Abstract
Background
Bipolar disorder is a mental illness with a high misdiagnosis rate and commonly misdiagnosed as other mental disorders including depression, schizophrenia, anxiety disorders, obsessive-compulsive disorders, and personality disorders, resulting in the mistreatment of clinical symptoms and increasing of recurrent episodes.
Aims
To understand the reasons for misdiagnosis of bipolar disorder in an outpatient setting in order to help clinicians more clearly identify the disease and avoid diagnostic errors.
Methods
Data from an outpatient clinic included two groups: those with a confirmed diagnosis of bipolar disorder (CD group) and those who were misdiagnosed (i.e. those who did in fact have bipolar disorder but received a different diagnoses and those without bipolar disorder who received a bipolar diagnosis [MD group]). Information between these two groups was compared.
Results
There were a total of 177 cases that met the inclusion criteria for this study. Among them, 136 cases (76.8%) were in the MD group and 41 cases (23.2%) were in the CD group. Patents with depression had the most cases of misdiagnosis (70.6%). The first episode of the patients in the MD group was more likely to be a depressive episode (χ2=5.206, p=0.023) and these patients had a greater number of depressive episodes during the course of the disease (Z=-2.268, p=0.023); the time from the onset of the disease to the first treatment was comparatively short (Z=-2.612, p=0.009) in the group with misdiagnosis; the time from the onset of disease to a confirmed diagnosis was longer (Z=-3.685, p<0.001); the overall course of disease was longer (Z=-3.274, p=0.001); there were more inpatients for treatment (χ2=4.539, p=0.033); and hospitalization was more frequent (Z=-2.164, p=0.031). The group with misdiagnosis had more psychotic symptoms (χ2=11.74, p= 0.001); particularly when depression occurred (χ2=7.63, p= 0.006), and the incidence of comorbidity was higher (χ2=5.23, p=0.022). The HCL-32 rating was lower in the misdiagnosis group (t=-2.564, p=0.011). There were more patients diagnosed with bipolar and other related disorders in the misdiagnosis group than in the confirmed diagnosis group (11.0% v. 4.9%) and there were more patients in the MD group diagnosed with depressive episodes who had a recent episode (78.7% v. 65.9%).
Conclusions
The rate of misdiagnosis of patients with bipolar receiving outpatient treatment was quite high and they often received a misdiagnosis of depression. In the misdiagnosis group the first episode tended to manifest as a depressive episode. In this group there were also a greater number of depressive episodes over the course of illness, accompanied by more psychotic symptoms and a higher incidence of comorbidity. Moreover, these patients apparently lacked insight into their own mania and hypomania symptoms, resulting in difficulties in early diagnosis, longer time needed to confirm the diagnosis, higher rate of hospitalization, and greater number of hospitalizations.
Key words: bipolar disorder, outpatient department, psychiatry, misdiagnosis
Abstract
背景
双相情感障碍是一种高误诊率的精神疾病,常被误诊为抑郁症、精神分裂症、焦虑症、强迫症和人格障碍等精神疾病,导致临床症状不能有效控制,病情呈反复发作趋势,故近年来双相情感障碍的误诊问题越来越引起精神科医生的重视。
目的
了解双相情感障碍在门诊的误诊情况,并分析其误诊原因,指导临床医师加强对双相情感障碍的识别,尽量避免或减少其误诊和漏诊。
方法
纳入专家门诊确诊为双相情感障碍的患者,了解其在门诊的就诊及误诊和漏诊情况,通过比较误诊组(包含漏诊者)和确诊组的临床资料进一步分析导致误诊和漏诊的可能原因。
结果
双相情感障碍在专家门诊就诊患者中占 31.5%。符合本研究入组标准的共有177 例,其中误诊组136 例(76.8%),确诊组41 例(23.2%),误诊为抑郁症者最多(70.6%)。误诊组患者首次发作更多的表现为抑郁发作(χ2=5.206, p=0.023),并且病程中抑郁发作次数更多(Z=-2.268, p=0.023);误诊组起病至首次治疗的时间较短(Z=-2.612, p=0.009)、而起病至确诊时间更长 (Z=-3.685, p<0.001),总病程更长(Z=-3.274, p=0.001),并且住院治疗的患者更多(χ2=4.539, p=0.033),住院次数也更多(Z=-2.164, p=0.031);误诊组伴有精神病性症状更多(χ2=11.74, p=0.001),尤其抑郁发作时(χ2=7.63, p=0.006),共病的发生率更高(χ2=5.23, p=0.022);误诊组HCL-32 评分更低(t=-2.564, p=0.011)。误诊组诊断为其他特定的双相及相关障碍的患者较确诊组多(11.0% v. 4.9%),并且误诊组最近发作情况表现为抑郁发作的 患者较多(78.7% v. 65.9%)。
结论
门诊双相情感障碍患者的误诊率高,常被误诊为抑郁症。误诊组患者首次发作更多的表现为抑郁发作,病程中抑郁发作次数更多,伴有精神病性症状更多,共病的发生率更高,并且患者对自身躁狂或轻躁狂发作情况明显认识不足,导致早期难以明确诊断,确诊所需时间更长,住院比率更高,住院次数更多。临床医生应提高对双相情感障碍的识别,避免或减少双相情感障碍的误诊和漏诊。
关键词: 双相情感障碍, 门诊, 精神科, 误诊
1. Background
Misdiagnosis is an incorrect diagnosis. The objectives of making a diagnosis are to determine the nature of a disease and to select targeted treatment so that the condition takes a favorable turn. Therefore, the incorrect, incomprehensive, or untimely diagnosis is considered to be a misdiagnosis. In clinical work, bipolar disorder is usually difficult to diagnose in its early stages, especially when it has an early onset. Hirschfeld and colleagues [1] reported that the misdiagnosis rate for bipolar disorder could reach as high as 69%. Only 20% of patients with bipolar disorder with a current depressive episode were given a confirmed diagnosis within the first year of treatment. A confirmed diagnosis was typically given 5 to 10 years after the first episode of the disease.[2] Generally, the disorder was misdiagnosed as major depressive disorder, schizophrenia, anxiety disorder, borderline personality disorder, or substance dependence.[3] It was most commonly misdiagnosed as major depressive disorder. [4] Because of psychotic symptoms, 31% of patients with bipolar I disorder were mistakenly diagnosed as having other disorders with obvious psychotic symptoms such as schizophrenia or substance use induced psychotic disorders.[5] The reason for this may be related to clinical practitioners who believe that Schneider’s first rank symptoms are specific symptoms of schizophrenia.[6] Patients with bipolar II disorder were usually misdiagnosed as having unipolar depression. [7] The reason might be related to the disease characteristics of bipolar disorder. When the clinical manifestation of the first episode was depression, the patient was often simply diagnosed as having depressive disorder.[6] Misdiagnosis also occurs when there are other comorbid disorders making affective symptoms, when there is not sufficient attention paid to medical history, or through overly restrictive use of the diagnostic criteria. Some studies showed that bipolar disorder has high comorbidity [8, 9] often combined with alcohol and drug dependence, personality disorder, and all sorts of anxiety disorders. The clinical manifestations of comorbidity often masked or were confused with affective symptoms, thereby causing clinical misdiagnosis.
Currently, there is still a lack of systematic research regarding the identification rate and the diagnostic rate of bipolar disorder and clinicians understanding of bipolar disorder. Therefore, we followed up and analyzed data from patients seen in our psychiatric specialist clinic receving treatment for bipolar disorder in order to further understand the reasons for misdiagnosis.
2. Methods
2.1 Participants
The participants in this study were patients with bipolar disorder that had consecutive consultations in the specialist outpatient clinic of our hospital from March 1st 2016 to August 31st 2016. There were a total of 181 cases. After selection, 177 cases were enrolled, including 85 males and 92 females. Range of ages was from 18 to 64 years old. The mean(SD) age was 29.1 (11.5) years old. All participants were in line with the following: (a) meeting diagnostic criteria for bipolar disorder according to DSM-V; (b) at least 2 consultation visits after enrollment into this study; (c) aged 18 to 65 years; (d) did not have severe somatic diseases, mental retardation, mental disorders caused by organic diseases, psychoactive substance or alcohol abuse. We excluded pregnant and lactating women, holdouts and people with incomplete clinical data. The enrolled participants were divided into two groups. The participants who were diagnosed with bipolar disorder in the first visit were regarded as the confirmed diagnosis group. The participants who were not diagnosed with bipolar disorder in the first visit and yet received a bipolar diagnosis in the return visit were regarded as the misdiagnosis group (including patients with missed diagnosis: The diagnosis was depression when the participants only showed depressive episode in the first consultation and there was no confirmed mania or hypomania episodes. The diagnosis was bipolar disorder when mania and hypomania were present in the return visit). There were 41 participants (23.2%) in the confirmed diagnosis group and 136 persons (76.8%) in the misdiagnosis group.
2.2 Study methods
Cross-sectional and retrospective study methods were used. Information were collected by professional psychiatrists. The method of information gathering was a combination of checking medical history and interviews with the patient and at least one immediate family member. The relevant clinical data was recorded in detail. Demographic data and clinical data of all patients with bipolar disorder were collected using a self-compiled questionnaire. Clinical data included the age of first onset, the clinical manifestation of the first episode, the time from the onset to the first consultation, the course of disease, the time from the onset to the confirmed diagnosis, diagnosis and classification, the number of manic depressive episodes, whether there were mixed characteristics to these episodes, whether or not patient was hospitalized for treatment, current clinical manifestation and treatment, whether or not there is a family history of mental illness, history of suicide, psychotic symptoms, and whether the bipolar disorder is rapid cycling or comorbid with another illness. All the enrolled patients were assessed with PHQ-9 and HCL-32 self-rating scales. The demographic data and clinical data of the MD group and CD group were compared.
2.3 Statistical methods
All data were processed using SPSS 17.0 Methods used included t-test, Mann-Whitney test, and chi-square test. A p value of less than 0.05 was considered statistically significant and less than 0.01 was considered highly statistically significant.
3. Results
3.1 Bipolar disorder consultation and misdiagnosis in an outpatient department
In this study, there were 574 cases of outpatients in the specialist clinic. Among these cases, there were 181 patients with bipolar disorder (31.5%). Of these, 177 cases that met the inclusion criteria. Among the cases, 136 cases had had misdiagnosis and the misdiagnosis rate reached 76.8% (see figure 2). The most common misdiagnosis was depression (96 cases, 70.6%) followed by schizophrenia (28 cases, 20.6%) and obsessive compulsive disorder (21 cases, 15.4%); also included were anxiety disorder (9 cases, 6.6%) and personality disorder (2 cases, 1.5%) (see figure 3). Among them, 16 patients were misdiagnosed with 2 disorders and 2 patients were misdiagnosed with 3 disorders.
Figure 2.
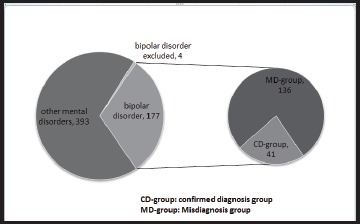
Bipolar disorder consultation in the specialist outpatient clinic
Figure 3.
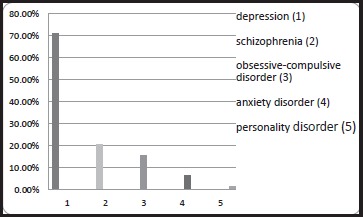
Other diagnoses besides Bipolar given (MD group)
3.2 Comparison of the demographic data between the MD group and CD group (see table 1)
Table 1.
Comparison of the demographic data between the bipolar disorder misdiagnosis group and confirmed diagnosis group
| Misdiagnosis group (N=136) |
Confirmed diagnosis group (N=41) |
t/X2 | p | |
|---|---|---|---|---|
|
mean (sd) age |
29.71 (10.11) |
26.95 (11.67) |
1.478 | 0.141 |
|
Gender [case (%)] |
0.920 | 0.338 | ||
| Male | 68 (50%) | 17 (41.5%) | ||
| Female | 68 (50%) | 24 (58.5%) | ||
|
Marriage [case (%)] |
0.039 | 0.844 | ||
| Unmarried | 94 (69.1%) | 29 (70.7%) | ||
| Married | 42 (30.9%) | 12 (28.3%) | ||
|
Education [case (%)] |
5.829 | 0.054 | ||
| University | 84 (61.8%) | 20 (48.8%) | ||
| Senior high school | 46 (33.8%) | 15 (36.6%) | ||
| Junior high school | 6 (4.4%) | 6 (14.6% ) | ||
|
Occupation [case (%)] |
3.172 | 0.205 | ||
| Working or attending school | 103(75.7%) | 26 (63.4%) | ||
| Sick leave or retire | 18 (13.3%) | 10 (24.4%) | ||
| Unemployed | 15 (11%) | 5 (12.2%) |
The difference between the demographic data of the two groups was not statistically significant in any category.
3.3 Comparison of the clinical characteristics between the bipolar disorder MD group and CD group
The age at first episode (t=-0.059, p=0.953), total number of episodes (Z= -1.019, p= 0.308), number of manic episodes (Z= -1.373, p= 0.17), and the PHQ-9 score during depressive episode (t=1.177, p=0.241) had no statistically significant differences. There was also no difference between the two groups in family history of bipolar disorder.
Patients in the MD group more commonly had depression during their first episode (χ2= 5.206, p= 0.023) and the number of depressive episodes was significantly more during the course of illness (Z= -2.268, p= 0.023). The time from the onset of illness to first treatment was significantly shorter (Z=-2.612, p=0.009) in the MD group, the time from the onset of illness to the confirmed diagnosis was longer (Z=-3.685, p<0.001), the overall course of disease was longer (Z=-3.274, p=0.001), there were more cases receiving inpatient treatment (χ2=4.539, p=0.033), and hospitalization was more frequent (Z=-2.164, p=0.031). The MD group had more psychotic symptoms (χ2=11.74, p= 0.001), particularly during depressive episodes (χ2=7.63, p= 0.006), and the incidence of comorbidity was higher (χ2=5.23, p=0.022). The HCL-32 rating was lower in the MD group (t=-2.564, p=0.011). See table 2.
Table 2.
Comparison of the clinical characteristics between the bipolar disorder misdiagnosis group and confirmed diagnosis group
| Misdiagnosis group (N=136) |
Confirmed diagnosis group (N=41) |
t/z/X2 | p | |
|---|---|---|---|---|
| Age at the first episode (year) | 22.07(8.42) | 22.17(11.73) | -0.059 | 0.953 |
| Time from onset to the first treatment (year) | 0.2(0.2,3.8) | 2.0(0.05,4.0) | -2.612 | 0.009** |
| Course of disease (year) | 6.0(3.0,10.0) | 4.0(3.0,5.0) | -3.274 | 0.001** |
| Total frequency of episodes | 7.0(4.0,13.0) | 5.0(3.0,10.0) | -1.019 | 0.308 |
| The frequency of manic episodes | 2.0(1.0,2.0) | 2.0(1.0,4.0) | -1.373 | 0.17 |
| The frequency of depressive episodes | 4.5(2.0,11.0) | 3.0(2.0,5.0) | -2.268 | 0.023* |
| First episode manifestation [case (%)] | 5.206 | 0.023* | ||
| Manic episode as the patient’s first episode | 29(21.3% ) | 16(39.0% ) | ||
| Depression as the patient’s first episode | 107(78.7% ) | 25(61.0% ) | ||
| Time from onset to confirmed diagnosis (year) | 4.0(1.23,8.0) | 2.0(0.2,4.0) | -3.685 | <0.001** |
| Number of hospitalizations | 0(0,1.0) | 0(0,0) | -2.164 | 0.031* |
| PHQ-9 score | 16.24(5.27) | 15.14(5.09) | 1.177 | 0.241 |
| HCL-32 score | 14.07(5.10) | 16.51(6.08) | -2.564 | 0.011* |
| Inpatient treatment [case (%)] | 43(31.6% ) | 6(14.6%) | 4.539 | 0.033* |
| With psychotic symptoms [case (%)] | 78(57.4%) | 11(26.8%) | 11.74 | 0.001** |
| With psychotic symptoms during manic episode[case (%)] | 34(25.0%) | 5(12.2%) | 3.007 | 0.083 |
| With psychotic symptoms during depressive episode[case (%)] | 59(43.4%) | 8(19.5%) | 7.63 | 0.006** |
| Family history of affective disorder [case (%)] | 19(14.0% ) | 5(12.2%) | 0.085 | 0.771 |
| Comorbidity | 45 (33.1%) | 6 (14.6%) | 5.23 | 0.022* |
| Obsessive-compulsive disorder | 27(19.9%) | 3(7.3%) | ||
| Anxiety | 13(9.6%) | 2(4.9%) | ||
| Personality disorder | 2(1.5%) | 0(0%) | ||
| Lycorexia | 3(2.2%) | 1(2.4%) |
3.4 Comparison of diagnosis and pharmacological treatment between the MD group and CD group
There was no statistically significant difference between the two groups in diagnostic classification (χ2=1.417, p=504), but there were more patients diagnosed with other specific bipolar and related disorders in the MD group than in the CD group (11.0% v. 4.9%). In terms of recent episodes and clinical medication, the differences between the 2 groups were not statistically significant (χ2=2.816, p=0.093). However, the patients in the misdiagnosis group that in recent mood episodes presented with depression were more (78.7% v. 65.9%). The ratio of rapid cycling episodes in the two groups (χ2=0.012, p=0.914) and having episodes with mixed features (χ2=0.086, p=0.770) were not statistically significant. See table 3
Table 3.
Comparison of the diagnosis and pharmacological treatment between the bipolar disorder misdiagnosis group and confirmed diagnosis group
| Misdiagnosis group (N=136) |
Confirmed diagnosis group (N=41) |
χ2 | p | |
|---|---|---|---|---|
| Diagnosis classification [case (%)] | 1.417 | 0.504 | ||
| Bipolar type I | 88 (64.7% ) | 30 (73.2%) | ||
| Bipolar type II | 33 (24.3% ) | 9 (21.9%) | ||
| Other specific bipolar and related disorders | 15 (11.0%) 27 (19.8%) | 2 (4.9%) 9 (21.9%) | ||
| With mixed features [case (%)] | 0.086 | 0.770 | ||
| Rapid cycling episode [case (%)] | 41 (30.1%) | 12 (29.3%) | 0.012 | 0.914 |
| Recent episodes [case (%)] | 2.816 | 0.093 | ||
| Manic episode | 29 (21.3%) | 14 (34.1%) | ||
| Depressive episode | 107 (78.7%) | 27 (65.9%) | ||
| Current drug treatment situation [case (%)] | 3.702 | 0.140 | ||
| Antipsychotics + mood stabilizers | 114 (83.8%) | 37 (90.2%) | ||
| Antipsychotics + mood stabilizers + antidepressants | 16 (11.8%) | 1 (2.5%) | ||
| Antipsychotic drugs alone or mood stabilizers | 6 (4.4%) | 3 (7.3%) |
*p<0.05
** p<0.01
3.5 Comparison of the number of manic and depressive episodes between the MD and CD groups
There were more depressive episodes than manic episodes reported in both groups. This difference in the MD had high statistical significance (Z= -9.034, p= 0.001). This difference in the CD group also had statistical significance (Z= -2.508, p= 0.012). See table 4
Table 4.
Comparison of the manic and depressive episodes between the bipolar disorder misdiagnosis group and confirmed diagnosis group
| Frequency of manic episode | Frequency of depressive episode | z | p | |
|---|---|---|---|---|
| Misdiagnosis group | 2.0 (1.0,2.0) | 4.5 (2.0,11.0) | -9.034 | <0.001** |
| Confirmed diagnosis group | 2.0 (1.0,4.25) | 3.0 (2.0,5.0) | -2.508 | 0.012* |
*p<0.05
** p<0.01
4. Discussion
4.1 Main findings
The results of this study show that the misdiagnosis rate of bipolar disorder was 76.8%. The misdiagnosis rate is slightly higher than the reported results in studies conducted outside of China.[1] This could be related to the source of our sample. All the patients selected for this study were from the specialist outpatient department, including a larger number of patients with refractory bipolar disorder and atypical symptoms. Of the 177 patients enrolled, 36 had mixed features, 53 had rapid cycling episodes, 51 had comorbidity with other disorders, and 17 were diagnosed with other specific bipolar and related disorders.
This study shows that bipolar disorder patients are most likely to be misdiagnosed with depression. The misdiagnosis rate is as high as 70.6%. The result shares similarity with other studies. [2,10] The reason may be related to the characteristics of the onset of bipolar disorder itself, especially when the episode of onset is depressive with no mania or hypomania.[2,11] In the entire course of bipolar disorder, there were apparently more depressive episodes than manic or hypomanic episodes.[12] In particular the patients with bipolar II disorder had a depressive presentation throughout most of their illness, [13] making the clinical diagnosis even more difficult. In the misdiagnosis group of this study, there were more patients having a depressive episode at onset and the frequency of depressive episodes was apparently higher than the manic episode, thereby prolonging the time for clinical diagnosis and increasing the misdiagnosis rate.
Patients with bipolar disorder are often misdiagnosed as having unipolar depression in many circumstances. The reason is related to clinicians or patients lacking knowledge about manic and hypomanic symptoms. Some research shows that the hypomanic state was often mistaken by clinicians or patients as the signs of improvement or remission of depression and they neglected the risk of the disorder further worsening, resulting in misdiagnosis.[14,15] The results of this study showed that the HCL-32 score of the patients in the MD group was lower, which also confirmed the above views.
The results of this study also showed that 20.6% of the patients with bipolar disorder were misdiagnosed as having schizophrenia. In addition, more than half of the 136 patients in the MD group had psychotic symptoms, so it was clear that the presence of psychotic symptoms increased the risk of being misdiagnosed as having schizophrenia especially during the onset of depression. In other studies, 61.5% of patients with bipolar disorder with psychotic symptoms were misdiagnosed as having other mental disorders at the time of first treatment. Moreover, 45% of the patients showed psychotic symptoms such as hallucinations or delusions during depressive episodes.[17] Some studies [18] showed that psychotic symptoms are one of the major risk factors for bipolar disorder in patients with depression. They can even be used as a predictor of whether patients with depression have bipolar disorder.
In this study, 15.4% of patients were misdiagnosed with obsessive-compulsive disorder, 6.6% of them were misdiagnosed with anxiety disorder, and 1.5% of them were misdiagnosed as having a personality disorder. The reason for misdiagnosis may be related to the comorbidity of bipolar disorder. Comorbidity was very common in bipolar disorder. This study showed that 1/3 of the patients in the MD group had comorbidity and it was more than in the CD group. It can be seen that the presence of comorbidity may mask emotional symptoms, leading to an increase in misdiagnosis rate. A meta-analysis [8] indicated that the incidence of comorbid anxiety disorders with bipolar disorder was 42.7% and comorbid obsessive-compulsive disorder was 10.7%. A systematic review of 64 related articles [9] indicated that the incidence of bipolar disorder comorbid with obsessive-compulsive disorder was between 11% and 21%. Comorbidity results in complex or atypical clinical symptoms, increases the rate of clinical misdiagnosis, and leads to treatment difficulties.
In terms of diagnosis classification, this study showed that there was no significant statistical difference between the two groups. However, the patients of the MD group diagnosed as other specific bipolar disorder and other related disorder were slightly more than the CD group. This could be one of the reasons for misdiagnosis. Many of the symptoms of the patients in this study were hypomanic or manic yet did not fit the time criteria for bipolar. For example hypomanic symptoms only lasted 2 to 3 days, or the time criteria for a hypomanic episode was met but the criteria for other symptoms were not met. These were harder to identify and diagnose at an early stage. However, this study was carried out in a clinic specializing in affective disorders therefore the staff in this setting may have a higher ability to diagnose this type of bipolar disorder.
4.2 Limitations
This study was a cross-sectional and retrospective study. The clinical data were collected mainly from checking past medical records and interviewing patients and at least one family member regarding history of illness. Although each patient had at least two follow-up visits and was asked carefully about the medical history in order to ensure the integrity of the medical history data, it is not guaranteed that the patients and their family members provided a complete medical history. Patients with a long medical history and recurrent episodes were especially unable to recall the timing and manifestation of each episdoe.
The sample for this study originated from a psychiatric clinic specializing in the diagnosis and treatment of affective disorders. The diagnosis and differential diagnosis in this clinic were more standardized; the compliance of the patients was good; the interruption rate of treatment was low; and the drop-out rate from follow-up visits was low. Therefore this sample should be somewhat conducive to follow-up and research development. However, the source of the sample was relatively narrow in this study as it did not include patients with other diagnoses or in other treatment settings. Moreover, the sample size was limited and the diagnosis and treatment situations of bipolar disorder in the general outpatient service were not covered. Therefore, a wider and larger sample study is needed to further explore the current status of bipolar disorder misdiagnosis in psychiatric outpatient clinics in China.
4.3 Implications
When bipolar disorder is misdiagnosed or missed altogether, symptoms cannot be effectively treated, episodes tend to be recurrent, and rapid cycling episodes are more commonly seen. [19] The risk of suicide increases, [20] which in turn increases the need for hospitalization and overall burden of the disease.[21] This can also explain why the patients in the MD group tended to have a higher rate of hospitalization. Therefore, early diagnosis is conducive to appropriate and timely treatment and is beneficial to the maximum recovery of the patients’ function. The earlier the correct diagnosis and treatment, the greater the chance that the patient will recover.
However, any doctor could make mistakes in cross-sectional diagnosis due to the complexity of the presentation of bipolar disorder. This study looked into the causes of bipolar disorder misdiagnosis and missed diagnosis in the outpatient service in hopes of improving guidance for clinical workers. In order to prevent the misdiagnosis of bipolar disorder, clinicians should conduct comprehensive and in-depth clinical examination, pay full attention to emotional symptoms, identify hypomanic symptoms carefully, search for diagnostic clues for bipolar disorder from the clinical symptoms of depression, ask about whether there were past episodes of hypomania or mania especially during medical history collection, and enhance the identification of bipolar disorder so as to avoid or reduce the misdiagnosis and missed diagnosis of bipolar disorder.
Subsequently, clinicians should try harder to identify psychiatric symptoms and affective symptoms and pay close attention to those depressive patients with psychotic symptoms. At the same time, they should consider that comorbidity with other disorders in bipolar is common. Clinicians should improve the identification of comorbidity and avoid or reduce the misdiagnosis and missed diagnosis of bipolar disorder so as to give timely and standardized treatment to patients with bipolar disorder and improve the short-term and long-term treatment effects and quality of life to the greatest extent.
Figure 1.

Flowchart of the study
Biography

Hui Shen acquired her bachelor’s degree in clinical medicine at Shanghai Second Medical University in 2003. In the same year she began working at the Shanghai Mental Health Center. She has 13 years of clinical work experience in psychiatry. At present, she is the chief rehabilitation doctor at SMHC. Her research interests are the treatment of schizophrenia and bipolar disorder, as well as the cognitive function and rehabilitation therapy of psychiatric patients.
Footnotes
Funding statement
Shanghai Mental Health Center affiliated to the Shanghai Jiao Tong University project (project code: 2016-YJ-12);
Shanghai Mental Health Center affiliated to the Shanghai Jiao Tong University project (project code: 2014 - YL - 04);
National Key Technology Research and Development Program (project code:2012BAI01B04)
Conflicts of interest statement
The authors declare no conflict of interest related to this manuscript.
Informed consent
Written informed consent was provided by all participants.
Ethical approval
This study was approved by the ethics committee of the Shanghai Mental Health Center affiliated to Shanghai Jiao Tong University.
Copyright permission on work’s translation
I have authorized the article to Shanghai Archives of Psychiatry for translation from Chinese to English. I have confirmed all the information included in this article is correct.
Authors’ contributions
Hui Shen: research design, data analysis, and article writing
Li Zhang: medical history collection, scale evaluation
Chuchen Xu: medical history collection, scale evaluation, and literature review
Meijuan Chen: research guidance
Yiru Fang: research guidance
Contributor Information
Meijuan CHEN (美娟 陈), Email: cmjlulu@163.com.
Yiru FANG (儒 方贻), Email: yirufang@aliyun.com.
References
- 1.Hirschfeld RM, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? Results of the national depressive and manic-depressive association 2000 survey of individuals with bipolar disorder. J Clin Psychiatry. 2003; 64(2): 161-74 [PubMed] [Google Scholar]
- 2.Baldessarini RJ, Tondo L, Baethge CJ, Lepri B, Bratti IM. Effects of treatment latency on response to maintenance treatment in manic-depressive disorders. Bipolar Disorder. 2007; 9(4): 386–393. doi: http://dx.doi.org/10.1111/j.1399-5618.2007.00385.x [DOI] [PubMed] [Google Scholar]
- 3.Young AH. Bipolar disorder: diagnostic conundrums and associated comorbidities. J Clin Psychiatry. 2009; 70(8): e26 doi: http://dx.doi.org/10.4088/JCP.7067br6c [DOI] [PubMed] [Google Scholar]
- 4.Smith DJ, Griffiths E, Kelly M, Hood K, Craddock N, Simpson SA. Unrecognised bipolar disorder in primary care patients with dression. Br J Psychiatry. 2011; 199(1): 49-56. doi: http://dx.doi.org/10.1192/bjp.bp.110.083840 [DOI] [PubMed] [Google Scholar]
- 5.Altamura AC, Goikolea JM. Differential diagnoses and management strategies in patients with schizophrenia and bipolar disorder. Neuropsychiatr Dis Treat. 2008; 4(1): 311-317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meyer F, Meyer TD. The misdiagnose is of bipolar disorder as a psychotic disorder:some of its causes and their influence on therapy. Affect Disord. 2009; 112(1-3): 174-183. doi: http://dx.doi.org/10.1016/j.jad.2008.04.022 [DOI] [PubMed] [Google Scholar]
- 7.Altamura AC, Buoli M, Albano A, Dell’Osso B. Age at onset and latency to treatment (duration of untreated illness) in patients with mood and anxiety disorders: a naturalistic study. Int Clin Psychopharmacol. 2010; 25(3): 172-179. doi: http://dx.doi.org/10.1097/YIC.0b013e3283384c74 [DOI] [PubMed] [Google Scholar]
- 8.Nabavi B, Mitchell AJ, Nutt D. A Lifetime Prevalence of Comorbidity between Bipolar Affective Disorder and Anxiety Disorders: A Meta-analysis of 52 Interview-based Studies of Psychiatric Population. Ebiomedicine. 2015; 2 (10): 1404-1419. doi: http://dx.doi.org/10.1016/j.ebiom.2015.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Amerio A, Odone A, Liapis CC, Ghaemi SN. Diagnostic validity of comorbid bipolar disorder and obsessive-compulsive disorder: a systematic review. Acta Psychiatr Scand. 2014; 129 (5): 343-358. doi: http://dx.doi.org/10.1111/acps.12250 [DOI] [PubMed] [Google Scholar]
- 10.Smith DJ, Griffiths E, Kelly M, Hood K, Craddock N, Sharon A. Simpson. Unrecognized bipolar disorder in primary care patients with depression. Br J Psychiatry. 2011; 199 (1): 49-56. doi: http://dx.doi.org/10.1192/bjp.bp.110.083840 [DOI] [PubMed] [Google Scholar]
- 11.Goodwin FK, Jamison KR, Ghaemi SN. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression, 2nd ed New York: Oxford University Press; 2007 [Google Scholar]
- 12.Judd LL, Schettler PJ, Akiskal HS, Maser J, Coryell W, Solomon D, et al. Long-term symptomatic status of bipolar I vs. bipolar II disorders. Int J Neuropsychopharmacol. 2003; 6(2): 127– 137. doi: http://dx.doi.org/10.1017/S1461145703003341 [DOI] [PubMed] [Google Scholar]
- 13.Ghaemi SN, Ko JY, Goodwin FK. “Cade’s disease” and beyond: misdiagnosis, antidepressant use, and a proposed definition for bipolar spectrum disorder. Can J Psychiatry. 2002; 47: 125–134. doi: http://dx.doi.org/10.1177/070674370204700202 [DOI] [PubMed] [Google Scholar]
- 14.He H, Xu G, Sun B, Ouyang H, Dang Y, Guo Y, et al. The use of 15-point hypomanic checklist in differentiating bipolar I and bipolar II disorder from major depressive disorder. Gen Hosp Psychiatry. 2014; 36: 347-351. doi: http://dx.doi.org/10.1016/j.genhosppsych.2013.12.008 [DOI] [PubMed] [Google Scholar]
- 15.Hoertel N, Le Strat Y, Limosin F, Dubertret C, Gorwood P. Prevalence of subthreshold hypomania and impact on internal validity of RCTs for major depressive disorder: Results from a national epidemiological sample. PLoS One. 2013; 8(2): e55448 doi: http://dx.doi.org/10.1371/journal.pone.0055448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Altamura AC, Buoli M, Caldiroli A, Caron L, Cumerlato Melter C, Dobrea C, et al. Misdiagnosis, duration of untreated illness (DUI) and outcome in bipolar patients with psychotic symptoms: A naturalistic study. J Affect Disord. 2015; 182: 70–75. doi: http://dx.doi.org/10.1016/j.jad.2015.04.024 [DOI] [PubMed] [Google Scholar]
- 17.Brugue E, Colom F, Sanchez-Moreno J, Cruz N, Vieta E. Depression subtypes in bipolar I and II disorders. Psychopathology. 2008; 41: 111–114. doi: http://dx.doi.org/10.1159/000112026 [DOI] [PubMed] [Google Scholar]
- 18.Salvatore P, Baldessarini RJ, Khalsa HM, Amore M, Di Vittorio C, Ferraro G, et al. Predicting diagnostic change among patients diagnosed with first-episode DSM-IV-TR major depressive disorder with psychotic features. J Clin Psychiatry. 2013; 74 (7): 723-731. doi: http://dx.doi.org/10.4088/JCP.12m08328 [DOI] [PubMed] [Google Scholar]
- 19.Schneck CD, Miklowitz DJ, Miyahara S, Araga M, Wisniewski S, Gyulai L, et al. The prospective course of rapid-cycling bipolar disorder: findings from the STEP-BD. Am J Psychiatry. 2008; 165(3): 370–377. doi: http://dx.doi.org/10.1176/appi.ajp.2007.05081484 [DOI] [PubMed] [Google Scholar]
- 20.Altamura AC, Dell’Osso B, Berlin HA, Buoli M, Bassetti R, Mundo E. Duration of untreated illness and suicide in bipolar disorder:a naturalistic study. Eur Arch Psychiatry Clin Neurosci. 2010; 260(5): 385-391. doi: http://dx.doi.org/10.1007/s00406-009-0085-2 [DOI] [PubMed] [Google Scholar]
- 21.Valenti M, Pacchiarotti I, Bonnin CM, Rosa AR, Popovic D, Nivoli AM, et al. Risk factors for antidepressant-related switch to mania. J Clin Psychiatry. 2012; 73(2): e271-e2716. doi: http://dx.doi.org/10.4088/JCP.11m07166 [DOI] [PubMed] [Google Scholar]


