Abstract
Over the last decades, the treatment of schizophrenia has shifted fundamentally from a focus on symptom reduction to a focus on recovery and improving aspects of functioning. In this study, we examined the effect of transcranial direct current stimulation (tDCS) on social cognitive and nonsocial neurocognitive functions, as well as on electroencephalogram (EEG) measures, in individuals with schizophrenia. Thirty-seven individuals with schizophrenia were administered one of three different tDCS conditions (cathodal, anodal, and sham) per visit over the course of three visits, with approximately one week between each visit. Order of conditions was randomized and counterbalanced across subjects. For the active conditions, the electrode was placed over the left dorsolateral prefrontal cortex with the reference electrode over right supraorbital cortex. Current intensity was 2 mA and was maintained for two 20-minute sessions, with a one hour break between the sessions. Assessments were conducted immediately following each session, in a counterbalanced order of administration. No systematic effects were found across the social and nonsocial cognitive domains, and no significant effects were detected on event-related potentials (ERPs). The very small effect sizes, further validated by post-hoc power analyses (large Critical Ns), demonstrated that these findings were not due to lack of statistical power. Except for mild local discomfort, no significant side effects were reported. Findings demonstrate the safety and ease of administration of this procedure, but suggest that a single dose of tDCS over these areas does not yield a therapeutic effect on cognition in schizophrenia.
Trial registration: ClinicalTrials.gov NCT02539797.
Introduction
Considerable evidence indicates that cognitive factors are key determinants of functional outcome for schizophrenia [1–3]. These cognitive factors can be divided into neurocognition and social cognition. Neurocognition refers to a wide range of performance abilities in domains such as learning and memory, vigilance / attention, speed of processing, reasoning and problem solving, and working memory [4, 5]. Social cognition refers to cognitive abilities that are needed to perceive, interpret, and process social information and include domains such as emotion perception, social context processing, attributional bias, and theory of mind [6, 7]. Both neurocognitive and social cognitive deficits have been extensively documented in schizophrenia literature and are considered a core feature of the illness [8–10].
In addition to the considerable efforts in recent years to stimulate the development of cognition-enhancing drugs [11, 12], other approaches to enhance patients’ cognitive functions have been explored. Neurostimulation has advantages over pharmacological therapy in reducing many potentially dangerous systemic side effects. Currently transcranial direct current stimulation (tDCS) has been developed as non-invasive tool using neurostimulation to treat epilepsy [13]. Unlike other non-invasive brain stimulation techniques, such as transcranial electrical stimulation or transcranial magnetic stimulation, tDCS does not induce neuronal firing by suprathreshold neuronal membrane depolarization but rather modulates spontaneous neuronal network activity [14]. In a review of 567 tDCS sessions administered over cortical areas on a total of 102 healthy participants and patients, none requested the stimulation to be terminated or needed any medical intervention during or after tDCS administration [15].
Despite the safety and tolerability of this procedure, findings regarding its potential clinical benefits in schizophrenia have been mixed. Early studies of single tDCS administration in schizophrenia reported positive effects [16–18]. For example, Brunelin et al. (2012) reported preliminary data showing that bifocal stimulation (anodal over DLPFC and cathodal over tempo-parietal cortex) improved scores on measures of auditory hallucinations and overall positive and negative symptoms in 2 patients with refractory schizophrenia. The clinical efficacy appeared immediately after stimulation sessions and was maintained or continued to improve during at least 3 months. The authors noted that no adverse events were reported, and that the two patients only described a transient mild tingling or a slight itching sensation associated with the onset of stimulation, thereby confirming the safety of this technique [16]. Additionally, Vercammen et al. (2011) examined whether anodal tDCS to the left DLPFC would reverse probabilistic association learning deficits in 20 individuals with schizophrenia. The authors reported no adverse effects following the procedure and demonstrated a beneficial effect of tDCS on performance, as assessed by the weather prediction test, in a subsets of individuals [19].
Other studies, however, reported negative findings. For example, in two randomized, double-blind, controlled trials, Fitzerald et al. (2014), examined the effects of unilateral and bilateral tDCS (anodal stimulation to the prefrontal cortex and cathodal stimulation to the temporoparietal junction) in patients with persistent hallucinations and negative symptoms of schizophrenia. They reported that, despite the tolerability of the procedure, neither unilateral nor bilateral tDCS resulted in a substantial change in either hallucinations or negative symptoms [20]. Mattai et al. (2011) investigated the tolerability aspects of tDCS in childhood-onset schizophrenia. The investigators administered bilateral anodal DLPFC stimulation or bilateral cathodal superior temporal gyrus (STG) stimulation to children between the ages 10–17. While demonstrating the safety and tolerability of this procedure in a pediatric population, no changes in cognitive measures in favor of any stimulation condition were observed [21].
The present study was an effort to evaluate the effect of single tDCS administration in schizophrenia on a broad range of social cognitive, nonsocial neurocognitive, and EEG measures. We employed a commonly used montage in cognitive enhancement tDCS studies over the course of three sessions, with approximately one week between each session: anodal tDCS over left DLPFC (cathodal over right supraorbital), cathodal tDCS over left DLPFC (anodal over right supraorbital), and sham stimulation. Using a reasonably well-powered cross-over design, we sought to detect a differential effect of these types of stimulation on performance-based tasks and brainwave activity that are mediated by frontal brain regions.
Material and methods
Participants
Participant recruitment and follow-up were conducted between May 2015 and July 2016. As described in detail previously [15, 17], participants were recruited by placing ads and receiving referrals from treating clinicians at outpatient clinics at the UCLA and the VA Greater Los Angeles Healthcare System and through presentations in the community. All patients were administered the Structured Clinical Interview for DSM-IV (SCID-P) [22]. All interviewers were trained to administer the SCID by the Diagnostic Core of the Mental Illness Research, Education, and Clinical Center (MIRECC) Treatment Unit, and were required to obtain a Kappa of 0.75 for key psychotic and mood items before proceeding to interview participants independently. Participants were included if they met the DSM-IV diagnostic criteria for Schizophrenia or Schizoaffective Disorder [23], were between the ages of 18–55, were able to understand spoken English sufficiently to comprehend testing procedures, and were under the current ongoing care of a psychiatrist, psychologist, or other qualified mental health professional. Patients were excluded if they had an identifiable neurological condition, metal in the cranium, intracardiac lines, cardiac pacemaker, medication pump, or increased intracranial pressure, psychiatric inpatient hospitalization in the last three months, substantial changes in their antipsychotic medications during the previous 6 weeks, IQ < 70 based on reading ability, or met criteria for substance dependence in the last six months.
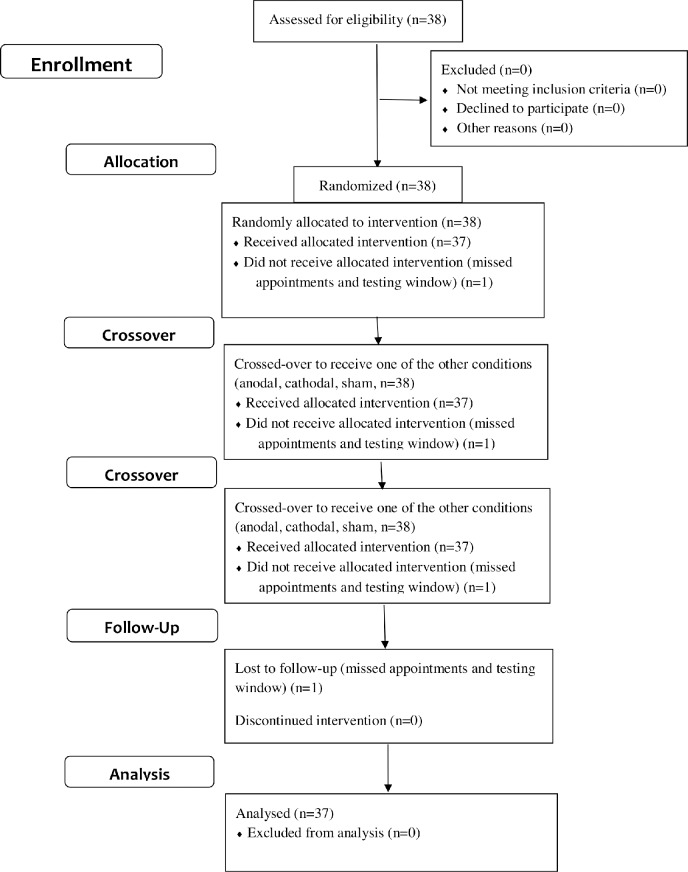
The present study included 38 individuals (one participant was lost to follow-up after missing several appointments and testing window; see Fig 1) with schizophrenia or schizoaffective disorder (68% males), all receiving antipsychotic medications (93% atypical). Mean age was 42.7 (SD = 8.57; range = 23–55), mean participants’ education was 12.8 (SD = 2.11; range = 8–18), and mean paternal education was 13.6 (SD = 3.51; range = 3–20). Patients’ mean illness chronicity was 20.1 years (SD = 9.54; range = 3–43). Mean symptom ratings on the Brief Psychiatric Rating Scale (BPRS) was 42.1 (SD = 12.0; range = 25–77) and on the Scale for the Assessment of Negative Symptoms (SANS) was 41.0 (SD = 16.0; range = 13–80). All participants gave written informed consent after receiving a full explanation of the research according to procedures approved by the UCLA and the VA Greater Los Angeles Healthcare System Institutional Review Boards. The approved protocol is included in supporting information (see S1 Protocol). The trial was registered at www.ClinicalTrials.gov (NCT02539797). The authors confirm that all ongoing and related trials for this intervention are registered.
Fig 1. CONSORT flow chart.
Assessments
Symptom ratings were collected using the expanded BPRS [24] and the SANS [25]. Standardized social cognitive and nonsocial cognitive assessments included a number of primary measures that have been used in schizophrenia research [7]. Participants also rated on a 5-point Likert scale (ranging from none to severe; 0–4) common side effects that are typically reported following tDCS administration [15, 17]. The measures administered are listed in Table 1 and are described fully below.
Table 1. Measure administered to assess the effect of stimulation.
| Social Cognitive Measures |
| MSCEIT |
| EIT |
| TASIT |
| EAT |
| Nonsocial Cognitive Measures |
| MCCB |
| EEG Measures |
| MMN |
| P300 |
| N170 |
MSCEIT: Mayer-Salovey-Caruso Emotional Intelligence Test; EIT: Emotion Identification Test; TASIT: The Awareness of Social Inference Test; EAT: Emphatic Accuracy Task; MCCB: MATRICS Consensus Cognitive Battery; EEG: Electroencephalogram; MMN: Mismatch Negativity; The order of assessments was fully counter-balanced across subjects.
Social cognitive measures
Managing Emotions component of Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT) [26] consists of 141 items and 8 ability subtests, which assess four components of emotional processing. In this study, only branches 1 and 4 were administered, focusing on the Managing Emotions component. Emotion Identification Test (EIT) from the Ekman Program is a test of identification of facial emotion based on photographs from the software developed by Ekman [27]. It includes 56 color photographs of eight different individuals displaying facial expressions of six basic emotions (happy, sad, angry, afraid, surprised, and disgusted). The Awareness of Social Inference Test (TASIT) [28] consists of 16 videotaped scenes with two or three actors appearing in each scene. The scenes involve two types of conversational exchanges, enacted as either a lie (a white lie or a sympathetic one) or sarcasm. After each scene, participants answer questions (yes/no) about the actors’ communicative intentions, such as whether the actors wanted the literal or nonliteral meaning of their messages to be believed. The Empathic Accuracy Task (EAT) [29] assesses the accuracy of empathic judgments using 12 video clips (six positive and six negative events), in which individuals (referred to as “targets”) discuss a positive or negative autobiographical event. As participants watch the clip, they use a 9-point scale to continuously rate how positive or negative they believe the target was feeling at each moment.
Nonsocial neurocognitive measures
The neurocognitive assessment consisted of the MATRICS Consensus Cognitive Battery (MCCB), which assesses seven separate cognitive subdomains, including one measure of social cognition, the managing emotions component of the MSCEIT [4, 30, 31]. Given the diminishing tDCS effect over time [32], we included four nonsocial neurocognitive tasks: speed of processing, working memory, verbal memory, and reasoning/problem solving. Normed T scores were calculated for each cognitive subdomain, as well as the cognitive composite score consisting of the average across the four subdomains.
EEG measures
EEG was acquired with a Neuroscan NuAmps amplifier (Compumedics USA, El Paso, Texas) continuously throughout the session. Data were sampled at 1000 Hz from DC to 100 Hz. Nineteen cap-mounted Ag-AgCl electrodes were positioned using a modified international 10–20 system placement scheme. Additionally, 2 electrodes were used to measure vertical electro-oculogram (placed above and below the left eye) and used in eyeblink correction [33]. All electrodes were referenced to the mastoids, unless otherwise noted.
Mismatch negativity (MMN) was measured using a passive attention auditory duration deviant paradigm. Subjects were presented with binaural tones (1 kHz 85 dB sound pressure level, with 10 ms rise/fall). Standard (90% probability; 50 ms duration) and duration-deviant (10% probability; 100 ms duration) tones were presented in a fixed, pseudorandom order. Full details regarding stimulus presentation and EEG recording and analysis are presented elsewhere [34]. The mean amplitude between 135–205 ms of the deviant-standard difference wave was calculated at electrode Fz.
Following MMN, P300 wave was measured using an active attention auditory oddball paradigm. Subjects were presented with standard (88% probability; 1 kHz frequency; 100 ms duration) and target (12% probability; 1.5 kHz frequency; 100 ms duration) tones. They were instructed to pay attention to the stimulus stream and press a button when they heard the high-pitched tone (infrequent target stimulus) while disregarding the low-pitched tone (standard stimulus). The peak amplitude between 300–600 ms at electrode Pz was extracted and analyzed for oddball stimuli.
The N170 wave was based on a modified procedure we previously developed, where details of recording and analyses are provided [35, 36]. Briefly, in separate blocks, participants viewed either faces or buildings. For faces [37], participants had to determine the emotion displayed (afraid, angry, ashamed, happy, sad, or surprised); for buildings, they had to determine if they were 1 or 2 stories tall. The EEG was re-referenced to the grand average of the 19 electrodes. The mean amplitude between 140–180 ms was averaged across electrodes P7 and P8 for faces and buildings.
Electrical stimulation
As described in detail previously [17], the tDCS was delivered by an Activa Dose II Iontophoresis Delivery Unit (IOMED, Inc), using a pair of saline-soaked sponge electrodes held in place by elastic bands. The 5 x 7 cm active electrode (anodal or cathodal) was placed over the left DLPFC (F3 EEG site), with the 5 x7 cm reference electrode over the right supraorbital cortex (Fp2 EEG site), in accordance with the 10/20 International System [38]. The current intensity was set at 2 mA with a current density of 0.057 mA/cm2 at the skin at each electrode. A variable resistor was included in series with each active electrode, which allowed for continuous monitoring of current delivered and ensured that equivalent intensity balanced at 1 mA per active electrode. In the sham condition, the current was turned on for 30 seconds and then ramped down to 0 mA. In this way, the participants experience the same initial sensation of mild tingling, thus preserving the sham manipulation [15]. The research assistants administering the procedure were not blinded to the stimulation condition.
Procedures
We used a cross-over counter-balanced design. Participants came for three visits, approximately one week apart. The duration of the first visit was approximately 4 hours, whereas the second and third visits each took approximately 2.5 hours. At each visit they were administered one of three randomly assigned tDCS conditions: anodal over left DLPFC (cathodal over right supraorbital), cathodal over left DLPFC (anodal over right supraorbital), or sham. (During the first visit, they also completed the diagnostic interviews and questionnaires.) At each visit, participants received two 20-minute stimulation sessions, with approximately 100 minutes between the sessions, in which one stimulation was followed by cognitive testing and the other was followed by EEG. To address potential practice effects, the design of the study was fully counterbalanced, making practice effects orthogonal to the condition effects and thus avoiding confounds with the experimental conditions. Specifically, the order of assessments (cognitive and EEG) was counter-balanced across subjects. Further, within the cognitive assessments, we counter-balanced social cognitive and neurocognitive measures across subjects.
Statistical analyses
Generalized Linear Mixed Models (GLMM) analyses were conducted, using IBM SPSS Statistics, Version 25, to examine the effects of tDCS on patients’ performance on social cognitive, neurocognitive, and EEG measures. For all non-significant findings, the results of post-hoc power analyses are presented as the critical N, that is, the sample size required for 80% power to detect an effect of this size. In cases where the estimated non-centrality parameter is negative (i.e., the observed differences between means are actually smaller than would be expected by chance), the critical N is reported as NA and observed power as 0, as the pattern of results is more consistent with the null hypothesis than any possible alternative; and regardless of how large the sample is, this pattern of results will never yield a significant result. The dataset is available in supporting information (see S1 Dataset).
Results
GLMM analyses were conducted to examine the effects of tDCS on patients’ performance. tDCS condition (anodal, cathodal, and sham) was modeled as a within-subject effect, and a random effect for patient effects was included to account for individual differences between participants. As can be seen in Table 2, none of the social cognitive measures were significantly affected by the stimulation condition. Similarly, tDCS condition had no significant effect on nonsocial cognition, or the cognitive composite. The only measure significantly affected by stimulation was working memory, showing higher performance in the sham condition than in the anodal and cathodal conditions. Finally, none of the EEG measures demonstrated a significant effect of tDCS (see Table 2).
Table 2. Performance data on measures of social cognition, neurocognition, and EEG (N = 37).
| Anodal | Cathodal | Sham | F | p | f2 | Observed | Critical | |
|---|---|---|---|---|---|---|---|---|
| M±SE | M±SE | M±SE | Power | N | ||||
| Social Cognition | ||||||||
| MSCEIT | 36.4±2.06 | 37.7±2.05 | 37.1±2.05 | 0.282 | 0.755 | 0.008 | 0 | NA |
| EIT | 44.9±1.39 | 43.9±1.37 | 44.9±1.39 | 0.475 | 0.624 | 0.013 | 0 | NA |
| TASIT | 22.1±0.71 | 22.4±0.70 | 22.5±0.70 | 0.457 | 0.635 | 0.013 | 0 | NA |
| EAT | 0.49±0.04 | 0.49±0.04 | 0.49±0.04 | 0.002 | 0.998 | <0.001 | 0 | NA |
| Neurocognition | ||||||||
| MCCB CCS | 45.0±1.65 | 45.2±1.65 | 45.8.6±1.64 | 0.462 | 0.632 | 0.013 | 0 | NA |
| MCCB SP | 44.7±2.19 | 45.4±2.18 | 45.1±2.18 | 0.148 | 0.862 | 0.004 | 0 | NA |
| MCCB WM | 38.2±2.19 | 38.0±2.18 | 40.9±2.18 | 3.754 | 0.028 | 0.110 | ||
| MCCB VM | 45.7±2.19 | 44.3±2.18 | 44.7±2.18 | 0.417 | 0.660 | 0.012 | 0 | NA |
| MCCB RPS | 51.4±1.68 | 53.1±1.67 | 52.5±1.67 | 0.683 | 0.509 | 0.020 | 0 | NA |
| EEG | ||||||||
| MMN FZ | -3.44±0.30 | -3.64±0.29 | -3.35±0.29 | 0.529 | 0.592 | 0.015 | 0 | NA |
| P300 Peak | ||||||||
| Latency | 472.6±16.1 | 440.5±15.5 | 422.8±15.7 | 3.076 | 0.053 | 0.090 | 0.61 | 54 |
| P300 Peak | ||||||||
| Amplitude | 7.22±0.98 | 7.03±0.96 | 7.73±0.97 | 0.494 | 0.613 | 0.014 | 0 | NA |
| N170 Emotion | -2.52±0.40 | -3.26±0.39 | -2.71±0.39 | 1.935 | 0.154 | 0.057 | 0.29 | 135 |
| N170 Building | 0.56±0.29 | 0.62±0.28 | 0.56±0.28 | 0.027 | 0.974 | <0.001 | 0 | NA |
MSCEIT: Mayer-Salovey-Caruso Emotional Intelligence Test; EIT: Emotion Identification Test; TASIT: The Awareness of Social Inference Test; EAT: Emphatic Accuracy Task; MCCB: MATRICS Consensus Cognitive Battery; CCS: Cognitive Composite Score; SP: Speed of Processing; WM: Working Memory; VM: Verbal Memory; RPS: Reasoning and Problem Solving; EEG: Electroencephalogram; MMN: Mismatch Negativity; M±SE: Mean±Standard Error; Critical N is the sample size required for 80% power to detect the reported effect; In cases where the estimated non-centrality parameter is negative, the critical N is reported as NA and observed power as < 0.05.
GLMM analyses were also conducted to examine the common side effects of tDCS. As can be seen in Table 3, participants reported significantly more itching, pain, burning, and heat sensations following the anodal and cathodal stimulations, as compared with sham. However, none of the side effects presented substantial discomfort for the participants, as most of the symptoms were rated either as none or mild (below 1) on the scale, and none requested to discontinue the procedure.
Table 3. Side effects following tDCS administration (N = 37).
| Anodal | Cathodal | Sham | F | p | |
|---|---|---|---|---|---|
| M±SE | M±SE | M±SE | |||
| Itching | 1.27±0.19 | 1.41±0.18 | 0.50±0.18 | 8.801 | <0.001 |
| Pain | 0.26±0.10 | 0.44±0.10 | 0.13±0.10 | 4.647 | 0.013 |
| Burning | 0.90±0.18 | 1.16±0.17 | 0.44±0.17 | 7.418 | 0.001 |
| Heat | 0.73±0.12 | 0.41±0.12 | 0.29±0.12 | 6.860 | 0.002 |
| Pinching | 0.32±0.12 | 0.39±0.12 | 0.19±0.12 | 0.836 | 0.438 |
| Iron Taste | 0.12±0.06 | 0.08±0.06 | 0.06±0.06 | 0.293 | 0.747 |
| Fatigue | 0.58±0.15 | 0.61±0.15 | 0.36±0.15 | 1.108 | 0.336 |
M±SE: Mean±Standard Error
Discussion
In this study, we examined the effect of single tDCS administration in schizophrenia on a broad range of social cognitive, nonsocial neurocognitive, and ERP measures. Employing a commonly used montage in cognitive enhancement tDCS studies in a cross-over design, we found that none of the social cognitive measures nor any of the EEG measures were significantly affected by the stimulation condition. Similarly, tDCS condition had no significant effect on nonsocial neurocognition, including the cognitive composite score. The only measure significantly affected by stimulation was working memory, with both anodal and cathodal stimulations adversely affecting performance. The very small effect sizes, further validated by post-hoc power analyses (large Critical Ns), demonstrated that these findings were not due to lack of statistical power.
The present findings, combined with the inconsistency of therapeutic effects reported in studies of single tDCS administration, underscore the need to examine alternative tDCS montages. Along these lines, recent studies have examined the effects of tDCS at different intensities and/or across multiple sessions [39–42]. For example, Hoy et al. (2014) examined the effects of anodal left dorsolateral prefrontal tDCS at different intensities (1mA, 2mA, sham) and measured performance across three time points post-stimulation (0, 20 and 40 min). They found a significant improvement in performance over time following 2 mA stimulation only, demonstrating the importance of dose of stimulation [42]. Similarly, Brunelin et al. (2012) administered active 2 mA tDCS to individuals with schizophrenia for 20 minutes twice a day on 5 consecutive weekdays. They reported a robust reduction in auditory verbal hallucinations, with the beneficial effect lasting for up to 3 months [40]. Smith et al. (2015) conducted a randomized double-blind, sham-controlled study of the effects of 5 sessions of tDCS on cognitive and psychiatric symptoms in individuals with schizophrenia or schizoaffective disorder. They reported significant improvements after the fifth tDCS session in MCCB Composite score and on the MCCB Working Memory and Attention-Vigilance domain scores, with large effect sizes [41]. These latter two studies demonstrate the potentially cumulative effect of multiple tDCS session.
Another approach that should be incorporated in future studies involves online (task-concurrent) tDCS. In this montage, participants engage in cognitive training while concurrently receiving active tDCS. Recent studies suggest that this paradigm may be particularly effective for enhancing certain cognitive functions [43–45]. Au et al. (2016), for example, administered 7 days of working memory training concurrent with active either active (left or right DLPFC) or sham tDCS to a sample of healthy individuals. They found that active tDCS enhanced training performance, which was preserved several months after training completion [43]. Similarly, Ruff et al. (2017) examined the effect on healthy adults of three consecutive training sessions concurrent with tDCS on both spatial and verbal working memory. They compared active tDCS over DLPFC in a task-congruent (spatial-right, verbal-left), task-incongruent (spatial-left, verbal-right), and sham stimulation in regards to the efficacy of WM training and found a steeper learning curve when WM training was combined with task-congruent tDCS, with effects lasting for up to nine months and transferring to respective untrained tasks [44]. Finally, Oldrati et al. (2018) compared the effects of online vs. offline tDCS on enhancing training on a visuospatial task. They administered anodal tDCS of DLPFC either before or during training to a sample of healthy volunteers and found that, compared with the sham condition, the largest improvement occurred in the online tDCS condition [45]. These studies thus underscore the facilitative and long-lasting effects of tDCS when applied concurrently with cognitive training.
Considerable efforts have been made to find ways to enhance cognition in schizophrenia, mostly focusing on psychopharmacological approaches [4, 11, 46]. In recent years, neurostimulation has been developed as a non-invasive tool for cognitive enhancement [19, 21, 47, 48]. Neurostimulation has some advantages over psychopharmacology in that it is relatively safe with few side effects [49]. The tDCS procedure was well-tolerated in our study, with most common side effects being itching, pain, burning, and heat sensations, which followed both the anodal and cathodal stimulations. Importantly, most of the side effects were rated as mild or below, and none of the participants requested to discontinue the procedure. These findings are consistent with numerous reports [15, 20, 21], clearly establishing the safety and tolerability of single tDCS administration.
A number of limitations of the current study should be noted. In an effort to blind participants to the type of stimulation, we created a sham condition in which the current was turned on for 30 seconds and then ramped down to 0 mA. In this way, participants experienced the same initial sensation of mild tingling that is experienced during anodal and cathodal stimulations. Nonetheless, when comparing self-reported measures of side effects across the stimulation conditions, participants reported significantly more itching, pain, burning, and heat sensations following the anodal and cathodal stimulations, as compared with sham. Thus, although these side effects were very mild, findings suggest that actual tDCS conditions are experienced differently than sham. Additionally, the research assistants administering the procedure were not blinded to the stimulation condition, which could have also potentially influenced the sensations reported by the participants. Importantly, these findings are limited to effects of single tDCS administration, as assessed by changes from baseline to immediately post-stimulation. It could have been informative to conduct multiple tDCS sessions, while analyzing potential effects on a session to session basis. Unfortunately, practice effects, which are inherent in most performance-based measures, limit the applicability of these approaches in clinical trials of this type.
In summary, although these findings support the safety and tolerability of single tDCS administration, using a reasonably well-powered cross-over design, we failed to detect a differential tDCS effect of stimulation condition on neurocognitive and social cognitive performance-based tasks, as well as on EEG measures. These findings thus add to the growing body of evidence suggesting the potentially suboptimal dose of the single tDCS administration and point to the need for basic dose-finding studies in tDCS, as there would be for a new pharmacological intervention. Given its safety, tolerability, portability, relatively cheap cost, and ease of administration, once therapeutic dose is established, tDCS could potentially become a valuable therapeutic tool in the treatment of neurocognitive and social cognitive deficits in schizophrenia.
Supporting information
(DOC)
(DOCX)
(XLSX)
Acknowledgments
We thank Albert Chung for assistance with tDCS equipment and method development.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by a NARSAD Independent Investigator Grant from the Brain & Behavior Research Foundation (22017).
References
- 1.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry. 1996;153(3):321–30. doi: 10.1176/ajp.153.3.321 [DOI] [PubMed] [Google Scholar]
- 2.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the "right stuff"? Schizophrenia Bulletin. 2000;26:119–36. [DOI] [PubMed] [Google Scholar]
- 3.Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophrenia Research. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009 [DOI] [PubMed] [Google Scholar]
- 4.Green MF, Nuechterlein KH, Gold JM, Barch DM, Cohen J, Essock S, et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: The NIMH-MATRICS conference to select cognitive domains and test criteria. Biological Psychiatry. 2004;56:301–7. doi: 10.1016/j.biopsych.2004.06.023 [DOI] [PubMed] [Google Scholar]
- 5.Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophrenia Research. 2004;72:29–39. doi: 10.1016/j.schres.2004.09.007 [DOI] [PubMed] [Google Scholar]
- 6.Pinkham AE, Penn DL, Perkins DO, Lieberman JA. Implications of a neural basis for social cognition for the study of schizophrenia. American Journal of Psychiatry. 2003;160(5):815–24. doi: 10.1176/appi.ajp.160.5.815 [DOI] [PubMed] [Google Scholar]
- 7.Green MF, Olivier B, Crawley JN, Penn DL, Silverstein S. Social cognition in schizophrenia: Recommendations from the MATRICS New Approaches Conference. Schizophrenia Bulletin. 2005;31:882–7. doi: 10.1093/schbul/sbi049 [DOI] [PubMed] [Google Scholar]
- 8.Gold JM, Green MF. Neurocognition in schizophrenia In: Sadock BJ, Sadock VA, editors. Comprehensive Textbook of Psychiatry. 8th ed. Baltimore: Lippincott, Williams & Wilkins; 2004. p. 1436–48. [Google Scholar]
- 9.Edwards J, Jackson HJ, Pattison PE. Emotion recognition via facial expression and affective prosody in schizophrenia: A methodological review. Clinical Psychology Review. 2002;22:789–832. [DOI] [PubMed] [Google Scholar]
- 10.Kee KS, Green MF, Mintz J, Brekke JS. Is emotional processing a predictor of functional outcome in schizophrenia? Schizophrenia Bulletin. 2003;29:487–97. [DOI] [PubMed] [Google Scholar]
- 11.Marder SR, Fenton WS. Measurement and treatment research to improve cognition in schizophrenia: NIMH MATRICS Initiative to support the development of agents for improving cognition in schizophrenia. Schizophrenia Research. 2004;72:5–10. doi: 10.1016/j.schres.2004.09.010 [DOI] [PubMed] [Google Scholar]
- 12.Stover EL, Brady L, Marder SR. New paradigms for treatment development. Schizophrenia bulletin. 2007;33(5):1093–9. doi: 10.1093/schbul/sbm085 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nitsche MA, Paulus W. Noninvasive Brain Stimulation Protocols in the Treatment of Epilepsy: Current State and Perspectives. Neurotherapeutics. 2009;6(2):244–50. PubMed PMID: WOS:000264659900005. doi: 10.1016/j.nurt.2009.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zaghi S, Acar M, Hultgren B, Boggio PS, Fregni F. Noninvasive Brain Stimulation with Low-Intensity Electrical Currents: Putative Mechanisms of Action for Direct and Alternating Current Stimulation. Neuroscientist. 2010;16(3):285–307. doi: 10.1177/1073858409336227 PubMed PMID: WOS:000277670200012. [DOI] [PubMed] [Google Scholar]
- 15.Poreisz C, Boros K, Antal A, Paulus W. Safety aspects of transcranial direct current stimulation concerning healthy subjects and patients. Brain Research Bulletin. 2007;72(4–6):208–14. doi: 10.1016/j.brainresbull.2007.01.004 PubMed PMID: WOS:000246753500005. [DOI] [PubMed] [Google Scholar]
- 16.Brunelin J, Mondino M, Haesebaert F, Saoud M, Suaud-Chagny MF, Poulet E. Efficacy and safety of bifocal tDCS as an interventional treatment for refractory schizophrenia. Brain Stimulation. 2012;5(3):431–2. doi: 10.1016/j.brs.2011.03.010 PubMed PMID: WOS:000307198700032. [DOI] [PubMed] [Google Scholar]
- 17.Rassovsky Y, Dunn W, Wynn J, Wu AD, Iacoboni M, Hellemann G, et al. The effect of transcranial direct current stimulation on social cognition in schizophrenia: A preliminary study. Schizophrenia Research. 2015;165(2–3):171–4. doi: 10.1016/j.schres.2015.04.016 PubMed PMID: WOS:000355562400011. [DOI] [PubMed] [Google Scholar]
- 18.Dunn W, Rassovsky Y, Wynn JK, Wu AD, Iacoboni M, Hellemann G, et al. Modulation of neurophysiological auditory processing measures by bilateral transcranial direct current stimulation in schizophrenia. Schizophrenia Research. 2016;174(1–3):189–91. doi: 10.1016/j.schres.2016.04.021 PubMed PMID: WOS:000377934800031. [DOI] [PubMed] [Google Scholar]
- 19.Vercammen A, Rushby JA, Loo C, Short B, Weickert CS, Weickert TW. Transcranial direct current stimulation influences probabilistic association learning in schizophrenia. Schizophrenia Research. 2011;131(1–3):198–205. doi: 10.1016/j.schres.2011.06.021 PubMed PMID: WOS:000295111400031. [DOI] [PubMed] [Google Scholar]
- 20.Fitzgerald PB, McQueen S, Daskalakis ZJ, Hoy KE. A Negative Pilot Study of Daily Bimodal Transcranial Direct Current Stimulation in Schizophrenia. Brain Stimulation. 2014;7(6):813–6. doi: 10.1016/j.brs.2014.08.002 PubMed PMID: WOS:000346455200007. [DOI] [PubMed] [Google Scholar]
- 21.Mattai A, Miller R, Weisinger B, Greenstein D, Bakalar J, Tossell J, et al. Tolerability of transcranial direct current stimulation in childhood-onset schizophrenia. Brain Stimulation. 2011;4(4):275–80. doi: 10.1016/j.brs.2011.01.001 PubMed PMID: WOS:000297568800012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition. New York: New York State Psychiatric Institute; 1997. [Google Scholar]
- 23.AmericanPsychiatricAssociation. Diagnostic and Statistical Manual of Mental Disorders. 4 ed. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 24.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the brief psychiatric rating scale: 'The Drift Busters'. International Journal of Methods in Psychiatric Research. 1993;3:221–4. [Google Scholar]
- 25.Andreasen NC. The scale for the assessment of negative symptoms (SANS). Iowa City, IA: The University of Iowa; 1984. [Google Scholar]
- 26.Mayer JD, Salovey P, Caruso DR. Technical Manual for the MSCEIT (Version 2.0). Toronto, Canada: Multi-Health Systems; 2002. [Google Scholar]
- 27.Ekman P. Subtle Expression Training Tool (SETT) & Micro Expression Training Tool (METT). Paul Ekman www.paulekman.com.; 2004.
- 28.McDonald S, Flanagan S, Rollins J. The Awareness of Social Inference Test. Suffolk, England: Thames Valley Test Company Limited; 2002. [Google Scholar]
- 29.Lee J, Zaki J, Harvey PO, Ochsner K, Green MF. Schizophrenia patients are impaired in empathic accuracy. Psychological Medicine. 2011;41(11):2297–304. doi: 10.1017/S0033291711000614 PubMed PMID: WOS:000296246300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kern RS, Nuechterlein KH, Green MF, Baade LE, Fenton WS, Gold JM, et al. The MATRICS Consensus Cognitive Battery: Part 2. co-norming and standardization. American Journal of Psychiatry. 2008;165:214–20. doi: 10.1176/appi.ajp.2007.07010043 [DOI] [PubMed] [Google Scholar]
- 31.Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch D, Cohen J, et al. The MATRICS Consensus Cognitive Battery: Part 1. test selection, reliability, and validity. American Journal of Psychiatry. 2008;165:203–13. doi: 10.1176/appi.ajp.2007.07010042 [DOI] [PubMed] [Google Scholar]
- 32.Brunoni AR, Nitsche MA, Bolognini N, Bikson M, Wagner T, Merabet L, et al. Clinical research with transcranial direct current stimulation (tDCS): Challenges and future directions. Brain Stimulation. 2012;5(3):175–95. doi: 10.1016/j.brs.2011.03.002 PubMed PMID: WOS:000307198700002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gratton G, Coles MGH, Donchin E. A NEW METHOD FOR OFF-LINE REMOVAL OF OCULAR ARTIFACT. Electroencephalography and Clinical Neurophysiology. 1983;55(4):468–84. doi: 10.1016/0013-4694(83)90135-9 PubMed PMID: WOS:A1983QJ92900013. [DOI] [PubMed] [Google Scholar]
- 34.Jahshan C, Wynn JK, Green MF. Relationship between auditory processing and affective prosody in schizophrenia. Schizophrenia research. 2013;143(2–3):348–53. doi: 10.1016/j.schres.2012.11.025 PubMed ; PubMed Central PMCID: PMC3551533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wynn JK, Jahshan C, Altshuler LL, Glahn DC, Green MF. Event-related potential examination of facial affect processing in bipolar disorder and schizophrenia. Psychological Medicine. 2013;43(1):109–17. doi: 10.1017/S0033291712001006 PubMed PMID: WOS:000312260500010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wynn JK, Lee J, Horan WP, Green MF. Using event related potentials to explore stages of facial affect recognition deficits in schizophrenia. Schizophrenia Bulletin. 2008;34(4):679–87. doi: 10.1093/schbul/sbn047 PubMed PMID: ISI:000257417300014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ekman P. Pictures of Facial Affect. Palo Alto, CA: Consulting Psychologists Press; 1976. [Google Scholar]
- 38.Koenigs M, Ukueberuwa D, Campion P, Grafman J, Wassermann E. Bilateral frontal transcranial direct current stimulation: Failure to replicate classic findings in healthy subjects. Clinical Neurophysiology. 2009;120(1):80–4. doi: 10.1016/j.clinph.2008.10.010 PubMed PMID: WOS:000262885000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mondino M, Haesebaert F, Poulet E, Suaud-Chagny MF, Brunelin J. Fronto-temporal transcranial Direct Current Stimulation (tDCS) reduces source-monitoring deficits and auditory hallucinations in patients with schizophrenia. Schizophrenia Research. 2015;161(2–3):515–6. doi: 10.1016/j.schres.2014.10.054 PubMed PMID: WOS:000348452100058. [DOI] [PubMed] [Google Scholar]
- 40.Brunelin J, Mondino M, Gassab L, Haesebaert F, Gaha L, Suaud-Chagny MF, et al. Examining Transcranial Direct-Current Stimulation (tDCS) as a Treatment for Hallucinations in Schizophrenia. American Journal of Psychiatry. 2012;169(7):719–24. doi: 10.1176/appi.ajp.2012.11071091 PubMed PMID: WOS:000305853400010. [DOI] [PubMed] [Google Scholar]
- 41.Smith RC, Boules S, Mattiuz S, Youssef M, Tobe RH, Sershen H, et al. Effects of transcranial direct current stimulation (tDCS) on cognition, symptoms, and smoking in schizophrenia: A randomized controlled study. Schizophrenia Research. 2015;168(1–2):260–6. doi: 10.1016/j.schres.2015.06.011 PubMed PMID: WOS:000361826400037. [DOI] [PubMed] [Google Scholar]
- 42.Hoy KE, Arnold SL, Emonson MRL, Daskalakis ZJ, Fitzgerald PB. An investigation into the effects of tDCS dose on cognitive performance over time in patients with schizophrenia. Schizophrenia Research. 2014;155(1–3):96–100. doi: 10.1016/j.schres.2014.03.006 PubMed PMID: WOS:000335442200015. [DOI] [PubMed] [Google Scholar]
- 43.Au J, Katz B, Buschkuehl M, Bunarjo K, Senger T, Zabel C, et al. Enhancing Working Memory Training with Transcranial Direct Current Stimulation. Journal of Cognitive Neuroscience. 2016;28(9):1419–32. doi: 10.1162/jocn_a_00979 PubMed PMID: WOS:000381523000014. [DOI] [PubMed] [Google Scholar]
- 44.Ruf SP, Fallgatter AJ, Plewnia C. Augmentation of working memory training by transcranial direct current stimulation (tDCS). Scientific Reports. 2017;7 doi: 10.1038/s41598-017-01055-1 PubMed PMID: WOS:000399973600001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oldrati V, Colombo B, Antonietti A. Combination of a short cognitive training and tDCS to enhance visuospatial skills: A comparison between online and offline neuromodulation. Brain Research. 2018;1678:32–9. doi: 10.1016/j.brainres.2017.10.002 PubMed PMID: WOS:000418974900005. [DOI] [PubMed] [Google Scholar]
- 46.Buchanan RW, Davis M, Goff D, Green MF, Keefe RSE, Leon AC, et al. A summary of the FDA-NIMH-MATRICS workshop on clinical trial design for neurocognitive drugs for schizophrenia. Schizophrenia Bulletin. 2005;31:5–19. doi: 10.1093/schbul/sbi020 [DOI] [PubMed] [Google Scholar]
- 47.Dedoncker J, Brunoni AR, Baeken C, Vanderhasselt MA. The effect of the interval-between-sessions on prefrontal transcranial direct current stimulation (tDCS) on cognitive outcomes: a systematic review and meta-analysis. Journal of Neural Transmission. 2016;123(10):1159–72. doi: 10.1007/s00702-016-1558-x PubMed PMID: WOS:000385171100006. [DOI] [PubMed] [Google Scholar]
- 48.Hasan A, Strube W, Palm U, Wobrock T. Repetitive Noninvasive Brain Stimulation to Modulate Cognitive Functions in Schizophrenia: A Systematic Review of Primary and Secondary Outcomes. Schizophrenia Bulletin. 2016;42:S95–S109. doi: 10.1093/schbul/sbv158 PubMed PMID: WOS:000386210400012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dresler M, Sandberg A, Ohla K, Bublitz C, Trenado C, Mroczko-Wasowicz A, et al. Non-pharmacological cognitive enhancement. Neuropharmacology. 2013;64:529–43. doi: 10.1016/j.neuropharm.2012.07.002 PubMed PMID: WOS:000311250300059. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOCX)
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.