Abstract
Objective
To investigate whether associations of hearing impairment (HI) with functional outcomes in older adults differ when using self-report versus pure-tone-audiometry.
Methods
We examined 1669 participants ≥70 years in National Health and Examination Survey from 2005–2006 and 2009–2010 whose hearing was assessed by self-report and pure-tone-audiometry. We explored functional outcomes associated with audiometric HI (low physical activity, poor physical functioning, and hospitalization).
Results
In adjusted models, we found significant associations of audiometric HI with both subjective and objective outcomes, (e.g., dichotomous HI with self-reported difficulty in activities of daily living (ADLs), OR=1.47[95%CI:1.05–2.06] and low accelerometer-measured physical activity, OR=2.19[95%CI:1.11–4.34]). In contrast, self-reported HI was only associated with subjective outcomes and not with objective outcomes (e.g., dichotomous HI with difficulty in ADLs, OR=1.63 [95%CI:1.12–2.38] and low accelerometer-measured physical activity OR=0.95 [95%CI:0.66–1.35]).
Discussion
Results using self-reported hearing should not be considered representative of results using audiometry and may provide distinct aspects of HI in older adults.
Introduction
Hearing impairment (HI) is highly prevalent in older adults (F. R. Lin, 2012; F. R. Lin, Thorpe, Gordon-Salant, & Ferrucci, 2011), and is independently associated with social isolation, depression, poor quality of life, and accelerated decline in cognitive functioning.(Dalton et al., 2003; Li et al., 2014; F. R. Lin, Ferrucci, et al., 2011; Weinstein & Ventry, 1982) There has been an increasing understanding that HI may be associated with impaired physical functioning in older adults (Chen, Genther, Betz, & Lin, 2014; Genther, Frick, Chen, Betz, & Lin, 2013; Gispen, Chen, Genther, & Lin, 2014; F. R. Lin, Metter, et al., 2011; F. R. Lin et al., 2013). Previous studies have explored several mechanistic pathways that could potentially mediate the association between HI and decline in physical functioning, which include increased cognitive load and shared attention in individuals with HI from constantly processing degraded signals, social isolation and loneliness from communicative impairment, and reduced awareness of auditory environment (Chen et al., 2014; Coppin et al., 2006; Perissinotto, Stijacic Cenzer, & Covinsky, 2012; Tun, McCoy, & Wingfield, 2009). However, epidemiologic studies investigating the association of HI with functional outcomes in older adults have been inconsistent at times with some studies demonstrating positive associations (Bess, Lichtenstein, Logan, Burger, & Nelson, 1989; Chia et al., 2007; Dargent-Molina, Hays, & Breart, 1996; Gopinath et al., 2012; Keller, Morton, Thomas, & Potter, 1999; Lopez-Torres Hidalgo et al., 2009; Reuben, Mui, Damesyn, Moore, & Greendale, 1999; Strawbridge, Wallhagen, Shema, & Kaplan, 2000; Viljanen et al., 2009) and others demonstrating no association (Laforge, 1992; M. Y. Lin et al., 2004; Rudberg, Furner, Dunn, & Cassel, 1993). These inconsistencies may be explained in part by differences in how HI has been measured across studies. While some studies have used audiometric measures of hearing (Bess et al., 1989; Chia et al., 2007; Gopinath et al., 2012; M. Y. Lin et al., 2004; Viljanen et al., 2009), others have relied on self-reported measures of hearing (Dargent-Molina et al., 1996; Laforge, 1992; Lopez-Torres Hidalgo et al., 2009; Reuben et al., 1999; Rudberg et al., 1993; Strawbridge et al., 2000). However, the agreement between self-reported assessments of hearing and gold-standard audiometric assessments varies substantively by demographic factors such as age, sex, race, and education. For example, older adults tend to underestimate their HI, and the agreement rates were relatively lower among older women, blacks, and Hispanics compared to their respective younger age groups. (Kamil, Genther, & Lin, 2015; Kiely, Gopinath, Mitchell, Browning, & Anstey, 2012; Sindhusake et al., 2001; Valete-Rosalino & Rozenfeld, 2005). The agreement rate between two different measures of hearing are also likely affected by other environmental and personal factors (e.g., personality, lifestyle, interactions with family members, etc). However, whether these factors are substantial enough to result in different levels of associations in epidemiologic studies with functional outcomes in older adults is unknown. The aim of this study is to investigate whether associations of HI with functional outcomes differ when using self-reported versus audiometric measures of hearing in a nationally representative cohort of older adults in the U.S.
Methods
Study Population
Our analytic cohort was composed of 1669 individuals participating in the National Health and Nutrition Examination Survey (NHANES) who were 70 years of age or older and who had complete data on both self-reported hearing and audiometric testing. NHANES is an ongoing program of studies designed to assess the health, function, and nutritional status of the non-institutionalized, civilian U.S. population. Each of the sequential, cross-sectional study cycles in NHANES uses a stratified, multistage probability sampling design to survey a sample of the U.S. population with selective oversampling of low-income individuals, racial minorities, and older adults. Sampling weights allow for analyses that account for the complex survey design and yield results that are generalizable to the U.S. population. Hearing was measured using self-reports in 1994 adults aged 70 year and older in two NHANES cycles, 2005–2006 and 2009–2010, and of these, 1669 (84%) had hearing measured using pure-tone audiometry. Those without audiometric measurement of hearing were more likely to be older, female, non-White, less educated, have lower income, and never smokers. Their characteristics did not differ across history of comorbidities including hypertension, diabetes, stroke, cardiovascular diseases or hearing aid use.
Audiometric Assessment
Audiometric assessment was performed by a trained examiner according to established NHANES protocols (McClay, Booth, Parry, Johnson, & Roland, 2008). A trained examiner determined the air conduction hearing threshold for each ear without hearing aid in a sound-isolated room in the mobile examination center. Testing was conducted according to a modified Hughson Westlake procedure using the automated testing mode of the audiometer (Model AD 226, Interacoustics, Assens, Denmark). Quality assurance and control were established through daily calibration of equipment and monitoring of ambient noise levels using a sound level meter. Thresholds were measured twice at 1kHz in each ear as an additional quality measure, and audiometry was repeated if there was a greater than 10 dB discrepancy between the threshold measurements. HI was defined as a speech-frequency pure tone average of thresholds at 0.5, 1, 2, and 4 kHz in the better-hearing ear as defined by the World Health Organization (Sennaroglu & Saatci, 2002). Severity of HI was categorized into ordinal and binary variables in our analyses based on the American Speech-Language Hearing Association guidelines (Clark, 1981) in order to allow for a comparison to the self-reported hearing (analyses using an ordinal indicator of audiometric hearing: “Normal hearing” ≤ 25 dB, “Mild HI” = 25.0–39.9 dB, and “Moderate-or-greater HI” ≥ 40.0 dB—individuals with moderate or greater HI were collapsed together to account for the small number of individuals with severe-to-profound HI, n=104; analyses using a binary indicator of audiometric hearing: “Normal hearing” < 25dB and “Any HI” ≥ 25dB).
Self-reported Hearing Assessment
Self-reported hearing was assessed by the interviewer using the Computer-Assisted Personal Interviewing (CAPI) system. Respondents were asked, “Which statement best describes your hearing (without a hearing aid)? Would you say your hearing is excellent, good, that you have a little trouble, moderate trouble, a lot of trouble, or are you deaf?” A priori, self-reported measure of hearing was categorized into ordinal variables comparable to the severity categories of audiometric hearing (“Excellent or good hearing”, “A little to moderate trouble hearing”, and “Moderate-or-greater trouble hearing”). Self-reported hearing was categorized into binary variables for additional comparison to the audiometric hearing, which were defined using relatively ubiquitous cutoffs for both audiometric and self-reported hearing (“Excellent or good hearing” and “Any trouble hearing”).
Objective Outcomes: Physical Activity and Hospitalization
As defined previously (Bamiou, Worth, Phelps, Sirimanna, & Rajput, 2001), physical activity was measured using accelerometers in the 2005–06 NHANES cycle (AM-7164, Actigraph, Fort Walton Beach, FL). Participants who were physically able to walk were asked to wear accelerometers for seven days (Gispen et al., 2014). Moderate activity was defined according to previously established thresholds of 2,020 intensity counts or more per minute, and vigorous activity was defined as 5,999 intensity counts or more per minute (Metzger et al., 2008; Troiano et al., 2008; Tucker, Welk, & Beyler, 2011). A minute of vigorous activity was counted as 2 minutes of moderate physical activity (MPA), and the final variable of physical activity was calculated by counting weekly minutes of MPA per participant. Accelerometer-measured physical activity was collapsed into three levels based on the Physical Activity Guidelines for Americans (“U.S. Department of Health and Human Services. Physical Activity Guidelines for Americnas: Appendix 1. Translating Scientific Evidnece About Total Amount and Intensity of Physical Activity Into Guidelines.,”). (“inactive”: 0 min/wk of MPA; “active”: < 150 min/wk of MPA; and “sufficiently active”: ≥ 150 min/wk of MPA).
Prior hospitalization was determined from interviews. Respondents were asked whether they had stayed in any hospital overnight or longer during the past 12 months (“yes” or “no”). Respondents were further questioned how many different times they had stayed in hospital during the past 12 months. The number of hospitalizations was categorized into “0”, “1”, and “>1”.
Subjective Outcomes: Self-reported Healthy Days and Difficulties in Physical Functioning
Subjective outcomes included measures of self-reported healthy days and difficulties in physical functioning that were previously found to be associated with audiometry-measured HI and that were based on qualitative self-ratings by participants (Chen et al., 2014; Genther et al., 2013). Self-reported healthy days were assessed by an interviewer using the CAPI system. Respondents were asked to specify the number of days in the last 30 days during which their physical health (physical illness and injury) was poor. As in a previous report, the final variable was analyzed as a binary variable where poor physical health was defined as reporting greater than 10 days of poor physical health out of the prior 30 days (Genther et al., 2013). Similarly, respondents were asked to specify the number of days during which their mental health (stress, depression, and problems with emotions) was poor. Poor mental health was defined as reporting greater than 10 days of poor mental health out of the prior 30 days (Genther et al., 2013).
Self-reported difficulties in physical functioning were assessed by an interviewer using the CAPI system. Respondents were asked a series of questions regarding any difficulties they had performing physical tasks. The physical tasks were categorized into five domains including Activities in Daily Living (ADLs) (i.e. difficulties getting in and out of bed, eating, and dressing), Instrumental Activities in Daily Living (IADLs) (i.e. difficulties managing money, performing house chores, and preparing meals), leisure and social activities (i.e. difficulties going to the movies, attending social events, and performing leisure activity at home), lower-extremity mobility (i.e. walking, stooping/kneeling/crouching, standing up), and general physical activities (lifting, reaching up, grasping/holding, standing/sitting for long periods) (Chen et al., 2014; Plantinga et al., 2011). Difficulty in a physical domain (“yes” or “no”) was defined as reporting some or more difficulty in at least one of the physical task questions within a domain. Respondents were also asked about whether they had general functional limitations (“yes” or “no”) in walking and limitations due to confusion and memory.
Other Study Variables
Data on demographics and medical history were obtained from interviews. Age was truncated at 80 in the NHANES database to protect confidentiality; therefore, age was treated as a categorical variable and was collapsed into three categories (70 to 74, 74 to 79, and 80 and older) instead of being treated as a continuous variable. Sex was included as a binary variable, and self-reported race and ethnicity were grouped as Hispanic (Mexican American or other Hispanic), white (non-Hispanic white), black (non-Hispanic black), or other race. Education was collapsed into 3 categories (<12th grade, high school graduate, or some college or more). Household income was collapsed into 5 categories (<$20,000, $20,000–44,000, $45,000–74000, ≥$75,000, and refused/do not know). Medical history variables included hypertension (having been diagnosed by a physician on at least two visits with high blood pressure or taking antihypertensive medication), cardiovascular disease (congestive heart failure, coronary artery disease, angina pectoris, or myocardial infarction), diabetes mellitus, stroke, and smoking status (current, former, never).
Statistical Methodology
The complex sampling design was accounted for by using sample weights according to the National Center for Health Statistics guidelines in all analyses except for Table 1. Table 1 provides the descriptive statistics using self-reported and audiometric measures of hearing as ordinal variables to characterize the study cohort, and therefore, unweighted numbers were reported. The Pearson chi-square test was used to compare baseline characteristics of the study participants.
Table 1.
Demographic and Health-related Characteristics of Participants Aged 70 and Older with Audiometric Testing and Self-report, NHANES, 2005–2006 and 2009–2010, N=1669
| Characteristics, n. (%) | Assessment of Hearing Impairment Using Speech-Frequency Pure-Tone Audiometry
|
Assessment of Hearing Impairment Using Self-report
|
||||||
|---|---|---|---|---|---|---|---|---|
| No Hearing Impairment n=529 |
Mild Hearing Impairment n=590 |
Moderate or Greater Hearing Impairment n=550 |
p-value | Excellent or Good Hearing n=828 |
A Little Trouble of Hearing n=433 |
Moderate or Greater Trouble Hearing n=408 |
p-value | |
| Age | ||||||||
| 70–74 | 289 (54.6) | 212 (35.9) | 107 (19.5) | <0.001 | 326 (39.4) | 168 (38.8) | 114 (27.9) | <0.001 |
| 75–79 | 138 (26.1) | 156 (26.4) | 127 (23.1) | 222 (26.8) | 99 (22.9) | 100 (24.5) | ||
| ≥ 80 | 102 (19.3) | 222 (37.6) | 316 (57.5) | 280 (33.8) | 166 (38.3) | 194 (47.6) | ||
| Femalea | 312 (59.0) | 303 (51.4) | 206 (37.5) | <0.001 | 473 (57.1) | 204 (47.1) | 144 (35.3) | <0.001 |
| Race | ||||||||
| White | 327 (61.8) | 427 (72.4) | 432 (78.6) | <0.001 | 548 (66.2) | 310 (71.6) | 328 (80.4) | <0.001 |
| Black | 117 (22.1) | 77 (13.1) | 40 (7.3) | 143 (17.3) | 59 (13.6) | 32 (7.8) | ||
| Hispanic | 68 (12.9) | 69 (11.7) | 62 (11.3) | 107 (12.9) | 50 (11.6) | 42 (10.3) | ||
| other | 17 (3.2) | 17 (2.9) | 16 (3.0) | 30 (3.6) | 14 (3.2) | 6 (1.5) | ||
| Education | ||||||||
| < 12th grade | 161 (30.5) | 202 (34.2) | 226 (41.2) | <0.001 | 270 (32.7) | 171 (39.5) | 148 (36.4) | 0.16 |
| High school graduate | 128 (24.2) | 175 (29.7) | 125 (22.8) | 222 (26.9) | 108 (24.9) | 98 (24.1) | ||
| Some college or more | 239 (45.3) | 213 (36.1) | 197 (36.0) | 334 (40.4) | 154 (35.6) | 161 (39.6) | ||
| Income, $ | ||||||||
| < 20,000 | 129 (24.4) | 181 (30.9) | 172 (31.3) | 0.02 | 239 (28.9) | 130 (30.2) | 113 (27.8) | 0.44 |
| 20,000–44,999 | 176 (33.3) | 201 (34.3) | 205 (37.3) | 269 (32.6) | 154 (35.7) | 159 (39.1) | ||
| 45,000–74,999 | 114 (21.6) | 103 (17.6) | 79 (14.4) | 163 (19.7) | 68 (15.8) | 65 (16.0) | ||
| ≥ 75,000 | 71 (13.4) | 65 (11.1) | 54 (9.8) | 99 (12.0) | 48 (11.1) | 43 (10.6) | ||
| Refused or do not know | 39 (7.4) | 36 (6.1) | 39 (7.1) | 56 (6.8) | 31 (7.2) | 27 (6.6) | ||
| Hypertensiona | 353 (66.9) | 373 (63.5) | 330 (60.1) | 0.07 | 535 (64.8) | 273 (63.3) | 248 (60.9) | 0.42 |
| Cardiovascular diseasea,b | 103 (19.5) | 153 (26.0) | 154 (28.0) | 0.003 | 164 (19.8) | 118 (27.3) | 128 (31.4) | <0.001 |
| Strokea | 38 (7.2) | 62 (10.5) | 68 (12.4) | 0.02 | 76 (9.2) | 42 (9.7) | 50 (12.3) | 0.23 |
| Diabetes mellitusa | 113 (21.4) | 142 (24.1) | 105 (19.1) | 0.12 | 181 (21.9) | 99 (22.9) | 80 (19.6) | 0.50 |
| Smoking | ||||||||
| Never | 258 (48.8) | 288 (48.8) | 246 (44.7) | 0.04 | 402 (48.6) | 204 (47.1) | 186 (45.6) | 0.32 |
| Former | 226 (42.7) | 254 (43.1) | 275 (50.0) | 357 (43.1) | 201 (46.4) | 197 (48.3) | ||
| Current | 45 (8.5) | 48 (8.1) | 29 (5.3) | 69 (8.3) | 28 (6.5) | 25 (6.1) | ||
| Hearing aid use | 1 (0.2) | 13 (2.2) | 185 (33.6) | <0.001 | 3 (0.4) | 30 (6.9) | 166 (40.7) | <0.001 |
| Accelerometer-measured physical activity (min/wk MPA) (n=522)c | ||||||||
| Inactive (0) | 120 (74.1) | 157 (84.9) | 147 (84.0) | 0.09 | 218 (82.9) | 102 (77.9) | 104 (81.3) | 0.82 |
| Insufficiently active (<150) | 32 (19.8) | 20 (10.8) | 22 (12.6) | 32 (12.2) | 21 (16.0) | 18 (14.1) | ||
| Sufficiently active (≥150) | 10 (6.2) | 8 (4.3) | 6 (3.4) | 13 (4.9) | 8 (6.1) | 6 (4.7) | ||
| Hospitalization in past 12 mo | ||||||||
| 0 | 430 (81.3) | 466 (79.3) | 400 (72.9) | 0.002 | 663 (80.2) | 325 (75.2) | 308 (75.7) | 0.15 |
| 1 | 81 (15.3) | 87 (14.8) | 104 (18.9) | 125 (15.1) | 75 (17.4) | 72 (17.7) | ||
| >1 | 18 (3.4) | 35 (6.0) | 45 (8.2) | 39 (4.7) | 32 (7.4) | 27 (6.6) | ||
| Self-rated healthy days in past 30 daysd | ||||||||
| ≥ 10 days of poor physical health | 78 (15.5) | 93 (16.6) | 90 (17.8) | 0.64 | 109 (14.1) | 77 (18.6) | 75 (19.8) | 0.02 |
| ≥ 10 days poor mental health | 37 (7.4) | 36 (6.4) | 39 (7.7) | 0.71 | 47 (6.1) | 31 (7.5) | 34 (9.0) | 0.18 |
| Self-reported functional difficulty | ||||||||
| Activities of daily living | 93 (17.7) | 127 (21.6) | 145 (26.4) | 0.002 | 148 (17.9) | 85 (19.7) | 132 (32.4) | <0.001 |
| Instrumental activities of daily living | 103 (21.7) | 131 (26.3) | 130 (29.4) | 0.03 | 155 (21.6) | 103 (27.3) | 106 (33.0) | <0.001 |
| Leisure and social activities | 95 (18.9) | 125 (22.8) | 124 (24.8) | 0.07 | 140 (17.9) | 94 (23.6) | 110 (29.4) | <0.001 |
| Lower extremity mobility | 261 (51.3) | 368 (65.4) | 350 (66.3) | <0.001 | 428 (54.0) | 273 (65.8) | 278 (70.9) | <0.001 |
| General physical activity | 260 (51.8) | 314 (57.0) | 316 (62.1) | 0.004 | 387 (50.0) | 241 (59.4) | 262 (68.6) | <0.001 |
| Walking limitation | 85 (16.1) | 137 (23.2) | 148 (26.9) | <0.001 | 147 (17.8) | 101 (23.3) | 122 (29.9) | <0.001 |
| Memory and confusion limitation | 60 (11.4) | 81 (13.8) | 97 (17.6) | 0.01 | 93 (11.3) | 61 (14.1) | 84 (20.6) | <0.001 |
Variables were considered as binary. E.g. number of patients with hypertension in audiometry-measured “no HI” group is 353. Therefore, total number of patients without hypertension is 179 (total n=523 minus 353)
Cardiovascular disease includes any history of congestive heart failure, coronary artery disease, angina pectoris, or myocardial infarction
Accelerometer data available for subset of complete cohort
Multivariable binary and ordinal logistic regression was used to examine the relationships between HI and measures of functional outcomes. These relationships were assessed using audiometric HI defined as three different types of variables: continuous, binary, and ordinal. Self-reported HI was defined in the analyses as two different types of variables: binary and ordinal. Regression models were adjusted for demographics and cardiovascular risk factors. The proportional odds assumption in ordinal models was assessed using the Brant test, and partial proportional odds models were used to address violations of proportionality. Ordinal covariate parameterizations were compared against categorical parameterizations using the likelihood ratio test. Linearity of associations with continuous covariates was assessed using smoothed residual plots. Significance was considered using a two-tailed t-test with p<.05. All analyses were conducted using Stata 11.1 (StataCorp, College Station, TX).
Results
Data from a total of 1669 participants aged 70 years or older were examined in this study (Table 1). Within the study population, 529 (31.7%) had normal audiometric-hearing, and 828 (49.6%) reported that they had excellent or good hearing based on self-report. The agreement rate between audiometric and self-reported binary assessments of HI was 69%, with 79% of misclassification attributable to underestimation of HI (kappa=0.38). Figure 1 shows the relationship between audiometry-measured hearing and self-reported general condition of hearing. There is an overall linear relationship between the two measures of hearing, but wide distributions within each category of self-reported hearing with trends towards underestimation of HI can be noted. Poorer hearing measured by both audiometry and self-report were associated with being male, older, white, having cardiovascular disease, and using hearing aids. Poorer hearing measured by audiometry alone was associated with having less education, lower income, history of stroke, and smoking history.
Figure 1.
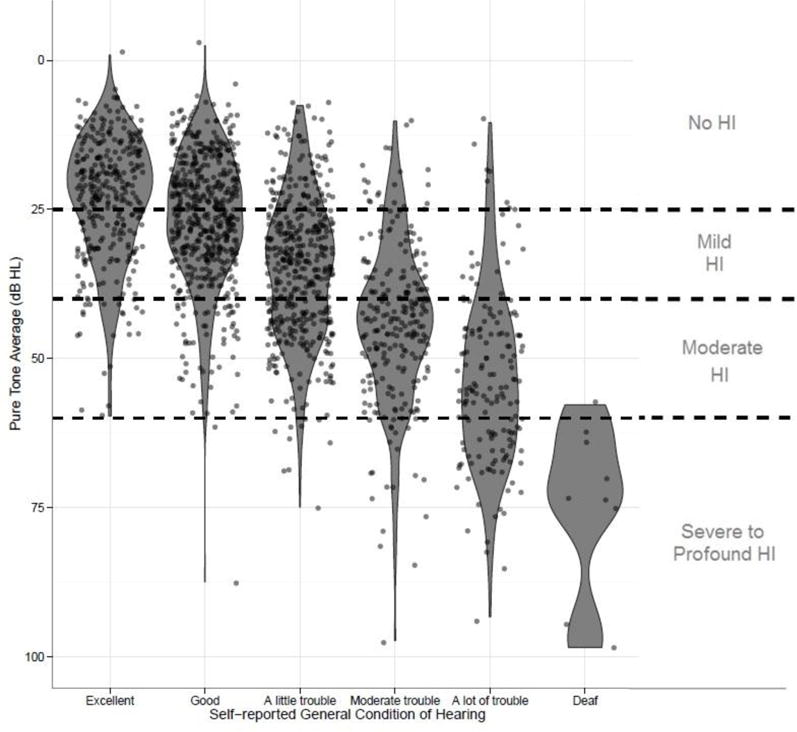
Violin plots combined with jittered scatter plots of self-reported general condition of hearing and pure-tone audiometry hearing level in dB among participants aged 70 and older, NHANES 2005–2006 and 2009–2010, N=1669
Associations between Hearing Impairment and Objective Outcomes
In a model adjusted for demographics and cardiovascular risk factors, a 25-dB difference in hearing threshold of the pure-tone average was associated with greater odds of being in a lower category of physical activity measured by accelerometer (OR = 1.67, 95% CI: 1.05–2.64), any hospitalization (OR = 1.32, 95% CI: 1.07=1.63), and greater number of hospitalizations (OR = 1.35, 95% CI: 1.09–1.68), as shown in Table 2. Ordinal measures of audiometric HI were also significantly associated with poorer physical activity and hospitalizations when comparing moderate-or-greater HI to normal hearing. In contrast, there were no significant associations between self-reported HI and accelerometer-measured physical activity or hospitalization. Compared to individuals reporting excellent or good hearing, individuals self-reporting moderate-or-greater trouble hearing did not have greater odds of being in a lower category of physical activity measured by accelerometer (OR = 1.19, 95% CI: 0.69–2.06), any hospitalization (OR = 1.14, 95% CI: 0.90–1.43), or number of hospitalizations (OR = 1.15, 95% CI: 0.92–1.44).
Table 2.
Association between Hearing Impairment (HI) and Functional Outcomes, NHANES 2005–2006 and 2009–2010, N=1669
| Outcomes | Assessment of Hearing Impairment Using Speech-Frequency Pure-Tone Audiometrya |
Assessment of Hearing Impairment Using Self-Report |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HI as a Continuous Variable in dB |
HI as a Binary Variable
|
HI as an Ordinal Variable
|
HI as a Binary Variable
|
HI as an Ordinal Variable
|
||||||||
| OR per 25dB of HI (95% CI) |
No HI | Any HI | No HI | Mild HI | Moderate or Greater HI |
Excellent or Good Hearing |
Any Trouble of Hearing |
Excellent or Good Hearing |
A Little Trouble of Hearing |
Moderate or Greater Trouble Hearing |
||
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |||||||
| Objective Outcomes | Accelerometer-Measured Physical Activityb | |||||||||||
| Next lower category of physical activityc | 1.7 (1.1–2.6) | ref | 2.2 (1.1–4.3) | ref | 2.3 (0.9–5.4) | 1.9 (1.0–3.4) | ref | 1.0 (0.7–1.4) | ref | 0.8 (0.5–1.4) | 1.2 (0.7–2.1) | |
| Hospitalization in past 12 monthsd | ||||||||||||
| Any (yes or no) | 1.3 (1.1–1.6) | ref | 1.3 (1.0 – 1.8) | ref | 1.2 (0.8 – 1.7) | 1.6 (1.2 – 2.2) | ref | 1.2 (0.9 – 1.6) | ref | 1.3 (0.9 – 1.8) | 1.1 (0.9 – 1.4) | |
| No. of hospitalizations (0, 1, >1) | 1.4 (1.1–1.7) | ref | 1.4 (1.0 – 1.9) | ref | 1.2 (0.8 – 1.7) | 1.7 (1.2 – 2.4) | ref | 1.2 (1.0 – 1.6) | ref | 1.3 (0.9 – 1.9) | 1.2 (0.9 – 1.4) | |
|
| ||||||||||||
| Subjective Outcomes | Self-reported Healthy Days in Past 30 daysd | |||||||||||
| ≥ 10 days with poor physical health | 1.4 (1.1–1.7) | ref | 1.4 (1.0 – 2.1) | ref | 1.3 (0.8 – 2.0) | 1.6 (1.1 – 2.5) | ref | 1.4 (1.0 – 2.0) | ref | 1.3 (0.9 – 2.1) | 1.5 (1.1 – 2.2) | |
| ≥ 10 days with poor mental health | 1.6 (1.2–2.1) | ref | 1.7 (1.0 – 3.0) | ref | 1.5 (0.8 – 3.0) | 2.1 (1.2 – 3.6) | ref | 1.8 (1.1 – 3.1) | ref | 1.6 (0.8 – 3.0) | 2.1 (1.2 – 3.8) | |
| Self-reported Functional Difficultyd | ||||||||||||
| ADL | 1.4 (1.1–1.9) | ref | 1.5 (1.1 – 2.1) | ref | 1.4 (1.0 – 1.9) | 1.7 (1.1 – 2.5) | ref | 1.6 (1.1–2.4) | ref | 1.1 (0.7 – 1.7) | 2.4 (1.6 – 3.8) | |
| IADL | 1.6 (1.2–2.2) | ref | 1.7 (1.1 – 2.5) | ref | 1.5 (1.0 – 2.4) | 1.9 (1.2 – 3.1) | ref | 2.0 (1.4 – 2.9) | ref | 1.7 (1.2 – 2.5) | 2.4 (1.5 – 3.7) | |
| Leisure and social activities | 1.5 (1.1–2.0) | ref | 1.5 (0.9 – 2.2) | ref | 1.4 (0.9 – 2.2) | 1.5 (0.9 – 2.4) | ref | 1.8 (1.4 – 2.3) | ref | 1.5 (1.0 – 2.1) | 2.1 (1.6 – 3.0) | |
| Lower extremity mobility | 1.4 (1.1–1.7) | ref | 1.7 (1.3 – 2.2) | ref | 1.7 (1.3 – 2.3) | 1.6 (1.1 – 2.2) | ref | 1.9 (1.4 – 2.6) | ref | 1.7 (1.2 – 2.4) | 2.3 (1.6 – 3.2) | |
| General physical activity | 1.3 (1.1–1.6) | ref | 1.3 (1.0 – 1.6) | ref | 1.2 (1.0 – 1.5) | 1.4 (1.0 – 2.0) | ref | 1.9 (1.4 – 2.4) | ref | 1.5 (1.1 – 2.1) | 2.4 (1.8 – 3.4) | |
| Walking lim. | 1.6 (1.3–2.0) | ref | 1.7 (1.3 – 2.2) | ref | 1.6 (1.2 – 2.1) | 1.9 (1.4 – 2.7) | ref | 1.8 (1.4 – 2.4) | ref | 1.5 (1.0 – 2.2) | 2.4 (1.8 – 3.1) | |
| Memory and confusion lim. | 1.4 (1.1–1.8) | ref | 1.3 (0.9 – 1.8) | ref | 1.2 (0.8 – 1.7) | 1.5 (1.0 – 2.1) | ref | 1.6 (1.1 – 2.5) | ref | 1.3 (0.9 – 2.1) | 2.0 (1.2 – 3.2) | |
Shaded in light grey: p<0.05, and shaded in dark grey: p<0.01
HI=Hearing Impairment, ADL=Activities of Daly Living, IADL=Instrumental Activities of Daily Living, lim.=limitation
Audiometry-measured hearing is defined as a speech-frequency pure tone average of hearing thresholds at 0.5, 1, 2, and 4 kHz in the better-hearing ear (normal PTA <25dB, mild hearing impairment 25–39dB, moderate or greater ≥ 40dB).
Adjusted for age, sex, race, education, income, hypertension, cardiovascular disease, stroke, and smoking status.
Categories of physical activity (inactive: 0min/wk of moderate-intensity physical activity (MPA), insufficiently active: <150 min/wk of MPA, sufficiently active: ≥ 150 min/wk of MPA)
Adjusted for age, sex, race, education, income, hypertension, cardiovascular disease, stroke, diabetes, and smoking status
Associations between Hearing Impairment and Subjective Outcomes
We observed an opposing pattern of results for associations of HI with subjectively measured outcomes. In general, both audiometric and self-reported assessments of hearing remained significantly associated with self-rated health and physical function, with the associations of the greatest magnitude being observed between self-reported assessments of hearing and subjective outcomes (Table 2). Relative to individuals with normal hearing, those with moderate or greater audiometric HI reported poorer self-rated physical health (OR=1.61, 95% CI: 1.14–2.46) as individuals with moderate or greater trouble hearing reported poorer health than those with excellent or good hearing (OR=1.54, 95% CI: 1.10–2.15). Self-reported limitations in several domains of physical functioning that were not significantly associated with binary measures of audiometric HI (limitation in leisure and social activities OR=1.45, 95% CI: 0.94–2.23; and work limitation OR=1.17, 95% CI: 0.85–1.60) were significantly associated with binary measures of self-reported HI (limitation in leisure and social activities OR=1.76, 95% CI: 1.36–2.27; and work limitation OR=1.51, 95% CI: 1.15–1.98).
Discussion
We investigated the association of audiometric versus self-reported measures of hearing with functional outcomes in older adults using a nationally representative sample of the U.S. population. Our results demonstrate that using self-reported measures of hearing in epidemiologic studies may underestimate the magnitude of associations of HI with objective functional outcomes, such as accelerometer-measured physical activity and number of hospitalizations. Conversely, using self-reported measures of hearing compared to audiometry may overestimate the magnitude of associations with subjective outcomes, such as self-reported healthy days and limitation in physical functioning. The differential associations by method of hearing assessment bring into question the validity of using self-reported hearing as a proxy for standard audiometry.
There have been several studies reporting the associations between HI measured by both audiometry and self-report and their selected functional outcomes. Gopinath et al. demonstrated significant association between moderate-or-greater HI and impaired ADL, which was not found when hearing was measured with the Hearing Handicap Inventory for the Elderly-Screening (HHIE-S). However, most of the previous studies have used either self-reported hearing or audiometry only. Even within the studies using self-reported hearing, the interview questions used to assess hearing varied depending on whether a single question or more detailed questionnaire (i.e. HHIE-S) was used, whether respondents rated their hearing with or without hearing aid, one or both ears were investigated, and/or tinnitus was considered as HI, (Curhan, Eavey, Wang, Stampfer, & Curhan, 2013; Dargent-Molina et al., 1996; Kiely et al., 2012; Laforge, 1992; Sindhusake et al., 2001; Strawbridge et al., 2000). The definitions of self-reported HI used in their analyses also varied significantly, with variables being defined as binary or categorical with or without combination with visual impairment, making it difficult to compare previous findings to the present study.
Our results indicate that there may be weaker associations of HI with objective outcomes including low physical activity and number of hospitalizations when using self-report versus audiometry. One potential explanation is that the imprecise assessment of hearing when using self-report causes attenuation of the observed associations as older adults often underestimate their HI, either considering it to be a normal part of the aging process or denying their HI altogether due to the stigma of HI being associated with ageism and the perception of hearing impairment as a disability (Dalton et al., 2003; Gopinath et al., 2012; Gordon-Salant, 2005; Kamil et al., 2015; Wallhagen, 2010; Wiley, Cruickshanks, Nondahl, & Tweed, 2000). Additionally, older adults may not report trouble hearing when its severity is mild due to the gradual nature of the age-related HI. Systematic misclassification of HI, such as the underestimation of HI observed in this cohort, results in bias, especially when factors associated with underestimation are also associated with the outcome of interest. The weaker associations observed in our study between self-reported measures of hearing and objective functional outcomes were similar to results from previous studies investigating differences between subjective and objective measures of physical activity and their associations with biomarkers (Atienza et al., 2011; Schmidt, Cleland, Thomson, Dwyer, & Venn, 2008).
In contrast to the objective outcomes, subjective functional outcomes were generally associated with self-reported HI. These results may be related to the concept of health pessimism, which purports that individuals who report difficulty hearing are more likely to report difficulties in other domains of health, such as physical functioning and self-reported general health status.(Bailey, 2013; Scheier & Carver, 1985; Vavreck, 2007). The potential threats to validity caused by using self-report for both independent and dependent variables have been discussed across various research fields (Chan, 2009; Del Boca & Noll, 2000; Podsakoff, MacKenzie, Lee, & Podsakoff, 2003; Spector, 1994; Vavreck, 2007). Drawing inferences from associations among self-report at one point in time is often difficult and warrants caution in its interpretation. Our findings suggest that self-reported measure of hearing may not be a proxy of audiometric hearing but rather provide distinct aspects of hearing in relation to the personal factors and communication environments. It is important to note that self-reported hearing may be a more sensitive measure of hearing in regards to the functional impairment in daily lives of older adults compared to the audiometric hearing (Louise Hickson, 2008). Additional use of validated measures of self-reported hearing, which provides useful information in association with self-perceived handicapping from HI and its impact, may improve rehabilitation of older adults with HI in clinical setting (Tomioka et al., 2013; Weinstein, 1994).
There are several limitations to the present study. The data from NHANES is cross-sectional, limiting the ability to assess the temporal order of the associations observed in this study. Secondly, potential effect modifiers (e.g., marital status, living status of partner, vision impairment, etc) that could affect the magnitude of the association between hearing and the functional outcomes were not addressed in this study. However, we note that all analyses were adjusted for potential confounders. Additionally, we collapsed self-reported and audiometric measures of hearing as ordinal variables a priori for simpler comparison of the two predictors. While it is possible that different results may have been obtained if we used different cutoffs for defining levels of these predictors, similar results were observed when both predictors were collapsed into binary variables which were defined with relatively ubiquitous cutoffs. Furthermore, quantitative comparison of the difference between the observed associations is not possible, as self-reported and audiometric assessments of hearing are fundamentally different, albeit related measures of HI. Our results only suggest differential patterns of associations with functional outcomes when using self-reported versus audiometric measures of hearing. Future research can further explore the difference between self-reported hearing and audiometric hearing measured on a continuous scale, by using the sums and differences of these measures as covariates in statistical models (Stern, 2006).
In summary, using self-reported hearing instead of audiometric hearing may underestimate the associations with objective functional outcomes and overestimate the associations with subjective outcomes in older adults relative to pure-tone audiometry. The results of this study suggest that epidemiological studies using self-reported hearing in older adults should be interpreted with caution, as self-reported measure may capture distinct aspects of HI among older adults. Results obtained from self-reported hearing should not be considered representative of results from using audiometric measure of hearing.
Acknowledgments
This manuscript was supported in part by NIH K23DC011279, the Eleanor Schwartz Charitable Foundation, a Triological Society/American College of Surgeons Clinician Scientist Award, and the Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by NIH TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Footnotes
Declaration of Conflicting Interests: Dr. Frank Lin reports being a consultant to Cochlear, on the scientific advisory board for Autifony and Pfizer, and a speaker for Med El and Amplifon
References
- Atienza AA, Moser RP, Perna F, Dodd K, Ballard-Barbash R, Troiano RP, Berrigan D. Self-reported and objectively measured activity related to biomarkers using NHANES. [Research Support, N.I.H., Extramural] Med Sci Sports Exerc. 2011;43(5):815–821. doi: 10.1249/MSS.0b013e3181fdfc32. [DOI] [PubMed] [Google Scholar]
- Bailey J. Pessimism-Bailey. Routledge; 2013. [Google Scholar]
- Bamiou DE, Worth S, Phelps P, Sirimanna T, Rajput K. Eighth nerve aplasia and hypoplasia in cochlear implant candidates: the clinical perspective. [Case Reports] Otol Neurotol. 2001;22(4):492–496. doi: 10.1097/00129492-200107000-00014. [DOI] [PubMed] [Google Scholar]
- Bess FH, Lichtenstein MJ, Logan SA, Burger MC, Nelson E. Hearing impairment as a determinant of function in the elderly. [Research Support, Non-U.S. Gov’t] J Am Geriatr Soc. 1989;37(2):123–128. doi: 10.1111/j.1532-5415.1989.tb05870.x. [DOI] [PubMed] [Google Scholar]
- Chan D. So why ask me? Are self-report data really that bad 2009 [Google Scholar]
- Chen DS, Genther DJ, Betz J, Lin FR. Association between hearing impairment and self-reported difficulty in physical functioning. #x0005B;Multicenter Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] J Am Geriatr Soc. 2014;62(5):850–856. doi: 10.1111/jgs.12800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chia EM, Wang JJ, Rochtchina E, Cumming RR, Newall P, Mitchell P. Hearing impairment and health-related quality of life: the Blue Mountains Hearing Study. [Research Support, Non-U.S. Gov’t] Ear Hear. 2007;28(2):187–195. doi: 10.1097/AUD.0b013e31803126b6. [DOI] [PubMed] [Google Scholar]
- Clark JG. Uses and abuses of hearing loss classification. ASHA. 1981;23(7):493–500. [PubMed] [Google Scholar]
- Coppin AK, Shumway-Cook A, Saczynski JS, Patel KV, Ble A, Ferrucci L, Guralnik JM. Association of executive function and performance of dual-task physical tests among older adults: analyses from the InChianti study. [Research Support, N.I.H., Intramural Research Support, Non-U.S. Gov’t] Age Ageing. 2006;35(6):619–624. doi: 10.1093/ageing/afl107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curhan SG, Eavey R, Wang M, Stampfer MJ, Curhan GC. Body mass index, waist circumference, physical activity, and risk of hearing loss in women. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] Am J Med. 2013;126(12):1142 e1141-1148. doi: 10.1016/j.amjmed.2013.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalton DS, Cruickshanks KJ, Klein BE, Klein R, Wiley TL, Nondahl DM. The impact of hearing loss on quality of life in older adults. [Research Support, U.S. Gov’t, P.H.S.] Gerontologist. 2003;43(5):661–668. doi: 10.1093/geront/43.5.661. [DOI] [PubMed] [Google Scholar]
- Dargent-Molina P, Hays M, Breart G. Sensory impairments and physical disability in aged women living at home. [Research Support, Non-U.S. Gov’t] Int J Epidemiol. 1996;25(3):621–629. doi: 10.1093/ije/25.3.621. [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. [Research Support, U.S. Gov’t, P.H.S. Review] Addiction. 2000;95(Suppl 3):S347–360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.] JAMA. 2013;309(22):2322–2324. doi: 10.1001/jama.2013.5912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gispen FE, Chen DS, Genther DJ, Lin FR. Association between hearing impairment and lower levels of physical activity in older adults. [Observational Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] J Am Geriatr Soc. 2014;62(8):1427–1433. doi: 10.1111/jgs.12938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopinath B, Schneider J, McMahon CM, Teber E, Leeder SR, Mitchell P. Severity of age-related hearing loss is associated with impaired activities of daily living. [Research Support, Non-U.S. Gov’t] Age Ageing. 2012;41(2):195–200. doi: 10.1093/ageing/afr155. [DOI] [PubMed] [Google Scholar]
- Gordon-Salant S. Hearing loss and aging: new research findings and clinical implications. [Research Support, N.I.H., Extramural Review] J Rehabil Res Dev. 2005;42(4 Suppl 2):9–24. doi: 10.1682/jrrd.2005.01.0006. [DOI] [PubMed] [Google Scholar]
- Kamil RJ, Genther DJ, Lin FR. Factors associated with the accuracy of subjective assessments of hearing impairment. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.] Ear Hear. 2015;36(1):164–167. doi: 10.1097/AUD.0000000000000075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller BK, Morton JL, Thomas VS, Potter JF. The effect of visual and hearing impairments on functional status. [Comparative Study] J Am Geriatr Soc. 1999;47(11):1319–1325. doi: 10.1111/j.1532-5415.1999.tb07432.x. [DOI] [PubMed] [Google Scholar]
- Kiely KM, Gopinath B, Mitchell P, Browning CJ, Anstey KJ. Evaluating a dichotomized measure of self-reported hearing loss against gold standard audiometry: prevalence estimates and age bias in a pooled national data set. [Research Support, Non-U.S. Gov’t] J Aging Health. 2012;24(3):439–458. doi: 10.1177/0898264311425088. [DOI] [PubMed] [Google Scholar]
- Laforge RG, Spector William D, Sternberg Josef. The relationship of vision and hearing impairment to one-year mortality and functional decline. Journal of Aging and Health. 1992;4(1):126–148. [Google Scholar]
- Li CM, Zhang X, Hoffman HJ, Cotch MF, Themann CL, Wilson MR. Hearing impairment associated with depression in US adults, National Health and Nutrition Examination Survey 2005–2010. [Research Support, N.I.H., Extramural Research Support, U.S. Gov’t, P.H.S.] JAMA Otolaryngol Head Neck Surg. 2014;140(4):293–302. doi: 10.1001/jamaoto.2014.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR. Hearing loss in older adults: who’s listening? [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] JAMA. 2012;307(11):1147–1148. doi: 10.1001/jama.2012.321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Ferrucci L, Metter EJ, An Y, Zonderman AB, Resnick SM. Hearing loss and cognition in the Baltimore Longitudinal Study of Aging. [Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural] Neuropsychology. 2011;25(6):763–770. doi: 10.1037/a0024238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Metter EJ, O’Brien RJ, Resnick SM, Zonderman AB, Ferrucci L. Hearing loss and incident dementia. [Research Support, N.I.H., Extramural Research Support, N.I.H., Intramural] Arch Neurol. 2011;68(2):214–220. doi: 10.1001/archneurol.2010.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Thorpe R, Gordon-Salant S, Ferrucci L. Hearing loss prevalence and risk factors among older adults in the United States. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] J Gerontol A Biol Sci Med Sci. 2011;66(5):582–590. doi: 10.1093/gerona/glr002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin FR, Yaffe K, Xia J, Xue QL, Harris TB, Purchase-Helzner E, Simonsick EM. Hearing loss and cognitive decline in older adults. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] JAMA Intern Med. 2013;173(4):293–299. doi: 10.1001/jamainternmed.2013.1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin MY, Gutierrez PR, Stone KL, Yaffe K, Ensrud KE, Fink HA, Mangione CM. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. [Multicenter Study Research Support, U.S. Gov’t, P.H.S.] J Am Geriatr Soc. 2004;52(12):1996–2002. doi: 10.1111/j.1532-5415.2004.52554.x. [DOI] [PubMed] [Google Scholar]
- Lopez-Torres Hidalgo J, Boix Gras C, Tellez Lapeira J, Lopez Verdejo MA, del Campo del Campo JM, Escobar Rabadan F. Functional status of elderly people with hearing loss. [Research Support, Non-U.S. Gov’t] Arch Gerontol Geriatr. 2009;49(1):88–92. doi: 10.1016/j.archger.2008.05.006. [DOI] [PubMed] [Google Scholar]
- Louise Hickson JA, Beswick Rachael, et al. Relationships between hearing disability, quality of life and wellbeing in older community-based Australians. The Australian and New Zealand Journal of Audiology. 2008;30:99–112. [Google Scholar]
- McClay JE, Booth TN, Parry DA, Johnson R, Roland P. Evaluation of pediatric sensorineural hearing loss with magnetic resonance imaging. Arch Otolaryngol Head Neck Surg. 2008;134(9):945–952. doi: 10.1001/archotol.134.9.945. [DOI] [PubMed] [Google Scholar]
- Metzger JS, Catellier DJ, Evenson KR, Treuth MS, Rosamond WD, Siega-Riz AM. Patterns of objectively measured physical activity in the United States. [Research Support, N.I.H., Extramural] Med Sci Sports Exerc. 2008;40(4):630–638. doi: 10.1249/MSS.0b013e3181620ebc. [DOI] [PubMed] [Google Scholar]
- Perissinotto CM, Stijacic Cenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. [Research Support, N.I.H., Extramural] Arch Intern Med. 2012;172(14):1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plantinga LC, Johansen K, Crews DC, Shahinian VB, Robinson BM, Saran R, Powe NR. Association of CKD with disability in the United States. [Comparative Study Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’ Research Support, U.S. Gov’t, P.H.S.] Am J Kidney Dis. 2011;57(2):212–227. doi: 10.1053/j.ajkd.2010.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Podsakoff PM, MacKenzie SB, Lee JY, Podsakoff NP. Common method biases in behavioral research: a critical review of the literature and recommended remedies. [Review] J Appl Psychol. 2003;88(5):879–903. doi: 10.1037/0021-9010.88.5.879. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Mui S, Damesyn M, Moore AA, Greendale GA. The prognostic value of sensory impairment in older persons. [Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S.] J Am Geriatr Soc. 1999;47(8):930–935. doi: 10.1111/j.1532-5415.1999.tb01286.x. [DOI] [PubMed] [Google Scholar]
- Rudberg MA, Furner SE, Dunn JE, Cassel CK. The relationship of visual and hearing impairments to disability: an analysis using the longitudinal study of aging. [Research Support, U.S. Gov’t, P.H.S.] J Gerontol. 1993;48(6):M261–265. doi: 10.1093/geronj/48.6.m261. [DOI] [PubMed] [Google Scholar]
- Scheier MF, Carver CS. Optimism, coping, and health: assessment and implications of generalized outcome expectancies. [Research Support, U.S. Gov’t, Non-P.H.S.] Health Psychol. 1985;4(3):219–247. doi: 10.1037//0278-6133.4.3.219. [DOI] [PubMed] [Google Scholar]
- Schmidt MD, Cleland VJ, Thomson RJ, Dwyer T, Venn AJ. A comparison of subjective and objective measures of physical activity and fitness in identifying associations with cardiometabolic risk factors. [Comparative Study Research Support, Non-U.S. Gov’t] Ann Epidemiol. 2008;18(5):378–386. doi: 10.1016/j.annepidem.2008.01.005. [DOI] [PubMed] [Google Scholar]
- Sennaroglu L, Saatci I. A new classification for cochleovestibular malformations. Laryngoscope. 2002;112(12):2230–2241. doi: 10.1097/00005537-200212000-00019. [DOI] [PubMed] [Google Scholar]
- Sindhusake D, Mitchell P, Smith W, Golding M, Newall P, Hartley D, Rubin G. Validation of self-reported hearing loss. The Blue Mountains Hearing Study. [Research Support, Non-U.S. Gov’t Validation Studies] Int J Epidemiol. 2001;30(6):1371–1378. doi: 10.1093/ije/30.6.1371. [DOI] [PubMed] [Google Scholar]
- Spector PE. Using self‐report questionnaires in OB research: a comment on the use of a controversial method. Journal of Organizational Behavior. 1994;15(5):385–392. [Google Scholar]
- Stern AGaH. The difference between “significant” and “not significant” is not itself statistically significant. The American Statistician. 2006;60(4):328–331. [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Shema SJ, Kaplan GA. Negative consequences of hearing impairment in old age: a longitudinal analysis. [Research Support, U.S. Gov’t, P.H.S.] Gerontologist. 2000;40(3):320–326. doi: 10.1093/geront/40.3.320. [DOI] [PubMed] [Google Scholar]
- Tomioka K, Ikeda H, Hanaie K, Morikawa M, Iwamoto J, Okamoto N, Kurumatani N. The Hearing Handicap Inventory for Elderly-Screening (HHIE-S) versus a single question: reliability, validity, and relations with quality of life measures in the elderly community, Japan. Quality of Life Research. 2013;22(5):1151–1159. doi: 10.1007/s11136-012-0235-2. [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. Am J Prev Med. 2011;40(4):454–461. doi: 10.1016/j.amepre.2010.12.016. [DOI] [PubMed] [Google Scholar]
- Tun PA, McCoy S, Wingfield A. Aging, hearing acuity, and the attentional costs of effortful listening. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t] Psychol Aging. 2009;24(3):761–766. doi: 10.1037/a0014802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Physical Activity Guidelines for Americnas: Appendix 1. Translating Scientific Evidnece About Total Amount and Intensity of Physical Activity Into Guidelines. Retrieved May 7, 2015, from http://www.health.gov/PAGuidelines/guidelines/appendix1.aspx.
- Valete-Rosalino CM, Rozenfeld S. Auditory screening in the elderly: comparison between self-report and audiometry. [Comparative Study Meta-Analysis Review] Braz J Otorhinolaryngol. 2005;71(2):193–200. doi: 10.1016/S1808-8694(15)31310-0. doi: /S0034-72992005000200013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vavreck L. The exaggerated effects of advertising on turnout: The dangers of self-reports. Quarterly Journal of Political Science. 2007;2(4):325–343. [Google Scholar]
- Viljanen A, Kaprio J, Pyykko I, Sorri M, Koskenvuo M, Rantanen T. Hearing acuity as a predictor of walking difficulties in older women. [Research Support, Non-U.S. Gov’t] J Am Geriatr Soc. 2009;57(12):2282–2286. doi: 10.1111/j.1532-5415.2009.02553.x. [DOI] [PubMed] [Google Scholar]
- Wallhagen MI. The stigma of hearing loss. [Comparative Study Research Support, N.I.H., Extramural] Gerontologist. 2010;50(1):66–75. doi: 10.1093/geront/gnp107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein BE. Age-Related Hearing-Loss - How to Screen for It, and When to Intervene. Geriatrics. 1994;49(8):40–45. [PubMed] [Google Scholar]
- Weinstein BE, Ventry IM. Hearing impairment and social isolation in the elderly. [Research Support, Non-U.S. Gov’t] J Speech Hear Res. 1982;25(4):593–599. doi: 10.1044/jshr.2504.593. [DOI] [PubMed] [Google Scholar]
- Wiley TL, Cruickshanks KJ, Nondahl DM, Tweed TS. Self-reported hearing handicap and audiometric measures in older adults. [Research Support, U.S. Gov’t, P.H.S.] J Am Acad Audiol. 2000;11(2):67–75. [PubMed] [Google Scholar]


