Abstract
Traumatic events can negatively impact clinical outcomes among HIV positive women, particularly when those events result in ongoing psychological distress. Consequently, there have been calls to integrate screening and treatment of traumatic experiences and associated mental health disorders into HIV care. In South Africa, screening for traumatic experiences and mental health is not a routine part of HIV care. The goal of this study was to examine the prevalence of traumatic experiences and mental health distress among women in an HIV clinic in Cape Town, South Africa, and to explore the acceptability of routine screening in this setting. Seventy HIV positive women were screened following referral from healthcare workers in the clinic. Among participants, 51% reported a history of sexual abuse and 75% reported physical intimate partner violence (physical IPV). Among all participants, 36% met screening criteria for depression; among those with traumatic experiences (n=57), 70% met screening criteria for post-traumatic stress disorder (PTSD). Compared to reporting no sexual abuse or physical IPV, having experienced both sexual abuse and physical IPV was significantly associated with higher odds of depression, while reporting either sexual abuse or physical IPV individually was not significantly associated with increased odds of depression. Among women reporting sexual abuse, 61% were disclosing their experience for the first time during the screening; 31% of women with physical IPV experience were disclosing for the first time. Overall, 98% of participants thought screening should be routine and extended to all women as part of clinic care. Screening women for sexual abuse and physical IPV may be an important component of ensuring HIV care engagement.
Keywords: South Africa, sexual abuse, trauma, HIV, mental health, intimate partner violence
Introduction
South Africa accounts for a disproportionate share of the global HIV burden, with approximately 7 million people infected (UNAIDS, 2015). Women are particularly vulnerable to the HIV epidemic, with an estimated 4 million South African women living with HIV (UNAIDS, 2015). In addition to high prevalence of HIV infection, women in South Africa also suffer from high prevalence of traumatic experiences, including childhood abuse and physical and sexual abuse in adulthood. Lifetime prevalence of any abuse has been reported at over 50% (Choi et al., 2014; Dunkle, Jewkes, Brown, Yoshihama, et al., 2004; Jewkes & Abrahams, 2002; Li et al., 2014).
Abuse and violence against South African women is rooted in gender inequality, patriarchy and normative use of violence in affirming power (Abrahams, Jewkes, Hoffman, & Laubsher, 2004; Jewkes, Levin, & Penn-Kekana, 2002; Jewkes, Penn-Kekana, Levin, Ratsaka, & Schrieber, 2001). In a nationally representative study, physical abuse by an intimate partner and childhood physical abuse were the most common forms of violence against women (Kaminer, Grimsrud, Myer, Stein, & Williams, 2008). High levels of sexual abuse of women have been documented in South Africa, with sexual abuse by intimate partners being most common (Dartnall & Jewkes, 2013; Jewkes & Naeema Abrahams, 2002). In addition to physical and sexual abuse, women also suffer from emotional and financial abuse within intimate relationships, and forms of abuse are often co-occurring (Jewkes et al., 2001).
A history of trauma1 can negatively impact clinical outcomes among women living with HIV, particularly when those lifetime events result in ongoing psychological distress and poor mental health (Hatcher, Smout, Turan, Christofides, & Stockl, 2015; Machtinger, Wilson, Haberer, & Weiss, 2012; Willie, Overstreet, Sullivan, Sikkema, & Hansen, 2016). Poor mental health impacts HIV outcomes through multiple mechanisms, including decreased cognitive and physical functioning (Leserman et al., 2005; O’Cleirigh, Skeer, Mayer, & Safren, 2009), continued risk-taking behaviors (Sikkema et al., 2011a; Smit et al., 2006), and decreased motivation and capacity to engage in HIV treatment (Meade, Hansen, Kochman, & Sikkema, 2009; Mugavero et al., 2006; Whetten et al., 2013). Post-traumatic stress disorder (PTSD), major depression, and anxiety are psychological sequelae of trauma that have been associated with poor HIV treatment outcomes among women (Machtinger et al., 2012; Willie et al., 2016). (Brezing, Ferrara, & Freudenreich, 2015; Seedat, 2012)
In sub-Saharan Africa, HIV care engagement over time is challenging; it has been estimated that 60% of patients who had initiated antiretroviral therapy (ART) are no longer in care (Piot et al., 2015). A history of traumatic experiences may be an important contributor to poor HIV care engagement,(Whetten et al., 2013). A qualitative study of HIV-infected South African women found that sexual trauma history affected HIV care engagement, particularly in the period immediately following HIV diagnosis (Watt et al., 2016). When patients do not fully engaging in care, they face increased risk of resistance, viral failure and forward transmission of HIV (Knobel, Carmona, Grau, Pedro-Botet, & Díez, 1998; Lamiraud et al., 2012).
Given the potential negative impacts of trauma on HIV care outcomes, there have been calls to develop and implement interventions that address trauma, in order to increase HIV care engagement and improve health outcomes (Collins, Holman, Freeman, & Patel, 2006; Seedat, 2012). More broadly, there is recognition of the importance of addressing trauma histories in HIV patients through a model of care called trauma informed care (Brezing et al., 2015; Machtinger, Cuca, Khanna, Rose, & Kimberg, 2015). Trauma informed care calls for the integration of trauma-related assessment, treatment and referral into health care services. This approaches necessarily includes screening for traumatic experiences and associated mental health disorders as part of routine care (Brezing et al., 2015; Machtinger et al., 2015).
Barriers to the implementation of screening for trauma and mental health symptoms include the potential of shame, stigma and cultural factors leading to non-disclosure of experiences, especially of sexual abuse (Fleming, 2013; Watt et al., 2016). In addition, structural barriers include high attrition of healthcare workers and high patient loads, lack of mental health training among healthcare workers and scarce psychosocial resources (Marais & Petersen, 2015; Undie, Maternowska, Mak’anyengo, & Askew, 2016).
Routine mental health screening has been successfully integrated into antenatal care settings in South Africa, which may provide a framework for screening and referring in an HIV care setting (Honikman, van Heyningen, Field, Baron, & Tomlinson, 2012; Vythilingum et al., 2013a). Using a stepped care approach, healthcare workers in this setting screen women for mental health symptoms during antenatal visits and refer cases to on-site non-specialist counsellors, who in turn refer severe cases to a psychiatrist (Honikman et al., 2012; Vythilingum et al., 2013a). In order to assess the potential for a similar model in HIV clinics, it necessary to examine whether screening is feasible and acceptable in the HIV care setting, and women’s willingness to disclose their traumatic experiences and related psychological distress.
The purpose of this study was to assess need and acceptability of a brief screening for sexual abuse, physical intimate partner violence (physical IPV), and mental health symptoms among female patients in a single HIV clinic in Cape Town, South Africa. The study had three aims: (1) to assess the prevalence of sexual abuse, physical IPV and mental health symptoms in this population, (2) to explore the associations between these traumatic experiences and depressive symptoms, and (3) to assess acceptability of screening among participants. Findings from the study can inform the design of trauma focused assessments and interventions for women living with HIV and can highlight the need for trauma informed HIV care in this setting.
Methods
Study setting
The study was conducted over an 8-week period during June and July 2015 at a primary health care HIV clinic located in a peri-urban township of Cape Town, South Africa. The clinic is one of the public service HIV treatment centres, where patients receive free HIV care, including antiretroviral therapy (ART). At the time of the study, the clinic had a total patient load of over 2,500 adult HIV patients. Initiation on ART at the clinic follows a standard protocol as per government guidelines (Western Cape Department of Health, 2015). After receiving an HIV diagnosis, patients are assessed based on the ART initiation criteria (i.e., CD4 <= 500 cells/mm3, AIDS defining illness, pregnant or breastfeeding, HIV positive in serodiscordant couples). Patients who do not yet meet ART initiation criteria receive care and regular assessments, including CD4 count monitoring, in the Wellness sub-clinic, until they meet the ART initiation criteria. Patients meeting ART initiation criteria receive three sessions of readiness counselling in the Counselling sub-clinic, after which they initiate ART and receive their care in the ART sub-clinic. Patients who default on ART return to the Counselling sub-clinic for adherence counselling sessions.
Participants and procedures
Data were collected via a cross-sectional screening survey of 70 female patients who were enrolled in HIV care at the study clinic and attending either the Wellness or Counselling sub-clinics. Women in the Wellness sub-clinic were eligible if they had recently met ART initiation criteria and were transitioning to the Counselling sub-clinic. All female patients in the Counselling sub-clinic were eligible, regardless of whether they were receiving counselling as an ART initiator or as an ART defaulter. We decided to target women who were initiating ART or returning to care after defaulting, because these moments represent critical points of HIV care where interventions, including mental health interventions for trauma, can be introduced to improve or maintain adherence and care engagement. All participants had to be 18 years or older and able to provide informed consent.
Healthcare workers in the Wellness and Counselling sub-clinics briefly informed eligible participants about a study for HIV positive women, but did not provide any study details. Interested individuals were referred to a female research assistant. The research assistant described the study in detail and, if interested, obtained oral consent. The research assistant verbally administered the screening instrument and recorded the participant’s responses on the paper copy of the instrument.
All participants were assessed for suicidal ideation and severity using items adapted from the suicidality subscale of the Mini International Neuropsychiatric Interview (Lecrubier et al., 1997). A psychologist on the study staff made referrals for participants with elevated psychological distress, including those deemed to be at high risk for suicide or self-harm. All participants were provided with a list of local organizations providing psychosocial services. Participants were offered complimentary tea and biscuits while waiting to be screened or afterward and did not receive any additional study incentives. The screening instrument took approximately 15 minutes to complete. The ethical review boards at Duke University and the University of Cape Town approved all study procedures.
Measures
The screening survey was created in English, and a parallel version was created through a process of translation and back-translation in Xhosa. The following constructs were measured in the survey.
Sexual abuse
Sexual abuse was defined as sexual abuse or assault that occurred during childhood, adolescence or adulthood. Sexual abuse was measured using four main questions, each with follow-up questions, based on the WHO CIDI (World Health Organization, 1990) and the Childhood Trauma Questionnaire (Bernstein et al., 2003). Participants were asked the following questions: whether someone had ever touched them in a sexual way or made them touch the person in a sexual way against their will; whether someone had ever threatened to hurt them unless they did something sexual with the person; whether someone had ever forced them (physically, emotionally or with a weapon) to have sexual intercourse or other sexual activities against their will; and whether they had ever had any other unwanted or threatening sexual experiences.
The four sexual abuse experience questions had yes/no response options. For yes responses, follow-up questions asked when the experience occcured (childhood, adolescence and/or adulthood), and whether the experiences were ongoing, happened in past year, or were not recent. Participants were categorized as having a sexual abuse history if they endorsed any of the four sexual abuse experience questions, at any point in their lives.
Physical intimate partner violence (physical IPV)
Physical IPV was measured using three items from the physical assault subscale of the revised Conflict Tactics Scale (CTS2) (Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Participants were asked the following questions: whether a sexual partner had ever threated to hit them or throw something at them; whether a sexual partner had ever beat them; and whether a sexual partner had ever used a knife or gun on them. Response options were yes/no, and for yes responses, participants were asked if the violence had occurred within the last 6 months. Participants were categorized as having a history of physical IPV if they endorsed a lifetime experience of any of the three items.
Depression
The PHQ-2 screener for depression measured the frequency of depressive symptoms in the past two weeks (Arroll et al., 2010). The measure has been validated for use in a primary care setting in South Africa (Bhana, Rathod, Selohilwe, Kathree, & Petersen, 2015). Response options ranged from 0 (“not at all”) to 3 (“nearly every day”). The two items were summed, with a score of three or more indicative of major depression (Bruce Arroll et al., 2010).
PTSD symptoms
PTSD symptoms in the past month were assessed using the seven-item Breslau PTSD screener (Breslau, Peterson, Kessler, & Schultz, 1999), which has been previously used in South Africa (Sikkema et al., 2011b). The PTSD measure was only administered to participants who had endorsed either sexual abuse or physical IPV history. Response options were yes/no for each question and captured whether a participant had experienced a particular symptom within the last month. A yes response corresponded to a score of one, creating a total summed score ranging from 0 to 7. A score of three or more was indicative of elevated PTSD symptoms (Kimerling et al., 2006).
Participants’ screening experience
Participants’ reactions to the screening process, its acceptability, and attitudes towards potential integration of screening into routine HIV care management were assessed with four open ended questions: 1) how they felt being asked the screening questions; 2) whether they would feel comfortable being asked these screening questions by a healthcare provider; 3) whether they thought it would be appropriate to screen all women; and 4) suggestions for how screening could be conducted in the future. Participants were probed to explain their answers for each question. Participants who had experienced trauma were separately asked whether they had ever disclosed their sexual abuse and/or physical IPV experience to anyone else before the screening (response yes/no for each type of traumatic experience). Lastly, all participants were asked whether they preferred either nurses or counsellors to conduct screening and the reasons for their preference.
Data analysis
Descriptive statistics were used to describe the demographic and other characteristics of the sample. Potential differences in these characteristics were examined by comparing participants with trauma histories (sexual abuse and/or physical IPV) and those without trauma histories. Due to the small sample sizes and distribution of variables, non-parametric statistical tests were used for comparisons. The Wilcoxon rank sum test was used to compare differences in age, years of education and time since HIV diagnosis. Fisher’s exact test was used to compare differences in employment, relationship status and pregnancy.
We examined the prevalence of mental health symptoms (depression and PTSD symptoms) among three categories of traumatic experiences (no trauma, sexual abuse or physical IPV, and sexual abuse and physical IPV history). Since PTSD symptoms were only assessed on participants with a trauma history, no PTSD symptoms results were reported for the no trauma history category. Fisher’s exact test was used to compare proportions of mental health symptoms across the three categories of traumatic experiences.
A logistic regression model was used to explore whether type(s) of trauma experience was predictive of depression, with depression as a categorical outcome based on the standard cut-off indicative of major depression (Arroll et al., 2010). Traumatic experience was examined as a categorical variable with three levels (no trauma, sexual abuse or physical IPV, sexual abuse and physical IPV), with no trauma as the referent group. Two variables, age and education, were examined as predictor variables. Since most women were from a high poverty setting, education was chosen as the best proxy for socioeconomic status.
Participants’ perceptions of the screening process were quantitatively summarized using proportions of participants endorsing the questions with categorical responses. Participants’ qualitative responses to how they felt about the screening process were coded into either positive/neutral or negative and quantitatively summarized using proportions. Participants’ qualitative responses were also analysed for emergent themes, with illustrative quotes representing the themes.
Results
Description of sample
Over the two-month study period, healthcare workers in the clinic referred 71 participants for screening. One participant declined to participate in the study, and 70 agreed to participate and completed the study instrument. Most of the participants were referred to the study from the counseling sub-clinic (76%, n=53), and the remaining were referred from the Wellness sub-clinic (24%, n=17). Of the 53 participants recruited from the counseling sub-clinic, 27 were attending ART readiness counseling sessions and 26 were attending ART adherence counseling sessions for defaulters. Thus, participants were either initiating or defaulting on ART. Table 1 summarizes the demographic and other characteristics of the participants, by traumatic experiences. There were no statistically significant differences in characteristics between those who had a trauma history (sexual abuse and/or physical IPV) and those without a trauma history.
Table 1.
Sample demographics and related characteristics
| Characteristic | Overall (n= 70) |
Trauma history (n = 57) |
No trauma history (n= 13) |
|---|---|---|---|
| Age (yrs.) | |||
| Mean (SD) | 31.6 (9.5) | 32.5 (9.9) | 27.5 (5.4) |
| Education (highest level) | |||
| =< Grade 7, n (%) | 7 (10) | 6 (10.5) | 1 (7.7) |
| Grade 8-11, n (%) | 42 (60) | 35 (61.4) | 7 (53.8) |
| Completed high school, n (%) | 20 (28.6) | 15 (26.3) | 5 (38.4) |
| Post-secondary education, n (%)Years of education | 1 (1.4) | 1 (1.8) | 0 (0) |
| Mean (SD) | 10.4 (1.9) | 10.2 (2.0) | 11 (1.3) |
| Employment | |||
| Employed, n (%) | 26 (37.1) | 20 (35.0) | 6 (46.1) |
| Relationship status | |||
| Single, n (%) | 12 (17.1) | 11 (19.2) | 1 (7.7) |
| Partner, n (%) | 39 (55.7) | 29 (50.8) | 10 (76.9) |
| Married, n (%) | 11 (15.7) | 9 (15.7) | 2 (15.3) |
| Divorced, n (%) | 8 (11.4) | 8 (8.8) | 0 (0) |
| Current partner | 50 (71.4) | 38 (66.6) | 12 (92.3) |
| Pregnancy | |||
| Pregnant, n (%) | 3 (4.3) | 2 (3.5) | 1 (7.7) |
| Time since HIV diagnosis (yrs.) | |||
| =< 2, n (%) | 38 (54.2) | 27 (47.3) | 11 (84.6) |
| 3-5, n (%) | 15 (21.4) | 13 (22.8) | 2 (15.4) |
| >5, n (%) | 17 (24.2) | 17 (11.1) | 0 (0) |
No statistically significant differences between participants who had a trauma history and those without a trauma history
Prevalence of trauma experiences
Both sexual abuse and physical IPV were highly prevalent in the sample. Most notably, 81% of the sample had a lifetime experience of either sexual abuse or physical IPV, with high rates of overlap between the two experiences (Figure 1). Over half of all participants (51%, 36/70) reported a lifetime experience of sexual abuse, of whom 25% (9/36) reported that the sexual abuse was currently ongoing or occurred within the past year. Most of the reported sexual abuse occurred in adulthood and adolescence, with only 11% (4/36) of experiences reported in childhood (Figure 2). Multiple forms of abuse throughout the life course were common.
Figure 1.
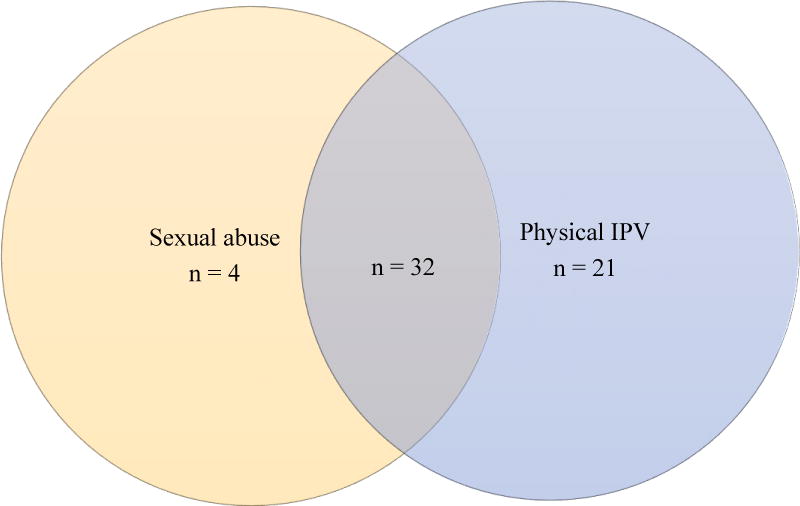
Overlap of sexual abuse and physical IPV among women with trauma history (n=57)1
113 women screened did not report a history of trauma
Figure 2.
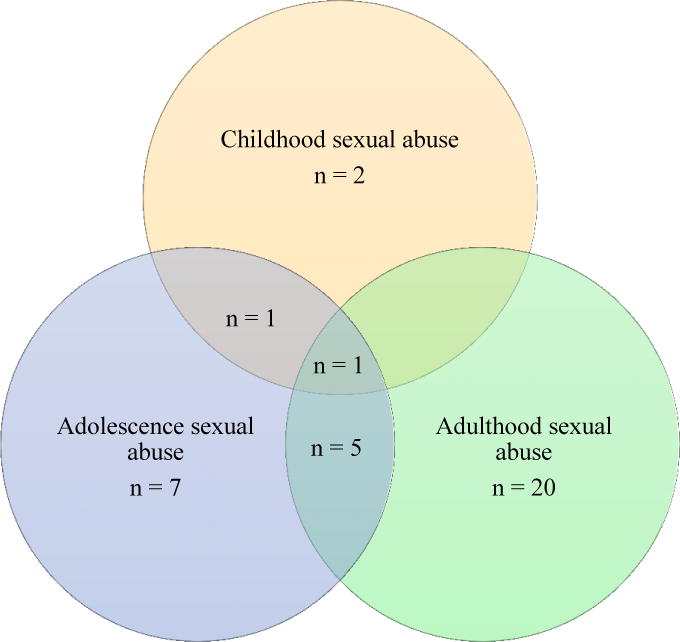
Overlap in sexual abuse experiences across the lifetime among women with sexual abuse history (n=36)1
134 women screened did not report sexual abuse
Three-quarters of participants (75%, 53/70) reported a lifetime experience of physical IPV, of whom 22% (12/53) reported experiencing physical IPV within the last six months. Of the sample of 70, only 13 participants (19%) had no history of trauma, 25 participants (36%) had one type of trauma (either sexual or physical IPV), and 32 participants (46%) had both sexual and physical IPV trauma. Of the 25 participants with one type of trauma, 21 of them had physical IPV and only 4 participants had sexual abuse only. No participant endorsed only the fourth sexual abuse item (whether they had ever had any other unwanted or threatening sexual experiences); thus, no participant was categorizeed as having sexual abuse based on this item alone.
Prevalence of mental health symptoms
Over one-third of participants (36%, 26/70) met screening criteria indicative of major depression. Among the 57 participants who had a trauma history (either sexual and/or physical IPV) and thus were screened for PTSD, 70% (40/57) met screening criteria that were indicative of elevated PTSD symptoms. Table 2 summarizes the prevalence of mental health symptoms by trauma history.
Table 2.
Mental health symptoms by trauma historya
| Measure | No trauma (n=13) |
Sexual abuse or physical IPV (n=25) |
Sexual abuse and physical IPV (n=32) |
P value |
|---|---|---|---|---|
| Elevated depression symptoms (%) | 15.3% | 20.0% | 59.3% | 0.002* |
| Mean score (SD) | 1.3 (1.8) | 1.7 (1.7) | 3.0 (1.9) | |
| Elevated PTSD symptoms (%) | N/A | 60.0% | 78.0% | 0.157 |
| Mean score (SD) | N/A | 3.0 (2.3) | 4.1 (2.2) |
Depression based on score of ≤ 3; PTSD based on score of ≤ 3.
p < 0.05
Association between trauma and depression
Table 3 summarizes the results of a logistic regression model predicting odds of elevated depression. Age and education were not associated with meeting screening criteria for depression. The odds of depression among women with either sexual abuse or physical IPV alone were not significantly different from the odds for women with no trauma experience. The odds of meeting the screening criteria for major depression for women with both sexual abuse and physical IPV were 8.11 times larger (OR = 8.11; 95% CI 1.48-44.34), compared with the odds for women with no trauma experience.
Table 3.
Association between depression and experiences of traumaa (n=70)
| Odds Ratio | 95% CI | P value | |
|---|---|---|---|
| Age | 0.99 | 0.93 – 1.05 | 0.787 |
| Education | 0.92 | 0.67 – 1.24 | 0.596 |
| Trauma experience | |||
| No trauma | [REF] | ||
| Sexual abuse or physical IPV | 1.30 | 0.21 - 8.10 | 0.773 |
| Sexual abuse and physical IPV | 8.11 | 1.48 – 44.34 | 0.016* |
No trauma = referent group
p < 0.05
Participants’ screening experiences
Participants’ perspectives on the screening process are summarized in Table 4. Almost all participants agreed to participate in the study and completed the entire study instrument. Among participants reporting sexual abuse, 61% were disclosing their experience for the first time; 31% of women with physical IPV experience were disclosing for the first time. Most participants viewed the screening process as an opportunity to speak about their experience and reported that it helped reduce their psychological distress. For example, a 41 years old participant with a history of physical IPV said: “I felt relieved, I really feel like telling people what happened because I want to move on and forget about my past”. However, a small portion (10%) of participants mentioned, that in combination with the positive sentiment, the questions elicited some distress and reflection while recalling their experiences. For example, a 23 years old participant with a history of sexual abuse and physical IPV said: “I feel a bit of relief, but at the same time I feel like crying. These are things I thought I am forgetting, trying to forget about. I want to move on”.
Table 4.
Participants’ screening experiences
| Question | Proportion of endorsement/response | ||
|---|---|---|---|
| Overall (n= 70) |
Trauma history (n=57) |
No trauma history (n= 13) |
|
| Acceptability of screening | |||
| Agreeing to screening | 98% a (70/71) | 100% (n=57/57) | 100% (n=13/13) |
| Disclosing sexual abuse for the first time | N/A | 61% (22/36)b | N/A |
| Disclosing physical IPV for the first time | N/A | 33% (18/53)b | N/A |
| Agree screening should be routine for women | 98% (69/70) | 100% (57/57) | 92% (12/13) |
| Emotional impact of screening | |||
| Screening had positive/neutral emotional impact | 88% (62/70) | 85% (49/57) | 100% (13/13) |
| Potential role of healthcare workers in screening | |||
| Would be comfortable with a nurse or counsellor conducting screening | 98% (69/70) | 100% (57/57) | 92% (12/13) |
| Would prefer being screened by a counsellor vs. a nurse | 81% (n =57/70) | 89% (51/57) | 46% (6/13) |
Percentage calculated on 71 referred to the study, overall sample in rest of table reports on final sample of 70 women who agreed to participate in study
Proportion based on those with the specific trauma experience in the question
Participants almost unanimously agreed that it would be appropriate and acceptable to screen all women in the clinic setting for trauma and mental health symptoms (98.6%, 69/70). The perceived therapeutic effect of the screening process was the main reason why participants thought universal screening in the clinic, as part of routine care, was important and would be acceptable to women. Another reason was the difficulty of discussing trauma and mental health with their friends/family. For example, a 45 years old participant with a history of physical IPV said: “Women will be able to speak about their problems. To talk out about your problems brings some kind of relief. Most people feel reluctant to speak to family members, [but] they might feel comfortable talking to someone at the clinic”.
Participants expressed comfort with having this type of screening conducted either by a nurse or by a counsellor in the clinic. However, 81.4% (57/70) participants expressed a preference for the screening to be conducted by a counsellor. Participants preferred being screened by counsellors because they saw it as a more “natural” role for them, preferring to receive medical advice from nurses and psychosocial advice from the counsellors. Others cited the nurses’ busy workload as reasons why it would be more appropriate for counsellors to conduct the screening. For example, a 41 years old participant with a history of physical IPV said: “Counsellors take time to speak with people and make people understand. The nurses are always busy running around attending to patients, so they don’t really have time to sit down and listen to each and every patient”.
Discussion
In conducting brief screening for traumatic experiences and related mental health distress among a small cross-sectional sample of women attending a public HIV clinic in Cape Town, South Africa, we found very high prevalence of lifetime sexual abuse or physical IPV, along with high prevalence of depression and PTSD symptoms. Screening was viewed by patients as highly acceptable and potentially therapeutic, many of whom had disclosed their traumatic experiences for the first time.
The prevalence of sexual abuse and/or physical IPV found in this study (81%) is on the high end of the range found in previous studies that have examined traumatic experiences among South African women (Dunkle, Jewkes, Brown, Gray, et al., 2004; Dunkle, Jewkes, Brown, Yoshihama, et al., 2004; Zembe et al., 2015, Bernstein et al., 2016). The prevalence of PTSD found in this study, among the subset of participants with sexual abuse and/or physical IPV experience, is higher than estimates of those found in a review of six previous studies among HIV positive populations in South Africa (Young, 2011). Notable differences in those prior studies included the HIV diagnosis as the traumatic event and the use of diagnostic interviews for PTSD, in contrast to the brief, non-diagnostic screening used in this study. Thus, it is not known whether higher prevalence of PTSD symptoms in this study is due to the presence of traumatic experience(s) or the use of a screening as opposed to a diagnostic procedure.
The prevalence of depression in this screening study is comparable to that found in prior studies among HIV positive populations in South Africa (Cholera et al., 2016; Pappin, Wouters, & Booysen, 2012; Ramirez-Avila et al., 2012). Depression was significantly associated with experiences of both sexual abuse and physical IPV, but not the experience of physical IPV alone. This result suggests that, in relation to depression, either the combination of traumatic experiences or the unique impact of sexual abuse is contributing to the elevated levels of depression. The overall high prevalence of physical IPV in the sample, and some research suggesting societal normalization and cultural acceptance of physical IPV (Joyner & Mash, 2012; Norman et al., 2007; Rees, Zweigenthal, & Joyner, 2014), could be reasons why physical IPV alone is not significantly associated with depression. It is important to note, this difference in level of symptomatology was not found in PTSD, which was elevated regardless of type of traumatic experience(s).
The high proportion of women disclosing their traumatic experiences for the first time, expressing a positive emotional impact of the screening, and agreeing that screening should be universal suggests that screening is acceptable. A high proportion of women expressed comfort with similar screening being conducted by healthcare workers, suggesting that screening could be integrated into clinical care. However, there is need to consider whether anonymity in the context of a research study contributed to the willingness by participants to disclose. Many women reported a perceived therapeutic effect of talking about their traumatic experiences and mental health, suggesting that screening, coupled with referral to services, can improve their wellbeing.
Healthcare workers referred HIV positive women to the study using a brief recruitment script, suggesting they could play a role in screening as part of an integrated care model similar to one implemented in a South African antenatal setting (Vythilingum et al., 2013b). However, healthcare provider shortages, work overburden observed in the study setting, and lack of mental health professionals might play a role in providers’ willingness to ask patients about trauma and mental health. Moreover, there is a need to understand healthcare workers’ perspectives on trauma and mental health and whether it is feasible and acceptable to patients for health care workers to conduct the screening.
Beyond integrating screening into HIV care, there is a need to consider how to link at risk women to psychological services and intervention. Study staff referred participants with elevated psychological distress to the social worker and psychologist at the clinic. The increased referrals ensuing from integrating screening into care may exceed the resource capacity of these specialist healthcare providers, hence the need to consider involving non-specialists, such as counsellors or peers, in delivery of evidence-based psychological interventions.
A number of study limitations must be noted. The study had a modest sample size and focused on the subset of women who were initiating or defaulting on ART, and thus might not be representative of the general HIV patient population in this setting. The sample was obtained through healthcare worker referrals, and although patients were not informed of the focus of the study, there might be differences between women who were referred to the study and those who were not referred or who declined referral to the study. PTSD symptoms were assessed in association with participant’s sexual abuse and physical IPV exposure, however it is possible that symptoms could be related to other events; the cross-sectional design limits conclusions of causality. Future studies should examine mental health outcomes in relation to other traumatic events and establish the differential impact that multiple traumas have on mental health outcomes. Furthermore, this study focused screening on sexual abuse and physical IPV, due to the brief nature of the screening. However, as noted earlier, other forms of violence against women are prevalent in this setting and should be investigated further. Finally, although the measures used to assess mental health were validated screening instruments, they were not diagnostic in nature.
In conclusion, the high prevalence of traumatic experiences and psychological distress in this study highlights an urgent need to integrate screening into routine HIV care. The study provides evidence of the acceptability of screening for trauma and mental health symptoms among HIV positive women, at the critical points of care engagement when they are initiating ART or have defaulted on ART. Additionally, there is need to link women screened to interventions and services, as part of trauma informed HIV care. Thus, policymakers should consider broader implementation of screening in HIV care settings and mobilize resources to provide treatment and services. To consolidate gains made in HIV treatment and stem the HIV care engagement cascade, it is necessary to integrate trauma and mental health treatment into HIV care.
Footnotes
Note that the word “trauma” is used throughout the paper to refer broadly to acts of sexual abuse and/or physical IPV experienced by participants. In using this word, we are referring to trauma exposure, as opposed to implying corresponding trauma symptoms. We also use the phrases “trauma history” and “traumatic experiences” interchangeably in the same way.
References
- Abrahams N, Jewkes R, Hoffman M, Laubsher R. Sexual violence against intimate partners in Cape Town: prevalence and risk factors reported by men. Bull World Health Organ. 2004;82(5):330–337. [PMC free article] [PubMed] [Google Scholar]
- Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Hatcher S. Validation of PHQ-2 and PHQ-9 to Screen for Major Depression in the Primary Care Population. Annals of Family Medicine. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arroll B, Goodyear-Smith F, Crengle S, Gunn J, Kerse N, Fishman T, Hatcher S. Validation of PHQ-2 and PHQ-9 to screen for major depression in the primary care population. Ann Fam Med. 2010;8(4):348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bernstein M, Phillips T, Zerbe A, McIntyre JA, Brittain K, Petro G, Myer L. Intimate partner violence experienced by HIV-infected pregnant women in South Africa: a cross-sectional study. BMJ Open. 2016;6(8) doi: 10.1136/bmjopen-2016-011999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhana A, Rathod SD, Selohilwe O, Kathree T, Petersen I. The validity of the Patient Health Questionnaire for screening depression in chronic care patients in primary health care in South Africa. BMC Psychiatry. 2015;15:118. doi: 10.1186/s12888-015-0503-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Peterson EL, Kessler RC, Schultz LR. Short screening scale for DSM-IV posttraumatic stress disorder. American Journal of Psychiatry. 1999;156(6):908–911. doi: 10.1176/ajp.156.6.908. [DOI] [PubMed] [Google Scholar]
- Brezing C, Ferrara M, Freudenreich O. The syndemic illness of HIV and trauma: implications for a trauma-informed model of care. Psychosomatics. 2015;56(2):107–118. doi: 10.1016/j.psym.2014.10.006. [DOI] [PubMed] [Google Scholar]
- Choi KW, Abler LA, Watt MH, Eaton LA, Kalichman SC, Skinner D, Sikkema KJ. Drinking before and after pregnancy recognition among South African women: the moderating role of traumatic experiences. BMC Pregnancy and Childbirth. 2014;14(1):1–9. doi: 10.1186/1471-2393-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cholera R, Pence BW, Gaynes BN, Bassett J, Qangule N, Pettifor A, Miller WC. Depression and Engagement in Care Among Newly Diagnosed HIV-Infected Adults in Johannesburg, South Africa. AIDS Behav. 2016 doi: 10.1007/s10461-016-1442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Holman AR, Freeman MC, Patel V. What is the relevance of mental health to HIV/AIDS care and treatment programs in developing countries? A systematic review. Aids. 2006;20(12):1571–1582. doi: 10.1097/01.aids.0000238402.70379.d4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dartnall E, Jewkes R. Sexual violence against women: The scope of the problem. Best Practice & Research Clinical Obstetrics & Gynaecology. 2013;27(1):3–13. doi: 10.1016/j.bpobgyn.2012.08.002. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet. 2004;363(9419):1415–1421. doi: 10.1016/s0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Yoshihama M, Gray GE, McIntyre JA, Harlow SD. Prevalence and patterns of gender-based violence and revictimization among women attending antenatal clinics in Soweto, South Africa. Am J Epidemiol. 2004;160(3):230–239. doi: 10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes RK, Brown HC, Yoshihama M, Gray GE, McIntyre JA, Harlow SD. Prevalence and Patterns of Gender-based Violence and Revictimization among Women Attending Antenatal Clinics in Soweto, South Africa. American Journal of Epidemiology. 2004;160(3):230–239. doi: 10.1093/aje/kwh194. [DOI] [PubMed] [Google Scholar]
- Fleming K, Kruger L-M. She keeps his secrets: A gendered analysis of the impact of shame on the non-disclosure of sexual violence in one low-income South African community. African Safety Promotion Journal. 2013;11(2):107–124. [Google Scholar]
- Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H. Intimate partner violence and engagement in HIV care and treatment among women: a systematic review and meta-analysis. Aids. 2015;29(16):2183–2194. doi: 10.1097/qad.0000000000000842. [DOI] [PubMed] [Google Scholar]
- Honikman S, van Heyningen T, Field S, Baron E, Tomlinson M. Stepped Care for Maternal Mental Health: A Case Study of the Perinatal Mental Health Project in South Africa. PLoS Medicine. 2012;9(5):e1001222. doi: 10.1371/journal.pmed.1001222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: an overview. Soc Sci Med. 2002;55(7):1231–1244. doi: 10.1016/s0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: an overview. Social Science & Medicine. 2002;55(7):1231–1244. doi: 10.1016/S0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Levin J, Penn-Kekana L. Risk factors for domestic violence: findings from a South African cross-sectional study. Social Science & Medicine. 2002;55(9):1603–1617. doi: 10.1016/S0277-9536(01)00294-5. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Penn-Kekana L, Levin J, Ratsaka M, Schrieber M. Prevalence of emotional, physical and sexual abuse of women in three South African provinces. S Afr Med J. 2001;91(5):421–428. [PubMed] [Google Scholar]
- Joyner K, Mash B. A comprehensive model for intimate partner violence in South African primary care: action research. BMC Health Services Research. 2012;12(1):1–10. doi: 10.1186/1472-6963-12-399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminer D, Grimsrud A, Myer L, Stein DJ, Williams DR. Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in South Africa. Soc Sci Med. 2008;67(10):1589–1595. doi: 10.1016/j.socscimed.2008.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling R, Ouimette P, Prins A, Nisco P, Lawler C, Cronkite R, Moos RH. BRIEF REPORT: Utility of a Short Screening Scale for DSM-IV PTSD in Primary Care. Journal of General Internal Medicine. 2006;21(1):65–67. doi: 10.1111/j.1525-1497.2005.00292.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knobel H, Carmona A, Grau S, Pedro-Botet J, Díez A. ADherence and effectiveness of highly active antiretroviral therapy. Archives of Internal Medicine. 1998;158(17):1953–1953. doi: 10.1001/archinte.158.17.1953. [DOI] [PubMed] [Google Scholar]
- Lamiraud K, Moatti JP, Raffi F, Carrieri MP, Protopopescu C, Michelet C, Spire B. Adherence to and effectiveness of highly active antiretroviral treatment for HIV infection: assessing the bidirectional relationship. Med Care. 2012;50(5):410–418. doi: 10.1097/MLR.0b013e3182422f61. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, Dunbar GC. The Mini International Neuropsychiatric Interview (MINI) A short diagnostic structured interview: reliability and validity according to the CIDI. European Psychiatry. 1997;12(5):224–231. doi: 10.1016/S0924-9338(97)83296-8. [DOI] [Google Scholar]
- Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosom Med. 2005;67(3):500–507. doi: 10.1097/01.psy.0000160459.78182.d9. [DOI] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. J Int AIDS Soc. 2014;17:18845. doi: 10.7448/ias.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From treatment to healing: the promise of trauma-informed primary care. Womens Health Issues. 2015;25(3):193–197. doi: 10.1016/j.whi.2015.03.008. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Wilson TC, Haberer JE, Weiss DS. Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav. 2012;16(8):2091–2100. doi: 10.1007/s10461-011-0127-4. [DOI] [PubMed] [Google Scholar]
- Marais DL, Petersen I. Health system governance to support integrated mental health care in South Africa: challenges and opportunities. International Journal of Mental Health Systems. 2015;9(1):1–21. doi: 10.1186/s13033-015-0004-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Hansen NB, Kochman A, Sikkema KJ. Utilization of medical treatments and adherence to antiretroviral therapy among HIV-positive adults with histories of childhood sexual abuse. AIDS Patient Care STDS. 2009;23(4):259–266. doi: 10.1089/apc.2008.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, Leserman J, Swartz M, Stangl D, Thielman N. Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care STDS. 2006;20(6):418–428. doi: 10.1089/apc.2006.20.418. [DOI] [PubMed] [Google Scholar]
- Norman R, Bradshaw D, Schneider M, Jewkes R, Mathews S, Abrahams N, Vos T. Estimating the burden of disease attributable to interpersonal violence in South Africa in 2000. South African Medical Journal. 2007;97:653. [PubMed] [Google Scholar]
- O’Cleirigh C, Skeer M, Mayer KH, Safren SA. Functional impairment and health care utilization among HIV-infected men who have sex with men: the relationship with depression and post-traumatic stress. J Behav Med. 2009;32(5):466–477. doi: 10.1007/s10865-009-9217-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappin M, Wouters E, Booysen FL. Anxiety and depression amongst patients enrolled in a public sector antiretroviral treatment programme in South Africa: a cross-sectional study. BMC Public Health. 2012;12(1):1–9. doi: 10.1186/1471-2458-12-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piot P, Abdool Karim SS, Hecht R, Legido-Quigley H, Buse K, Stover J, Sidibe M. Defeating AIDS–advancing global health. Lancet. 2015;386(9989):171–218. doi: 10.1016/s0140-6736(15)60658-4. [DOI] [PubMed] [Google Scholar]
- Ramirez-Avila L, Regan S, Giddy J, Chetty S, Ross D, Katz JN, Bassett IV. Depressive Symptoms and Their Impact on Health-seeking Behaviors in Newly-diagnosed HIV-infected Patients in Durban, South Africa. AIDS and behavior. 2012;16(8):2226–2235. doi: 10.1007/s10461-012-0160-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees K, Zweigenthal V, Joyner K. Implementing intimate partner violence care in a rural sub-district of South Africa: a qualitative evaluation. 2014;2014:7. doi: 10.3402/gha.v7.24588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seedat S. Interventions to improve psychological functioning and health outcomes of HIV-infected individuals with a history of trauma or PTSD. Curr HIV/AIDS Rep. 2012;9(4):344–350. doi: 10.1007/s11904-012-0139-3. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Meade CS, Ranby KW, Kalichman SC, Skinner D, Pieterse D. Mental health and HIV sexual risk behavior among patrons of alcohol serving venues in Cape Town, South Africa. J Acquir Immune Defic Syndr. 2011a;57(3):230–237. doi: 10.1097/QAI.0b013e3182167e7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikkema KJ, Watt MH, Meade CS, Ranby KW, Kalichman SC, Skinner D, Pieterse D. Mental health and HIV sexual risk behavior among patrons of alcohol serving venues in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndromes. 2011b;57(3):230–237. doi: 10.1097/QAI.0b013e3182167e7a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smit J, Myer L, Middelkoop K, Seedat S, Wood R, Bekker LG, Stein DJ. Mental health and sexual risk behaviours in a South African township: a community-based cross-sectional study. Public Health. 2006;120(6):534–542. doi: 10.1016/j.puhe.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2): Development and Preliminary Psychometric Data. Journal of Family Issues. 1996;17(3):283–316. doi: 10.1177/019251396017003001. [DOI] [Google Scholar]
- UNAIDS. HIV and AIDS estimates. 2015. Retrieved from. [Google Scholar]
- Undie CC, Maternowska MC, Mak’anyengo M, Askew I. Is Routine Screening for Intimate Partner Violence Feasible in Public Health Care Settings in Kenya? J Interpers Violence. 2016;31(2):282–301. doi: 10.1177/0886260514555724. [DOI] [PubMed] [Google Scholar]
- Vythilingum B, Field S, Kafaar Z, Baron E, Stein DJ, Sanders L, Honikman S. Screening and pathways to maternal mental health care in a South African antenatal setting. Archives of Women’s Mental Health. 2013a;16(5):371–379. doi: 10.1007/s00737-013-0343-1. [DOI] [PubMed] [Google Scholar]
- Vythilingum B, Field S, Kafaar Z, Baron E, Stein DJ, Sanders L, Honikman S. Screening and pathways to maternal mental health care in a South African antenatal setting. Arch Womens Ment Health. 2013b;16(5):371–379. doi: 10.1007/s00737-013-0343-1. [DOI] [PubMed] [Google Scholar]
- Watt MH, Dennis AC, Choi KW, Ciya N, Joska JA, Robertson C, Sikkema KJ. Impact of Sexual Trauma on HIV Care Engagement: Perspectives of Female Patients with Trauma Histories in Cape Town, South Africa. AIDS Behav. 2016:1–10. doi: 10.1007/s10461-016-1617-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Western Cape Department of Health. The Western Cape Consolidated Guidelines for HIV Treatment: Prevention of Mother-to-Child Transmission of HIV (PMTCT), Children, Adolescents and Adults. 2015 Retrieved from. [Google Scholar]
- Whetten K, Shirey K, Pence BW, Yao J, Thielman N, Whetten R, CRT Trauma History and Depression Predict Incomplete Adherence to Antiretroviral Therapies in a Low Income Country. PLoS ONE. 2013;8(10):e74771. doi: 10.1371/journal.pone.0074771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetten K, Shirey K, Pence BW, Yao J, Thielman N, Whetten R, Reddy E. Trauma history and depression predict incomplete adherence to antiretroviral therapies in a low income country. PLoS One. 2013;8(10):e74771. doi: 10.1371/journal.pone.0074771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willie TC, Overstreet NM, Sullivan TP, Sikkema KJ, Hansen NB. Barriers to HIV Medication Adherence: Examining Distinct Anxiety and Depression Symptoms among Women Living with HIV Who Experienced Childhood Sexual Abuse. Behav Med. 2016;42(2):120–127. doi: 10.1080/08964289.2015.1045823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview. Geneva, Switzerland: 1990. Retrieved from. [Google Scholar]
- Young C. Understanding HIV-related posttraumatic stress disorder in South Africa: a review and conceptual framework. African Journal of AIDS Research (AJAR) 2011;10(2):139. doi: 10.2989/16085906.2011.593376. [DOI] [PubMed] [Google Scholar]
- Zembe YZ, Townsend L, Thorson A, Silberschmidt M, Ekstrom AM. Intimate Partner Violence, Relationship Power Inequity and the Role of Sexual and Social Risk Factors in the Production of Violence among Young Women Who Have Multiple Sexual Partners in a Peri-Urban Setting in South Africa. PLoS One. 2015;10(11):e0139430. doi: 10.1371/journal.pone.0139430. [DOI] [PMC free article] [PubMed] [Google Scholar]


