Abstract
Introduction
U.S. black women have the highest rates of obesity and report frequent binge eating behaviors. To our knowledge, no intervention research has aimed to treat binge eating specifically among black women. The purpose of this study was to investigate the feasibility and preliminary effect of Appetite Awareness Treatment (AAT), an 8-week cognitive-behavioral binge eating intervention, among black women with obesity, and who report binge eating.
Methods
Participants (N=31), had a mean (±SD) age of 48.8 ±12.8 years, a body mass index of 33.7 ± 3.9 kg/m2, and reported at least one binge or loss of control (LOC) eating episode monthly over the last three months. Using a randomized controlled trial design, black women were randomized to AAT or a wait-list control group (WAIT) group. We examined recruitment, attendance, retention, and adherence. Linear mixed models explored preliminary differences between the AAT and WAIT on the primary outcome variables of binge eating and eating self-efficacy measured at baseline and 8-weeks.
Results
Approximately one-third of screened participants were eligible and did enroll. Participants completed 55% of homework assignments, and attended 59% of intervention sessions. Retention to AAT was 87.5%. Compared to participants in the WAIT group, AAT participants had greater decreases in binge eating scores and greater improvements in eating self-efficacy scores at the end of Week 8.
Conclusion
Results suggest that AAT is feasible among black women with binge eating behaviors, with evidence of preliminary efficacy, providing a rationale for a trial of AAT in a larger sample of black women.
Keywords: binge eating, black, African-American, weight gain prevention, obesity
1. Introduction
Over 70% of US adults are impacted by overweight or obesity; however, black women are over represented in this group. Current estimates indicate that 82% of black women are affected by overweight or obesity, compared to only 63.5% of White women (National Center for Health Statistics, 2017). Many lifestyle behavioral interventions designed to encourage participants to lose weight, adopt healthy diets, and increase physical activity have been developed and evaluated (Diabetes Prevention Program Research, 2002; Fitzgibbon et al., 2010; Johns, Hartmann-Boyce, Jebb, Aveyard, & Behavioural Weight Management Review, 2014; McTigue, Hess, & Ziouras, 2006). Black women, however, have not generally fared well. Not only has their inclusion in treatment trials been limited, but when they participate, they lose less weight on average than their White counterparts (Goode, Styn, Mendez, & Gary-Webb, 2017; Wingo, Carson, & Ard, 2014).
Recently, investigators have observed that a significant number of Black women may have untreated eating disorders and mental health concerns that increase their vulnerability to obesity and contribute to their limited success in standard weight-loss treatment (Adamus-Leach et al., 2013; Harrington, Crowther, Henrickson, & Mickelson, 2006; Harrington, Crowther, & Shipherd, 2010; Hrabosky & Grilo, 2007; Lydecker & Grilo, 2016; Marcus, Bromberger, Wei, Brown, & Kravitz, 2007). A particular behavior pattern of concern is binge eating, as it is associated with higher levels of obesity (Hudson, Hiripi, Pope, & Kessler, 2007; Yanovski, 2003). Binge eating is described by having episodes of eating large amounts, i.e. more than a typical person would eat in a discrete period, while concurrently experiencing a sense of loss of control over eating (LOC) (American Psychiatric Association, 2013). Susceptibility to binge eating places one at risk to develop Binge Eating Disorder (BED), and BED is strongly associated with other co-morbid conditions of serious concern, including that of severe obesity, substance disorders, and depression (Guss, Kissileff, Devlin, Zimmerli, & Walsh, 2002; Hudson et al., 2007; Pike, Dohm, Striegel-Moore, Wilfley, & Fairburn, 2001; Striegel-Moore, Wilfley, Pike, Dohm, & Fairburn, 2000).
Among Black women, frequent binge eating has been reported at similar (Fitzgibbon et al., 1998; Franko et al., 2012; Jarosz, Dobal, Wilson, & Schram, 2007) or rates higher than reported in White women (Lydecker & Grilo, 2016; Marques et al., 2011). In studies where racial differences were reported, binge eating (regardless of diagnosis) among Black women has been observed at 4.5–4.8%, compared to only 2.5–2.6% in Non-Latino White women (Marques et al., 2011; Striegel-Moore et al., 2000). Moreover, among Black women with severe obesity (BMI ≥40), rates of binge eating were found to be higher than 30% (Mazzeo, Saunders, & Mitchell, 2005). Black women may use binge eating as a way to regulate emotion and as a strategy to cope with various traumas, including poverty, sexual abuse, and depressive symptoms (Adamus-Leach et al., 2013; Harrington et al., 2010; Thompson, 1992). Despite reporting similar or greater levels of eating disorder pathology, Black women, however, are far less likely to seek eating disorder treatment when compared to non-Hispanic White women (Marques et al., 2011; Striegel-Moore et al., 2003; Wilfley, Pike, Dohm, Striegel-Moore, & Fairburn, 2001). Thus, current reports of binge eating in Black women may not accurately reflect the scope of the problem.
Several psychological and behavioral interventions (e.g., Cognitive Behavioral Therapy (CBT), Interpersonal Psychotherapy; behavioral weight loss treatment) are effective in decreasing binge eating in adults (Hilbert, Hildebrandt, Agras, Wilfley, & Wilson, 2015; Wilson, Wilfley, Agras, & Bryson, 2010). There is, however, scant intervention research conducted among Black women who report binge eating, and this population has been severely underrepresented in clinical trials (Franko et al., 2012; Mama et al., 2015; Thompson-Brenner et al., 2013). A specific CBT intervention, Appetite Awareness Training (AAT) (Craighead, 2006), which targets both binge and overeating, may hold particular promise with this population. The primary focus of the intervention is to provide specific training to help participants recognize and then utilize their biological signals of hunger and satiety to guide eating decisions. Because Black women have reported difficulty being aware of internal cues of hunger and satiety(Willig, Richardson, Agne, & Cherrington, 2014), and may experience cultural norms that normalize overeating as a coping mechanisim (Beauboeuf-Lafontant, 2003; Jackson, Knight, & Rafferty, 2010; Lovejoy, 2001; Thompson, 1992), the specific training provided in AAT may be particularly beneficial. AAT has been successful in helping participants diagnosed with BED and bulimia nervosa reduce binge eating, overeating, and urges to eat in response to non-appetite stimuli (Allen & Craighead, 1999; Dicker & Craighead, 2004; Hill, Craighead, & Safer, 2011). Moreover, AAT has demonstrated similar levels of binge reduction and weight gain prevention as other CBT treatments, but the samples have been primarily White, adult women (Allen & Craighead, 1999; Blumenthal et al., 2010; Craighead, 2006; Dicker & Craighead, 2004).
1.1 Study rationale and aims
While Black women may be less likely to seek treatment for disordered eating behaviors, there is ample evidence to suggest their willingness to participate in weight management programs (Bronner & Boyington, 2002; Fitzgibbon et al., 2012; Marques et al., 2011; Pike et al., 2001; Wingo et al., 2014). Thus, developing appropriate interventions to treat binge eating behaviors that may augment existing weight management interventions may be important next steps in the prevention and treatment of obesity in this population. Thus, the purpose of this study was to test AAT in a sample of Black women with overweight or obesity, and also report binge eating, and examine both the feasibility and preliminary effects of an 8-week, community-based AAT intervention. Because AAT had never been tested in this population before, we felt it was important to determine the feasibility of the original intervention (e.g., no cultural tailoring). Using a randomized study design with a wait-list control (a delayed intervention control group), we examined the feasibility of recruitment, attendance, adherence to homework assignments, and retention in the study. Additionally, we examined the preliminary effects of the intervention by exploring differences between the two conditions on the primary variables, binge eating and eating self-efficacy, and the secondary variables, weight, blood pressure, waist circumference, and depressive symptoms.
2. Methods
2.1 Inclusion Criteria
Individuals were eligible if they identified as non-Latino Black women, over 18 years of age, with a BMI between 25–40 kg/m2 and reported experiencing at least one binge eating episode monthly (within the last 3 months). The rationale for the upper limit on BMI was to explore whether AAT may be viable as an intervention to prevent weight gain, progression to Class III obesity, in addition to the exacerbation of binge eating.
2.2 Exclusion Criteria
Individuals were excluded if they were currently pregnant, in substance abuse treatment, currently involved in a weight reduction program, had a history of anorexia, were purging, or self-reported intravenous drug use or the consumption of >4 alcoholic beverages/day. The rationale for these exclusion criteria was that the presence of these conditions may interfere with adhering to the intervention protocol or completing the study.
2.3 Recruitment
Participants were recruited to the study by face-to-face methods (e.g, community events) and with flyers and bulletin board announcements in urban community centers, doctor’s offices, and churches in the Greater Pittsburgh Metropolitan Area between August 2015 and February 2016. Additionally, we advertised and recruited on the research participant registry located at the University of Pittsburgh. In study advertisements, potential participants were asked if they “felt out of control around food” and wanted help to “lose weight or to stop gaining weight”.
2.4 Appetite Awareness Training
AAT was comprised of eight, 60-minute group sessions (Table 1) (Craighead, 2006). The goal of AAT is to enable participants to re-learn and use their stomach’s hunger signals and begin to obey and monitor functions of satiety (Craighead, 2006). Participants are encouraged to discover hunger signals, avoid allowing themselves to become too hungry, and to develop appropriate coping skills to manage urges to eat when not hungry (Craighead, 2006). In addition, participants were assigned homework assignments to self-monitor adhering to their appetite. On a paper form, participants were asked to record each eating episode, and rate hunger and satiety on a scale of 1 (very hungry) to 7 (overly full) at the start and end of each episode.
Table 1.
AAT Session Content
| Session | Content |
|---|---|
| 1. Introduction to AAT | Participants discussed past experience with dieting, and explored their history with preferences for food, fullness, and their eating patterns. Participants were introduced to appetite monitoring, and developing patterns of regular eating. |
| 2. Beginning Appetite Monitoring | Participants received continued instruction on appetite monitoring, and further training on using biological signals of hunger and satiety to guide eating decisions. Participants were trained to use daily forms to self-monitor their appetite before and after each eating episode. |
| 3. Learning the AAT Model for Eating | Participants received psychoeducation on the four paths of eating (e.g, binge eating/getting stuffed, ignoring fullness, restrictive eating, and normal eating), and were provided instruction on how to return to the normal path after an episode of “getting off track.” |
| 4. Take Back your Power | Participants received training on remaining in control of eating behaviors in spite of external cues for eating. |
| 5. Effective Emotional Eating | Participants received instruction to manage strong emotions, and urges to eat when not hungry, including guidance for the development of alternative, non-eating coping skills. |
| 6. Food Awareness Training | Participants received instruction about the importance of monitoring food type, and awareness of how certain foods feel in the body after consumption. Participants also received information about low-calorie density foods that may be alternatives to current high-density foods in their diet. |
| 7. Self-Coaching for Life | Participants received support to eat mindfully without reliance on the written forms. Participants were also provided instruction on tools for weight management (e.g., regular self-weighing) after group session ended. |
| 8. Review of Progress and Celebration | Participants reviewed lessons learned about self-monitoring appetite, and were provided support to troubleshoot any concerns that might derail making continued progress on their own. |
2.5 Procedures
Study approval was provided by the Institutional Review Board at the University of Pittsburgh. Potential participants were screened for preliminary eligibility by phone or a web-based survey generated by using Qualtrics software (Qualtrics, 2017). Eligible participants were given a date and time to meet with the Principal Investigator (PI) to complete a baseline assessment, which was held at a local church, community agency, or in the participant’s home. At this appointment, participants provided informed consent, and were interviewed to verify the presence of at least one monthly episode of binge eating over the last 3 months as determined by the overeating section of the Eating Disorder Examination (Fairburn & Cooper, 1993). Participants also had their height, weight, blood pressure, and waist circumference measured at this visit, and completed self-report measures.
Eligible participants were randomly assigned to one of the two treatment conditions: AAT or delayed intervention control group (WAIT). Intervention sessions were held at either a church or local community agency. Following the eight-week AAT intervention, participants completed their final assessment. WAIT participants received the intervention after the completion of the 8-week assessment. Participants were compensated with a $25 gift card for completing assessments at baseline and 8-weeks.
2.6 Group leaders
AAT was led by the PI and a lay health advisor. At the time of study, the PI was a PhD student in Social Work; the developer of AAT provided supervision. A lay health advisor, a member of the community who expressed interest in the study, but did not have any formal research training, served as an intervention assistant, and was trained in the AAT intervention by the PI.
2.7 Measures
2.7.1 Eating Disorder Examination – Overeating Section (EDE) (Fairburn & Cooper, 1993)
Participants completed the overeating section of this semi-structured interview to assess objective binge episodes (OBE) (consumption of an objectively large amount of food and LOC), and the presence of LOC eating (presence of subjective and/or objective binge episodes) within the last 3 months. The EDE has well-established validity, reliability, and internal consistency (Cronbach’s alpha = .67–.90); the EDE is considered the “gold standard” for the assessment of binge eating (Cooper, Cooper, & Fairburn, 1989; Guest, 2000).
2.7.2 Sociodemographic Questionnaire
This questionnaire collected the following data: age, race/ethnicity; marital status, education, neighborhood residence, employment status, household size, religious background, and income.
2.7.3 Height and Weight
Weight was measured on a digital scale and height on a portable stadiometer. BMI was calculated as weight in kilograms divided by height in meters squared (kg/m2).
2.7.4 Waist Circumference
Participants were measured twice with a Gullick II measuring tape. If the two values are within 2cm of each other, they were averaged to obtain a mean value; if not, measurements were taken again until they were within 2cm.
2.7.5 Blood pressure
This assessment was measured using a GE Dinamap Procare Auscultatory 400 Multi-Parameter Patient Monitor with the participant in a sitting position after at least a one-minute rest period.
2.7.6 Binge Eating Scale (BES) (Gormally, Black, Daston, & Rardin, 1982)
This 16-item self-report questionnaire assessed behavior and feelings associated with a binge-eating episode. Individuals rated responses on a four-item scale, ranging from 0 (no/low severity of binge eating symptoms) to 3 (high severity of binge eating symptoms). Scores were calculated as a sum of items; higher scores indicated greater severity of binge eating behaviors. Presence of severe binge eating is associated with scores ≥27, and scores ≤17 indicate mild or no binge eating. The BES has good psychometric properties, and has been shown to have high internal consistency in samples of black women, with a Cronbach’s alpha of .88 (Duarte, Pinto-Gouveia, & Ferreira, 2015; Harrington et al., 2006; Wilson et al., 2012).
2.7.7 Beck Depression Inventory (BDI) (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961)
This 21-item questionnaire measures the severity of depressive symptoms. Individuals rated their response on a four- item scale (from 0 to 3), with larger numbers indicating greater intensity. In the BDI, Cronbach’s alpha has been observed at .86–.88 (Beck & Steer, 1984).
2.7.8 Weight Efficacy Life-Style Questionnaire (WEL) (Clark, Abrams, Niaura, Eaton, & Rossi, 1991)
The WEL assesses confidence in resisting eating in varied situations and in different emotional states, with higher scores indicating more confidence. Responses to this 20-item questionnaire are rated on a 10-point scale from 0 (not confident) to 9 (very confident). The questionnaire has been tested among samples of Black women (Dutton, Martin, Rhode, & Brantley, 2004), and the Cronbach’s alpha ranged from .70–.90.
2.7.9 Adherence to Homework Assignments
Adherence was assessed by the number of homework assignments (out of five) that were completed (reported self-monitoring and returned assignment to class the next week).
2.8 Analytic Strategy
To determine the feasibility of recruiting Black women with overweight or obesity to participate in the AAT intervention, we examined response to recruitment strategies, percent of participants who met inclusion criteria and agreed to participate, attendance, compliance with homework, and study retention. Although this was a feasibility study, and not adequately powered to determine outcome differences between groups, we did conduct a preliminary investigation of changes between conditions. Linear mixed-effects models evaluated the impact of the AAT intervention on the primary outcomes of binge eating and eating self-efficacy, and the secondary outcomes of depressive symptoms, waist circumference, blood pressure, and weight. We used an intent-to-treat approach to analysis and all participants who were randomized were included in the final analyses. Participants who did not attend the final assessment had their baseline data carried forward, assuming no change in the outcome variable. A completers analysis, including only those who completed both assessments, was also performed to determine if there were any differences in results. All significant outcomes remained the same with both analyses (intent-to-treat and completers). Additionally, residuals were examined for normality after linear mixed modeling analyses were completed. Between-group effect sizes (Cohen’s d) were calculated by observing the difference between the means of the AAT and the WAIT group on each outcome variable. Due to the presence of multiple comparisons (n=9) and the possibility of a false discovery, the Bonferroni Correction was used. The new p-value was set to p=.005.
3. Results
3.1 Feasibility: Recruitment
Participants were 31 Black women, who had a mean (±SD) age of 48.8 ±12.8 years, and a BMI of 33.7 ± 3.9 kg/m2 (Table 2). At baseline, participants reported mean BES score of 22.6 ± 7.0, monthly OBE episodes of 2.8 ± 5.5, and monthly LOC eating episodes of 16.8 ± 15.5. Four waves of participants were randomized to either AAT or WAIT.
Table 2.
Baseline characteristics of the study population (N=31)
| Measure | AAT (n=16) | Wait-List Control (n=15) | p-value |
|---|---|---|---|
| Age | 48.44 ± 12.47 | 49.20 ± 13.56 | .87 |
| Education (yrs.) | 14.19 ± 2.64 | 15.73 ± 2.71 | .12 |
| BMI | 33.19 ± 4.19 | 34.24 ± 3.64 | .46 |
| Waist Circumference | 121.88 ± 11.62 | 124.43 ± 13.40 | .49 |
| Systolic Blood Pressure | 121.88 ± 11.62 | 124.43 ± 13.40 | .57 |
| Diastolic Blood | 81.16 ± 7.18 | 82.20 ± 11.60 | .76 |
| Pressure | |||
| Income (No., %) | .53 | ||
| $<29,999 | 5 (31.25) | 4 (26.67) | |
| $30–69,999 | 4 (25.00) | 7 (46.67) | |
| $>70,000 | 6 (37.50) | 4 (26.67) | |
| Marital Status (No., %) | .59 | ||
| Never Married | 5 (31.25) | 7 (46.67) | |
| Currently Married | 7 (43.75) | 5 (33.33) | |
| Divorced | 3 (18.75) | 2 (13.33) | |
| Other | 1(6.25) | 1 (6.60) |
Participants were referred by the research participant registry at the University of Pittsburgh, (42%), face-to-face recruitment events (35%), word of mouth (10%), flyer (10%), and Facebook (3%). After the initial screening, 33.3% (n=33) were eligible, 55.5% (n=55) were not eligible, and 11% (n=11) declined to participate (Figure 1).
Figure 1.
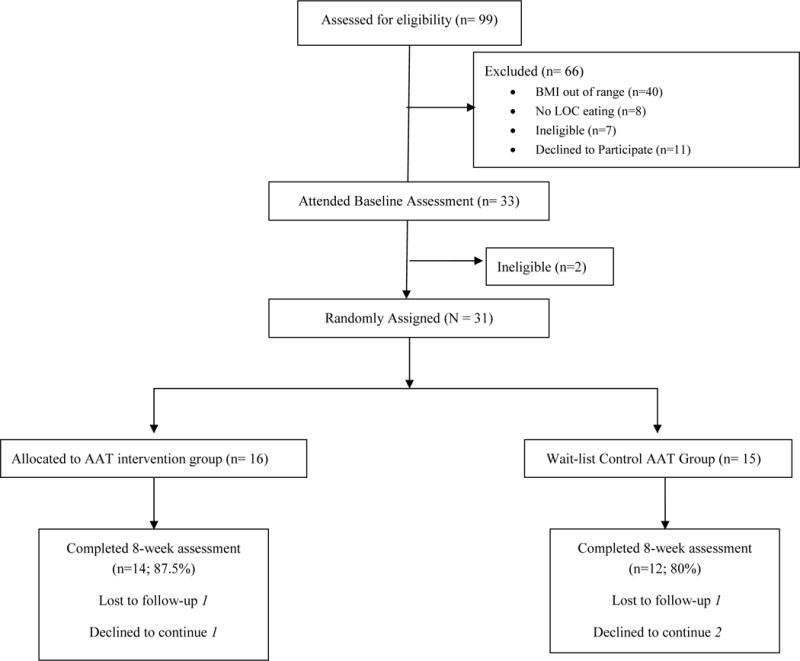
CONSORT flow diagram
3.2 Feasibility: Participant Attendance, Adherence, and Attrition
On average, AAT participants (n=16) attended 4.7 (59%) of the 8 sessions, compared to 6.6 (82%) of the 8 sessions in the WAIT group (n=15). In sum, 58% of participants attended at least 75% of the weekly sessions. AAT participants completed 2.73/5 (55%) of homework assignments, compared to 3.12/5 (63%) in WAIT. Within the total sample, 84% (n=26) of participants completed assessments at 8 weeks.
3.3 Secondary Outcomes
Compared to wait-list control, AAT participants demonstrated reductions from baseline to 8 weeks on BES score (AAT: −5.87 (0.61); WAIT: 0 (0.01); group × time; p=.002; d=.52) and increases in WEL score (AAT: +25.14 (6.67); WAIT: −1.27 (4.15); group × time; p=.002; d=1.06). There were significant time effects for objective binge eating episodes (p=.003), LOC eating episodes (p<.001), and BDI score (p=.003). There were no significant group effects, time effects, or group × time interactions for weight, waist circumference, and blood pressure. (See Table 3).
Table 3.
Outcome Differences between Treatment Groups at Week 8
| Outcome Variable | AAT (n=16) (mean ± sd) |
WAIT (n=15) (mean ± sd) |
Group | Time | Group × Time |
|---|---|---|---|---|---|
| Objective Binge Eating (episodes per month) | |||||
| Baseline | 2.19 ± 3.58 | 3.47 ± 7.06 | p=.644 | p=.003 | p=.097 |
| Week 8 | 0.25 ± .683 | 2.80 ± 7.24 | |||
| Binge Eating Scale | |||||
| Baseline | 23.75 ± 7.33 | 21.33 ± 6.60 | p=.336 | p<.001 | p=.002 |
| Week 8 | 17.88 ± 6.72 | 21.33 ± 6.61 | |||
| LOC Eating (episodes per month) | |||||
| Baseline | 18.82 ± 17.12 | 15.11 ± 14.08 | p=.558 | p<.001 | p<.01 |
| Week 8 | 2.31 ± 2.81 | 7.81 ± 9.79 | |||
| Weight Efficacy Lifestyle Questionnaire | |||||
| Baseline | 80.77 ± 31.31 | 70.80 ± 36.08 | p=.411 | p<.001 | p=.002 |
| Week 8 | 106.81 ± 37.98 | 69.53 ± 31.93 | |||
| Weight (lbs.) | |||||
| Baseline | 196.70 ± 20.10 | 203.16 ± 31.31 | p=.552 | p=.378 | p=.521 |
| Week 8 | 195.88 ± 29.34 | 203.20 ± 31.19 | |||
| Waist Circumference (cm.) | |||||
| Baseline | 103.56 ±10.36 | 106.60 ± 13.47 | p=.479 | p=.128 | p=.791 |
| Week 8 | 101.99 ±9.54 | 104.65 ± 10.84 | |||
| Systolic Blood Pressure | |||||
| Baseline | 121.88 ± 11.62 | 124.43 ± 13.41 | p=.570 | p=.920 | p=.652 |
| Week 8 | 122.19 ± 17.63 | 122.73 ± 11.98 | |||
| Diastolic Blood Pressure | |||||
| Baseline | 81.16 ± 7.18 | 82.20 ± 11.60 | p=.762 | p=.657 | p=.444 |
| Week 8 | 80.19 ± 11.08 | 83.63 ± 11.27 | |||
| Beck Depression Inventory | |||||
| Baseline | 12.73 ± 9.15 | 14.73 ± 12.63 | p=.717 | p=.003 | p=.057 |
| Week 8 | 8.47 ± 11.54 | 13.87 ± 10.38 |
4. Discussion
This study examined the feasibility and preliminary effectiveness of Appetite Awareness Treatment (AAT) to reduce binge eating among Black women with overweight or obesity. Recruitment was feasible, and one-third of those who expressed interest, were eligible, and enrolled in the study. Helpful recruitment sites included face-to-face community events, and a university-based research registry. Participants attended approximately two-thirds of all sessions and completed over half of the homework assignments. Moreover, AAT participants exhibited reductions in binge eating scores and improvements in eating self-efficacy, suggesting that this approach holds promise for future research.
A great deal is unknown about the binge eating behaviors of Black women. Binge eating remains undertreated within Black women, and they have been severely underrepresented in clinical trials (Franko et al., 2012; Thompson-Brenner et al., 2013). At baseline, both groups had a mean BES score (22.98±6.98) that indicated the presence of moderate binging activity. However, at 8 weeks, participants in the AAT group had decreased their binge eating score (−5.87), compared to no change observed among participants in the WAIT group. Participants for this study did not have to meet full diagnostic criteria for BED; it is not surprising that they had slightly lower scores on the BES at baseline, and did not exhibit the same degree of score reduction between baseline and 8 weeks when compared to 8-week AAT conducted in a sample of predominately White women (mean age: 21±1.2 years) diagnosed with BED (Allen & Craighead, 1999). Additionally, due to our conservative p-value (.005), change in LOC eating episodes was not statistically significant. However, it is still noteworthy to report that the AAT group demonstrated a greater decrease in their LOC eating episodes (18.8 to 2.3). Thus, we conclude that AAT has potential as a treatment to reduce binge and LOC eating in Black women with overweight or obesity.
Similarly, the current sample reported fewer OBEs compared to prior reports of Black women who were treatment-seeking adults diagnosed with DSM-IV-defined BED (Franko et al., 2012; Lydecker & Grilo, 2016; Pike et al., 2001). As part of EDE scoring, participants needed to endorse the consumption of an objectively large amount of food, and scorers need to have some knowledge on the norms for a social group, and/or what would be the usual amount eaten under the circumstances (Fairburn & Cooper, 1993). Because cultural norms may permit consumption of large portions as acceptable(Beauboeuf-Lafontant, 2003; Thompson, 1992), there may be some racial and cultural considerations that need further exploration in the assessment and the measurement of binge eating; of recent, these differences in the presentation of binge and LOC eating are underexplored (Goldschmidt, 2017).
Within our study, 58% of participants attended at least 75% of the weekly sessions; attendance within this study was comparable to what has been observed among Blacks in other group-based behavioral weight loss interventions. For example, within the Weight Loss Maintenance trial, 57% of Black men and 51% of Black women attended over 80% of sessions during the 6-month weight loss program (Hollis et al., 2008). Additionally, within the first 6 months of the ORBIT trial, participants attended an average of 53% of classes, with approximately 60% of participants attending at least half of all classes offered (Fitzgibbon et al., 2010).
Scheduling intervention sessions in the evening and in familiar community locations (e.g. church, neighborhood association) may have increased accessibility and contributed to the attendance and study retention in the present study. Due to their community relevance, churches have great potential to reduce health disparities, and are often an excellent place to hold interventions when engaging Black participants (Campbell et al., 2007; Yeary et al., 2015). We held the intervention in two different neighborhoods that were both easily accessible by public transportation. Additionally, intervention sessions were held on a weekday, during the evening. Moreover, we provided participants the flexibility of having their assessments done on site and/or at their individual home. In sum, these accommodations may have reduced the burden on participants, and may have made fully participating in the intervention feasible.
Another positive outcome of this study was the increase in eating self-efficacy observed in our sample. At baseline, both groups had a mean eating self-efficacy score that was relatively low. By the end of 8 weeks, the AAT group had significantly improved their score (+26.0 ± 6.7), compared to no change in the WAIT group (−1.3 ± 4.2). Improving self-efficacy is an important goal of behavioral weight loss interventions; past evidence has found the increase in eating and diet self-efficacy was associated with improved dietary intake, physical activity, and weight loss (Hays, Finch, Saha, Marrero, & Ackermann, 2014; Nezami et al., 2016). Among Black women, however, investigators have observed a decrease in self-efficacy over time, and its association with less weight loss and/or weight gain (Martin, Dutton, & Brantley, 2004; Murphy & Williams, 2013). Thus, based on our results, AAT demonstrates significant promise to assist Black women to improve their confidence to resist eating in varied emotional states and situations.
4.1 Lessons Learned
Of all who expressed interest in the study, approximately 40% were not eligible due to possessing a BMI above the study threshold, which was a significant barrier to recruitment. Because of the desire to examine AAT’s potential as an intervention for weight gain prevention, the BMI criterion was restricted to women who did not exceed Class II obesity. Thus, future research should investigate the feasibility of this intervention among women with a higher BMI, where one may expect more severe binge eating patterns. While treating binge eating in women with overweight may serve to prevent the development of obesity, with over 54% of Black women meeting established criteria for obesity (Hales, Carroll, Fryar, & Ogden, 2017), there is clear evidence for further exploration of binge eating behaviors among women with severe obesity.
We also reflected on the amount of homework that was completed by participants. Because a little over half of the homework was completed, future research should assess the utility of the current homework structure. Potential barriers may have been the structure of the form, and/or the use of a paper form. In recent trials, investigators used technology to reduce the burden of self-monitoring (Burke et al., 2011; Burke et al., 2016); a change to an electronic version of self-monitoring may be a viable tool in future AAT intervention development.
These results provide further evidence to increase the focus on eating behaviors within our weight management interventions. With 8-weeks of training to modify specific eating behaviors (e.g., improve reliance on biological signals of hunger and satiety), participants increased their eating self-efficacy, and reduced their binge eating, and loss of control eating episodes. If individuals do not fully understand the mechanisms of eating (hunger, satiety, importance of regular eating episodes), we may be naïve to believe they will be motivated to make long-term changes in their eating patterns. Part of the reason for relapse within behavioral weight loss interventions may be that participants still have episodes of binging, overeating, and emotional eating behaviors that have not been adequately addressed. Future eating behavior intervention studies may be of great benefit to increase our understanding of the necessary components of effective treatments for obesity and the prevention of weight gain in Black women.
4.2 Strengths and Limitations
There were several limitations to this study. First, the sample was small and was predominately comprised of Black women who were over the age of 40. Second, the absence of an active control condition limits our ability to determine the specific factors associated with change during the study. Additionally, the restriction on the BMI range limits the generalizability of findings to this population. Moreover, the use of self-report measures to assess binge eating, eating self-efficacy, and depressive symptoms, includes a risk of social desirability, recall bias, and errors in self-observation. Furthermore, the PI was responsible for the conduct of the intervention and all assessments. This may increase the risk of bias of study findings. Finally, there was also no follow-up to determine if changes in eating behaviors were sustained after the completion of the 8-week study.
Despite these limitations, this study had several strengths. First, to the best of our knowledge, this is the first intervention study to report treatment outcomes specific to Black women with overweight or obesity, and report binge eating behaviors. In addition, this study demonstrated the feasibility of recruiting Black women to participate in a randomized clinical trial in a community-based setting, and provided helpful information to guide further interventions.
5. Conclusion
The results of this study indicate the viability of AAT as a treatment for binge eating for Black women with overweight and obesity, and support the recommendation for a longer term, adequately powered pilot study to document the effectiveness of the AAT intervention to reduce binge eating, and prevent weight gain in Black women. Though preliminary, the current results indicate that participating in AAT was feasible, and may reduce binge eating and increase self-efficacy. Future studies, however, may consider widening the inclusion criteria, particularly in the BMI range. Moreover, making modifications to the intervention homework, and considering e-health methods to improve homework engagement may have benefit to this population.
Highlights.
AAT is feasible in black women with binge eating behaviors.
Participants completed over 50% of homework assignments.
AAT participants had greater reductions in binge eating behaviors.
AAT participants had greater improvements in eating self-efficacy.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adamus-Leach HJ, Wilson PL, O’Connor DP, Rhode PC, Mama SK, Lee RE. Depression, stress and body fat are associated with binge eating in a community sample of African American and Hispanic women. Eat Weight Disord. 2013;18(2):221–227. doi: 10.1007/s40519-013-0021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen HN, Craighead LW. Appetite monitoring in the treatment of binge eating disorder. Behavior Therapy. 1999;30:253–272. [Google Scholar]
- American Psychiatric Association (Producer) Feeding and Eating Disorders. 2013 Mar 30; 2015. Retrieved from http://www.dsm5.org/Documents/EatingDisordersFactSheet.pdf.
- Beauboeuf-Lafontant T. Strong and large black women? Exploring relationships between deviant womanhood and weight. Gender & Society. 2003;17(1):111–121. [Google Scholar]
- Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol. 1984;40(6):1365–1367. doi: 10.1002/1097-4679(198411)40:6<1365::aid-jclp2270400615>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med. 2010;170(2):126–135. doi: 10.1001/archinternmed.2009.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronner Y, Boyington JE. Developing weight loss interventions for African-American women: elements of successful models. J Natl Med Assoc. 2002;94(4):224–235. [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Conroy MB, Sereika SM, Elci OU, Styn MA, Acharya SD, Glanz K. The effect of electronic self-monitoring on weight loss and dietary intake: a randomized behavioral weight loss trial. Obesity (Silver Spring) 2011;19(2):338–344. doi: 10.1038/oby.2010.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke LE, Shiffman S, Siewiorek D, Smailagic A, Kriska A, Ewing LJ, Rathbun SL. Triggers of Temptation and Urges Do Not Change During a 12-month Behavioral Intervention for Weight Loss. Paper presented at the American Heart Association Epidemiology and Lifestyle and Cardiometabolic Health Councils; Phoenix, AZ. 2016. http://circ.ahajournals.org/content/133/Suppl_1/AP251.abstract?sid=fb01e578-644f-45e5-b224-2f03d320f56c. [Google Scholar]
- Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59(5):739–744. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- Craighead L. The Appetite Awareness Workbook. Oakland, CA: New Harbinger Publications; 2006. [Google Scholar]
- Diabetes Prevention Program Research, G. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dicker SL, Craighead LW. Appetite-Focused Cognitive-Behavioral Therapy in the Treatment of Binge Eating with Purging. Cognitive Behavioral Practice. 2004;2004(11):213–221. [Google Scholar]
- Duarte C, Pinto-Gouveia J, Ferreira C. Expanding binge eating assessment: Validity and screening value of the Binge Eating Scale in women from the general population. Eat Behav. 2015;18:41–47. doi: 10.1016/j.eatbeh.2015.03.007. [DOI] [PubMed] [Google Scholar]
- Dutton GR, Martin PD, Rhode PC, Brantley PJ. Use of the weight efficacy lifestyle questionnaire with African American women: validation and extension of previous findings. Eat Behav. 2004;5(4):375–384. doi: 10.1016/j.eatbeh.2004.04.005. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nautre, assessment, and treatment. 12th. New York: Guilford Press; 1993. pp. 333–360. [Google Scholar]
- Fitzgibbon ML, Spring B, Avellone ME, Blackman LR, Pingitore R, Stolley MR. Correlates of binge eating in Hispanic, black, and white women. Int J Eat Disord. 1998;24(1):43–52. doi: 10.1002/(sici)1098-108x(199807)24:1<43::aid-eat4>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Stolley MR, Schiffer L, Sharp LK, Singh V, Dyer A. Obesity reduction black intervention trial (ORBIT): 18-month results. Obesity (Silver Spring) 2010;18(12):2317–2325. doi: 10.1038/oby.2010.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgibbon ML, Tussing-Humphreys LM, Porter JS, Martin IK, Odoms-Young A, Sharp LK. Weight loss and African-American women: a systematic review of the behavioural weight loss intervention literature. Obes Rev. 2012;13(3):193–213. doi: 10.1111/j.1467-789X.2011.00945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franko DL, Thompson-Brenner H, Thompson DR, Boisseau CL, Davis A, Forbush KT, Wilson GT. Racial/ethnic differences in adults in randomized clinical trials of binge eating disorder. J Consult Clin Psychol. 2012;80(2):186–195. doi: 10.1037/a0026700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldschmidt AB. Are loss of control while eating and overeating valid constructs? A critical review of the literature. Obes Rev. 2017;18(4):412–449. doi: 10.1111/obr.12491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode RW, Styn MA, Mendez DD, Gary-Webb TL. African Americans in Standard Behavioral Treatment for Obesity, 2001–2015: What Have We Learned? West J Nurs Res. 2017;39(8):1045–1069. doi: 10.1177/0193945917692115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gormally J, Black S, Daston S, Rardin D. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- Guest T. Using the eating disorder examination in the assessment of bulimia and anorexia: issues of reliability and validity. Soc Work Health Care. 2000;31(4):71–83. doi: 10.1300/J010v31n04_05. [DOI] [PubMed] [Google Scholar]
- Guss JL, Kissileff HR, Devlin MJ, Zimmerli E, Walsh BT. Binge size increases with body mass index in women with binge-eating disorder. Obes Res. 2002;10(10):1021–1029. doi: 10.1038/oby.2002.139. [DOI] [PubMed] [Google Scholar]
- Hales CM, Carroll MD, Fryar CD, Ogden CL. Prevalence of Obesity among Adults and Youth: United States, 2015–2016. 2017;(288) Retrieved from https://www.cdc.gov/nchs/data/databriefs/db288.pdf. [PubMed]
- Harrington EF, Crowther JH, Henrickson HC, Mickelson KD. The relationships among trauma, stress, ethnicity, and binge eating. Cultur Divers Ethnic Minor Psychol. 2006;12(2):212–229. doi: 10.1037/1099-9809.12.2.212. [DOI] [PubMed] [Google Scholar]
- Harrington EF, Crowther JH, Shipherd JC. Trauma, binge eating, and the “strong Black woman”. J Consult Clin Psychol. 2010;78(4):469–479. doi: 10.1037/a0019174. [DOI] [PubMed] [Google Scholar]
- Hays LM, Finch EA, Saha C, Marrero DG, Ackermann RT. Effect of self-efficacy on weight loss: a psychosocial analysis of a community-based adaptation of the diabetes prevention program lifestyle intervention. Diabetes Spectr. 2014;27(4):270–275. doi: 10.2337/diaspect.27.4.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbert A, Hildebrandt T, Agras WS, Wilfley DE, Wilson GT. Rapid response in psychological treatments for binge eating disorder. J Consult Clin Psychol. 2015;83(3):649–654. doi: 10.1037/ccp0000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill DM, Craighead LW, Safer DL. Appetite focused dialectical behavior therapy for the treatment of binge eating with purging: a preliminary trial. International Journal of Eating Disorders. 2011;44(3):249–261. doi: 10.1002/eat.20812. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Gullion CM, Stevens VJ, Brantley PJ, Appel LJ, Ard JD, Weight Loss Maintenance Trial Research, G Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med. 2008;35(2):118–126. doi: 10.1016/j.amepre.2008.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hrabosky JI, Grilo CM. Body image and eating disordered behavior in a community sample of Black and Hispanic women. Eat Behav. 2007;8(1):106–114. doi: 10.1016/j.eatbeh.2006.02.005. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61(3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson JS, Knight KM, Rafferty JA. Race and unhealthy behaviors: chronic stress, the HPA axis, and physical and mental health disparities over the life course. Am J Public Health. 2010;100(5):933–939. doi: 10.2105/AJPH.2008.143446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarosz PA, Dobal MT, Wilson FL, Schram CA. Disordered eating and food cravings among urban obese African American women. Eat Behav. 2007;8(3):374–381. doi: 10.1016/j.eatbeh.2006.11.014. [DOI] [PubMed] [Google Scholar]
- Johns DJ, Hartmann-Boyce J, Jebb SA, Aveyard P, Behavioural Weight Management Review, G. Diet or exercise interventions vs combined behavioral weight management programs: a systematic review and meta-analysis of direct comparisons. J Acad Nutr Diet. 2014;114(10):1557–1568. doi: 10.1016/j.jand.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovejoy M. Distrubances in the Social Body: Differences in Body Image and Eating Problems among African-American and White Women. Gender & Society. 2001;15(2):239–261. [Google Scholar]
- Lydecker JA, Grilo CM. Different yet similar: Examining race and ethnicity in treatment-seeking adults with binge eating disorder. J Consult Clin Psychol. 2016;84(1):88–94. doi: 10.1037/ccp0000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mama SK, Schembre SM, O’Connor DP, Kaplan CD, Bode S, Lee RE. Effectiveness of lifestyle interventions to reduce binge eating symptoms in African American and Hispanic women. Appetite. 2015;95:269–274. doi: 10.1016/j.appet.2015.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus MD, Bromberger JT, Wei HL, Brown C, Kravitz HM. Prevalence and selected correlates of eating disorder symptoms among a multiethnic community sample of midlife women. Ann Behav Med. 2007;33(3):269–277. doi: 10.1080/08836610701359720. [DOI] [PubMed] [Google Scholar]
- Marques L, Alegria M, Becker AE, Chen CN, Fang A, Chosak A, Diniz JB. Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int J Eat Disord. 2011;44(5):412–420. doi: 10.1002/eat.20787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin PD, Dutton GR, Brantley PJ. Self-efficacy as a predictor of weight change in African-American women. Obes Res. 2004;12(4):646–651. doi: 10.1038/oby.2004.74. [DOI] [PubMed] [Google Scholar]
- Mazzeo SE, Saunders R, Mitchell KS. Binge eating among African American and Caucasian bariatric surgery candidates. Eat Behav. 2005;6(3):189–196. doi: 10.1016/j.eatbeh.2004.12.001. [DOI] [PubMed] [Google Scholar]
- McTigue KM, Hess R, Ziouras J. Obesity in older adults: a systematic review of the evidence for diagnosis and treatment. Obesity (Silver Spring) 2006;14(9):1485–1497. doi: 10.1038/oby.2006.171. [DOI] [PubMed] [Google Scholar]
- Murphy PJ, Williams RL. Weight-loss study in African-American Women: lessons learned from project take HEED and future, technologically enhanced directions. Perm J. 2013;17(2):55–59. doi: 10.7812/TPP/12-094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health. Hyattsville, MD: 2017. Retrieved from https://www.cdc.gov/nchs/data/hus/hus16.pdf-053. [PubMed] [Google Scholar]
- Nezami BT, Lang W, Jakicic JM, Davis KK, Polzien K, Rickman AD, Tate DF. The Effect of Self-Efficacy on Behavior and Weight in a Behavioral Weight-Loss Intervention. Health Psychol. 2016 doi: 10.1037/hea0000378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pike KM, Dohm FA, Striegel-Moore RH, Wilfley DE, Fairburn CG. A comparison of black and white women with binge eating disorder. Am J Psychiatry. 2001;158(9):1455–1460. doi: 10.1176/appi.ajp.158.9.1455. [DOI] [PubMed] [Google Scholar]
- Qualtrics. Qualtrics (Version August 2015) Provo, UT: 2017. Retrieved from http://www.qualtrics.com/ [Google Scholar]
- Striegel-Moore RH, Dohm FA, Kraemer HC, Taylor CB, Daniels S, Crawford PB, Schreiber GB. Eating disorders in white and black women. Am J Psychiatry. 2003;160(7):1326–1331. doi: 10.1176/appi.ajp.160.7.1326. [DOI] [PubMed] [Google Scholar]
- Striegel-Moore RH, Wilfley DE, Pike KM, Dohm FA, Fairburn CG. Recurrent binge eating in black American women. Arch Fam Med. 2000;9(1):83–87. doi: 10.1001/archfami.9.1.83. [DOI] [PubMed] [Google Scholar]
- Thompson B. “A way outa no way”: Eating problems among African-American, Latina, and White women. Gender & Society. 1992;6(4):546–561. [Google Scholar]
- Thompson-Brenner H, Franko DL, Thompson DR, Grilo CM, Boisseau CL, Roehrig JP, Wilson GT. Race/ethnicity, education, and treatment parameters as moderators and predictors of outcome in binge eating disorder. J Consult Clin Psychol. 2013;81(4):710–721. doi: 10.1037/a0032946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilfley DE, Pike KM, Dohm FA, Striegel-Moore RH, Fairburn CG. Bias in binge eating disorder: how representative are recruited clinic samples? J Consult Clin Psychol. 2001;69(3):383–388. doi: 10.1037//0022-006x.69.3.383. [DOI] [PubMed] [Google Scholar]
- Willig AL, Richardson BS, Agne A, Cherrington A. Intuitive eating practices among African-American women living with type 2 diabetes: a qualitative study. J Acad Nutr Diet. 2014;114(6):889–896. doi: 10.1016/j.jand.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson GT, Wilfley DE, Agras WS, Bryson SW. Psychological treatments of binge eating disorder. Arch Gen Psychiatry. 2010;67(1):94–101. doi: 10.1001/archgenpsychiatry.2009.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson PL, O’Connor DP, Kaplan CD, Bode S, Mama SK, Lee RE. Relationship of Fruit, Vegetable, and Fat Consumption to Binge Eating Symptoms and African-American and Hispanic or Latina Women. Eating Behaviors. 2012;13(2):179–182. doi: 10.1016/j.eatbeh.2012.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingo BC, Carson TL, Ard J. Differences in weight loss and health outcomes among African Americans and whites in multicentre trials. Obes Rev. 2014;15(Suppl 4):46–61. doi: 10.1111/obr.12212. [DOI] [PubMed] [Google Scholar]
- Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003;34(Suppl):S117–120. doi: 10.1002/eat.10211. [DOI] [PubMed] [Google Scholar]
- Yeary KH, Cornell CE, Prewitt E, Bursac Z, Tilford JM, Turner J, Harris K. The WORD (Wholeness, Oneness, Righteousness, Deliverance): design of a randomized controlled trial testing the effectiveness of an evidence-based weight loss and maintenance intervention translated for a faith-based, rural, African American population using a community-based participatory approach. Contemp Clin Trials. 2015;40:63–73. doi: 10.1016/j.cct.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]


