Abstract
Background
The development of thrombocytopenia in sepsis is a poor prognostic indicator associated with a significantly increased mortality risk. Mechanisms underlying this phenomenon remain to be clearly elucidated. Matrix metalloproteinases (MMPs) are enzymes that regulate the turnover of the extra-cellular matrix. MMP-2 is recognised as a platelet agonist with MMP-9 proposed as an inhibitor of platelet activation. The existence of MMP-9 in platelets is a subject of debate. There is limited evidence thus far to suggest that toll-like receptor 4 (TLR-4) and platelet-leukocyte aggregate (PLA) formation may be implicated in the development of sepsis-associated thrombocytopenia.
Objectives
To investigate whether MMP -2/-9, toll-like receptor 4 (TLR-4) or platelet-leukocyte aggregate (PLA) formation are implicated in a decline in platelet numbers during septic shock.
Methods
This was an observational study which recruited healthy controls, non-thrombocytopenic septic donors and thrombocytopenic septic donors. MMP-2, MMP-9 and TLR-4 platelet surface expression as well as PLA formation was examined using flow cytometry. In addition MMP-2 and MMP-9 were examined by gelatin zymography and enzyme-linked immunosorbent assay (ELISA) using a 3 compartment model (plasma, intraplatelet and platelet membrane).
Results
There was no difference found in MMP-2, MMP-9 or TLR-4 levels between non-thrombocytopenic and thrombocytopenic septic donors. PLA formation was increased in thrombocytopenic patients. MMP-9 was detected in platelets using flow cytometry, gelatin zymography and ELISA techniques.
Conclusions
Platelet consumption into PLAs may account for the development of thrombocytopenia in septic shock. MMP-9 is found in platelets and it is upregulated during septic shock.
Introduction
Severe sepsis is often associated with a decrease in platelet numbers. With platelet counts below 150,000/μl widely accepted as thrombocytopenia [1], reported rates of sepsis-associated thrombocytopenia in the literature range from 14.5% to 70.6% [2, 3]. If thrombocytopenia does occur during sepsis it is associated with a significant increase in mortality [4–8]. Thrombocytopenia may occur due to a decreased production of platelets [9], so called “marrow failure” [10], alternatively, thrombopoiesis may be increased during sepsis [11, 12].
Matrix metalloproteinases (MMPs) are a group of zinc-dependent endopeptidases that remodel the extracellular matrix [13]. However, MMP-2 is also recognised as a mediator of platelet activation [14, 15]. Interestingly, another gelatinase, MMP-9, has been proposed as an inhibitor of platelet aggregation [16]; however, whether MMP-9 can actually be found in platelets remains a matter of debate [17–19].
Toll-like receptors (TLRs) are key players in innate immunity, acting as pathogen recognition receptors [20]. Animal studies suggest that platelet TLR-4 is involved in the development of sepsis-associated thrombocytopenia [21–23].
Following platelet adhesion to the subendothelium, adenosine diphosphate (ADP) is released from dense granules in addition to fibrinogen and P-selectin being released from α-granules. Thus P-selectin is widely regarded as a marker of platelet activation. Activated platelets can adhere to circulating leukocytes to form platelet-leukocyte aggregates (PLAs) and those are considered to be reliable indicators of a prothrombotic state. PLAs are associated with several cardiovascular disorders [24] and are also increased during sepsis [25, 26].
The main objective of this work was to study mechanisms that could contribute to the development of sepsis-associated thrombocytopenia focusing on the MMP-2/-9 platelet dependent pathway, platelet TLR-4 signalling and PLA formation in sepsis.
Materials and methods
Participants
Ethical approval was obtained from the Research Ethics Committee of St James’s hospital (REC reference: 2013/07/03 RTC). Consecutive patients with septic shock (as defined by the Surviving Sepsis guidelines 2012 [27]) were recruited from the ICU of St James’s hospital over an 18 month period. Exclusion criteria are listed in Table 1. Sampling took place within 72 hours of admission to the ICU. Patients’ clinical data was recorded including age, gender, diagnosis, platelet and white cell counts, microbiological culture results, Sequential Organ Failure Assessment (SOFA) score and Acute Physiology and Chronic Health Evaluation II (APACHE II) score. For classification of a patient as “thrombocytopenic” the patient had either (a) a platelet count on admission or within 72 hours of admission of less than 100,000/μl or (b) a drop in platelet count of greater than 50% from their platelet count on admission within 72 hours of that admission. We chose a limit of 100,000/μl as opposed to 150,000 because we wanted to capture clinically relevant data. A drop of >50% in platelet count is also a safe margin of error for this given that other studies have used a lesser proportional decrease. Male and female healthy controls, aged over 18, who refrained from drinking alcohol and smoking tobacco for 48 hours prior to sampling and had not taken any drugs in the preceding 14 days were recruited as controls.
Table 1. Exclusion criteria for patient selection.
| Age below 18 |
| Use of drugs known to affect platelet function |
| Cardiopulmonary bypass or extracorporeal life support in preceding 2 weeks |
| History of haematological malignancy |
| Disorders affecting thrombopoiesis e.g. essential thrombocytosis |
| Thrombotic microangiopathies e.g. thrombotic thrombocytopenic pupura |
| Pregnancy or the postpartum period |
| Therapeutic anticoagulation with unfractionated heparin and activated partial thromboplastin time > 40 seconds |
| Congenital platelet disorder e.g Bernard-Soulier syndrome |
| Massive transfusion of blood products (greater than their normal circulating blood volume) in preceding week |
| Platelet transfusion in preceding week |
Ethics statement
Ethical approval was obtained from the Research Ethics Committee of St James’s hospital, Dublin, Ireland (REC reference: 2013/07/03 RTC). Written informed consent was obtained from patients or their next of kin.
Reagents
All reagents were purchased from Sigma-Aldrich (Dublin, Ireland) unless otherwise indicated.
Sample preparation
Peripheral blood samples were obtained from healthy controls via venepuncture into antecubital fossa veins using 21G needles mounted on a 50 mL syringe. Blood samples from septic patients were withdrawn from indwelling central venous catheters. Whole blood was collected and processed immediately. Firstly it was mixed with 3.15% sodium citrate solution in a 9:1 ratio. Platelet-rich plasma (PRP) was prepared by centrifugation as previously described [28]. PRP was then centrifuged at 900g for 10 minutes at room temperature for the preparation of platelet-poor plasma (PPP) and platelet pellets [28]. PPP and platelet pellets were stored at -20°C and thawed for batch analysis.
Platelet surface expression of P-selectin, MMP-2, MPP-9 and TLR-4
Flow cytometry (FC) is a laser-based technique that measures optical and fluorescence characteristics of single cells or particles. It can be used to measure the platelet surface expression of P-selectin, MMP-2, MMP-9 and TLR-4. Whole blood samples were analysed by FC within 30 minutes of collection. Primary antibodies used were CD62P APC (BD Pharmingen) (used to stain for P-selectin expression), MMP-2 PE (R&D Systems), MMP-9 (Pierce antibodies) and TLR-4 Biotin (BD Pharmingen) for platelets and CD45 PerCP (ImmunoTools) as a leukocyte marker. For TLR-4 and MMP-9, secondary antibodies anti-biotin (Miltenyi Biotec) and anti-IgG2a (Miltenyi Biotec) were used respectively. Thrombin receptor activating peptide (TRAP-6) was used as a platelet agonist. As per manufacturers’ instructions primary antibodies were incubated with whole blood in the dark for 30 minutes and secondary antibodies for 20 minutes at 4°C. Following incubation, red cell lysis was performed using an ammonium chloride/potassium bicarbonate buffer (155 mM NH4Cl, 10 mM KHCO3). Isotype controls were used to set the negative populations and experiments were run on a CyanADP (Beckman Coulter) flow cytometer. The platelet population was identified and gated based on its characteristic forward and side scatter light profile [29]. A minimum of 30,000 events were recorded per sample. Analysis of data was performed using FlowJo v10 software (Treestar) and antibody binding was expressed as the percentage of platelets positive for the antibody.
Enzymatic activity of MMP-2 and MMP-9
Zymography is a technique for measuring enzymatic activity that is based on the degradation of their respective substrates [30], thus gelatin zymography measures the activity of the gelatinases MMP-2 and MMP-9. MMP-2 and MMP-9 gelatinolytic activity was analysed as a 3 compartment model–plasma, intraplatelet (platelet lysate) and platelet membrane (platelet homogenate). To prepare platelet lysates 0.2% (w/v) sodium chloride solution at 4°C was added to each platelet pellet, gently resuspended and kept on ice for 10 minutes. For homogenisation Triton 0.1% solution in solubilising buffer was added to each sample. Samples were centrifuged at 4°C for 10 minutes at 13,000rpm after each step and the supernatant (lysate and homogenate) kept at -80C until further used. Protein concentrations were quantified by the Bradford method [31] using the Bio-Rad Protein Assay (Bio-Rad, Alpha Technologies, Ireland). Zymography was performed as described previously [32, 33]. For plasma and lysate samples, 100μg or 30μg of protein per lane respectively, were subjected to 8% sodium dodecylsulfate-polyacrylamide gel electrophoresis (SDS-PAGE) with co-polymerized gelatin. For homogenate samples 7.9μg of protein per lane was used. Following electrophoresis, gels were washed 3 times in 2.5% Triton X-100, twice in developing buffer (50mM Tris-HCl pH 7.6, 150mM NaCl, 5mM CaCl2 and 0.05% NaN3) and incubated overnight at 37°C. Gels were stained in 40% methanol, 10% acetic acid and 0.1% (w/v) Coomassie Blue R-250 and destained in a 4% methanol and 8% acetic acid solution. The resulting gels had “clear bands” corresponding to the gelatinolytic activity of the MMPs against a blue background. The gels were imaged and quantified by scanning densitometry using a gel-documentation system (Gel Doc ™ XR+ system) and Chemidoc software (Biorad, Alpha Technologies, Ireland). The conditioned medium of HT1080 human fibrosarcoma cells was used as MMP-2/MMP-9 standards [16]. Pro- and active- MMP-2/-9 bands were measured together in units of intensity x millimetres.
Imaging of platelet-leukocyte aggregates
Immunohistochemistry (IHC) is an imaging technique based on the binding of antigens to specific antibodies in biological specimens which was used here to image PLAs. Samples of PRP were fixed with a 10% solution of formaldehyde (pH 7.4). Samples were centrifuged and the resulting pellet dehydrated in ethanol and exchanged with xylene. Subsequently, samples were embedded in paraffin and dissected into 4μm sections. For immunohistochemical localization, formalin-fixed tissue sections were treated with 3% hydrogen peroxide. Heat-induced epitope retrieval was performed in sodium citrate buffer solution (10 mM sodium citrate, 0.05% Tween 20, pH 6.0) at 98°C for 30 minutes. Sections were incubated at room temperature with 10 μg/ml of anti-CD62P antibody (Abcam) and washed in Tris-buffered saline (Dako Corporation). For antigen-antibody visualization the Ultra Vision LP Values Detection System (Lab Vision) together with DAB (3,30-diaminobenzidine) (DAKO corporation) were used. Finally, sections were washed and counterstained with Mayer’s haematoxylin.
Enzyme-linked immunosorbent assay (ELISA)
Platelets from healthy controls, septic patients and septic thrombocytopenic patients were prepared as described above and the concentration of MMP-2 and MMP-9 measured in those samples using the Human ELISA Genie MMP-2 and MMP-9 kits (Reagent Genie Ltd, Dublin, Ireland) following the manufacturer instructions. The total protein concentration used for the assay was adjusted for all samples (100μg for plasma; 25 μg for lysate and 2.3 μg for homogenates).
Statistical analysis
Patient data is reported as means or medians as appropriate. Categorical data was compared with Chi-squared tests. For all other results comparison of two groups was with independent samples t-tests or Mann-Whitney U tests. The Shapiro-Wilk test was used to test for normality. One-way analysis of variance (ANOVA) or Kruskal-Wallis (KW) tests were used for comparison of 3 groups, as appropriate, for data that was normally or non-normally distributed. Tukey’s honestly significant difference (HSD) is reported for multiple comparisons post ANOVA. For KW tests if a significant result was found pairwise comparison was performed using Dunn’s procedure with a Bonferroni correction for multiple comparisons and the adjusted p-values are reported. Comparison of 2 paired groups was with paired T-tests. If the data were not normally distributed the Wilcoxon Signed Rank test for related samples was used. Comparison of more than 2 paired groups used repeated measures ANOVA. If the assumption of sphericity was violated the Greenhouse-Geisser correction was applied. All analysis was performed with SPSS v20 software from IBM. A p value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
A total of 26 septic patients were recruited, 31% developed thrombocytopenia either when admitted to the ICU or within 72 hours of admission (Table 2). The most common site of infection was intra-abdominal and the second was lung. Nineteen patients (73%) had a community-acquired infection and 7 a hospital-acquired or healthcare-associated infection. The most commonly identified organisms were gram-positive bacteria (30.8%) followed by gram-negative organisms (26.9%). Healthy controls were mostly male (60%) and had mean age of 40.2 years.
Table 2. Patient Demographics and Clinical characteristics.
| All patients | Non-thrombocytopenic | Thrombocytopenic | P-value for difference | |
|---|---|---|---|---|
| Number | 26 | 18 | 8 | |
| Age | 61.3 | 61 | 61.9 | .873 |
| % Male | 58% | 55.5% | 62.5% | 1.0 |
| APACHE II score | 27.6 | 28 | 26.7 | .552 |
| SOFA score | 12.6 | 10.3 | 11.75 | .125 |
| Survival to ICU discharge | 22/26 (84.6%) |
17/18 (94.4%) |
5/8 (62.5%) |
.072 |
| Survival to hospital discharge | 18/26 (69.2%) |
13/18 (72.2%) |
5/8 (62.5%) |
.667 |
| Median platelet count at admission (per μl) | 264,000 | 309,000 | 173,000 | .944 |
| Median platelet count at sampling (per μl) | 236,500 | 267,000 | 84,000 | .000* |
| Median white cell count at sampling (per μl) | 13,400 | 15,000 | 10,350 | .338 |
Flow cytometry of Platelet MMP-2/-9, TLR-4 and P-selectin expression
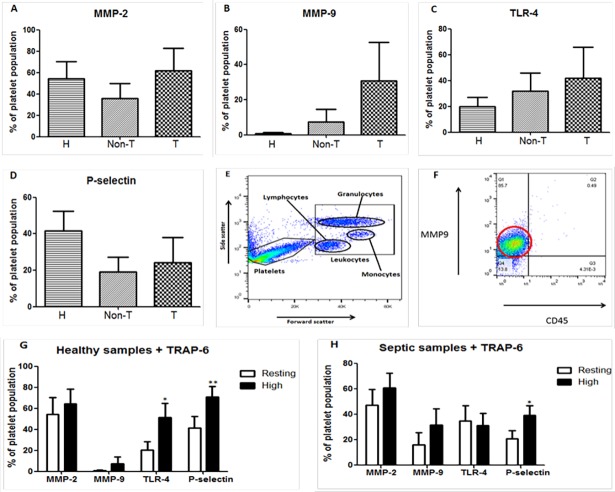
Whole blood samples obtained from patients and healthy subjects were first examined by FC in the absence of stimulation for platelet surface expression of MMP-2/-9, TLR-4 and P-selectin. There were no significant differences found in the platelet surface expression of these 4 proteins between healthy controls and septic donors in any of the analyzed subroups (Fig 1A–1F). Of note, MMP-9 was detected in small amounts in 2 out of 6 healthy control samples. With the addition of TRAP-6, MMP-9 was detected in a further 2 samples. In septic patients MMP-9 was detected in 6 out of the 8 patient samples. If platelet MMP-9 levels in healthy controls are independently compared to thrombocytopenic donors there is a significant increase noted (p = .048).
Fig 1. Flow cytometry (FC) analysis of whole blood samples from healthy controls (H), non-thrombocytopenic septic (Non-T) and septic thrombocytopenic (T) donors.
A–D, Non-significant differences in the platelet surface expression of MMP-2, -9, TLR-4 and P-selectin between the 3 groups represented as the mean plus the standard error of the mean. E, Gating of the platelet population based on characteristic side and forward scatter. F, Representative graph from FC analysis in a thrombocytopenic septic patient demonstrating the presence of MMP-9 on platelets. The signal intensity of the MMP-9 antibody is highlighted by the red circle. In this case 85.7% of the gated platelet population is positive for the presence of MMP-9. G, Response of healthy platelets to agonist TRAP-6 with increased expression of TLR-4 and P-selectin. H, Response of platelets from septic patients to TRAP-6 with increased expression only in P-selectin. Data are mean ± SEM. n = 8 healthy controls, n = 5–9 non-thrombocytopenic donors, n = 3–5 thrombocytopenic donors. *p < 0.05 and **p < 0.01.
The platelet agonist TRAP-6 (25μM) was used to analyse the response of MMP-2, -9, TLR-4 and P-selectin to platelet activation (Fig 1G and 1H). MMP-2 did not increase with the addition of TRAP-6 in neither the healthy nor the septic groups. Similarly, no significant differences in MMP-9 were demonstrated in healthy controls or septic donors. TLR-4 expression was significantly upregulated in healthy controls with the addition of TRAP-6 (p = 0.028) but not in septic patients. Platelet P-selectin increased in both healthy controls (p = 0.002) and septic patients (p = 0.031).
Flow cytometry of PLA formation
As described before, the population of PLAs were examined in whole blood by gating the CD45+/CD62P+ population [34]. When examined as 2 groups—healthy controls and septic patients–no differences were found. However when examined as 3 groups–healthy controls, septic non-thrombocytopenic patients and septic thrombocytopenic patients—significantly more PLAs had developed in the thrombocytopenic patients (p = .038). In a pairwise comparison, only a difference between the septic non-thrombocytopenic and septic thrombocytopenic group (p = .032) was found (Fig 2A). An example of a large PLA taken from a septic thrombocytopenic donor is shown in Fig 2B. In addition, all septic patients were examined according to their survival outcome and the development of PLAs. Although there was a trend towards increased formation of PLAs in non-survivors (mean 8% versus 3.5% in survivors) this was not statistically significant (p = .053).
Fig 2. PLA formation in sepsis.
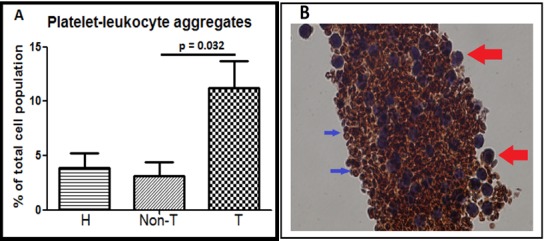
A, Increased PLA formation in the thrombocytopenic (T) group (n = 4) compared to the non-thrombocytopenic (Non-T) group (n = 9); healthy (H) controls (n = 8). B, Immunohistochemical staining of a large PLA from a septic thrombocytopenic donor using a 10x objective lens magnification (100x). In the enhanced picture the large red arrows point to leukocytes and the smaller blue arrows point to platelets. Leukocytes are larger, nucleated and stained violet with haematoxylin. Platelets are smaller, stained with anti-CD62P and are rust in colour.
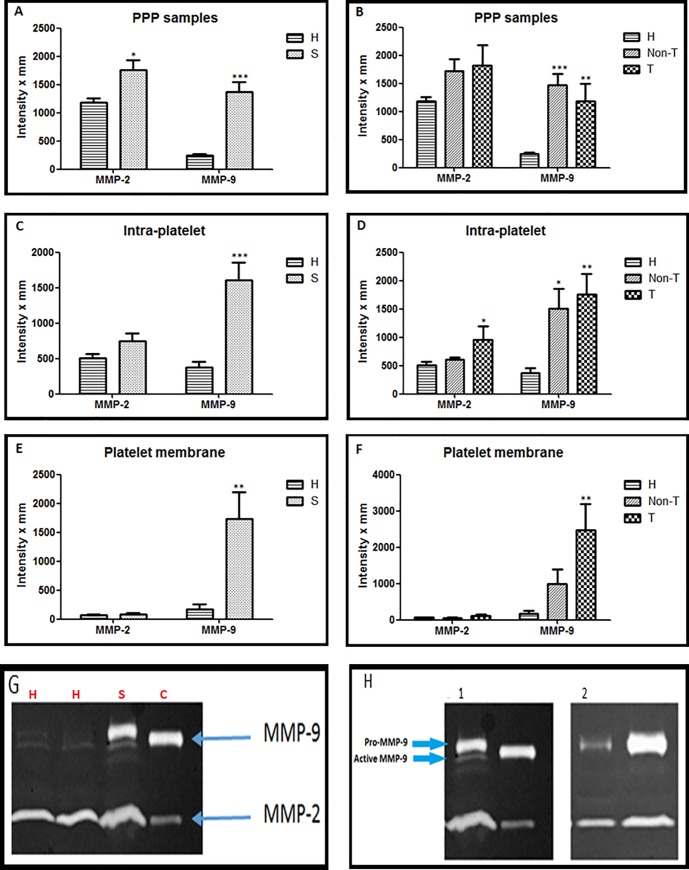
Examination of activity of gelatinases in sepsis using a 3 compartment model
MMP-2 activity was significantly higher in the plasma of septic patients versus healthy controls (Fig 3A). Levels of MMP-2 were similar in non-thrombocytopenic and thrombocytopenic patients (Fig 3B). MMP-9 activity in plasma was higher in septic patients compared to controls with no differences between the non-thrombocytopenic and thrombocytopenic patients (Fig 3B). Although intra-platelet MMP-2 activity was not modified when healthy controls and septic donors were compared, when examined as 3 groups it was significantly higher in the thrombocytopenic group (Fig 3C and 3D). Intra-platelet MMP-9 activity was higher in septic patients than controls, with similar activity in non-thrombocytopenic and thrombocytopenic patients (Fig 3C and 3D). Platelet membrane samples showed low activity of MMP-2 in both healthy and septic groups (Fig 3E and 3F). However, there was a significantly higher activity of MMP-9 found in the platelet membranes of septic patients compared to healthy controls with no differences between the non-thrombocytopenic and thrombocytopenic patients (Fig 3E and 3F). Plasma levels of MMP-2 and -9 in septic patients were compared based upon their survival and significantly higher MMP-9 levels were found in non-survivors (Fig 4).
Fig 3. Examination of the activity of MMP-2 and -9 by gelatin zymography in septic shock as a 3 compartment model.
Results are shown firstly as both healthy controls (H) and septic patients (S) and then with the septic patients categorised as non-thrombocytopenic (Non-T) and thrombocytopenic (T) patients. A and B, PPP samples at protein concentration (100μg/lane)–H (n = 20), Non-T (n = 13) and T (n = 7). C and D, Intraplatelet or lysate samples at protein concentration 30μg/lane–H (n = 10), Non-T (n = 7) and T (n = 5). E and F, Homogenate or plasma membrane samples at maximal protein concentration of 7.9 μg/lane–H (n = 9), Non-T (n = 5) and T (n = 5). G, Representative gel zymography showing both healthy controls (lane 1 and 2) and septic donors (lane 3); control = lane 4 (HT1080 media). H, Zymography gels. 1 shows PPP sample on the left lane and positive control on the right lane. On the left lane, a small band can be seen directly under the upper line. This small line corresponds to the active MMP-9 (82 kDa). This line is not visible in 2, where lysate samples of septic patients were evaluated. Data are mean ± SEM. Results are compared to healthy controls *p < 0.05, **p < 0.01 and ***p < 0.001.
Fig 4. Survival outcomes.
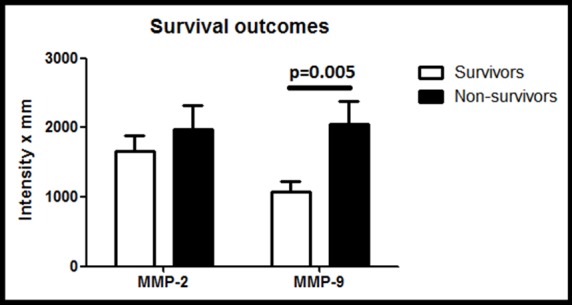
Plasma levels of MMP-9 were significantly higher in non-survivors (n = 6) compared to survivors (n = 14) (p = 0.005). No association was found between MMP-2 levels in PPP and mortality (p = 0.477).
To confirm our findings a series of ELISA experiments were performed using a small group of donors–healthy controls (n = 3), non-thrombocytopenic septic donors (n = 3) and thrombocytopenic septic donors (n = 3). Regarding MMP-2, as per the GZ results there was no significant difference in the intraplatelet and platelet membrane levels of MMP-2 between healthy controls and septic donors. An increase in plasma levels of MMP-2 in septic shock was not found using this technique. However, the presence of MMP-9 in platelets was confirmed with significant differences in the plasma (p = .016) and intraplatelet (p = .029) levels of MMP-9 in septic patients as compared to healthy controls. Contrary to the GZ findings platelet membrane expression of MMP-9 was not elevated in septic patients as compared to healthy controls. No significant difference was found between the non-thrombocytopenic and thrombocytopenic donors in MMP-2/-9 values in plasma, platelet membrane or intraplatelet compartment when examined with ELISA.
Discussion
Given the significance of the development of thrombocytopenia in sepsis, approximately doubling the expected mortality, should the mechanism underlying SAT be clarified, it is likely that this would represent an appropriate target for the treatment of sepsis. The expression and activity of MMP-2 and MMP-9 was examined in patients with septic shock by FC and using a 3 compartment model (plasma, intraplatelet and platelet membrane) by gelatin zymography. Interestingly, both MMP-2 (in contrast to prior studies [35–37]) and MMP-9 were found to be increased in the plasma of septic patients. Importantly, higher levels of MMP-9, but not MMP-2, were found in plasma of patients who did not survive sepsis.
The presence of MMP-9 on platelets has been confirmed in this study under the conditions tested. In contrast to previous studies [38], we have detected platelet surface expression of MMP-9 in unstimulated whole blood samples by FC in 2 out of 6 healthy controls and 6 out of 8 septic donors. Sheu et al have previously shown intraplatelet expression of MMP-9 using immunogold labelling and electron microscopy [18]. Additionally we have demonstrated the presence of MMP-9 in platelets using zymography and ELISA techniques. It has been demonstrated that MMP-9 secretion from leukocytes significantly increases during inflammation and sepsis. Our findings suggest that platelet expression of MMP-9 is also upregulated in sepsis. In three studies where MMP-9 was not expressed by platelets, small groups of healthy controls were studied [17, 19, 39]. These differences in study populations may also account for some of the conflicting data from the literature. It was notable that when platelets were examined for the response to the platelet agonist TRAP-6, no significant increased level of MMP-9 was found. It may be that platelet expression of the gelatinases MMP-2 and -9 are independent of the PAR-1/PAR-4 platelet activation pathway [40].
Studies in larger cohorts have previously demonstrated increased platelet TLR-4 expression in patients suffering from sepsis [41]. Although platelet TLR-4 was not found to be upregulated in septic patients in this study, there appeared to be a trend of increased expression especially in the thrombocytopenic group. Two previous studies using genetically modified mice have demonstrated that TLR-4 deficiency attenuates lipopolysaccharide induced thrombocytopenia [21, 22]. The proposal that sepsis-associated thrombocytopenia is mediated via stimulation of TLR-4 receptors in platelets could not be corroborated in our study and it may be due to differences between humans and mice in the modulation of TLR expression [21]. We found that the addition of TRAP-6 increased TLR-4 expression on platelets in healthy controls but not in septic patients, possibly because TLR-4 expression had already been upregulated in this population. This finding is interesting as increased TLR-4 platelet expression in response to a platelet agonist has not been reported previously.
P-selectin expression was not found to be upregulated in septic patients. It has become increasingly recognised that PLAs are a better indicator of platelet activation in vivo than P-selectin platelet surface expression [42, 43]. We found an increased proportion of circulating PLAs in thrombocytopenic patients suggesting that consumption of a proportion of the circulating platelet population into PLAs could contribute to sepsis-associated thrombocytopenia. Interestingly, there is evidence that the release of MMPs such as MMP-2 and MMP-9 promotes generation of PLAs [34]. The role of PLAs in the pathophysiology of sepsis is unclear. Some authors have concluded that PLA formation is likely a significant pathological event contributing to microthrombi formation and the dysregulation of the microvasculature that is pathognomonic of sepsis [26, 44].
The main limitation of this study may be the small samples sizes involved as a result of the strict exclusion criteria employed. However, in order to capture clinically relevant findings in investigations we believe it is a better approach to apply stricter recruitment criteria despite the attendant problems with recruitment.
Conclusions
Based on our results we believe that the consumption of platelets into platelet-leukocyte aggregates may contribute to a decline in platelet numbers in septic shock and therefore to the development of sepsis-associated thrombocytopenia. MMP-9 is found in platelets and may be an inducible enzyme in this setting.
Supporting information
(XLSX)
Acknowledgments
We thank the Intensive Care Society of Ireland (www.intensivecare.ie), Abbvie (www.abbvie.ie) and Merck Sharpe Dohme (www.msd-ireland.com) for their support of this study and Niamh Buckley, Patrick Collins, Brona Staunton and Louise Walsh for their assistance. Nadhim Kamil Hante is funded by the Ministry of Higher Education (MoHER) from Iraq.
Institutions
The study was undertaken in the Intensive Care Unit of St James’s hospital, Dublin, Ireland and the laboratory facilities of the School of Pharmacy and Pharmaceutical Sciences and Trinity Biomedical Sciences Institute, Trinity College Dublin, Dublin, Ireland.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Reagents for this study were purchased from funding received from the Intensive Care Society of Ireland, Abbvie and Merck Sharpe Dohme. None of the investigators were renumerated for their work on the study. Nadhim Kamil Hante is funded by the Ministry of Higher Education (MoHER) from Iraq. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Strauss R, Wehler M, Mehler K, Kreutzer D, Koebnick C, Hahn EG. Thrombocytopenia in patients in the medical intensive care unit: bleeding prevalence, transfusion requirements, and outcome. Critical care medicine. 2002;30(8):1765–71. Epub 2002/08/07. . [DOI] [PubMed] [Google Scholar]
- 2.Martin CM, Priestap F, Fisher H, Fowler RA, Heyland DK, Keenan SP, et al. A prospective, observational registry of patients with severe sepsis: the Canadian Sepsis Treatment and Response Registry. Critical care medicine. 2009;37(1):81–8. Epub 2008/12/04. doi: 10.1097/CCM.0b013e31819285f0 . [DOI] [PubMed] [Google Scholar]
- 3.Aydemir H, Piskin N, Akduman D, Kokturk F, Aktas E. Platelet and mean platelet volume kinetics in adult patients with sepsis. Platelets. 2012. Epub 2012/06/27. doi: 10.3109/09537104.2012.701027 . [DOI] [PubMed] [Google Scholar]
- 4.Horino T, Chiba A, Kawano S, Kato T, Sato F, Maruyama Y, et al. Clinical characteristics and risk factors for mortality in patients with bacteremia caused by Pseudomonas aeruginosa. Internal medicine (Tokyo, Japan). 2012;51(1):59–64. Epub 2012/01/05. . [DOI] [PubMed] [Google Scholar]
- 5.Azkarate I, Sebastian R, Cabarcos E, Choperena G, Pascal M, Salas E. [A prospective, observational severe sepsis/septic shock registry in a tertiary hospital in the province of Guipuzcoa (Spain)]. Medicina intensiva / Sociedad Espanola de Medicina Intensiva y Unidades Coronarias. 2012;36(4):250–6. Epub 2011/12/14. doi: 10.1016/j.medin.2011.10.006 . [DOI] [PubMed] [Google Scholar]
- 6.Sharma B, Sharma M, Majumder M, Steier W, Sangal A, Kalawar M. Thrombocytopenia in septic shock patients—a prospective observational study of incidence, risk factors and correlation with clinical outcome. Anaesthesia and intensive care. 2007;35(6):874–80. Epub 2007/12/19. . [DOI] [PubMed] [Google Scholar]
- 7.Cohen P, Gardner FH. Thrombocytopenia as a laboratory sign and complication of gram-negative bacteremic infection. Archives of internal medicine. 1966;117(1):113–24. Epub 1966/01/01. . [PubMed] [Google Scholar]
- 8.Vandijck DM, Blot SI, De Waele JJ, Hoste EA, Vandewoude KH, Decruyenaere JM. Thrombocytopenia and outcome in critically ill patients with bloodstream infection. Heart & lung: the journal of critical care. 2010;39(1):21–6. Epub 2010/01/30. doi: 10.1016/j.hrtlng.2009.07.005 . [DOI] [PubMed] [Google Scholar]
- 9.Bessman JD, Gardner FH. Platelet size in thrombocytopenia due to sepsis. Surgery, gynecology & obstetrics. 1983;156(2):177–80. Epub 1983/02/01. . [PubMed] [Google Scholar]
- 10.de Stoppelaar SF, van 't Veer C, van der Poll T. The role of platelets in sepsis. Thrombosis and haemostasis. 2014;112(2). Epub 2014/06/27. doi: 10.1160/th14-02-0126 . [DOI] [PubMed] [Google Scholar]
- 11.Segre E, Pigozzi L, Lison D, Pivetta E, Bosco O, Vizio B, et al. May thrombopoietin be a useful marker of sepsis severity assessment in patients with SIRS entering the emergency department? Clinical chemistry and laboratory medicine: CCLM / FESCC. 2014;52(10):1479–83. Epub 2014/06/03. doi: 10.1515/cclm-2014-0219 . [DOI] [PubMed] [Google Scholar]
- 12.Zakynthinos SG, Papanikolaou S, Theodoridis T, Zakynthinos EG, Christopoulou-Kokkinou V, Katsaris G, et al. Sepsis severity is the major determinant of circulating thrombopoietin levels in septic patients. Critical care medicine. 2004;32(4):1004–10. Epub 2004/04/09. . [DOI] [PubMed] [Google Scholar]
- 13.Page-McCaw A, Ewald AJ, Werb Z. Matrix metalloproteinases and the regulation of tissue remodelling. Nature reviews Molecular cell biology. 2007;8(3):221–33. Epub 2007/02/24. doi: 10.1038/nrm2125 ; PubMed Central PMCID: PMCPMC2760082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sawicki G, Salas E, Murat J, Miszta-Lane H, Radomski MW. Release of gelatinase A during platelet activation mediates aggregation. Nature. 1997;386(6625):616–9. Epub 1997/04/10. doi: 10.1038/386616a0 . [DOI] [PubMed] [Google Scholar]
- 15.Choi WS, Jeon OH, Kim HH, Kim DS. MMP-2 regulates human platelet activation by interacting with integrin alphaIIbbeta3. Journal of thrombosis and haemostasis: JTH. 2008;6(3):517–23. Epub 2007/12/20. doi: 10.1111/j.1538-7836.2007.02871.x . [DOI] [PubMed] [Google Scholar]
- 16.Fernandez-Patron C, Martinez-Cuesta MA, Salas E, Sawicki G, Wozniak M, Radomski MW, et al. Differential regulation of platelet aggregation by matrix metalloproteinases-9 and -2. Thrombosis and haemostasis. 1999;82(6):1730–5. Epub 1999/12/29. . [PubMed] [Google Scholar]
- 17.Wrzyszcz A, Wozniak M. On the origin of matrix metalloproteinase-2 and -9 in blood platelets. Platelets. 2012;23(6):467–74. Epub 2012/06/01. doi: 10.3109/09537104.2012.682103 . [DOI] [PubMed] [Google Scholar]
- 18.Sheu JR, Fong TH, Liu CM, Shen MY, Chen TL, Chang Y, et al. Expression of matrix metalloproteinase-9 in human platelets: regulation of platelet activation in in vitro and in vivo studies. British Journal of Pharmacology. 2004;143(1):193–201. Epub 2004/08/04. doi: 10.1038/sj.bjp.0705917 ; PubMed Central PMCID: PMCPMC1575278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalvegren H, Jonsson S, Jonasson L. Release of matrix metalloproteinases-1 and -2, but not -9, from activated platelets measured by enzyme-linked immunosorbent assay. Platelets. 2011;22(8):572–8. Epub 2011/07/16. doi: 10.3109/09537104.2011.583300 . [DOI] [PubMed] [Google Scholar]
- 20.Gay NJ, Symmons MF, Gangloff M, Bryant CE. Assembly and localization of Toll-like receptor signalling complexes. Nature reviews Immunology. 2014;14(8):546–58. Epub 2014/07/26. doi: 10.1038/nri3713 . [DOI] [PubMed] [Google Scholar]
- 21.Aslam R, Speck ER, Kim M, Crow AR, Bang KW, Nestel FP, et al. Platelet Toll-like receptor expression modulates lipopolysaccharide-induced thrombocytopenia and tumor necrosis factor-alpha production in vivo. Blood. 2006;107(2):637–41. Epub 2005/09/24. doi: 10.1182/blood-2005-06-2202 . [DOI] [PubMed] [Google Scholar]
- 22.Andonegui G, Kerfoot SM, McNagny K, Ebbert KV, Patel KD, Kubes P. Platelets express functional Toll-like receptor-4. Blood. 2005;106(7):2417–23. Epub 2005/06/18. doi: 10.1182/blood-2005-03-0916 . [DOI] [PubMed] [Google Scholar]
- 23.Zhang G, Han J, Welch EJ, Ye RD, Voyno-Yasenetskaya TA, Malik AB, et al. Lipopolysaccharide stimulates platelet secretion and potentiates platelet aggregation via TLR4/MyD88 and the cGMP-dependent protein kinase pathway. Journal of immunology (Baltimore, Md: 1950). 2009;182(12):7997–8004. Epub 2009/06/06. doi: 10.4049/jimmunol.0802884 ; PubMed Central PMCID: PMCPMC2787095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cerletti C, Tamburrelli C, Izzi B, Gianfagna F, de Gaetano G. Platelet-leukocyte interactions in thrombosis. Thrombosis research. 2012;129(3):263–6. Epub 2011/11/15. doi: 10.1016/j.thromres.2011.10.010 . [DOI] [PubMed] [Google Scholar]
- 25.Johansson D, Shannon O, Rasmussen M. Platelet and neutrophil responses to Gram positive pathogens in patients with bacteremic infection. PloS one. 2011;6(11):e26928 Epub 2011/12/06. doi: 10.1371/journal.pone.0026928 ; PubMed Central PMCID: PMCPMC3226579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kirschenbaum LA, Aziz M, Astiz ME, Saha DC, Rackow EC. Influence of rheologic changes and platelet-neutrophil interactions on cell filtration in sepsis. American journal of respiratory and critical care medicine. 2000;161(5):1602–7. Epub 2000/05/12. doi: 10.1164/ajrccm.161.5.9902105 . [DOI] [PubMed] [Google Scholar]
- 27.Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Critical care medicine. 2013;41(2):580–637. Epub 2013/01/29. doi: 10.1097/CCM.0b013e31827e83af . [DOI] [PubMed] [Google Scholar]
- 28.Radomski M, Moncada S. An improved method for washing of human platelets with prostacyclin. Thrombosis research. 1983;30(4):383–9. Epub 1983/05/15. . [DOI] [PubMed] [Google Scholar]
- 29.Shattil SJ, Cunningham M, Hoxie JA. Detection of activated platelets in whole blood using activation-dependent monoclonal antibodies and flow cytometry. Blood. 1987;70(1):307–15. Epub 1987/07/01. . [PubMed] [Google Scholar]
- 30.Gross J, Lapiere CM. Collagenolytic activity in amphibian tissues: a tissue culture assay. Proceedings of the National Academy of Sciences of the United States of America. 1962;48:1014–22. Epub 1962/06/15. ; PubMed Central PMCID: PMCPMC220898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Analytical biochemistry. 1976;72:248–54. Epub 1976/05/07. . [DOI] [PubMed] [Google Scholar]
- 32.Medina C, Jurasz P, Santos-Martinez MJ, Jeong SS, Mitsky T, Chen R, et al. Platelet aggregation-induced by caco-2 cells: regulation by matrix metalloproteinase-2 and adenosine diphosphate. The Journal of pharmacology and experimental therapeutics. 2006;317(2):739–45. Epub 2006/01/21. doi: 10.1124/jpet.105.098384 . [DOI] [PubMed] [Google Scholar]
- 33.Bazou D, Santos-Martinez M, Medina C, Radomski M. Elucidation of flow-mediated tumour cell-induced platelet aggregation using an ultrasound standing wave trap. British Journal of Pharmacology. 2011;162(7):1577–89. doi: 10.1111/j.1476-5381.2010.01182.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chung AWY, Radomski A, Alonso-Escolano D, Jurasz P, Stewart MW, Malinski T, et al. Platelet–leukocyte aggregation induced by PAR agonists: regulation by nitric oxide and matrix metalloproteinases. British Journal of Pharmacology. 2004;143(7):845–55. doi: 10.1038/sj.bjp.0705997 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Muhl D, Nagy B, Woth G, Falusi B, Bogar L, Weber G, et al. Dynamic changes of matrix metalloproteinases and their tissue inhibitors in severe sepsis. Journal of critical care. 2011;26(6):550–5. Epub 2011/05/03. doi: 10.1016/j.jcrc.2011.02.011 . [DOI] [PubMed] [Google Scholar]
- 36.Albert J, Radomski A, Soop A, Sollevi A, Frostell C, Radomski MW. Differential release of matrix metalloproteinase-9 and nitric oxide following infusion of endotoxin to human volunteers. Acta anaesthesiologica Scandinavica. 2003;47(4):407–10. Epub 2003/04/16. . [DOI] [PubMed] [Google Scholar]
- 37.Hoffmann U, Bertsch T, Dvortsak E, Liebetrau C, Lang S, Liebe V, et al. Matrix-metalloproteinases and their inhibitors are elevated in severe sepsis: prognostic value of TIMP-1 in severe sepsis. Scandinavian journal of infectious diseases. 2006;38(10):867–72. Epub 2006/09/30. doi: 10.1080/00365540600702058 . [DOI] [PubMed] [Google Scholar]
- 38.Seizer P, May AE. Platelets and matrix metalloproteinases. Thrombosis and haemostasis. 2013;110(5):903–9. Epub 2013/07/19. doi: 10.1160/TH13-02-0113 . [DOI] [PubMed] [Google Scholar]
- 39.Galt SW, Lindemann S, Allen L, Medd DJ, Falk JM, McIntyre TM, et al. Outside-in signals delivered by matrix metalloproteinase-1 regulate platelet function. Circulation research. 2002;90(10):1093–9. Epub 2002/06/01. . [DOI] [PubMed] [Google Scholar]
- 40.Soslau G, Mason C, Lynch S, Benjamin J, Ashak D, Prakash JM, et al. Intracellular matrix metalloproteinase-2 (MMP-2) regulates human platelet activation via hydrolysis of talin. Thrombosis and haemostasis. 2014;111(1):140–53. Epub 2013/10/19. doi: 10.1160/TH13-03-0248 . [DOI] [PubMed] [Google Scholar]
- 41.Wang B, Wang YQ, Cao SH, Liang Y. [Platelet parameters and platelet Toll-like receptor 4 (TLR4) expression in patients with sepsis, and the effect of a joint treatment-plan integrating traditional Chinese and western medicine: a clinical study]. Zhongguo wei zhong bing ji jiu yi xue = Chinese critical care medicine = Zhongguo weizhongbing jijiuyixue. 2011;23(10):616–20. Epub 2011/10/19. . [PubMed] [Google Scholar]
- 42.Michelson AD, Barnard MR, Krueger LA, Valeri CR, Furman MI. Circulating monocyte-platelet aggregates are a more sensitive marker of in vivo platelet activation than platelet surface P-selectin: studies in baboons, human coronary intervention, and human acute myocardial infarction. Circulation. 2001;104(13):1533–7. Epub 2001/09/26. . [DOI] [PubMed] [Google Scholar]
- 43.Hurley SM, Lutay N, Holmqvist B, Shannon O. The Dynamics of Platelet Activation during the Progression of Streptococcal Sepsis. PloS one. 2016;11(9):e0163531 Epub 2016/09/23. doi: 10.1371/journal.pone.0163531 ; PubMed Central PMCID: PMCPMC5033464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gawaz M, Dickfeld T, Bogner C, Fateh-Moghadam S, Neumann FJ. Platelet function in septic multiple organ dysfunction syndrome. Intensive care medicine. 1997;23(4):379–85. Epub 1997/04/01. . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.