Abstract
Study Objective
Epidural analgesia may be associated with fewer postoperative complications and is associated with improved survival after colon cancer resection. This study used the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) to assess any association between epidural analgesia (versus non-epidural) and complications after colectomy.
Design
Retrospective cohort study.
Setting
603 hospitals in the United States reporting data to NSQIP.
Patients
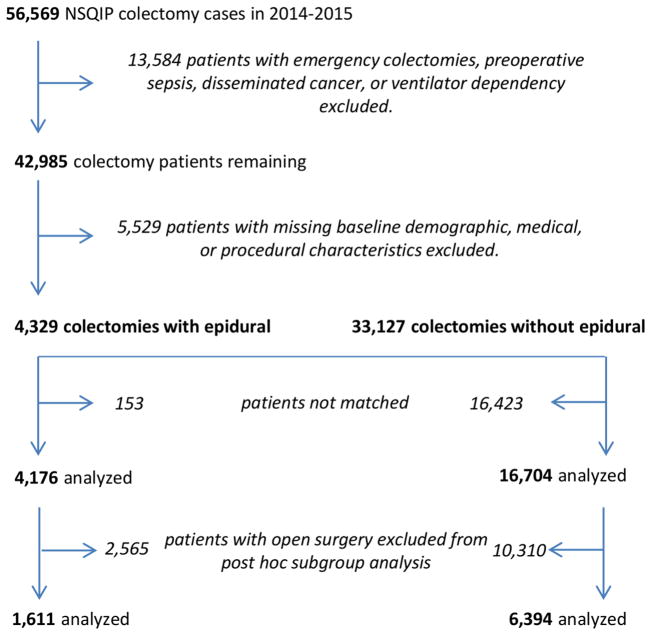
From 2014–15 data, 4,176 patients undergoing colectomy with records indicating epidural analgesia were matched 1:4 via propensity scores to 16,704 patients without.
Interventions
None (observational study).
Measurements
Primarily, we assessed the association between epidural analgesia and a composite of cardiopulmonary complications using an average relative effect generalized estimating equations model. Secondary outcomes included neurologic, renal, and surgical complications and length of hospitalization. Sensitivity analyses repeated the analyses on a subgroup of only open colectomies.
Main Results
We found no association between epidural analgesia and the primary outcome: average relative effect (95% CI) 0.87 (0.68, 1.11); P = 0.25. We found no significant associations with any secondary outcomes. In the 8,005 open colectomies, however, there was a significant association between epidural analgesia and fewer cardiopulmonary complications (average relative effect odds ratio [95% CI] of 0.58 [0.35, 0.95]; P = 0.03) and shortened hospital stay (HR for time to discharge [98.75% CI] of 1.10 [1.02, 1.18]; P<0.001).
Conclusions
We found no overall association between epidural analgesia and reduced complications after colectomy. In open colectomies, however, epidural analgesia was associated with fewer cardiopulmonary complications and shorter hospitalization. This may inform analgesic choice when planning open colectomy.
Keywords: Anesthesia, Epidural, Complication, Postoperative, Colectomy, Pain, Postoperative
1. Introduction
In recent years, there has been much interest in the potential effects of regional anesthesia or analgesia on outcomes after surgery. We previously used the linked Surveillance, Epidemiology, and End Results (SEER)-Medicare database to assess the impact of epidural analgesia use on recurrence and survival after colon cancer resection and found that epidural analgesia was associated with improved survival but not recurrence.[1]
Although our previous analysis was unable to find a difference in cancer recurrence, there was an early and persistent survival advantage among patients receiving epidural analgesia, even adjusting for multiple covariates. A decrease in perioperative adverse events could explain much of the observed mortality difference. Indeed, recent analysis of Cochrane Database systematic reviews suggests that epidural anesthesia may confer a mortality benefit in some patients.[2] There is also evidence showing epidural analgesia reduces postoperative pain and reduces a number of postoperative complications in various settings.[3–9] Our previous analysis, however, was unable to address the specific reasons for the mortality difference because the SEER-Medicare database has limited clinical detail to reliably capture many postoperative complications.
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) provides a rich, validated data source concerning perioperative care and postoperative complications from 603 participating hospitals (in 2015) in the United States, both academic and private (https://www.facs.org/quality-programs/acs-nsqip).[10] Each participating site has a trained Surgical Clinical Reviewer and a “Surgeon Champion” responsible for auditing cases to ensure data quality. Cases from each site are randomly sampled on a risk-adjusted basis, so the NSQIP data only provide a sample of the overall case volume at each center. Starting in 2014, an additional variable was added to capture additional anesthetic techniques such as epidural analgesia, providing the ability to evaluate the impact of epidural analgesia on perioperative outcomes. We therefore used the 2014–15 ACS NSQIP Colectomy Procedure-Targeted and standard Participant Use Data Files (PUFs) to identify patients undergoing non-emergent colectomy and evaluate the primary hypothesis that patients with epidural analgesia (as defined below) would have a lower composite risk of 30-day mortality and cardiopulmonary complications than those without epidural analgesia. Secondary analyses tested the hypotheses that epidural analgesia is associated with fewer renal, neurologic, and surgical complications as well as shorter length of hospital stay than systemic analgesia. Because of the significant clinical differences between open and laparoscopic procedures, a subgroup analysis of only open colectomies was performed to evaluate whether the associations of epidural analgesia with the composite outcomes differ by procedure type.
2. Materials and Methods
This study using de-identified data was determined by the Cleveland Clinic Institutional Review Board to be exempt from review. We assessed the association between epidural analgesia around the time of colectomy (versus no epidural analgesia) on postoperative complications and hospital length of stay using the 2014 and 2015 NSQIP standard and colectomy procedure-targeted data. Patients undergoing colectomy for all indications were included. Patients were excluded from the analysis if they had emergency surgery, preoperative sepsis, disseminated cancer, or ventilator dependence. Further, patients with missing baseline, demographic, medical, or procedural characteristics were excluded.
Colectomy patients with epidural analgesia were compared descriptively to patients without epidural analgesia on baseline demographic, medical, and procedural characteristics defined in Table 1 using appropriate summary statistics (i.e., mean (standard deviation) for normally distributed data, median [interquartile range] for skewed data, or N (%) for categorical data). Epidural cases were defined as any colectomies with appropriate values for the “primary anesthesia” or “other anesthesia” variables. The primary anesthesia variable describes the main anesthetic technique used. The other anesthesia variable (introduced in 2014) aims to capture other techniques such as epidural analgesia or peripheral nerve blocks used in conjunction with general anesthesia.
Table 1.
Balance of treatment groups on baseline demographic, medical, and procedural characteristics of the study population before and after propensity score matching.
| Factor | Before matching Epidural (N = 4,329) | No Epidural (N = 33,127) | ASD* | After matching Epidural (N = 4,176) | No Epidural (N = 16,704) | ASD* |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age (years; range: 18–89 for all groups) | 59 (15) | 61 (15) | 0.095 | 59 (15) | 59 (15) | 0.002 |
| Female, n (%) | 2,299 (53%) | 17,475 (53%) | 0.007 | 2,212 (53%) | 8,878 (53%) | 0.004 |
| White, n (%)+ | 3,774 (87%) | 28,421 (86%) | 0.041 | 3,633 (87%) | 14,479 (87%) | 0.009 |
| Body mass index (kg m−2) | 27 [24, 32] | 28 [24, 32] | 0.046 | 27 [24, 32] | 27 [24, 32] | 0.002 |
| Smoker, n (%) | 709 (16%) | 5,564 (17%) | 0.011 | 678 (16%) | 2,669 (16%) | 0.007 |
| ASA Status, n (%) | 0.087 | 0.002 | ||||
| 1 | 70 (2%) | 767 (2%) | 70 (2%) | 277 (2%) | ||
| 2 | 1,906 (44%) | 15,552 (47%) | 1,879 (45%) | 7,509 (45%) | ||
| 3 | 2,204 (51%) | 15,589 (47%) | 2,088 (50%) | 8,366 (50%) | ||
| ≥4 | 149 (3%) | 1,219 (4%) | 139 (3%) | 552 (3%) | ||
| Partially/totally dependent functional status, n (%) | 62 (1%) | 676 (2%) | 0.047 | 54 (1%) | 247 (1%) | 0.016 |
| Medical History | ||||||
| Steroid or immunosuppressant use, n (%) | 497 (11%) | 2,985 (9%) | 0.082 | 462 (11%) | 1,817 (11%) | 0.006 |
| Chemotherapy within 90 days of surgery, n (%) | 287 (7%) | 1,413 (4%) | 0.104 | 248 (6%) | 1,008 (6%) | 0.004 |
| Baseline hematocrit (%)+‡ | 38 (6) | 38 (6) | 0.019 | 38 (6) | 38 (6) | 0.024 |
| Baseline creatinine (mmol L−1)+§ | 0.84 [0.70, 1.00] | 0.85 [0.70, 1.00] | 0.009 | 0.85 [0.70, 1.00] | 0.83 [0.70, 1.00] | 0.041 |
| Baseline albumin (g L−1)+|| | 3.8 (0.6) | 3.8 (0.6) | 0.049 | 3.8 (0.6) | 3.8 (0.6) | 0.019 |
| Transfusion within 72 hours of surgery, n (%) | 58 (1%) | 621 (2%) | 0.043 | 57 (1%) | 199 (1%) | 0.015 |
| Acute renal failure prior to surgery, n (%)+ | 5 (0%) | 49 (0%) | 0.009 | 5 (0%) | 19 (0%) | 0.002 |
| End stage renal disease on dialysis, n (%) | 25 (1%) | 217 (1%) | 0.010 | 24 (1%) | 98 (1%) | 0.002 |
| History of severe COPD, n (%) | 188 (4%) | 1,506 (5%) | 0.010 | 176 (4%) | 694 (4%) | 0.003 |
| History of congestive heart failure, n (%) | 32 (1%) | 287 (1%) | 0.014 | 32 (1%) | 127 (1%) | 0.001 |
| Presence of dyspnea, n (%) | 280 (6%) | 1,953 (6%) | 0.024 | 259 (6%) | 1,030 (6%) | 0.001 |
| Hypertension requiring medication, n (%) | 1,938 (45%) | 15,750 (48%) | 0.056 | 1,877 (45%) | 7,535 (45%) | 0.003 |
| Diabetes mellitus, n (%) | 0.064 | 0.010 | ||||
| Insulin-dependent | 184 (4%) | 1,719 (5%) | 178 (4%) | 718 (4%) | ||
| Non-insulin dependent | 369 (9%) | 3,240 (10%) | 363 (9%) | 1,405 (8%) | ||
| None | 3,776 (87%) | 28,168 (85%) | 3,635 (87%) | 14,581 (87%) | ||
| Bleeding disorder or anticoagulant use, n (%) | 104 (2%) | 984 (3%) | 0.035 | 101 (2%) | 377 (2%) | 0.011 |
| Weight loss (>10%) in the last 6 months, n (%) | 257 (6%) | 1,317 (4%) | 0.090 | 221 (5%) | 853 (5%) | 0.008 |
| Presence of ascites, n (%) | 18 (0.4%) | 88 (0.2%) | 0.026 | 14 (0.3%) | 50 (0.3%) | 0.006 |
| Colectomy for colorectal cancer, n (%) | 1,632 (38%) | 12,595 (38%) | 0.007 | 1,582 (38%) | 6,357 (38%) | 0.004 |
| Procedural characteristics | ||||||
| Estimated Probability of Morbidity (%) | 12 [8, 17] | 11 [8, 16] | 0.149 | 12 [8, 17] | 12 [8, 17] | 0.020 |
| Estimated Probability of Mortality (%) | 0.3 [0.1, 0.8] | 0.3 [0.1, 0.8] | 0.069 | 0.3 [0.1, 0.8] | 0.3 [0.1, 0.8] | 0.001 |
| Open surgery, n (%) | 1,644 (38%) | 12,977 (39%) | 0.025 | 1,611 (39%) | 6,394 (38%) | 0.006 |
| Duration of surgery (minutes) | 181 [131, 248] | 164 [118, 226] | 0.202 | 178 [130, 242] | 178 [126, 247] | 0.006 |
| Wound Class, n (%) | 0.071 | 0.007 | ||||
| 1-Clean | 30 (1%) | 296 (1%) | 29 (1%) | 111 (1%) | ||
| 2-Clean/contaminated | 3,347 (77%) | 26,401 (80%) | 3,246 (78%) | 13,028 (78%) | ||
| 3-Contaminated | 576 (13%) | 4,053 (12%) | 549 (13%) | 2,166 (13%) | ||
| 4-Dirty/infected | 376 (9%) | 2,377 (7%) | 352 (8%) | 1,399 (8%) | ||
Summary statistics are presented as mean (standard deviation), median [Q1, Q3], or n (%) as appropriate.
Absolute standardized difference, defined as the absolute difference in means, mean ranks, or proportions divided by the pooled standard deviation. Variables with ASD > 0.1 are defined as imbalanced.
Not included in the propensity score model due to missing data or very low incidence.
Hematocrit not measured for 324 epidural patients and 1,793 non-epidural patients before matching and 317 epidural and 850 non-epidural patients after matching.
Creatinine not measured for 383 epidural patients and 2,741 non-epidural patients before matching and 373 epidural and 1,325 non-epidural patients after matching.
Albumin not measured for 1,268 epidural patients and 10,330 non-epidural patients before matching and 1,247 epidural and 5,063 non-epidural patients after matching.
To maximize statistical power, laparoscopic cases were included in the primary analysis because of the sizable number of such cases (2,725) with epidural analgesia. Because of the likely difference in clinical effects of epidural analgesia on laparoscopic versus open procedures, planned sensitivity analyses excluded laparoscopic cases to focus on open colectomy. Missing entries for the “other anesthesia” variable were interpreted as non-epidural cases if the primary anesthesia variable was not recorded as epidural.
We used propensity score matching to control for observed potential confounding.[11] Propensity scores (i.e., the probability of receiving epidural analgesia) were estimated using a multivariable logistic regression model of receiving epidural analgesia (versus non-epidural) as a function of all of the potentially confounding variables listed in Table 1 (except for hematocrit, creatinine, and albumin due to missing data). Each epidural analgesia patient was matched to 4 patients who did not receive epidural analgesia using a greedy distance matching algorithm limiting distance to within 0.02 propensity score logit standard deviations of each other.[12]
Balance between groups on patient characteristics was assessed before and after propensity score matching using absolute standardized difference (ASD), defined as the absolute difference in means, mean ranks, or proportions divided by the pooled standard deviation. Variables with ASD > 0.10 were defined as imbalanced.[11]
2.1 Primary Analysis
We compared patients who received epidural analgesia to those who did not on a composite of cardiopulmonary complications including three components: cardiac complications, pulmonary complications, and 30-day mortality (defined in Table 2). Cardiac and pulmonary complications are each collapsed composites of various cardiac and pulmonary conditions (Table 2). A multivariate analysis was used to assess associations with the composite outcome, allowing capture of information about individual morbidities and the correlation between morbidities within each composite.
Table 2.
Incidence of primary and secondary outcomes by treatment group among matched patients.
| Primary outcome | Epidural (N = 4,176) | No Epidural (N = 16,704) |
|---|---|---|
| 1. Cardiopulmonary complications and mortality* | ||
| Cardiac complications | 28 (0.7) | 123 (0.7) |
| Intraoperative or postoperative myocardial infarction | 21 (0.5) | 77 (0.5) |
| Cardiac arrest requiring CPR | 9 (0.2) | 57 (0.3) |
| Pulmonary complications | 157 (4) | 685 (4) |
| Pneumonia | 58 (1) | 258 (2) |
| Unplanned tracheal intubation | 49 (1) | 192 (1) |
| Pulmonary embolism | 28 (0.7) | 94 (0.6) |
| Deep vein thrombosis/thrombophlebitis | 53 (1) | 191 (1) |
| Failure of weaning from ventilator (> 48 hours) | 40 (1) | 170 (1) |
| 30-day mortality | 24 (0.6) | 123 (0.7) |
| Secondary outcomes+ | ||
| 1. Stroke | 6 (0.1) | 34 (0.2) |
| 2. Renal complications+ | 43 (1.0) | 170 (1.0) |
| Progressive renal insufficiency without need for dialysis | 30 (0.7) | 121 (0.7) |
| Acute renal failure requiring new dialysis | 13 (0.3) | 50 (0.3) |
| 3. Surgical complications+‡ | 514 (12)‡ | 2,129 (13)‡ |
| Return to OR within 30 days | 173 (4) | 751 (5) |
| All-cause 30 day hospital readmission§ | 420 (10)§ | 1,687 (10)§ |
| 4. Days from operation to discharge|| | 5 [3, 7] | 5 [3, 7] |
| Exploratory outcomes | ||
| 1. Infectious complications | ||
| Superficial surgical site infection | 206 (5) | 740 (4) |
| Deep incisional surgical site infection | 41 (1) | 152 (1) |
| Organ space surgical site infection | 151 (4) | 731 (4) |
| Wound disruption | 31 (0.7) | 140 (0.8) |
| 2. Sepsis | ||
| Sepsis | 102 (2) | 546 (3) |
| Septic shock | 41 (1) | 204 (1) |
| 3. Prolonged ileus¶ | 582 (14) | 2,402 (14) |
Summary statistics are presented as n (%) or median [Q1, Q3] as appropriate.
The primary outcome is a composite consisting of 3 components: cardiac complications, pulmonary complications, and mortality. The 3 components were simultaneously analyzed using an average relative effect generalized estimating equations model using an unstructured covariance matrix.
Renal complications and surgical complications are each collapsed composite analyzed using separate logistic regression models.
No data for 9 patients who received epidurals and 43 patients who did not.
No readmission data for 9 patients who received epidurals and 44 patients who did not.
Length of stay not reported for 9 patients who did not receive epidural analgesia.
No data for 4 patients who received epidurals and 22 patients who did not.
The association between epidural analgesia and the composite of cardiopulmonary complications was assessed using an average relative effect generalized estimating equations (GEE) model with an unstructured correlation structure.[13] This approach estimates the average association across components and therefore is not driven by components with higher incidence. This approach also accounts for correlation among components and allows assessment of the heterogeneity of the associations between epidural analgesia status and each outcome component. Heterogeneity of epidural analgesia use across the composite was assessed by testing for epidural-by-component interaction using a significance criterion of P < 0.10. We also assessed whether the association between epidural analgesia and the composite differed among patients with colectomy for colorectal cancer by testing for the colorectal cancer-by-epidural interaction using a significance criterion of P < 0.10.
2.2 Secondary Analyses
We assessed the associations between epidural analgesia (versus non-epidural) and separate composites of neurological, renal/urinary, and surgical complications using separate multivariable logistic regression models. The association between epidural analgesia and hospital length of stay was assessed using a Cox proportional hazard regression model adjusting for imbalanced baseline variables after matching. Patients who died before discharge were censored to the longest observed duration of hospitalization.
2.3 Sensitivity Analysis
To determine if the association between epidural analgesia and outcomes varied by surgical approach (laparoscopic versus open), the primary and secondary analyses were repeated using a subset of the cohort consisting only of patients undergoing open colectomy. Procedures involving unplanned conversion from laparoscopic to open surgery were considered open.
Both the primary and secondary analyses were completed using an alpha of 0.05, with a significance criterion of 0.05 for the primary outcome and 0.0125 for each secondary outcome (i.e., 0.05/4). Analyses were completed using R version 3.3.2 (The R Foundation for Statistical Computing, Vienna, Austria) and SAS version 9.4 (SAS Institute, Carey, NC, USA).
2.4 Sample Size and Power
Empirical power was calculated based on the observed incidence of cardiopulmonary complications among patients who did not receive epidural analgesia (Table 2), a conservative correlation coefficient of 0.3 between outcomes, and the observed 4,176 patients who received epidural analgesia during colectomy. We estimated power using the MULTBINPOW SAS macro, which estimates power for average relative effect GEE models given varying correlations and sample sizes [Mascha EJ: Power Calculations for Tests on a Vector of Binary Outcomes (MULTBINPOW), Cleveland Clinic Statistical Software Series (http://www.lerner.ccf.org/qhs/software/multbinpow.php), 1.0 edition, Cleveland, Ohio 2011]. This SAS program uses simulations to compute and display comparative power of several parallel-group multivariate tests for treatment effect on a vector of binary events[14]. There was > 90% power at the 0.05 significance level to detect a 10% or greater relative difference in complications among epidural analgesia patients.
3. Results
The 2014 and 2015 NSQIP data included 56,569 colectomy cases. Among those, 4,329 colectomy patients who received epidural analgesia and 33,127 patients who did not were eligible for this analysis (Figure 1). 4,176 colectomy patients who received epidural analgesia were successfully matched 1:4 to 16,704 who did not (99% matched). Balance of groups on potentially confounding patient characteristics are presented before and after matching in Table 1. Virtually all patients received general anesthesia for their surgery, regardless of epidural analgesia use (4,136 of 4,176 epidural patients and 16,653 of 16,704 non-epidural patients). Groups were balanced on all patient characteristics after matching (i.e., ASD < 0.10 for all variables), so none were adjusted for in the primary or secondary analyses.
Figure 1.
Study flow diagram.
3.1 Primary analysis
The incidences of cardiopulmonary complications and each component of this composite are presented by treatment group in Table 2. There was no significant association between receiving epidural analgesia and the composite of cardiopulmonary complications, with an estimated average relative effect odds ratio (95% CI) of 0.87 (0.68, 1.11); P = 0.25 (Table 3).
Table 3.
Association between epidural use and primary and secondary outcomes among matched patients.
| Primary analysis | Average relative effect odds ratio* (95% CI)‡ | P-value‡ |
|---|---|---|
| Cardiopulmonary complications/mortality | 0.87 (0.68, 1.11) | 0.25 |
|
| ||
| Secondary analyses | Odds ratio§ (98.75% CI)|| | P-value|| |
|
| ||
| Stroke | 0.71 (0.23, 2.13) | 0.43 |
| Renal complications | 1.01 (0.66, 1.55) | 0.94 |
| Surgical complications¶ | 0.96 (0.85, 1.10) | 0.47 |
| Hazard ratio** (98.75% CI) | ||
| Time to discharge alivea | 1.04 (0.99, 1.08) | 0.04 |
Odds ratio estimated using an average relative effect generalized estimating equations model using an unstructured covariance matrix.
Significance criterion of 0.05 was used for the primary analysis.
Odds ratios estimated from separate logistic regression models.
Significance criterion of 0.0125 used for each secondary analysis (i.e., 0.05/4, Bonferroni).
52 patients removed from analysis due to missing surgical complications data.
Hazard ratio estimated using Cox proportional hazards regression. Patients who died before discharge were censored to the longest observed hospital length of stay.
9 patients who did not receive an epidural excluded from analysis due to unreported hospital length of stay.
There was no significant epidural-by-component interaction (P = 0.74), suggesting that the primary association is consistent across components of the composite. There was also no interaction between colorectal cancer and epidural analgesia during colectomy, suggesting that the primary association is consistent regardless of whether the colectomy was performed to treat colorectal cancer (P = 0.50).
3.2 Secondary analysis
There was no association between epidural analgesia (versus non-epidural) and any of the secondary complications, with estimated odds ratios (98.75% CI) of 0.71 (0.23, 2.13) for stroke (P = 0.43), 1.01 (0.66, 1.55) for renal complications (P = 0.94), and 0.96 (0.85, 1.10) for surgical complications (P = 0.47); Table 3. Incidences of each complication are presented in Table 2.
There was no association between epidural analgesia and time to hospital discharge alive using Cox proportional hazards regression, with an estimated hazard ratio (98.75% CI) of 1.04 (0.99, 1.08); P = 0.04; Table 3. Median [Q1, Q3] time to hospital discharge was 5 [3, 7] days in each group (Table 2).
3.3 Sensitivity Analysis—Open Colectomy
Of the 20,880 patients included in the primary and secondary analyses, 8,005 (38%) underwent open surgery, including 1,611 epidural patients and 6,394 without epidural analgesia. Included in this subgroup are 1,860 cases involving unplanned conversion from laparoscopic to open, 314 of whom had epidural analgesia and 1,546 who did not. Assessment of absolute standardized difference between these subgroups indicated that covariates remained balanced (data not shown). Among the open surgery patients, epidural analgesia was significantly associated with a reduced composite of cardiopulmonary complications, with an average relative effect odds ratio (95% CI) of 0.58 (0.35, 0.95); P = 0.03 (Table 4). Epidural analgesia was also associated with a shorter duration of hospitalization in this subgroup, with a hazard ratio (98.75% CI) of 1.10 (1.02, 1.18) for time to discharge alive (P < 0.001). However, there was no difference between groups in terms of stroke, renal complications, or surgical complications.
Table 4.
The association between epidural use and primary and secondary outcomes among subset of matched patients who underwent open surgery (N = 8,005 patients, 1,611 of which had an epidural).
| Primary analysis | Average relative effect odds ratio* (95% CI)‡ | P-value‡ |
|---|---|---|
| Cardiopulmonary complications/mortality | 0.58 (0.35, 0.95) | 0.03 |
|
| ||
| Secondary analyses | Odds ratio§ (98.75% CI)|| | P-value|| |
|
| ||
| Stroke | 1.19 (0.23, 6.18) | 0.80 |
| Renal complications | 0.47 (0.20, 1.15) | 0.03 |
| Surgical complications¶ | 0.96 (0.78, 1.19) | 0.63 |
| Hazard ratio** (98.75% CI) | ||
| Time to discharge alivea | 1.10 (1.02, 1.18) | < 0.001 |
Odds ratio estimated using an average relative effect generalized estimating equations model using an unstructured covariance matrix.
Significance criterion of 0.05 was used for the primary analysis.
Odds ratios estimated from separate logistic regression models.
Significance criterion of 0.0125 used for each secondary analysis (i.e., 0.05/4, Bonferroni).
9 patients removed from analysis due to missing surgical complications data.
Hazard ratio estimated using Cox proportional hazards regression. Patients who died before discharge were censored to the longest observed hospital length of stay.
10 patients who did not receive an epidural excluded from analysis due to unreported hospital length of stay.
4. Discussion
In this analysis, despite adequate post-hoc power, we found no overall significant association between epidural analgesia and the primary composite outcome. There was also no association with other complications or length of stay after colectomy. When looking specifically at open procedures, however, there was a significant association between epidural analgesia and a reduction in the primary composite outcome as well as shorter hospital length of stay.
There is ample reason to expect that epidural analgesia would improve patients’ perioperative outcomes: epidural analgesia has been shown to reduce postoperative pain and pulmonary complications after major abdominal surgery,[3] to reduce the postoperative hypercoaguable state,[4] to hasten the return of bowel function and exercise capacity after colectomy,[5–7] to reduce cardiac and pulmonary complications after abdominal aortic surgery,[8] and to be associated with improved outcomes after esophagectomy.[9] In a recent meta-analysis of multiple types of surgery, epidural analgesia was associated with a reduction in multiple postoperative complications and mortality.[15] Of note, since the vast majority of patients in our analysis also received general anesthesia, it will be difficult to separate any effects of epidural anesthesia from those of postoperative analgesia without detailed clinical information.
The NSQIP program provides a large, validated dataset covering over 600 institutions in the United States. This allows multicenter investigations at the national level without relying on often inaccurate administrative data.[16] Although it is a very large national database, the NSQIP program has been underutilized for anesthesiology research and holds great promise for further analyses. To our knowledge, this is the first study using NSQIP data to evaluate the association between epidural analgesia and outcomes after colectomy. Also using NSQIP data, Saied and colleagues demonstrated a reduction in several complications and hospital length of stay after a variety of procedures when comparing regional anesthesia to general anesthesia. Their analysis, however, utilized the primary anesthetic technique variable (for intraoperative care) and not the secondary anesthetic variable which would identify postoperative epidural analgesia. Notably, they did not find a reduction in myocardial infarction or mortality with regional anesthesia.[17]
The difference in results based on surgical approach (open versus laparoscopic) is consistent with prior work. Epidural analgesia is thought to be beneficial in general, but the specific context may be very important. Laparoscopic surgery is associated with less incisional pain, faster recovery and fewer postoperative complications than open procedures and is a key element of many enhanced recovery programs.[18] Instituting an enhanced recovery program including laparoscopic surgery may achieve many of the observed benefits of epidural analgesia. Indeed, within the context of an enhanced recovery protocol (that included laparoscopic surgery), epidural analgesia was not found to be advantageous other than providing slightly faster return of bowel function and improved pain scores.[19] It is also conceivable that some of the putative benefits of epidural or regional analgesia are due to systemic action of absorbed local anesthetic, as there can be significant systemic uptake.[20]
The finding of decreased length of stay among patients with epidural analgesia in the open colectomy group stands in contrast to the results of an analysis by the ERAS Compliance Group, who found an association between epidural analgesia and increased length of hospitalization in the context of an enhanced recovery program for colorectal cancer surgery.[18] Again, this may result from the enhanced recovery program favoring laparoscopic surgical approaches and utilizing other elements (transversus abdominis plane or other blocks, intravenous fluid minimization, early ambulation, and others) to hasten time to hospital discharge. There was also no detectable difference in the incidence of prolonged ileus, although the specific times to return of bowel function are not recorded and an undetected smaller difference may exist. Additionally, epidural analgesia is associated with complications (particularly hypotension and urinary retention) that may negatively affect the postoperative course.[15] Reassuringly, though, there were no differences detected in major complications between the groups.
As a retrospective cohort analysis, this study is limited by the available data and subject to confounding by unmeasured covariates. Although the NSQIP PUF is a rich data source, it lacks many perioperative details including anesthetic and analgesic management and does not allow for identification of individual hospital sites. Thus, the database only indicates that epidural analgesia was used but does not provide information about clinical management or allow for stratified analysis. Finally, although it contains many records from over 600 institutions, the NSQIP PUF only provides a relatively small sample of the total surgical volume in the United States (estimated at 320,000 colectomy procedures annually[21]), which may limit generalizability.
Although it was adequately powered for the primary outcome, there are a number of limitations to this analysis. We planned this analysis to have 90% power at the 0.05 significance level to detect a 10% relative reduction in complications among epidural analgesia patients, so there is a small chance that we observed false negative primary findings. We expected 20% of colectomy patients would receive an epidural, but only observed an 11.5% incidence of epidural use. However, the “other anesthesia” record was not required to be filled out in the 2014 NSQIP data, likely leading to under-coding. Missing entries for this field were considered as non-epidural cases in this analysis, potentially causing misclassification bias towards a null result. Additionally, clinical details about the epidural analgesia (such as location, choice of medication, dosing regimen, and timing) were not available. For the sensitivity analyses, there were many laparoscopic colectomies identified with epidural analgesia. This limits the power of any subgroup analysis and may lead to not identifying a true association (should one exist) between epidural analgesia and other complications in open procedures. There were also numerous missing entries for cancer staging data, so cancer stage was not able to be used as a covariate. This is a potential confounder in the analysis, although all other covariates were balanced after propensity score matching.
Our analyses used listwise deletion, removing patients with missing baseline or procedural characteristics from the analysis, assuming that these were missing completely at random. If this assumption does not hold, listwise deletion could potentially bias our results. Our sensitivity analysis found that groups differed on key characteristics including colectomy for colon cancer, incidence of open surgery, and intraoperative epidural use. Most of the missing data occurred only due to unreported race, accounting for 14% of exclusions. Race, however, has been shown to have a significant impact on outcomes after colectomy[22, 23] and we therefore believe it is reasonable to exclude patients with missing race data from the analysis.
Finally, our primary analysis examined the association between epidural analgesia and a composite of cardiopulmonary complications and mortality. Traditionally, analyses of composite outcomes are difficult to interpret when using a collapsed composite approach (e.g., any versus no outcome) if the frequency, severity, or association with the exposure differs across components. We have avoided these challenges by choosing components with similar severity and performing a multivariate analysis. Instead of estimating the association between epidural use and the odds of having any component, we estimated the average association across individual components of the composite (e.g., “average relative effect” odds ratio). Therefore, results are not driven by components with the highest frequency. We verified that the association between epidural use and the composite was consistent across components by assessing the epidural by component interaction. Thus, our analysis avoids many common limitations when using composite outcomes.
In conclusion, using 2014 and 2015 NSQIP colectomy data, we were unable to demonstrate an overall association between epidural analgesia and reduced complications after colectomy. For open procedures, however, epidural analgesia may be associated with fewer cardiopulmonary complications and decreased length of hospital stay. Our findings support a possible role for epidural analgesia in a multimodal analgesic regimen after open colectomy. Future prospective research should include an increased focus on functional outcomes (quality of recovery, discharge readiness, and others) as well as investigation into the systemic effect (if any) of epidurally-administered local anesthetics.
Highlights.
Overall, epidural analgesia showed no difference in postoperative complications.
In open colectomy, epidural analgesia is associated with fewer complications.
Epidural analgesia may improve outcomes and speed recovery after open colectomy.
Acknowledgments
Funding: L.C.C. was supported by an American College of Gastroenterology Junior Faculty Development Grant. G.S.C. was supported by National Institutes of Health grant P50 CA150964 (Case GI SPORE), UL1 TR000439 (Case Clinical & Translational Science Collaborative), P30 CA043703 (Case Comprehensive Cancer Center), and P30 DK097948 (Cleveland Digestive Diseases Research Core Center)
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Footnotes
Declarations of Interest: None
Disclosures: L.C.C. was supported by an American College of Gastroenterology Junior Faculty Development Grant. G.S.C. was supported by National Institutes of Health grant P50 CA150964 (Case GI SPORE), UL1 TR000439 (Case Clinical & Translational Science Collaborative), P30 CA043703 (Case Comprehensive Cancer Center), and P30 DK097948 (Cleveland Digestive Diseases Research Core Center)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cummings KC, 3rd, Xu F, Cummings LC, Cooper GS. A comparison of epidural analgesia and traditional pain management effects on survival and cancer recurrence after colectomy: a population-based study. Anesthesiology. 2012;116:797–806. doi: 10.1097/ALN.0b013e31824674f6. [DOI] [PubMed] [Google Scholar]
- 2.Guay J, Choi PT, Suresh S, Albert N, Kopp S, Pace NL. Neuraxial anesthesia for the prevention of postoperative mortality and major morbidity: an overview of cochrane systematic reviews. Anesth Analg. 2014;119:716–25. doi: 10.1213/ANE.0000000000000339. [DOI] [PubMed] [Google Scholar]
- 3.Rigg JR, Jamrozik K, Myles PS, Silbert BS, Peyton PJ, Parsons RW, et al. Epidural anaesthesia and analgesia and outcome of major surgery: a randomised trial. Lancet. 2002;359:1276–82. doi: 10.1016/S0140-6736(02)08266-1. [DOI] [PubMed] [Google Scholar]
- 4.Tuman KJ, McCarthy RJ, March RJ, DeLaria GA, Patel RV, Ivankovich AD. Effects of Epidural Anesthesia and Analgesia on Coagulation and Outcome After Major Vascular Surgery. Anesth Analg. 1991;73:696–704. doi: 10.1213/00000539-199112000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Carli MDMPF, Mayo PDN, Klubien MDK, Schricker MDPDT, Trudel MDMSJ, Belliveau MDP. Epidural Analgesia Enhances Functional Exercise Capacity and Health-related Quality of Life after Colonic Surgery Results of a Randomized Trial. Anesthesiology. 2002;97:540–9. doi: 10.1097/00000542-200209000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Carli F, Trudel J, Belliveau P. The effect of intraoperative thoracic epidural anesthesia and postoperative analgesia on bowel function after colorectal surgery. Dis Colon Rectum. 2001;44:1083–9. doi: 10.1007/BF02234626. [DOI] [PubMed] [Google Scholar]
- 7.Taqi A, Hong X, Mistraletti G, Stein B, Charlebois P, Carli F. Thoracic epidural analgesia facilitates the restoration of bowel function and dietary intake in patients undergoing laparoscopic colon resection using a traditional, nonaccelerated, perioperative care program. Surg Endosc. 2007;21:247–52. doi: 10.1007/s00464-006-0069-5. [DOI] [PubMed] [Google Scholar]
- 8.Guay J, Kopp S. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd; 2016. Epidural pain relief versus systemic opioid-based pain relief for abdominal aortic surgery. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Whooley BP, Law S, Murthy SC, Alexandrou A, Wong J. Analysis of reduced death and complication rates after esophageal resection. Ann Surg. 2001;233:338–44. doi: 10.1097/00000658-200103000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shiloach M, Frencher SK, Jr, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210:6–16. doi: 10.1016/j.jamcollsurg.2009.09.031. [DOI] [PubMed] [Google Scholar]
- 11.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10:150–61. doi: 10.1002/pst.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mascha EJ, Sessler DI. Design and Analysis of Studies with Binary- Event Composite Endpoints: Guidelines for Anesthesia Research. Anesth Analg. 2011;112:1461–71. doi: 10.1213/ANE.0b013e31821796d3. [DOI] [PubMed] [Google Scholar]
- 14.Mascha EJ, Imrey PB. Factors affecting power of tests for multiple binary outcomes. Stat Med. 2010;29:2890–904. doi: 10.1002/sim.4066. [DOI] [PubMed] [Google Scholar]
- 15.Popping DM, Elia N, Van Aken HK, Marret E, Schug SA, Kranke P, et al. Impact of epidural analgesia on mortality and morbidity after surgery: systematic review and meta-analysis of randomized controlled trials. Ann Surg. 2014;259:1056–67. doi: 10.1097/SLA.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 16.Lawson EH, Louie R, Zingmond DS, Brook RH, Hall BL, Han L, et al. A comparison of clinical registry versus administrative claims data for reporting of 30-day surgical complications. Ann Surg. 2012;256:973–81. doi: 10.1097/SLA.0b013e31826b4c4f. [DOI] [PubMed] [Google Scholar]
- 17.Saied NN, Helwani MA, Weavind LM, Shi Y, Shotwell MS, Pandharipande PP. Effect of anaesthesia type on postoperative mortality and morbidities: a matched analysis of the NSQIP database. BJA: British Journal of Anaesthesia. 2017;118:105–11. doi: 10.1093/bja/aew383. [DOI] [PubMed] [Google Scholar]
- 18.The ERAS Compliance Group. The Impact of Enhanced Recovery Protocol Compliance on Elective Colorectal Cancer Resection: Results From an International Registry. Ann Surg. 2015;261:1153–9. doi: 10.1097/SLA.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 19.Khan SA, Khokhar HA, Nasr ARH, Carton E, El-Masry S. Effect of epidural analgesia on bowel function in laparoscopic colorectal surgery: a systematic review and meta-analysis. Surg Endosc. 2013;27:2581–91. doi: 10.1007/s00464-013-2794-x. [DOI] [PubMed] [Google Scholar]
- 20.Yokoyama M, Mizobuchi S, Nagano O, Fujii H, Yamashita M, Hirakawa M. The effects of epidural insertion site and surgical procedure on plasma lidocaine concentration. Anesth Analg. 2001;92:470–5. doi: 10.1097/00000539-200102000-00036. [DOI] [PubMed] [Google Scholar]
- 21.Weiss AJ, Elixhauser A. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville (MD): 2014. Trends in Operating Room Procedures in U.S. Hospitals, 2001–2011: Statistical Brief #171. [Google Scholar]
- 22.Parsons HM, Habermann EB, Stain SC, Vickers SM, Al-Refaie WB. What happens to racial and ethnic minorities after cancer surgery at American College of Surgeons National Surgical Quality Improvement Program hospitals? J Am Coll Surg. 2012;214:539–47. doi: 10.1016/j.jamcollsurg.2011.12.024. discussion 47–9. [DOI] [PubMed] [Google Scholar]
- 23.Esnaola NF, Hall BL, Hosokawa PW, Ayanian JZ, Henderson WG, Khuri SF, et al. Race and surgical outcomes: it is not all black and white. Ann Surg. 2008;248:647–55. doi: 10.1097/SLA.0b013e31818a159a. [DOI] [PubMed] [Google Scholar]