Abstract
Background
Postpartum Depression affects a considerable number of women worldwide. This condition inflicts severe consequences to mother and child health. Thus far, available treatments have low response and high relapse rates. We designed this trial to evaluate a safe and more efficacious innovative therapy.
Aims
To report a feasible and ethical study design to assess the safety and efficacy of a high frequency repetitive Transcranial Magnetic Stimulation 10 Hz (rTMS) compared to sham rTMS in women with moderate to severe Post-Partum Depression using standard treatment (sertraline).
To conduct an ancillary, exploratory, randomized, active controlled, double blind study with a hypothesis to assess the safety and efficacy of 10 Hz rTMS compared to sertraline.
Methods
A multicenter, parallel arm, randomized, placebo-controlled, double-blind design to assess safety and efficacy of 10 Hz rTMS compared to sham.
An ancillary study will be conducted with parallel arm, randomized, active controlled and double dummy design to assess safety and efficacy of 10 Hz rTMS compared to sertraline.
Keywords: Postpartum depression, repetitive Transcranial Magnetic Stimulation, Research clinical trial
1. Introduction
As of 2012, the Diagnostic and Statistical Manual of Mental Disorders-5 redefined postpartum depression (PPD) as a subset of Major Depressive Disorder (MDD) persistent up to 4 weeks after delivery with a peripartum onset [1]. Although MDD and PPD share many clinical similarities, a meta-analysis of 11 randomized clinical trials showed differences between the diseases on neuroimaging, gonadal steroidal hormone involvement, and response to treatments [2].
Postpartum Depression has a prevalence of 14% in the general population of pregnant women [3]. It is responsible for maternal suicide and infanticide in the most severe cases [4]. Studies have shown that PPD impairs maternal-newborn bond producing a greater risk of child abuse and negligence; resulting in irreversible cognitive and social deficits later in child life [3], [5]. Postpartum depression is the number one cause of maternal morbidity after childbirth [6].
The first-line therapy for moderate to severe PPD is of Selective Serotonin Reuptake Inhibitor (SSRI) such as sertraline [3], [7]. Although it is considered relatively safe for breastfeeding, mothers still have a concern regarding newborn consumption of drug metabolites in the breast milk compromising treatment adherence [8], [9]. Additionally, the efficacy of SSRI has come into question with low response rates and high relapse rates. High latency to response of these SSRI also plays an important role for this population and reconciling the mother-to-child bond. Hence there is a need to test new therapies for this specific population.
Repetitive Transcranial Magnetic Stimulation (rTMS) is a noninvasive brain stimulation technique that has been FDA approved in the treatment of refractory MDD [10]. rTMS functions by eliciting focal magnetic waves to the brain. It induces neuroplasticity by promoting synaptogenesis in targeted cortical areas [11]. Low frequency rTMS stimulates inhibitory GABA neurons while high frequency stimulates the excitatory neurons. This treatment modality combined with standard therapy has demonstrated a faster response in MDD compared to standard therapy alone [12]. This results in a reduced exposure to SSRI adverse effects.
Only two pilot studies thus far have evaluated the effects of rTMS in PPD patients. Both trials showed safety and positive results of combined therapy of rTMS and SSRI [13], [14]. This warrants further investigation of this treatment modality as a viable option in women with PPD to modulate the effect of standard therapy by increasing its efficacy. It has potential to reduce time to response and adverse effect profile of treatment.
In this trial, we aim to investigate the safety and efficacy of high frequency rTMS (10 Hz) compared to sham rTMS in women with moderate to severe PPD using standard therapy (sertraline). This would pave the way towards finding a safe and efficacious evidence-based therapy for postpartum depression and with a better safety profile than standard therapy alone. By adding a third arm, we also aim to conduct an ancillary, exploratory, double dummy study [23] to assess the safety and efficacy of rTMS compared to Sertraline. To our knowledge, this direct comparison has never been evaluated in patients with postpartum depression and would provide a basis for future trials.
2. Methods
2.1. Trial design
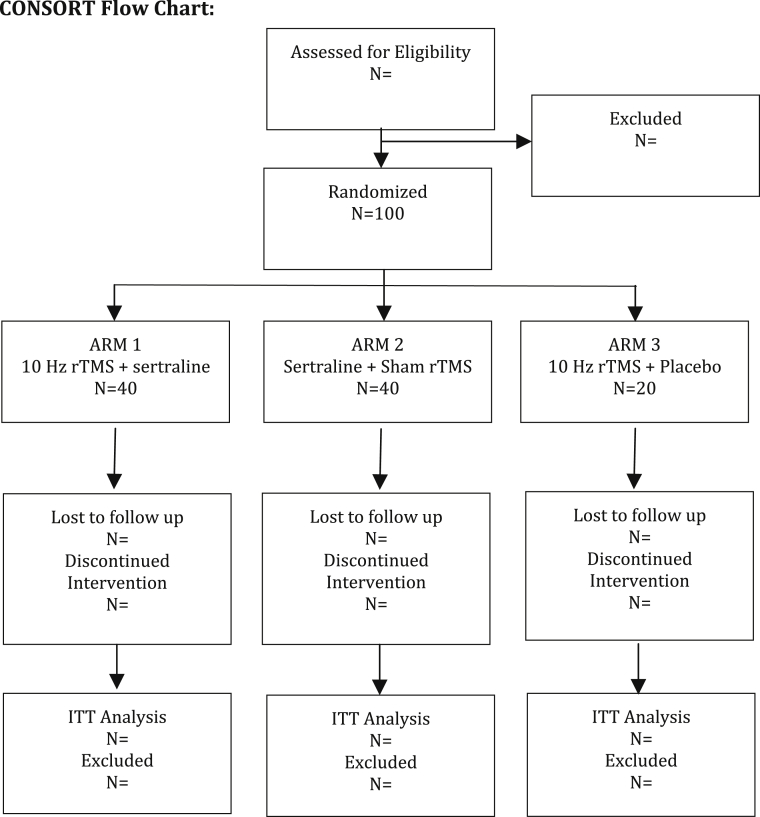
A multicenter, parallel arm, randomized, placebo-controlled, double-blind study design to assess safety and efficacy of 10 Hz rTMS compared to sham rTMS in postpartum depressed patients using standard treatment (sertraline). A third arm with patients using 10 Hz rTMS + placebo is needed to address the ancillary hypothesis. The ancillary study will be conducted as a parallel arm, randomized, active controlled and double dummy design to assess safety and efficacy of 10 Hz rTMS compared to sertraline. Subjects will be randomly allocated to either arm 1, 2 or 3 in a 2:2:1 ratio by random blocks of 3 or 6 subjects. Stratification will be done to control for study center.
Treatment will start after delivery once our screening process confirms PPD. Active and sham rTMS will be administered for a 6 weeks Treatment Phase and a 6 weeks Maintenance Phase following pivotal trial and FDA guidelines for TMS and Major Depression [10]. 50 mg Sertraline and placebo will be given for 12 weeks duration with possible increase of an additional 50 mg.
2.2. Participants
Women over 18 years of age, with moderate to severe PPD (based on HAMD-17 scale score >18) will be included. We will exclude patients based on three broad categories of contraindications for rTMS, contraindications for SSRI therapy (for safety), and based on confounders that may affect our outcomes. Table 1 summarizes the eligibility criteria.
Table 1.
Eligibility criteria.
| Inclusion |
| Females who have completed delivery |
| >18 years old |
| Confirmed PPD diagnosis by DSM-5 criteria |
| Moderate to Severe Depression by score of >18 score on HAM-D17 scale |
| Exclusion |
| rtms contraindications |
| Previous Stroke, Seizure or CNS Disease |
| Previous or current drug or alcohol abuse |
| Ferromagnetic metallic implants |
| SSRI therapy contraindications |
| Bipolar Depression or previously diagnosed mental health disorder |
| Allergy to components of the medication |
| History of Liver or kidney Disease |
| Other exclusions |
| Previous 6 month treatment with SSRI or rTMS prior to randomization |
| Suicidal ideation and History of suicidal attempt |
| Puerperal blues |
| Secondary causes of Depression (e.g. Hypothyroidism, Sheehan Syndrome etc.) |
2.2.1. Study setting
In order to achieve sufficient generalizability of the results, and to ease the burden of recruitment, this trial will be a multicenter trial. To our knowledge, this is the first multi-center trial testing the safety and efficacy of rTMS in PPD patients. The trial will be conducted at four study sites in USA, Brazil, Portugal and Turkey.
2.2.2. Study site eligibility criteria
-
1.
All necessary equipment and infrastructure available, including qualified, trained and licensed staff, rooms, laboratory with necessary equipment for rTMS.
-
2.
Proven ability to reach recruitment milestones by access to our target patient population.
-
3.
Approval from the Ethical Committee of each site
2.3. Intervention
In our trial, active rTMS (Arms 1 and 3) or sham rTMS (Arm 2) will be applied to the Left Dorsolateral Prefrontal Cortex (LDLPFC) of all patients. The left DLPFC is a common target for rTMS and has been used in several major trials that proved efficacy in MDD [13], [14], [15]. We will localize the LDLPFC by using the “5 cm rule” [16], a standard procedure to accurately find the LDLPFC for the application of rTMS.
The rTMS protocol recommended by the FDA [17] calls for a treatment phase of 30 sessions over 6 weeks followed by a tapered 6-week maintenance phase of 7 sessions. The schedule of sessions can be found in Table 2. Patients will undergo a total of 37 sessions of 10 Hz rTMS stimulation to their LDLPFC as follows: 75 trains (3000 pulses) per day, each train lasted 4 s and 26 s off between trains, for a total of 37.5 min. Sham rTMS in Arm 2 will follow an identical schedule and will mimic the active intervention. The equipment to be use is the MagVenture MagPro R380. Due to its manufacturing features, it is possible to apply sham and active rTMS, maintaining our double blind study design.
Table 2.
Treatment phases.
| Time | Frequency of rTMS administration | |
|---|---|---|
| Treatment phase | Week 1–6 | 5 times per week |
| Maintenance phase | Week 7 | 3 times per week |
| Week 8 | 2 times per week | |
| Week 9 | 1 time per week | |
| Week 11 | 1 time per week |
2.4. SSRI rationale & dosing
First line treatment of moderate to severe PPD is either Sertraline or Paroxetine. Although both drugs have shown no incidence of infant abnormalities [18], we referred to several systematic reviews and trials comparing SSRI metabolite content in breast milk and in infant serum and concluded that Sertraline had a slightly safer profile than Paroxetine [19]. Additionally, Psychiatric guidelines recommend the use of sertraline rather than paroxetine for PPD [8].
Thus, patients in all arms, will be given the initial dose of 50 mg Sertraline (Arms 1 & 2), or placebo (Arm 3) orally, once daily. The drug will be given at the same time as the rTMS procedure and patients will be given doses to take home during weekend. The dose of sertraline or placebo may be increased by 50 mg per week up to a total of 200 mg, if no improvement within two weeks as deemed by the recommendations of the Data Safety Monitoring Committee.
2.5. Outcome
Our primary endpoint is the absolute change in the 17 item Hamilton Depression Scale Score between patients in Arm 1 and Arm 2. For comparability with previous studies, this validated scale will be our primary outcome to assess efficacy of 10 Hz rTMS over sham rTMS.
Secondary endpoints include adverse event reporting, Edinburgh Post Natal Depression Scale (EPDS) changes, EEG changes, Cortical Silence Period (cSP), 36-Item Short Form Survey (SF-36) quality of life scale, and neurocognitive battery tests (Victoria Stroop, Wisconsin card sorting test, controlled oral word association test). Table 3 summarizes the data collection schedule for all the outcomes.
Table 3.
Time line for endpoints measurements.
| Week | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Outcome | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
| SF-36 | X | X | X | ||||||||||
| EPDS | X | X | X | ||||||||||
| HAMD-17 | X | X | X | X | X | X | X | X | X | X | X | X | |
| EEG | X | X | X | ||||||||||
| cSP | X | X | X | X | X | X | X | X | X | X | X | X | |
| Estrogen levels | X | X | X | X | X | ||||||||
| Safety lab tests | X | X | X | X | X | ||||||||
SF-36: 36-Item Short Form Survey (SF-36).
EPDS: Edinburgh Post Natal Depression Scale.
HAMD-17: 17-item Hamilton Scale.
EEG: Electroencephalogram.
cSP: Cortical Silence Period.
2.6. Randomization
Upon meeting eligibility criteria and signing informed consent, patients will be randomized in a 2:2:1 (Arm 1: Arm 2: Arm 3) ratio in random blocks of 3 or 6 participants per block. Randomization will be stratified by study center. A computer-generated randomization sequence will be issued and an outsider clinician will assign allocation by Interactive Voice Response System.
2.7. Blinding
Investigator, stimulator, assessors, patients, and study staff during the trial will be blinded. Blinded assessors will collect data such as HAM-D17 scale score, SF-36, EPDS, adverse event report.
In order to maintain blinding, sertraline will have a matched placebo pill (appearance, texture & taste). Both drugs will be administered in identical containers according to the treatment-code generated by computer randomization. An open label study pharmacist will dispense it.
The trained rTMS operator will be blinded. They will be responsible for applying rTMS treatment and to collect EEG and cSP data after each intervention. To maintain the blinding in this role, we will use the Mag Venture TMS device. This device has a two-sided coil; one side is for sham TMS and the other for the active treatment. Both procedures will appear identical. Upon entering the patient ID into the device, it will guide the stimulator to the unmarked appropriate positioning of the coil (sham or active) according to the pre-determined, saved randomization sequence. This feature ensures that the responsible for the brain stimulation remains blinded.
Blinding will be assessed at the end of the trial by a questionnaire completed by stimulators, assessors, investigators and patients. In case of patients dropping out of the study, those will be contacted and encouraged to complete the questionnaire.
2.8. Unblinding
In cases of Severe Adverse Effects (SAE), the Data Safety Monitoring Committee will provide guidance on the need for unblinding. The IVRS system accounts for a code breaking option that only the open label pharmacist has access to. In case of unblinding, investigator will keep records of the date, time, and reasons for unblinding and patient exclusion from the trial. Unblinding is authorized in cases of severe emergency that require information about treatment received by the patient in order to provide appropriate medical care. Unblinding information will only be revealed to study staff that is deemed necessary for patient safety.
2.8.1. Discontinuation/stoppage criteria
-
•Discontinuation from the study may occur under the following circumstances:
-
○Patient withdraws consent from the trial.
-
○Sudden or severe changes in the patient's psychiatric, neurological function or general medical condition related to the intervention(s) administered in the trial.
-
○Receiving external medical attention that are contraindication to the intervention administered in the trial.
-
○Non-compliance.
-
○
2.9. Sample size
Sample size was calculated to have 80% power to detect an effect size of 0.67, with a significance alpha level of 0.05 for the primary hypothesis. A drop out rate of 10% was considered. The effect size was estimated based on historical data from previous trials with major depression, SSRI and rTMS [20]. We used this data to base our calculations of the effect size due to the new classification of DSM-V that considers PPD an onset of major depression. All the calculations were performed on Stata providing a final sample size of 100 subjects.
2.10. Statistical analysis
Baseline characteristics will be assessed by ANOVA. The primary outcome will be assessed by t-test. Secondary analysis to control for covariates such as sertraline dose, age, and estrogen level will be performed by ANCOVA with an Intention to Treat (ITT) analysis. Kaplan-Meier and Cox-PH models with censoring for missing data will be used to evaluate time to remission of PPD. For the survival analysis, time-to-remission will be defined as the time to achieve a change of 50% on baseline HAM-D17 scale score through 6 and 12 weeks. Descriptive statistics will be used for safety analysis and EEG changes. Table 4 summarizes the main tests for primary and secondary hypotheses.
Table 4.
Study hypothesis, design, endpoint and statistical analysis.
| Treatment ARM1 | Treatment ARM 2 | Endpoints | Statistical analysis | |
|---|---|---|---|---|
| Primary hypothesis |
|
|
Primary: Reduction of 50% baseline HAM-D17 scale score |
Unpaired t-test based on Central Limit Theorem |
|
Treatment ARM 2 |
Treatment ARM 3 |
Endpoints |
Statistical analysis |
|
| Ancillary hypothesis |
|
|
Secondary: Reduction of 50% baseline HAM-D17 scale score after 6 weeks and 12 weeks time points |
Unpaired t-test based on Central Limit Theorem |
3. Discussion
3.1. Rationale for the trial design
For this study, several trial designs were considered to evaluate safety and efficacy of rTMS on PPD based on existing knowledge and ethical concerns with the study population. We considered several study designs such as a non-inferiority design to our two arm and double blind trial compared to sertraline, a superiority trial and our current design with an exploratory question.
In order to prove non-inferiority of rTMS compared to sertraline, two primary considerations were taken into account: assay sensitivity and inferiority margin calculation. Assay sensitivity poses a challenge due to the moderate effect size of SSRI over placebo. A meta-analysis of RCTs showed a 1.01 odds ratio at the lower margin of the confidence interval. This means that in the most conservative estimation, there is no significant difference between SSRI and placebo [21]. This makes the choice of an appropriate inferiority margin unfeasible to detect the expected effect size. Therefore, although it would be an interesting study design, there is not enough data supporting the notion that rTMS non inferiority over SSRI represents a true effect over placebo rather than equivalent ineffectiveness over placebo.
Our second option was a two-arm double-dummy superiority design to test rTMS over sertraline. While this design has the advantage of a direct comparison of the two treatments as mono-therapies, no direct comparison between both interventions has been done previously in this population. Hence, there is not enough evidence to support this design, and it is not prudent to conduct a larger late phase II trial without a precedent pilot trial.
Therefore, we designed a study that would provide evidence regarding the efficacy of rTMS compared to sham rTMS in postpartum depressed women under standard treatment (sertraline). This design allows the evaluation of the combination therapy (rTMS and SSRI) over standard mono-therapy in the PPD population through the primary question - a phenomenon with numerous supporting literature [13], [14], [15]. Meanwhile, it admits an ancillary question involving an exploratory evaluation of rTMS over sertraline mono-therapy. Regardless of positive or negative results, this will pave the way for future head-to-head comparison trials.
3.2. Recruitment strategy
We target to keep the inclusion criteria as general as possible in order to encompass all women over 18 years old who have moderate to severe PPD. As a late phase II trial, this provides the generalizability required for a pivotal device trial. We also followed the guidance of the previous two pilot PPD trials [13], [14].
We expect low drop-out rates based on acceptability of the treatment [11] and previous pilot studies that demonstrated high adherence rates for this population receiving rTMS combined with SSRI [13], [14]. Despite this, we will use several retention strategies such as, providing regular communication with patients, compensating for transportation, involving family members as much as possible, and offering childcare services while the patient undergoes treatment. Furthermore, to increase compliance, investigators will administer monitored doses of SSRI during study visits for rTMS treatment. Data about safety of SSRI use, during breastfeeding, will be shared with the patient. On days with no rTMS treatment, patients will be given doses to take home with an electronic diary to continuously monitor compliance.
Due to the time commitment required by patients in this trial, and the time sensitivity to enroll the patient post-delivery, the perceived challenge for this trial is not adherence but recruitment. To address recruitment obstacles, we have a multicenter design to reduce the recruitment burden at any particular site. In addition, we will begin with a broad recruitment strategy early in the pregnancy by public awareness campaigns that will aim to inform expecting mothers of the prevalence of PPD, and the risks involved.
This strategy attempts to engage all expecting mothers who feel they may be prone to mood disorders. We will also rely on referrals by psychiatrists and obstetricians in order to have a wide selection of potential participants in the targeted 4 week post-delivery window period. Additionally, we will reach out to pediatricians to give information about our trials to mothers of newborns receiving their early childhood immunizations. All patients will be screened for eligibility by our study team.
Our randomization strategy supports our recruitment targets. We determined it would be favorable to randomize in a 2:2:1 ratio as to have a favorable chance of enrolment into our primary arms of the trial, only requiring a total of 72 completers (36 per arm) to reach sufficient power to detect the appropriate effect size.
3.3. Ethical considerations
In dealing with a vulnerable population such as pregnant women with a moderate to severe psychiatric condition, sound ethical rationale must be incorporated into our study design.
Firstly, safety of rTMS procedure has been repeatedly demonstrated in the general population and specifically in PPD patients in pilot studies [13], [14]. Secondly, since the effects of rTMS on pregnant women have not been established to date, we will only initiate treatment post-delivery. Thirdly, our randomization ratio allows for 80% of patients to receive standard therapy with active or sham rTMS treatment. Only 20% of our patients will receive rTMS alone. Although rTMS monotherapy has a proven efficacy in MDD [22], we will employ a Data Safety Monitoring Committee to oversee all the trial data in a blinded fashion on an ongoing basis. Patients with worsening symptoms, or serious adverse events, will be evaluated by the DSMC and guidance will be given in regards to SSRI dose adjustment, unblinding, reverting to standard therapy or discontinuation.
3.4. Limitations
In designing this trial, we perceive limitations that need to be addressed. Blinding in medical device trials is a well-known challenge. In addition, our ancillary study may simply serve as a pilot arm and results should be interpreted as such.
The MagVenture TMS device provides the added feature of an unmarked single, two-sided coil for both sham and active treatments allowing for a blinded operator. However; there are inevitable telltale signs of active and sham treatments by an experienced stimulator. For instance, muscle twitches intensity during calibration by motor threshold and the stimulation itself. For this reason, we will add an additional layer of protection against unblinding by ensuring our blinded stimulator is unrelated to any other trial activities, data analysis, and have limited contact with researchers. By the same mechanism, patients with previous experience with active rTMS may be unblinded by the differences between sham and active treatments sensation. Therefore, these patients will be excluded from the trial.
3.5. Strengths
We find that this trial design allows for an ethical alternative to evaluate a particularly vulnerable population that is difficult to study. This trial has the benefit of evaluating rTMS as a combination therapy as well as an exploratory monotherapy as a basis for future trials. The ancillary exploration fills a gap in the literature that has not been previously explored in this population. Furthermore, our robust design, tests two parallel hypotheses using easily interpretable statistical tests. Because of the strong evidence of TMS in depressive disorders and FDA approval for this indication, we have strongly validated outcomes to evaluate its efficacy and a well-established rationale for our hypothesis, making it likely to show positive results.
4. Conclusion
We designed a study protocol scientifically feasible, ethical for the investigation of an innovative treatment for PPD. In addition, this subject is relevant for the scientific community, and has an impact on women's health care and on public health.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
We thank the guidance by Dr Felipe Fregni, Laboratory of Neumodulation - Harward Medical School; and the entire team of Principles and Practices of Clinical Research course of 2015.
Contributor Information
Tomas Andriotti, Email: tomas.andriotti@me.com.
Rafaelly Stavale, Email: rafaellystavale@gmail.com.
Tarek Nafee, Email: tarekomarnafee@gmail.com.
Stephanie Fakhry, Email: fakhrystephmd@gmail.com.
Mahmoud M.A. Mohamed, Email: ph.mahmmoud.soliman@gmail.com.
Nigar Sofiyeva, Email: nigarsofiyeva@gmail.com.
Ana Ganho- Ávila, Email: anaganho@gmail.com.
Andreas Bogner, Email: Andreas.Bogner@unikliniklum-dresden.de.
Sara P. Barbosa, Email: sarabarbosa@usp.br, saraenfer@uahoo.com.br.
Luciana S. Piton, Email: lupiton@hotmail.com.
André Luís S. Hirayama, Email: Xkandre1979@yahoo.com.br.
Gisele Gaccia, Email: gicaccia@yahoo.com.br.
Tomas P. Smith-Howard Junior, Email: tomaspsh@hotmail.com.
Priscila C. Miranda, Email: pritcp@gmail.com.
Alvaro Gragera, Email: alvarogragera@gmail.com.
Hiroki Nishiwaki, Email: nwacky1978@yj8.so-net.ne.jp.
References
- 1.Stone K. What the new DSM-V says about postpartum depression & psychosis. Postpartum Prog. 2013;1:186–187. http://www.postpartumprogress.com/what-the-new-dsm-v-says-about-postpartum-depression-psychosis [Google Scholar]
- 2.Fiorelli, Marco Magnetic resonance imaging studies of postpartum depression: an overview. Behav. Neurol. 2015:1–7. doi: 10.1155/2015/913843. http://www.hindawi.com/journals/bn/2015/913843/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim D.R., Epperson C.N., Weiss A.R., Wisner K.L. Pharmacotherapy of postpartum depression: an update. Expert Opin. Pharmacother. 2014;15(9):1223–1234. doi: 10.1517/14656566.2014.911842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lembke A.A. Psychosocial approach to postpartum depression. Psychiatr. Times. June 2002;20(26) [Google Scholar]
- 5.National Institute for Healthcare Management – NIHM. Identifying and Treating Maternal Depression: Strategies & Considerations for Health Plans. June 2010. [Google Scholar]
- 6.Dennis Cindy-Lee. Peer support for postpartum depression: volunteers' perceptions, recruitment strategies and training from a randomized controlled trial. Health Promote Int. June 2013;28(2):187–196. doi: 10.1093/heapro/das003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roy-Byrne Peter. 2016. Unipolar Major Depression in Pregnant Women: Treatment. Uptodate.Com. N.P. Web. 13 Sep. 2015. [Google Scholar]
- 8.Carrie Amstrong. ACOG guidelines on psychiatric medication use during pregnancy and lactation. Am. Fam. Physician. 2008 Sep 15;78(6):772–778. [Google Scholar]
- 9.Lanza T., Wisner K. Antidepressant medication use during breastfeeding. Clin. Obstetrics Gynecol. 2009;52(3):483–497. doi: 10.1097/GRF.0b013e3181b52bd6. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2902256/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horvath J.C., Mathews J., Demitrack M.A., Pascual-Leone A. The NeuroStar TMS device: conducting the FDA approved protocol for treatment of depression. J. Vis. Exp. 2010 doi: 10.3791/2345. http://www.jove.com/details.php?id=2345 e2345, 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu B., Zhang Y., Zhang L., Li L. Repetitive transcranial magnetic stimulation as an augmentative strategy for treatment-resistant depression, a meta-analysis of randomized, double-blind and sham-controlled study. BMC Psychiatry. 2014;14:342. doi: 10.1186/s12888-014-0342-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O' Reardon Efficacy and safety of transcranial magnetic stimulation in acute treatment of major depression: a multisite randomized controlled triall. Biol. Psychiatry. 2007;62:1208–1216. doi: 10.1016/j.biopsych.2007.01.018. [DOI] [PubMed] [Google Scholar]
- 13.Garcia K., Flynn P., Pierce K., Caudle M. Repetitive transcranial magnetic stimulation treats postpartum depression. Brian Stimul. 2010;3:36–41. doi: 10.1016/j.brs.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 14.Myczkowski Effects of repetitive transcranial magnetic stimulation on clinical, social, and cognitive performance in postpartum depression. Dovepress Neuropsychiatric Dis. Treat. 2012;8:491–500. doi: 10.2147/NDT.S33851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rossi S., Hallett M., Rossini P.M., Pascual-Leone A. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin. Neurophysiol. 2009;120(12):2008–2039. doi: 10.1016/j.clinph.2009.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spronk D., Arns M., Fitzgerald P.B. Elsevier; 2010. Repetitive Transcranial Magnetic Stimulation in Depression: Protocols, Mechanisms and New Developments. Neuromodulation and Neurofeedback: Techniques and Applications. [Google Scholar]
- 17.Guidance for Industry and FDA Staff Class II Special Controls Guidance Document: Repetitive Transcranial Magnetic Stimulation (rTMS) Systems. July 2011. http://www.fda.gov/RegulatoryInformation/Guidances/ucm265269.htm [Google Scholar]
- 18.Pearlstein T. Perinatal depression: treatment options and dilemmas. J. Psychiatry Neurosci. 2008;33(4):304. [PMC free article] [PubMed] [Google Scholar]
- 19.Pearlstein T. Perinatal depression: treatment options and dilemmas. J. Psychiatry Neurosci. 2008;33(4):304. [PMC free article] [PubMed] [Google Scholar]
- 20.Huang M., Luo B., Hu J. Repetitive transcranial magnetic stimulation in combination with citalopram in young patients with first-episode major depressive disorder: a double-blind, randomized, sham-controlled trial. Aust. N. Z. J. Psychiatry. 2012;46(3):257–264. doi: 10.1177/0004867411433216. [DOI] [PubMed] [Google Scholar]
- 21.Sharma V., Sommerdyk C. Are antidepressants effective in the treatment of postpartum depression? A systematic review. Prim. Care Companion CNS Disord. 2013;15(6) doi: 10.4088/PCC.13r01529. PCC.13r01529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee J., Blumberger D., Fitzgerald P. The role of transcranial magnetic stimulation in treatment-resistant depression: a review. Curr. Pharm. Des. 2012;18(36):5846–5850. doi: 10.2174/138161212803523644. [DOI] [PubMed] [Google Scholar]
- 23.Marušić Ana, Ferenčić Stella Fatović. Adoption of the double dummy trial design to reduce observer bias in testing treatments. J. R. Soc. Med. 2013;106(5):196–198. doi: 10.1177/0141076813485350. PMC. Web. 9 Dec. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]