Abstract
Symptomatic intestinal strictures develop in more than one third of patients with Crohn’s disease (CD) within 10 years of disease onset. Strictures can be inflammatory, fibrotic or mixed and result in a significant decline in quality of life, frequently requiring surgery for palliation of symptoms. Patients under the age of 40 with perianal disease are more likely to suffer from disabling ileocolonic disease thus may have a greater risk for fibrostenotic strictures. Treatment options for fibrostenotic strictures are limited to endoscopic and surgical therapy. Endoscopic balloon dilatation (EBD) appears to be a safe, less invasive and effective alternative modality to replace or defer surgery. Serious complications are rare and occur in less than 3% of procedures. For non-complex strictures without adjacent fistulizaation or perforation that are less than 5 cm in length, EBD should be considered as first-line therapy. The aim of this review is to present the current literature on the endoscopic management of small bowel and colonic strictures in CD, which includes balloon dilatation, adjuvant techniques of intralesional injection of steroids and anti-tumor necrosis factor, and metal stent insertion. Short and long-term outcomes, complications and safety of EBD will be discussed.
Keywords: Endoscopy, Crohn’s disease, Stricture, Stenosis, Inflammatory bowel disease, Endoscopic balloon dilation
Core tip: Endoscopic balloon dilation (EBD) for Crohn’s disease-related fibrostenotic strictures has been recognized as a safe, and less invasive intervention with rare complications that occur in less than 3% of procedures. EBD can replace or defer surgery and help avoid frequent intestinal resections, which result in short bowel syndrome and impair quality of life. For non-complex strictures without adjacent fistulization or perforation that are less than 5 cm in length, EBD should be considered as first-line therapy. In this review we discuss safety, short and long-term outcomes, as well as adjuvant techniques of intralesional injection of steroids, anti-tumor necrosis factor, and metal stent insertion.
INTRODUCTION
Intestinal strictures are a common complication of Crohn’s disease (CD) affecting one-third of the patient population within 10 years of disease onset. This number, however, is likely under-reported[1,2]. In general, CD strictures are classified into inflammatory, fibrotic or mixed, although all symptomatic inflammatory strictures likely have some component of fibrosis and vice-versa[2,3]. Risk factors and predictors of intestinal strictures to date are clinical, environmental, genetic or endoscopic parameters[4] (Table 1). Although no clinical factors exist which can accurately predict the stricturing phenotype of CD, there do exist factors which may predict the likelihood of small bowel disease and a disabling disease course thus indirectly may suggest an increased risk for the development of fibrostenotic disease. These factors include the presence of perianal disease, age of CD diagnosis less than 40 years old and the need for steroids during the first flare[4,5]. Patients frequently complain of progressive post-prandial abdominal pain, bloating, nausea, vomiting and weight loss. The diagnosis of intestinal strictures usually coincides with a spiraling decline in quality of life and results in surgery in 75% of patients at least once during their lifetime[1]. CD patients will frequently undergo multiple bowel resections over their lifetime that repeatedly exposes them to immediate and long-term post-operative complications such as anastomotic leaks with intra-abdominal sepsis, short bowel syndrome, and adhesions with recurrent bowel obstructions[2,6].
Table 1.
Risk factors and predictors of fibrostenosing Crohn’s disease
| Clinical[4] | Age at diagnosis < 40 yr |
| Perianal disease at diagnosis | |
| Need for steroids during first flare | |
| Small bowel disease location | |
| Prior appendectomy | |
| Environmental[4] | Smoking |
| Endoscopic[4] | Deep mucosal ulcerations |
| Genetic[4] | Nucleotide oligomerisation domain 2 (NOD2) variants |
| Janus-associated kinase 2 (JAK2) | |
| Caspase-recruitment domain 15 (CARD15) | |
| NOD2/CARD15 mutations on both chromosomes | |
| TNF superfamily 15 (TNFSF15) in Asians | |
| 5T5T in the MMP3 gene | |
| rs1363670 | |
| Serological[4] | Antimicrobial antibodies |
| anti-Saccharomyces cerevisiae antibodies (ASCA) IgA in Asians |
The pathogenesis of CD complications develops from chronic accumulation of inflammatory bowel damage variably leading to stricture, fistula and/or abscess formation[2]. Stricture development, although not fully understood, involves the progressive deposition of extracellular matrix protein (ECM) produced by myofibroblasts at variable sites of the bowel being injured by chronically uncontrolled relapsing and remitting transmural inflammation[7]. During chronic intestinal inflammation, the baseline release of profibrotic cytokines (e.g., IL-4 and IL-13) increases over time further accelerating the process of excessive matrix deposition[7,8]. There may also exist a point where inflammation is no longer required to trigger fibrosis. As ECM is deposited during chronic inflammation, the bowel wall becomes stiffer. Bowel wall stiffness acts independently as a mesenchymal cell activator, resulting in ongoing myofibroblast stimulation, thus progressive fibrotic stenosis[9].
Treatment options for fibrostenotic strictures are limited to endoscopic and surgical therapy (i.e., stricturoplasty and small bowel resection)[10]. Fortunately, most de novo strictures form in the ileum and ileocolic regions, which are accessible by ileocolonoscopy or balloon-assisted enteroscopy[11]. Although pharmacotherapy may delay the time before operative management, it has not been shown to prevent it[12]. Approximately 80% of patients will have their first bowel resection 10 years following their diagnosis of CD[2]. To date no specific intestinal anti-fibrotic therapy exists, nor has any immunosuppressant or biologic therapy been shown to prevent stricture formation.
The following review presents the current data on the endoscopic management of small bowel and colonic strictures in CD. Short and long-term outcomes, complications and a description of the procedure will be discussed.
EFFICACY OF ENDOSCOPIC BALLOON DILATION
Endoscopic balloon dilation (EBD) is a minimally invasive bowel-length preserving mean of managing symptomatic CD patients with short fibrotic strictures (Figure 1). EBD has become an established modality of therapy and often plays an important role in delaying or acting as a bridge to surgery[10,13]. The most common location of the small bowel to undergo EBD using a colonoscope is the distal ileum or at the ileocolonic anastomosis of a patient following a small bowel resection[14]. Strictures located in the distal duodenum to proximal jejunum or distal jejunum to proximal ileum may be accessed with ante- or retrograde enteroscopy, respectively[15].
Figure 1.
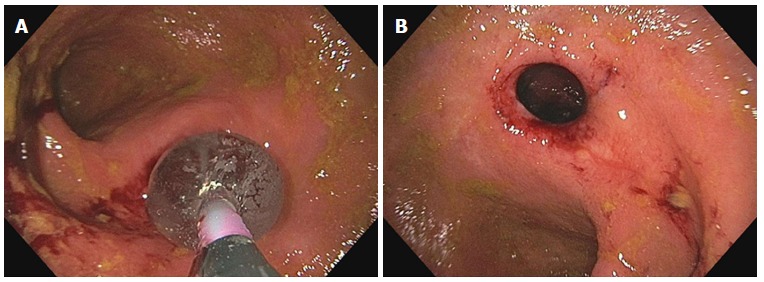
Endoscopic balloon dilatation of ileocolonic anastomosis (A) and endoscopic appearance post endoscopic dilatation (B).
Short- and long-term efficacy has been inconsistently defined in studies[13]. In general, short-term efficacy has been described as the technical success of the procedure or the ability to traverse the dilated area freely with the endoscope immediately after dilatation[13,16]. Long-term efficacy, in most studies, has been described as the time elapsed until another intervention (either surgical or endoscopic) is required[2,13,16]. Despite the lack of a formal definition, excellent short- and moderate long-term efficacy of EBD for CD strictures has been documented in many studies[14,16,17]. Table 2 shows a summary of published studies on EBD using conventional colonoscopy in CD patients. In a systematic review and descriptive pooled analysis of 12 studies conducted between 1991 to 2013 evaluating 1463 CD patients who underwent 3213 EBD procedures, the technical success rate was 89% with an associated relief of clinical symptoms in 81% of patients[14]. The majority of strictures were ileal (98.6%) at anastomotic sites (62%), which were 2 cm or less. However, the recurrence rate of strictures was high. At the 36.6 mo median follow-up, 47.5% of patients had symptomatic recurrence and 28.6% of all patients had required surgical intervention. This study concluded that the chance of requiring repeat EBD or surgical intervention at 2 years was 73.5% and 42.9%, respectively[14]. Another large recent systematic review with meta-analysis involving 1089 patients (2664 EBDs) across 25 studies revealed similar results[17]. The technical success rate was 92.3% with a reported symptomatic response rate of 70.4%. The proportion of patients requiring a repeat dilation after 1 and 2 years was 31.6% (160/506) and 25.9% (117/451), respectively. Most patients within 5 years required recurrent dilations (80%) and/or surgical interventions (75%)[17]. Of interest is the lower symptomatic success rate as compared to the technical success rate across studies. This likely occurred due to a lack of a standardized means of reporting technical and clinical efficacy and/or a superimposed process existing that contributed to the patient’s symptoms (e.g., ongoing inflammation, intestinal bacterial overgrowth, IBS, etc.)[10]. Despite this discrepancy, the short-term clinical success rate remains high.
Table 2.
Summary of published studies on endoscopic balloon for Crohn’s disease strictures
| Authors | Pubished year | No. of patients | Anastomotic strictures (%) | Maximum balloon caliber (mm) | Technical success (%) | Clinical efficacy (%) | Major complication (%) |
| Blomberg et al[52] | 1991 | 27 | 100 | 25 | 100 | 67 | 0 |
| Williams et al[53] | 1991 | 7 | 71 | 20 | 71 | 71 | 0 |
| Breysem et al[54] | 1992 | 18 | 78 | 18 | 89 | 50 | 0 |
| Cockuyt et al[55] | 1995 | 55 | 67 | 20 | 85 | 62 | 8 |
| Ramboer et al[56] | 1995 | 13 | 69 | 18 | 100 | 100 | 0 |
| Matsui et al[57] | 2000 | 55 | 43 | 20 | 86 | 78 | 2 |
| Dear et al[58] | 2001 | 22 | 95 | 18 | 100 | 73 | 0 |
| Brooker et al[59] | 2003 | 14 | 79 | 20 | 100 | 79 | 0 |
| Morini et al[60] | 2003 | 43 | 67 | 18 | 79 | 42 | 0 |
| Sabate et al[61] | 2003 | 38 | 68 | 25 | 84 | 53 | 3 |
| Thomas-Gibson et al[62] | 2003 | 59 | 90 | 18 | 73 | 41 | 3 |
| Singh et al[63] | 2005 | 17 | 35 | 20 | 100 | 76 | 18 |
| Aljouni et al[64] | 2006 | 37 | 37 | 20 | 90 | 87 | 3 |
| Ferlitsch et al[65] | 2006 | 46 | 59 | 20 | 85 | 66 | 4 |
| Nomura et al[66] | 2006 | 16 | 35 | 20 | 94 | 65 | 6 |
| Foster et al[67] | 2008 | 24 | 41 | 20 | 92 | NA | 13 |
| Hoffman et al[68] | 2008 | 25 | 57 | 20 | 100 | 52 | 16 |
| Stienecker et al[69] | 2009 | 25 | 42 | 18 | 97 | 94 | 3 |
| Mueller et al[70] | 2010 | 55 | 23 | 18 | 95 | 76 | 2 |
| Thienpont et al[71] | 2010` | 138 | 84 | 18 | 97 | 76 | 3 |
| Scimeca et al[72] | 2011 | 37 | 90 | 20 | 84 | 89 | 0 |
| Gustavsson et al[51] | 2012 | 178 | 80 | 25 | 89 | 64 | 11 |
| Karstensen et al[73] | 2012 | 23 | 24 | 15 | 83 | 74 | 1.9 |
| De’Angelis et al[74] | 2013 | 26 | 52 | 18 | 100 | 93 | 2 |
| Endo et al[75] | 2013 | 30 | 36 | 20 | 94 | 64 | 10 |
| Honzawa et al[76] | 2013 | 25 | 21 | 20 | 88 | 62 | 12 |
| Nanda et al[77] | 2013 | 31 | 100 | 18 | 100 | 45 | 0 |
| Atreja et al[78] | 2014 | 128 | 48 | 20 | 83 | 67 | 3 |
| Bhalme et al[79] | 2014 | 79 | 61 | 20 | 95 | 77 | 0 |
| Hagel et al[80] | 2014 | 77 | 57 | 20 | 55 | 65 | 10 |
| Krauss et al[81] | 2014 | 20 | 25 | 18 | 100 | NA | 14 |
| Ding et al[82] | 2016 | 54 | 100 | 20 | 89 | 82 | 2 |
Clinical efficacy was defined according to each study (i.e., resolution of obstructive symptoms after dilation with the avoidance of surgery or additional intervention). Technical success was defined by successful passage of the endoscope or colonoscope immediately after dilation. Clinical efficacy was defined as the resolution of obstructive symptoms after dilation with the avoidance of surgery. Major complications (calculated per number of dilations) included were perforations, bleeding, intra-abdominal abscesses or fistulas. NA: Not available.
In the setting of small bowel strictures not in reach of the enteroscope or colonoscope, the double balloon enteroscope can be used in an antegrade or retrograde fashion for diagnostic and/or therapeutic intervention[15]. Although there are only a few small studies which have evaluated its use in dilating small bowel CD strictures, the results were positive[18,19]. Nishida et al[20] performed a retrospective review on their center’s experience with dilating small bowel strictures between 2006 to 2015. Overall, small bowel dilation using the double balloon enteroscope was found to be successful but there was a greater risk for requiring surgery in patients with multiple strictures as compared to those with a single stricture (adjusted hazard ratio, 14.94; 95%CI: 1.91-117.12; P = 0.010)[20]. As such, a single stricture but not necessarily multiple strictures may be a good indication for considering dilation using the double balloon enteroscope.
PREDICTORS OF SUCCESSFUL ENDOSCOPIC DILATATION
Factors that are predictive of a successful EBD include short straight strictures in-line with the bowel lumen distal to the duodenum, which are non-ulcerated in a location without any adjacent abscess and at least 5 cm from a fistula orifice[21,22]. Strictures located in the duodenum were found to have a 5 fold increased hazard for time to shorter surgery as compared to strictures located in the jejunum/ileum or colon (HR = 4.7, P = 0.038; HR = 5.6, P = 0.03; respectively)[23]. Additionally, a stricture length ≤ 5 cm was associated with a lower chance of requiring surgical intervention following EBD (HR = 2.5, 95%CI: 1.4-4.4; P = 0.002). For every 1 cm increase in stricture length, the risk for surgery increased by 8% (P = 0.005)[23]. In contrast to popular belief, anastomotic strictures have been associated with poorer short-term outcomes than de novo strictures[23,24]. This was highlighted in the aforementioned review by Bettenworth et al[14] which documented a lower technical success rate for post-surgical strictures as compared to native strictures (OR = 2.3, P < 0.001). Similarly, a recent study published by the Cleveland Clinic group after performing a retrospective review on 307 patients who had undergone either EBD or surgical resection for an ileocolonic anastomotic stricture had worse short-term outcomes (i.e., technical success) but similar long-term outcomes as compared to the aforementioned studies evaluating EBD of de novo strictures[24]. Of the 176 patients who had undergone EBD, the technical success rate was 86% (range 71% to 100%) with a long-term clinical efficacy, defined as an avoidance of surgery, of 58% over a follow-up period of 33 mo[24]. The presence of active inflammation identified on endoscopy, elevated CRP, medical treatment after dilation, cigarette smoking and intralesional steroid injection have demonstrated conflicting results with respect to the need for surgery and successful EBD[2,17,23,24].
ENDOSCOPIC ADJUVANT TECHNIQUES
Intralesional injection of steroids has been demonstrated to be effective for peptic, corrosive, anastomotic or post-radiotherapy fibrotic strictures[25]. However, strong evidence for the use of intralesional injection of steroids in CD is lacking[25-28]. Studies that have evaluated its use in CD have used the formulation triamcinolone due to its rapid onset of action and long-lasting duration of effectiveness of 3-4 wk[29]. Only two small randomized placebo controlled studies have been performed evaluating the use of intralesional steroids versus saline injection after failing medical therapy and EBD. The first study conducted in 2007, included 13 adult patients with short (≤ 5 cm) ileocolonic anastomotic strictures[30]. Five of the seven patients in the intervention group required re-dilation after the procedure and one patient had a complication versus one of six in the placebo group required re-dilation. There was no significant difference with respect to success of the procedure between groups[30]. This trial was stopped early due to the trend toward harm and remains the influential study behind the current American College of Gastroenterology and British Society of Gastroenterology position statements against the routine use of intralesional steroids[31,32]. The second study published in 2010 included 29 pediatric patients with short ileal or colonic strictures (12 anastomotic, 17 de novo)[33]. In contrast, this study did demonstrate a reduction in time to re-dilation and surgery in the intervention group. Within the sub-group of patients evaluated in a recent large systematic review evaluating the management of CD strictures, intralesional steroid injection did not improve outcomes[33]. Similarly, a review conducted in 2013 summarizing the findings from five retrospective case-series evaluating the use of intralesional steroids in CD patients concluded the data to be contradictory and limited[34].
Although controversial, intralesional injection of anti-tumor necrosis factor has been evaluated in patients with small bowel and colonic CD strictures with promising results, but concerns related to immunization may limit its potential as a therapeutic option[35,36]. One small case series evaluated the effect of a 90-120 mg intralesional injection of infliximab in three symptomatic patients with colonic CD strictures. All three patients had an improved endoscopic appearance of the stricture as well as relief of their obstructive symptoms for at least four months following the injection[35]. Similarly, another small case series evaluating intralesional injections of 40 mg of infliximab into small bowel CD strictures combined with EBD in six patients was associated with improved symptoms and a reduction in their modified simple endoscopic score for Crohn’s disease (SES-CD)[37]. The results of a larger randomized controlled trial evaluating the efficacy of performing intralesional injections of adalimumab into intestinal CD strictures are awaited[38].
Endoscopic metal stent insertion has been attempted in few patients with CD strictures. Although the technical success rate has been reportedly high, major complications such as bowel perforation, stent migration and fistulization was reported in 67% of patients[39]. Additionally, in order to avoid stent impaction, most studies suggest removing the stent after one month[40-42]. One small prospective cohort study concluded the risk for complications was too high to suggest the use of endoscopic metal stents as a treatment option for CD strictures after evaluating the data from 11 patients at their center[40]. The use of biodegradable instead of metal stents has been evaluated recently in a case-series last year involving six patients with intestinal and colonic CD strictures. Although technical success was good, premature stent failure occurred in all of the patients[43].
SAFETY OF ENDOSCOPIC BALLOON DILATION
Although EBD is a minimally invasive procedure, bowel perforation and severe bleeding has been reported in most large studies[17,23,24]. In the aforementioned review by Bettenworth et al[14], major complications requiring hospitalization occurred in 2.8% of patients. Similarly, another large systematic review evaluating 24 non-randomized studies including 1163 patients found the rate of iatrogenic perforation to be 3%[44]. The rate for major complications including infection and hemorrhage in this study was 4%[44]. In a study directly comparing EBD to surgical intervention for the management of intestinal CD strictures, perforation occurred in 1.1% of the patients in the EBD group whereas the post-operative complication rate (e.g., intra-abdominal sepsis) was 8.8%[24]. Despite these significant complications, no deaths have been reported to date. Since benign or inflammatory intestinal strictures are indistinguishable from early adenocarcinoma on imaging, there exists a risk that malignancy may be missed when EBD is performed instead of surgical excision[3]. Population based studies have suggested a greater risk for small bowel malignancy in patients with longstanding CD. Several case reports exist documenting the development of small bowel malignancy following stricturoplasty and bypassed loops[45-51]. As such, biopsies of the stricture should occur prior to dilation[22]. There has been no evidence to suggest obtaining biopsies prior to EBD increases the risk for perforation.
CONCLUSION
EBD remains a safe and effective modality of treating CD strictures in appropriately selected patients. Although it may not be able to prevent operative management in all patients, it can significantly delay it. For an isolated intestinal fibrostenotic CD stricture less than or equal to 5 cm in length without adjacent fistulization or perforation, EBD should be considered as first-line therapy (Table 3).
Table 3.
Practical considerations
| Predictors favoring successful dilation[11,22-25] | Symptomatic predominantly fibrotic stricture |
| Short (≤ 5 cm) stricture | |
| Single straight stricture | |
| Stricture distal to the duodenum | |
| Anastomotic stricture more favorable than de novo stricture | |
| First dilation | |
| Lack of a superimposed process contributing to symptoms (e.g., SIBO or IBS) | |
| Risk factors for complications[22-25] | Predominantly inflammatory stricture without medical optimization |
| Stricture greater than 5 cm | |
| Multiple small bowel strictures | |
| Strictures caused by extrinsic compression (e.g., adhesions) | |
| Fistulization within 5 cm of the area to be dilated | |
| Adjacent perforation or intra-abdominal collection | |
| Complete small bowel obstruction | |
| Tortuous or tethered small bowel or significant stricture angulation | |
| Duodenal stricture | |
| 1Short term outcome[15,18] | 85%-95% (technical success), 70%-80% (clinical response) |
| 2Long term outcome[15,18] | 32% (year 1 post dilation), 80% (year 5 post dilation) |
| 3Complication rate[25,45] | 1%-4% |
Short term outcome refers to the time elapsed immediately after the dilation takes place; technical success refers to the ability to successfully complete the dilation; clinical response refers to the symptomatic improvement of the patient immediately following the dilation;
Long term outcome refers to the percentage of patients requiring a repeat intervention;
Complication rate encompasses only major complications requiring urgent intervention such as bleeding, perforation and infection.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Canada
Peer-review report classification
Grade A (Excellent): A, A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: None.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: March 11, 2018
First decision: March 29, 2018
Article in press: April 23, 2018
P- Reviewer: Gangl A, M’Koma A, Souza JL, Wittmann T S- Editor: Gong ZM L- Editor: A E- Editor: Huang Y
Contributor Information
Talat Bessissow, Division of Gastroenterology, Department of Medicine, McGill University Health Center, Montreal, QC H3G1A4, Canada. talat.bessissow@mcgill.ca.
Jason Reinglas, Division of Gastroenterology, Department of Medicine, McGill University Health Center, Montreal, QC H3G1A4, Canada.
Achuthan Aruljothy, Division of Gastroenterology, Department of Medicine, McGill University Health Center, Montreal, QC H3G1A4, Canada.
Peter L Lakatos, Division of Gastroenterology, Department of Medicine, McGill University Health Center, Montreal, QC H3G1A4, Canada; 1st Department of Medicine, Semmelweis University, Budapest 1085, Hungary.
Gert Van Assche, Division of Gastroenterology and Hepatology, University Hospitals Leuven, Belgium and University of Leuven, Leuven 3000, Belgium.
References
- 1.Cosnes J, Cattan S, Blain A, Beaugerie L, Carbonnel F, Parc R, Gendre JP. Long-term evolution of disease behavior of Crohn’s disease. Inflamm Bowel Dis. 2002;8:244–250. doi: 10.1097/00054725-200207000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Rieder F, Zimmermann EM, Remzi FH, Sandborn WJ. Crohn’s disease complicated by strictures: a systematic review. Gut. 2013;62:1072–1084. doi: 10.1136/gutjnl-2012-304353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bettenworth D, Nowacki TM, Cordes F, Buerke B, Lenze F. Assessment of stricturing Crohn’s disease: Current clinical practice and future avenues. World J Gastroenterol. 2016;22:1008–1016. doi: 10.3748/wjg.v22.i3.1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rieder F, Lawrance IC, Leite A, Sans M. Predictors of fibrostenotic Crohn’s disease. Inflamm Bowel Dis. 2011;17:2000–2007. doi: 10.1002/ibd.21627. [DOI] [PubMed] [Google Scholar]
- 5.Burke JP, Mulsow JJ, O’Keane C, Docherty NG, Watson RW, O’Connell PR. Fibrogenesis in Crohn’s disease. Am J Gastroenterol. 2007;102:439–448. doi: 10.1111/j.1572-0241.2006.01010.x. [DOI] [PubMed] [Google Scholar]
- 6.Shivananda S, Hordijk ML, Pena AS, Mayberry JF. Crohn’s disease: risk of recurrence and reoperation in a defined population. Gut. 1989;30:990–995. doi: 10.1136/gut.30.7.990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fiocchi C, Lund PK. Themes in fibrosis and gastrointestinal inflammation. Am J Physiol Gastrointest Liver Physiol. 2011;300:G677–G683. doi: 10.1152/ajpgi.00104.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Graham MF, Diegelmann RF, Elson CO, Lindblad WJ, Gotschalk N, Gay S, Gay R. Collagen content and types in the intestinal strictures of Crohn’s disease. Gastroenterology. 1988;94:257–265. doi: 10.1016/0016-5085(88)90411-8. [DOI] [PubMed] [Google Scholar]
- 9.Wells RG. The role of matrix stiffness in regulating cell behavior. Hepatology. 2008;47:1394–1400. doi: 10.1002/hep.22193. [DOI] [PubMed] [Google Scholar]
- 10.Gionchetti P, Dignass A, Danese S, Magro Dias FJ, Rogler G, Lakatos PL, Adamina M, Ardizzone S, Buskens CJ, Sebastian S, et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 2: Surgical Management and Special Situations. J Crohns Colitis. 2017;11:135–149. doi: 10.1093/ecco-jcc/jjw169. [DOI] [PubMed] [Google Scholar]
- 11.Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn’s disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cosnes J, Nion-Larmurier I, Beaugerie L, Afchain P, Tiret E, Gendre JP. Impact of the increasing use of immunosuppressants in Crohn’s disease on the need for intestinal surgery. Gut. 2005;54:237–241. doi: 10.1136/gut.2004.045294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klag T, Wehkamp J, Goetz M. Endoscopic Balloon Dilation for Crohn’s Disease-Associated Strictures. Clin Endosc. 2017;50:429–436. doi: 10.5946/ce.2017.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bettenworth D, Gustavsson A, Atreja A, Lopez R, Tysk C, van Assche G, Rieder F. A Pooled Analysis of Efficacy, Safety, and Long-term Outcome of Endoscopic Balloon Dilation Therapy for Patients with Stricturing Crohn’s Disease. Inflamm Bowel Dis. 2017;23:133–142. doi: 10.1097/MIB.0000000000000988. [DOI] [PubMed] [Google Scholar]
- 15.Tharian B, Caddy G, Tham TC. Enteroscopy in small bowel Crohn’s disease: A review. World J Gastrointest Endosc. 2013;5:476–486. doi: 10.4253/wjge.v5.i10.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hirai F. Current status of endoscopic balloon dilation for Crohn’s disease. Intest Res. 2017;15:166–173. doi: 10.5217/ir.2017.15.2.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morar PS, Faiz O, Warusavitarne J, Brown S, Cohen R, Hind D, Abercrombie J, Ragunath K, Sanders DS, Arnott I, Wilson G, Bloom S, Arebi N; Crohn’s Stricture Study (CroSS) Group. Systematic review with meta-analysis: endoscopic balloon dilatation for Crohn’s disease strictures. Aliment Pharmacol Ther. 2015;42:1137–1148. doi: 10.1111/apt.13388. [DOI] [PubMed] [Google Scholar]
- 18.Gill RS, Kaffes AJ. Small bowel stricture characterization and outcomes of dilatation by double-balloon enteroscopy: a single-centre experience. Therap Adv Gastroenterol. 2014;7:108–114. doi: 10.1177/1756283X13513995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fukumoto A, Tanaka S, Yamamoto H, Yao T, Matsui T, Iida M, Goto H, Sakamoto C, Chiba T, Sugano K. Diagnosis and treatment of small-bowel stricture by double balloon endoscopy. Gastrointest Endosc. 2007;66:S108–S112. doi: 10.1016/j.gie.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 20.Nishida Y, Hosomi S, Yamagami H, Yukawa T, Nagami Y, Tanaka F, Kamata N, Tanigawa T, Shiba M, Watanabe T, et al. Analysis of the Risk Factors of Surgery after Endoscopic Balloon Dilation for Small Intestinal Strictures in Crohn’s Disease Using Double-balloon Endoscopy. Intern Med. 2017;56:2245–2252. doi: 10.2169/internalmedicine.8224-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen M, Shen B. Endoscopic Therapy in Crohn’s Disease: Principle, Preparation, and Technique. Inflamm Bowel Dis. 2015;21:2222–2240. doi: 10.1097/MIB.0000000000000433. [DOI] [PubMed] [Google Scholar]
- 22.Rieder F, Latella G, Magro F, Yuksel ES, Higgins PD, Di Sabatino A, de Bruyn JR, Rimola J, Brito J, Bettenworth D, et al. European Crohn’s and Colitis Organisation Topical Review on Prediction, Diagnosis and Management of Fibrostenosing Crohn’s Disease. J Crohns Colitis. 2016;10:873–885. doi: 10.1093/ecco-jcc/jjw055. [DOI] [PubMed] [Google Scholar]
- 23.Bettenworth D, Rieder F. Medical therapy of stricturing Crohn’s disease: what the gut can learn from other organs - a systematic review. Fibrogenesis Tissue Repair. 2014;7:5. doi: 10.1186/1755-1536-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lian L, Stocchi L, Remzi FH, Shen B. Comparison of Endoscopic Dilation vs Surgery for Anastomotic Stricture in Patients With Crohn’s Disease Following Ileocolonic Resection. Clin Gastroenterol Hepatol. 2017;15:1226–1231. doi: 10.1016/j.cgh.2016.10.030. [DOI] [PubMed] [Google Scholar]
- 25.Nelson RS, Hernandez AJ, Goldstein HM, Saca A. Treatment of irradiation esophagitis. Value of hydrocortisone injection. Am J Gastroenterol. 1979;71:17–23. [PubMed] [Google Scholar]
- 26.Kochhar R, Poornachandra KS. Intralesional steroid injection therapy in the management of resistant gastrointestinal strictures. World J Gastrointest Endosc. 2010;2:61–68. doi: 10.4253/wjge.v2.i2.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kochhar R, Makharia GK. Usefulness of intralesional triamcinolone in treatment of benign esophageal strictures. Gastrointest Endosc. 2002;56:829–834. doi: 10.1067/mge.2002.129871. [DOI] [PubMed] [Google Scholar]
- 28.Ramage JI Jr, Rumalla A, Baron TH, Pochron NL, Zinsmeister AR, Murray JA, Norton ID, Diehl N, Romero Y. A prospective, randomized, double-blind, placebo-controlled trial of endoscopic steroid injection therapy for recalcitrant esophageal peptic strictures. Am J Gastroenterol. 2005;100:2419–2425. doi: 10.1111/j.1572-0241.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 29.Roques C, Téot L. The use of corticosteroids to treat keloids: a review. Int J Low Extrem Wounds. 2008;7:137–145. doi: 10.1177/1534734608320786. [DOI] [PubMed] [Google Scholar]
- 30.East JE, Brooker JC, Rutter MD, Saunders BP. A pilot study of intrastricture steroid versus placebo injection after balloon dilatation of Crohn’s strictures. Clin Gastroenterol Hepatol. 2007;5:1065–1069. doi: 10.1016/j.cgh.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 31.Lichtenstein GR, Hanauer SB, Sandborn WJ; Practice Parameters Committee of American College of Gastroenterology. Management of Crohn’s disease in adults. Am J Gastroenterol. 2009;104:465–83; quiz 464, 484. doi: 10.1038/ajg.2008.168. [DOI] [PubMed] [Google Scholar]
- 32.Carter MJ, Lobo AJ, Travis SP; IBD Section, British Society of Gastroenterology. Guidelines for the management of inflammatory bowel disease in adults. Gut. 2004;53 Suppl 5:V1–16. doi: 10.1136/gut.2004.043372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Di Nardo G, Oliva S, Passariello M, Pallotta N, Civitelli F, Frediani S, Gualdi G, Gandullia P, Mallardo S, Cucchiara S. Intralesional steroid injection after endoscopic balloon dilation in pediatric Crohn’s disease with stricture: a prospective, randomized, double-blind, controlled trial. Gastrointest Endosc. 2010;72:1201–1208. doi: 10.1016/j.gie.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 34.Bevan R, Rees CJ, Rutter MD, Macafee DAL. Review of the use of intralesional steroid injections in the management of ileocolonic Crohn’s strictures. Frontline Gastroenterol. 2013;4:238–243. doi: 10.1136/flgastro-2012-100297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Swaminath A, Lichtiger S. Dilation of colonic strictures by intralesional injection of infliximab in patients with Crohn’s colitis. Inflamm Bowel Dis. 2008;14:213–216. doi: 10.1002/ibd.20318. [DOI] [PubMed] [Google Scholar]
- 36.Sorrentino D, Avellini C, Beltrami CA, Pasqual E, Zearo E. Selective effect of infliximab on the inflammatory component of a colonic stricture in Crohn’s disease. Int J Colorectal Dis. 2006;21:276–281. doi: 10.1007/s00384-005-0739-0. [DOI] [PubMed] [Google Scholar]
- 37.Hendel J, Karstensen JG, Vilmann P. Serial intralesional injections of infliximab in small bowel Crohn’s strictures are feasible and might lower inflammation. United European Gastroenterol J. 2014;2:406–412. doi: 10.1177/2050640614547805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.ClinicalTrials. gov [Internet] Nov 18. Identifier. Bethesda (MD): National Library of Medicine (US); 2013. pp. NCT01986127, A Randomized, Double–blinded, Placebo-controlled Study on the Effects of Adalimumab Intralesional Intestinal Strictures of Crohn's Disease Patients; [cited Dec 29, 2017]. Available from: https://clinicaltrials.gov/ct2/show/study/NCT01986127 ClinicalTrials.gov. [Google Scholar]
- 39.Levine RA, Wasvary H, Kadro O. Endoprosthetic management of refractory ileocolonic anastomotic strictures after resection for Crohn’s disease: report of nine-year follow-up and review of the literature. Inflamm Bowel Dis. 2012;18:506–512. doi: 10.1002/ibd.21739. [DOI] [PubMed] [Google Scholar]
- 40.Attar A, Maunoury V, Vahedi K, Vernier-Massouille G, Vida S, Bulois P, Colombel JF, Bouhnik Y; GETAID. Safety and efficacy of extractible self-expandable metal stents in the treatment of Crohn’s disease intestinal strictures: a prospective pilot study. Inflamm Bowel Dis. 2012;18:1849–1854. doi: 10.1002/ibd.22844. [DOI] [PubMed] [Google Scholar]
- 41.Branche J, Attar A, Vernier-Massouille G, Bulois P, Colombel JF, Bouhnik Y, Maunoury V. Extractible self-expandable metal stent in the treatment of Crohn’s disease anastomotic strictures. Endoscopy. 2012;44 Suppl 2 UCTN:E325–E326. doi: 10.1055/s-0032-1309854. [DOI] [PubMed] [Google Scholar]
- 42.Loras C, Pérez-Roldan F, Gornals JB, Barrio J, Igea F, González-Huix F, González-Carro P, Pérez-Miranda M, Espinós JC, Fernández-Bañares F, et al. Endoscopic treatment with self-expanding metal stents for Crohn’s disease strictures. Aliment Pharmacol Ther. 2012;36:833–839. doi: 10.1111/apt.12039. [DOI] [PubMed] [Google Scholar]
- 43.Karstensen JG, Christensen KR, Brynskov J, Rønholt C, Vilmann P, Hendel J. Biodegradable stents for the treatment of bowel strictures in Crohn’s disease: technical results and challenges. Endosc Int Open. 2016;4:E296–E300. doi: 10.1055/s-0042-101940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Navaneethan U, Lourdusamy V, Njei B, Shen B. Endoscopic balloon dilation in the management of strictures in Crohn’s disease: a systematic review and meta-analysis of non-randomized trials. Surg Endosc. 2016;30:5434–5443. doi: 10.1007/s00464-016-4902-1. [DOI] [PubMed] [Google Scholar]
- 45.Menon AM, Mirza AH, Moolla S, Morton DG. Adenocarcinoma of the small bowel arising from a previous strictureplasty for Crohn’s disease: report of a case. Dis Colon Rectum. 2007;50:257–259. doi: 10.1007/s10350-006-0771-3. [DOI] [PubMed] [Google Scholar]
- 46.Partridge SK, Hodin RA. Small bowel adenocarcinoma at a strictureplasty site in a patient with Crohn’s disease: report of a case. Dis Colon Rectum. 2004;47:778–781. doi: 10.1007/s10350-003-0101-y. [DOI] [PubMed] [Google Scholar]
- 47.Barwood N, Platell C. Case report: adenocarcinoma arising in a Crohn’s stricture of the jejunum. J Gastroenterol Hepatol. 1999;14:1132–1134. doi: 10.1046/j.1440-1746.1999.02020.x. [DOI] [PubMed] [Google Scholar]
- 48.Jaskowiak NT, Michelassi F. Adenocarcinoma at a strictureplasty site in Crohn’s disease: report of a case. Dis Colon Rectum. 2001;44:284–287. doi: 10.1007/BF02234306. [DOI] [PubMed] [Google Scholar]
- 49.Collier PE, Turowski P, Diamond DL. Small intestinal adenocarcinoma complicating regional enteritis. Cancer. 1985;55:516–521. doi: 10.1002/1097-0142(19850201)55:3<516::aid-cncr2820550308>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 50.Ribeiro MB, Greenstein AJ, Heimann TM, Yamazaki Y, Aufses AH Jr. Adenocarcinoma of the small intestine in Crohn’s disease. Surg Gynecol Obstet. 1991;173:343–349. [PubMed] [Google Scholar]
- 51.Gustavsson A, Magnuson A, Blomberg B, Andersson M, Halfvarson J, Tysk C. Endoscopic dilation is an efficacious and safe treatment of intestinal strictures in Crohn’s disease. Aliment Pharmacol Ther. 2012;36:151–158. doi: 10.1111/j.1365-2036.2012.05146.x. [DOI] [PubMed] [Google Scholar]
- 52.Blomberg B, Rolny P, Järnerot G. Endoscopic treatment of anastomotic strictures in Crohn’s disease. Endoscopy. 1991;23:195–198. doi: 10.1055/s-2007-1010654. [DOI] [PubMed] [Google Scholar]
- 53.Williams AJ, Palmer KR. Endoscopic balloon dilatation as a therapeutic option in the management of intestinal strictures resulting from Crohn’s disease. Br J Surg. 1991;78:453–454. doi: 10.1002/bjs.1800780421. [DOI] [PubMed] [Google Scholar]
- 54.Breysem Y, Janssens JF, Coremans G, Vantrappen G, Hendrickx G, Rutgeerts P. Endoscopic balloon dilation of colonic and ileo-colonic Crohn’s strictures: long-term results. Gastrointest Endosc. 1992;38:142–147. doi: 10.1016/s0016-5107(92)70379-4. [DOI] [PubMed] [Google Scholar]
- 55.Couckuyt H, Gevers AM, Coremans G, Hiele M, Rutgeerts P. Efficacy and safety of hydrostatic balloon dilatation of ileocolonic Crohn’s strictures: a prospective longterm analysis. Gut. 1995;36:577–580. doi: 10.1136/gut.36.4.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ramboer C, Verhamme M, Dhondt E, Huys S, Van Eygen K, Vermeire L. Endoscopic treatment of stenosis in recurrent Crohn’s disease with balloon dilation combined with local corticosteroid injection. Gastrointest Endosc. 1995;42:252–255. doi: 10.1016/s0016-5107(95)70101-x. [DOI] [PubMed] [Google Scholar]
- 57.Matsui T, Ikeda K, Tsuda S, Yao K, Sou S, Satoh S, Hatakeyama S, Matake H, Sakurai T, Yao T. Long-term outcome of endoscopic balloon dilation in obstructive gastrointestinal Crohn’s disease: a prospective long-term study. Diagn Ther Endosc. 2000;6:67–75. doi: 10.1155/DTE.6.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Dear KL, Hunter JO. Colonoscopic hydrostatic balloon dilatation of Crohn’s strictures. J Clin Gastroenterol. 2001;33:315–318. doi: 10.1097/00004836-200110000-00012. [DOI] [PubMed] [Google Scholar]
- 59.Brooker JC, Beckett CG, Saunders BP, Benson MJ. Long-acting steroid injection after endoscopic dilation of anastomotic Crohn’s strictures may improve the outcome: a retrospective case series. Endoscopy. 2003;35:333–337. doi: 10.1055/s-2003-38145. [DOI] [PubMed] [Google Scholar]
- 60.Morini S, Hassan C, Lorenzetti R, Zullo A, Cerro P, Winn S, Giustini M, Taggi F. Long-term outcome of endoscopic pneumatic dilatation in Crohn’s disease. Dig Liver Dis. 2003;35:893–897. doi: 10.1016/j.dld.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 61.Sabaté JM, Villarejo J, Bouhnik Y, Allez M, Gornet JM, Vahedi K, Modigliani R, Lémann M. Hydrostatic balloon dilatation of Crohn’s strictures. Aliment Pharmacol Ther. 2003;18:409–413. doi: 10.1046/j.1365-2036.2003.01715.x. [DOI] [PubMed] [Google Scholar]
- 62.Thomas-Gibson S, Brooker JC, Hayward CM, Shah SG, Williams CB, Saunders BP. Colonoscopic balloon dilation of Crohn’s strictures: a review of long-term outcomes. Eur J Gastroenterol Hepatol. 2003;15:485–488. doi: 10.1097/01.meg.0000059110.41030.bc. [DOI] [PubMed] [Google Scholar]
- 63.Singh VV, Draganov P, Valentine J. Efficacy and safety of endoscopic balloon dilation of symptomatic upper and lower gastrointestinal Crohn’s disease strictures. J Clin Gastroenterol. 2005;39:284–290. doi: 10.1097/01.mcg.0000155128.31208.44. [DOI] [PubMed] [Google Scholar]
- 64.Ajlouni Y, Iser JH, Gibson PR. Endoscopic balloon dilatation of intestinal strictures in Crohn’s disease: safe alternative to surgery. J Gastroenterol Hepatol. 2007;22:486–490. doi: 10.1111/j.1440-1746.2006.04764.x. [DOI] [PubMed] [Google Scholar]
- 65.Ferlitsch A, Reinisch W, Püspök A, Dejaco C, Schillinger M, Schöfl R, Pötzi R, Gangl A, Vogelsang H. Safety and efficacy of endoscopic balloon dilation for treatment of Crohn’s disease strictures. Endoscopy. 2006;38:483–487. doi: 10.1055/s-2006-924999. [DOI] [PubMed] [Google Scholar]
- 66.Nomura E, Takagi S, Kikuchi T, Negoro K, Takahashi S, Kinouchi Y, Hiwatashi N, Shimosegawa T. Efficacy and safety of endoscopic balloon dilation for Crohn’s strictures. Dis Colon Rectum. 2006;49:S59–S67. doi: 10.1007/s10350-006-0685-0. [DOI] [PubMed] [Google Scholar]
- 67.Foster EN, Quiros JA, Prindiville TP. Long-term follow-up of the endoscopic treatment of strictures in pediatric and adult patients with inflammatory bowel disease. J Clin Gastroenterol. 2008;42:880–885. doi: 10.1097/MCG.0b013e3181354440. [DOI] [PubMed] [Google Scholar]
- 68.Hoffmann JC, Heller F, Faiss S, von Lampe B, Kroesen AJ, Wahnschaffe U, Schulzke JD, Zeitz M, Bojarski C. Through the endoscope balloon dilation of ileocolonic strictures: prognostic factors, complications, and effectiveness. Int J Colorectal Dis. 2008;23:689–696. doi: 10.1007/s00384-008-0461-9. [DOI] [PubMed] [Google Scholar]
- 69.Stienecker K, Gleichmann D, Neumayer U, Glaser HJ, Tonus C. Long-term results of endoscopic balloon dilatation of lower gastrointestinal tract strictures in Crohn’s disease: a prospective study. World J Gastroenterol. 2009;15:2623–2627. doi: 10.3748/wjg.15.2623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mueller T, Rieder B, Bechtner G, Pfeiffer A. The response of Crohn’s strictures to endoscopic balloon dilation. Aliment Pharmacol Ther. 2010;31:634–639. doi: 10.1111/j.1365-2036.2009.04225.x. [DOI] [PubMed] [Google Scholar]
- 71.Thienpont C, D’Hoore A, Vermeire S, Demedts I, Bisschops R, Coremans G, Rutgeerts P, Van Assche G. Long-term outcome of endoscopic dilatation in patients with Crohn’s disease is not affected by disease activity or medical therapy. Gut. 2010;59:320–324. doi: 10.1136/gut.2009.180182. [DOI] [PubMed] [Google Scholar]
- 72.Scimeca D, Mocciaro F, Cottone M, Montalbano LM, D’Amico G, Olivo M, Orlando R, Orlando A. Efficacy and safety of endoscopic balloon dilation of symptomatic intestinal Crohn’s disease strictures. Dig Liver Dis. 2011;43:121–125. doi: 10.1016/j.dld.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 73.Karstensen JG, Hendel J, Vilmann P. Endoscopic balloon dilatation for Crohn’s strictures of the gastrointestinal tract is feasible. Dan Med J. 2012;59:A4471. [PubMed] [Google Scholar]
- 74.de’Angelis N, Carra MC, Borrelli O, Bizzarri B, Vincenzi F, Fornaroli F, De Caro G, de’Angelis GL. Short- and long-term efficacy of endoscopic balloon dilation in Crohn’s disease strictures. World J Gastroenterol. 2013;19:2660–2667. doi: 10.3748/wjg.v19.i17.2660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Endo K, Takahashi S, Shiga H, Kakuta Y, Kinouchi Y, Shimosegawa T. Short and long-term outcomes of endoscopic balloon dilatation for Crohn’s disease strictures. World J Gastroenterol. 2013;19:86–91. doi: 10.3748/wjg.v19.i1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Honzawa Y, Nakase H, Matsuura M, Higuchi H, Toyonaga T, Matsumura K, Yoshino T, Okazaki K, Chiba T. Prior use of immunomodulatory drugs improves the clinical outcome of endoscopic balloon dilation for intestinal stricture in patients with Crohn’s disease. Dig Endosc. 2013;25:535–543. doi: 10.1111/den.12029. [DOI] [PubMed] [Google Scholar]
- 77.Nanda K, Courtney W, Keegan D, Byrne K, Nolan B, O’Donoghue D, Mulcahy H, Doherty G. Prolonged avoidance of repeat surgery with endoscopic balloon dilatation of anastomotic strictures in Crohn’s disease. J Crohns Colitis. 2013;7:474–480. doi: 10.1016/j.crohns.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 78.Atreja A, Aggarwal A, Dwivedi S, Rieder F, Lopez R, Lashner BA, Brzezinski A, Vargo JJ, Shen B. Safety and efficacy of endoscopic dilation for primary and anastomotic Crohn’s disease strictures. J Crohns Colitis. 2014;8:392–400. doi: 10.1016/j.crohns.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 79.Bhalme M, Sarkar S, Lal S, Bodger K, Baker R, Willert RP. Endoscopic balloon dilatation of Crohn’s disease strictures: results from a large United kingdom series. Inflamm Bowel Dis. 2014;20:265–270. doi: 10.1097/01.MIB.0000439067.76964.53. [DOI] [PubMed] [Google Scholar]
- 80.Hagel AF, Hahn A, Dauth W, Matzel K, Konturek PC, Neurath MF, Raithel M. Outcome and complications of endoscopic balloon dilatations in various types of ileocaecal and colonic stenosis in patients with Crohn’s disease. Surg Endosc. 2014;28:2966–2972. doi: 10.1007/s00464-014-3559-x. [DOI] [PubMed] [Google Scholar]
- 81.Krauss E, Agaimy A, Gottfried A, Maiss J, Weidinger T, Albrecht H, Hartmann A, Hohenberger W, Neurath MF, Kessler H, et al. Long term follow up of through-the-scope balloon dilation as compared to strictureplasty and bowel resection of intestinal strictures in crohn’s disease. Int J Clin Exp Pathol. 2014;7:7419–7431. [PMC free article] [PubMed] [Google Scholar]
- 82.Ding NS, Yip WM, Choi CH, Saunders B, Thomas-Gibson S, Arebi N, Humphries A, Hart A. Endoscopic Dilatation of Crohn’s Anastomotic Strictures is Effective in the Long Term, and Escalation of Medical Therapy Improves Outcomes in the Biologic Era. J Crohns Colitis. 2016;10:1172–1178. doi: 10.1093/ecco-jcc/jjw072. [DOI] [PubMed] [Google Scholar]


