Abstract
Silicosis is an ancient but still life-threatening occupational lung disease because of its incurable nature. Although its risks are known in many occupational settings and effective control strategies are well established, new cases, even epidemics, continue to occur in different sectors of Turkey. Before taking action, defining the magnitude of the problem is essential. In this concise review, we aimed to present the current situation of silicosis in Turkey. According to the data available to date, silicosis continues to be a major health problem in different sectors. Sandblasting seems to have the highest risk for the development of silicosis. Disease onset at early age and history of short exposure duration may indicate intense silica exposure. After denim sandblasters, dental technicians seem to be the new and recently recognized high-risk occupation group as per the increasing reports.
Because of the lack of a definite treatment of silicosis, prevention of the disease should be the main target. Better occupational disease registry systems would be useful to assess the magnitude of the problem. In addition to implementing the necessary regulations, a close inspection of the workplaces for potential risks is essential. Other social and economic factors related with the occurrence of disease, such as unregistered employment rate and unlicensed and uninsured work, should also be considered. Finally, optimal healthcare and better living conditions for patients with silicosis should be ensured.
Keywords: Epidemiology, silica, silicosis, prevention, pneumoconiosis, occupational lung diseases
INTRODUCTION
“We cannot solve our problems with the same thinking we used when we created them.”
- Albert Einstein
As Albert Einstein said, we need to change the way of thinking to be able to make impactful changes. Silicosis is a global concern, but it is more prevalent in developing countries, because occupational health and safety issues usually go parallel with the type and structure of economy. Many workers face “dirty jobs” mainly because of economic reasons [1]. High unemployment rate and having no other options for earning money usually forces the workers to accept any kind of job, sometimes, by taking the apparent work-related risk. Although the risks are well known in many occupational settings and effective control strategies are well established, new cases, even epidemics, still continue to occur [1]. The high rate of occupational diseases, including silicosis, in a country, may reflect the absence of effectiveness of regulations, implementations, and control [2].
Silicosis is an incurable occupational lung disease caused by inhalation and accumulation of free inhalable crystalline silica in the lungs. The silica dust causes a tissue reaction, which is associated with exposure intensity and duration. It is one of the oldest and most prevalent occupational diseases worldwide. Harmful exposure to silica can only be prevented by awareness of the hazard and effective control measures. Otherwise, lack of recognition of the hazard may cause a delay in controlling the exposure until the workers become sick. In that case, the diagnosis of the disease and its association with the workplace can only be identified by an astute physician, as occurred many times in the past [3]. For economic reasons, as in developing countries or developed countries with the industrial developments, a known agent in a new and unexpected occupational setting or a new agent with unknown respiratory health effects can be the cause of occupational disease [4,5]. Turkey is geographically and economically in the transition zone and carries both risks.
Implementation of primary preventive interventions and effective control measures become crucial for the control of occupational diseases. Thus, before moving forward, defining the magnitude of the problem is essential. In this concise review, we aimed to present the current status of silicosis in Turkey using the available published data. For this purpose, we performed a search on PubMed, Google Scholar, and “Turkish Medicine Index (Türk Tıp Dizini)” using the terms “silica,” “silicosis,” “pneumoconiosis,” and “Turkey.” To obtain previous publications, we also collected the references of the available publications. Additionally, the statistical data produced by the government, which are officially available on the websites, were also examined.
MAGNITUDE OF THE SILICOSIS PROBLEM IN TURKEY
It is extremely difficult to visualize a clear and entire picture of the problem because of the lack of specific surveillance systems for silicosis or other occupational diseases in Turkey. The second important challenge is the presence of high unregistered employment rate. According to the report of Turkish Statistical Institute, the labor force in 2017 was around 32 million, and the rate of unregistered employment is 33.6% [6]. This might be the negative side, which is out of our sight, and it may be much more problematic as previously observed among denim sandblasters, that almost all cases were unregistered and uninsured and most of the workplaces were unregistered or unlicensed [7].
The only available and relatively reliable data come from Turkey’s Social Security Institution, which annually publishes the records of the loss of earning capacity [8,9] in the profession. However, this data can only reflect the tip of the iceberg because the occupations of uninsured workers are not included in the records and it only presents the data of relatively severe cases. Nevertheless, this data might be reasonably useful to project silicosis among the other diseases annually. According to the statistics of the duration between 2013 and 2016, the number of workers who had suffered the loss of earning capacity was 351, 494, 510, and 594, sequentially [8]. Among them, the pneumoconiosis rate shows a slightly increasing trend as 18%, 20%, 35%, and 33% between the above-mentioned years. Although the data are insufficient to reach a robust conclusion, it depicts the increasing trend of pneumoconiosis parallel to the increase of the total number. Compared to asbestosis and coal worker’s pneumoconiosis, silicosis is the main responsible disease for this increasing trend (Figure 1). The data are extremely farfetched to show the real situation, but it gives us an idea about the past or recent past, according to the latency periods of the diseases, drawing an analogy to the stars on the sky having different ages but seen altogether on the same sky on a given day.
Figure 1.
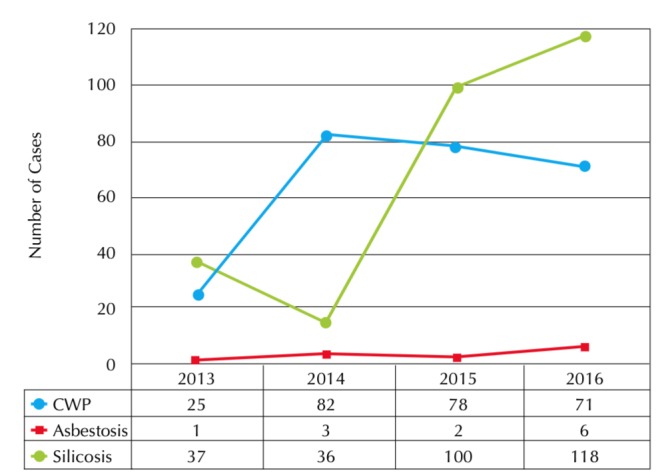
The number of cases of coal workers pneumoconiosis, asbestosis, and silicosis with loss of earning capacity between 2013 and 2016 according to Turkey Social Security Institution Statistics [8]
The electronic health records of hospitals might be another useful piece to solve the jigsaw puzzle. Although the state hospitals have a common network and can share data among them, the university hospitals, either government or private ones, keep their records to themselves, thus making it difficult to visualize the complete picture. Information regarding this group of patients can be obtained only when the researchers from those hospitals regularly publish their patient data as case series. Although they are few in number, they can still be useful. The three specific hospitals dedicated to occupational diseases can also provide some data about the situation. Hospitals in Istanbul and Ankara receive applications throughout the country, but the hospital in Zonguldak mainly deals with coal mine workers who work in the mines around Zonguldak. For example, according to the data of Istanbul Occupational Diseases Hospital for 2008–2010, denim sandblasters (50.5%), dental technicians (12.0%), and coal miners (6.7%) are ranked as the top three groups acquiring pneumoconiosis out of the 208 workers [10], followed by others, including casters, Teflon-pot sandblasters, ceramic workers, sandblasters for other reasons, welders, quartz workers, tunnel workers, raw glass workers, and lathe workers, in the decreasing order. According to a university hospital-based study [11], analyzing the data of 60 workers for 2013–2015, ceramic workers and dental technicians comprised 80% of the cases, in equal numbers (24 for both), and were followed by sandblasters, welders, miners, and marble cutters.
THE EXAMPLE OF COAL MINES
Coal mines in Turkey have always been in the public eye because of the tragic accidents. The most tragic one occurred recently in Soma on May 13, 2014, wherein 301 lives were lost during the disaster [12,13]. The coal mine industry can also be considered the starting point of occupational disease awareness and implementation of dust control measures in Turkey, and we can infer some important lessons from the coal mine experience. In the previous years, pneumoconiosis was the major reason for the application for the loss of earning capacity. Among 5000 applications for the loss of earning capacity between 1994–1996, pneumoconiosis rate was 59.8% [14]. Most of them were coal workers pneumoconiosis, which is now considered a subgroup of the recently termed “coal mine dust lung diseases” [15]. The proportional decrease in the number of pneumoconiosis cases reported in the following years may reflect either the success of rigorous surveillance system by Turkish Coal Enterprises (TCE) in coal mines or an increase of awareness of other occupational diseases other than pneumoconiosis and lung diseases.
In a study investigating the condition of coal mines from 1985 to 2004, pneumoconiosis prevalence was found to be very low compared to the other sectors as shown in Table 1: 2.47% in 2004 and 1.63% in 2004, with a temporary increase to 6.23% in 1999 followed by a decline again [16]. However, the number of total workers also decreased from 38.231 in 1985 to 12.261 in 2004. The decreasing number of workers in TCE might reflect a shift from TCE coal mines to small and private enterprises where control measures are expected to be lower. Inadequate and ineffective regulations or control measures might end up to the resurgence of the problem [17].
Table 1.
Silicosis prevalence studies performed in different sectors other than coal mining*
| Sector | Study | Year | Mean age, years | Total exposure duration | Silicosis rate |
|---|---|---|---|---|---|
| Ceramic | Sakar A., et al. [25] | 2005 | 36±6 | 140±74 months | 24/365 (6.6%) |
| Denim sandblasting | Akgun M, et al. [7] | 2008 | 23±6 | 36±25 months | 77/145 (53.1%) |
| Akgun M, et al. [21] | 2015 | 27±6 | 41±27 months | 80/83 (96.4%) | |
| Dental technicians | Cimrin A., et al. [22] | 2009 | 28±8 | 12±9 years | 33/140 (23.6%), general 22/44 (50.0%), only sandblasters |
| Özdemir D., et al. [26] | 2010 | 29±8 | 14 years | 5/36 (13.8%) | |
| Ergün D., et al.[23] | 2014 | 35±9 | 11±8 years | 90/888 (10.1%), general 79/171 (46.1%), only sandblasters |
|
| Kahraman H., et al. [20] | 2014 | 32±8 | 17±9 years | 35/76 (46.1%), HRCT based | |
| Berk S., et al.[27] | 2016 | 31±9 | 14±9 years | 10/32 (31.3%), chest x-ray 22/32 (68.8%), HRCT |
|
| Foundry | Akkurt I, et al. [28] | 1997 | 34±4 | 10±4 years | 9/48 (18.7%), high dust exposure 4/36 (11%), low dust exposure |
| Quarry | Karadağ Ö.K., et al. [29] | 2001 | 40±0 | 10±0 years | 27/85 (32.1%), high risk 43/109 (22.7%), low risk |
| Akkaya A., et al. [30] | 2001 | 40±6 | 12±7 years | 45/50 (90.0%), heavy exposure | |
| 34±7 | 3±4 years | 21/40 (52.5%), low exposure | |||
| Quartz mill | Polatlı M., et al. [31] | 2001 | 36±8 | 9±3 years | 8/67 (11.9%) |
| Öztürk A., et al. [32] | 2012 | 32±8 | ≤5 years (80.5%) | 103/448 (23.0%) | |
| Sandblasting | Sevinç C., et al.[33] | 2003 | 32±11 | 8±6 years | 3/11 (27.2%), chest x-ray 4/11 (36.3%), HRCT |
| Welding | Cömert M, et al. [34] | 2014 | 39±8 | 17±9 years | 8/44 (18.2%) |
Among the recent studies available as full text, those providing prevalence rate and exposure duration were included in the table.
EPIDEMIOLOGIC STUDIES ON SILICOSIS
The epidemiologic studies on silicosis occurring in different sectors had different screening methods, including either chest x-ray evaluation or high-resolution computerized tomography (HRCT) evaluation or both, which indicate different rates of silicosis according to the sectors. The prevalence of silicosis is higher in the studies using HRCT as a screening tool compared to standard chest x-ray evaluation [18–20]. As shown in Table 1, silicosis is currently observed in different sectors and sandblasting seems to have the highest risk amongst various sectors. Although the prevalence of silicosis was 53.1% among denim sandblasters in 2007, it increased to 96%, which is the highest prevalence reported to date, after 4 years follow-up of the same population with no further exposure history [7,21]. In dental technicians, the prevalence increases 2 to 5 folds for sandblasting [22,23]. Among other sectors, the ceramic sector seems to have the lowest prevalence [24,25].
Compared to the coal miners, patients with silicosis were younger who had relatively short exposure duration. Relatively younger age and lower exposure duration may be considered an indicator of worse working conditions and higher silica exposure [16]. Additionally, the type of the job seems to have an effect on the amount of the exposed inhalable dust and therefore different rates of prevalence of silicosis within the same workplace (Table 1) [26–34].
INCREASED AWARENESS OF SILICOSIS AND ITS HAZARD
Although implementing effective surveillance and control programs can prevent silicosis, there are many obstacles in achieving this goal [35]. As seen in several instances, its hazard in a new occupational setting is usually neglected or underestimated, but it costs lives and only attracts public attention following a disaster as observed in the Hawk’s Nest Disaster in the US [36] and the epidemics of silicosis among former sandblasters because of denim sandblasting in Turkey [37]. Unfortunately, despite facing repercussions of such disasters, precautionary measures are not taken and similar events occur in new settings in the same country or another place.
The awareness of silicosis in Turkey has increased following the epidemics in denim sandblasters in the beginning of this century [7,21,37–44]. The increased awareness had some positive effects; sandblasting using silica-containing material was banned, the uninsured workers were provided access to free healthcare, and compensation rights were given to those with severe disease. It also alarmed the authorities to review the regulations and control measures. However, workers who were diagnosed with silicosis suffered psychosocial challenges, thereby making their lives more difficult. The diagnosis of silicosis is usually considered as a cause of imminent death among the workers due to spread of the death news of silicosis patients, who were mostly denim sandblasters, on the media [45]. Because many new job applications require a healthy individual, it is extremely difficult to get a new job for such workers and to earn a living.
Silicosis leads to death in several industries and workplaces, such as quarries, mining, tunneling, foundries, glass industry, ceramics, cement, and all the sectors in which sandblasting is used. In the past, around the 1930s, silica exposure and silicosis were mainly observed in mining sectors and in quarry workers [46]; the areas of concern currently are the silicosis among dental technicians and construction workers, particularly those involved in huge urban renovation projects throughout the country. Although silicosis cases in the ceramic sector are of high importance in the media, there is no currently available data to assess the real situation. Acute and accelerated silicosis cases have been incidentally reported in various fields, such as in Teflon-coated pan manufacturing because of sandblasting and electric cable manufacturing with fatal outcomes [47–49].
CONCLUSION
Because of the lack of a definite treatment of silicosis, prevention of the disease should be the main target. Better occupational disease registry systems would be useful to be able to assess the magnitude of the problem, which is required to combat the occupational diseases. Thus, in addition to the implementation of effective regulations, which does not always mean better control, sustained close inspections of the workplaces and routine screening of the workers are required to achieve the desired control. To decrease unregistered employment rate, unlicensed and uninsured work should be discouraged. For the workers who are already diagnosed with silicosis, a new comprehensive approach is mandatory not only to provide them better healthcare but also better social and economic conditions.
Footnotes
Peer-review: Externally peer-reviewed.
Author contributions: Concept - M.A., B.E.; Design -M.A.; Supervision - M.A., B.E.; Resource - M.A., B.E.; Materials - M.A., B.E.; Data Collection and/or Processing - M.A., B.E.; Analysis and/or Interpretation - M.A., B.E.; Literature Search - M.A., B.E.; Writing - M.A., B.E.; Critical Reviews - M.A., B.E.
Conflict of Interest: No conflict interest was declared that this study has received no financial support.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Cullinan P, Muñoz X, Suojalehto H, et al. Occupational lung diseases: from old and novel exposures to effective preventive strategies. Lancet Respir Med. 2017;5:445–55. doi: 10.1016/S2213-2600(16)30424-6. [DOI] [PubMed] [Google Scholar]
- 2.Artvinli F. The ethics of occupational health and safety in turkey: responsibility and consent to risk. Acta Bioeth. 2016;22:111–8. doi: 10.4067/S1726-569X2016000100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henneberger PK, Weissman DN. Old adversaries in new places. Occup Environ Med. 2018;75:1–2. doi: 10.1136/oemed-2017-104731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Matteis S, Heederik D, Burdorf A, et al. Current and new challenges in occupational lung diseases. Eur Respir Rev. 2017;26(146) doi: 10.1183/16000617.0080-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martínez-González C. Changes in the Profile Of Diseases Caused By The Inhalation Of Silica. Arch Bronconeumol. 2018;54:5–6. doi: 10.1016/j.arbres.2017.06.024. [DOI] [PubMed] [Google Scholar]
- 6.Turkish Statistical Institute. Labour Force Statistics. Nov, 2017. [Last accessed on 12 March 2018]. Available at: http://www.turkstat.gov.tr/PreHaberBultenleri.do?id=27687.
- 7.Akgun M, Araz O, Akkurt I, et al. An epidemic of silicosis among former denim sandblasters. Eur Respir J. 2008;32:1295–303. doi: 10.1183/09031936.00093507. [DOI] [PubMed] [Google Scholar]
- 8.Social Security Institution. Statistical Yearbook (2007–2016) [Last accessed on 12 March 2018]. Available at: http://www.sgk.gov.tr/wps/portal/sgk/tr/kurumsal/istatistik/sgk_istatistik_yilliklari.
- 9.Davoodi S, Haghighi KS, Kalhori SRN, et al. Occupational disease registries-characteristics and experiences. Acta Inform Med. 2017;25:136–40. doi: 10.5455/aim.2017.25.136-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Altinöz H, Çelikkalkan C, Horasan GD, et al. Socio-demographic and clinical characteristics of turkish workers with pneumoconiosis. Cent Eur J Public Health. 2016;2:231–3. doi: 10.21101/cejph.a4694. [DOI] [PubMed] [Google Scholar]
- 11.Alıcı NŞ, Çimrin A, Coşkun Beyan A. Pneumoconiosis in different sectors and their differences in Turkey. Tuberk Toraks. 2016;64(4):275–82. doi: 10.5578/tt.27995. [DOI] [PubMed] [Google Scholar]
- 12.Akgun M. Coal mine accidents. Turk Thorac J. 2015;16:S1–S2. doi: 10.5152/ttd.2015.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atalay F. The history of the coal mining industry and mining accidents in the world and turkey. Turk Thorac J. 2015;16:S5–S8. doi: 10.5152/ttd.2015.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saygun M, Tunçbilek A, Karabıyıloğlu G. The cases of pneumoconiosis evaluated in SSK high health committee between 1994–1996. Tuberculosis Thorax. 2002;50:358–68. [Google Scholar]
- 15.Petsonk EL, Rose C, Cohen R. Coal mine dust lung disease. New lessons from old exposure. Am J Respir Crit Care Med. 2013;187:1178–85. doi: 10.1164/rccm.201301-0042CI. [DOI] [PubMed] [Google Scholar]
- 16.Tor M, Özturk M, Altın R, Cimrin AH. Working conditions and pneumoconiosis in Turkish coal miners between 1985 and 2004: a report from Zonguldak coal basin, Turkey. Tuberk Toraks. 2010;58:252–60. [PubMed] [Google Scholar]
- 17.Blackley DJ, Crum JB, Halldin CN, et al. Resurgence of progressive massive fibrosis in coal miners - eastern kentucky, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:1385–9. doi: 10.15585/mmwr.mm6549a1. [DOI] [PubMed] [Google Scholar]
- 18.Ergün R, Ergün D, Evcik E, et al. Evaluation of dental technician’s pneumoconiosis using chest X-ray and HRCT: correlation between radiological and functional findings. Turk J Med Sci. 2017;47:252–9. doi: 10.3906/sag-1604-146. [DOI] [PubMed] [Google Scholar]
- 19.Yurdasal B, Bozkurt N, Bozkurt AI, et al. The evaluation of the dust-related occupational respiratory disorders of dental laboratory technicians working in Denizli Province. Ann Thorac Med. 2015;10:249–55. doi: 10.4103/1817-1737.167073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kahraman H, Koksal N, Cinkara M, et al. Pneumoconiosis in dental technicians: HRCT and pulmonary function findings. Occup Med (Lond) 2014;64:442–7. doi: 10.1093/occmed/kqu047. [DOI] [PubMed] [Google Scholar]
- 21.Akgün M, Araz O, Ucar EY, et al. Silicosis appears inevitable among former denim sandblasters: a 4-year follow-up study. Chest. 2015;148:647–54. doi: 10.1378/chest.14-2848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cimrin A, Kömüs N, Karaman C, et al. Pneumoconiosis and work-related health complaints in Turkish dental laboratory workers. Tuberk Toraks. 2009;57:282–8. [PubMed] [Google Scholar]
- 23.Ergün D, Ergün R, Özdemir C, et al. Pneumoconiosis and respiratory problems in dental laboratory technicians: analysis of 893 dental technicians. Int J Occup Med Environ Health. 2014;27:785–96. doi: 10.2478/s13382-014-0301-9. [DOI] [PubMed] [Google Scholar]
- 24.Cimrin A, Erdut Z. General aspect of pneumoconiosis in Turkey. Indian J Occup Environ Med. 2007;11:50–5. doi: 10.4103/0019-5278.34528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sakar A, Kaya E, Celik P, et al. [Evaluation of silicosis in ceramic workers]. Tuberk Toraks. 2005;53:148–55. [In Turkish] [PubMed] [Google Scholar]
- 26.Ozdemir Dogan D, Ozdemir AK, Polat NT, Dal U, Gumus C, Akkurt I. Prevalence of respiratory abnormalities and pneumoconiosis in dental laboratory technicians. Tuberk Toraks. 2010;58:135–41. [PubMed] [Google Scholar]
- 27.Berk S, Dogan DO, Gumus C, et al. Relationship between radiological (X-ray/HRCT), spirometric and clinical findings in dental technicians’ pneumoconiosis. Clin Respir J. 2016;10:67–73. doi: 10.1111/crj.12187. [DOI] [PubMed] [Google Scholar]
- 28.Akkurt İ, Şimşek C, Erdem N, et al. [Pulmonary Findings in Foundry Workers]. Turkiye Klinikleri J Med Sci. 1997;17:28–31. [In Turkish] [Google Scholar]
- 29.Karadağ ÖK, Akkurt İ, Önal B, Altınörs M, Bilir N, Ersoy N, et al. [Silicosis and Respiratory Findings in Quarry Workers]. Tuberk Toraks. 2001;49:73–80. [In Turkish] [Google Scholar]
- 30.Akkaya A, Turgut E, Şahin Ü, Ünlü M, Çetin M. [Investigation of symptoms of respiratory systems, pulmonary function tests, radiological results and free radicals on the querry workers]. Turberk Toraks. 2001;49:64–72. [In Turkish] [Google Scholar]
- 31.Polatlı M, Türkan H, Akdilli A, Çildağ O. [Silicosis Risk in Quartz Workers]. Solunum Hastalıkları. 2001;12:90–5. [In Turkish] [Google Scholar]
- 32.Öztürk A, Cimrin A, Tür M, et al. [Prevalence of silicosis among employees in feldspat and quartz mills and associated factors with silicosis]. Tuberk Toraks. 2012;60:224–9. doi: 10.5578/tt.3684. [In Turkish] [DOI] [PubMed] [Google Scholar]
- 33.Sevinc C, Cimrin AH, Manisali M, et al. Sandblasting under uncontrolled and primitive conditions in Turkey. J Occup Health. 2003;45:66–9. doi: 10.1539/joh.45.66. [DOI] [PubMed] [Google Scholar]
- 34.Cömert M, Yılmaz H, Gebeşoğlu B, Tutkun E, et al. [Evaluation of Risk Factors in Pneumoconiosis Development Among Welders]. Ankara Medical Journal. 2014;14:11–4. doi: 10.17098/amj.73950. [In Turkish] [DOI] [Google Scholar]
- 35.Antao VC, Pinheiro GA. Surveillance for occupational respiratory diseases in developing countries. Semin Respir Crit Care Med. 2015;36:449–54. doi: 10.1055/s-0035-1549456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thomas CR, Kelley TR. A brief review of silicosis in the United States. Environ Health Insights. 2010;4:21–6. doi: 10.4137/EHI.S4628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Akgun M. Denim production and silicosis. Curr Opin Pulm Med. 2016;22:165–9. doi: 10.1097/MCP.0000000000000249. [DOI] [PubMed] [Google Scholar]
- 38.Bayram H, Ghio AJ. Killer jeans and silicosis. Am J Respir Crit Care Med. 2011;184:1322–4. doi: 10.1164/rccm.201108-1440ED. [DOI] [PubMed] [Google Scholar]
- 39.Bakan ND, Ozkan G, Çamsari G, et al. Silicosis in denim sandblasters. Chest. 2011;140:1300–4. doi: 10.1378/chest.10-1856. [DOI] [PubMed] [Google Scholar]
- 40.Cimrin A. ‘Silicosis’ over again; causes and responsibilities. Tuberk Toraks. 2007;55:118–22. [PubMed] [Google Scholar]
- 41.Sahbaz S, Inonu H, Ocal S, et al. Denim sandblasting and silicosis two new subsequent cases in Turkey. Tuberk Toraks. 2007;55:87–91. [PubMed] [Google Scholar]
- 42.Akgun M, Mirici A, Ucar EY, et al. Silicosis in Turkish denim sandblasters. Occup Med (Lond) 2006;56:554–8. doi: 10.1093/occmed/kql094. [DOI] [PubMed] [Google Scholar]
- 43.Akgun M, Gorguner M, Meral M, et al. Silicosis caused by sandblasting of jeans in Turkey: a report of two concomitant cases. J Occup Health. 2005;47:346–9. doi: 10.1539/joh.47.346. [DOI] [PubMed] [Google Scholar]
- 44.Baş HD, Başer K, Nugent K. Silicosis in denim sandblasters in Turkey. Gaziantep Med J. 2016;22:89–94. [Google Scholar]
- 45.Yildiz T, Essizoglu A, Onal S, et al. Quality of life, depression and anxiety in young male patients with silicosis due to denim sandblasting. Tuberk Toraks. 2011;59:120–5. doi: 10.5578/tt.1606. [DOI] [PubMed] [Google Scholar]
- 46.Sauvé JF. Historical and emerging workplaces affected by silica exposure since the 1930 Johannesburg conference on Silicosis, with special reference to construction. Am J Ind Med. 2015;58:67–71. doi: 10.1002/ajim.22507. [DOI] [PubMed] [Google Scholar]
- 47.Köksal N, Kahraman H. Acute silicosis in teflon-coated pan manufacturing due to metal sandblasting. Int J Occup Environ Health. 2011;17:210–3. doi: 10.1179/oeh.2011.17.3.210. [DOI] [PubMed] [Google Scholar]
- 48.Sari G, Simsek C, Gulgosteren S, et al. Accelerated Silicosis in Teflon-Coated Pan Manufacturing: Case Report. Am J Respir Crit Care Med. 2017;195:A5963. [Google Scholar]
- 49.Talay F, Gurel K, Gurel S, et al. Silicosis in manufacture of electric cable: report of four cases. J Occup Health. 2007;49:405–10. doi: 10.1539/joh.49.405. [DOI] [PubMed] [Google Scholar]


