Abstract
Objective
Intraoperative hypotension during hip fracture surgery is frequent in the elderly. No study has compared the haemodynamic effect of hypobaric unilateral spinal anaesthesia (HUSA) and standardised general anaesthesia (GA) in elderly patients undergoing hip fracture surgical repair.
Methods
We performed a prospective, randomised open study, including 40 patients aged over 75 years, comparing the haemodynamic effects of HUSA (5 mg isobaric bupivacaine with 5 μg sufentanil and 1 mL sterile water) and GA (induction with etomidate/remifentanil and maintenance with desflurane/remifentanil). An incidence of severe hypotension, defined by a decrease in systolic blood pressure of >40% from baseline, was the primary endpoint.
Results
The incidence of severe hypotension was lower in the HUSA group compared with that in the GA group (32% vs. 71%, respectively, p=0.03). The median [IQR] ephedrine consumption was lower (p=0.001) in the HUSA group (6 mg, 0–17 mg) compared with that in the GA group (36 mg, 21–57 mg). Intraoperative muscle relaxation and patients’ and surgeons’ satisfaction were similar between groups. No difference was observed in 5-day complications or 30-day mortality.
Conclusion
This study shows that HUSA provides better haemodynamic stability than GA, with lower consumption of ephedrine and similar operating conditions. This new approach of spinal anaesthesia seems to be safe and effective in elderly patients undergoing hip fracture surgery.
Keywords: Frail elderly, bupivacaine, spinal anesthesia, fractures, hip
Introduction
Both general and spinal anaesthesia can be used for surgical repair of traumatic hip fracture in elderly patients; however, which of the two techniques is more optimal remains a matter of debate. Several studies and meta-analyses suggest that compared with general anaesthesia (GA), regional anaesthesia may reduce one-month mortality; however, no conclusions can be drawn for longer-term mortality (1–6). A recent retrospective study including 18,158 patients reported that regional anaesthesia was associated with a lower adjusted odds ratio of in-hospital mortality and pulmonary complications related to GA after hip surgery (7). However, another recent retrospective study including 73,284 patients found no difference in the mortality risk by anaesthesia type, suggesting that the beneficial effect of regional anaesthesia may be more modest than previously reported (8). This was also reported in a retrospective study including 56,729 patients, which showed no difference in 30-day mortality between regional and GA, although a modestly shorter length of stay was observed (9).
Although research suggests that overall mortality may not be lowered by either general or regional anaesthesia, patients experiencing hypotension and tachycardia during surgery with increased perioperative troponin are at risk of perioperative cardiovascular complications, in particular geriatric patients with existing coronary disease (1–7). Several regional anaesthesia techniques aim to avoid deleterious decreases in arterial blood pressure and tachycardia in this specific population. Continuous spinal anaesthesia is a suitable technique for maintaining haemodynamic parameters during traumatic hip fracture surgical repair in elderly patients; however, its use is often limited by the frequent use of antiplatelet treatments in this population, such as clopidogrel (10). Using lipophilic opioids as adjuncts to spinal and unilateral spinal anaesthesia allows for a smaller dose of intrathecal local anaesthetic with lower haemodynamic effects compared with bilateral spinal or GA (11–14). Hypobaric unilateral spinal anaesthesia (HUSA) with a low dose (5mg bupivacaine) of a local anaesthetic combined with opioids (sufentanil 5 μg) has moderate haemodynamic effects (15). However, previous studies have not compared this technique with general anaesthesia. This study aimed to compare the haemodynamic effects of low-dose HUSA combined with opioids versus a conventional standardised GA in elderly patients aged over 75 years undergoing hip fracture surgical repair.
Methods
Study design
The present study was a single-centre, prospective, randomised, open control trial and was promoted by the Hospices Civils de Lyon (HCL/P 2006.433/26), registered by the French authorities on 10th May, 2007 (AFSSAPS registration number 2007-A00461-52), authorised by the French Ministry of Health on 24th August, 2007 (DGS 2007-0435) and approved by the Institutional Review Board (Comité de Protection des Personnes Sud-Est IV, reference number A07-139). Written informed consent was obtained from all patients or their closest relative. The design and description of the current trial adhered to the guidelines of the Consolidated Standards of Reporting Clinical Trials (CONSORT) statement (16).
Study population
Consecutive patients aged over 75 years undergoing emergent hip fracture surgical repair, between December 2006 and December 2007, in the emergent surgery ward of a university teaching hospital and with the American Society of Anaesthesiologists (ASA) physical status I–III, were enrolled. Exclusion criteria were consent refusal and contraindications to spinal anaesthesia (coagulation disorders, hyperthermia >38°C, local anaesthetic allergy and antiplatelet treatment using clopidogrel within 5 days).
Preoperative care
Preoperative care included providing hydration with 2 litres of 5% glucose and electrolytes (NaCl=4 g L−1, KCl = 2 g L−1) per day. When surgery was scheduled more than 12 hours after admission, preoperative anticoagulant treatment was initiated twice a day using 7500 IU of subcutaneous calcium heparin. Patients treated with oral anticoagulant therapy received a slow intravenous dose of 5 mg vitamin K followed by subcutaneous calcium heparin injections thrice per day, adjusted to activate partial thromboplastin time (aPTT), which is the standard protocol used at our institution.
Study protocol
The cognitive function of all patients was assessed during the preoperative visit using the mini mental state examination (MMSE) test (17). Before admission to the operating room, the attending anaesthesiologist, randomly assigned patients in a 1:1 ratio for parallel arms using a sealed-envelope technique from a computer-generated random list to receive either HUSA or GA. Patients, surgeons and anaesthesiologists were not blinded to group assignment because of the study protocol. All patients received an infusion of 5 mL kg−1 hydroxyethyl starch (HES) 130/0.4 administered in 15 min before spinal or GA to prevent hypotension (18–20). Standard monitoring during the procedure included continuous electrocardiography, pulse oximetry and non-invasive blood pressure measurements, conducted every 3 min during 30 min then and 5 min thereafter.
Patients receiving spinal anaesthesia were carefully turned to the lateral position for performing lumbar puncture with the fracture side up using a 22/25 gauge Quincke point needle (Polymedic®, SAS, Carrières-sur-Seine, France), positioned midline at the L3–L4 interspace by an experienced physician. To avoid any interference with cognitive function, no sedation was used during the procedure. The anaesthetic solution comprised 5 mg isobaric bupivacaine (rendered hypobaric by the addition of 1 mL sterile water) and 1 mL of 5 μg mL−1 sufentanil. The injection was made over 10–15 s, needle side opening up, without aspiration of the spinal fluid to avoid paddling, which may render the spinal anesthesia bilateral (21). Lateral position was maintained for 15 min and the patients were then positioned for surgery (reinstalled in dorsal decubitus or left in side decubitus according to the intervention) (15). The level of sensory blockade and intensity of motor blockade were bilaterally evaluated 15 min after spinal anaesthesia using the modified Bromage scale (0: able to lift extended leg at hip; 1: able to flex knee, but unable to lift extended leg; 2: able to move foot only and 3: unable to move even foot) and the pinprick sensory test. The total duration of motor and sensory block was measured. All patients received supplemental oxygen (3 L min−1) through an oxygen nasal cannula during the procedure.
Patients undergoing general anaesthesia received intravenous etomidate (0.3 mg kg−1) and remifentanil (0.5 μg kg−1 in 1 min), administered using an infusion pump. Remifentanil infusion was initiated at the same time as that of etomidate. The duration of etomidate injection was 30 s. The depth of anaesthesia was monitored using bispectral index (BIS) for careful titration of anaesthetic drugs (22). Tracheal intubation was performed when the BIS value was <40. In case the 0.3 mg kg−1 etomidate bolus was insufficient to obtain a BIS value <40 after one minute, another bolus of 0.1 mg kg−1 was administered every minute until a BIS value <40 was obtained. If the BIS value exceeded 60 during laryngoscopy, remifentanil infusion was increased to 0.75 μg kg−1 min−1 and laryngoscopy was postponed for one minute. Cisatracurium (0.15 mg kg−1) was used to facilitate tracheal intubation. Anaesthesia was maintained using remifentanil at a rate of 0.05–0.20 μg−1 kg−1 min−1, at the discretion of the attending anaesthesiologist, according to haemodynamic parameters and with desflurane adapted to the elderly population with a BIS target value of 40–60 (23, 24).
For all study patients, ‘moderate’ hypotension was defined by a decrease of systolic blood pressure (SBP) of >20% from the baseline SBP measured just before the induction of GA or HUSA. ‘Deep’ hypotension was defined by a decrease of >30% from baseline. ‘Severe’ hypotension was defined by a decrease of >40% from baseline. Severe hypotension or a SBP <100 mmHg were treated with an intravenous injection of 6 mg ephedrine every 3 min until the SBP was restored. Bradycardia, defined as heart rate (HR) <45 bpm, was treated with 0.5 mg intravenous atropine. SBP, diastolic blood pressure, mean blood pressure (MBP), HR, BIS values, peripheral saturation in oxygen (SpO2) and ephedrine consumption were measured every 3 min from the moment of SA needle withdrawal or GA induction during the first 30 min and every 5 min thereafter, until 120 min. In addition to the HES loading dose, patients received additional HES corresponding to the blood loss volume and lactated Ringer’s solution at a rate of 5 mL kg−1 h−1 for intraoperative volume expansion. The need for red blood cell transfusion was left at the discretion of the attending anaesthesiologist in case of estimated blood loss >500 mL.
Postoperative care
Postoperative analgesia was initiated one hour before the predictable end of surgery. It included intravenous administration of paracetamol (1 g) and nefopam (20 mg) in slow infusions of 30 min every 8 hrs. After arrival in the postanesthesia care unit (PACU), all patients received intravenous morphine titration if the pain estimated by a 0–10 numerical rating scale was higher than 3 or in the case of behaviours associated with acute pain in cognitively impaired patients (flailing, screaming, groaning, grimacing, resistance to movement or rigid body posture) (25). Patient satisfaction was estimated using the PACU as follows: excellent, good, fair or poor. Muscle relaxation during surgery and satisfaction with the provided anaesthesia were estimated by the surgeon at the end of the surgery as follows: excellent, good, fair or poor. All patients received deep vein thrombosis prophylaxis with 2.5 mg subcutaneous fondaparinux per day administered at least 8 hours after the end of the surgery or with 7500 IU subcutaneous calcium heparin twice a day in case of contraindication to fondaparinux. The occurrence of postoperative complications (cardiovascular events, red blood cell transfusion and mortality) within the first 5 postoperative days was recorded, and MMSE was repeated at day 5 for all patients.
Statistical analysis
The incidence of severe hypotension (decrease in SBP by >40%) when using HUSA in comparison with GA was the primary outcome. For power analysis, we referred to the studies of Minville et al. (10) and Casati et al. (14). The first study compared the incidence of hypotension after SA performed in elderly patients undergoing either hip fracture surgery with 7.5 mg bupivacaine or continuous SA with a median dose of 5 mg (10). The authors observed a 68% incidence of hypotension (decrease in SBP by >20% from baseline) in the SA group vs. 31% in the continuous SA group, and a 51% incidence of severe hypotension (decrease in SBP by >30% from baseline) vs. 8% in the continuous SA group (p<0.05). The second study compared the incidence of hypotension after SA using 7.5 mg of hyperbaric 0.5% bupivacaine or sevoflurane-based GA in elderly patients (14). In this study, hypotension (decrease in SBP by >20% from baseline) occurred in 46% patients receiving SA and in 80% receiving GA (p=0.05), and phenylephrine was required in 21% SA patients and 26% GA patients (NS). We found no previous study evaluating the effects of small dose hypobaric bupivacaine with opioid on severe hypotension after HUSA. We hypothesised a 50% difference in the incidence of severe hypotension between our two groups (60% in the GA and 30% in the HUSA group). Using a two-sided test, a power calculation with a probability level of 0.05 and a power of 80% yielded a sample size of 42 patients per group. An interim analysis on the incidence of severe hypotension was conducted by an independent data monitoring board after enrolment of the first 40 patients.
Quantitative data were expressed as mean±standard deviation (SD) or median [interquartile] according to the normality of their distribution assessed using the Shapiro-Wilk’s test. Student’s t-test was used for comparisons when the variables were normally distributed, whereas the Mann-Whitney U test was used otherwise. Hemodynamic parameters (HR and SBP) were compared during 120 min after the induction of GA or HUSA using analysis of variance (ANOVA) for repeated measures. Qualitative data were expressed as numbers (%) and were compared using χ2 or Fisher’s exact tests. P<0.05 was considered statistically significant. Data were analysed using the Statistica software® 8.0 (StatSoft Inc., Tulsa, OK, USA).
Results
For ethical reasons, the independent monitoring board stopped the trial after interim analysis of the first 40 patients because a statistically significant lower incidence of severe hypotension and total dose of ephedrine were observed in the HUSA group. Of the 54 patients initially enrolled, 2 refused to participate and 12 did not meet the inclusion criteria (Figure 1). Forty patients (32 women and 8 men; 21 with GA and 19 with HUSA) were randomised and were included in the analysis (Figure 1).
Figure 1.
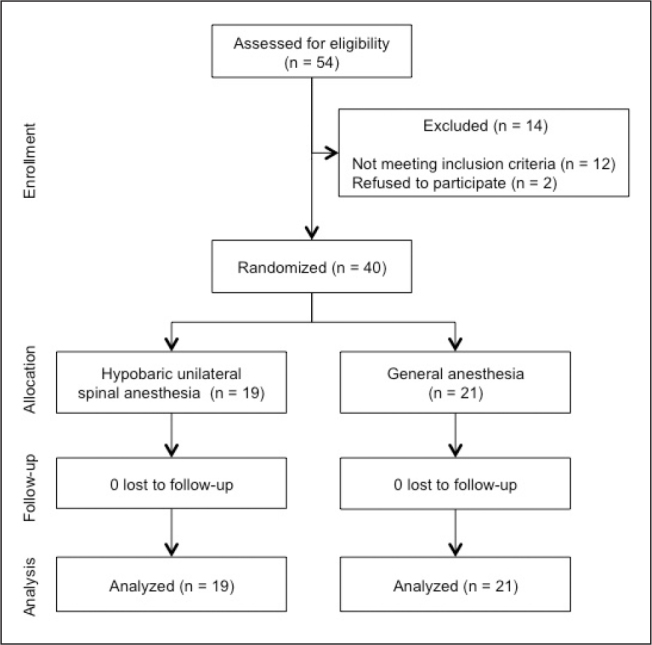
Flow chart
Table 1 includes patient and surgery characteristics, which show no significant differences. The times between admission and surgery, anaesthetic induction and skin incision and the duration and type of surgery were comparable between the groups (Table 1). The incidence of severe hypotension (primary endpoint) was lower in the HUSA group than that in the GA group (32% vs. 71%, respectively, p=0.03) (Table 2). The incidence of deep hypotension was also lower in the HUSA group; however, there was no difference in the incidence of moderate hypotension between the groups (Table 2). The median [IQR] number of episodes of deep hypotension (0 [0–1] vs. 4 [0–9], respectively, p<0.001) and the median [IQR] ephedrine dose (6 [0–17] vs. 36 [21–57], respectively, p<0.001) were lower in the HUSA group compared with that in the GA group (Table 2). The intraoperative administration of fluids or transfusion of red blood cells, incidence of postoperative nausea and vomiting and the total dose of morphine received in the PACU was similar between the groups (Table 2). There was a time-group interaction (p<0.01) for SBP (Figure 2) and HR (Figure 3) during the procedure in the HUSA and GA groups.
Table 1.
Patient and surgery characteristics. Results are expressed as mean±SD, median [IQR] or n (%)
| Hypobaric unilateral spinal anaesthesia (n=19) | General anaesthesia (n=21) | p | |
|---|---|---|---|
| Age (years) | 83±6 | 85±5 | 0.47 |
| Height (cm) | 158±7 | 161±6 | 0.22 |
| Weight (kg) | 54±14 | 59±12 | 0.23 |
| Gender | |||
| Male | 2 (11) | 6 (29) | |
| Female | 17 (89) | 15 (71) | 0.15 |
| ASA physical status | |||
| I | 2 (11) | 0 (0) | |
| II | 8 (42) | 10 (48) | |
| III | 9 (47) | 11 (52) | 0.31 |
| Comorbidities | |||
| Hypertension | 10 (53) | 10 (47) | 0.75 |
| Myocardial ischaemia | 5 (26) | 4 (19) | 0.58 |
| Chronic heart failure | 2 (11) | 3 (14)0.72 | |
| Delay to surgery (days) | 1 [1–3] | 1 [1–3] | 0.89 |
| MMSE | |||
| Preoperative visit | 19 [12–26] | 21 [12–24] | 0.75 |
| At day 5 | 22 [14–26] | 20 [12–23] | 0.50 |
| Time to incision* (min) | 43 [36–45] | 40 [35–46] | 0.96 |
| Type of surgery | |||
| Intramedullary nail | 14 (74) | 12 (57) | |
| DHS plate | 3 (16) | 2 (10) | |
| Hip arthroplasty | 2 (10) | 7 (33) | 0.22 |
| Duration of surgery (min) | 35 [30–49] | 45 [34–53] | 0.33 |
Time between induction of spinal or general anaesthesia and skin incision.
ASA: American Society of Anaesthesiologists; DHS: dynamic hip screw; MMSE: mini mental status examination (18)
Table 2.
Study data. Results are expressed as mean±SD, median [IQR] or n (%)
| Hypobaric unilateral spinal anaesthesia (n=19) | General anaesthesia (n=21) | p | |
|---|---|---|---|
| Incidence of hypotension | |||
| Moderatea | 17 (89) | 21 (100) | 0.22 |
| Deepb | 11 (58) | 21 (100) | <0.001 |
| Severec | 6 (32) | 15 (71) | 0.03 |
| Episodes of hypotension | |||
| Moderatea | 6 [1–9] | 3 [2–6] | 0.49 |
| Deepb | 1 [0–7] | 5 [2–7] | 0.08 |
| Severec | 0 [0–1] | 4 [0–9] | <0.001 |
| Ephedrine (mg) | 6 [0–17] | 36 [21–57] | <0.001 |
| Fluids (mL) | |||
| Crystalloids | 375 [282–483] | 435 [347–546] | 0.20 |
| HES 130/0.4 | 250 [231–311] | 300 [269–318] | 0.91 |
| Intraoperative RBC transfusion | 3 (16) | 5 (24) | 0.81 |
| PONV in PACU | 3 (16) | 1 (5) | 0.53 |
| Morphine in PACU (mg) | 0 [0–2] | 0 [0–4] | 0.59 |
| Muscle relaxation | 0.11 | ||
| Excellent | 12 (63) | 19 (90) | |
| Good | 6 (32) | 2 (10) | |
| Fair | 1 (5) | 0 (0) | |
| Poor | 0 (0) | 0 (0) | |
| Surgeon satisfaction | 0.19 | ||
| Excellent | 13 (68) | 19 (90) | |
| Good | 5 (26.5) | 2 (10) | |
| Fair | 1 (5.5) | 0 (0) | |
| Poor | 0 (0) | 0 (0) | |
| Patient satisfaction | 0.32 | ||
| Excellent | 10 (53) | 5 (23) | |
| Good | 7 (37) | 10 (50) | |
| Fair | 0 (0) | 1 (4) | |
| Poor | 0 (0) | 0 (0) | |
| No answer | 2 (10) | 5 (23) | |
| Postoperative complications ≤5 days | |||
| Troponin elevation | 1 (5) | 2 (10) | 0.93 |
| RBC transfusion | 1 (5) | 0 (0) | 0.96 |
| IDDVT | 1 (5) | 1 (5) | 0.51 |
DHS: dynamic hip screw; HES: hydroxyethyl starch; IDDVT: isolated distal deep vein thrombosis, PACU: postanesthesia care unit; PONV: postoperative nausea and vomiting; RBC: red blood cell
Systolic blood pressure decrease by >20% from baseline
Systolic blood pressure decrease by >30% from baseline
Systolic blood pressure decrease by >40% from baseline
Figure 2.
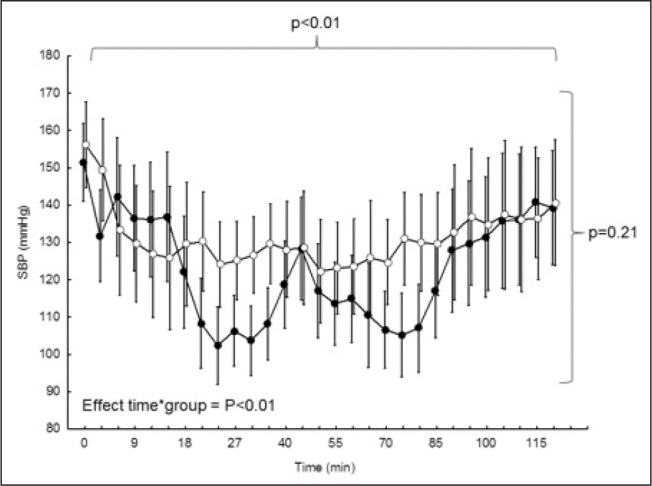
Evolution of systolic blood pressure with time between the groups (analysis of variance for repeated measures)
Open circles (○) represent unilateral spinal anaesthesia and filled circles (●) represent general anaesthesia. Error bars denote 95% confidence interval
Figure 3.
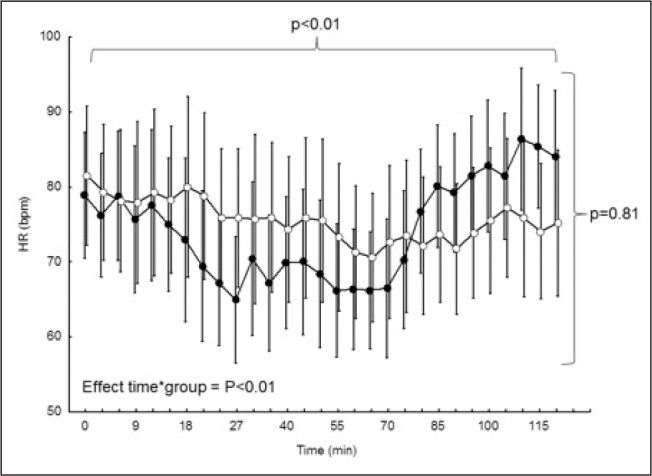
Evolution of heart rate with time between the groups (analysis of variance for repeated measures)
Open circles (○) represent unilateral spinal anaesthesia and filled circles (●) represent general anaesthesia. Error bars denote 95% confidence interval
The quality of muscle relaxation was rated excellent or good by the surgeon for majority of patients, with no difference between the groups (Table 2). There were no significant differences in patient or surgeon satisfaction between the groups (Table 2), although patient satisfaction was not measured in 7 patients because of cognitive function impairment. In the HUSA group, the mean±SD duration of motor and sensory blockade in the operated side were 100±13 min and 135±24 min, respectively. The duration of surgery exceeded 2 hours in two patients from each group, with one patient in the HUSA group requiring additional analgesia by remifentanil. In the HUSA group, 2 patients presented intraoperative agitation requiring propofol administration (40 mg) and 1 patient presented an intraoperative pruritus. In the GA group, the mean±SD infusion rate of remifentanil was 0.13±0.07 μg kg−1 min−1. During surgery, BIS value was maintained between 40 and 60 with low end-tidal desflurane concentrations at 0.5–0.7 MAC, adapted to the elderly population (23, 24). One urinary tract infection occurred at day 5 in the HUSA group. Cardiovascular complications are presented in Table 2, which show no difference between the groups. No mortality was observed at day 30 in any patient.
Discussion
Our study is the first to demonstrate that haemodynamic stability, defined by numerous criteria of evaluation, particularly the consumption of vasopressors and the occurrence of severe hypotension episodes, is better with HUSA than with GA during hip fracture surgery in the elderly.
These results contradict the results of the meta-analysis conducted by Urwin et al., who showed more frequent intraoperative hypotension with SA (34%) compared with GA (26%) for hip fracture surgery (Peto OR=1.5; 95% CI=1.1–2.0) (3). However, the anaesthetic agents used for SA and GA and the criteria defining hypotension were not clearly reported in this meta-analysis. Bijker et al. (26) established a literature review and brought to light a wide disparity of definitions of intraoperative arterial hypotension. The authors reported that, depending on the used definition, the incidence of intraoperative arterial hypotension varies from 5% to 99%. Besides, 41% of the patients experienced at least one episode of arterial hypotension <80 mmHg and 93% experienced at least one arterial episode of hypotension of >20% from baseline.
More recently, a pilot study was performed in 20 patients assessing the haemodynamic changes associated with SA and GA for hip fracture surgery in a severe ASA III elderly population using invasive monitoring (27). This study has shown that severe hypotension was common after both GA and SA for hip fracture surgery in the elderly population; it also showed that SA provides a more stable haemodynamic profile with less intervention required to maintain mean arterial pressure close to baseline levels. Although the anaesthetic protocol was different compared with that of the current study (GA combining propofol and remifentanil and SA combining levobupivacaine and sufentanil), the results were consistent with those of the current study.
Intraoperative arterial hypotension is one of the main determiners of the occurrence of myocardial infarction in the postoperative period when anaemia is concerned (28). The definition of intraoperative arterial hypotension is very variable (26). Considering the incidence of the hypotensive events over 20%, 30% and 40% from baseline with GA, the results of our study are 100%, 100% and 71%, respectively. These results are superior to those found in the review by Bijker et al. (26) (93%, 77% and 52%), which can be attributed to the older population included in the current study. In a study concerning hip fracture surgery in patients aged over 65 years using sevoflurane GA, Casati et al. (14) observed an 80% incidence of arterial hypotension, which was superior to 20% from baseline.
Concerning spinal anaesthesia, 89% of our study patients presented hypotension superior to 20%. This result contradicts the findings of Minville et al. (10), which bring to light an incidence of only 31% with a 5 mg dose of bupivacaine. The very low incidences found in this study can be attributed to the fact that the administration of the local anaesthetic was titrated through a spinal catheter and that the preoperative volume expansion of the patients was different (crystalloid: 8 mL kg−1). In the same study, 68% of the patients undergoing unilateral SA with 7.5 mg of isobaric bupivacaine presented a hypotensive episode over 20% from baseline; however, the blood pressure measures were much more spaced out. With a protocol of identical anaesthesia for the same type of surgery, Casati et al. (14) found an incidence of 46% of hypotensive episodes superior to 20%. Even there, blood pressure monitoring was different. The closed monitoring in our study is one possible explanation for these differences. In another study by Ben-David et al. (11), spinal anaesthesia with 4 mg isobaric bupivacaine associated with 20 μg fentanyl was compared with spinal anaesthesia with 10 mg isobaric bupivacaine; the incidence of hypotension superior to 25% of the MBP was 10% and 90%, respectively. Because the primary outcome (MBP) was different from that of our study, it was not possible to compare these percentages with those of our study. Nevertheless, SA using local anaesthetic at very low doses may provide better haemodynamic stability.
The ephedrine dose used to maintain haemodynamic parameters in predefined values in our study was chosen as a surrogate marker of haemodynamic stability. The median [IQR] consumption of ephedrine with HUSA was 6 [0–17] mg vs. 36 [21–57] mg with GA (p<0.001). Minville et al. (10) found a mean±SD consumption of ephedrine of 11±2 mg in a case of unilateral SA with 7.5 mg isobaric bupivacaine. Ben-David et al. (11) found a consumption similar to that reported in our study (5 mg) and much lower than that used during conventional SA (35 mg). Four patients in our study required a surgery exceeding two hours. In that case, continuous spinal anaesthesia may be used; however, this technique is contraindicated in the case of treatment with antiplatelet drugs.
Low doses (7.5 mg) and even very low doses (4 mg) of bupivacaine, in association with an opiate are sufficient for femoral neck fracture surgery in the elderly (14, 15). Using doses superior or equal to 10 mg of bupivacaine entails haemodynamic instability and is no more recommended (29). Opiates such as sufentanil, added to local anaesthetics, prolong the duration of the sensory block without prolonging the duration of the motor block (30). Sufentanil doses usually recommended in this indication range from 2.5 to 10 μg (30). Besides, the spinal addition of opiates allows the reduction of local anaesthetic doses and, consequently, better haemodynamic stability (31, 32).
According to Minville et al. (10), 5 mg bupivacaine without opiate would be sufficient for hip fracture surgical repair in elderly patients. It is, nevertheless, necessary to specify that this dose was administered through a spinal catheter, with the possibility of intraoperative supplemental doses in the case of insufficient analgesia. Considering these observations, we opted for a very low dose of bupivacaine (5 mg) associated with 5 μg sufentanil. This association seemed reasonable and safe for this type of surgery.
This study presents several limitations because it compares two radically different anaesthetic techniques. It was not thus possible to perform a double-blind study. Besides, our choice of the anaesthesia protocol, particularly the GA protocol, is not the only choice for an old and fragile population. The clinical equipoise between regional and GA is unlikely, potentially introducing recording and reporting bias (33). We chose etomidate and desflurane because these agents allow rapid anaesthetic induction, excellent intraoperative control of anaesthesia and rapid emergence and recovery from anaesthesia in geriatric patients (34). However, hypotension following induction of GA using etomidate is very frequent, with a reported mean decrease in mean arterial pressure of 35%, which is similar to that found in the current study (35).
Intraoperative BIS monitoring was systematically used to optimise the administration of hypnotic drugs in these frail elderly patients, although no evidence-based data are yet available to support it (22). Indeed, there is no evidence that BIS monitoring, in particular avoidance of BIS values <45, decreases intermediate-term mortality in patients undergoing non-cardiac surgery (36). We also used remifentanil as an opioid, considering its handiness and pharmacokinetic reversibility (37). Its administration was made in weight-adjusted infusion and not in target-controlled infusion (TCI) because of its feasibility in the department (availability of the material). It has been shown that using TCI remifentanil may improve the haemodynamics and decrease remifentanil requirement in vascular patients undergoing carotid surgery (38). However, the benefit of TCI, compared with manually controlled infusion of remifentanil, remains to be determined in elderly patients undergoing hip fracture surgery.
Concerning HUSA, despite it being clearly demonstrated that obtaining strict unilateral spinal anaesthesia is more frequent when using hyperbaric solutions, we used a hypobaric solution to improve patient comfort (39, 40). Side decubitus with the broken limb in the superior position reduces the patient’s pain and discomfort during spinal anaesthesia. However, to ensure that spinal anaesthesia was unilateral, the anaesthetic solution was injected through a 22/25 gauge Quincke point needle without aspiration of the spinal fluid to avoid paddling, which is responsible for a bilateral extension of the block (21, 31). Another use of a hypobaric solution is it allows slower installation of the sympathetic block as compared with a hyperbaric solution (32, 41).
Although our study showed better intraoperative haemodynamics using HUSA, we did not observe a lower rate of postoperative complications or 30-day mortality in comparison with GA. This may be because of the trial design, wherein 30-day mortality was not the primary outcome. The problems in determining which primary and secondary outcomes should be measured in studies concerning the type of anaesthesia for hip fracture surgery have been recently reported (33). Indeed, although having 30-day mortality as the primary outcome would be interesting, it would require a very large sample size to detect any significant difference between HUSA and GA (33).
Hip fracture surgery in the elderly is frequent in clinical practise and concerns a growing population with numerous comorbidities. It is a major global public health issue, with 1.6 million patients suffering from hip fracture every year along with a 25% increase every decade (22). The optimisation of intraoperative haemodynamics is a constant concern for the anaesthetist. Intraoperative hypotension, the main complication of the anaesthesia, is frequent in this fragile population. The debate concerning the type of anaesthesia (regional or general) is not closed. Our results show better haemodynamic stability as well as reduced consumption of vasopressors in patients undergoing HUSA. Furthermore, the operating conditions and the satisfaction of the surgeon and patients in the HUSA group are comparable with those of the GA group.
Conclusion
The present study shows that HUSA is a safe and effective technique for the care of hip fracture in the elderly. In our study population, HUSA with bupivacaine and sufentanil provided better haemodynamic stability than GA with etomidate, desflurane, remifentanil and reduced consumption of vasopressors with similar operating conditions. Further studies with different anaesthetic protocols are however required to confirm our results.
Acknowledgements
The authors wish to thank Dr Liana Caruso, Dr Robert Deléat-Besson, Dr Bernard Rousselet and Dr Bruno Thouverez for participating in this study.
Footnotes
This study was previously presented in part in French and reproduced with the authorization of the publisher (Webanesthésie 2009;3:09011).
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Comité de Protection des Personnes Sud-Est IV, reference number A07-139.
Informed Consent: Written informed consent was obtained from all patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – P.M., B.V., M.H., E.B.; Design – P.M., B.V., E.B.; Supervision – B.A.; Data Collection and/or Processing – P.M., L.B., B.V., M.H., E.B.; Analysis and/or Interpretation – L.B., B.A., E.B.; Literature Search – P.M., E.B.; Writing Manuscript – P.M., E.B.; Critical Review – B.V., M.H., B.A., L.B.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Sutcliffe AJ, Parker M. Mortality after spinal and general anaesthesia for surgical fixation of hip fractures. Anaesthesia. 1994;49:237–40. doi: 10.1111/j.1365-2044.1994.tb03430.x. [DOI] [PubMed] [Google Scholar]
- 2.O’Hara DA, Duff A, Berlin JA, Poses RM, Lawrence VA, Huber EC, et al. The effect of anesthetic technique on postoperative outcomes in hip fracture repair. Anesthesiology. 2000;92:947–57. doi: 10.1097/00000542-200004000-00011. https://doi.org/10.1097/00000542-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 3.Urwin SC, Parker MJ, Griffiths R. General versus regional anaesthesia for hip fracture surgery: a meta-analysis of randomized trials. Br J Anaesth. 2000;84:450–5. doi: 10.1093/oxfordjournals.bja.a013468. https://doi.org/10.1093/oxfordjournals.bja.a013468. [DOI] [PubMed] [Google Scholar]
- 4.Rodgers A, Walker N, Schug S, McKee A, Kehlet H, van Zundert A, et al. Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: results from overview of randomised trials. BMJ. 2000;321:1493. doi: 10.1136/bmj.321.7275.1493. https://doi.org/10.1136/bmj.321.7275.1493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004:CD000521. doi: 10.1002/14651858.CD000521.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Gulur P, Nishimori M, Ballantyne JC. Regional anaesthesia versus general anaesthesia, morbidity and mortality. Best Pract Res Clin Anaesthesiol. 2006;20:249–63. doi: 10.1016/j.bpa.2005.10.002. https://doi.org/10.1016/j.bpa.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117:72–92. doi: 10.1097/ALN.0b013e3182545e7c. https://doi.org/10.1097/ALN.0b013e3182545e7c. [DOI] [PubMed] [Google Scholar]
- 8.Patorno E, Neuman MD, Schneeweiss S, Mogun H, Bateman BT. Comparative safety of anesthetic type for hip fracture surgery in adults: retrospective cohort study. BMJ. 2014;348:g4022. doi: 10.1136/bmj.g4022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neuman MD, Rosenbaum PR, Ludwig JM, Zubizarreta JR, Silber JH. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA. 2014;311:2508–17. doi: 10.1001/jama.2014.6499. https://doi.org/10.1001/jama.2014.6499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minville V, Fourcade O, Grousset D, Chassery C, Nguyen L, Asehnoune K, et al. Spinal anesthesia using single injection small-dose bupivacaine versus continuous catheter injection techniques for surgical repair of hip fracture in elderly patients. Anesth Analg. 2006;102:1559–63. doi: 10.1213/01.ane.0000218421.18723.cf. https://doi.org/10.1213/01.ane.0000218421.18723.cf. [DOI] [PubMed] [Google Scholar]
- 11.Ben-David B, Frankel R, Arzumonov T, Marchevsky Y, Volpin G. Minidose bupivacaine-fentanyl spinal anesthesia for surgical repair of hip fracture in the aged. Anesthesiology. 2000;92:6–10. doi: 10.1097/00000542-200001000-00007. https://doi.org/10.1097/00000542-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 12.Olofsson C, Nygards EB, Bjersten AB, Hessling A. Low-dose bupivacaine with sufentanil prevents hypotension after spinal anesthesia for hip repair in elderly patients. Acta Anaesthesiol Scand. 2004;48:1240–4. doi: 10.1111/j.1399-6576.2004.00504.x. https://doi.org/10.1111/j.1399-6576.2004.00504.x. [DOI] [PubMed] [Google Scholar]
- 13.Kelly JD, McCoy D, Rosenbaum SH, Brull SJ. Haemodynamic changes induced by hyperbaric bupivacaine during lateral decubitus or supine spinal anaesthesia. Eur J Anaesthesiol. 2005;22:717–22. doi: 10.1017/s0265021505001183. https://doi.org/10.1017/S0265021505001183. [DOI] [PubMed] [Google Scholar]
- 14.Casati A, Aldegheri G, Vinciguerra E, Marsan A, Fraschini G, Torri G. Randomized comparison between sevoflurane anaesthesia and unilateral spinal anaesthesia in elderly patients undergoing orthopaedic surgery. Eur J Anaesthesiol. 2003;20:640–6. doi: 10.1017/s0265021503001030. https://doi.org/10.1017/S0265021503001030. [DOI] [PubMed] [Google Scholar]
- 15.Khatouf M, Loughnane F, Boini S, Heck M, Meuret P, Macalou D, et al. Rachianesthésie hypobare unilatérale chez le sujet âgé pour la chirurgie traumatique de la hanche: étude pilote. Ann Fr Anesth Réanim. 2005;24:249–54. doi: 10.1016/j.annfar.2004.12.027. https://doi.org/10.1016/j.annfar.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Schulz KF, Altman D, Group C. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA. 2001;285:1987–91. doi: 10.1001/jama.285.15.1987. https://doi.org/10.1016/j.annfar.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. https://doi.org/10.1001/jama.285.15.1992. [DOI] [PubMed] [Google Scholar]
- 18.Buggy D, Higgins P, Moran C, O’Brien D, O’Donovan F, McCarroll M. Prevention of spinal anesthesia-induced hypotension in the elderly: comparison between preanesthetic administration of crystalloids, colloids, and no prehydration. Anesth Analg. 1997;84:106–10. doi: 10.1097/00000539-199701000-00020. https://doi.org/10.1213/00000539-199701000-00020. [DOI] [PubMed] [Google Scholar]
- 19.Marhofer P, Faryniak B, Oismuller C, Koinig H, Kapral S, Mayer N. Cardiovascular effects of 6% hetastarch and lactated Ringer’s solution during spinal anesthesia. Reg Anesth Pain Med. 1999;24:399–404. doi: 10.1016/s1098-7339(99)90004-4. https://doi.org/10.1016/S1098-7339(99)90004-4. [DOI] [PubMed] [Google Scholar]
- 20.Sharma SK, Gajraj NM, Sidawi JE. Prevention of hypotension during spinal anesthesia: a comparison of intravascular administration of hetastarch versus lactated Ringer’s solution. Anesth Analg. 1997;84:111–4. doi: 10.1097/00000539-199701000-00021. https://doi.org/10.1213/00000539-199701000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Anderson L, Walker J, Brydon C, Serpell MG. Rate of injection through Whitacre needles affects distribution of spinal anaesthesia. Br J Anaesth. 2001;86:245–8. doi: 10.1093/bja/86.2.245. https://doi.org/10.1093/bja/86.2.245. [DOI] [PubMed] [Google Scholar]
- 22.Boddaert J, Raux M, Khiami F, Riou B. Perioperative management of elderly patients with hip fracture. Anesthesiology. 2014;121:1336–41. doi: 10.1097/ALN.0000000000000478. https://doi.org/10.1097/ALN.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 23.Matsuura T, Oda Y, Tanaka K, Mori T, Nishikawa K, Asada A. Advance of age decreases the minimum alveolar concentrations of isoflurane and sevoflurane for maintaining bispectral index below 50. Br J Anaesth. 2009;102:331–5. doi: 10.1093/bja/aen382. https://doi.org/10.1093/bja/aen382. [DOI] [PubMed] [Google Scholar]
- 24.Gold MI, Abello D, Herrington C. Minimum alveolar concentration of desflurane in patients older than 65 yr. Anesthesiology. 1993;79:710–4. doi: 10.1097/00000542-199310000-00012. https://doi.org/10.1097/00000542-199310000-00012. [DOI] [PubMed] [Google Scholar]
- 25.Morrison RS, Siu AL. A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage. 2000;19:240–8. doi: 10.1016/s0885-3924(00)00113-5. https://doi.org/10.1016/S0885-3924(00)00113-5. [DOI] [PubMed] [Google Scholar]
- 26.Bijker JB, van Klei WA, Kappen TH, van Wolfswinkel L, Moons KG, Kalkman CJ. Incidence of intraoperative hypotension as a function of the chosen definition: literature definitions applied to a retrospective cohort using automated data collection. Anesthesiology. 2007;107:213–20. doi: 10.1097/01.anes.0000270724.40897.8e. https://doi.org/10.1097/01.anes.0000270724.40897.8e. [DOI] [PubMed] [Google Scholar]
- 27.Messina A, Frassanito L, Colombo D, Vergari A, Draisci G, Della Corte F, et al. Hemodynamic changes associated with spinal and general anesthesia for hip fracture surgery in severe ASA III elderly population: a pilot trial. Minerva Anestesiol. 2013;79:1021–9. [PubMed] [Google Scholar]
- 28.Lienhart A, Auroy Y, Pequignot F, Benhamou D, Warszawski J, Bovet M, et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006;105:1087–97. doi: 10.1097/00000542-200612000-00008. https://doi.org/10.1097/00000542-200612000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Favarel-Garrigues JF, Sztark F, Petitjean ME, Thicoipe M, Lassie P, Dabadie P. Hemodynamic effects of spinal anesthesia in the elderly: single dose versus titration through a catheter. Anesth Analg. 1996;82:312–6. doi: 10.1097/00000539-199602000-00017. https://doi.org/10.1213/00000539-199602000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Milligan KR. Recent advances in local anaesthetics for spinal anaesthesia. Eur J Anaesthesiol. 2004;21:837–47. doi: 10.1017/s0265021504000158. https://doi.org/10.1097/00003643-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Casati A, Fanelli G, Cappelleri G, Aldegheri G, Leoni A, Casaletti E, et al. Effects of spinal needle type on lateral distribution of 0.5% hyperbaric bupivacaine. Anesth Analg. 1998;87:355–9. doi: 10.1097/00000539-199808000-00022. https://doi.org/10.1097/00000539-199808000-00022. [DOI] [PubMed] [Google Scholar]
- 32.Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JA. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 2005;94:107–11. doi: 10.1093/bja/aei008. https://doi.org/10.1093/bja/aei008. [DOI] [PubMed] [Google Scholar]
- 33.White SM, Griffiths R, Moppett I. Type of anaesthesia for hip fracture surgery - the problems of trial design. Anaesthesia. 2012;67:574–8. doi: 10.1111/j.1365-2044.2012.07120.x. https://doi.org/10.1111/j.1365-2044.2012.07120.x. [DOI] [PubMed] [Google Scholar]
- 34.Passot S, Servin F, Pascal J, Charret F, Auboyer C, Molliex S. A comparison of target- and manually controlled infusion propofol and etomidate/desflurane anesthesia in elderly patients undergoing hip fracture surgery. Anesth Analg. 2005;100:1338–42. doi: 10.1213/01.ANE.0000149542.04833.55. https://doi.org/10.1213/01.ANE.0000149542.04833.55. [DOI] [PubMed] [Google Scholar]
- 35.Larsen R, Rathgeber J, Bagdahn A, Lange H, Rieke H. Effects of propofol on cardiovascular dynamics and coronary blood flow in geriatric patients. A comparison with etomidate. Anaesthesia. 1988;43(Suppl):25–31. doi: 10.1111/j.1365-2044.1988.tb09064.x. [DOI] [PubMed] [Google Scholar]
- 36.Kertai MD, Palanca BJ, Pal N, Burnside BA, Zhang L, Sadiq F, et al. Bispectral index monitoring, duration of bispectral index below 45, patient risk factors, and intermediate-term mortality after noncardiac surgery in the B-Unaware Trial. Anesthesiology. 2011;114:545–56. doi: 10.1097/ALN.0b013e31820c2b57. https://doi.org/10.1097/ALN.0b013e31820c2b57. [DOI] [PubMed] [Google Scholar]
- 37.Komatsu R, Turan AM, Orhan-Sungur M, McGuire J, Radke OC, Apfel CC. Remifentanil for general anaesthesia: a systematic review. Anaesthesia. 2007;62:1266–80. doi: 10.1111/j.1365-2044.2007.05221.x. https://doi.org/10.1111/j.1365-2044.2007.05221.x. [DOI] [PubMed] [Google Scholar]
- 38.De Castro V, Godet G, Mencia G, Raux M, Coriat P. Target-controlled infusion for remifentanil in vascular patients improves hemodynamics and decreases remifentanil requirement. Anesth Analg. 2003;96:33–8. doi: 10.1097/00000539-200301000-00008. https://doi.org/10.1213/00000539-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Kaya M, Oguz S, Aslan K, Kadiogullari N. A low-dose bupivacaine: a comparison of hyperbaric and hypobaric solutions for unilateral spinal anesthesia. Reg Anesth Pain Med. 2004;29:17–22. doi: 10.1016/j.rapm.2003.09.006. https://doi.org/10.1097/00115550-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 40.Kuusniemi KS, Pihlajamaki KK, Pitkanen MT. A low dose of plain or hyperbaric bupivacaine for unilateral spinal anesthesia. Reg Anesth Pain Med. 2000;25:605–10. doi: 10.1053/rapm.2000.8500. https://doi.org/10.1053/rapm.2000.8500. [DOI] [PubMed] [Google Scholar]
- 41.Kallio H, Snall EV, Tuomas CA, Rosenberg PH. Comparison of hyperbaric and plain ropivacaine 15 mg in spinal anaesthesia for lower limb surgery. Br J Anaesth. 2004;93:664–9. doi: 10.1093/bja/aeh257. https://doi.org/10.1093/bja/aeh257. [DOI] [PubMed] [Google Scholar]


