Abstract
Background:
Augmentation mammoplasty remains the most common cosmetic surgery procedure performed. The objective of this article is to evaluate the impact of augmented volume of the reconstructed breast in patients that undergo nipple-sparing mastectomy and patients previously augmented who undergo mastectomy with tissue expander/implant-based reconstruction.
Methods:
Patients undergoing skin-sparing mastectomy, nipple-sparing mastectomy, and mastectomy after previous augmentation followed by tissue expander/implant-based reconstruction between June 2011 and April 2015 by 2 surgeons at the same institution were included. Retrospective chart review of the patients identified using these criteria was performed to record patient characteristics, complications, breast volume, implant volume, and percentage change in volume at the time of reconstruction. Percentage change of breast volume was calculated using the formula (implant breast weight)/(breast weight) for skin-sparing and nipple-sparing mastectomy patients and (final breast implant weight − [breast weight + augmentation breast implant weight])/([breast weight + augmentation breast implant]) for patients undergoing mastectomy following previous augmentation.
Results:
A total of 293 patients were included in the study with 63 patients who underwent nipple-sparing mastectomy, 166 patients who underwent skin-sparing mastectomy, and 64 patients who underwent previous augmentation with subsequent mastectomy. Mean percentage change in breast volume was 66% in the nipple-sparing mastectomy group, 15% for the right breast and 18% for the left breast in the skin-sparing mastectomy group, and 81% for the right breast and 72% for the left breast in the mastectomy following previous augmentation group. Complication rate for nipple-sparing mastectomy was 27%, mastectomy following previous augmentation was 20.3%, and skin-sparing mastectomy group was 18.7%.
Conclusion:
Patients who undergo nipple-sparing mastectomy or mastectomy following previous augmentation have the ability to achieve greater volume in their reconstructed breast via tissue expander/implant-based reconstruction.
Keywords: breast, reconstruction, augmentation, breast cancer, tissue expander, implant, mastectomy
Introduction
According to the American Society of Plastic Surgery augmentation, mammoplasty has been the most common procedure performed by plastic surgeons since 2006. In a total of 279, 143 breast augmentations were performed in 2015.1 The large population of women who pursue breast augmentation has implications to the reconstructive surgeon as many patients who present for reconstructive surgery have the desire for enhancement of their native breast volume. Following mastectomy patients who undergo breast reconstruction have been shown to have increased satisfaction with surgical outcomes and better body image compared to women who do not pursue reconstructive measures.2-4
Breast cancer remains the most common form of cancer in women regardless of race or ethnicity affecting approximately 123 per 100 000 women annually. In 2013, 230 815 women were diagnosed with breast cancer.5 Options for treatment of breast cancer include breast-conserving therapy, mastectomy, and mastectomy followed by reconstruction. Over the past 10 years, there has been a trend toward an increase in number of nipple-sparing mastectomies performed with a decrease in the number of nonnipple-nonskin–sparing mastectomies as well as a trend toward implant-based reconstruction.6 Of the 106 338 reconstructive breast procedures performed in 2015, 73% were tissue expander/implant-based reconstruction.1
The trend toward nipple-sparing mastectomy in the appropriately selected patient with implant-based reconstruction allows for the reconstructive plastic surgeon to augment the native skin envelope of the breast. In a society of women who desire increased breast volume via augmentation mammoplasty, this combination of mastectomy and reconstructive technique would allow for women to achieve breasts which are larger than their native breasts. A previous article from this institution demonstrated patients who undergo skin-sparing mastectomy with tissue expander/implant-based reconstruction with final implants larger in volume than the native breast have increased satisfaction with their reconstruction without an increase in complication rate.7 The authors believe an increase in reconstructed breast volume can also be achieved via nipple-sparing mastectomy in patients who desire a reconstructed breast that is larger than the native breast. Similarly, in patients with a history of breast augmentation who undergo mastectomy, a reconstructed breast volume that is greater than their previous volume can be achieved.
Methods
After institutional review board approval (pro 00019460), a retrospective chart review was performed on patients who underwent skin-sparing mastectomy, nipple-sparing mastectomy, and mastectomy after previous augmentation followed by tissue expander/implant-based reconstruction between June 2011 and April 2015 by 2 surgeons at a single institution. All patients had their procedures performed at Moffitt Cancer Center, a National Cancer Institute Comprehensive Cancer Center. Patients who underwent additional flap reconstruction and those with incomplete data were excluded. Retrospective chart review of the patients identified using these criteria was performed to record patient characteristics, complications (including hematoma, seroma, infection, wound dehiscence, and full thickness skin loss requiring reoperation), native breast volume, augmentation implant volume, implant volume, and percentage change in volume at the time of reconstruction.
The change in breast volume was calculated using the following formula for skin-sparing and nipple-sparing mastectomy:
For patients with previous breast augmentation who underwent mastectomy, the following formula was used:
The recorded mastectomy specimen mass was used as a measure for native breast volume. Density of breast tissue was assumed to be 1 g/mL for all cases. Each breast was considered separately regardless of whether the reconstruction was unilateral or bilateral.
Statistical calculations were performed with Number Cruncher Statistical System 2007 Statistical Software (Utah) program for Windows. Standard descriptive statistical calculations were collected; unpaired t test was used in the comparison of groups. Statistical significance was established at P < .05.
Results
A total of 293 patients were included in the study with 63 patients who underwent nipple-sparing mastectomy, 166 patients who underwent skin-sparing mastectomy, and 64 patients with history of breast augmentation who underwent mastectomy. Mean change in breast volume was 66% bilaterally in the nipple-sparing mastectomy group, 15% for the right breast and 18% for the left breast in the skin-sparing mastectomy group, and 81% for the right breast and 72% for the left breast in the mastectomy following previous augmentation group (Table 1 and Figure 1). Complication rate for nipple-sparing mastectomy was 27%, mastectomy following previous augmentation was 20.3%, and skin-sparing mastectomy group was 18.7% (Table 2).
Table 1.
Comparison of Patient Characteristics in Women Undergoing Tissue Expander/Implant-Based Reconstruction.
| Group | Age at Reconstruction (years) | Right Implant Volume (mL) | Left Implant Volume (mL) | % Change in Right Breast Volume | % Change in Left Breast Volume |
|---|---|---|---|---|---|
| Nipple-sparing mastectomy | |||||
| N | 63 | 63 | 63 | 63 | 63 |
| Mean | 48 | 607 | 607 | .66 | .66 |
| Median | 48 | 560 | 560 | .63 | .63 |
| Standard deviation | 10.77 | 156 | 156 | .51 | .51 |
| Minimum | 27 | 325 | 325 | -.15 | -.15 |
| Maximum | 66 | 900 | 900 | 1.93 | 1.93 |
| Skin-sparing mastectomy | |||||
| N | 166 | 157 | 150 | 136 | 138 |
| Mean | 54 | 579 | 620 | .25 | .25 |
| Median | 55 | 600 | 640 | .15 | .18 |
| Standard deviation | 12.15 | 203 | 166 | .62 | .59 |
| Minimum | 23 | 120 | 120 | -1.0 | -1.0 |
| Maximum | 82 | 1100 | 1100 | 3.11 | 3.24 |
| Previous augmentation and mastectomy | |||||
| N | 64 | 53 | 50 | 48 | 48 |
| Mean | 51 | 551 | 551 | .81 | .72 |
| Median | 51 | 550 | 575 | .75 | .76 |
| Standard deviation | 11.16 | 145 | 152 | .54 | .61 |
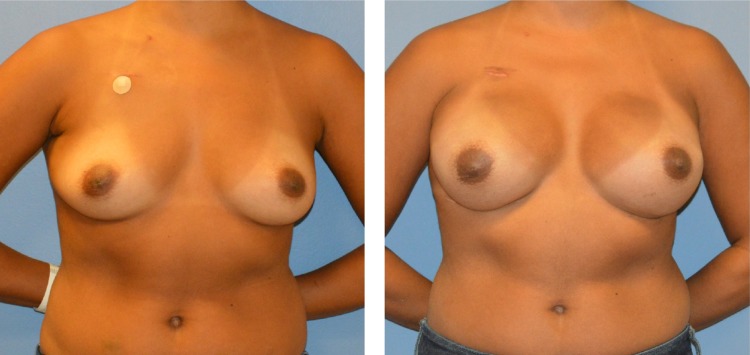
Figure 1.
Patient prior to mastectomy (left) and after nipple-sparing mastectomy with tissue expander/implant reconstruction (right).
Table 2.
Comparison of Complication Rates Between Nipple-Sparing Mastectomy, Skin-Sparing Mastectomy, and History of Augmentation Followed by Mastectomy.
| Procedure Performed | Number of Complications | % Within Group |
|---|---|---|
| Nipple-sparing mastectomy | 17/63 | 27 |
| Skin-sparing mastectomy | 31/166 | 18.7 |
| History of augmentation followed by mastectomy | 13/64 | 20.3 |
Discussion
Traditionally, the goal of reconstruction has been to restore the patient to their preoperative state; however, many women desire augmentation of their native breast tissue. Reconstructive plastic surgeons now have the ability to achieve outcomes that are analogous with esthetic standards of cosmetic breast surgery.8 In women pursuing cosmetic breast augmentation, the motivation toward augmentation was found to be related to 1 basic drive (femininity) and 6 generating factors (appearance dissatisfaction, ideal figure, self-esteem, comments, clothes, and sexuality).9 These factors likely also play a role in patient expectations in reconstructive breast surgery.
Women who have undergone previous breast augmentation that are later diagnosed with breast cancer are more likely to pursue implant-based reconstruction with the goal of maintaining and enhancing breast volume.10,11 In this series, patients with a history of breast augmentation who underwent mastectomy had an average age of 51 with a mean percentage change in breast volume at reconstruction of 81% in the right breast and 72% in the left breast. Women with a history of cosmetic augmentation likely pursue implant-based reconstruction as this will allow for them to most closely achieve the results they originally obtained from their cosmetic procedure. This group of patients demonstrated the largest increase in breast volume in our series of patients. The reasoning behind this finding is likely multifactorial in nature; however, it is suspected to be related to patient expectations as these women had undergone breast enhancement surgery in the past and desired the augmented appearance with larger volume breasts than their native tissue.
Recently, a trend toward an increase in the number of nipple-sparing mastectomies performed has been observed in the appropriately selected patients. Traditionally, contraindications to this procedure have been gigantomastia and grade III ptosis; however, it has been shown that the esthetic and reconstructive benefits of performing nipple-sparing mastectomy in patients with larger breasts are greater than the risk of complications including skin necrosis and wound breakdown.12 In a series of 913 patients treated with nipple-sparing mastectomy, 92.2% of all cases underwent implant-based reconstruction either directly to implant or by the use of tissue expander to implant.13 In our series of patients, 63 women with an average age of 48 were treated with nipple-sparing mastectomy followed by tissue expander/implant-based reconstruction. The change in breast volume was found to be 66% for the bilateral breasts, thereby demonstrating the tendency toward increased volume in the reconstructive breast in this practice. The complication rate noted for this group of patients in our series was 27%.
A previous study from this institution evaluating increased breast volume following skin-sparing mastectomy with implant-based reconstruction reported an increase in patient satisfaction scores with outcomes of sexual well-being, satisfaction with information, and satisfaction with surgeon without a significant increase in complication rates.7 Published complication rates in bilateral tissue expander/implant reconstruction have been reported between 18% and 21%.7,14,15 These complication rates are similar to the rates reported in this study with 18.7% in patients treated with skin-sparing mastectomy, 20.3% in patients with history of augmentation undergoing mastectomy, and 27% in patients undergoing nipple-sparing mastectomy. The comparable complication rates in women treated with implant-based reconstruction with increased breast volume highlight that this is a viable option to women who desire enhancement of their premastectomy breast volume.
There are several limitations to our study. Although we have objective data regarding increase in volume of breasts related to complication rates, there has been a strong shift toward patient-reported outcomes that have not been included in this study. Further research regarding patient satisfaction in our cohort of patients who achieved larger volume in the reconstructed breasts following nipple-sparing mastectomy and mastectomy in patients with a history of breast augmentation could reinforce the psychosocial benefit of the procedure. Furthermore, evaluation of patients treated with tissue expander/implant-based reconstruction to match their native breast tissue who later desire increase in volume of their reconstructed breasts may further serve to highlight patients’ desire for enhancement of the native breast tissue in reconstruction. A portion of included participants underwent unilateral reconstructions which may skew that data as the individual breasts were included in that data for increase in volume with reconstruction and in unilateral cases, the goal would be for symmetry with the contralateral breast rather than augmentation of the native breast. In addition, the study used a presumed breast density of 1 gm/mL to calculate mastectomy specimen volume. Breast parenchyma density has been reported at 1.07 gm/mL in premenopausal women and 1.06 gm/mL in postmenopausal women.16 The use of 1 gm/mL slightly distorts data during conversion of mastectomy sample mass to volumetric measurement. Although formulas have been proposed to convert mastectomy mass into breast volume, there has yet to be a validated tool published in the current literature.17
Conclusion
In the age of breast augmentation, breast reconstruction can provide women with the opportunity to increase their native breast volume. Women who undergo nipple-sparing mastectomy and mastectomy with a history of augmentation can increase the volume of their reconstructed breasts without an increased rate of complications.
Footnotes
Authors’ Note: No significant relationships exist between the authors and the companies/organizations whose products or services may be referenced in this article. Poster presented at the annual Southeastern Society of Plastic and Reconstructive Surgeons 2016.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Plastic Surgery Statistics Report. ASPS National Clearinghouse of Plastic Surgery Procedural Statistics. 2015; http://www.plasticsurgery.org/.
- 2. Nicholson RM, Leinster S, Sassoon EM. A comparison of the cosmetic and psychological outcome of breast reconstruction, breast conserving surgery and mastectomy without reconstruction. Breast. 2007;16(4):396–410. [DOI] [PubMed] [Google Scholar]
- 3. Aguiar IC, Veiga DF, Marques TF, Novo NF, Sabino Neto M, Ferreira LM. Patient-reported outcomes measured by BREAST-Q after implant-based breast reconstruction: a cross-sectional controlled study in Brazilian patients. Breast. 2016;31:22–25. [DOI] [PubMed] [Google Scholar]
- 4. Rubino C, Figus A, Lorettu L, Sechi G. Post-mastectomy reconstruction: a comparative analysis on psychosocial and psychopathological outcomes. J Plast Reconstr Aesthet Surg. 2007;60(5):509–518. [DOI] [PubMed] [Google Scholar]
- 5. U.S. Cancer Statistics Working Group. United States Cancer Statistics: 1999-2013 Incidence and Mortality Web Based Report. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2016. [Google Scholar]
- 6. Chang JM, Kosiorek HE, Dueck AC, et al. Trends in mastectomy and reconstruction for breast cancer; a twelve year experience from a tertiary care center. Am J Surg. 2016;212(6):1201–1210. [DOI] [PubMed] [Google Scholar]
- 7. Huber KM, Zemina KL, Tugertimur B, et al. Outcomes of breast reconstruction after mastectomy using tissue expander and implant reconstruction. Ann Plast Surg. 2016;76(suppl 4):S316–S319. [DOI] [PubMed] [Google Scholar]
- 8. Rochlin DH, Davis CR, Nguyen DH. Breast augmentation and breast reconstruction demonstrate equivalent aesthetic outcomes. Plast Reconstr Surg Glob Open. 2016;4(7):e811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Solvi AS, Foss K, von Soest T, Roald HE, Skolleborg KC, Holte A. Motivational factors and psychological processes in cosmetic breast augmentation surgery. J Plast Reconstr Aesthet Surg. 2010;63(4):673–680. [DOI] [PubMed] [Google Scholar]
- 10. Spear SL, Slack C, Howard MA. Postmastectomy reconstruction of the previously augmented breast: diagnosis, staging, methodology, and outcome. Plast Reconstr Surg. 2001;107(5):1167–1176. [DOI] [PubMed] [Google Scholar]
- 11. Carlson GW, Moore B, Thornton JF, Elliott M, Bolitho G. Breast cancer after augmentation mammaplasty: treatment by skin-sparing mastectomy and immediate reconstruction. Plast Reconstr Surg. 2001;107(3):687–692. [DOI] [PubMed] [Google Scholar]
- 12. Wang F, Alvarado M, Ewing C, Esserman L, Foster R, Sbitany H. The impact of breast mass on outcomes of total skin-sparing mastectomy and immediate tissue expander-based breast reconstruction. Plast Reconstr Surg. 2015;135(3):672–679. [DOI] [PubMed] [Google Scholar]
- 13. Casella D, Calabrese C, Orzalesi L, et al. Current trends and outcomes of breast reconstruction following nipple-sparing mastectomy: results from a national multicentric registry with 1006 cases over a 6-year period. Breast Cancer. 2016;24(3):451–457. [DOI] [PubMed] [Google Scholar]
- 14. Alderman AK, Hu E, Atisha D, Wilkins EG. Surgical outcomes of breast reconstruction: comparison of autogenous tissue and expander/implant techniques. Expert Rev Pharmacoecon Outcomes Res. 2007;7(4):385–391. [DOI] [PubMed] [Google Scholar]
- 15. Antony AK, McCarthy C, Disa JJ, Mehrara BJ. Bilateral implant breast reconstruction: outcomes, predictors, and matched cohort analysis in 730 2-stage breast reconstructions over 10 years. Ann Plast Surg. 2014;72(6):625–630. [DOI] [PubMed] [Google Scholar]
- 16. Parmar C, West M, Pathak S, Nelson J, Martin L. Weight versus volume in breast surgery: an observational study. JRSM Short Rep. 2011;2(11):87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Georgiou CA, Ihrai T, Chamorey E, Flipo B, Chignon-Sicard B. A formula for implant volume choice in breast reconstruction after nipple sparing mastectomy. Breast. 2012;21(6):781–782. [DOI] [PubMed] [Google Scholar]