Monack DM. Caspase-11 increases susceptibility to Salmonella infection in the absence of caspase-1. Nature. 2012;490:288–291. doi: 10.1038/nature11419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho FA, Nalbantoglu I, Aitken JD, Uchiyama R, Su Y, Doho GH, Vijay-Kumar M, Gewirtz AT. Cytosolic flagellin receptor NLRC4 protects mice against mucosal and systemic challenges. Mucosal Immunol. 2012;5:288–298. doi: 10.1038/mi.2012.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowley SM, Knodler LA, Vallance BA. Salmonella and the Inflammasome: Battle for Intracellular Dominance. Curr Top Microbiol Immunol. 2016;397:43–67. doi: 10.1007/978-3-319-41171-2_3. [DOI] [PubMed] [Google Scholar]
- Driggers PH, Ennist DL, Gleason SL, Mak WH, Marks MS, Levi BZ, Flanagan JR, Appella E, Ozato K. An interferon gamma-regulated protein that binds the interferon-inducible enhancer element of major histocompatibility complex class I genes. Proc Natl Acad Sci. 1990;87:3743–3747. doi: 10.1073/pnas.87.10.3743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eklund EA, Jalava A, Kakar R. PU. 1, Interferon Regulatory Factor 1, and Interferon Consensus Sequence-binding Protein Cooperate to Increase gp91 phox Expression. J Biol Chem. 1998;273:13957–13965. doi: 10.1074/jbc.273.22.13957. [DOI] [PubMed] [Google Scholar]
- Fàbrega A, Vila J. Salmonella enterica Serovar Typhimurium Skills To Succeed in the Host: Virulence and Regulation. Clin Microbiol Rev. 2013;26:308–341. doi: 10.1128/CMR.00066-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner JE, Starr R, Cornish AL, Zhang JG, Metcalf D, Schreiber RD, Sheehan K, Hilton DJ, Alexander WS, Hertzog PJ. Suppressor of cytokine signaling 1 regulates the immune response to infection by a unique inhibition of type I interferon activity. Nat Immunol. 2006;7:33–39. doi: 10.1038/ni1287. [DOI] [PubMed] [Google Scholar]
- Fernandes-Alnemri T, Yu JW, Juliana C, Solorzano L, Kang S, Wu J, Datta P, McCormick M, Huang L, McDermott E, et al. The AIM2 inflammasome is critical for innate immunity to Francisella tularensis. Nat Immunol. 2010;11:385–393. doi: 10.1038/ni.1859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franchi L, Amer A, Body-Malapel M, Kanneganti TD, Özören N, Jagirdar R, Inohara N, Vandenabeele P, Bertin J, Coyle A, et al. Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1β in salmonella-infected macrophages. Nat Immunol. 2006;7:576–582. doi: 10.1038/ni1346. [DOI] [PubMed] [Google Scholar]
- Fujita T, Kimura Y, Miyamoto M, Barsoumian EL, Taniguchi T. Induction of endogenous IFN-α and IFN-β genes by a regulatory transcription factor, IRF-1. Nature. 1989;337:270–272. doi: 10.1038/337270a0. [DOI] [PubMed] [Google Scholar]
- Glasmacher E, Agrawal S, Chang AB, Murphy TL, Zeng W, Lugt BV, Khan AA, Ciofani M, Spooner CJ, Rutz S, et al. A Genomic Regulatory Element That Directs Assembly and Function of Immune-Specific AP-1–IRF Complexes. Science. 2012;338:975–980. doi: 10.1126/science.1228309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorp HV, Saavedra PHV, de Vasconcelos NM, Opdenbosch NV, Walle LV, Matusiak M, Prencipe G, Insalaco A, Hauwermeiren FV, Demon D, et al. Familial Mediterranean fever mutations lift the obligatory requirement for microtubules in Pyrin inflammasome activation. Proc Natl Acad Sci. 2016;113:14384–14389. doi: 10.1073/pnas.1613156113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harada H, Fujita T, Miyamoto M, Kimura Y, Maruyama M, Furia A, Miyata T, Taniguchi T. Structurally similar but functionally distinct factors, IRF-1 and IRF-2, bind to the same regulatory elements of IFN and IFN-inducible genes. Cell. 1989;58:729–739. doi: 10.1016/0092-8674(89)90107-4. [DOI] [PubMed] [Google Scholar]
- Henry T, Brotcke A, Weiss DS, Thompson LJ, Monack DM. Type I interferon signaling is required for activation of the inflammasome during Francisella infection. J Exp Med. 2007;204:987–994. doi: 10.1084/jem.20062665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda K, Yanai H, Negishi H, Asagiri M, Sato M, Mizutani T, Shimada N, Ohba Y, Takaoka A, Yoshida N, et al. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature. 2005;434:772–777. doi: 10.1038/nature03464. [DOI] [PubMed] [Google Scholar]
- Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- Ivashkiv LB, Donlin LT. Regulation of type I interferon responses. Nat Rev Immunol. 2014;14:36–49. doi: 10.1038/nri3581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iwata A, Durai V, Tussiwand R, Briseño CG, Wu X, Grajales-Reyes GE, Egawa T, Murphy TL, Murphy KM. Quality of TCR signaling determined by differential affinities of enhancers for the composite BATF-IRF4 transcription factor complex. Nat Immunol. 2017;18:563–572. doi: 10.1038/ni.3714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CL, Napier BA, Sampson TR, Llewellyn AC, Schroeder MR, Weiss DS. Subversion of Host Recognition and Defense Systems by Francisella spp. Microbiol Mol Biol Rev. 2012;76:383–404. doi: 10.1128/MMBR.05027-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JDG, Vance RE, Dangl JL. Intracellular innate immune surveillance devices in plants and animals. Science. 2016;354:aaf6395. doi: 10.1126/science.aaf6395. [DOI] [PubMed] [Google Scholar]
- Jones JW, Kayagaki N, Broz P, Henry T, Newton K, O’Rourke K, Chan S, Dong J, Qu Y, Roose-Girma M, et al. Absent in melanoma 2 is required for innate immune recognition of Francisella tularensis. Proc Natl Acad Sci. 2010a;107:9771–9776. doi: 10.1073/pnas.1003738107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones JW, Kayagaki N, Broz P, Henry T, Newton K, O’Rourke K, Chan S, Dong J, Qu Y, Roose-Girma M, et al. Absent in melanoma 2 is required for innate immune recognition of Francisella tularensis. Proc Natl Acad Sci. 2010b;107:9771–9776. doi: 10.1073/pnas.1003738107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanneganti TD, Özören N, Body-Malapel M, Amer A, Park JH, Franchi L, Whitfield J, Barchet W, Colonna M, Vandenabeele P, et al. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 2006;440:233–236. doi: 10.1038/nature04517. [DOI] [PubMed] [Google Scholar]
- Kato H, Takeuchi O, Sato S, Yoneyama M, Yamamoto M, Matsui K, Uematsu S, Jung A, Kawai T, Ishii KJ, et al. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature. 2006;441:101–105. doi: 10.1038/nature04734. [DOI] [PubMed] [Google Scholar]
- Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, Newton K, Qu Y, Liu J, Heldens S, et al. Non-canonical inflammasome activation targets caspase-11. Nature. 2011;479:117–121. doi: 10.1038/nature10558. [DOI] [PubMed] [Google Scholar]
- Kayagaki N, Stowe IB, Lee BL, O’Rourke K, Anderson K, Warming S, Cuellar T, Haley B, Roose-Girma M, Phung QT, et al. Caspase-11 cleaves gasdermin D for non-canonical inflammasome signalling. Nature. 2015;526:666–671. doi: 10.1038/nature15541. [DOI] [PubMed] [Google Scholar]
- Kimura T, Kadokawa Y, Harada H, Matsumoto M, Sato M, Kashiwazaki Y, Tarutani M, Tan RS, Takasugi T, Matsuyama T, et al. Essential and non-redundant roles of p48 (ISGF3 gamma) and IRF-1 in both type I and type II interferon responses, as revealed by gene targeting studies. Genes Cells Devoted Mol Cell Mech. 1996;1:115–124. doi: 10.1046/j.1365-2443.1996.08008.x. [DOI] [PubMed] [Google Scholar]
- Kofoed EM, Vance RE. Innate immune recognition of bacterial ligands by NAIPs determines inflammasome specificity. Nature. 2011;477:592–595. doi: 10.1038/nature10394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortmann J, Brubaker SW, Monack DM. Cutting Edge: Inflammasome Activation in Primary Human Macrophages Is Dependent on Flagellin. J Immunol. 2015;195:815–819. doi: 10.4049/jimmunol.1403100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuehne SA, Collery MM, Kelly ML, Cartman ST, Cockayne A, Minton NP. Importance of Toxin A, Toxin B, and CDT in Virulence of an Epidemic Clostridium difficile Strain. J Infect Dis. 2014;209:83–86. doi: 10.1093/infdis/jit426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurotaki D, Tamura T. Transcriptional and Epigenetic Regulation of Innate Immune Cell Development by the Transcription Factor, Interferon Regulatory Factor-8. J Interferon Cytokine Res. 2016;36:433–441. doi: 10.1089/jir.2015.0138. [DOI] [PubMed] [Google Scholar]
- Langlais D, Barreiro LB, Gros P. The macrophage IRF8/IRF1 regulome is required for protection against infections and is associated with chronic inflammation. J Exp Med. 2016;213:585–603. doi: 10.1084/jem.20151764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehtonen A, Matikainen S, Julkunen I. Interferons up-regulate STAT1, STAT2, and IRF family transcription factor gene expression in human peripheral blood mononuclear cells and macrophages. J Immunol. 1997;159:794–803. [PubMed] [Google Scholar]
- Liu J, Guan X, Tamura T, Ozato K, Ma X. Synergistic Activation of Interleukin-12 p35 Gene Transcription by Interferon Regulatory Factor-1 and Interferon Consensus Sequence-binding Protein. J Biol Chem. 2004;279:55609–55617. doi: 10.1074/jbc.M406565200. [DOI] [PubMed] [Google Scholar]
- Liu X, Zhang Z, Ruan J, Pan Y, Magupalli VG, Wu H, Lieberman J. Inflammasome-activated gasdermin D causes pyroptosis by forming membrane pores. Nature. 2016;535:153. doi: 10.1038/nature18629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Kanneganti TD. Regulation of inflammasome activation. Immunol Rev. 2015;265:6–21. doi: 10.1111/imr.12296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Hopkins LJ, Nugent E, Cox S, Glück IM, Tourlomousis P, Wright JA, Cicuta P, Monie TP, Bryant CE. Inflammasome activation causes dual recruitment of NLRC4 and NLRP3 to the same macromolecular complex. Proc Natl Acad Sci. 2014;111:7403–7408. doi: 10.1073/pnas.1402911111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Karki R, Malireddi RKS, Neale G, Vogel P, Yamamoto M, Lamkanfi M, Kanneganti TD. The transcription factor IRF1 and guanylate-binding proteins target activation of the AIM2 inflammasome by Francisella infection. Nat Immunol. 2015;16:467–475. doi: 10.1038/ni.3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Karki R, Briard B, Burton A, Gingras S, Pelletier S, Kanneganti T-D. Differential roles of caspase-1 and caspase-11 in infection and inflammation. Sci Rep. 2017;7:srep45126. doi: 10.1038/srep45126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariathasan S, Newton K, Monack DM, Vucic D, French DM, Lee WP, Roose-Girma M, Erickson S, Dixit VM. Differential activation of the inflammasome by caspase-1 adaptors ASC and Ipaf. Nature. 2004;430:213–218. doi: 10.1038/nature02664. [DOI] [PubMed] [Google Scholar]
- Martone R, Euskirchen G, Bertone P, Hartman S, Royce TE, Luscombe NM, Rinn JL, Nelson FK, Miller P, Gerstein M, et al. Distribution of NF-κB-binding sites across human chromosome 22. Proc Natl Acad Sci. 2003;100:12247–12252. doi: 10.1073/pnas.2135255100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masumi A, Tamaoki S, Wang IM, Ozato K, Komuro K. IRF-8/ICSBP and IRF-1 cooperatively stimulate mouse IL-12 promoter activity in macrophages. FEBS Lett. 2002;531:348–353. doi: 10.1016/s0014-5793(02)03556-1. [DOI] [PubMed] [Google Scholar]
- Matsuyama T, Kimura T, Kitagawa M, Pfeffer K, Kawakami T, Watanabe N, Kündig TM, Amakawa R, Kishihara K, Wakeham A, et al. Targeted disruption of IRF-1 or IRF-2 results in abnormal type I IFN gene induction and aberrant lymphocyte development. Cell. 1993;75:83–97. [PubMed] [Google Scholar]
- Miao EA, Alpuche-Aranda CM, Dors M, Clark AE, Bader MW, Miller SI, Aderem A. Cytoplasmic flagellin activates caspase-1 and secretion of interleukin 1β via Ipaf. Nat Immunol. 2006;7:569–575. doi: 10.1038/ni1344. [DOI] [PubMed] [Google Scholar]
- Mostafavi S, Ray D, Warde-Farley D, Grouios C, Morris Q. GeneMANIA: a real-time multiple association network integration algorithm for predicting gene function. Genome Biol. 2008;9:S4. doi: 10.1186/gb-2008-9-s1-s4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller U, Steinhoff U, Reis LF, Hemmi S, Pavlovic J, Zinkernagel RM, Aguet M. Functional role of type I and type II interferons in antiviral defense. Science. 1994;264:1918–1921. doi: 10.1126/science.8009221. [DOI] [PubMed] [Google Scholar]
- Olsson A, Venkatasubramanian M, Chaudhri VK, Aronow BJ, Salomonis N, Singh H, Grimes HL. Single-cell analysis of mixed-lineage states leading to a binary cell fate choice. Nature. 2016;537:698–702. doi: 10.1038/nature19348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rathinam VAK, Vanaja SK, Waggoner L, Sokolovska A, Becker C, Stuart LM, Leong JM, Fitzgerald KA. TRIF Licenses Caspase-11-Dependent NLRP3 Inflammasome Activation by Gram-Negative Bacteria. Cell. 2012;150:606–619. doi: 10.1016/j.cell.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch I, Tenthorey JL, Nichols RD, Moussawi KA, Kang JJ, Kang C, Kazmierczak BI, Vance RE. NAIP proteins are required for cytosolic detection of specific bacterial ligands in vivo. J Exp Med. 2016;213:657–665. doi: 10.1084/jem.20151809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson JT, Thorvaldsdóttir H, Winckler W, Guttman M, Lander ES, Getz G, Mesirov JP. Integrative genomics viewer. Nat Biotechnol. 2011;29:24–26. doi: 10.1038/nbt.1754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato M, Suemori H, Hata N, Asagiri M, Ogasawara K, Nakao K, Nakaya T, Katsuki M, Noguchi S, Tanaka N, et al. Distinct and Essential Roles of Transcription Factors IRF-3 and IRF-7 in Response to Viruses for IFN-α/β Gene Induction. Immunity. 2000;13:539–548. doi: 10.1016/s1074-7613(00)00053-4. [DOI] [PubMed] [Google Scholar]
- Sauer JD, Sotelo-Troha K, von Moltke J, Monroe KM, Rae CS, Brubaker SW, Hyodo M, Hayakawa Y, Woodward JJ, Portnoy DA, et al. The N-ethyl-N-nitrosourea-induced Goldenticket mouse mutant reveals an essential function of Sting in the in vivo interferon response to Listeria monocytogenes and cyclic dinucleotides. Infect Immun. 2011;79:688–694. doi: 10.1128/IAI.00999-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoggins JW, MacDuff DA, Imanaka N, Gainey MD, Shrestha B, Eitson JL, Mar KB, Richardson RB, Ratushny AV, Litvak V, et al. Pan-viral specificity of IFN-induced genes reveals new roles for cGAS in innate immunity. Nature. 2014;505:691–695. doi: 10.1038/nature12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sellin ME, Müller AA, Felmy B, Dolowschiak T, Diard M, Tardivel A, Maslowski KM, Hardt WD. Epithelium-Intrinsic NAIP/NLRC4 Inflammasome Drives Infected Enterocyte Expulsion to Restrict Salmonella Replication in the Intestinal Mucosa. Cell Host Microbe. 2014;16:237–248. doi: 10.1016/j.chom.2014.07.001. [DOI] [PubMed] [Google Scholar]
- Shi J, Zhao Y, Wang K, Shi X, Wang Y, Huang H, Zhuang Y, Cai T, Wang F, Shao F. Cleavage of GSDMD by inflammatory caspases determines pyroptotic cell death. Nature. 2015;526:660–665. doi: 10.1038/nature15514. [DOI] [PubMed] [Google Scholar]
- Sichien D, Scott CL, Martens L, Vanderkerken M, Van Gassen S, Plantinga M, Joeris T, De Prijck S, Vanhoutte L, Vanheerswynghels M, et al. IRF8 Transcription Factor Controls Survival and Function of Terminally Differentiated Conventional and Plasmacytoid Dendritic Cells, Respectively. Immunity. 2016;45:626–640. doi: 10.1016/j.immuni.2016.08.013. [DOI] [PubMed] [Google Scholar]
- Storek KM, Monack DM. Bacterial recognition pathways that lead to inflammasome activation. Immunol Rev. 2015;265:112–129. doi: 10.1111/imr.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suthar MS, Ramos HJ, Brassil MM, Netland J, Chappell CP, Blahnik G, McMillan A, Diamond MS, Clark EA, Bevan MJ, et al. The RIG-I-like receptor LGP2 controls CD8(+) T cell survival and fitness. Immunity. 2012;37:235–248. doi: 10.1016/j.immuni.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutterwala FS, Mijares LA, Li L, Ogura Y, Kazmierczak BI, Flavell RA. Immune recognition of Pseudomonas aeruginosa mediated by the IPAF/NLRC4 inflammasome. J Exp Med. 2007;204:3235–3245. doi: 10.1084/jem.20071239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tailor P, Tamura T, Kong HJ, Kubota T, Kubota M, Borghi P, Gabriele L, Ozato K. The Feedback Phase of Type I Interferon Induction in Dendritic Cells Requires Interferon Regulatory Factor 8. Immunity. 2007;27:228–239. doi: 10.1016/j.immuni.2007.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamura T, Yanai H, Savitsky D, Taniguchi T. The IRF family transcription factors in immunity and oncogenesis. Annu Rev Immunol. 2008;26:535–584. doi: 10.1146/annurev.immunol.26.021607.090400. [DOI] [PubMed] [Google Scholar]
- Tokuhiro S, Yamada R, Chang X, Suzuki A, Kochi Y, Sawada T, Suzuki M, Nagasaki M, Ohtsuki M, Ono M, et al. An intronic SNP in a RUNX1 binding site of SLC22A4, encoding an organic cation transporter, is associated with rheumatoid arthritis. Nat Genet. 2003;35:341–348. doi: 10.1038/ng1267. [DOI] [PubMed] [Google Scholar]
- Veals SA, Schindler C, Leonard D, Fu XY, Aebersold R, Darnell JE, Levy DE. Subunit of an alpha-interferon-responsive transcription factor is related to interferon regulatory factor and Myb families of DNA-binding proteins. Mol Cell Biol. 1992;12:3315–3324. doi: 10.1128/mcb.12.8.3315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang IM, Contursi C, Masumi A, Ma X, Trinchieri G, Ozato K. An IFN-γ-Inducible Transcription Factor, IFN Consensus Sequence Binding Protein (ICSBP), Stimulates IL-12 p40 Expression in Macrophages. J Immunol. 2000;165:271–279. doi: 10.4049/jimmunol.165.1.271. [DOI] [PubMed] [Google Scholar]
- Wei CL, Wu Q, Vega VB, Chiu KP, Ng P, Zhang T, Shahab A, Yong HC, Fu Y, Weng Z, et al. A Global Map of p53 Transcription-Factor Binding Sites in the Human Genome. Cell. 2006;124:207–219. doi: 10.1016/j.cell.2005.10.043. [DOI] [PubMed] [Google Scholar]
- Xiong H, Zhu C, Li H, Chen F, Mayer L, Ozato K, Unkeless JC, Plevy SE. Complex Formation of the Interferon (IFN) Consensus Sequence-binding Protein with IRF-1 Is Essential for Murine Macrophage IFN-γ-induced iNOS Gene Expression. J Biol Chem. 2003;278:2271–2277. doi: 10.1074/jbc.M209583200. [DOI] [PubMed] [Google Scholar]
- Xu H, Yang J, Gao W, Li L, Li P, Zhang L, Gong YN, Peng X, Xi JJ, Chen S, et al. Innate immune sensing of bacterial modifications of Rho GTPases by the Pyrin inflammasome. Nature. 2014;513:237–241. doi: 10.1038/nature13449. [DOI] [PubMed] [Google Scholar]
- Yamagata T, Nishida J, Tanaka S, Sakai R, Mitani K, Yoshida M, Taniguchi T, Yazaki Y, Hirai H. A novel interferon regulatory factor family transcription factor, ICSAT/Pip/LSIRF, that negatively regulates the activity of interferon-regulated genes. Mol Cell Biol. 1996;16:1283–1294. doi: 10.1128/mcb.16.4.1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto M, Sato S, Hemmi H, Hoshino K, Kaisho T, Sanjo H, Takeuchi O, Sugiyama M, Okabe M, Takeda K, et al. Role of adaptor TRIF in the MyD88-independent toll-like receptor signaling pathway. Science. 2003;301:640–643. doi: 10.1126/science.1087262. [DOI] [PubMed] [Google Scholar]
- Yang J, Zhao Y, Shi J, Shao F. Human NAIP and mouse NAIP1 recognize bacterial type III secretion needle protein for inflammasome activation. Proc Natl Acad Sci. 2013;110:14408–14413. doi: 10.1073/pnas.1306376110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamboni DS, Kobayashi KS, Kohlsdorf T, Ogura Y, Long EM, Vance RE, Kuida K, Mariathasan S, Dixit VM, Flavell RA, et al. The Birc1e cytosolic pattern-recognition receptor contributes to the detection and control of Legionella pneumophila infection. Nat Immunol. 2006;7:318–325. doi: 10.1038/ni1305. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Shao F. The NAIP–NLRC4 inflammasome in innate immune detection of bacterial flagellin and type III secretion apparatus. Immunol Rev. 2015;265:85–102. doi: 10.1111/imr.12293. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Yang J, Shi J, Gong YN, Lu Q, Xu H, Liu L, Shao F. The NLRC4 inflammasome receptors for bacterial flagellin and type III secretion apparatus. Nature. 2011;477:596–600. doi: 10.1038/nature10510. [DOI] [PubMed] [Google Scholar]
- Zhao Y, Shi J, Shi X, Wang Y, Wang F, Shao F. Genetic functions of the NAIP family of inflammasome receptors for bacterial ligands in mice. J Exp Med. 2016;213:647–656. doi: 10.1084/jem.20160006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zitvogel L, Galluzzi L, Kepp O, Smyth MJ, Kroemer G. Type I interferons in anticancer immunity. Nat Rev Immunol. 2015;15:405–414. doi: 10.1038/nri3845. [DOI] [PubMed] [Google Scholar]
References
- Broz P, Newton K, Lamkanfi M, Mariathasan S, Dixit VM, Monack DM. Redundant roles for inflammasome receptors NLRP3 and NLRC4 in host defense against Salmonella. J Exp Med. 2010;207:1745–1755. doi: 10.1084/jem.20100257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar R, Domrachev M, Lash AE. Gene Expression Omnibus: NCBI gene expression and hybridization array data repository. Nucleic Acids Res. 2002;30:207–210. doi: 10.1093/nar/30.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenner JE, Starr R, Cornish AL, Zhang JG, Metcalf D, Schreiber RD, Sheehan K, Hilton DJ, Alexander WS, Hertzog PJ. Suppressor of cytokine signaling 1 regulates the immune response to infection by a unique inhibition of type I interferon activity. Nat Immunol. 2006;7:33–39. doi: 10.1038/ni1287. [DOI] [PubMed] [Google Scholar]
- Franchi L, Amer A, Body-Malapel M, Kanneganti TD, Özören N, Jagirdar R, Inohara N, Vandenabeele P, Bertin J, Coyle A, et al. Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1β in salmonella-infected macrophages. Nat Immunol. 2006;7:576–582. doi: 10.1038/ni1346. [DOI] [PubMed] [Google Scholar]
- Glaccum MB, Stocking KL, Charrier K, Smith JL, Willis CR, Maliszewski C, Livingston DJ, Peschon JJ, Morrissey PJ. Phenotypic and functional characterization of mice that lack the type I receptor for IL-1. J Immunol Baltim Md 1950. 1997;159:3364–3371. [PubMed] [Google Scholar]
- Gorp HV, Saavedra PHV, de Vasconcelos NM, Opdenbosch NV, Walle LV, Matusiak M, Prencipe G, Insalaco A, Hauwermeiren FV, Demon D, et al. Familial Mediterranean fever mutations lift the obligatory requirement for microtubules in Pyrin inflammasome activation. Proc Natl Acad Sci. 2016;113:14384–14389. doi: 10.1073/pnas.1613156113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Honda K, Yanai H, Negishi H, Asagiri M, Sato M, Mizutani T, Shimada N, Ohba Y, Takaoka A, Yoshida N, et al. IRF-7 is the master regulator of type-I interferon-dependent immune responses. Nature. 2005;434:772–777. doi: 10.1038/nature03464. [DOI] [PubMed] [Google Scholar]
- Hood RD, Singh P, Hsu F, Güvener T, Carl MA, Trinidad RRS, Silverman JM, Ohlson BB, Hicks KG, Plemel RL, et al. A Type VI Secretion System of Pseudomonas aeruginosa Targets a Toxin to Bacteria. Cell Host Microbe. 2010;7:25–37. doi: 10.1016/j.chom.2009.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang DW, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- Jones JW, Kayagaki N, Broz P, Henry T, Newton K, O’Rourke K, Chan S, Dong J, Qu Y, Roose-Girma M, et al. Absent in melanoma 2 is required for innate immune recognition of Francisella tularensis. Proc Natl Acad Sci. 2010;107:9771–9776. doi: 10.1073/pnas.1003738107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanneganti TD, Özören N, Body-Malapel M, Amer A, Park JH, Franchi L, Whitfield J, Barchet W, Colonna M, Vandenabeele P, et al. Bacterial RNA and small antiviral compounds activate caspase-1 through cryopyrin/Nalp3. Nature. 2006;440:233–236. doi: 10.1038/nature04517. [DOI] [PubMed] [Google Scholar]
- Kato H, Takeuchi O, Sato S, Yoneyama M, Yamamoto M, Matsui K, Uematsu S, Jung A, Kawai T, Ishii KJ, et al. Differential roles of MDA5 and RIG-I helicases in the recognition of RNA viruses. Nature. 2006;441:101–105. doi: 10.1038/nature04734. [DOI] [PubMed] [Google Scholar]
- Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, Newton K, Qu Y, Liu J, Heldens S, et al. Non-canonical inflammasome activation targets caspase-11. Nature. 2011;479:117–121. doi: 10.1038/nature10558. [DOI] [PubMed] [Google Scholar]
- Kimura T, Kadokawa Y, Harada H, Matsumoto M, Sato M, Kashiwazaki Y, Tarutani M, Tan RS, Takasugi T, Matsuyama T, et al. Essential and non-redundant roles of p48 (ISGF3 gamma) and IRF-1 in both type I and type II interferon responses, as revealed by gene targeting studies. Genes Cells Devoted Mol Cell Mech. 1996;1:115–124. doi: 10.1046/j.1365-2443.1996.08008.x. [DOI] [PubMed] [Google Scholar]
- Lightfield KL, Persson J, Brubaker SW, Witte CE, von Moltke J, Dunipace EA, Henry T, Sun YH, Cado D, Dietrich WF, et al. Critical function for Naip5 in inflammasome activation by a conserved carboxy-terminal domain of flagellin. Nat Immunol. 2008;9:1171–1178. doi: 10.1038/ni.1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Karki R, Malireddi RKS, Neale G, Vogel P, Yamamoto M, Lamkanfi M, Kanneganti TD. The transcription factor IRF1 and guanylate-binding proteins target activation of the AIM2 inflammasome by Francisella infection. Nat Immunol. 2015;16:467–475. doi: 10.1038/ni.3118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Man SM, Karki R, Briard B, Burton A, Gingras S, Pelletier S, Kanneganti T-D. Differential roles of caspase-1 and caspase-11 in infection and inflammation. Sci Rep. 2017;7:srep45126. doi: 10.1038/srep45126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuyama T, Kimura T, Kitagawa M, Pfeffer K, Kawakami T, Watanabe N, Kündig TM, Amakawa R, Kishihara K, Wakeham A, et al. Targeted disruption of IRF-1 or IRF-2 results in abnormal type I IFN gene induction and aberrant lymphocyte development. Cell. 1993;75:83–97. [PubMed] [Google Scholar]
- Mostafavi S, Ray D, Warde-Farley D, Grouios C, Morris Q. GeneMANIA: a real-time multiple association network integration algorithm for predicting gene function. Genome Biol. 2008;9:S4. doi: 10.1186/gb-2008-9-s1-s4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller U, Steinhoff U, Reis LF, Hemmi S, Pavlovic J, Zinkernagel RM, Aguet M. Functional role of type I and type II interferons in antiviral defense. Science. 1994;264:1918–1921. doi: 10.1126/science.8009221. [DOI] [PubMed] [Google Scholar]
- Sato M, Suemori H, Hata N, Asagiri M, Ogasawara K, Nakao K, Nakaya T, Katsuki M, Noguchi S, Tanaka N, et al. Distinct and Essential Roles of Transcription Factors IRF-3 and IRF-7 in Response to Viruses for IFN-α/β Gene Induction. Immunity. 2000;13:539–548. doi: 10.1016/s1074-7613(00)00053-4. [DOI] [PubMed] [Google Scholar]
- Sauer JD, Sotelo-Troha K, von Moltke J, Monroe KM, Rae CS, Brubaker SW, Hyodo M, Hayakawa Y, Woodward JJ, Portnoy DA, et al. The N-ethyl-N-nitrosourea-induced Goldenticket mouse mutant reveals an essential function of Sting in the in vivo interferon response to Listeria monocytogenes and cyclic dinucleotides. Infect Immun. 2011;79:688–694. doi: 10.1128/IAI.00999-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoggins JW, MacDuff DA, Imanaka N, Gainey MD, Shrestha B, Eitson JL, Mar KB, Richardson RB, Ratushny AV, Litvak V, et al. Pan-viral specificity of IFN-induced genes reveals new roles for cGAS in innate immunity. Nature. 2014;505:691–695. doi: 10.1038/nature12862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz S, West TE, Boyer F, Chiang WC, Carl MA, Hood RD, Rohmer L, Tolker-Nielsen T, Skerrett SJ, Mougous JD. Burkholderia Type VI Secretion Systems Have Distinct Roles in Eukaryotic and Bacterial Cell Interactions. PLOS Pathog. 2010;6:e1001068. doi: 10.1371/journal.ppat.1001068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon P, Markiel A, Ozier O, Baliga NS, Wang JT, Ramage D, Amin N, Schwikowski B, Ideker T. Cytoscape: a software environment for integrated models of biomolecular interaction networks. Genome Res. 2003;13:2498–2504. doi: 10.1101/gr.1239303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suthar MS, Ramos HJ, Brassil MM, Netland J, Chappell CP, Blahnik G, McMillan A, Diamond MS, Clark EA, Bevan MJ, et al. The RIG-I-like receptor LGP2 controls CD8(+) T cell survival and fitness. Immunity. 2012;37:235–248. doi: 10.1016/j.immuni.2012.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takeda K, Tsutsui H, Yoshimoto T, Adachi O, Yoshida N, Kishimoto T, Okamura H, Nakanishi K, Akira S. Defective NK cell activity and Th1 response in IL-18-deficient mice. Immunity. 1998;8:383–390. doi: 10.1016/s1074-7613(00)80543-9. [DOI] [PubMed] [Google Scholar]
- Trapnell C, Roberts A, Goff L, Pertea G, Kim D, Kelley DR, Pimentel H, Salzberg SL, Rinn JL, Pachter L. Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat Protoc. 2012;7:562–578. doi: 10.1038/nprot.2012.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamamoto M, Sato S, Hemmi H, Hoshino K, Kaisho T, Sanjo H, Takeuchi O, Sugiyama M, Okabe M, Takeda K, et al. Role of adaptor TRIF in the MyD88-independent toll-like receptor signaling pathway. Science. 2003;301:640–643. doi: 10.1126/science.1087262. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Liu T, Meyer CA, Eeckhoute J, Johnson DS, Bernstein BE, Nusbaum C, Myers RM, Brown M, Li W, et al. Model-based analysis of ChIP-Seq (MACS) Genome Biol. 2008;9:R137. doi: 10.1186/gb-2008-9-9-r137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Release of cytokines IL-1β, IL-6, TNF and LDH in BMDMs after infection with F. novicida (MOI, 100).
(B) Release of IL-6, TNF, KC and LDH in BMDMs transfected with poly(dA:dT).
(C) Release of IL-1β, IL-6, TNF and LDH in BMDMs primed with LPS and stimulated with ATP.
(D) Release of IL-6, TNF, KC and LDH in BMDMs primed with LPS and transfected with LPS.
NS, not significant; **P < 0.01 and ***P < 0.001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are from 3 independent experiments (mean ± SEM).
(A) Flow cytometric analysis of side-scattered light (SSC), forward-scattered light (FSC); and expression of F4/80 and CD11b of BMDMs generated from WT and Irf8−/− mice.
(B) Immunoblot analysis of IRF8, GBP2, GBP5, and β-actin (loading control) in BMDMs at various times after infection with F. novicida.
(C–E) Immunoblot analysis of caspase-1 in BMDMs that were infected with multiple MOIs of S. Typhimurium, P. aeruginosa, or B. thailandensis.
(F) Immunoblot analysis of IRF8 in BMDMs stimulated with LPS or infected with S. Typhimurium or B. thailandensis.
Data are representative of 2 independent experiments.
(A) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with S. Typhimurium (MOI, 0.1).
(B and C) Microscopic images and cell death analysis of BMDMs infected with ΔfliCΔfljB (MOI, 1) or ΔSPI-2 (MOI, 1).
(D) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with P. aeruginosa (MOI, 1).
(E) Release of IL-1β, TNF, IL-6 and LDH in BMDMs after infection with B. thailandensis (MOI, 1).
Scale bars, 100 μm (B), NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are representative of 3 (B) or from 3 (A and C–E) independent experiments (mean ± SEM).
(A) Immunoblot analysis of caspase-1 in WT BMDMs transfected with a control siRNA or Irf8 siRNA and then infected with S. Typhimurium (MOI, 0.1) for 4 h or F. novicida (MOI, 100) for 20 h. Nlrc4−/− (left) or Aim2−/− (right) BMDMs were used as controls.
(B) Relative expression of the gene encoding IRF8 in WT BMDMs transfected with a control siRNA or Irf8 siRNA.
(C) Immunoblot analysis of caspase-1 in BMDMs that were infected with S. Typhimurium (MOI, 0.1) and collected after 4 h.
(D) Microscopic images of BMDMs that were infected with S. Typhimurium (MOI, 0.1).
(E) Immunoblot analysis of caspase-1 in BMDMs that were transfected with different doses of flagellin.
(F and G) Release of IL-1β and KC in BMDMs treated with DOTAP, transfected with flagellin (DOTAP + Flgn), or treated with flagellin (Flgn).
(H and I) Immunoblot analysis of caspase-1 and assessment of IL-18 levels in BMDMs untreated or transfected with flagellin.
(J) Microscopic images of BMDMs transfected with PrgI (DOTAP + PrgI) or PrgJ (DOTAP + PrgJ).
Scale bars, 100 μm (D and J), NS, not significant; *P < 0.05, **P < 0.01, ***P < 0.001 and ****P < 0.0001 (One-way ANOVA with Dunnett’s multiple comparisons test). Data are from 3 (F and G) or 2 (I) or representative of 2 (A–E, H, and J) independent experiments (mean ± SEM).
RT-PCR analysis of genes encoding NAIPs and NLRC4 in BMDMs, normalized to that of the gene encoding HPRT.
Data are from 2 independent experiments (mean ± SEM).
(A) Survival of 8-week-old WT (n=11) and Irf8−/− (n=7) mice infected intranasally with 5 × 104 CFU of B. thailandensis.
(B) Bacterial burden in the lungs, liver and spleen of WT (n=10) and Irf8−/− (n=9) mice on day 2 after infection as (A).
(C) Analysis of IL-18 in the lungs, liver, spleen, and serum collected from WT (n=10) and Irf8−/− (n=9) mice on day 2 after infection as (A).
(D) H&E staining of lungs collected from WT and Irf8−/− mice on day 2 after infection as (A).
(E–H) RT-PCR analysis of genes encoding NAIPs and NLRC4 in spleen and lungs collected from WT (n=10) and Irf8−/− (n=9) mice before (day 0) and after infection (day 2) as (A), presented relative to that of the gene encoding HPRT.
Scale bars, 250 μm (D), NS, not significant; *P < 0.05, **P < 0.001, ***P < 0.0001 and ****P < 0.0001 (log-rank test [A] or two-tailed t test [B and C] or Two-way ANOVA with Tukey’s multiple comparisons test [E–H]). Data are representative of 2 (D) or from 2 (A–C and E–H) independent experiments.
(A) Blood cell counts from peripheral blood of WT (n=10), Irf8−/− (n=6), and Nlrc4−/− (n=10) mice on day 3 after intraperitoneal infection with 103 CFU of S. Typhimurium.
(B) Blood cell counts from peripheral blood of WT (n=10) and Irf8−/− (n=9) mice on day 2 after intranasal infection with 5 × 104 CFU of B. thailandensis.
NS, not significant; *P < 0.05, **P < 0.01 and ***P < 0.001 (One-way ANOVA with Dunnett’s multiple comparisons test [A] or two-tailed t test [B]). Data are from 1 independent experiment.